Abstract
Objective
To report the incidence of and evaluate demographic, ocular comorbidities, and intraoperative factors for rhegmatogenous retinal detachment (RRD) and retinal tear (RT) after cataract surgery in the American Academy of Ophthalmology IRIS® Registry (Intelligent Research in Sight).
Design
Retrospective cohort study.
Participants
Patients aged ≥ 40 years who underwent cataract surgery between 2014 and 2017.
Methods
Multivariable logistic regression was used to evaluate demographic, comorbidity, and intraoperative factors associated with RRD and RT after cataract surgery.
Main Outcome Measures
Incidence and risk factors for RRD or RT within 1 year of cataract surgery.
Results
Of the 3 177 195 eyes of 1 983 712 patients included, 6690 (0.21%) developed RRD and 5489 (0.17%) developed RT without RRD within 1 year after cataract surgery. Multivariable logistic regression odds ratios (ORs) showed increased risk of RRD and RT, respectively, among men (OR 3.15; 95% confidence interval [CI], 2.99–3.32; P < 0.001 and 1.79; 95% CI, 1.70–1.89; P < 0.001), and younger ages compared with patients aged > 70, peaking at age 40 to 50 for RRD (8.61; 95% CI, 7.74–9.58; P < 0.001) and age 50 to 60 for RT (2.74; 95% CI, 2.52–2.98; P < 0.001). Increased odds of RRD were observed for procedure eyes with lattice degeneration (LD) (10.53; 95% CI, 9.82–11.28; P < 0.001), hypermature cataract (1.61; 95% CI, 1.06–2.45; P = 0.03), complex cataract surgery (1.52; 95% CI, 1.4–1.66; P < 0.001), posterior vitreous detachment (PVD) (1.24; 95% CI, 1.15–1.34; P < 0.001), and high myopia (1.2; 95% CI, 1.14–1.27; P < 0.001). Lattice degeneration conferred the highest odds of RT (43.86; 95% CI, 41.39–46.49; P < 0.001).
Conclusion
In the IRIS Registry, RRD occurs in approximately 1 in 500 cataract surgeries in patients aged > 40 years within 1 year of surgery. The presence of LD conferred the highest odds for RRD and RT after surgery. Additional risk factors for RRD included male gender, younger age, hypermature cataract, PVD, and high myopia. These data may be useful during the informed consent process for cataract surgery and help identify patients at a higher risk of retinal complications.
Financial Disclosure(s)
The author(s) have no proprietary or commercial interest in any materials discussed in this article.
Keywords: Cataract surgery, High myopia, Lattice degeneration, Rhegmatogenous retinal detachment, Retinal tear
Cataract surgery is one of the most commonly performed surgical procedures in the United States, with > 2 million surgeries performed annually.1 The volume of cataract surgery in the United States has increased steadily over the past decades, reflecting an increase in the population age and associated increase in cataract development.2, 3, 4, 5
Although cataract surgery is safe and effective in improving vision and visual functioning, postsurgical complications may occur. Rhegmatogenous retinal detachments (RRDs) and retinal tears (RTs) without RRD are uncommon but serious complications that may occur after cataract surgery and potentially result in reduced visual acuity.6,7 Several studies have investigated the incidence of these events after cataract surgery in a retrospective series. A 2020 literature review that included 16 studies found the 10-year incidence of RRD after phacoemulsification cataract surgery to range between 0.36% and 2.9%.8 This literature review also indicated that demographic features (age and sex), ocular comorbidities (lattice degeneration [LD] and high myopia), and intraoperative complications (posterior capsular rupture [PCR]) may increase the risk of RRD.8
The American Academy of Ophthalmology IRIS® Registry (Intelligent Research in Sight), a large national registry containing > 70 million patient records, offers an opportunity to study the incidence and risk factors for RRDs and RTs in patients undergoing modern phacoemulsification cataract surgery in practices across the United States.9 This report analyzed > 3 million cataract operations identified in the IRIS Registry from 2014 to 2017 to estimate the frequency of RRD and RT without RRD within 1 year after cataract surgery, evaluated demographic and ocular risk factors for retinal events postcataract surgery, and compared differences in rates of retinal events among uncomplicated and complicated cataract procedures.
Methods
Primary Data Source
The data used in this study come from the American Academy of Ophthalmology IRIS Registry. This consists of clinical information directly extracted from electronic health records.9, 10, 11 As of October 2021, the IRIS Registry contained data on > 70.8 million distinct patients across the United States.10 Data collection and aggregation methods for the IRIS Registry database have previously been described.12 The IRIS Registry contains data sets of unique, randomly-generated identifiers for patients mapped to demographic features, structured diagnosis and procedure codes, and clinical observation, including visual acuity.12 For this study, we utilized a version of the data set codenamed Chicago (version V), last modified on April 16, 2021. This study adhered to the tenets of the Declaration of Helsinki. Given the use of deidentified patient data from an established database, the study was exempt from the Wills Eye Hospital Institutional Review Board review. Data were queried from the IRIS Registry using PostgreSQL 8.0.2. Statistical analysis and descriptive statistics were generated using R (https://www.r-project.org/).
Study Population
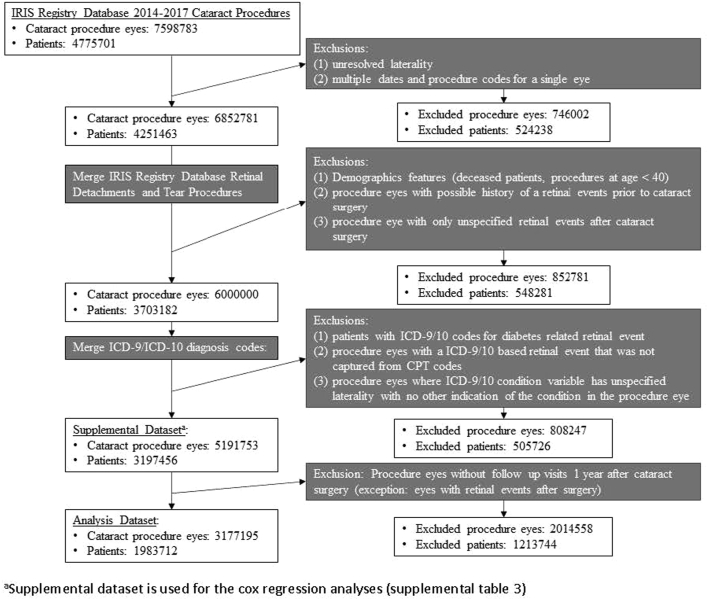
All patient eyes receiving cataract surgery from 2014 to 2017 were considered for inclusion in these analyses. The inclusion methodology is summarized in Figure 1. Cataract surgery procedures were identified by the Current Procedural Terminology (CPT) codes of 66982, 66983, and 66984. To be included, the determination of procedure laterality was required, which amounted to 90.2%, (6 852 781/7 598 783) of the unique cataract procedure eye entries in the IRIS Registry. Cataract procedures with procedure eyes designated as “bilateral” or “unspecified” went through the after resolution process for inclusion. Bilateral cataract procedures identified as immediate sequential bilateral procedures, i.e., duplicate procedures codes on the same date with 1 entry as “bilateral,” were included as separate entries for the left and right eyes. For cataract procedures designated “unspecified,” visual acuity data on postoperative day 1 was used to resolve laterality. If visual acuity data were present the day after a cataract procedure and specified to be in a single eye, the unspecified cataract procedure was adjusted to the procedure eye noted in the visual acuity results. Bilateral and unspecified procedure eyes that were not resolved after this process were excluded.
Figure 1.
IRIS (Intelligent Research in Sight) Registry Data Processing Methodology. ICD = International Classification of Diseases.
Additional exclusion criteria included: cataract procedures in patients aged < 40 years, patients with a history of diabetic retinopathy in either eye, and procedure eyes with a history of RRD or RT based on the preoperative presence of a relevant CPT or International Classification of Diseases (ICD) 9/ICD10 code. Finally, to be included in the logistic regression analyses, procedure eyes had to have either (1) an outcome event (RRD or RT) within 1 year after cataract surgery or (2) no outcome event with follow-up visits up to 1 year after cataract surgery. These criteria refined the number of cataract procedures included in the logistic regression analyses from 5 191 753 to 3 177 195.
Outcome Variables – RRD and RT
The outcome measure for this study was the incidence rate (IR) of RRD or RT without RRD occurring within 1 year of cataract surgery. Retinal events were identified by CPT codes for RRD (67101, 67105, 67107, 67108, 67110, and 67113) and RT (67141 and 67145). For the purpose of this report, RT without RRD was defined as any indication for performing CPT codes 67141 or 67145. The retinal procedures selected for inclusion in the data analyses went through the same resolution process as performed with the cataract procedure data. However, procedure eyes designated as “bilateral” and “unspecified” that were not resolved after this process were retained in the data set.
Data on cataract procedure code, laterality of cataract surgery, and days between cataract surgery and RRD or RT were obtained. These clinical variables were used to calculate days between cataract surgery and retinal events (RRD or RT) within 1 year of cataract surgery.
Patient Characteristics, Comorbid Ophthalmic Conditions, and Indicators of Cataract Surgery Complexity
Demographic characteristics (age [years], birth sex, race, and ethnicity) and ophthalmic comorbidities (presence of posterior vitreous detachment (PVD) before cataract surgery, LD, high myopia, hypermature cataract, pseudoexfoliation, and floppy iris syndrome) were identified from the IRIS Registry using the appropriate ICD9/ICD10 diagnosis codes. Indicators of cataract surgery complexity included ICD9/ICD10 codes for hypermature cataract, pseudoexfoliation, floppy iris syndrome, and use of the complex cataract surgery CPT code 66982. Mappings of the ICD9/ICD10 diagnosis codes are shown in Table S1 (available at www.ophthalmologyscience.org).
For specific ophthalmic comorbidities (high myopia, floppy iris syndrome, and pseudoexfoliation), bilaterality was assumed if the condition was present in 1 eye. Other comorbidities (PVD, LD, and hypermature cataract) were assumed to only be present in the eyes specified in the data (left, right, bilateral [adjusted to entries of left and right], and unspecified).
Statistical Analyses
The incidence of RRD and RT was estimated within 1 year after cataract surgery. Chi-square tests were used to assess the association between demographic characteristics and each of the following: RRD, RT, and any retinal event (RRD or RT). Risk factors assessed included demographics (age [categorical], sex, race, and ethnicity), comorbidities (LD, PVD, and high myopia), and intraoperative factors associated with surgery complexity (hypermature cataract, pseudoexfoliation, floppy iris syndrome, and complex surgery CPT code 66982). Univariable and multivariable analyses (logistic regression models) were used to estimate odds ratios (ORs) with 95% confidence intervals (CIs) for each demographic feature, ocular comorbidity, and intraoperative factor as calculated from the model coefficients. Confidence intervals for each OR were computed using the Wald method. A 2-sided P value of < 0.05 was considered statistically significant.
A separate Cox regression analysis was completed, which includes procedure eyes without follow-up visits up to 1 year after cataract surgery and adjusts for a time parameter of days from the cataract procedure to the most recent patient visit.
Results
Study Population and IRs of RRD and RT Postcataract Surgery
A total of 3 177 195 cataract procedures (eyes) in 1 983 712 patients from the IRIS Registry between 2014 and 2017 were included in this study. One-year incidence of events, overall and by demographic characteristics, are summarized in Table 2. A total of 6690 (0.21%) RRDs, 5489 (0.17%) RTs, and 11 676 (0.37%) of either event were identified as occurring within 1 year after cataract surgery. The 1-year incidence of RRD after cataract surgery was higher for younger than older adults (1.01%, 0.62%, 0.25%, and 0.10% for cataract procedures at ages [year] 40–50, 51–60, 61–70, and > 70, respectively; P < 0.001), for men than women (0.37% vs. 0.11%; P < 0.001), for White than Asian and Black patients (0.23% vs. 0.16% and 0.13%; P < 0.001), and for non-Hispanic and non-Latino ethnicities than Hispanic and Latino ethnicities (0.23% vs. 0.19%, P = 0.001).
Table 2.
Incidence (per 100; %) of RRDs and RTs within 1 Year after Cataract Surgery by Demographic Characteristics
| Characteristic | Group | Cataract Procedures |
Retinal Events (RRD or RT) |
RRD |
RT |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | Incidence Rate (%) | P Value (Chi-square Test) | n | Incidence Rate (%) | P Value (Chi-square Test) | n | Incidence Rate (%) | P Value (Chi-square Test) | ||
| All procedures | Total | 3 177 195 | NA | 11 676 | 0.37 | NA | 6690 | 0.21 | NA | 5489 | 0.17 | NA |
| Age at surgery (yrs) | 40–50 | 45 969 | 1 | 590 | 1.28 | < 0.001 | 464 | 1.01 | < 0.001 | 157 | 0.34 | < 0.001 |
| 51–60 | 275 219 | 9 | 2565 | 0.93 | 1698 | 0.62 | 1008 | 0.37 | ||||
| 61–70 | 1 195 134 | 38 | 5559 | 0.47 | 2947 | 0.25 | 2867 | 0.24 | ||||
| > 70 | 1 660 873 | 52 | 2962 | 0.18 | 1581 | 0.10 | 1457 | 0.09 | ||||
| Sex | Female | 1 963 770 | 62 | 4648 | 0.24 | < 0.001 | 2243 | 0.11 | < 0.001 | 2574 | 0.13 | < 0.001 |
| Male | 1 213 425 | 38 | 7028 | 0.58 | 4447 | 0.37 | 2915 | 0.24 | ||||
| Race | Asian | 73 937 | 2 | 240 | 0.32 | < 0.001∗ | 116 | 0.16 | < 0.001 | 128 | 0.17 | < 0.001 |
| Black or African American | 188 446 | 6 | 478 | 0.25 | 251 | 0.13 | 236 | 0.13 | ||||
| White | 2 498 683 | 79 | 9900 | 0.40 | 5744 | 0.23 | 4614 | 0.18 | ||||
| Other | 27 951 | 1 | 159 | 0.57 | 81 | 0.29 | 85 | 0.30 | ||||
| Unknown | 388 178 | 12 | 899 | 0.23 | 498 | 0.13 | 426 | 0.11 | ||||
| Ethnicity | Hispanic or Latino | 190 370 | 6 | 632 | 0.33 | < 0.001† | 363 | 0.19 | 0.001 | 288 | 0.15 | 0.001 |
| Not Hispanic or Latino | 2 535 675 | 80 | 9990 | 0.39 | 5767 | 0.23 | 4667 | 0.18 | ||||
| Unknown | 451 150 | 14 | 1054 | 0.23 | 560 | 0.12 | 534 | 0.12 | ||||
RRD = rhegmatogenous retinal detachment; RT = retinal tear.
∗For race, entries labeled as unknown were excluded from chi-square test allowing for comparison between White, Black, and Asian races.
†For ethnicity, entries labeled as unknown were excluded from chi-square test allowing for comparison between Hispanic or Latino and Non-Hispanic or Latino.
Similarly, the 1-year incidence of RT after cataract surgery was also higher for men than women (0.24% vs. 0.13%; P < 0.001), for White than Asian and Black patients (0.18% vs. 0.17% and 0.13%; P < 0.001), and for non-Hispanic and non-Latino ethnicities than Hispanic and Latino ethnicities (0.18% vs. 0.15%, P = 0.001). For age at cataract surgery, the incidence of postcataract RT was highest at ages 40 to 60 years (0.34% for 40–50 years and 0.37% for 51–60 years) and then decreased for older ages (0.24%, and 0.09% for cataract procedures at ages 61–70 years, and > 70 years; P < 0.001),
The IR of RRD and RT by the year (2014–2017) are noted in Table S3 (available at www.ophthalmologyscience.org).
Time Course of Retinal Events Postcataract Surgery
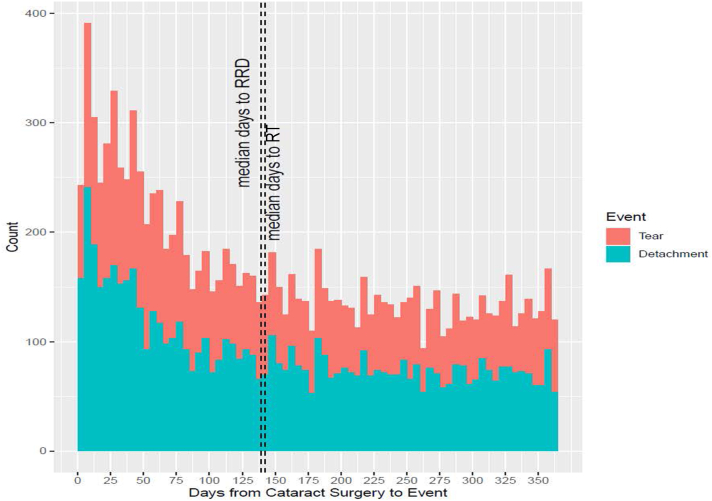
The timing of all RRD and RT within a 1-year period after cataract surgery is depicted in Figure 2. The timing of events after cataract surgery was similar for RRD and RT. Rhegmatogenous retinal detachment occurred at a median of 139 days (first–third quartiles, 50–246 days) after cataract surgery, and RT occurred at a median of 142 days (first–third quartiles, 58–251 days) after cataract surgery. Overall, 15.9% of RRD and 13.3% of RT occurred within 1 month (30 days) after cataract surgery, 37.3% of RRD and 29.7% of RT occurred within 3 months (90 days) after cataract surgery, and 59.9% of RRD and 48.5% of RT occurred within 6 months (180 days) after cataract surgery.
Figure 2.
Frequency of retinal events (rhegmatogenous retinal detachment [RRD] and retinal tear [RT]) by day after cataract surgery.
Risk Factors for RRD and RT Postcataract Surgery
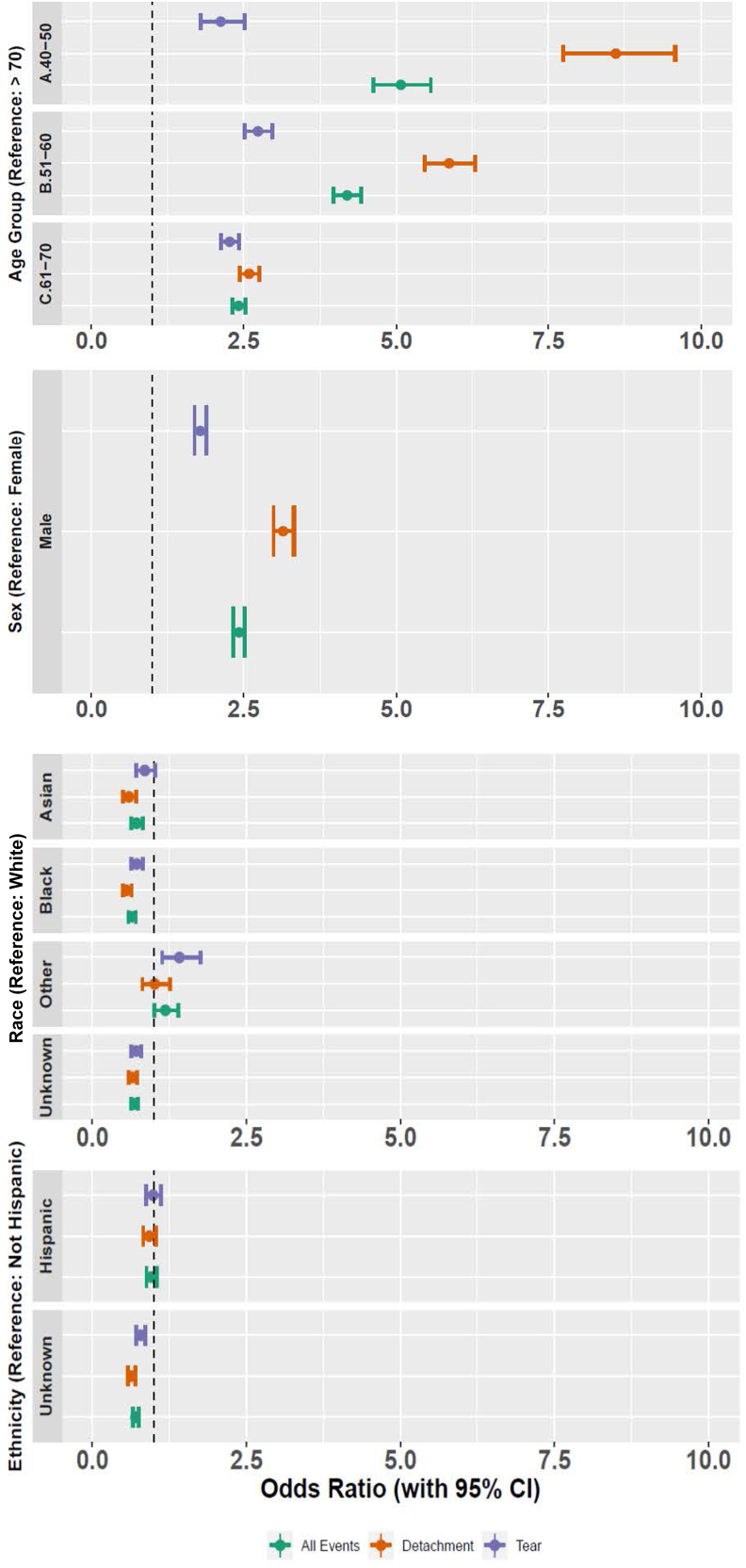
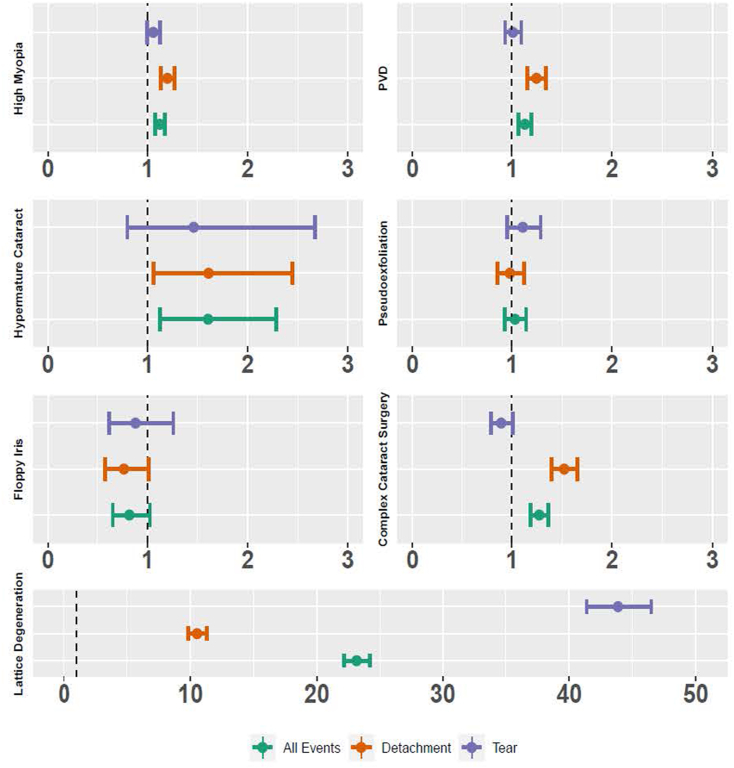
Results of univariable and multivariable logistic regression analyses assessing demographic features, comorbidities, and indicators of cataract surgery complexity as risk factors for RRD or RT without RRD are presented in Tables 2 and 3 and Figures 3 and 4, and are described below.
Figure 3.
Forest plots of odds ratios (95% confidence interval [CI]) for rhegmatogenous retinal detachments and retinal tears after cataract surgery by demographic characteristic.
Figure 4.
Forest plots of odds ratios for rhegmatogenous retinal detachments and retinal tears after cataract surgery by comorbidities and cataract surgery complexity factors. PVD = posterior vitreous detachment.
RRD
Demographic features
Demographic features associated with retinal events after cataract surgery are summarized in Table 4 and Figure 3. Odds ratios based on multivariate logistic regression revealed an increased risk of RRD 1 year after cataract surgery for cataract procedures at 40 to 50 years of age (8.61; 95% CI, 7.74–9.54; P < 0.001), 51 to 60 years of age (5.87; 95% CI, 5.47–6.29; P < 0.001), and 61 to 70 years of age (2.59; 95% CI, 2.44–2.76; P < 0.001) when compared with procedures at > 70 years of age. Multivariable logistic regression results also showed an increased risk of RRD for men compared with women (3.15; 95% CI, 2.99–3.32; P < 0.001), and decreased risk of RRD for Black (0.56; 95% CI, 0.49–0.64; P < 0.001) and Asian (0.59; 95% CI, 0.49–0.71; P < 0.001) patients when compared with White patients. The OR for Hispanic or Latino ethnicity was not statistically significant when compared with non-Hispanic or Latino ethnicity in multivariable regression analysis.
Table 4.
Multivariable ORs of RRDs or RTs after Cataract Surgery by Demographic Characteristics
| Demographic Characteristics | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographic Category | Group | Cataract Procedures | Retinal Events (RRD or RT) |
RRD |
RT |
|||||||||
| Uni OR (95% CI)∗ | P Value | Multi-OR (95% CI)† | P Value | Uni OR (95% CI)∗ | P Value | Multi-OR (95% CI)† | P Value | Uni OR (95% CI)∗ | P Value | Multi-OR (95% CI)† | P Value | |||
| All Procedures | NA | 3 177 195 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Age at Surgery (yrs) | > 70 | 1 660 873 | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) |
| 61-70 | 1 195 134 | 2.62 (2.5−2.74) | < 0.001 | 2.42 (2.31−2.53) | < 0.001 | 2.59 (2.44−2.76) | < 0.001 | 2.59 (2.44−2.76) | < 0.001 | 2.74 (2.57−2.92) | < 0.001 | 2.27 (2.13−2.42) | < 0.001 | |
| 51–60 | 275 219 | 5.27 (4.99−5.55) | < 0.001 | 4.19 (3.97−4.43) | < 0.001 | 6.52 (6.08−6.98) | < 0.001 | 5.87 (5.47−6.29) | < 0.001 | 4.19 (3.86−4.54) | < 0.001 | 2.74 (2.52−2.98) | < 0.001 | |
| 40–50 | 45 969 | 7.28 (6.66−7.95) | < 0.001 | 5.07 (4.62−5.57) | < 0.001 | 10.7 (9.65−11.87) | < 0.001 | 8.61 (7.74−9.58) | < 0.001 | 3.9 (3.31−4.6) | < 0.001 | 2.13 (1.79−2.52) | < 0.001 | |
| Sex | Female | 1 963 770 | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) |
| Male | 1 213 425 | 2.46 (2.37−2.55) | < 0.001 | 2.43 (2.34−2.52) | < 0.001 | 3.22 (3.06−3.38) | < 0.001 | 3.15 (2.99−3.32) | < 0.001 | 1.83 (1.74−1.93) | < 0.001 | 1.79 (1.7−1.89) | < 0.001 | |
| Race | White | 2 498 683 | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) |
| Asian | 73 937 | 0.82 (0.72−0.93) | 0.002 | 0.72 (0.63−0.82) | < 0.001 | 0.68 (0.57 −0.82) | < 0.001 | 0.59 (0.49−0.71) | < 0.001 | 0.94 (0.79−1.12) | 0.47 | 0.85 (0.71−1.02) | 0.07 | |
| Black or African American | 188 446 | 0.64 (0.58−0.7) | < 0.001 | 0.64 (0.58−0.7) | < 0.001 | 0.58 (0.51−0.66) | < 0.001 | 0.56 (0.49−0.64) | < 0.001 | 0.68 (0.59−0.77) | < 0.001 | 0.72 (0.63−0.82) | < 0.001 | |
| Other | 27 951 | 1.44 (1.23−1.68) | < 0.001 | 1.18 (1.01−1.39) | 0.03971 | 1.26 (1.01−1.57) | 0.038 | 1.01 (0.81−1.26) | 0.92473 | 1.65 (1.33−2.04) | < 0.001 | 1.41 (1.13−1.76) | 0.002 | |
| Unknown | 388 178 | 0.58 (0.55−0.62) | < 0.001 | 0.68 (0.63−0.74) | < 0.001 | 0.56 (0.51−0.61) | < 0.001 | 0.65 (0.59−0.72) | < 0.001 | 0.59 (0.54−0.66) | < 0.001 | 0.71 (0.63−0.79) | < 0.001 | |
| Ethnicity | Not Hispanic or Latino | 2 535 675 | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) |
| Hispanic or Latino | 190 370 | 0.84 (0.78−0.91) | < 0.001 | 0.96 (0.88−1.04) | 0.31735 | 0.84 (0.75−0.93) | 0.001 | 0.92 (0.82−1.03) | 0.16 | 0.82 (0.73−0.93) | 0.001 | 0.98 (0.87−1.12) | 0.80 | |
| Unknown | 451 150 | 0.59 (0.56−0.63) | < 0.001 | 0.7 (0.65−0.75) | < 0.001 | 0.55 (0.5−0.59) | < 0.001 | 0.63 (0.58−0.7) | < 0.001 | 0.64 (0.59−0.7) | < 0.001 | 0.78 (0.71−0.86) | < 0.001 | |
CI = confidence interval; NA = not applicable; OR = odds ratio; (Ref) = reference; RRD = rhegmatogenous retinal detachment; RT = retinal tear.
Bold OR (95% CI) values indicate statistical significance (P < 0.05).
Univariable odds ratios are based on coefficients from a logistic regression model of the single variable.
Multivariable ORs are based on coefficients from a multivariable logistic regression model containing all of the demographic factors (age at cataract surgery, sex, race, ethnicity, indicator for the presence of bilateral cataract surgeries), comorbidities (lattice degeneration, high myopia, posterior vitreous detachment), and factors associated with cataract surgery complexity (hypermature cataract, pseudoexfoliation, floppy iris syndrome, and complex cataract surgery Current Procedural Terminology code). Analyses adjusted for intereye correlation yielded similar results.
Ocular Comorbidities and Surgical Complexity Factors
Ocular comorbidities and surgical complexity factors associated with retinal events after cataract surgery are summarized in Table 5 and Figure 4. Multivariable adjusted ORs showed an increased risk of RRDs, in the order of magnitude, for eyes with LD (OR = 10.53; 95% CI, 9.82–11.28; P < 0.001), PVD (OR = 1.24; 95% CI, 1.15–1.34; P < 0.001), and high myopia (OR = 1.2; 95% CI, 1.14–1.27; P < 0.001). Among indicators of cataract surgery complexity evaluated (hypermature cataract, pseudoexfoliation, floppy iris syndrome, and complex cataract surgery CPT code 66982), the presence of a hypermature cataract (1.61; 95% CI, 1.06–2.45; P = 0.03) and use of complex cataract surgery CPT code (1.22; 95% CI, 1.13–1.33; P < 0.001) were associated with an increased risk of RRD.
Table 5.
Multivariable ORs of RRDs or RTs after Cataract Surgery by Ocular Comorbidity and Cataract Surgery Complexity
| Comorbidities and Cataract Surgery Complexity Indicators | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Condition | Present Before Cataract Procedure | Cataract Procedures | Retinal Events (RRD or RT) |
RRD |
RT |
|||||||||
| Uni OR (95% CI)∗ | P Value | Multi-OR (95% CI)† | P Value | Uni OR (95% CI)∗ | P Value | Multi-OR (95% CI)† | P Value | Uni OR (95% CI)∗ | P Value | Multi-OR (95% CI)† | P Value | |||
| Lattice degeneration | No | 3 139 456 | 31.22 (29.91–32.59) | < 0.001 | 23.14 (22.13–24.2) | < 0.001 | 15.92 (14.89–17.02) | < 0.001 | 10.53 (9.82–11.28) | < 0.001 | 54.48 (51.55–57.59) | < 0.001 | 43.86 (41.39–46.49) | < 0.001 |
| Yes | 37 739 | |||||||||||||
| High myopia | No | 2 519 634 | 1.49 (1.44–1.56) | < 0.001 | 1.12 (1.08–1.17) | < 0.001 | 1.51 (1.43–1.59) | < 0.001 | 1.2 (1.14–1.27) | < 0.001 | 1.51 (1.43–1.6) | < 0.001 | 1.06 (1–1.12) | 0.07 |
| Yes | 657 561 | |||||||||||||
| Posterior vitreous detachment | No | 2 845 917 | 1.27 (1.2–1.34) | < 0.001 | 1.13 (1.07–1.2) | < 0.001 | 1.2 (1.12–1.29) | < 0.001 | 1.24 (1.15–1.34) | < 0.001 | 1.35 (1.25–1.46) | < 0.001 | 1.01 (0.93–1.09) | 0.81 |
| Yes | 331 278 | |||||||||||||
| Hypermature cataract | No | 3 172 635 | 1.98 (1.4–2.79) | < 0.001 | 1.61 (1.13–2.28) | 0.01 | 2.41 (1.6–3.63) | < 0.001 | 1.61 (1.06–2.45) | 0.03 | 1.4 (0.77–2.53) | 0.27 | 1.46 (0.8–2.67) | 0.22 |
| Yes | 4560 | |||||||||||||
| Pseudoexfoliation | No | 3 067 803 | 1 (0.9–1.1) | 0.96 | 1.03 (0.93–1.14) | 0.57 | 1 (0.88–-1.14) | 0.96 | 0.98 (0.86–1.12) | 0.77 | 0.99 (0.86–1.15) | 0.94 | 1.11 (0.96–1.29) | 0.17 |
| Yes | 109 392 | |||||||||||||
| Floppy iris syndrome | No | 3 155 198 | 1.01 (0.82–1.26) | 0.90 | 0.82 (0.66–1.03) | 0.08 | 1.1 (0.84–1.45) | 0.49 | 0.77 (0.58–1.02) | 0.06 | 0.84 (0.59–1.19) | 0.33 | 0.88 (0.62–1.26) | 0.49 |
| Yes | 21 997 | |||||||||||||
| Use of complex cataract surgery CPT Code (66982) | No | 2 975 930 | 1.25 (1.17–1.34) | < 0.001 | 1.27 (1.19–1.37) | < 0.001 | 1.59 (1.47–1.72) | < 0.001 | 1.52 (1.4–1.66) | < 0.001 | 0.82 (0.73–0.92) | 0.001 | 0.89 (0.79–1.01) | 0.07 |
| Yes | 201 265 | |||||||||||||
CI = confidence interval; CPT = Current Procedural Terminology; IR = incidence rate; OR = odds ratio; (Ref) = reference; RRD = rhegmatogenous retinal detachment; RT = retinal tear.
Bold OR (95% CI) values indicate statistical significance (P < 0.05).
Univariable ORs are based on coefficients from a logistic regression model of the single variable.
Multivariable ORs are based on coefficients from a multivariable logistic regression model containing all of the demographic factors (age at cataract surgery, sex, race, ethnicity, indicator for the presence of bilateral cataract surgeries), comorbidities (lattice degeneration, high myopia, posterior vitreous detachment), and factors associated with cataract surgery complexity (hypermature cataract, pseudoexfoliation, floppy iris syndrome, and complex cataract surgery CPT code). Analyses adjusted for intereye correlation yielded similar results.
RT without RRD
Demographic features
Multivariable adjusted ORs showed an increased risk of RT 1 year after cataract surgery for cataract procedures at 40 to 50 years of age (OR = 2.13; 95% CI, 1.79–2.52; P < 0.001), 51 to 60 years of age (OR = 2.74; 95% CI, 2.52–2.98; P < 0.001), and 61 to 70 years of age (OR = 2.27; 95% CI, 2.13–2.42; P < 0.001) when compared with procedures at > 70 years. Multivariable adjusted OR results also showed an increased risk of RT for men compared with women (OR = 1.79; 95% CI, 1.7–1.89; P < 0.001), and decreased risk of RT for Black patients when compared with White patients (OR = 0.72; 95% CI, 0.63–0.82; P < 0.001), whereas Hispanic or Latino ethnicity was not statistically significantly associated with RT without RRD occurrence within 1 year after surgery.
Ocular Comorbidities and Surgical Complexity Factors
For comorbidities and surgical complexity indicators, only LD conferred an increased risk of RT (43.86; 95% CI, 41.39–46.49; P < 0.001).
Additional analysis
Univariable and multivariable Cox regression analyses were also performed to account for time to event and adjust for varying follow-up period among patients and are noted in Table S6 (available at www.ophthalmologyscience.org). These analyses were performed for the specific demographic features, comorbidities, and indicators of cataract surgery complexity described earlier. Multivariable adjusted hazard ratios from these models were consistent in magnitude and significance with the logistic regression ORs for all factors with the exceptions of the following: (1) hypermature cataract showing no significance change in risk of RRD (1.43; 95% CI, 0.95–2.16; P = 0.09), (2) high myopia showing increased risk of RT (1.11; 95% CI, 1.04–1.18; P = 0.001), and (3) use of complex cataract surgery complexity CPT code 66982 being associated with decreased risk of RT (0.87; 95% CI, 0.77–0.99; P = 0.03).
Discussion
Prior studies (before modern day small incision cataract surgery) have reported the 1-year incidence of RRD after cataract surgery to range from 0.6% to 1.7%,13, 14, 15, 16, 17 representing a > 30-fold increased risk of RRD when compared with rates in the general population of 0.007% to 0.018%.17, 18, 19, 20, 21 However, more recent studies have demonstrated that this IR may be declining. A retrospective study from Western Australia evaluating 129 982 cataract surgery patients found the 5-year RRD rate after cataract surgery to have declined from 1.05% in 1980 to 1984 to 0.45% in 1995 to 2001.22 In addition, a literature review looking at studies from 1996 to 2014 found that cataract operations after year 2000 have an inferred 1-year incidence of RRD after cataract surgery (cumulative RRD IR/study length) between 0.04% and 0.29%.8 Lastly, a 2015 population study from France analyzing 2 680 167 cataract procedure eyes between 2009 and 2012 found the 4-year cumulative RRD after cataract surgery to be 0.99% (0.25% inferred 1-year incidence).23
In this analysis of > 3 million United States cataract operations from 2014 to 2017 in the IRIS Registry, the incidence of RRD within 1-year of cataract surgery was 0.21%, or approximately 1 in 500 cataract surgeries. This IR is in line with the declining IRs noted in recent studies. Moreover, the incidence of RT after cataract surgery was found to be 0.17%. In regard to time course, 59.9% of RRD and 48.5% of RT occurred within the first 6 months (180 days) after cataract surgery. Multivariable logistic regression ORs revealed an increased risk of RRD among males and younger ages compared with patients aged > 70 years, and procedure eyes with LD, high myopia, PVD, hypermature cataract, or use of complex cataract surgery CPT code 66982. Among the evaluated factors, LD conferred the strongest risk of RRD and RT. The proportion of patients with LD diagnosed before cataract surgery who developed retinal detachment within 1 year after cataract surgery was 1.44%. The interpretation must recognize that there may be an observation bias increasing the identification of LD when a patient develops retinal detachment and decreasing the identification of lattice before cataract surgery with incomplete peripheral retinal examination because of cataract or other limitations precluding complete retinal examination (Table S7, available at www.aaojournal.org).
Demographic factors for RRD after cataract surgery have been investigated in previous studies. Two major demographic risk factors for RRD after cataract surgery that have been identified are younger age and male gender.23, 24, 25 The cause of higher RRD risk in younger and male patients remains speculative, but may be associated with the higher likelihood of eye trauma. In addition, differences in the incidence of RRD in the general population by race have been studied, with Asian and Black patients having lower incidences of RRD than White patients.26,27 This analysis of the IRIS Registry was in line with these prior findings, with higher odds of RRD noted for younger ages, male gender, and among White patients than older ages, female gender, and Black or Asian patients.
Ocular comorbidities have also been evaluated as risk factors for RRD after cataract surgery. A 1996 population-based case-control study found that a history of RRD (OR = 2.7; 95% CI, 1.2–6.1; P < 0.05), larger axial length (OR = 1.21/mm; 95% CI, 1.03–1.43; P < 0.05), and LD (OR = 6.6; 95% CI, 1.6–27.1; P < 0.05) were associated with an increased risk of RRD after cataract surgery.28 High myopia, as defined by axial length > 26 mm, had also been established as a risk factor for RRD after cataract surgery.24,26 Multivariable logistic regression results from the present study show similar trends of increased RRD after cataract surgery in patients with high myopia and LD. In our study, LD appears to have the highest OR for RRD (OR = 10.53; 95% CI, 9.82–11.28; P < 0.001) and RT (OR = 43.86; 95% CI, 41.39–46.49; P < 0.001)) after cataract surgery. Further studies are warranted to explain the high magnitude of risk this feature has on acute retinal events after cataract surgery, and perhaps more importantly clinically, if prophylactic treatment (e.g., laser retinopexy) may alter this risk. This study is not able to assess the potential impact of laser retinopexy prophylaxis. Another consideration is that cataract surgery may improve the detection of some preexistent LD-associated retinal holes or tears and that the surgery itself may not lead to the development of these events.
The role of PVD has also been an area of interest regarding retinal events after cataract surgery.29 However, the documentation of PVD in prior reports and in this report may be limited by the variability of reporting and accuracy of detection. Further, the extent of vitreous separation from the retina (posterior pole toward the vitreous base) may be more relevant to the development of RTs and retinal detachment than observation of a posterior vitreous ring (Weiss ring) or posterior vitreous floaters that are construed as PVD. Occurrence of PVD after cataract surgery may be the initial precursor to a retinal event, such as a detachment or tear.17,30,31 However, eyes with a preexisting PVD may be at a lower risk of RRD than those without a PVD.31,32 Therefore, the presence of a PVD before cataract surgery has been postulated to reduce the risk of RRD after cataract surgery.8,23 In the present study, the presence of PVD before cataract surgery was associated with an increased risk of RRD (OR = 1.24; 95% CI, 1.15–1.34; P < 0.001) after cataract surgery. Further study is required to understand this observation, which may be explained in part by the older age of patients included in this study, with 90% aged > 60 and 52% aged > 70 years. These findings may also be complicated by the variable accuracy of PVD diagnoses in the absence of standardized protocols for assessment and should be interpreted with caution. In addition, electronic health records documentation of PVD may have been less robust if the presenting symptoms for the patient visit were related to the primary diagnosis of a cataract. Although preexisting PVD may be relevant in the development of RRD or RT in some patients postcataract surgery, other comorbidities, such as LD and high myopia were, in this data set, more consequential. Although a registry data set has methodologic limitations in identifying those who “develop PVD” after cataract surgery but in whom it was not present before cataract surgery, in this study, identification of PVD within 1 year after cataract surgery in those without PVD before surgery was associated with an increased risk of a RT (0.09% vs. 1.02%) or retinal detachment (0.15% vs. 0.84%) compared with those in whom PVD was not identified in that time frame (Table S8, www.ophthalmologyscience.org).
Finally, intraoperative complications are thought to be a major cause of RRD after cataract surgery. Posterior capsular rupture has been estimated to increase the risk of RRD up to 12-fold because of presumed vitreous traction.8,6,17,25,33 Given the lack of a CPT code or ICD code which correlates to PCR, the association of PCR with RRD or RT could not be assessed within the IRIS Registry. Of the conditions associated with procedure complexity evaluated, the presence of hypermature cataract and the use of the complex cataract surgery CPT code were associated with an increased risk of RRD. Interestingly, other features that may be associated with cataract surgery complexity, such as pseudoexfoliation and floppy iris syndrome, did not seem to increase the risk of RRD after surgery. These results may be attributed to improved knowledge and tools for addressing surgical complexities.
Several limitations exist in this study of the IRIS Registry data. First, data may be biased by variable reporting accuracy in diagnosing ocular comorbidities, and also, variability in the completeness and accuracy of coding entry to capture these diagnoses. The data available in the IRIS Registry could only be evaluated by specific CPT and ICD codes, and it is possible that follow-up visits could occur at a non-IRIS registry provider. Therefore, certain measures, such as axial length, and intraoperative events without a specific CPT code, such as PCR, could not be directly assessed. Moreover, our strict criteria for retaining only procedures and conditions with defined laterality may lead to underreporting the IRs of retinal events. The strengths of this study include the large population size, the large data sets of specific demographic and ocular subsets of interests (e.g., younger patients with cataract surgery, floppy iris syndrome, or complex cataract surgery procedures), the ability to define procedure specifics including laterality and sequence, and the relevancy of these findings to clinical decision making. The use of CPT codes with defined laterality in the IRIS Registry and the robust methodology for the data processing increase the likelihood that retinal events captured in our analysis data set accurately correspond to a cataract eye procedure with accurate timing of these events relative to cataract procedures. Because the IRIS Registry is comprised from providers residing in the United States and its territories (for example, Puerto Rico), this study provides a standard of findings more relevant to patients in United States than previous international studies.
In conclusion, analysis of the IRIS Registry reveals an overall risk of RRD and RT within a 1-year span, postcataract surgery, to be 0.21% and 0.17%, or approximately 1 in 500 cataract surgeries. Careful monitoring in patients with LD may be warranted, particularly in younger men. These rates and risk factors may be useful in guiding the consent process for cataract surgery by informing patients about the risk of retinal complications. Additional analyses, including visual acuity outcomes, efficacy of prophylactic laser surgery, and features of retinal detachment, such as macular status, will be of interest and are worthy of additional study.
Manuscript no. XOPS-D-22-00211R2.
Footnotes
Supplemental material available atwww.ophthalmologyscience.org.
Disclosures:
All authors have completed and submitted the ICMJE disclosures form.
The authors made the following disclosures: D.M.W.: Volunteer – Wills Eye Alumni Society.
J.A.H.: Leadership – AAO Foundation Board.
L.H.: Consultant – TRUST (Treatment of Central Vein Occlusion using Stem Cell Study), Spectacle Prescribing in Early Childhood (SPEC), Village-Integrated Eye Worker Trial II (VIEW II), Azithromycin Reduction to Reach Elimination of Trachoma (ARRET), Kebele Elimination of Trachoma for Ocular Health (KETFO) Study, Sanitation, Water, And Instruction in Face-Washing for Trachoma (SWIFT II); Leadership – AUPO- Research Director Council, ARVO- Women’s Leadership Development Program.
M.A.K.: Grant – Regeneron; Consultant – Genentech, Apellis.
A.C.H.: Consultant – Alcon. The other authors have no proprietary or commercial interest in any materials discussed in this article.
HUMAN SUBJECTS: Human subjects were included in this study. This study adhered to the tenets of the declaration of Helsinki. Given the use of deidentified patient data from an established database, the study was exempt from Wills Eye Hospital Institutional Review Board (IRB) review.
No animal subjects were used in this study.
Author Contributions:
Conception and design: Morano, Khan, Zhang, Halfpenny, Wisner, Sharpe, Li, Tomaiuolo, Haller, Hyman, Ho.
Data collection: Morano.
Analysis and interpretation: Morano, Khan, Zhang, Halfpenny, Wisner, Sharpe, Li, Tomaiuolo, Haller, Hyman, Ho.
Obtained funding: N/A
Overall responsibility: Morano, Halfpenny, Hyman, Ho.
Supplementary Data
References
- 1.Olson R.J., Braga-Mele R., Chen S.H., et al. Cataract in the adult eye preferred practice pattern. Ophthalmology. 2017;124:P1–P119. doi: 10.1016/j.ophtha.2016.09.027. [DOI] [PubMed] [Google Scholar]
- 2.Gollogly H.E., Hodge D.O., St Sauver J.L., Erie J.C. Increasing incidence of cataract surgery: population-based study. J Cataract Refract Surg. 2013;39:1383–1389. doi: 10.1016/j.jcrs.2013.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schein O.D., Cassard S.D., Tielsch J.M., Gower E.W. Cataract surgery among Medicare beneficiaries. Ophthalmic Epidemiol. 2012;19:257–264. doi: 10.3109/09286586.2012.698692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erie J.C., Baratz K.H., Hodge D.O., et al. Incidence of cataract surgery from 1980 through 2004: 25-year population-based study. J Cataract Refract Surg. 2007;33:1273–1277. doi: 10.1016/j.jcrs.2007.03.053. [DOI] [PubMed] [Google Scholar]
- 5.Erie J.C. Rising cataract surgery rates: demand and supply. Ophthalmology. 2014;121:2–4. doi: 10.1016/j.ophtha.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Petousis V., Sallam A.A., Haynes R.J., et al. Risk factors for retinal detachment following cataract surgery: the impact of posterior capsular rupture. Br J Ophthalmol. 2016;100:1461–1465. doi: 10.1136/bjophthalmol-2015-307729. [DOI] [PubMed] [Google Scholar]
- 7.Flaxel C.J., Adelman R.A., Bailey S.T., et al. Posterior vitreous detachment, retinal breaks, and lattice degeneration preferred practice pattern [published correction appears in Ophthalmology. 2020 Sep;127(9):1279] Ophthalmology. 2020;127:P146–P181. doi: 10.1016/j.ophtha.2019.09.027. [DOI] [PubMed] [Google Scholar]
- 8.Qureshi M.H., Steel D.H.W. Retinal detachment following cataract phacoemulsification-a review of the literature [published correction appears in Eye (Lond). 2019 Oct 28] Eye (Lond) 2020;34:616–631. doi: 10.1038/s41433-019-0575-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee C.S., Blazes M., Lorch A., et al. American Academy of Ophthalmology Intelligent Research in Sight (IRIS) Registry and the IRIS Registry Analytic Center Consortium. Ophthalmol Sci. 2022;2 doi: 10.1016/j.xops.2022.100112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.IRIS Registry Data Analysis: Overview. American Academy of Ophthalmology. https://www.aao.org/iris-registry/data-analysis/requirements Published December 16, 2021. Accessed April 26, 2022.
- 11.Rich W.L., III, Chiang M.F., Lum F., et al. Performance rates measured in the American Academy of Ophthalmology IRIS Registry (Intelligent Research in Sight) Ophthalmology. 2018;125:782–784. doi: 10.1016/j.ophtha.2017.11.033. [DOI] [PubMed] [Google Scholar]
- 12.Chiang M.F., Sommer A., Rich W.L., et al. The 2016 American Academy of Ophthalmology IRIS® Registry (Intelligent Research in Sight) database: characteristics and methods. Ophthalmology. 2018;125:1143–1148. doi: 10.1016/j.ophtha.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Kraff M.C., Sanders D.R. Incidence of retinal detachment following posterior chamber intraocular lens surgery. J Cataract Refract Surg. 1990;16:477–480. doi: 10.1016/s0886-3350(13)80802-4. [DOI] [PubMed] [Google Scholar]
- 14.Lois N., Wong D. Pseudophakic retinal detachment. Surv Ophthalmol. 2003;48:467–487. doi: 10.1016/s0039-6257(03)00083-3. [DOI] [PubMed] [Google Scholar]
- 15.Erie J.C., Raecker M.E., Baratz K.H., et al. Risk of retinal detachment after cataract extraction, 1980-2004: a population-based study. Trans Am Ophthalmol Soc. 2006;104:167–175. [PMC free article] [PubMed] [Google Scholar]
- 16.Tuft S.J., Minassian D., Sullivan P. Risk factors for retinal detachment after cataract surgery: a case-control study. Ophthalmology. 2006;113:650–656. doi: 10.1016/j.ophtha.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 17.Haug S.J., Bhisitkul R.B. Risk factors for retinal detachment following cataract surgery. Curr Opin Ophthalmol. 2012;23:7–11. doi: 10.1097/ICU.0b013e32834cd653. [DOI] [PubMed] [Google Scholar]
- 18.Haimann M.H., Burton T.C., Brown C.K. Epidemiology of retinal detachment. Arch Ophthalmol. 1982;100:289–292. doi: 10.1001/archopht.1982.01030030291012. [DOI] [PubMed] [Google Scholar]
- 19.Laatikainen L., Tolppanen E.M., Harju H. Epidemiology of rhegmatogenous retinal detachment in a Finnish population. Acta Ophthalmol (Copenh) 1985;63:59–64. doi: 10.1111/j.1755-3768.1985.tb05216.x. [DOI] [PubMed] [Google Scholar]
- 20.Algvere P.V., Jahnberg P., Textorius O. The Swedish Retinal Detachment Register. I. A database for epidemiological and clinical studies. Graefes Arch Clin Exp Ophthalmol. 1999;237:137–144. doi: 10.1007/s004170050208. [DOI] [PubMed] [Google Scholar]
- 21.Rowe J.A., Erie J.C., Baratz K.H., et al. Retinal detachment in Olmsted County, Minnesota, 1976 through 1995. Ophthalmology. 1999;106:154–159. doi: 10.1016/S0161-6420(99)90018-0. [DOI] [PubMed] [Google Scholar]
- 22.Clark A., Morlet N., Ng J.Q., et al. Whole population trends in complications of cataract surgery over 22 years in Western Australia. Ophthalmology. 2011;118:1055–1061. doi: 10.1016/j.ophtha.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 23.Daien V., Le Pape A., Heve D., et al. Incidence, risk factors, and impact of age on retinal detachment after cataract surgery in France: a national population study. Ophthalmology. 2015;122:2179–2185. doi: 10.1016/j.ophtha.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 24.Sheu S.J., Ger L.P., Ho W.L. Late increased risk of retinal detachment after cataract extraction. Am J Ophthalmol. 2010;149:113–119. doi: 10.1016/j.ajo.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 25.Tuft S.J., Gore D.M., Bunce C., et al. Outcomes of pseudophakic retinal detachment. Acta Ophthalmol. 2012;90:639–644. doi: 10.1111/j.1755-3768.2011.02124.x. [DOI] [PubMed] [Google Scholar]
- 26.Mowatt L., Shun-Shin G., Price N. Ethnic differences in the demand incidence of retinal detachments in two districts in the West Midlands. Eye (Lond) 2003;17:63–70. doi: 10.1038/sj.eye.6700245. [DOI] [PubMed] [Google Scholar]
- 27.Weiss H., Tasman W.S. Rhegmatogenous retinal detachments in blacks. Ann Ophthalmol. 1978;10:799–806. [PubMed] [Google Scholar]
- 28.Tielsch J.M., Legro M.W., Cassard S.D., et al. Risk factors for retinal detachment after cataract surgery. A population-based case-control study. Ophthalmology. 1996;103:1537–1545. doi: 10.1016/s0161-6420(96)30465-x. [DOI] [PubMed] [Google Scholar]
- 29.Ripandelli G., Coppé A.M., Parisi V., et al. Posterior vitreous detachment and retinal detachment after cataract surgery. Ophthalmology. 2007;114:692–697. doi: 10.1016/j.ophtha.2006.08.045. [DOI] [PubMed] [Google Scholar]
- 30.Coppé A.M., Lapucci G. Posterior vitreous detachment and retinal detachment following cataract extraction. Curr Opin Ophthalmol. 2008;19:239–242. doi: 10.1097/ICU.0b013e3282fc9c4a. [DOI] [PubMed] [Google Scholar]
- 31.Steel D. Retinal detachment. BMJ Clin Evid. 2014;2014 [PMC free article] [PubMed] [Google Scholar]
- 32.Richardson P.S., Benson M.T., Kirkby G.R. The posterior vitreous detachment clinic: do new retinal breaks develop in the six weeks following an isolated symptomatic posterior vitreous detachment? Eye (Lond) 1999;13:237–240. doi: 10.1038/eye.1999.58. [DOI] [PubMed] [Google Scholar]
- 33.Kim J., Ryu S.Y., Hong J.H., Chung E.J. Incidence and risk factors for retinal detachment after cataract surgery in Korea: a nationwide population-based study from 2011 to 2015. Graefes Arch Clin Exp Ophthalmol. 2019;257:2193–2202. doi: 10.1007/s00417-019-04423-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.