Abstract
Abstract
Purpose of Review
Several studies have found that medical students have a significant prevalence of sleep issues, such as poor sleep quality, excessive daytime sleepiness, and inadequate sleep duration. The purpose of this review is to carefully evaluate the current research on sleep problems among medical students and, as a result, estimate the prevalence of these disturbances. The EMBASE, PsychINFO, PubMed/MEDLINE, ScienceDirect, Scopus, and Web of Science and retrieved article reference lists were rigorously searched and rated for quality. Random effects meta-analysis was performed to compute estimates.
Recent Findings
The current meta-analysis revealed an alarming estimated pooled prevalence of poor sleep quality (K = 95, N = 54894) of 55.64% [95%CI 51.45%; 59.74%]. A total of 33.32% [95%CI 26.52%; 40.91%] of the students (K = 28, N = 10122) experienced excessive sleepiness during the day. The average sleep duration for medical students (K = 35, N = 18052) is only 6.5 h per night [95%CI 6.24; 6.64], which suggests that at least 30% of them get less sleep than the recommended 7–9 h per night.
Summary
Sleep issues are common among medical students, making them a genuine problem. Future research should focus on prevention and intervention initiatives aimed at these groups.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40675-023-00258-5.
Keywords: Excessive daytime sleepiness, COVID-19, Sleep, Medical students, Pittsburgh sleep quality index, Insomnia, Project registration: Open Science Framework Identifier: DOI 10.17605/OSF.IO/UVH5C
Introduction
Sleep is, without question, one of the most important physiological activities for the human body to function correctly and is essential to maintaining the human body’s health and well-being. Insufficient sleep has negative effects on cardiovascular diseases [1–3] neurocognitive function [4–7], psychological disorders [8–10], metabolic abnormalities [11–13] immunological response [14–16], and academic performance [17, 18].
According to both the National Sleep Foundation and the American Academy of Sleep Medicine, it is recommended that adults obtain 7–9 h of sleep every night, while the recommendation for school-aged children and teens is get up to 11 h [19–21]. Despite this, several studies have demonstrated that sleep disturbances are more frequent than we realize. For example, a 2020 research study in Australia of 836 participants revealed that 41% of females and 42% of males have sleep problems. Another study in Turkey with 5021 participants found that more than half (53%) of the individuals had sleep disturbances [22].
Because admission to medical school requires high academic and professional achievement, it is regarded as one of the most demanding professions. As a result, stress and psychological state are important factors that might impair sleep quality and quantity [10, 23], and medical students as a group are particularly stressed. It is expected that they are prone to numerous forms of sleep problems. Sleep disruption is described as a pandemic in the population of medical students compared to the general population [24], with particular reports of falling asleep late and having difficulty initiating sleep, as well as sleeping fewer hours [20, 24, 25]. It has also been found that using mobile phones and watching television are highly linked to sleep-related difficulties in medical students [26–28].
Due to the demanding nature of medical school and the possible consequences of poor sleep on outcomes in academics, clinical care, and mental health, sleep quality is a crucial concern for medical students. High academic demands, long study and clinical hours, and other factors that can cause sleep disturbances and sleep disorders are faced by medical students [29, 30].
Poor sleep hygiene can have an adverse effect on patient care and safety by lowering cognitive function, judgment, and clinical abilities [29, 30]. Additionally, sleep disorders and disturbances can worsen mental health conditions like depression, anxiety, and burnout as well as raise the risk of developing chronic illnesses like diabetes and cardiovascular disease [29, 30]. The importance of sleep health in medical students can enhance their performance in the classroom and in the clinic, enhance general wellbeing, and have a beneficial impact on future healthcare outcomes [29, 30].
The ongoing global COVID-19 pandemic, which the WHO proclaimed in March 2020, has had a profound impact on many facets of everyday life. Wearing masks, social distancing, travel limitations, shift to online instruction, and quarantine were all undertaken to minimize the virus’ spread. In addition, students encountered a radically new daily schedule after switching to online learning, which altered their learning experience, sleep patterns, and social connections.
There are several meta-analyses being conducted on sleep difficulties in the medical student community [24, 29–31]. However, there has been limited data on the influence of COVID-19 on sleep problems among medical students. As a result, this study aims to determine the prevalence of sleep problems among medical students during the COVID-19 pandemic using data from international English language studies.
It is crucial to examine sleep issues among medical students before and after COVID-19 for a number of reasons. First, it is widely recognized that medical students are more susceptible to sleep disorders and poor sleep quality, both of which can have a detrimental effect on their academic performance, clinical abilities, and general well-being [32–34]. Second, because of adjustments in their academic and clinical training, medical students have been profoundly impacted by the COVID-19 pandemic [29, 35–37]. Online learning and virtual clinical encounters have required medical students to adjust, which may have affected their sleep habits and quality. Additionally, medical students have been involved in the care of COVID-19 patients, which might have contributed to their increased stress levels and poorer quality sleep [36]. Researchers can learn more about the possible effects of these changes on medical students' academic and clinical performance by examining how the epidemic has affected their sleep habits and sleep disorders.
Methodology
PRISMA 2020 (Preferred Reporting Items for Systematic Review and Meta-analysis) criteria were followed for this systematic review and meta-analysis [38]. The project was registered on the open science framework (OSF), identifier: DOI 10.17605/OSF.IO/UVH5C.
Information Sources and Search Strategy
From the inception to January 15, 2023, three authors (MBJ, ISA, RAA) independently conducted a systematic literature search utilizing five electronic databases (EMBASE, PsychINFO, PubMed/MEDLINE, ScienceDirect, Scopus, and Web of Science).
We broadened our search by consulting additional sources (i.e., backward, and forward citation tracking of all included articles). After removing duplicates, two authors (any two of MBJ, ISA, RAA, YSI) independently examined titles, abstracts, tables, and graphs in the first screening stage, and completed texts in the second eligibility step to determine whether publications satisfied eligibility requirements. Consensus was used to settle disagreements between any two judges.
The following keywords were used in the search strategy: 'medical student' AND 'sleep dis*' OR 'sleep issue(s)' OR 'sleep quality' OR 'sleep length**' OR 'excessive daytime sleepiness' OR 'sleep disorder' OR 'sleep habit' OR 'sleep hygiene'. The * included disruption and disturbance; and the ** included variants of the keyword length including duration, sufficient, and insufficient. Only English-language research publications were considered. However, the characteristics of the subjects were not restricted.
Data Collection Process and Eligibility Criteria
Two authors (any two of MBJ, ISA, RAA, YSI) screened the title and abstract of all studies found in the systematic search to identify studies that met our criteria for inclusion in the meta-analysis. The inclusion criteria were as follows: (1) research published in the English language, (2) date of publication from the inception of the database until the second week of January 2023, (3) medical students as the targeted population, (4) reported data on the prevalence of sleep disturbance using a validated, commonly utilized measurement tool.
Our exclusion criteria included the following: (1) case reports and case series; (2) studies that reported results for medical students with non-medical students in the same group but did not provide a subgroup analysis; (3) lack of study availability and inability to obtain the full text after contacting the authors; and (4) studies that concentrated on particular sleep disorders (e.g., sleep apnea, insomnia, etc.) among medical students.
Outcomes Measures
The population, intervention, comparison, and outcome design (PICO) [39] method dictated the following inclusion criteria: population; (1) medical students; (2)intervention/exposure; sleep issues; (3) comparison; none;( 4) outcomes; poor sleep quality, increased daytime drowsiness, and sleep duration.
The predicted results from this systematic review and meta-analysis were to conduct the prevalence of sleep disturbance among medical students during the COVID-19 pandemic. Thus, we used the following specific measure: (1) the Pittsburgh Sleep Quality Index (PSQI) [40] to determine the score and the corresponding prevalence of poor sleep quality as measured by the index, subjects with PSQI overall score greater than five are considered poor sleepers [40]; (2) the Epworth Sleepiness Scale (ESS) to determine the prevalence of excessive[41]; (3) the reported mean duration of sleep per night. Finally, (4) age, gender, country, and the COVID-19 pandemic were covariates/factors of sleep quality and excessive daytime sleepiness among medical students.
The Pittsburgh Sleep Quality Index (PSQI) [40]. The PSQI assesses sleep quality by examining seven core areas over the preceding month: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction [40]. After assessing these components, the PSQI provides a composite score on a 0 to 21-point scale to evaluate sleep quality, a score of 5 or higher indicates poor overall sleep quality [40].
The Epworth Sleepiness Scale (ESS) assesses the level of daytime sleepiness by asking patients to rate their likely sleepiness on a four-point scale in eight different situations [41]. This results in a “sleepiness score” between 0 and 24, with higher numbers indicating greater sleepiness [41]. The ESS is a sensitive tool that can provide insight into how a patient’s sleepiness is affecting their daily life, a score of 11 or higher indicating excessive daytime sleepiness (EDS) [41].
Data Extraction
Following the research selection procedure, two reviewers (any two of MBJ, ISA, RAA, YSI) retrieved data from the original studies separately. Extracted data comprised basic features such as the date of publication and the geographical location of the study. The following demographic information was extracted: age and sex (proportion of males); data on sleep quality, sleep duration, and daytime sleepiness, as well as the evaluation technique utilized. Disagreements between reviewers were solved by consulting a third reviewer (HJ).
Quality Evaluation (Risk of Bias Assessment)
The study quality was assessed using the Newcastle-Ottawa scale (NOS) [42]. Each study received a quality score based on the groups included in the study, comparability, and assessment of the result and exposure. Overall scores varied from 0 to 9, with 0–4, 5–7, and more than 8 indicating low, moderate, and high-risk of bias studies, respectively. Based on the quality ranking, no studies were omitted. Two authors (any two of MBJ, ISA, RAA, YSI) rated the risk of bias separately, and differences between the two judges were addressed by discussion with HJ.
Data Analysis
Using the meta [43] and metafor [44] packages in R, version 4.2.2, the analysis was conducted [45]. A random-effects model was used for estimating poor sleep quality, EDS, and average sleep duration pooled prevalence rates. We reported point estimates and the corresponding 95% confidence intervals (95% CI) [46]. We calculated the pooled results using the inverse variance method with DerSimonian-Laird estimator to calculate the heterogeneity variance τ2 and Jackson method for confidence intervals of τ2 and τ. The Hartung-Knapp adjustment was applied to address uncertainty in estimating the between-study variance. To facilitate the presentation of the results, we presented results visually in forest plot format using the package forester [47]. We used the sensitivity analysis termed as “one study eliminated,” which examines what impact does each included study have on the total effect estimate [48].
Egger’s test [49] for funnel plot [49] asymmetry and Begg’s rank correlation [50] were used to determine publication bias. Statistically significant publication bias was adjusted for by using the trim-and-fill method [51]. Cochran's Q [52] and I2 [53, 54] statistics were used to test for between-study heterogeneity, with I2 values of 25%, 50%, and 75% reflecting low, moderate, and high levels of heterogeneity, respectively [53, 54]. To further aid interpreting heterogeneity, we computer predicted intervals (PI). A prediction interval is a group of values that is likely to include the value of a single new observation given the predictors’ preset parameters. For example, we can be 95% certain that the next new (i.e., future) observation will fall inside a 95% prediction interval (95% PI) [55].
We performed subgroup analyses using random-effects models to identify possible sources of heterogeneity based on study location (i.e., country) and COVID-19 status (pre- vs. during- COVID-19) [55]. To determine whether subgroup differences can be explained solely by sampling error, Q tests were conducted. The mean age and sex (proportion of males) of each estimate were corrected using meta-regressions under random-effects models [55, 56].
Results
Descriptive Results
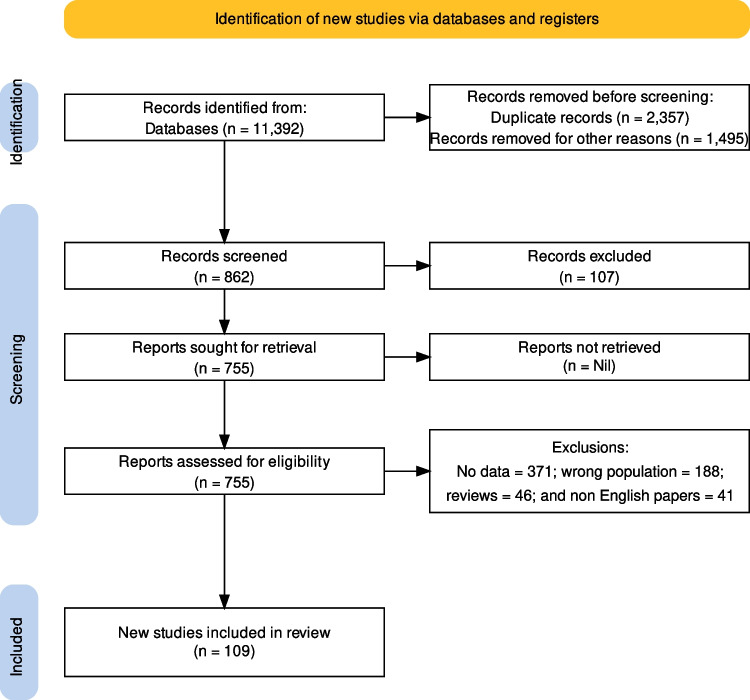
The electronic database search identified a total of 862 studies after removing duplicates and automated screening. The selection process described in Fig. 1 resulted in 109 qualified studies for this meta-analysis. All the studies were published after the year 2000 (i.e., 2001–2023), with a total of 59,427 participants from 31 countries. Detailed results are shown in Table 1.
Fig. 1.
PRISMA 2020 flow diagram for study selection
Table 1.
Characteristics of the included studies
| SN | Ref | Study | Country | Sample size | Sex (%Male) | Age (Years) | Sleep parameters | COVID19 | Risk of bias (NOS) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | [107] | Abdali et al., 2019 | Iran | 400 | 42.8 | 22.4 | SQ | No | Low | ||
| 2 | [64] | Abdulghani et al., 2012 | KSA | 491 | 37.5 | 24.4 | EDS | No | Low | ||
| 3 | [100] | Al Khani et al., 2019 | KSA | 200 | 76 | 20.8 | SQ | No | Moderate | ||
| 4 | [92] | Al Otaibi et al., 2020 | KSA | 282 | 64.5 | 21 | SQ | No | Moderate | ||
| 5 | [108] | Al Shammari et al., 2020 | KSA | 180 | 36 | NR | EDS | SQ | SD | No | Moderate |
| 6 | [109] | Al Sulami et al., 2019 | KSA | 702 | 41.6 | 21.34 | SQ | SD | No | Low | |
| 7 | [59] | Almojali et al., 2017 | KSA | 263 | 68.8 | 21.9 | SQ | SD | No | Moderate | |
| 8 | [110] | Alnomsi et al., 2018 | KSA | 169 | 48.5 | 22.9 | SQ | SD | No | Moderate | |
| 9 | [111] | AlQahtani et al., 2017 | KSA | 237 | 61.2 | 22 | EDS | No | Moderate | ||
| 10 | [60] | Alsaggaf et al., 2016 | KSA | 305 | 41.6 | 22 | EDS | SQ | SD | No | Moderate |
| 11 | [112] | Alshahrani et al., 2019 | KSA | 225 | NR | NR | EDS | SQ | No | Moderate | |
| 12 | [27] | Amiri et al., 2020 | Iran | 300 | 55 | 21.94 | SQ | No | Moderate | ||
| 13 | [113] | Asiri et al., 2018 | KSA | 286 | 63.6 | 22.4 | SQ | SD | No | Moderate | |
| 14 | [114] | Atlam et al., 2020 | Egypt | 899 | 66 | 21.98 | EDS | No | Low | ||
| 15 | [115] | Attal et al., 2021 | Yemen | 240 | 41 | 23.3 | SQ | SD | No | Moderate | |
| 16 | [77] | Awasthi et al., 2020 | India | 221 | 23 | 20.24 | SQ | No | Moderate | ||
| 17 | [116] | BaHammam et al., 2005 | KSA | 129 | 50 | 21.2 | EDS | SD | No | Moderate | |
| 18 | [117] | Belingheri et al., 2020 | Italy | 215 | NR | NR | EDS | No | Moderate | ||
| 19 | [95] | Bogati et al., 2020 | India | 350 | 57 | 21.97 | SQ | No | Moderate | ||
| 20 | [118] | Brick et al., 2010 | USA | 314 | 42.4 | 27.8 | SQ | No | Moderate | ||
| 21 | [74] | Brubaker et al., 2020 | USA | 287 | 49 | 24.8 | SQ | SD | No | Moderate | |
| 22 | [119] | Carpi et al., 2022 | Italy | 407 | 16.2 | 24.2 | SQ | SD | Yes | Low | |
| 23 | [120] | Chatterjee et al., 2021 | India | 224 | 46.42 | 21.085 | SQ | No | Moderate | ||
| 24 | [97] | Chen et al., 2022 | China | 1227 | 48.4 | NR | SQ | Yes | Moderate | ||
| 25 | [121] | Christodoulou et al., 2021 | France | 177 | 36.2 | NR | SQ | No | Moderate | ||
| 26 | [122] | Copaja-Corzo et al., 2022 | Peru | 3139 | 38.9 | NR | SQ | Yes | Moderate | ||
| 27 | [123] | Correa et al., 2017 | Brazil | 372 | 37.1 | 21.3 | SQ | No | Moderate | ||
| 28 | [124] | Dhamija et al., 2021 | India | 499 | 38 | 20 | SQ | Yes | Low | ||
| 29 | [97] | Ding et al., 2022 | China | 1524 | 40.9 | 19.9 | SQ | SD | Yes | Low | |
| 30 | [125] | Dudo et al., 2022 | Germany | 1103 | 35 | NR | SQ | SD | No | Moderate | |
| 31 | [62] | ElArab et al., 2014 | Egypt | 435 | 48.5 | 21.4 | EDS | No | Low | ||
| 32 | [126] | Eleftheriou et al., 2021 | Greece | 559 | 30.2 | NR | SQ | Yes | Moderate | ||
| 33 | [127] | Elwasify et al., 2016 | Egypt | 1182 | 32.3 | 21.4 | SQ | No | Low | ||
| 34 | [128] | Ergin et al., 2021 | Turkey | 127 | NR | NR | SQ | No | Moderate | ||
| 35 | [58] | Fawzy and Hamed 2017 | Egypt | 700 | 35.4 | 21.22 | SQ | SD | No | Low | |
| 36 | [129] | Feng et al., 2022 | China | 450 | 38.7 | NR | SQ | No | Moderate | ||
| 37 | [130] | Fernandes et al., 2022 | Brazil | 142 | 27.27 | 22.01 | SQ | Yes | Moderate | ||
| 38 | [131] | Fowler et al., 2022 | USA | 41 | 24.3 | 23.94 | SQ | SD | Yes | High | |
| 39 | [78] | Giri et al., 2013 | India | 150 | 40 | 22.4 | EDS | No | High | ||
| 40 | [57] | Gladius et al., 2018 | India | 203 | 40.4 | 21.3 | SQ | No | Moderate | ||
| 41 | [132] | Gui et al., 2022 | China | 2646 | 44.4 | 20.13 | SQ | No | Low | ||
| 42 | [81] | Guo et al., 2022 | China | 72 | 43 | 23.9 | SQ | Yes | High | ||
| 43 | [133] | Gupta et al., 2020 | India | 222 | 68.5 | 20.73 | SQ | No | Moderate | ||
| 44 | [134] | Ibrahim et al., 2017 | KSA | 576 | 35.8 | 21 | EDS | SQ | No | Moderate | |
| 45 | [135] | James et al., 2011 | Nigeria | 255 | 49 | 24.45 | SQ | No | Moderate | ||
| 46 | [136] | Javaid et al., 2020 | Pakistan | 810 | 30.4 | 21.35 | EDS | SQ | SD | No | Low |
| 47 | [137] | Jniene et al., 2019 | Morocco | 294 | 38.8 | 20.6 | SQ | SD | No | Moderate | |
| 48 | [138] | Johnson et al., 2017 | USA | 307 | 35.8 | 26.4 | EDS | No | Moderate | ||
| 49 | [139] | Kalyani et al., 2017 | Iran | 278 | 34.9 | 19.88 | SQ | No | Moderate | ||
| 50 | [86] | Kang and Chen et al., 2009 | China | 160 | 50.6 | 20.3 | EDS | SQ | SD | No | Moderate |
| 51 | [140] | Kawyannejad et al., 2019 | Iran | 321 | 39.9 | 22.03 | SQ | No | Moderate | ||
| 52 | [141] | Khero et al., 2019 | Pakistan | 281 | 26.33 | NR | SQ | No | Moderate | ||
| 53 | [142] | Kumar et al., 2019 | India | 150 | 41.3 | NR | SQ | No | Moderate | ||
| 54 | [143] | Kumar et al., 2016 | India | 308 | 57.1 | 21.4 | SQ | No | Moderate | ||
| 55 | [93] | Lamoria et al., 2020 | India | 170 | NR | 20.48 | SD | No | Moderate | ||
| 56 | [28] | Lawson et al., 2019 | Ghana | 153 | 45.8 | 23.1 | SQ | SD | No | Moderate | |
| 57 | [144] | Li et al., 2022 | China | 364 | 43 | 20.1 | SQ | No | Moderate | ||
| 58 | [145] | Lima et al., 2002 | Brazil | 27 | 48.1 | 20.2 | SQ | SD | No | High | |
| 59 | [146] | Mahadule et al., 2022 | India | 101 | 71 | 20.18 | EDS | SQ | Yes | Moderate | |
| 60 | [147] | Maheshwari et al., 2019 | Pakistan | 797 | 33.37 | NR | SQ | SD | No | Moderate | |
| 61 | [98] | Mahgoub et al., 2022 | Sudan | 273 | NR | NR | SQ | Yes | Moderate | ||
| 62 | [148] | Mazar et al., 2021 | Israel | 87 | 41 | 25.86 | EDS | SQ | No | High | |
| 63 | [73] | Mazurkiewicz et al., 2012 | USA | 86 | 25.6 | 21.8 | SQ | No | High | ||
| 64 | [65] | Medeiros et al., 2001 | Brazil | 36 | 58 | 20.7 | SQ | SD | No | High | |
| 65 | [25] | Meer et al., 2022 | UAE | 96 | 21.9 | 20 | SQ | SD | No | High | |
| 66 | [149] | Meo et al., 2022 | KSA | 410 | NR | NR | SQ | SD | Yes | Moderate | |
| 67 | [75] | Mirghani et al., 2015 | Sudan | 140 | NR | NR | SD | No | Moderate | ||
| 68 | [150] | Mirghani et al., 2017 | Sudan | 140 | 27.9 | 22.8 | SQ | No | Moderate | ||
| 69 | [151] | Mishra et al., 2022 | India | 284 | 40.5 | 20.6 | SQ | SD | Yes | Moderate | |
| 70 | [152] | Mohammadbeigi et al., 2016 | Iran | 363 | 30.3 | 21.8 | SQ | No | Moderate | ||
| 71 | [76] | Mokros et al., 2017 | Poland | 140 | 50 | 21.3 | SQ | No | Moderate | ||
| 72 | [79] | Nadeem et al., 2018 | Pakistan | 362 | 40 | 19.57 | SQ | No | Moderate | ||
| 73 | [153] | Nsengimana et al., 2023 | Rwanda | 290 | 58.3 | 24 | SQ | Yes | Moderate | ||
| 74 | [154] | Olarte-Durand et al., 2021 | Peru | 310 | 37.7 | 21.6 | SQ | Yes | Moderate | ||
| 75 | [72] | Pagnin et al., 2014 | Brazil | 127 | 44.9 | 21.3 | EDS | SQ | No | Moderate | |
| 76 | [155] | Patil et al., 2019 | India | 463 | 38.2 | 19.55 | SQ | No | Low | ||
| 77 | [83] | Perotta et al., 2021 | Brazil | 1350 | 47.1 | 22.8 | EDS | SQ | No | Low | |
| 78 | [156] | Prashanth et al., 2015 | India | 503 | 48.1 | 21.8 | EDS | No | Low | ||
| 79 | [157] | Priya et al., 2017 | India | 307 | 76.5 | 20.5 | EDS | SQ | No | Moderate | |
| 80 | [158] | Ramamoorthy et al., 2014 | India | 121 | 53.7 | 21.8 | EDS | No | Moderate | ||
| 81 | [67] | Rasekhi et al., 2016 | Iran | 177 | 46.9 | 20.99 | SQ | SD | No | Moderate | |
| 82 | [159] | Rathi et al., 2018 | India | 160 | 55.6 | 20.93 | SQ | No | Moderate | ||
| 83 | [160] | Rique et al., 2013 | Brazil | 221 | 55.7 | 22.3 | EDS | SQ | No | Moderate | |
| 84 | [161] | Riskawati et al., 2022 | Indonesia | 444 | 32 | 21 | EDS | SQ | No | Low | |
| 85 | [162] | Safhi et al., 2020 | KSA | 326 | 50.6 | 21.86 | SQ | No | Moderate | ||
| 86 | [163] | Saguem et al., 2021 | Tunisia | 251 | 17.5 | NR | SQ | Yes | Moderate | ||
| 87 | [88] | Sahraian and Javadpour 2010 | Iran | 159 | 49.7 | 21.52 | SQ | No | Moderate | ||
| 88 | [164] | Sarbazvatan et al., 2017 | Iran | 80 | 50 | 19.2 | SQ | SD | No | High | |
| 89 | [99] | Satti et al., 2019 | Pakistan | 219 | 43 | NR | SQ | No | Moderate | ||
| 90 | [165] | Saygin et al., 2016 | Turkey | 337 | 42.1 | 21.3 | EDS | SQ | SD | No | Moderate |
| 91 | [166] | Shadzi et al., 2020 | Iran | 402 | 49.7 | 22.4 | SQ | No | Low | ||
| 92 | [96] | Shafique et al., 2021 | Pakistan | 100 | 49 | 21.13 | SQ | Yes | Moderate | ||
| 93 | [167] | Shrestha et al., 2021 | Nepal | 168 | 64.29 | 21.57 | SQ | SD | Yes | Moderate | |
| 94 | [94] | Siddiqui et al., 2016 | KSA | 318 | 64.8 | 22.35 | SQ | SD | No | Moderate | |
| 95 | [89] | Soakin et al., 2019 | Georgia | 44 | 50 | 21.62 | EDS | No | High | ||
| 96 | [168] | Sun et al., 2019 | China | 5497 | 32.7 | 20.2 | SQ | No | Low | ||
| 97 | [169] | Sundas et al., 2020 | Nepal | 217 | 47.5 | 21.39 | SQ | SD | No | Moderate | |
| 98 | [170] | Surani et al., 2015 | Pakistan | 504 | 40.5 | 20 | EDS | SQ | No | Low | |
| 99 | [171] | Tahir et al., 2021 | Multiple | 2749 | 36 | NR | SQ | Yes | Moderate | ||
| 100 | [90] | Teimouri et al., 2021 | Iran | 290 | 40 | NR | SQ | No | Moderate | ||
| 101 | [172] | Thaipisuttikul et al., 2022 | Thailand | 165 | 58.2 | 20.77 | EDS | SQ | SD | No | Moderate |
| 102 | [173] | Wang et al., 2020 | China | 3738 | 41.52 | 18.8 | SQ | No | Low | ||
| 103 | [174] | Wang et al., 2016 | China | 6085 | 27.3 | 21.3 | SQ | SD | No | Low | |
| 104 | [61] | Waqas et al., 2015 | Pakistan | 263 | 43.7 | 21.1 | SQ | No | Moderate | ||
| 105 | [175] | Wondie et al., 2021 | Ethiopia | 576 | 53.8 | 21.5 | SQ | No | Low | ||
| 106 | [176] | Xie et al., 2020 | China | 1026 | 36.4 | 21.375 | SQ | Yes | Low | ||
| 107 | [177] | Yazdi et al., 2016 | Iran | 285 | 47.4 | 22.8 | SQ | No | Moderate | ||
| 108 | [178] | Yeluri et al., 2021 | India | 398 | 49.1 | NR | SQ | No | Moderate | ||
| 109 | [84] | Zailinawati et al., 2009 | Malaysia | 792 | 41 | 20.8 | EDS | SD | No | Low | |
EDS, excessive daytime sleepiness measured using Epworth sleepiness scale; NOS, The Newcastle-Ottawa Scale for rating nonrandomized research in meta-analyses; NR, not reported; SD, sleep duration measured in hours; SQ, sleep quality measured using Pittsburg sleep quality index
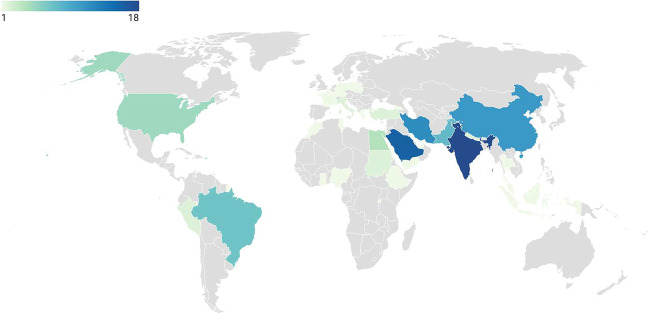
The countries included Brazil (K = 7), China (K = 11), Egypt (K = 4), Ethiopia (K = 1), France (K = 1), Georgia (K = 1), Germany (K = 1), Ghana (K = 1), Greece (K = 1), India (K = 18), Indonesia (K = 1), Iran (K = 12), Israel (K = 1), Italy (K = 2), Kingdom of Saudi Arabia (KSA, K = 16), Malaysia (K = 1), Morocco (K = 1), Multiple countries (K = 1), Nepal (K = 2), Nigeria (K = 1), Pakistan (K = 8), Peru (K = 2), Poland (K = 1), Rwanda (K = 1), Sudan (K = 2), Thailand (K = 1), Tunisia (K = 1), Turkey (K = 2), UAE (K = 1), USA (K = 5), and Yemen (K = 1). K denotes the number of studies per country. The four countries providing the most studies were India (K = 18, 16.5%), KSA (K = 16, 14.67%), Iran (K = 12, 11.01%), and China (K = 11, 10.1%). Figure 2 shows the distribution of the studies worldwide.
Fig. 2.
Distribution of studies worldwide
The mean number of participants per study was 545 (range 27–6085), and their mean age was 21.6 (range 18.8–27.8 years); 44.2% of the participants were males. The Newcastle-Ottawa Scale was used to assess the quality of the assessment and the risk of bias (NOS). Eighty-five percent of the studies were of high or moderate quality. Figure 3 shows that the selection dimension, specifically the sample size and representativeness, exhibits the greatest risk bias. Supplemental Fig. 1 presents a thorough analysis of the quality rating for each study analyzed in the meta-analysis.
Fig. 3.
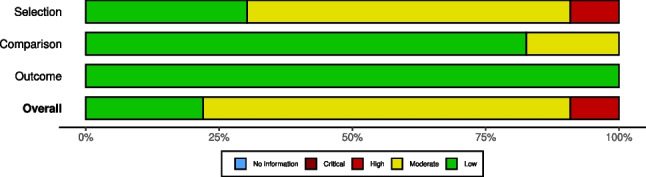
Summary of the included studies
Narrative Summary of the Literature About Sleep Problems Among Medical Students
Research has repeatedly shown that sleep issues are quite common among medical students [32, 35]. It was noted that about 50–60% of them had poor sleep, with female students more likely to have it. This rate is higher than that of the general population and other college students [29].
The high prevalence of sleep difficulties among medical students is the result of several factors. These factors include increased academic workload, shift work and unpredictable schedules, lifestyle factors, and mental health issues. According to previous research, among these factors are as follows: (1) Increased academic workload: Medical students must complete a demanding academic program that necessitates extended study sessions and clinical responsibilities [57–61]. Increased stress and anxiety can have a negative impact on sleep quality because of the pressure to perform well in school and the fear of failing [17, 62–67]. (2) Shift work and unpredictable schedules: Clinical rotations and on-call responsibilities are frequent among medical students, which might disturb their sleep cycles [68]. Their unpredictable schedules may cause circadian rhythm abnormalities and poor sleep as a result [35, 41, 69]. (3) Lifestyle factors: Medical students may develop harmful behaviors to deal with their demanding schedules, such as excessive caffeine use and inconsistent eating times [70, 71]. (4) Mental health: High levels of stress, burnout, and depression are regularly reported by medical students, which can make it difficult to fall asleep [32, 72, 73]. Poor sleep can exacerbate mental health problems and vice versa due to the bidirectional association between sleep and mental health [32, 72–74].
The effects of sleep disturbances on medical students can be severe, with a variety of potential repercussions. Academic performance can be harmed by sleep deprivation because it has been demonstrated to impede cognitive function, memory consolidation, and learning ability [17, 57, 60, 62–67, 75]. Mental health can suffer as sleep disturbances are linked to an increased risk of anxiety, depression, and burnout. This vicious cycle can make sleep issues worse by increasing the risk of these mental health issues [60, 76, 77]. Physical health can be impaired as chronic sleep loss has been linked to a number of physical health issues, including as obesity, diabetes, and heart disease [29, 78]. Finally, the ability to deliver patient care can be compromised as medical students who have sleep issues may be more likely to make mistakes with patient safety and care delivery [32, 72–74].
Prevalence of Poor Sleep Quality
A random effects meta-analysis of all the available studies evaluated sleep quality in medical students (K = 95, N = 54894). The overall pooled prevalence rate of sleep quality was 55.64% 95% CI [51.45%; 59.74%], with statistically significant evidence of between-study heterogeneity τ2 = 0.69 [0.47; 0.93]; τ = 0.83 [0.69; 0.90]; I2 = 98.8% [98.7%; 98.9%]; H = 9.08 [8.74; 9.45]; 95% PI [19.26%; 86.83%]. Neither age nor sex explained heterogeneity in sleep quality. Detailed results are shown in Table 2.
Table 2.
A meta-analysis of sleep problems in medical students
| Analysis | K | N | Random effects model | Heterogeneity | Moderators | Publication bias | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pooled results [95% CI] | Forest plot | I2 | τ | τ2 | H | Q | Cochran's Q P-valued | Age (Years) | Sex (%Male) | Egger's test | Peter's test | |||
| PSQI | ||||||||||||||
| All studies | 95 | 54894 | 55.64% [51.45%; 59.74%] | Figure 4 | 98.8% | 0.83 | 0.69 | 9.08 | 7757.02 | 0.001 | - | - | NS | NS |
| Iran | 11 | 3055 | 55.26% [47.01%; 63.23%] | Not shown | 93.1% | 0.45 | 0.2 | - | 145.29 | 0.001 | - | - | NS | NS |
| Kingdom of Saudi Arabia | 13 | 4242 | 54.94% [37.31%; 71.42%] | 98.7% | 1.13 | 1.28 | - | 925.43 | - | - | NS | NS | ||
| India | 14 | 3890 | 56.1% [45.49%; 66.17%] | 96.3% | 0.65 | 0.43 | - | 351.17 | - | - | NS | NS | ||
| United States of America | 4 | 728 | 61.57% [18.83%; 91.71%] | 97.6% | 1.23 | 1.51 | - | 124.2 | - | - | NS | NS | ||
| China | 11 | 22789 | 41.25% [31.55%; 51.68%] | 99.3% | 0.57 | 0.33 | - | 1335.79 | - | - | NS | NS | ||
| Brazil | 7 | 2275 | 56.67% [41.77%; 70.45%] | 93.5% | 0.52 | 0.27 | - | 92.78 | - | - | NS | NS | ||
| Pakistan | 8 | 3336 | 56.73% [41.15%; 71.08%] | 98.4% | 0.83 | 0.7 | - | 426.32 | - | - | NS | NS | ||
| Pre COVID-19 | 75 | 41322 | 53.83% [49.05%; 58.55%] | Figure Supplemental 4 | 98.5% | 0.75 | 0.57 | - | 4852.67 | 0.001 | - | - | NS | NS |
| During COVID-19 | 20 | 13572 | 62.11 % [53.51%; 70.01%] | 98.7% | 0.76 | 0.57 | - | 1422.64 | - | - | NS | NS | ||
| ESS | ||||||||||||||
| All studies | 28 | 10122 | 33.32% [26.52%; 40.91%] | Figure 5 | 96.2% | 0.59 | 0.34 | 5.13 | 709.37 | 0.001 | - | - | NS | NS |
| Kingdom of Saudi Arabia | 7 | 2148 | 40.64% [29.91%; 52.35%] | Not shown | 91.7% | 0.4 | 0.16 | - | 72.18 | 0.001 | - | - | NS | NS |
| India | 5 | 1082 | 28.56% [12.16%; 53.6%] | 96.3% | 0.89 | 0.79 | - | 108.65 | - | - | NS | NS | ||
| Pre COVID-19 | 27 | 10021 | 32.62% [25.79%; 40.27%] | Supplemental 7 | 96.3% | 0.58 | 0.34 | - | 695.54 | 0.011 | - | - | NS | NS |
| During COVID-19 | 1 | 101 | 54.46% [44.7%; 63.88%] | - | - | - | - | 0.1 | - | - | NS | NS | ||
| Sleep duration (SD) | ||||||||||||||
| All studies | 35 | 18052 | 6.44% [6.24%; 6.64%] | Figure 6 | 99.2% | 0.59 | 0.35 | 11.07 | 4168.9 | 0.001 | - | - | NS | NS |
| Kingdom of Saudi Arabia | 9 | 2762 | 5.85% [5.6%; 6.09%] | Not Shown | 95.3% | 0.35 | 0.12 | - | 171.69 | 0.001 | - | - | NS | NS |
| Pre COVID-19 | 29 | 15218 | 6.33% [6.14%; 6.52%] | Supplemental 10 | 98.7% | 0.5 | 0.25 | - | 2104.54 | 0.001 | - | - | NS | NS |
| During COVID-19 | 6 | 2834 | 6.97% [6.17%; 7.76%] | 99.7% | 0.99 | 0.98 | - | 1727.44 | - | - | NS | NS | ||
EES, Epworth sleepiness scale to measure excessive daytime sleepiness; NS, not significant; PSQI, Pittsburg sleep quality index to measure sleep quality; SD, sleep duration measured in hours
Using the PSQI to measure sleep quality in medical students, the raw prevalence estimates for poor sleep quality varied from 12.6 to 92%. The forest plot of the meta-analysis of sleep disturbances in all populations using PSQI is shown in Fig. 4.
Fig. 4.
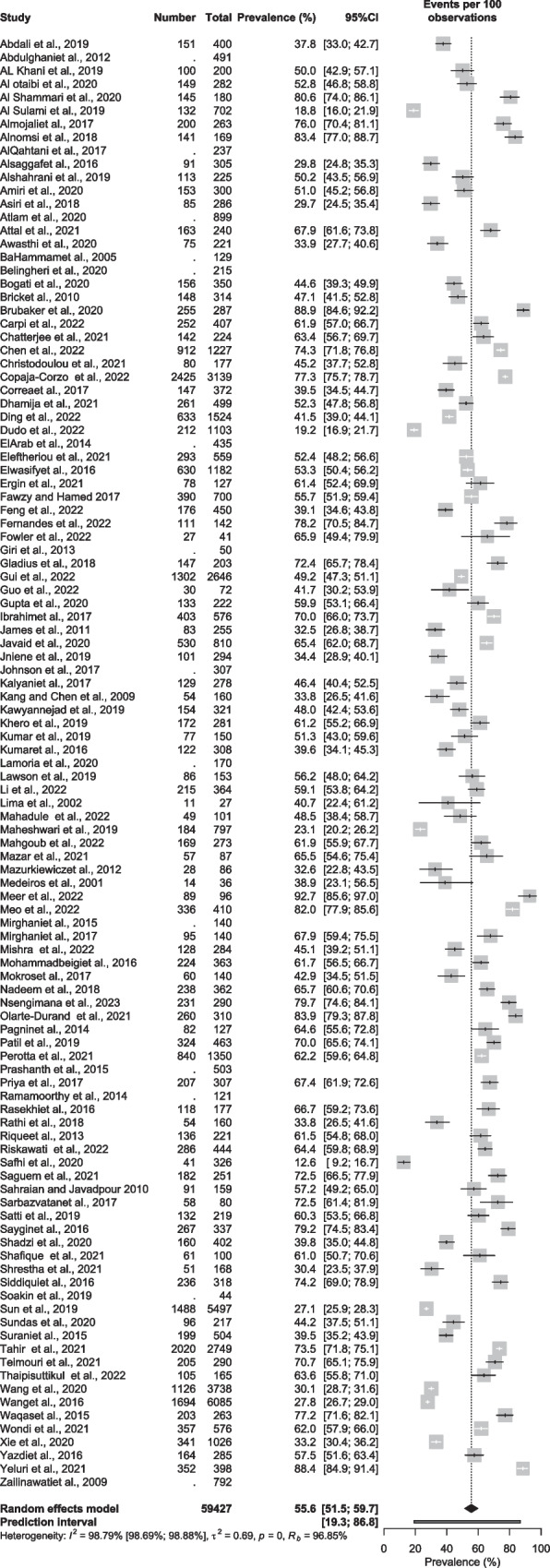
Meta-analysis of the prevalence of poor sleep quality in medical students
According to a (leave-one-out) sensitivity analysis, no study influenced the global prevalence estimate of more than 1%. Visual inspection of the funnel plot (Supplemental Fig. 2) and radial plot (Supplemental Fig. 3) indicates a modest publication bias; however, Begg’s test (z = 1.14, p-value = 0.26) was not significant, suggesting that there was no significant publication bias.
A subgroup analysis of the pooled prevalence of poor sleep quality by country was performed, highlighting countries with (K > 3). Results show that the highest prevalence was in the USA (K= 4) with a pooled prevalence of 61.57% [18.83%; 91.71%]; τ2 = 1.51; τ = 1.23. India, Brazil, and Pakistan followed sharing the same estimated pooled prevalence of 56% with India (K = 14) 95% CI [45.49%; 66.17%], τ2 = 0.4326, τ = 0.6578, Brazil (K = 7) 95% CI [41.77%; 70.45%], τ2 = 0.27; τ = 0.53, and Pakistan (K = 8) 95% CI [41.15%; 71.08%]; τ2 = 0.71; τ = 0.84, respectively. China (K = 11) demonstrated the lowest estimated pooled prevalence of 41.25% [31.55%; 51.68%], τ2 = 0.33, τ = 0.57. Iran (K = 11) and KSA (K = 13) fell in the middle with a pooled prevalence of 55.26% CI [47.01%; 63.23%]; τ2 = 0.21 τ = 0.45, and 54.94% [37.31%; 71.42%]; τ2 = 1.28, τ = 1.13, respectively. A statistically significant difference between countries was observed (P-value <0.001).
A subgroup analysis of the pooled prevalence of poor sleep quality by COVID-19 was conducted. Results before the pandemic being (K = 75) 53.83% [49.05%; 58.55%], τ2 = 0.57, τ = 0.76. In contrast, the pooled prevalence of poor sleep quality during the pandemic (K = 20) was 62.11% [53.51%; 70.01%], τ2 = 0.57, τ = 0.76, revealing an increased pooled prevalence of poor sleep quality after the pandemic; however, this difference was statistically not significant (P-value = 0.08), see (Supplemental Fig. 4).
Excessive Daytime Sleepiness
The random effects meta-analytical pooling of the estimate of EDS (K = 28, N = 10122) yielded a crude prevalence rate of 33.32% 95% CI [26.52%; 40.91%] with statistically significant evidence of between-study heterogeneity τ2 = 0.35 [0.30; 1.02]; τ = 0.59 [0.54; 1.01] I2 = 96.2% [95.3%; 96.9%]; H = 5.13 [4.61; 5.70]; 95% PI [12.66%; 63.27%]. Using ESS to measure EDS, the raw prevalence estimates of EDS reported among medical students using the ESS ranged from 10.3 to 100%, as illustrated in Fig. 5. Neither age nor sex explained heterogeneity for EDS. Detailed results are shown in Table 2.
Fig. 5.
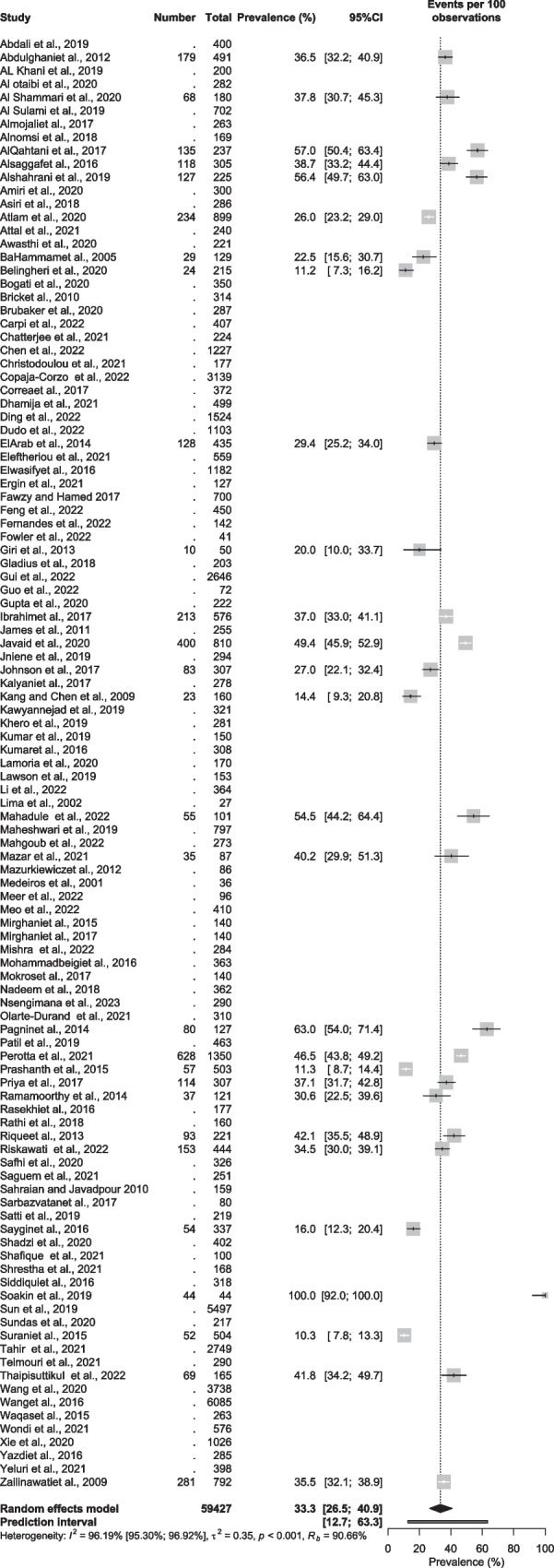
Meta-analysis of the prevalence of excessive daytime sleepiness in medical students
According to a (leave-one-out) sensitivity analysis, no study influenced the global EDS prevalence estimate of more than 1%. Visual inspection of the funnel plot (Supplemental Fig. 5) and radial plot (Supplemental Fig. 6) indicates no publication bias; this was supported by a non-significant Begg’s test (z = -0.91, p-value = 0.36).
A subgroup analysis of EDS by country was conducted. Highlighting countries with (K > 3), results yielded the highest prevalence rate of EDS was in Brazil (K = 3) with 49.88% [25.54%; 74.27%]; τ2 = 0.09, τ = 0.30. India holding the lowest prevalence rate (K = 5) of 28.56% [12.16%; 53.60%]; τ2 = 0.79; τ = 0.89. KSA with 40.64% [29.91%; 52.35%]; τ2 = 0.16; τ = 0.40. A statistically significant difference between countries was observed (P-value <0.001).
A subgroup analysis of ESS by COVID-19 was also conducted. Results show a total of (K = 27) studies of EDS were done before the pandemic with a pooled prevalence rate of 32.62% [25.79%; 40.27%]; τ2 = 0.34; τ = 0.59. Only one study was found to measure the EDS using ESS among medical students during COVID-19 and revealed a result of 54.46% [44.7%; 63.88%], see (Supplemental Fig. 7).
Sleep Duration
The meta-analytic pooling of the point estimates (K = 35, N = 18052) of nightly sleep duration revealed that on average medical students sleep about 6.5 h per night 95% CI [6.24; 6.64], with statistically significant evidence of between-study heterogeneity τ2 = 0.35 [0.22; 0.73]; τ = 0.59 [0.46; 0.85]; I2 = 96.2% [95.3%; 96.9%]; H = 5.13 [4.61; 5.70]; 95% PI [5.21; 7.68]. The raw mean of sleep duration reported among medical students ranged from 5.3 to 7.9, as illustrated in Fig. 6. Detailed results are shown in Table 2.
Fig. 6.
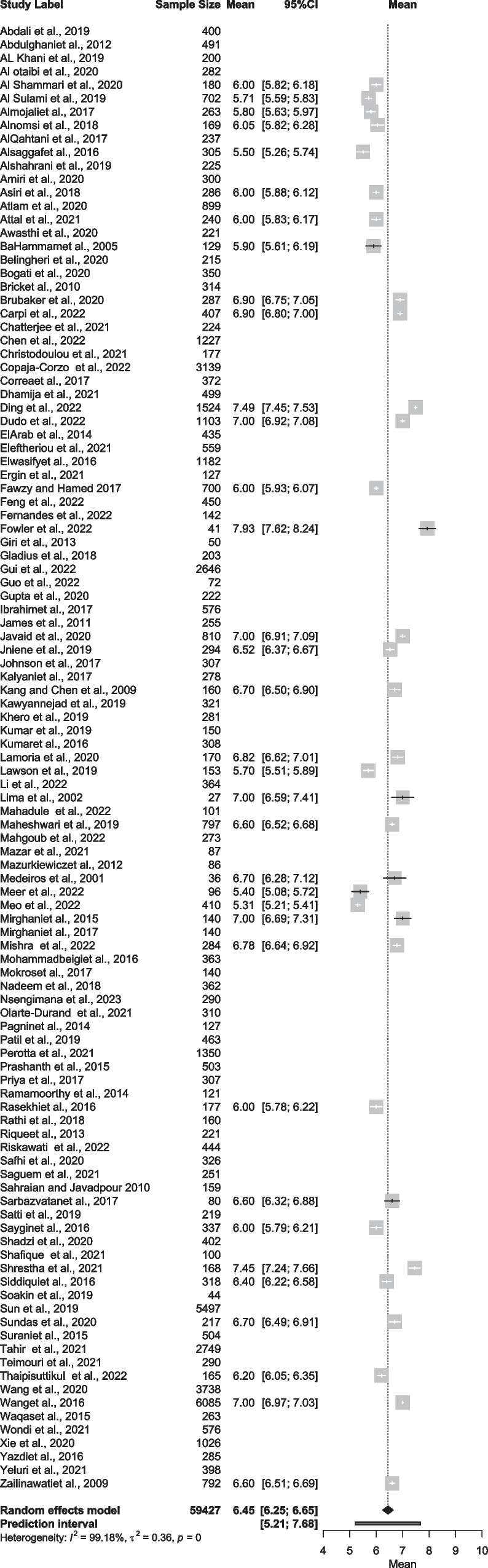
Meta-analysis of the mean sleep duration in medical students
A leave-one-out sensitivity analysis indicated that no study influenced the results by more than 0.25 h (i.e., 15 min) of sleep per night. Publication bias was assessed by visual inspection of the funnel plot (Supplemental Fig. 8) and radial plot (Supplemental Fig. 9), which indicated a slight publication bias; however, Begg’s test (z = 0.16, p-value = 0.87) was not significant.
A subgroup analysis by country was obtained. Highlighting countries with (K >3). Results revealed the highest mean of sleep duration was in China (K = 3) with 7.00 h of sleep per night [95% CI 6.67; 7.45]; τ2 = 0.11; τ = 0.34. The lowest was in KSA (K = 9), with a mean of 5.8 h of sleep per night [95% CI 5.60; 6.09]; τ2 = 0.12; τ = 0.35. Iran with 6.5 h of sleep per night [95% CI 5.93; 7.11]; τ2 = 0.25; τ = 0.50. There was a statistically significant difference between countries (P-value <0.001).
A subgroup analysis by COVID-19 was also conducted. Results yielded that pre-COVID-19 era (K = 29) medical students, on average, got about 6.3 h of sleep per night [95% CI 6.14; 6.52]; τ2 = 0.26; τ = 0.51. In contrast, the average sleep duration during COVID-19 (K = 6) was 7.00 h of sleep per night [95% CI 6.17; 7.76]; τ2 = 0.98; τ = 0.99. The difference in sleep duration was not statistically significant between pre-COVID-19 and during COVID-19 (P-value = 0.87), see (Supplemental Fig. 10).
Discussion
This meta-analysis found a worldwide estimated pooled prevalence of poor sleep quality of 57% and an EDS prevalence of 33% in medical students, who also were found to be short sleepers, averaging 6.5 h per night, which suggests that at least 30% of the students were sleeping less than the recommended 7–9 h per night.
Insufficient sleep among medical students is of growing concern, with serious consequences for their health, academic performance, and career [29, 30]. Recent studies have found that medical students are more likely to experience sleep deprivation than their peers in other fields, due to the intense academic and clinical demands of medical school [61, 79]. This lack of sleep can profoundly impact medical students’ physical and mental health, leading to various negative effects [80]. The most obvious consequence of insufficient sleep is decreased alertness and focus [58, 81]. Sleep is crucial for learning and consolidation of memory [82]; without adequate rest, medical students may find it difficult to concentrate in lectures and clinical rotations [81]. This can lead to poor academic performance and a greater risk of making mistakes in the clinical setting [63]. Furthermore, insufficient sleep can lead to impaired decision-making, which can have serious implications for patient care [29]. Unfortunately, it has been shown that sleep-deprived students who struggle academically are unaware of the extent to which their sleep loss can affect their capacity to perform cognitive tasks [63]. Pilcher and Walters exposed 44 college students to complete sleep deprivation for one night. They discovered that the sleep-deprived students considerably underperformed on cognitive tasks compared to the normal-sleep group [66]. However, the students who performed poorly due to lack of sleep also reported greater levels of estimated performance and incorrectly judged their performance as being higher than those who were not sleep deprived [66].
In addition to the cognitive effects of insufficient sleep, medical students may also experience physical health problems [14, 16, 83]. It can also lead to an increased risk of motor vehicle accidents, as well as an increased risk of depression and anxiety [14, 84, 85]. Finally, sleep deprivation can significantly impact medical students’ professional development. Studies have found that medical students who experience insufficient sleep are more likely to experience burnout and lack motivation [29, 32]. This can lead to decreased job satisfaction and a greater risk of medical school dropout [29, 32].
Considering these potential consequences, it is essential that medical students take steps to ensure they are getting adequate rest. College students need to be taught about good sleep behaviors, which may include establishing a consistent sleep schedule, avoiding caffeine and alcohol before bed and avoiding screens before bed [18, 86, 87]. Additionally, educators and college administrators must actively consider sleep habits and disturbances in the context of students' health and academic achievement [63]. Active measures should include providing students with resources to help them manage their sleep habits, e.g., lifestyle counseling and intervention techniques [23].
University students usually have poorer sleep quality than the overall population [29, 30]. According to a recent meta-analysis, this can be explained by the challenging nature of the academic subject, the test season, side jobs, the fear of missing out, and irregular daytime schedules [60, 88, 89]. Due to their rigorous academic schedule, the competitive nature of the medical field, exposure to death and illness situations, and on-call and night shifts, medical students seem more susceptible to sleep issues than their academic peers [90].
Academic performance in medical students has been shown to be severely impacted by lower nocturnal sleep time, later bedtimes during weekdays and weekends, catching up on sleep on the weekends, and increased daytime sleepiness [63, 91]. Moreover, a recent study demonstrated a significant negative association between sleep quality and grade point average (GPA), supporting the idea that poor sleep quality is linked to subpar academic performance [18].
Poor sleep quality can be caused by a variety of factors, such as stress, long hours of studying, and lack of time management [60, 92]. In order to prevent and improve poor sleep quality, several solutions can be implemented [20, 93, 94]. One solution is to create a healthy sleep schedule and stick to it. By having a consistent bedtime and wake time, the body’s internal clock will become used to the routine and help with sleep quality. Additionally, by avoiding caffeine and other stimulants close to bedtime, the body will be more relaxed and ready for sleep [70, 95].
Another solution is to reduce stress levels. Stress can be a major factor in poor sleep quality, and medical students often experience high levels of stress due to the demanding nature of their studies [29, 30]. Finding ways to reduce stress, such as exercise, relaxation techniques, yoga, or mindfulness, can be beneficial in improving sleep quality [30]. Finally, medical students should practice time management. By breaking down tasks into smaller, more manageable pieces and setting realistic goals, medical students can avoid feeling overwhelmed and reduce the amount of stress they experience [96–98]. By implementing these solutions, medical students can improve their sleep quality and, ultimately, their well-being and academic performance [67, 99, 100].
Understanding how the epidemic affects medical students’ sleep could have wider effects on healthcare. It is well recognized that sleep issues are linked to a number of detrimental health effects, such as a higher chance of medical errors, burnout, and poor patient safety [32–34, 101]. Researchers can learn more about the possible long-term health effects of the COVID-19 pandemic on this high-risk demographic by examining changes in the quality and amount of sleep among medical students before and after the epidemic. Utilizing this knowledge can help create interventions that enhance medical students' sleep health, ultimately enhancing patient safety and healthcare outcomes [68, 102, 103].
When it comes to sleep issues, medical students are particularly susceptible, especially during a pandemic. It is crucial for medical students to regulate their sleep health to lessen the possible deleterious effects of interrupted sleep patterns and sleep disorders during future pandemics. Setting sleep hygiene as a priority is a crucial first step [32–34, 84]. This entails keeping a regular sleep schedule, avoiding stimulating activities right before bed, and establishing a relaxing sleeping environment. To control stress and enhance sleep, medical students may also find it helpful to practice relaxation techniques like meditation or deep breathing [32–34, 84].
Maintaining physical activity and exercise, which has been demonstrated to enhance sleep quality and lower stress, is another crucial measure. Medical students may need to come up with novel ways to exercise during a pandemic, such as working out at home or going for walks or runs in empty spaces [32–34]. It is crucial for medical students to stay socially connected and ask for help when they need it. During a pandemic, social isolation and stress are frequent, and these elements might impair sleep quality. By using technology to stay in touch with loved ones, medical students can also gain from consulting mental health professionals when needed [32–34].
Self-reported assessments and cross-sectional study designs are frequent drawbacks in many studies. The impact of the pandemic on pupils who are known to have medical or mental health issues is still another crucial factor in addition to these restrictions.
Students who already have physical or mental health issues may be more susceptible to the pandemic's effects on their sleep health. For instance, students who already struggle with anxiety or depression may become even more stressed and anxious because of the pandemic, which may have a detrimental effect on how well they sleep. Like this, students who suffer from medical conditions like sleep apnea or chronic pain may find that changes in their daily routines and elevated stress levels exacerbate their symptoms.
Future research can follow students over time and evaluate the pandemic’s effects on their sleep health using more rigorous study methods, such as longitudinal studies, to address these shortcomings. Studies can also reduce the impact of self-report bias by using objective measurements of sleep quality, such as actigraphy or polysomnography. Additionally, research can examine potential interventions to lessen the pandemic’s detrimental effects on students who already have medical conditions or mental health issues, as well as the impact of the pandemic on those students.
To improve the sleep health of medical students, several treatment approaches could be utilized. The incorporation of sleep education and counseling programs into medical school curricula is one potential remedy. Students could learn through these programs the value of good sleep hygiene as well as techniques for increasing both the quantity and quality of sleep [37, 104]. Programs for sleep education and counseling may be organized as group sessions or one-on-one counseling sessions, and they may be provided by qualified individuals like sleep specialists or mental health professionals [32, 105].
The inclusion of sleep hygiene in wellness programs for medical schools is another potential strategy. These programs could contain elements aimed at enhancing sleep quality, such stress-reduction strategies or exercise regimens. To help medical students monitor and enhance their sleep quality, medical institutions may also think about offering them tools like sleep aids or sleep tracking applications [32].
Medical schools could implement policies to promote sleep health among medical students, such as limiting the number of consecutive hours medical students are required to work or providing accommodations for medical students with sleep problems [35]. These policies could help to promote a culture of sleep health within the medical school system and prioritize the well-being of medical students [30].
The current review has several merits: First, we included three important sleep issues, i.e., sleep duration, sleep quality, and excessive daytime sleepiness, as outcomes facing students. Second robust statistical modeling was applied, correcting for bias, outliers, and moderators; thus, the results of the present review are anticipated to be highly generalizable.
Nevertheless, this review has a few drawbacks: First, we only incorporated research written in English. Second, epidemiological meta-analyses will inevitably have substantial heterogeneity [29, 30, 106]. In our meta-analysis, the heterogeneity remained considerable even after undertaking subgroup analyses or moderator analyses using meta-regression approaches. To deal with this, we reported 95% prediction intervals to generalize easier. Additional sources of variability, like lifestyle factors, sleep disorders (like obstructive sleep apnea), and stress, could not be investigated because of the studies’ low availability of common information. Third, every study that was part of this review was a cross-sectional survey. To understand the causes linked to sleep issues in this cohort, longitudinal studies examining changes in sleep quality during medical education are required. Finally, the prevalence rates examined here were based on self-report measures. While the PSQI and the ESS are validated and widely used clinical and research instruments, the components of sleep quality and EDS they measure are limited. Future research is encouraged to look at additional aspects of sleep, such as objective sleep quality measurement, which includes polysomnography.
Conclusion
The current meta-analysis revealed that the worldwide estimated pooled prevalence of poor sleep quality is about 57% and of excessive daytime sleepiness is about 33%. The average sleep duration for medical students is only 6.5 h per night, which suggests that at least 30% of them get less sleep than the recommended 7–9 h per night. These are alarming figures as they indicate that a third to more than half of all medical students are sleeping insufficiently and are subject to all the consequences of this lack of adequate sleep. Due to the detrimental effects on their health, regular screening for poor sleep and proposed remedies are required for medical students. Sleep problems are frequent among medical students, making them a priority problem. Future studies should concentrate on preventative and intervention programs geared at these populations.
Medical students should pay careful attention to the amount of rest that they are getting and take steps to ensure that they are getting adequate amounts of sleep. This includes establishing a good sleep routine and avoiding technology for a few hours before bed. Additionally, medical students should seek help from professors and other resources on campus if they are having trouble managing their workload or are feeling overwhelmed.
Supplementary Information
Supplemental Figure 1: Traffic light of the included studies.
Supplemental Figure 2: Funnel plot of poor sleep quality in medical students.
Supplemental Figure 3: Radial plot of poor sleep quality in medical students.
Supplemental Figure 4: Subgroup meta-analysis of poor sleep quality in medical students by COVID-19 status.
Supplemental Figure 5: Funnel plot of excessive daytime sleepiness in medical students.
Supplemental Figure 6: Radial plot of excessive daytime sleepiness in medical students.
Supplemental Figure 7: Subgroup meta-analysis of excessive daytime sleepiness in medical students by COVID-19 status.
Supplemental Figure 8: Funnel plot of the mean sleep duration in medical students.
Supplemental Figure 9: Radial plot of the mean sleep duration in medical students.
Supplemental Figure 10: Subgroup meta-analysis of the mean sleep duration in medical students by COVID-19 status.
Declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the original authors have been previously published and complied with all applicable ethical standards (including the Helsinki Declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mohammed A. Binjabr, Email: Mhaljabr@gmail.com
Idrees S. Alalawi, Email: Idreesalalawi@gmail.com
Rayan A. Alzahrani, Email: Rayan.zahrani97@gmail.com
Othub S. Albalawi, Email: Othubalbalawi@gmail.com
Rakan H. Hamzah, Email: Rakanhamzah@hotmail.com
Yazed S. Ibrahim, Email: ybinibrahem@gmail.com
Fatima Buali, Email: Fatima.buali.md@gmail.com.
Mariwan Husni, Email: mariwanh@agu.edu.bh.
Ahmed S. BaHammam, Email: ashammam2@gmail.com
Michael V. Vitiello, Email: vitiello@uw.edu
Haitham Jahrami, Email: haitham.jahrami@outlook.com.
References
- 1.Newman AB, Enright PL, Manolio TA, Haponik EF, Wahl PW, Group CHSR Sleep disturbance, psychosocial correlates, and cardiovascular disease in 5201 older adults: the Cardiovascular Health Study. J Am Geriatr Soc. 1997;45(1):1–7. doi: 10.1111/j.1532-5415.1997.tb00970.x. [DOI] [PubMed] [Google Scholar]
- 2.Wang Q, Xi B, Liu M, Zhang Y, Fu M. Short sleep duration is associated with hypertension risk among adults: a systematic review and meta-analysis. Hypertens Res. 2012;35(10):1012–1018. doi: 10.1038/hr.2012.91. [DOI] [PubMed] [Google Scholar]
- 3.Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price NJ, Dinges DF, et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol. 2004;43(4):678–683. doi: 10.1016/j.jacc.2003.07.050. [DOI] [PubMed] [Google Scholar]
- 4.Palma J-A, Urrestarazu E, Iriarte J. Sleep loss as risk factor for neurologic disorders: a review. Sleep Med. 2013;14(3):229–236. doi: 10.1016/j.sleep.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 5.Hanke JM, Schindler KA, Seiler A. On the relationships between epilepsy, sleep, and Alzheimer’s disease: a narrative review. Epilepsy Behav. 2022;129:108609. doi: 10.1016/j.yebeh.2022.108609. [DOI] [PubMed] [Google Scholar]
- 6.Scott LD, Arslanian-Engoren C, Engoren MC. Association of sleep and fatigue with decision regret among critical care nurses. Am J Crit Care. 2014;23(1):13–23. doi: 10.4037/ajcc2014191. [DOI] [PubMed] [Google Scholar]
- 7.Basner M, Rao H, Goel N, Dinges DF. Sleep deprivation and neurobehavioral dynamics. Curr Opin Neurobiol. 2013;23(5):854–863. doi: 10.1016/j.conb.2013.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.López-Muciño LA, García-García F, Cueto-Escobedo J, Acosta-Hernández M, Venebra-Muñoz A, Rodríguez-Alba JC. Sleep loss and addiction. Neurosci Biobehav Rev. 2022;10(141) 10.1016/j.neubiorev.2022.104832. [DOI] [PubMed]
- 9.Lim J, Dinges DF. A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychological bulletin. 2010;136(3):375. doi: 10.1037/a0018883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freeman D, Sheaves B, Waite F, Harvey AG, Harrison PJ. Sleep disturbance and psychiatric disorders. Lancet Psychiatry. 2020;7(7):628–637. doi: 10.1016/S2215-0366(20)30136-X. [DOI] [PubMed] [Google Scholar]
- 11.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33(2):414–420. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spaeth AM, Dinges DF, Goel N. Effects of experimental sleep restriction on weight gain, caloric intake, and meal timing in healthy adults. Sleep. 2013;36(7):981–990. doi: 10.5665/sleep.2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu M, Ahmed WL, Zhuo L, Yuan H, Wang S, Zhou F. Association of sleep patterns with type 2 diabetes mellitus: a cross-sectional study based on latent class analysis. Int J Environ Res Public Health. 2022;20(1):393. doi: 10.3390/ijerph20010393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spiegel K, Sheridan JF, Van Cauter E. Effect of sleep deprivation on response to immunizaton. Jama. 2002;288(12):1471–1472. doi: 10.1001/jama.288.12.1469. [DOI] [PubMed] [Google Scholar]
- 15.Prather AA, Hall M, Fury JM, Ross DC, Muldoon MF, Cohen S, et al. Sleep and antibody response to hepatitis B vaccination. Sleep. 2012;35(8):1063–1069. doi: 10.5665/sleep.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. 2016;80(1):40–52. doi: 10.1016/j.biopsych.2015.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. 2006;10(5):323–337. doi: 10.1016/j.smrv.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 18.Asarnow LD, McGlinchey E, Harvey AG. The effects of bedtime and sleep duration on academic and emotional outcomes in a nationally representative sample of adolescents. J Adolesc Health. 2014;54(3):350–356. doi: 10.1016/j.jadohealth.2013.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–43. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 20.Yassin A, Al-Mistarehi A-H, Yonis OB, Aleshawi AJ, Momany SM, Khassawneh BY. Prevalence of sleep disorders among medical students and their association with poor academic performance: a cross-sectional study. Ann Med Surg. 2020;58:124–129. doi: 10.1016/j.amsu.2020.08.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alfawaz RA, Aljuraiban GS, AlMarzooqi MA, Alghannam AF, BaHammam AS, Dobia AM, et al. The recommended amount of physical activity, sedentary behavior, and sleep duration for healthy Saudis: a joint consensus statement of the Saudi Public Health Authority. Ann Thorac Med. 2021;16(3):239–244. doi: 10.4103/atm.atm_33_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McArdle N, Ward SV, Bucks RS, Maddison K, Smith A, Huang R-C, et al. The prevalence of common sleep disorders in young adults: a descriptive population-based study. Sleep. 2020;43(10):zsaa072. doi: 10.1093/sleep/zsaa072. [DOI] [PubMed] [Google Scholar]
- 23.López-Muciño LA, García-García F, Cueto-Escobedo J, Acosta-Hernández M, Venebra-Muñoz A, Rodríguez-Alba JC. Sleep loss and addiction. NeurosciBiobehav Rev. 2022;141:104832. doi: 10.1016/j.neubiorev.2022.104832. [DOI] [PubMed] [Google Scholar]
- 24.Seoane HA, Moschetto L, Orliacq F, Orliacq J, Serrano E, Cazenave MI, et al. Sleep disruption in medicine students and its relationship with impaired academic performance: a systematic review and meta-analysis. Sleep Med Rev. 2020;53:101333. doi: 10.1016/j.smrv.2020.101333. [DOI] [PubMed] [Google Scholar]
- 25.Meer H, Jeyaseelan L, Sultan MA. Sleep quality and emotional state of medical students in Dubai. Sleep Disord. 2022;2022 [DOI] [PMC free article] [PubMed]
- 26.Abdelmoaty Goweda R, Hassan-Hussein A, Ali Alqahtani M, Janaini MM, Alzahrani AH, Sindy BM, et al. Prevalence of sleep disorders among medical students of umm Al-Qura University, Makkah, Kingdom of Saudi Arabia. J Public Health Res. 2020;9(1_suppl) jphr. 2020.1921 [DOI] [PMC free article] [PubMed]
- 27.Janatmakan Amiri A, Morovatdar N, Soltanifar A, Rezaee R. Prevalence of sleep disturbance and potential associated factors among medical students from Mashhad, Iran. Sleep Disord. 2020;2020 [DOI] [PMC free article] [PubMed]
- 28.Lawson HJ, Wellens-Mensah JT, Attah NS. Evaluation of sleep patterns and self-reported academic performance among medical students at the University of Ghana School of Medicine and Dentistry. Sleep Disord. 2019;2019 [DOI] [PMC free article] [PubMed]
- 29.Jahrami H, Dewald-Kaufmann J, MeA-I F, AlAnsari AM, Taha M, AlAnsari N. Prevalence of sleep problems among medical students: a systematic review and meta-analysis. J Public Health. 2020;28:605–622. doi: 10.1007/s10389-019-01064-6. [DOI] [Google Scholar]
- 30.Jahrami H, Alshomili H, Almannai N, Althani N, Aloffi A, Algahtani H, et al. Predictors of excessive daytime sleepiness in medical students: a meta-regression. Clocks Sleep. 2019;1(2):209–219. doi: 10.3390/clockssleep1020018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rao W-W, Li W, Qi H, Hong L, Chen C, Li C-Y, et al. Sleep quality in medical students: a comprehensive meta-analysis of observational studies. Sleep Breath. 2020;24(3):1151–1165. doi: 10.1007/s11325-020-02020-5. [DOI] [PubMed] [Google Scholar]
- 32.Almutairi H, Alsubaiei A, Abduljawad S, Alshatti A, Fekih-Romdhane F, Husni M, et al. Prevalence of burnout in medical students: a systematic review and meta-analysis. Int J Soc Psychiatry. 2022;68(6):1157–1170. doi: 10.1177/00207640221106691. [DOI] [PubMed] [Google Scholar]
- 33.Pandi-Perumal SR, Zaki NFW, Qasim M, Elsayed Morsy N, Manzar MD, BaHammam AS, et al. Neuropsychiatric consequences of COVID-19 pandemic: a synthetic review from a global perspective. Alpha Psychiatry. 2022;23(4):144–154. doi: 10.5152/alphapsychiatry.2022.21783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Habbash F, Ben Salah A, Almarabheh A, Jahrami H. Insomnia and related factors during the delta wave of the COVID-19 pandemic in the Kingdom of Bahrain: a cross-sectional study. Nat Sci Sleep. 2022;14:1963–1975. doi: 10.2147/nss.S380141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jahrami HA, Alhaj OA, Humood AM, Alenezi AF, Fekih-Romdhane F, AlRasheed MM, et al. Sleep disturbances during the COVID-19 pandemic: a systematic review, meta-analysis, and meta-regression. Sleep Med Rev. 2022;62:101591. doi: 10.1016/j.smrv.2022.101591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.da Silva ML, Rocha RSB, Buheji M, Jahrami H, Cunha KDC. A systematic review of the prevalence of anxiety symptoms during coronavirus epidemics. J Health Psychol. 2021;26(1):115–125. doi: 10.1177/1359105320951620. [DOI] [PubMed] [Google Scholar]
- 37.Alsalman A, Jahrami H, Mubarak H, Aljabal M, Abdulnabi M, Yusuf A, et al. The psychological impact of COVID-19 pandemic on the population of Bahrain. Acta Biomed. 2020;91(4):e2020131. doi: 10.23750/abm.v91i4.10336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. doi: 10.1016/j.ijsu.2021.105906. [DOI] [PubMed] [Google Scholar]
- 39.Schardt C, Adams MB, Owens T, Keitz S, Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak. 2007;7:1–6. doi: 10.1186/1472-6947-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 41.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 42.Lo CK-L, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:1–5. doi: 10.1186/1471-2288-14-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schwarzer G, Schwarzer MG. Package ‘meta’. R Found Stat Comput. 2012;9:27. [Google Scholar]
- 44.Viechtbauer W, Viechtbauer MW. Package ‘metafor’. The Comprehensive R Archive Network Package ‘metafor’ http://cran r-project org/web/packages/metafor/metafor pdf. 2015.
- 45.Team RC. R: A language and environment for statistical computing. Published online 2023. 2023.
- 46.Sidik K, Jonkman JN. A simple confidence interval for meta-analysis. Stat Med. 2002;21(21):3153–3159. doi: 10.1002/sim.1262. [DOI] [PubMed] [Google Scholar]
- 47.Boyes R. Forester: an R package for creating publication-ready forest plots. R Package Version 0. 032021.
- 48.Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008;37(5):1148–1157. doi: 10.1093/ije/dyn065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;40:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 51.Duval S, Tweedie R. Trim and Fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455-463. doi: https://doi.org/10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed]
- 52.Cochran WG. Some methods for strengthening the common χ 2 tests. Biometrics. 1954;10(4):417–451. doi: 10.2307/3001616. [DOI] [Google Scholar]
- 53.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 54.Higgins J, Li T, Deeks J, Thomas J, Chandler J, Cumpston M, et al. Cochrane Handbook for Systematic Reviews of Interventions. 2017. Obtaining standard errors from confidence intervals and P values: absolute (difference) measures. [Google Scholar]
- 55.Harrer M, Cuijpers P, Furukawa TA, Ebert DD. Doing meta-analysis with R: A hands-on guide. Chapman and Hall/CRC; 2021. [Google Scholar]
- 56.Knapp G, Hartung J. Improved tests for a random effects meta-regression with a single covariate. Stat Med. 2003;22(17):2693-2710. doi: https://doi.org/10.1002/sim.1482. [DOI] [PubMed]
- 57.Gladius Jennifer H, Sowmiya K, Vidya D, Archana Lakshmi P, William RF. A study of mobile phone usage on sleep disturbance, stress and academic performance among medical students in Tamil Nadu. Int J Commun Med Publ Health. 2018;5(1):365. [Google Scholar]
- 58.Fawzy M, Hamed SA. Prevalence of psychological stress, depression and anxiety among medical students in Egypt. Psychiatry Res. 2017;255:186–194. doi: 10.1016/j.psychres.2017.05.027. [DOI] [PubMed] [Google Scholar]
- 59.Almojali AI, Almalki SA, Alothman AS, Masuadi EM, Alaqeel MK. The prevalence and association of stress with sleep quality among medical students. J Epidemiol Glob Health. 2017;7(3):169–174. doi: 10.1016/j.jegh.2017.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Alsaggaf MA, Wali SO, Merdad RA, Merdad LA. Sleep quantity, quality, and insomnia symptoms of medical students during clinical years: relationship with stress and academic performance. Saudi Med J. 2016;37(2):173. doi: 10.15537/smj.2016.2.14288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Waqas A, Khan S, Sharif W, Khalid U, Ali A. Association of academic stress with sleeping difficulties in medical students of a Pakistani medical school: a cross sectional survey. PeerJ. 2015;3:e840. doi: 10.7717/peerj.840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.ElArab HE, Rabie MA, Ali DH. Sleep behavior and sleep problems among a medical student sample in relation to academic performance: a cross-sectional questionnaire-based study. Middle East Curr Psychiatry. 2014;21(2):72–80. doi: 10.1097/01.XME.0000444452.76469.05. [DOI] [Google Scholar]
- 63.Bahammam AS, Alaseem AM, Alzakri AA, Almeneessier AS, Sharif MM. The relationship between sleep and wake habits and academic performance in medical students: a cross-sectional study. BMC Med Educ. 2012;12:61. doi: 10.1186/1472-6920-12-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Abdulghani HM, Alrowais NA, Bin-Saad NS, Al-Subaie NM, Haji AM, Alhaqwi AI. Sleep disorder among medical students: relationship to their academic performance. Med Teach. 2012;34(sup1):S37–S41. doi: 10.3109/0142159X.2012.656749. [DOI] [PubMed] [Google Scholar]
- 65.Medeiros ALD, Mendes DB, Lima PF, Araujo JF. The relationships between sleep-wake cycle and academic performance in medical students. Biol Rhythm Res. 2001;32(2):263–270. doi: 10.1076/brhm.32.2.263.1359. [DOI] [Google Scholar]
- 66.Pilcher JJ, Walters AS. How sleep deprivation affects psychological variables related to college students' cognitive performance. J Am Coll Health. 1997;46(3):121–126. doi: 10.1080/07448489709595597. [DOI] [PubMed] [Google Scholar]
- 67.Rasekhi S, Ashouri FP, Pirouzan A. Effects of sleep quality on the academic performance of undergraduate medical students. Health Scope. 1970;5(3)
- 68.Nair M, Moss N, Bashir A, Garate D, Thomas D, Fu S, et al. Mental health trends among medical students. Proc (Bayl Univ Med Cent). 2023;36(3):408–410. doi: 10.1080/08998280.2023.2187207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jahrami H, BaHammam AS, Bragazzi NL, Saif Z, Faris M, Vitiello MV. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2021;17(2):299–313. doi: 10.5664/jcsm.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jahrami H, Al-Mutarid M, Penson PE, Al-Islam Faris M, Saif Z, Hammad L. Intake of caffeine and its association with physical and mental health status among university students in Bahrain. Foods. 2020;9(4) 10.3390/foods9040473. [DOI] [PMC free article] [PubMed]
- 71.Jahrami H, Sater M, Abdulla A, MeA-I F, AlAnsari A. Eating disorders risk among medical students: a global systematic review and meta-analysis. Eat Weight Disord-Stud Anorexia Bulimia Obesity. 2019;24:397–410. doi: 10.1007/s40519-018-0516-z. [DOI] [PubMed] [Google Scholar]
- 72.Pagnin D, de Queiroz V, Carvalho YTMS, Dutra ASS, Amaral MB, Queiroz TT. The relation between burnout and sleep disorders in medical students. Acad Psychiatry. 2014;38:438–444. doi: 10.1007/s40596-014-0093-z. [DOI] [PubMed] [Google Scholar]
- 73.Mazurkiewicz R, Korenstein D, Fallar R, Ripp J. The prevalence and correlations of medical student burnout in the pre-clinical years: a cross-sectional study. Psychol Health Med. 2012;17(2):188–195. doi: 10.1080/13548506.2011.597770. [DOI] [PubMed] [Google Scholar]
- 74.Brubaker JR, Swan A, Beverly EA. A brief intervention to reduce burnout and improve sleep quality in medical students. BMC Med Educ. 2020;20(1):1–9. doi: 10.1186/s12909-020-02263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mirghani HO, Mohammed OS, Almurtadha YM, Ahmed MS. Good sleep quality is associated with better academic performance among Sudanese medical students. BMC Res Notes. 2015;8(1):1–5. doi: 10.1186/s13104-015-1712-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mokros Ł, Witusik A, Michalska J, Łężak W, Panek M, Nowakowska-Domagała K, et al. Sleep quality, chronotype, temperament and bipolar features as predictors of depressive symptoms among medical students. Chronobiol Int. 2017;34(6):708–720. doi: 10.1080/07420528.2017.1316730. [DOI] [PubMed] [Google Scholar]
- 77.Awasthi AATN, Maheshwari S, Gupta T. Prevalence of internet addiction, poor sleep quality, and depressive symptoms among medical students: a cross-sectional study. Osong Public Health Res Perspect. 2020;10(11) [DOI] [PMC free article] [PubMed]
- 78.Giri PA, Baviskar MP, Phalke DB. Study of sleep habits and sleep problems among medical students of Pravara Institute of Medical Sciences Loni, Western Maharashtra, India. Ann Med Health Sci Res. 2013;3(1):51–54. doi: 10.4103/2141-9248.109488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nadeem A, Cheema MK, Naseer M, Javed H. Assessment of sleep quality and patterns suggestive of somniopathies among students of Army Medical College, Rawalpindi. Pakistan Armed Forces Med J. 2018;68(1):143–148. [Google Scholar]
- 80.Chen J, Tuersun Y, Yang J, Xiong M, Wang Y, Rao X, et al. Association of depression symptoms and sleep quality with state-trait anxiety in medical university students in Anhui Province, China: a mediation analysis. BMC Med Educ. 2022;22(1):1–10. doi: 10.1186/s12909-022-03683-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Guo XST, Xiao H, Xiao R, Xiao Z. Using 24-h heart rate variability to investigate the sleep quality and depression symptoms of medical students. Front Psychiatry. 2022;12:781673. doi: 10.3389/fpsyt.2021.781673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Machado A, Ricardo L, Wendt A, Wehrmeister C. Association between sleep duration and academic, cognitive and socioeconomic outcomes: a systematic literature review of population-based studies. Sleep Epidemiol. 2022;2:100034. doi: 10.1016/j.sleepe.2022. [DOI] [Google Scholar]
- 83.Perotta B, Arantes-Costa FM, Enns SC, Figueiro-Filho EA, Paro H, Santos IS, et al. Sleepiness, sleep deprivation, quality of life, mental symptoms and perception of academic environment in medical students. BMC Med Educ. 2021;21(1):1–13. doi: 10.1186/s12909-021-02544-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zailinawati AH, Teng CL, Chung YC, Teow TL, Lee PN, Jagmohni KS. Daytime sleepiness and sleep quality among Malaysian medical students. Med J Malaysia. 2009;64(2):108–110. [PubMed] [Google Scholar]
- 85.Al MM. Anxiety and depression during the COVID-19 pandemic and their impact on sleep. COVID-19 and Sleep: A Global Outlook. Springer; 2023. pp. 41–59. [Google Scholar]
- 86.Kang J-H, Chen S-C. Effects of an irregular bedtime schedule on sleep quality, daytime sleepiness, and fatigue among university students in Taiwan. BMC Public Health. 2009;9(1):1–6. doi: 10.1186/1471-2458-9-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Boukhris O, Jahrami H, Trabelsi K, Glenn JM, Bragazzi NL. Impact of screen time during the pandemic of COVID-19 on sleep habits. COVID-19 and Sleep: A Global Outlook. Springer; 2023. pp. 281–294. [Google Scholar]
- 88.Sahraian A, Javadpour A. Sleep disruption and its correlation to psychological distress among medical students. Shiraz E-Medical Journal. 2010;11(1):12–17. [Google Scholar]
- 89.Soakin B, Maharaj N, Sakhelashvili I. Sleep disturbances and stress among foreign medical students at European University, Georgia. MedEdPublish. 2019;8(235):235. doi: 10.15694/mep.2019.000235.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Teimouri A, Amra B. Association between sleep quality and gastroesophageal reflux in medical students. Middle East J Digest Dis. 2021;13(2):139. doi: 10.34172/mejdd.2021.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Falloon K, Bhoopatkar H, Moir F, Nakatsuji M, Wearn A. Sleep well to perform well: the association between sleep quality and medical student performance in a high-stakes clinical assessment. SLEEP. Advances. 2022;3(1) 10.1093/sleepadvances/zpac019. [DOI] [PMC free article] [PubMed]
- 92.Alotaibi AD, Alosaimi FM, Alajlan AA, Abdulrahman KAB. The relationship between sleep quality, stress, and academic performance among medical students. J Fam Community Med. 2020;27(1):23. doi: 10.4103/jfcm.JFCM_132_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lamoria M, Sharma S, Poorey K, Bishnoi S. Effect of late-night mobile use on sleep quantity and quality in medical students. 2020.
- 94.Siddiqui AF, Al-Musa H, Al-Amri H, Al-Qahtani A, Al-Shahrani M, Al-Qahtani M. Sleep patterns and predictors of poor sleep quality among medical students in King Khalid University, Saudi Arabia. Malaysian J Med Sci: MJMS. 2016;23(6):94. doi: 10.21315/mjms2016.23.6.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bogati SST, Paudel S, Adhikari B, Baral D. Association of the pattern and quality of sleep with consumption of stimulant beverages, cigarette and alcohol among medical students. J Nepal Health Res Coun. 2020;13:379–385. doi: 10.33314/jnhrc.v18i3.2633. [DOI] [PubMed] [Google Scholar]
- 96.Shafique ZSF, Naz S, Urooj S, Khan S, Javed S. Assessment of factors affecting the sleep hygiene of medical students in Bahawalpur, Pakistan: a cross-sectional study. Sleep Sci. 2021;14(3):273–280. doi: 10.5935/1984-0063.20200063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ding P, Li J, Chen H, Zhong C, Ye X, Shi H. Independent and joint effects of sleep duration and sleep quality on suboptimal self-rated health in medical students: a cross-sectional study. Front Public Health. 2022;10:957409. doi: 10.3389/fpubh.2022.957409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Abdelghyoum Mahgoub A, Mustafa SS. P05-08 correlation between physical activity, sleep componants and quality: in the context of type and intensity: a cross-sectional study among sudanese medical students. Eur J Public Health. 2022;32(Supplement_2):75. doi: 10.1093/eurpub/ckac095.075. [DOI] [Google Scholar]
- 99.Satti MZ, Khan TM, Azhar MJ, Javed H, Yaseen M, Raja MT, et al. Association of physical activity and sleep quality with academic performance among fourth-year MBBS students of Rawalpindi Medical University. Cureus. 2019;11(7) [DOI] [PMC free article] [PubMed]
- 100.Al-Khani AMSM, Zaghloul MS, Ewid M, Saquib N. A cross-sectional survey on sleep quality, mental health, and academic performance among medical students in Saudi Arabia. Biomed Res Notes. 2019;12(1) 10.1186/s13104-019-4713-2. [DOI] [PMC free article] [PubMed]
- 101.AlRasheed MM, Fekih-Romdhane F, Jahrami H, Pires GN, Saif Z, Alenezi AF, et al. The prevalence and severity of insomnia symptoms during COVID-19: a global systematic review and individual participant data meta-analysis. Sleep Med. 2022;100:7–23. doi: 10.1016/j.sleep.2022.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Liu X, Peng L, Wang Z, Zeng P, Mi Y, Xu H. Effects of interpersonal sensitivity on depressive symptoms in postgraduate students during the COVID-19 pandemic: Psychological capital and sleep quality as mediators. Front Psychiatry. 2023;14:1100355. doi: 10.3389/fpsyt.2023.1100355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Śliż D, Wiecha S, Gąsior JS, Kasiak PS, Ulaszewska K, Lewandowski M, et al. Impact of COVID-19 infection on cardiorespiratory fitness, sleep, and psychology of endurance Athletes-CAESAR study. J Clin Med. 2023;12(8) 10.3390/jcm12083002. [DOI] [PMC free article] [PubMed]
- 104.Carpi M, Vestri A. The mediating role of sleep quality in the relationship between negative emotional states and health-related quality of life among Italian medical students. Int J Environ Res Public Health. 2023;20(1):26. doi: 10.3390/ijerph20010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jahrami H, Haji EA, Saif ZQ, Aljeeran NO, Aljawder AI, Shehabdin FN, et al. Sleep quality worsens while perceived stress improves in healthcare workers over two years during the COVID-19 pandemic: results of a longitudinal study. Healthcare (Basel). 2022;10(8) 10.3390/healthcare10081588. [DOI] [PMC free article] [PubMed]
- 106.Sedov ID, Cameron EE, Madigan S, Tomfohr-Madsen LM. Sleep quality during pregnancy: a meta-analysis. Sleep Med Rev. 2018;38:168–176. doi: 10.1016/j.smrv.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 107.Abdali NNM, Ghorbani R. Evaluation of emotional intelligence, sleep quality, and fatigue among Iranian medical, nursing, and paramedical students: a cross-sectional study. Qatar Med J. 2019;3 10.5339/qmj.2019. [DOI] [PMC free article] [PubMed]
- 108.Al Shammari MA, Al Amer NA, Al Mulhim SN, Al Mohammedsaleh HN, AlOmar RS. The quality of sleep and daytime sleepiness and their association with academic achievement of medical students in the eastern province of Saudi Arabia. J Fam Commun Med. 2020;27(2):97. doi: 10.4103/jfcm.JFCM_160_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Alsulami A, Bakhsh D, Baik M, Merdad M, Aboalfaraj N. Assessment of sleep quality and its relationship to social media use among medical students. Med Sci Educ. 2019;29:157–161. doi: 10.1007/s40670-018-00650-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Shelian AN, Khalid AB, Omar AA, Waled AB, Wedyan AB, Hyder M. The chronotype [eveningness-morningness] effects on academic achievement among medical students in Tabuk City, Saudi Arabia. Egyp J Hospital Med. 2018;71:3504–3507. [Google Scholar]
- 111.AlQahtani MS, Alkhaldi TM, Al-Sultan AM, Bin Shihah AS, Aleid AS, Alzahrani ZK, et al. Sleeping disorders among medical students in Saudi Arabia; in relation to anti-insomnia medications. Egyp J Hospital Med. 2017;69(7):2750–2753. doi: 10.12816/0042561. [DOI] [Google Scholar]
- 112.Alshahrani MATY. Sleep hygiene awareness: its relation to sleep quality among medical students in King Saud University, Riyadh, Saudi Arabia. J Family Med Prim Care. 2019;8(8) [DOI] [PMC free article] [PubMed]
- 113.Asiri AK, Almetrek MA, Alsamghan AS, Mustafa O, Alshehri SF. Impact of Twitter and WhatsApp on sleep quality among medical students in King Khalid University, Saudi Arabia. Sleep Hypnosis (Online). 2018;20(4):247–252. doi: 10.5350/Sleep.Hypn.2018.20.0158. [DOI] [Google Scholar]
- 114.Atlam SAEH. Sleep habits and their association with daytime sleepiness among medical students of Tanta University, Egypt. Epidemiol Methods. 2020;1(1):1–10. [Google Scholar]
- 115.Attal BABM, Abdulqader A. Quality of sleep and its correlates among Yemeni medical students: a cross-sectional study. Sleep Disord. 2021;1(18) [DOI] [PMC free article] [PubMed]
- 116.Bahammam AS, Al-Khairy OK, Al-Taweel AA. Sleep habits and patterns among medical students. Neurosci J. 2005;10(2):159–162. [PubMed] [Google Scholar]
- 117.Belingheri MPA, Facchetti R, De Vito G, Cesana G, Riva MA. Self-reported prevalence of sleep disorders among medical and nursing students. Occupational Med. 2020;3(2):127–130. doi: 10.1093/occmed/kqaa011. [DOI] [PubMed] [Google Scholar]
- 118.Brick CA, Seely DL, Palermo TM. Association between sleep hygiene and sleep quality in medical students. Behav Sleep Med. 2010;8(2):113–121. doi: 10.1080/15402001003622925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Carpi MVA. The mediating role of sleep quality in the relationship between negative emotional states and health-related quality of life among Italian medical students. Int J Environ ResPublic Health. 2022;20(1):26–33. doi: 10.3390/ijerph20010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chatterjee S, Kar SK. Smartphone addiction and quality of sleep among Indian medical students. Psychiatry. 2021;84(2):182–191. doi: 10.1080/00332747.2021.1907870. [DOI] [PubMed] [Google Scholar]
- 121.Christodoulou N, Maruani J, d’Ortho M-P, Lejoyeux M, Geoffroy P. Sleep quality of medical students and relationships with academic performances. L’encephale. 2021;49 [DOI] [PubMed]
- 122.Copaja-Corzo CM-CB, Vizcarra-Jiménez D, Hueda-Zavaleta M, Rivarola-Hidalgo M, Parihuana-Travezaño EG, Taype-Rondan A. Sleep disorders and their associated factors during the COVID-19 pandemic: data from Peruvian medical students. Medicina. 2022;58(10):1325. doi: 10.3390/medicina58101325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Corrêa CC, Oliveira FK, Pizzamiglio DS, Ortolan EVP, Weber SAT. Sleep quality in medical students: a comparison across the various phases of the medical course. J Brasileiro de Pneumol. 2017;43:285–289. doi: 10.1590/s1806-37562016000000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Dhamija. Prevalence of smartphone addiction and its relation with sleep disturbance and low self- esteem among medical college students. Ind Psychiatry J. 2021;30(1):S189. doi: 10.4103/0972-6748.328813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Dudo KEE, Fuchs S, Herget S, Watzke S, Unverzagt S, Frese T. The association of sleep patterns and depressive symptoms in medical students: a cross-sectional study. BMC Res Notes. 2022;15(1):1–6. doi: 10.1186/s13104-022-05975-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Eleftheriou ARA, Arvaniti A, Nena E, Steiropoulos P. Sleep quality and mental health of medical students in Greece during the COVID-19 pandemic. Front Public Health. 2021;9:1823. doi: 10.3389/fpubh.2021.775374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Elwasify M, Barakat DH, Fawzy M, Elwasify M, Rashed I, Radwan DN. Quality of sleep in a sample of Egyptian medical students. Middle East Curr Psychiatry. 2016;23(4):200–207. doi: 10.1097/01.XME.0000490933.67457.d4. [DOI] [Google Scholar]
- 128.Ergin N, Kılıç BB, Ergin A, Varlı S. Sleep quality and related factors including restless leg syndrome in medical students and residents in a Turkish university. Sleep Breath. 2022;26(3):1299–1307. doi: 10.1007/s11325-021-02437-6. [DOI] [PubMed] [Google Scholar]
- 129.Feng Z, Diao Y, Ma H, Liu M, Long M, Zhao S, et al. Mobile phone addiction and depression among Chinese medical students: the mediating role of sleep quality and the moderating role of peer relationships. BMC Psychiatry. 2022;22(1):567. doi: 10.1186/s12888-022-04183-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Fernandes ACPD, de Moura AC, de Aquino CE, de Araújo Lima IB, Mota-Rolim SA. COVID-19 pandemic decreased sleep quality of medical students. Sleep Sci. 2022;15(4):436. doi: 10.5935/1984-0063.20220075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Fowler LAKN. The effect of COVID-19 pandemic stay-at-home orders on sleep deprivation in medical students: a retrospective study. SN. Soc Sci. 2022;2(3):29. doi: 10.1007/s43545-022-00323-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gui ZSL, Zhou C. Self-reported sleep quality and mental health mediate the relationship between chronic diseases and suicidal ideation among Chinese medical students. Sci Rep. 2022;12(1):18835. doi: 10.1038/s41598-022-23207-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gupta R, Taneja N, Anand T, Gupta A, Gupta R, Jha D, et al. Internet addiction, sleep quality and depressive symptoms amongst medical students in Delhi, India. Commun Mental Health J. 2021;57:771–776. doi: 10.1007/s10597-020-00697-2. [DOI] [PubMed] [Google Scholar]
- 134.Ibrahim N, Badawi F, Mansouri Y, Ainousa A, Jambi S, Fatani A. Sleep quality among medical students at King Abdulaziz University: a cross-sectional study. J Community Med Health Educ. 2017;7(561):2161–2711. [Google Scholar]
- 135.James BO, Omoaregba JO, Igberase OO. Prevalence and correlates of poor sleep quality among medical students at a Nigerian university. Ann Nigerian Med. 2011;5(1):1. doi: 10.4103/0331-3131.84218. [DOI] [Google Scholar]
- 136.Javaid R, Momina A, Sarwar MZ, Naqi SA. Quality of sleep and academic performance among medical university students. Medical Educ. 2020; [DOI] [PubMed]
- 137.EL JA, El Hangouche AJ, Rkain H, Aboudrar S, El Ftouh M, Dakka T. Perception of sleep disturbances due to bedtime use of blue light-emitting devices and its impact on habits and sleep quality among young medical students. BioMed Res Int. 2019;2019:12. doi: 10.1155/2019/7012350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Johnson KM, Simon N, Wicks M, Barr K, O’Connor K, Schaad D. Amount of sleep, daytime sleepiness, hazardous driving, and quality of life of second year medical students. Acad Psychiatry. 2017;41:669–673. doi: 10.1007/s40596-017-0668-6. [DOI] [PubMed] [Google Scholar]
- 139.Najafi Kalyani M, Jamshidi N, Salami J, Pourjam E. Investigation of the relationship between psychological variables and sleep quality in students of medical sciences. Depression Res Treat. 2017;2017 [DOI] [PMC free article] [PubMed]
- 140.Kawyannejad R, Mirzaei M, Valinejadi A, Hemmatpour B, Karimpour HA, AminiSaman J, et al. General health of students of medical sciences and its relation to sleep quality, cell phone overuse, social networks and internet addiction. BioPsychoSoc Med. 2019;13(1):1–7. doi: 10.1186/s13030-019-0150-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Khero M, Fatima M, Shah MAA, Tahir A. Comparison of the status of sleep quality in basic and clinical medical students. Cureus. 2019;11(3) [DOI] [PMC free article] [PubMed]
- 142.Kumar VA, Chandrasekaran V, Brahadeeswari H. Prevalence of smartphone addiction and its effects on sleep quality: a cross-sectional study among medical students. Ind Psychiatry J. 2019;28(1):82. doi: 10.4103/ipj.ipj_56_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kumar A, Aslami AN. Analgesics self-medication and its association with sleep quality among medical undergraduates. J Clin Diagn Res: JCDR. 2016;10(12):FC07. doi: 10.7860/JCDR/2016/22504.8953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Li M, Han Q, Pan Z, Wang K, Xie J, Zheng B, Lv J. Effectiveness of multidomain dormitory environment and roommate intervention for improving sleep quality of medical college students: a cluster randomised controlled trial in China. Int J Environ Res Public Health. 2022;19(22):15337. doi: 10.3390/ijerph192215337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lima P, Medeiros A, Araujo J. Sleep-wake pattern of medical students: early versus late class starting time. Braz J Med Biol Res. 2002;35:1373–1377. doi: 10.1590/S0100-879X2002001100016. [DOI] [PubMed] [Google Scholar]
- 146.Mahadule. Sleep quality and sleep hygiene in preclinical medical students of tertiary care center amidst COVID-19 pandemic: a cross-sectional observational study. Naational Library of Medicine2022. [DOI] [PMC free article] [PubMed]
- 147.Maheshwari G, Shaukat F. Impact of poor sleep quality on the academic performance of medical students. Cureus. 2019;11(4) [DOI] [PMC free article] [PubMed]
- 148.Mazar D, Gileles-Hillel A, Reiter J. Sleep education improves knowledge but not sleep quality among medical students. J Clin Sleep Med. 2021;17(6):1211–1215. doi: 10.5664/jcsm.9170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Meo SA, Alkhalifah JM, Alshammari NF, Alnufaie WS, Algoblan AF. Impact of COVID-19 pandemic on sleep quality among medical and general science students: King Saud University Experience. Pakistan J Med Sci. 2022;38(3Part-I):639. doi: 10.12669/pjms.38.3.5171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Mirghani HO. The effect of chronotype (morningness/eveningness) on medical students' academic achievement in Sudan. J Taibah Univ Med Sci. 2017;12(6):512–516. doi: 10.1016/j.jtumed.2017.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Mishra J, Panigrahi A, Samanta P, Dash K, Mahapatra P, Behera MR. Sleep quality and associated factors among undergraduate medical students during Covid-19 confinement. Clin Epidemiol Global Health. 2022;15:101004. doi: 10.1016/j.cegh.2022.101004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Mohammadbeigi A, Absari R, Valizadeh F, Saadati M, Sharifimoghadam S, Ahmadi A, et al. Sleep quality in medical students; the impact of over-use of mobile cellphone and social networks. J Res Health Sci. 2016;16(1):46. [PMC free article] [PubMed] [Google Scholar]
- 153.Nsengimana A, Mugabo E, Niyonsenga J, Hategekimana JC, Biracyaza E, Mutarambirwa R, et al. Sleep quality among undergraduate medical students in Rwanda: a comparative study. Sci Rep. 2023;13(1):265. doi: 10.1038/s41598-023-27573-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Olarte-Durand M, Roque-Aycachi JB, Rojas-Humpire R, Canaza-Apaza JF, Laureano S, Rojas-Humpire A, et al. Mood and sleep quality in Peruvian medical students during COVID-19 pandemic. Revista Colombiana de Psiquiatria. 2021; [DOI] [PubMed]
- 155.Patil A, Chaudhury S, Srivastava S. Eyeing computer vision syndrome: awareness, knowledge, and its impact on sleep quality among medical students. Ind Psychiatry J. 2019;28(1):68. doi: 10.4103/ipj.ipj_93_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Prashanth S, Kavyashree H, Krishnamurthy L, Deshpande D, Kalasuramath RPADS. Quality of sleep in medical students. J Public Health Med Res. 2015;3:8–10. [Google Scholar]
- 157.Priya J, Singh J, Kumari S, Res A. Study of the factors associated with poor sleep among medical students. Indian J Basic Appl Med Res. 2017;6(3):422–429. [Google Scholar]
- 158.Ramamoorthy S, Mohandas M, Sembulingam P, Swaminathan VR. Prevalence of excessive daytime sleepiness (EDS) among medical students. World. J Pharm Res. 2014;3(4)
- 159.Rathi A, Ransing RS, Mishra KK, Narula N. Quality of sleep among medical students: relationship with personality traits. J Clin Diagn Res. 2018;12(9)
- 160.Rique GLN, Fernandes Filho GMC, Ferreira ADC, de Sousa-Munoz RL. Relationship between chronotype and quality of sleep in medical students at the Federal University of Paraiba, Brazil. Sleep Sci. 2014;7(2):96–102. doi: 10.1016/j.slsci.2014.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Riskawati YK, Alfarabyn SU, Soeroso DA, Rakhmatiar R. The physical activity level of medical students does not correlate with their sleep quality and excessive daytime sleepiness (EDS). BIO Web of Conf: EDP Sci; 2022. p. 03003.
- 162.Safhi MA, Alafif RA, Alamoudi NM, Alamoudi MM, Alghamdi WA, Albishri SF, et al. The association of stress with sleep quality among medical students at King Abdulaziz University. J Fam Med Prim Care. 2020;9(3):1662. doi: 10.4103/jfmpc.jfmpc_745_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Saguem B, Nakhli J, Romdhane I, Nasr S. Predictors of sleep quality in medical students during COVID-19 confinement. L'encephale. 2022;48(1):3–12. doi: 10.1016/j.encep.2021.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Sarbazvatan H, Amini A, Aminisani N, Shamshirgaran SM. Sleep quality and academic progression among students of Tabriz University of Medical Sciences, Northwest of Iran. Res Dev Med Educ. 2017;6(1):29–33. doi: 10.15171/rdme.2017.006. [DOI] [Google Scholar]
- 165.Saygın M, Öztürk Ö, Gonca T, Has M, Hayri UB, Kurt Y, et al. Investigation of sleep quality and sleep disorders in students of medicine. Turk Thorac J. 2016;17(4):132. doi: 10.5578/ttj.30513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Shadzi MR, Salehi A, Vardanjani HM. Problematic internet use, mental health, and sleep quality among medical students: a path-analytic model. Ind J Psychol Med. 2020;42(2):128–135. doi: 10.4103/IJPSYM.IJPSYM_238_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Shrestha D, Adhikari SP, Rawal N, Budhathoki P, Pokharel S, Adhikari Y, et al. Sleep quality among undergraduate students of a medical college in Nepal during COVID-19 pandemic: an online survey. F1000Research. 2021;10(505):505. doi: 10.12688/f1000research.53904.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Sun J, Chen M, Cai W, Wang Z, Wu S, Sun X, et al. Chronotype: implications for sleep quality in medical students. Chronobiol Int. 2019;36(8):1115–1123. doi: 10.1080/07420528.2019.1619181. [DOI] [PubMed] [Google Scholar]
- 169.Sundas NGS, Bhusal S, Pandey R, Rana K, Dixit H. Sleep quality among medical students of a tertiary care hospital: a descriptive cross-sectional study. JNMA: J Nepal Med Assoc. 2020;58(222):76. doi: 10.31729/jnma.4813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Surani AA, Zahid S, Surani A, Ali S, Mubeen M, Khan RH. Sleep quality among medical students of Karachi, Pakistan. J Pak Med Assoc. 2015;65(4):380–382. [PubMed] [Google Scholar]
- 171.Tahir MJ, Malik NI, Ullah I, Khan HR, Perveen S, Ramalho R, Siddiqi AR, Waheed S, Shalaby MMM, De Berardis D, Jain S. Internet addiction and sleep quality among medical students during the COVID-19 pandemic: A multinational cross-sectional survey. PLOS One. 2021;16(11):e0259594. doi: 10.1371/journal.pone.0259594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Thaipisuttikul P, Theansukont T, Boonmueng R, Wisajun P. Sleep quality problems in Thai medical students. Sleep Sci. 2022;15(Spec 1):244. doi: 10.5935/1984-0063.20220023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wang Y, Zhao Y, Liu L, Chen Y, Ai D, Yao Y, et al. The current situation of internet addiction and its impact on sleep quality and self-injury behavior in Chinese medical students. Psychiatry Investig. 2020;17(3):237. doi: 10.30773/pi.2019.0131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wang L, Qin P, Zhao Y, Duan S, Zhang Q, Liu Y, et al. Prevalence and risk factors of poor sleep quality among Inner Mongolia Medical University students: a cross-sectional survey. Psychiatry Res. 2016;244:243–248. doi: 10.1016/j.psychres.2016.04.011. [DOI] [PubMed] [Google Scholar]
- 175.Wondie T, Molla A, Mulat H, Damene W, Bekele M, Madoro D, et al. Magnitude and correlates of sleep quality among undergraduate medical students in Ethiopia: cross–sectional study. Sleep Sci Pract. 2021;5(1):1–8. [Google Scholar]
- 176.Xie J, Li X, Luo H, He L, Bai Y, Zheng F, et al. Depressive symptoms, sleep quality and diet during the 2019 novel coronavirus epidemic in China: a survey of medical students. Front Public Health. 2021;8:588578. doi: 10.3389/fpubh.2020.588578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Yazdi Z, Loukzadeh Z, Moghaddam P, Jalilolghadr S. Sleep hygiene practices and their relation to sleep quality in medical students of Qazvin University of Medical Sciences. J Car Sci. 2016;5(2):153. doi: 10.15171/jcs.2016.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Yeluri. Electronic gadget screen-time, perceived sleep quality & quantity and academic performance in medical students. J Assoc Phys India. 2021;69(11):11–12. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1: Traffic light of the included studies.
Supplemental Figure 2: Funnel plot of poor sleep quality in medical students.
Supplemental Figure 3: Radial plot of poor sleep quality in medical students.
Supplemental Figure 4: Subgroup meta-analysis of poor sleep quality in medical students by COVID-19 status.
Supplemental Figure 5: Funnel plot of excessive daytime sleepiness in medical students.
Supplemental Figure 6: Radial plot of excessive daytime sleepiness in medical students.
Supplemental Figure 7: Subgroup meta-analysis of excessive daytime sleepiness in medical students by COVID-19 status.
Supplemental Figure 8: Funnel plot of the mean sleep duration in medical students.
Supplemental Figure 9: Radial plot of the mean sleep duration in medical students.
Supplemental Figure 10: Subgroup meta-analysis of the mean sleep duration in medical students by COVID-19 status.