Abstract
Background
Acute appendicitis is one of the most common surgical emergencies worldwide. Preoperative assessment of the risk of complicated appendicitis may aid in treatment planning. We sought to investigate the association between pre-appendectomy hyponatremia and diagnosis of complicated appendicitis.
Methods
The TriNetX platform, a federated health research network that aggregates de-identified electronic health record data of over 90 million patients across the United States, was queried for patients who underwent appendectomy starting January 2019 and who had at least one sodium value from the preoperative period. The study population was stratified into three age groups: pediatric (age < 18), adult (age 18–64), and older adult (age ≥ 65). These groups were subdivided into patients with preoperative hyponatremia (<135 mmol/L) and normonatremia (135–145 mmol/L).
Results
Among the 61,245 patients who met inclusion criteria, 17,546 were included for analysis following propensity score matching. The odds of complicated appendicitis were highest in pediatric patients (age < 18) with pre-appendectomy hyponatremia (odds ratio [OR] = 2.91, 95 % CI [2.53, 3.35]). Patients age 18–64 and aged ≥ 65 with preoperative hyponatremia also demonstrated increased odds of a complicated appendicitis diagnosis, but to a lesser extent (OR = 2.11, 95 % CI [1.92, 2.32] (OR = 1.49, 95 % CI [1.25, 1.77], respectively).
Conclusions
In a large analysis of matched patients with acute appendicitis, we found an association between immediate preoperative hyponatremia and complicated appendicitis. Future studies are indicated to further evaluate the role of hyponatremia as a potential diagnostic marker for complicated appendicitis in all age groups.
Key message
This study suggests a role of hyponatremia as one of multiple variables to incorporate into future clinical decision tools for complicated acute appendicitis.
Keywords: Hyponatremia, Appendectomy, Acute appendicitis, Complicated appendicitis
Highlights
-
•
Increased odds of complicated appendicitis with preoperative hyponatremia
-
•
Greatest effect observed in pediatric appendicitis patients with hyponatremia
-
•
Older adults had lowest odds of complicated appendicitis among all age groups.
-
•
Uncomplicated appendicitis less common in patients with preoperative hyponatremia
Introduction
Acute appendicitis is one of the most common surgical emergencies, with nearly 300,000 appendectomies performed in the United States annually [1]. Complicated appendicitis accounts for up to 25 % of appendectomies and includes cases that have progressed to perforation, gangrene, or abscess formation [[2], [3], [4]]. Perforation and gangrene are associated with worse postoperative outcomes, such as paralytic ileus and surgical site infection, that often lead to a prolonged hospital stay [[5], [6], [7]]. Uncomplicated cases of appendicitis are often amenable to nonoperative treatment with antibiotics, but the same cannot necessarily be said in cases of complicated appendicitis [6,[8], [9], [10], [11]]. Although there is disagreement in the literature [[10], [12]], some studies report that early recognition and treatment of complicated appendicitis may avoid inappropriate medical-only management and the associated delays in operative therapy, resulting in less patient morbidity and shorter hospital stays [[13], [14], [15]]. Therefore, early differentiation between complicated and uncomplicated cases is important in providing optimal care.
Computed tomography (CT) scans are commonly employed in the workup of acute appendicitis, particularly to increase diagnostic specificity. However, indications for abdominopelvic CT scans are far more restrictive in pediatric appendicitis workup. Despite efforts to decrease the exposure to ionizing radiation related to CT use in pediatric appendicitis, high CT utilization remains an issue [16], with one study finding that more than one-third or children undergo CT scan prior to surgery [17]. Identifying a reliable preoperative marker of complicated appendicitis has become a common theme in surgical literature in recent years, offering the potential to improve diagnostic accuracy without surgical intervention or ionizing radiation. Hyponatremia is one of several laboratory values that has been investigated as a marker of complicated appendicitis in both pediatric and adult populations. A recent single-center study of 129 patients over 14 years of age found that hyponatremia was a reliable predictor of perforation, gangrene, or abscess [18]; similar studies at other institutions corroborate these findings [19,20]. The largest adult-only retrospective study to date included 1550 patients and defined complicated appendicitis as either a perforated or gangrenous appendix. Based on exploratory logistic regression, four independent predictors for complicated appendicitis were identified by the authors, of which hyponatremia demonstrated the strongest association [3]. However, this study was limited by a single-center analysis. Large-scale, population-level data about the relationship between hyponatremia and complicated appendicitis has yet to be reported.
This study aims to further assess the risk of developing complicated appendicitis in patients with preoperative hyponatremia. We utilized a very large set of aggregated electronic health record (EHR) data to compare outcomes in the preoperative hyponatremia population to those with normal sodium measurements prior to surgery. We hypothesized that the preoperative hyponatremia group would reflect a higher incidence of pathologies associated with complicated appendicitis compared to the preoperative normonatremia group.
Materials and methods
Study population
Data for this study were obtained from the US Collaborative Network of the TriNetX Research Network platform, a global federated network of electronic health record (EHR) data. TriNetX provides access to continuously updated, de-identified aggregate EHR data including demographics, diagnoses (based on the International Classification of Diseases, Tenth Revision, Clinical Modification [ICD-10-CM] codes), procedures (coded in The International Classification of Diseases, Tenth Revision, Procedure Coding System [ICD-10-PCS], Current Procedural Terminology [CPT], and Systematized Nomenclature of Medicine [SNOMED] Clinical Terms), laboratory tests (coded in Logical Observation Identifiers Names and Codes [LOINC]), in addition to medications and genomics. TriNetX only contains de-identified EHR data and, for population level queries, has been deemed exempt by the MetroHealth System's Institutional Review Board (IRB) as defined in Section §164.514(b)(1) of the HIPAA Privacy Rule. At the time of investigation, the TriNetX US Collaborative Network contained aggregate data for 91,793,238 patients across 56 healthcare organizations (HCOs) across the United States.
We queried the platform to identify patients who underwent appendectomy according to CPT, ICD-10-PCS, and SNOMED codes related to appendectomy. Interval and incidental appendectomies were excluded, as well as any patients with a history of appendiceal malignancies, or “other appendicitis” (ICD-10-CM K36), utilized for chronic or recurrent appendicitis. A complete list of inclusion and exclusion criteria is available in Supplementary Data 1. Prior changes to ICD-10 coding for appendicitis have significantly affected related quality metrics [21]. Therefore, only surgeries occurring on or after January 1st 2019 were included for analysis as this marked the implementation of the current iteration of ICD-10 diagnosis codes for appendicitis [22,23]. Patients were stratified into three cohorts by age at the time of surgery: pediatric (age < 18 years old), adult (age 18–64), and older adult (age ≥ 65). These cohorts were further subdivided into those with hyponatremia (<135 mmol/L) and normonatremia (135–145 mmol/L) in the immediate preoperative setting. Age stratification was performed to account for the increasing rate of baseline hyponatremia among elderly patients [24], as well as the higher incidence of appendicitis in the pediatric population. Preoperative sodium levels were included for analysis if they occurred within three days before surgery. This inclusion period was selected to capture patients who may have been monitored expectantly for 1–2 days as recommended by certain practice guidelines [25]. Patient assignment to the hyponatremia cohort was based on any sodium measurement <135 mmol/L in the 3-day preoperative period, regardless of whether additional values were within normal limits in the same period. Thus, patients who initially presented with hyponatremia but normalized ahead of surgery were still included in the hyponatremia cohort. Inclusion in the normonatremia group required at least one sodium measurement within the 135–145 mmol/L range and no measurements below 135 mmol/L at any time in the 3-day preoperative period.
Measures and outcomes
Baseline characteristics of age, sex, race, and ethnicity were identified for each patient. If available, the most recent sodium lab value over a period ranging from 3 years to 14 days prior to the surgery was also included as part of the patient's baseline characteristics. Patients were not excluded if there was no baseline sodium value. This methodology was selected given the acute nature of appendicitis, which also most commonly affects younger patients, meaning that acute appendicitis may be the first presentation to a given HCO.
Severity of appendicitis was extrapolated from ICD-10-CM codes, which were evaluated from the day of surgery through the third postoperative day. Recent studies have demonstrated the difficulty of differentiating uncomplicated from complicated appendicitis, particularly when relying solely on ICD-10-CM diagnostic codes [21,26,27]. The clinical delineation between complicated and uncomplicated disease is also not entirely consistent in the literature. For example, one 2018 study proposed that gangrenous appendicitis can be treated as uncomplicated acute appendicitis, provided there are no other features of complex appendicitis (perforation, diffuse purulence outside of the pelvis, an extraluminal fecalith, or a well-formed abscess) [28].
In defining our categories of appendicitis severity, a similar approach to that of Georgeades et al. [29] was used, with two refinements: 1) gangrenous appendicitis without other complicating features was categorized separately from both uncomplicated appendicitis (without gangrene) and complicated appendicitis; and 2) only billable codes were included in our analysis to increase the likelihood that the diagnosis code was validated by clinical billing departments against physician documentation. Thus, non-specific “parent codes,” such as K35.8 were excluded from analysis (but K35.80, K35.890, and K35.891 were included).
In our analysis, uncomplicated appendicitis includes diagnosis codes without associated abscess, gangrene, or perforation; “unspecified appendicitis” (K37) was also included as it is included as a billable code and is also frequently used in cases of uncomplicated appendicitis. Uncomplicated appendicitis with gangrene was defined as a separate category, including codes K35.31 and K35.891. Lastly, complicated appendicitis was defined as any diagnosis associated with perforation, including K35.32 and K35.33 (acute appendicitis with perforation, localized peritonitis, and gangrene, with or without abscess, respectively). Acute appendicitis with generalized peritonitis (K35.20 and K35.21) was also included in the complicated appendicitis category, as the description of K35.2 also includes “appendicitis (acute) with generalized (diffuse) peritonitis following rupture or perforation of appendix” [23]. The complete list of relevant ICD-10-CM codes with associated descriptions and severity categorization is summarized in Supplementary Data 2.
Given the financial incentives associated with thorough documentation to achieve more valuable Medicare Severity Diagnosis-Related Group Principal Diagnosis (MS-DRG) codes, a secondary definition of complicated appendicitis was incorporated into our analysis. This definition is based on Centers for Medicare & Medicaid Services (CMS) criteria linked to a “complicated principal diagnosis” of appendicitis. This definition differs slightly from common clinical descriptions, in that it only includes codes K35.21, K35.22, and K35.33, but does not include K35.20 (acute appendicitis with generalized peritonitis without abscess) [30]. Collectively, excluding non-billable codes and including CMS billing criteria is intended to minimize the risk of confounding inherent in large aggregated databases, particularly given the inability to access pathological, operative and imaging reports.
Statistical analysis
To minimize the effect of confounding factors, propensity score matching was performed to generate study populations with similar baseline characteristics, including age at appendectomy, sex, race, ethnicity, and baseline sodium level (refer to Measures and Outcomes for explanation of baseline lab criteria). Cohort matching was performed with analytics functionality included with the TriNetX package, which performs 1:1 nearest neighbor greedy matching methodology with a caliper of 0.1 pooled standard deviations. The 3-day odds of outcomes were compared between the propensity score-matched hyponatremia cohort and normonatremia cohort. Overall event frequency, odds ratios, and 95 % confidence intervals (CI) were calculated. Separate analyses were performed across the three age groups; pediatric, adult, and older adult. All cohorts were individually balanced using the aforementioned methodology. All statistical tests were performed on the TriNetX platform on 4/6/2023 with a significance level set at p < 0.05.
Results
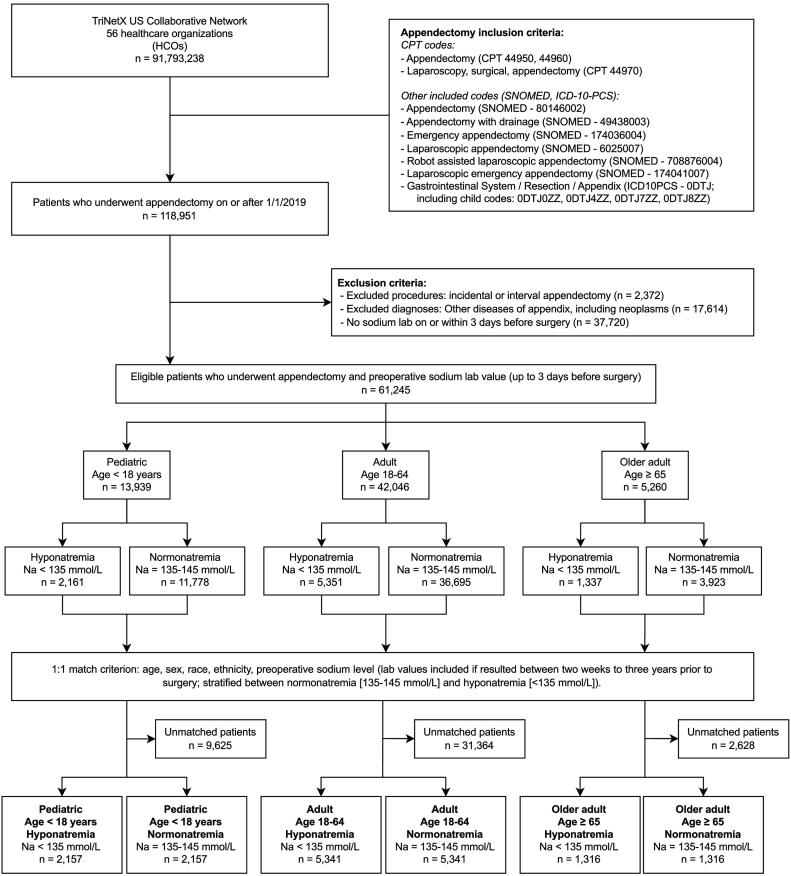
Between January 2019 and March 2023, 118,808 patients were identified as having undergone appendectomy. Of these patients, 61,245 met inclusion criteria (Fig. 1). The study population was stratified according to age at time of surgery: pediatric (age < 18, n = 13,939), adult (age 18–64, n = 42,046), and older adult (age ≥ 65, n = 5260). Each stratum was further subdivided into preoperative hyponatremia and normonatremia cohorts prior to propensity score matching (Supplementary Data 3). After matching, the pediatric cohort contained 2157 patients in both immediate preoperative hyponatremia and normonatremia groups, while the adult and older adult strata included 5341 and 1316 in each of their respective subgroups (Fig. 1). Prior to propensity matching, older patients were more likely to have baseline sodium values (14.3 % in pediatric, 37.2 % in adult, and 60.8 % in older adult patients, dated between 14 days and 3 years prior to appendectomy). Prior to matching, pediatric hyponatremia patients were more likely to be male, but this difference was not observed in non-pediatric cohorts (Supplemental Table 3). Pediatric patients with immediate preoperative hyponatremia were also slightly younger, with a mean age at surgery of 9.4 years, compared to 11.4 years in the normonatremia group. In the 18–64 age group, patients with immediate preoperative hyponatremia were older, with a mean age of 41.7, compared to 36.9 in the normonatremia subgroup. In the older adult cohort, mean age at surgery was relatively similar between the hyponatremia and normonatremia groups (72.5 and 71.9 years, respectively), despite their difference being statistically significant. Characteristics of propensity matched cohorts are summarized in Table 1.
Fig. 1.
Flow chart of cohort construction.
HCO, healthcare organization.
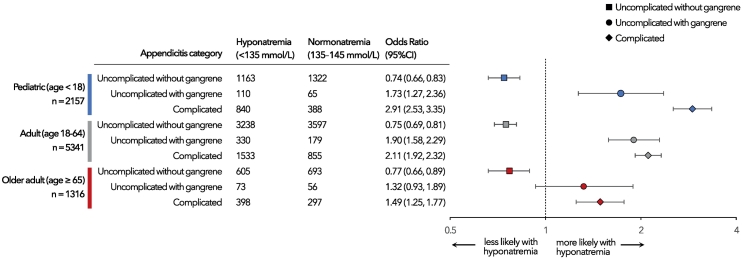
Across all subgroups, pediatric patients with pre-appendectomy hyponatremia demonstrated the strongest association with complicated appendicitis (odds ratio [OR] = 2.91, 95 % CI [2.53, 3.35]; Fig. 2). Conversely, older adults (age ≥ 65) with preoperative hyponatremia had the lowest odds of complicated appendicitis among all age groups. However, these odds were still increased compared to their normonatremic counterparts (OR = 1.49, 95 % CI [1.25, 1.77]). When restricting diagnosis codes to those meeting MS-DRG “complicated principal diagnosis” criteria (ICD-10-CM codes K35.21, K35.22, and K35.33), the odds ratio of complicated appendicitis was slightly higher across all strata with immediate preoperative hyponatremia (pediatric, age < 18, OR = 2.95, 95 % CI [2.55, 3.42]; adult, age 18–64, OR = 2.22, 95 % CI [2.01,2.45]; older adult, age ≥ 65, OR = 1.55, 95 % CI [1.30, 1.85] – see Supplementary Data 4). Both pediatric and adult cohorts demonstrated increased odds of uncomplicated appendicitis with gangrene when presenting with immediate preoperative hyponatremia (OR = 1.73, 95 % CI [1.27, 2.36] and OR = 1.90, 95 % CI [1.58, 2.29], respectively; Fig. 2). However, older adults with immediate preoperative hyponatremia did not demonstrate significantly increased odds of uncomplicated appendicitis with gangrene (OR = 1.32, 95 % CI [0.93, 1.89]). The odds of uncomplicated appendicitis were lower in patients with immediate preoperative hyponatremia across all three age strata (pediatric, age < 18, OR = 0.74, 95 % CI [0.66, 0.83]; adult, age 18–64, OR = 0.75, 95 % CI [0.69, 0.81]; older adult, age ≥ 65, OR = 0.77, 95 % CI [0.66, 0.89]).
Fig. 2.
Forest plot of age-stratified odds of appendicitis diagnosis in patients with pre-appendectomy hyponatremia compared to patients with preoperative normonatremia.
Discussion
The search for laboratory markers to aid in the clinical diagnosis of complicated acute appendicitis has become a popular endeavor in emergency and surgical research. There remains an unmet need for a generalizable, validated predictive model to delineate complicated from uncomplicated appendicitis prior to surgical intervention. Some of the most well-known clinical decision tools pertaining to appendicitis, such as the Alvarado Score and the Pediatric Appendicitis Score (PAS) are limited to ruling the diagnosis of acute appendicitis in or out. The latter is also specific to patients 3–18 years old. Greater generalizability, as well as validated risk stratification between uncomplicated and complicated appendicitis, will aid in treatment planning, surgery timing, and patient counseling.
While abdominal CTs have become a mainstay in appendicitis workup, they are not without their limitations, particularly in differentiating between uncomplicated and complicated appendicitis [31]. Perforation is a hallmark of complicated appendicitis and as such was utilized in our definition of complicated appendicitis for this study (the reader is directed to the Measures and outcomes section for full disease characterization, as well as Supplementary Data 2). A 2005 study by Foley et al. found that abdominal CT showed only moderate sensitivity in depicting appendiceal perforation [32], limiting clinicians' ability to definitively identify patients who are candidates for medical management of appendicitis. Abdominal computed tomography is also not without risks, as one study showed that the benefit of universal scanning for appendicitis (avoiding 12 negative appendectomies) came with a cost of one radiation-induced cancer death [33]. The impetus to avoid ionizing radiation is even greater in the pediatric population, who also represent the major age demographic for acute appendicitis. Multiple studies have found high CT utilization rates across many hospitals, despite specific guidelines against their use in children presenting with suspected appendicitis [16]; Childers et al. identified that more than one-third of children underwent abdominal CT scans prior to surgery, attributed primarily by transferring hospital.
Many researchers have investigated patient symptoms, clinical signs, lab values, and radiographic findings that distinguish complicated from uncomplicated appendicitis, including hyponatremia at time of presentation [3,[18], [19], [20],[34], [35], [36], [37]]. Hyponatremia has been identified as a marker of several other complicated infections, including necrotizing soft tissue infections, gangrenous cholecystitis, and ischemic or perforated bowel in small bowel obstruction [[38], [39], [40], [41]]. A review by Swart et al. describes a pathophysiologic mechanism that implicates increased interleukin-6 levels during inflammation. This cytokine is thought to mediate a cascade of non-osmotic secretion of antidiuretic hormone and resultant hyponatremia [42]. This immuno-neuroendocrine pathway may explain the pathophysiology behind hyponatremia in severe infectious processes, including complicated appendicitis.
Serum sodium measurement is a timely and routine clinical data point that may help delineate uncomplicated from complicated appendicitis, informing the assessment of which patients should proceed directly to surgery. In our study, we used a large set of aggregated EHR data to compare the frequency of complicated appendicitis based on patients' serum sodium levels prior to appendectomy. Among the 17,628 patients included in our analysis after propensity score matching, we found that patients with preoperative hyponatremia are significantly more likely than their normonatremic counterparts to be diagnosed with complicated appendicitis, which we defined as appendicitis with perforation. The association between immediate preoperative hyponatremia and complicated appendicitis was strongest in the youngest age cohort and weakest in the older adult group. This finding is particularly of interest given this age group stands to benefit the most from avoiding abdominal CT scans and the associated dose of ionizing radiation.
This study elucidates the potential of hyponatremia as a predictive marker for complicated appendicitis; utilizing the largest sample size to date, it corroborates findings of previous studies in both pediatric and adult populations [3,[18], [19], [20],[34], [35], [36], [37],43,44]. A single-center study of 129 patients over 14 years of age found that hyponatremia was significantly more common among patients with perforation or gangrene, at an incidence of 41.2 % in the complicated appendicitis group and 1.6 % in the non-complicated appendicitis group [18]. The largest available retrospective study of adult patients by Kim et al. found that preoperative hyponatremia had the strongest association with complicated appendicitis (OR = 2.8; 95 % CI [2.1–3.8]) compared to other possible predictors, including tachycardia, neutrophilia, and extended duration of pain [3]. Most published studies of adult patients have been retrospective, but a prospective study of 80 pediatric patients found a median plasma sodium concentration of 134 mmol/L in perforated cases and 139 mmol/L in non-perforated cases, with an odds ratio of 31.9 for perforation in hyponatremic patients [45]. Findings from large scale population studies, such as those presented here, offer a means to support the generalizability of results obtained through smaller, generally single-institution studies.
While this study adds to the body of knowledge regarding the potential to incorporate pre-appendectomy hyponatremia into clinical decision making, it is not without its limitations [3,16,17,28,29]. Most patients did not have multiple sodium levels from which to evaluate for chronic hyponatremia, which is a potential confounder and significantly more common among elderly patients [24,46]. However, >60 % of the older adult patients (age ≥ 65) did have baseline lab values from which we were able to perform propensity score matching, mitigating some of the potential confounding. Pediatric patients were least likely to have baseline labs for comparison, but they are also at a low risk of chronic hyponatremia.
Our cohort setup and binary categorization of sodium status were suitable to the TriNetX platform, but prevented us from performing a multivariate logistic regression, which may change the results of this study when other potentially predictive variables are included. However, our propensity-score matching approach accomplishes the equivalent task as logistic regression for those variables included in our propensity matching. Additionally, dichotomization of continuous variables (i.e. serum sodium levels), which was a limitation of the analytics tools, results in a potential loss of information, but typically leads to measurement of a small effect. Therefore, the true association between preoperative hyponatremia and complicated appendicitis may be greater than reported here [47].
As with any large aggregated EHR database, there is an inherent inability to validate diagnoses with manual chart review, specifically imaging, pathology, and operative reports in the case of appendicitis. As mentioned previously, diagnostic coding for acute appendicitis has presented numerous challenges over the years, not least with the transition from ICD-9 to ICD-10 coding [21,26,28,29]. Restricting our use of ICD-10-CM codes to billable codes and further narrowing criteria to those directly impacting MS-DRG level was intended to take advantage of health system financial incentives to enhance data validity (Supplementary Data 2, Supplementary Data 4). Given that the codes of greatest interest—those corresponding to complicated appendicitis—are also associated with increased reimbursement, we presume that documentation completeness and coding accuracy would be additionally supported by hospital billing and coding departments. Conversely, there is likely less incentive to differentiate between K35.80, Unspecified acute appendicitis and K37, Unspecified appendicitis, which clinicians in practice may use almost interchangeably, depending on their EHR setup. Both of the latter codes fall under the definition of “uncomplicated appendicitis” in this study, among others [29].
The reliance of TriNetX on diagnostic and procedural codes also potentially contributes to an underestimation of the risk of complicated appendicitis with hyponatremia. Only patients with a charted procedural code for appendectomy were included in our analysis (refer to Supplemental Data 1 for a complete list of codes). As such, patients who were managed non-operatively were not included in our analysis. Presumably, patients managed nonoperatively experience lower rates of complicated appendicitis diagnoses. Thus, their absence may diminish the odds of a complicated appendicitis diagnosis. However, patients managed nonoperatively also lack the surgical pathology, which is often used to confirm appendicitis diagnosis and severity, particularly in retrospective research studies. Therefore, regardless of the limitations inherent to studies utilizing aggregate EHR data, this population presents a challenge in terms of diagnosis validation.
Conclusion
This study offers a very large population-level analysis of the association between immediate preoperative hyponatremia and complicated appendicitis. The association between hyponatremia and complicated appendicitis is strongest among pediatric patients but is partially diminished in older patient cohorts. These findings contribute to a larger conversation about the preoperative identification of patients who might require more urgent surgery or who be more appropriately managed through non-operative options. Prospective studies evaluating the effect of hyponatremia (as well as other predictive markers) on complicated appendicitis are indicated.
The following are the supplementary data related to this article.
Description of inclusion and exclusion criteria and associated codes for cohort building.
Categorization of appendicitis severity used in outcomes analysis, with associated ICD-10-CM codes.
Descriptive characteristics of study populations, stratified by age group and preoperative hyponatremia, prior to propensity matching.
Age-stratified odds of appendicitis meeting MS-DRG “complicated principal diagnosis” criteria, among patients with pre-appendectomy hyponatremia, compared to those with normal preoperative sodium levels.
Funding sources
This project was supported in part by the Clinical and Translational Science Collaborative (CTSC) of Cleveland which is funded by the National Institutes of Health (NIH), National Center for Advancing Translational Science (NCATS), Clinical and Translational Science Award (CTSA) grant, UL1TR002548. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Ethics approval
This study was determined to be exempt by the MetroHealth System Institutional Review Board due to all the data being deidentified by a third-party database prior to obtaining access and query results only being at the population level. All statistical tests were performed on the TriNetx platform.
CRediT authorship contribution statement
Lauren M. Poston: conceptualization, investigation, formal analysis, writing (original draft). Tripp Leavitt: methodology, investigation, formal analysis, writing (reviewing & editing), visualization. Samantha Pope: project administration, writing (reviewing & editing). Hannah Hill: validation, resources, writing (reviewing & editing). Luis E. Tollinche: validation, supervision, writing (reviewing & editing). David C. Kaelber: methodology, resources, supervision, writing (reviewing & editing). Jonathan A. Alter: conceptualization, validation, supervision, writing (reviewing & editing).
Declaration of competing interest
Luis E. Tollinche is a grant recipient through Merck Investigator Studies Program (MISP) to fund a clinical trial at MSKCC (NCT03808077). LET serves a consultancy and advisory role for Merck & Co. Pharmaceutical Company. LET serves a consultancy and advisory role for GE Healthcare. LET receives stipend for his role as examiner with The American Board of Anesthesiology. These relationships have not conflicted with the quality or integrity of the work presented. The other authors have no competing interests to declare.
References
- 1.Livingston E.H., Woodward W.A., Sarosi G.A., Haley R.W. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg. 2007;245(6):886. doi: 10.1097/01.sla.0000256391.05233.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perez K.S., Allen S.R. Complicated appendicitis and considerations for interval appendectomy. J Am Acad Physician Assist. 2018;31(9):35–41. doi: 10.1097/01.JAA.0000544304.30954.40. [DOI] [PubMed] [Google Scholar]
- 3.Kim D.Y., Nassiri N., de Virgilio C., Ferebee M.P., Kaji A.H., Hamilton C.E., et al. Association between hyponatremia and complicated appendicitis. JAMA Surg. 2015;150(9):911–912. doi: 10.1001/jamasurg.2015.1258. [DOI] [PubMed] [Google Scholar]
- 4.Buckius M.T., McGrath B., Monk J., Grim R., Bell T., Ahuja V. Changing epidemiology of acute appendicitis in the United States: study period 1993–2008. J Surg Res. 2012;175(2):185–190. doi: 10.1016/j.jss.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 5.Ponsky T.A., Huang Z.J., Kittle K., Eichelberger M.R., Gilbert J.C., Brody F., et al. Hospital- and patient-level characteristics and the risk of appendiceal rupture and negative appendectomy in children. JAMA. 2004;292(16):1977–1982. doi: 10.1001/jama.292.16.1977. [DOI] [PubMed] [Google Scholar]
- 6.Romano A., Parikh P., Byers P., Namias N. Simple acute appendicitis versus non-perforated gangrenous appendicitis: is there a difference in the rate of post-operative infectious complications? Surg Infect (Larchmt) 2014;15(5):517–520. doi: 10.1089/sur.2013.106. [DOI] [PubMed] [Google Scholar]
- 7.Bhangu A., Søreide K., di Saverio S., Assarsson J.H., Drake F.T. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386(10000):1278–1287. doi: 10.1016/S0140-6736(15)00275-5. [DOI] [PubMed] [Google Scholar]
- 8.Sallinen V., Akl E.A., You J.J., Agarwal A., Shoucair S., Vandvik P.O., et al. Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br J Surg. 2016;103(6):656. doi: 10.1002/bjs.10147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Talan D.A., di Saverio S. Treatment of acute uncomplicated appendicitis. N Engl J Med. 2021;385(12):1116–1123. doi: 10.1056/NEJMcp2107675. [DOI] [PubMed] [Google Scholar]
- 10.Simillis C., Symeonides P., Shorthouse A.J., Tekkis P.P. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon) Surgery. 2010;147(6):818–829. doi: 10.1016/j.surg.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 11.Becker P., Fichtner-Feigl S., Schilling D. Clinical therapeutic review clinical management of appendicitis. Visc Med. 2018;34:453–458. doi: 10.1159/000494883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Helling T.S., Soltys D.F., Seals S. Operative versus non-operative management in the care of patients with complicated appendicitis. Am J Surg. 2017;214(6):1195–1200. doi: 10.1016/j.amjsurg.2017.07.039. [DOI] [PubMed] [Google Scholar]
- 13.Bonadio W., Rebillot K., Ukwuoma O., Saracino C., Iskhakov A. Management of pediatric perforated appendicitis: comparing outcomes using early appendectomy versus solely medical management. Pediatr Infect Dis J. 2017;36(10):937–941. doi: 10.1097/INF.0000000000001025. [DOI] [PubMed] [Google Scholar]
- 14.Gavriilidis P., de’Angelis N., Katsanos K., Saverio S. di. Acute appendicectomy or conservative treatment for complicated appendicitis (phlegmon or abscess)? A systematic review by updated traditional and cumulative meta-analysis. J Clin Med Res. 2019;11(1):56. doi: 10.14740/jocmr3672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Almeida Leite R.M., de Souza A.V., Bay C.P., Cauley C., Bordeianou L., Goldstone R., et al. Delayed operative management in complicated acute appendicitis—is avoiding extended resection worth the wait? Results from a global cohort study. J Gastrointest Surg. 2022;26(7):1482–1489. doi: 10.1007/s11605-022-05311-2. [DOI] [PubMed] [Google Scholar]
- 16.Hu A., Chaudhury A.S., Fisher T., Garcia E., Berman L., Tsao K., et al. Barriers and facilitators of CT scan reduction in the workup of pediatric appendicitis: a pediatric surgical quality collaborative qualitative study. J Pediatr Surg. 2022;57(11):582–588. doi: 10.1016/j.jpedsurg.2021.11.026. [DOI] [PubMed] [Google Scholar]
- 17.Childers C.P., Dworsky J.Q., Massoumi R.L., Shenoy R., Maggard-Gibbons M., Lee S.L., et al. The contemporary appendectomy for acute uncomplicated appendicitis in children. Surgery. 2019;165(5):1027–1034. doi: 10.1016/j.surg.2018.12.019. [DOI] [PubMed] [Google Scholar]
- 18.Symeonidis N.G., Pavlidis E.T., Psarras K.K., Stavrati K., Nikolaidou C., Marneri A., et al. Preoperative hyponatremia indicates complicated acute appendicitis. Surg Res Pract. 2022;2022:1–5. doi: 10.1155/2022/1836754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pérez-Soto R.H., Ponce de León-Ballesteros G., Álvarez-Bautista F., Trolle-Silva A.M., Medina-Franco H. Thrombocytosis and hyponatremia as predictors of complicated acute appendicitis. Predictors of appendicitis. J Surg Res. 2021;261:369–375. doi: 10.1016/j.jss.2020.12.050. [DOI] [PubMed] [Google Scholar]
- 20.Heymowski A., Boström L., Dahlberg M. Plasma sodium and age are important markers of risk of perforation in acute appendicitis. J Gastrointest Surg. 2021;25(1):287–289. doi: 10.1007/s11605-020-04753-w. [DOI] [PubMed] [Google Scholar]
- 21.Tian Y., Ingram M.C.E., Hall M., Raval M.V. ICD-10 transition influences trends in perforated appendix admission rate. J Surg Res. 2021;266:345–351. doi: 10.1016/j.jss.2021.04.028. [DOI] [PubMed] [Google Scholar]
- 22.2019 ICD-10-CM | CMS [Internet]. [cited 2023 Apr 17].
- 23.Centers for Disease Control and Prevention . 2017. ICD-10 coordination and maintenance committee meeting. March 7–8. [Diagnosis Agenda] [Google Scholar]
- 24.Upadhyay A., Jaber B.L., Madias N.E. Incidence and prevalence of hyponatremia. Am J Med. 2006;119(7 Suppl 1) doi: 10.1016/j.amjmed.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 25.Smink D., Soybel D. In: Management of acute appendicitis in adults. Weiser M., Chen W., editors. 2023. UpToDate. [cited 2023 Apr 17] [Google Scholar]
- 26.Bouchard M.E., Kan K., Tian Y., Casale M., Smith T., De Boer C., et al. Association between neighborhood-level social determinants of health and access to pediatric appendicitis care. JAMA Netw Open. 2022;5(2) doi: 10.1001/jamanetworkopen.2021.48865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fonnes S., Erichsen R., Rosenberg J. Validity of the coding for appendicitis, appendectomy, and diagnostic laparoscopy in the Danish National Patient Registry. Scand J Surg. 2023;112(1):48–55. doi: 10.1177/14574969221148078. [DOI] [PubMed] [Google Scholar]
- 28.Nordin A.B., Diefenbach K., Sales S.P., Christensen J., Besner G.E., Kenney B.D. Gangrenous appendicitis: no longer complicated. J Pediatr Surg. 2019;54(4):718–722. doi: 10.1016/j.jpedsurg.2018.10.064. [DOI] [PubMed] [Google Scholar]
- 29.Georgeades C., Farazi M.R., Gainer H., Flynn-O’Brien K.T., Leys C.M., Gourlay D., et al. Distribution of acute appendicitis care in children: a statewide assessment of the surgeons and facilities providing surgical care. Surgery. 2023;173(3):765–773. doi: 10.1016/j.surg.2022.06.053. [DOI] [PubMed] [Google Scholar]
- 30.ICD-10-CM/PCS MS-DRG v37.0 definitions manual [Internet] 2019. [cited 2023 Apr 17] [Google Scholar]
- 31.Gaskill C.E., Simianu V.V., Carnell J., Hippe D.S., Bhargava P., Flum D.R., et al. Use of computed tomography to determine perforation in patients with acute appendicitis. Curr Probl Diagn Radiol. 2018;47(1):6–9. doi: 10.1067/j.cpradiol.2016.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Foley T.A., Earnest F., IV, Nathan M.A., Hough D.M., Schiller H.J., Hoskin T.L. Differentiation of nonperforated from perforated appendicitis: accuracy of CT diagnosis and relationship of CT findings to length of hospital stay. Radiology. 2005;235(1):89–96. doi: 10.1148/radiol.2351040310. [DOI] [PubMed] [Google Scholar]
- 33.Rogers W., Hoffman J., Noori N. Harms of CT scanning prior to surgery for suspected appendicitis. Evid Based Med. 2015;20(1):3–4. doi: 10.1136/ebmed-2014-110075. [DOI] [PubMed] [Google Scholar]
- 34.Pogorelić Z., Lukšić B., Ninčević S., Lukšić B., Polašek O. Hyponatremia as a predictor of perforated acute appendicitis in pediatric population: a prospective study. J Pediatr Surg. 2021;56(10):1816–1821. doi: 10.1016/j.jpedsurg.2020.09.066. [DOI] [PubMed] [Google Scholar]
- 35.Giannis D., Matenoglou E., Moris D. Hyponatremia as a marker of complicated appendicitis: a systematic review. Surgeon. 2020;18(5):295–304. doi: 10.1016/j.surge.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 36.Zhan W., Deng W., Liu Y., Feng S. Hyponatremia as a predictor of complicated appendicitis in children: a systematic review and meta-analysis. Asian J Surg. 2022;45(10):2009–2011. doi: 10.1016/j.asjsur.2022.04.058. [DOI] [PubMed] [Google Scholar]
- 37.Pham X.B.D., Sullins V.F., Kim D.Y., Range B., Kaji A.H., de Virgilio C.M., et al. Factors predictive of complicated appendicitis in children. J Surg Res. 2016;206(1):62–66. doi: 10.1016/j.jss.2016.07.023. [DOI] [PubMed] [Google Scholar]
- 38.Wong C.H., Khin L.W., Heng K.S., Tan K.C., Low C.O. The LRINEC (laboratory risk indicator for necrotizing fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med. 2004;32(7):1535–1541. doi: 10.1097/01.ccm.0000129486.35458.7d. [DOI] [PubMed] [Google Scholar]
- 39.Yaghoubian A., de Virgilio C., Dauphine C., Lewis R.J., Lin M. Use of admission serum lactate and sodium levels to predict mortality in necrotizing soft-tissue infections. Arch Surg. 2007;142(9):840–846. doi: 10.1001/archsurg.142.9.840. [DOI] [PubMed] [Google Scholar]
- 40.Falor A.E., Zobel M., Kaji A., Neville A., de Virgilio C. Admission variables predictive of gangrenous cholecystitis. Am Surg. 2012;78(10):1075–1078. [PubMed] [Google Scholar]
- 41.O’Leary M.P., Neville A.L., Keeley J.A., Kim D.Y., de Virgilio C., Plurad D.S. Predictors of ischemic bowel in patients with small bowel obstruction. Am Surg. 2016;82(10):992–994. [PubMed] [Google Scholar]
- 42.Swart R.M., Hoorn E.J., Betjes M.G., Zietse R. Hyponatremia and inflammation: the emerging role of interleukin-6 in osmoregulation. Nephron Physiol. 2011;118(2):p45–p51. doi: 10.1159/000322238. [DOI] [PubMed] [Google Scholar]
- 43.Sasaki Y., Komatsu F., Kashima N., Suzuki T., Takemoto I., Kijima S., et al. Clinical prediction of complicated appendicitis: a case-control study utilizing logistic regression. World J Clin Cases. 2020;8(11):2127. doi: 10.12998/wjcc.v8.i11.2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walsh A., Lala S., Wells C., Upadhyay V. Hyponatremia an indicator of complicated appendicitis in children: starship experience. ANZ J Surg. 2022;92(4):747–752. doi: 10.1111/ans.17425. [DOI] [PubMed] [Google Scholar]
- 45.Lindestam U., Almström M., Jacks J., Malmquist P., Lönnqvist P.A., Jensen B.L., et al. Low plasma sodium concentration predicts perforated acute appendicitis in children: a prospective diagnostic accuracy study. Eur J Pediatr Surg. 2020;30(4):350–356. doi: 10.1055/s-0039-1687870. [DOI] [PubMed] [Google Scholar]
- 46.Filippatos T.D., Makri A., Elisaf M.S., Liamis G. Hyponatremia in the elderly: challenges and solutions. Clin Interv Aging. 2017;12:1957–1965. doi: 10.2147/CIA.S138535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nuzzo R.L. Making continuous measurements into dichotomous variables. PM&R. 2019;11(10):1132–1134. doi: 10.1002/pmrj.12228. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of inclusion and exclusion criteria and associated codes for cohort building.
Categorization of appendicitis severity used in outcomes analysis, with associated ICD-10-CM codes.
Descriptive characteristics of study populations, stratified by age group and preoperative hyponatremia, prior to propensity matching.
Age-stratified odds of appendicitis meeting MS-DRG “complicated principal diagnosis” criteria, among patients with pre-appendectomy hyponatremia, compared to those with normal preoperative sodium levels.