Abstract
Objective
A relationship between the 2017 American College of Cardiology and American Heart Association blood pressure thresholds and adverse pregnancy outcomes has been reported, but few studies have explored the diagnostic test properties of these cutoffs.
Data Sources
We systematically searched electronic databases (from 2017 to 2021) for reports of blood pressure measurements in pregnancy, classified according to 2017 American College of Cardiology and American Heart Association criteria, and their relationship with pregnancy outcomes.
Study Eligibility Criteria
Studies recording blood pressure at <20 weeks gestation were included.
Methods
Meta-analyses were used to investigate the strength of the association between blood pressure cutoffs and adverse outcomes, and the diagnostic test properties were calculated.
Results
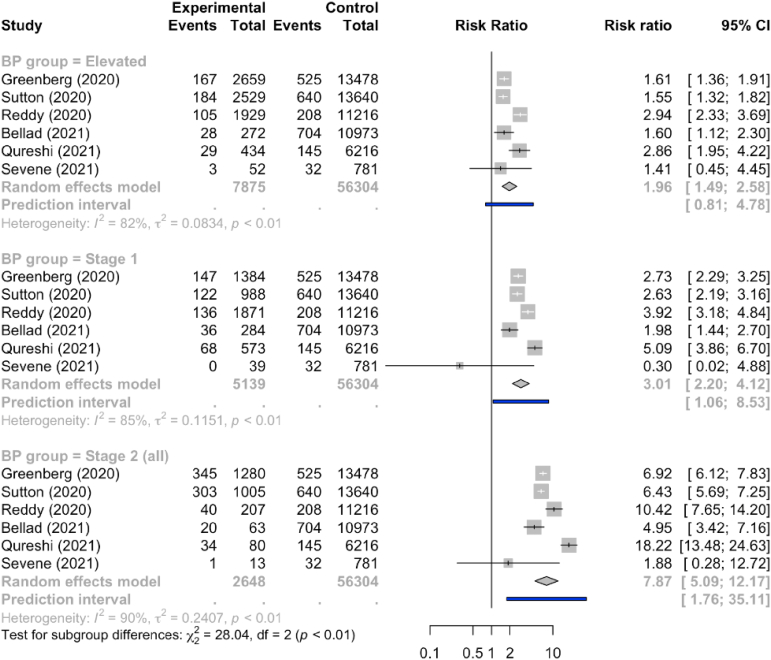
Of 23 studies included, there was a stepwise relationship between the American College of Cardiology and American Heart Association blood pressure category (when compared with normal blood pressure of <120/80 mmHg) and the strength of the association with preeclampsia. The category of elevated blood pressure had a risk ratio of 2.0 (95% prediction interval, 0.8–4.8), the stage 1 hypertension category had a risk ratio of 3.0 (95% prediction interval, 1.1–8.5), and the stage 2 hypertension category had a risk ratio of 7.9 (95% prediction interval, 1.8–35.1). Between-study variability was related to the magnitude of the association with stronger relationships in larger studies at low risk of bias and with unselected populations with multiple routine blood pressure measurements. None of the systolic blood pressure measurements of <120 mmHg, <130/80 mmHg, or <140/90 mmHg were useful to rule out the development of preeclampsia (all negative likelihood ratios >0.2). Only a blood pressure measurement of ≥140/90 mmHg was a good predictor for the development of preeclampsia (positive likelihood ratio, 5.95). The findings were similar for other outcomes.
Conclusion
Although a blood pressure of 120 to 140 over 80 to 90 mmHg at <20 weeks gestation is associated with a heightened risk for preeclampsia and adverse pregnancy outcomes and may assist in risk prediction in multivariable modelling, lowering the diagnostic threshold for chronic hypertension would not assist clinicians in identifying women at heightened risk.
Key words: cardiovascular systematic review, chronic hypertension in pregnancy, preeclampsia, pregnancy complications, pregnancy-induced hypertension
Introduction
Higher blood pressure (BP) measurements are associated with more adverse outcomes outside of and during pregnancy.1, 2, 3, 4 To stratify risk management and justify additional investigations and interventions, a systolic BP (sBP) ≥140 mmHg and diastolic BP (dBP) ≥90 mmHg have long been categorized as hypertension. In pregnancy, hypertension has been regarded as chronic if hypertension is recorded at <20 weeks gestation and as gestational if hypertension first appears ≥20 weeks gestation. When gestational hypertension occurs with proteinuria, another maternal end-organ complication, or uteroplacental dysfunction, the criteria are met for classification as preeclampsia, the hypertensive disorder of pregnancy associated with the highest maternal and perinatal risks.5
AJOG at a Glance.
Why was this study conducted?
A relationship between the 2017 American College of Cardiology and the American Heart Association blood pressure (BP) thresholds and adverse pregnancy outcomes has been reported, but few studies have explored the diagnostic test properties of these cutoffs.
Key findings
Although higher BP values <20 weeks gestation is associated with adverse outcomes, lowering the threshold for chronic hypertension would not improve the identification of women and babies at risk. No abnormal BP threshold <20 weeks gestation, including the current 140/90 mmHg threshold, provides reassurance about the development of preeclampsia or adverse pregnancy outcomes.
What does this add to what is known?
Our findings do not support lowering the BP level component of the definition for chronic hypertension in pregnancy to below the current 140/90 mmHg threshold.
In 2017, the American College of Cardiology (ACC) and the American Heart Association (AHA) recommended lowering the BP thresholds for diagnosis of hypertension outside of pregnancy based on the association of these lower BP values with elevated cardiovascular risk. BP was considered to be normal if <120/80 mmHg, and the traditional definition of hypertension (sBP ≥140 mmHg and diastolic BP ≥90 mmHg) has been termed stage 2 hypertension. Two new BP categories were created, namely elevated BP (sBP, 120–129 mmHg and dBP <80 mmHg) and stage 1 hypertension (sBP, 130–139 mmHg and dBP, 80–89 mmHg).6
Since 2017, the diagnostic criteria for hypertension from a sBP ≥140 mmHg and a diastolic BP ≥90 mmHg have not been changed in any of the pregnancy hypertension guidelines.7 In 2019, the American College of Obstetricians and Gynecologists (ACOG) called for investigation into the consequences of adopting the 2017 ACC-AHA BP criteria. Many studies have been published, evaluating the association between preeclampsia (and other adverse pregnancy outcomes) and elevated BP, stage 1 hypertension, or a combination of both, particularly when BP was measured <20 weeks gestation.8, 9, 10, 11, 12, 13, 14
Objective
We aimed to evaluate whether the definition of chronic hypertension in pregnancy should be revised according to the ACC-AHA criteria. Here, we present a systematic review of published studies on the association of BP values measured before 20 weeks gestation, classified according to ACC-AHA BP criteria, with preeclampsia and other adverse pregnancy outcomes.
Materials and Methods
This systematic review was prospectively registered with the International Prospective Register of Systematic Reviews under identifier CRD42021229131.
Eligibility criteria, information sources, search strategy
We searched Ovid MEDLINE, PubMed, Embase, Cumulative Index to Nursing and Allied Health Literature, Cochrane Central Register of Controlled Trials, Latin American and Caribbean Health Sciences Literature, and International Clinical Trials Registry Platform from January 1, 2017 to January 15, 2021, for all original research reports in peer-reviewed journals addressing BP in pregnancy according to the 2017 ACC/AHA guideline criteria.6 The search was updated monthly throughout the data collection and synthesis phase of the review up to September 9, 2021. The search terms used were (“American College of Cardiology/American Heart Association” OR “ACC/AHA” OR “Stage 1 hypertension” OR “Stage 2 hypertension” OR “prehypertension”) AND (“{Pregnancy [mh] OR Pregnan∗ OR Gestation∗ OR pregnant women[mh] OR Pregnancy Complications[mh] OR “Postpartum Period”[Mesh] OR Puerperium OR postpartum OR “Peripartum Period”[Mesh] OR Peripartum∗ OR Perinatal Care[mh] OR perinatal} AND {hypertension, hypertensive disorders of pregnancy, pregnancy-induced hypertension, preeclampsia, pregnancy toxemias, OR gestational hypertension}). The final list was confirmed using Google Scholar, using “pregnancy” AND (“prehypertension” OR “stage 1 hypertension” OR “ACC/AHA” OR “American College of Cardiology/American Heart Association”). There were no language restrictions. In addition, reference lists of included papers were searched for additional eligible publications.
Study selection
Included were reports of BP measurements in pregnancy before 20 weeks gestation as defined by study authors, classified according to the 2017 ACC/AHA criteria, and their relationship with maternal or fetal and newborn outcomes in pregnancy.
BP was categorized as normal (sBP <120 mmHg and dBP <80 mmHg), elevated BP (sBP 120–129 mmHg and dBP <80 mmHg), stage 1 hypertension (sBP 130–139 mmHg and/or dBP 80–89 mmHg), or stage 2 hypertension (sBP ≥140 mmHg and/or dBP ≥90 mmHg), which was also subdivided into nonsevere (sBP 140–159 mmHg and/or dBP 90–109 mmHg) and severe (sBP ≥160 mmHg and/or dBP ≥110 mmHg).2 A diagnosis of stage 2 hypertension was confirmed by a prescription of antihypertensive therapy (because there is no precedent for routine treatment of BP <140/90 mmHg).
Excluded were case reports, duplicate publications (including the more complete or recent data set), and studies that presented BP as a continuous variable without categorization.
Outcomes
The main outcomes were preeclampsia (as defined by individual authors), serious maternal complications (composite as defined by individual authors, including cerebrovascular accident, cortical blindness, retinal detachment, pulmonary edema, acute kidney injury, liver capsule hematoma or rupture), preterm birth, fetal and newborn death, small-for-gestational age (SGA) infants, and admission to a neonatal intensive care unit (NICU).
The secondary maternal outcomes were miscarriage; maternal death; eclampsia; hemolysis, elevated liver enzymes, and low platelet (HELLP) syndrome; admission to intensive care; intubation or ventilation (other than for childbirth); placental abruption; cesarean delivery; and postpartum hemorrhage.
The secondary neonatal outcomes were respiratory support and neonatal seizures.
All outcome definitions specified by the study authors were accepted and catalogued. We did not evaluate severe preeclampsia separately from preeclampsia because of the international move away from use of an outcome that is variably defined15; instead, we used the outcome only when information on all combined preeclampsia cases was unavailable.
Severe maternal morbidities (eg, acute kidney injury) were not included individually; although they are core maternal outcomes in pregnancy hypertension, these are reported infrequently and also occur infrequently.
Data extraction
Search results were reviewed by 3 reviewers (L.S., M.B., and N.S.) and the full text of all relevant studies were retrieved and reviewed for inclusion. Any disagreement about the eligibility of studies was resolved through consensus with the remainder of the review team. Authors were contacted for clarification when required.
Data were abstracted by 2 reviewers for each included study using a review-specific form to collect characteristics of the study, patients enrolled (including type of hypertension), BP measurement details (and treatment, if applicable), and outcome definitions. Data abstraction was undertaken by all the authors with each study having data extracted by 2 authors. Any disagreement was addressed by consulting the remainder of the group to reach a consensus.
Study authors were contacted for information that was unclear or to enquire about accessing data for individual outcomes if only composite outcomes were reported.
Assessment of risk of bias
Methodologic quality was assessed by 2 reviewers, independently, using the Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) tool for primary diagnostic accuracy studies.16 Any disagreement was resolved by a third reviewer. Studies were classified as being at high risk of bias overall if determined to be at high risk in any of the domains, at low risk of bias if judged to be at low risk in all the domains, and as unclear risk of bias when the risk in any category was uncertain.17
Data synthesis and meta-analysis
Our primary aim was to assess the usefulness of the ACC-AHA BP criteria for abnormal BP <20 weeks gestation by estimating the strength of the association with adverse outcomes and the associated diagnostic test properties. To undertake meaningful comparisons, we pooled outcome data when evaluated in more than 3 studies.
To evaluate the association between each BP category and adverse outcomes, we conducted a meta-analysis using the Mantel-Haenszel method for combing risk ratios.18 Results were summarized using pooled risk ratios (RRs) and 95% prediction intervals. Heterogeneity was summarized using the I2 statistic and classified as may not be important (I2 <40%), may represent moderate heterogeneity (30%–60%), may represent substantial heterogeneity (50%–90%), and considerable (≥75%).19
To evaluate the diagnostic test properties of the lower limit of each BP category as a cutoff (in the way that we currently treat a BP of 140/90 mmHg), we estimated each study’s sensitivity, specificity, and positive (+LR) and negative (−LR) likelihood ratios. Pooled estimates of the likelihood ratios were calculated from the estimated sensitivity and specificity from the bivariate random effects models. Confidence intervals were computed using 100,000 Markov Chain Monte Carlo resamples from the joint bivariate normal distribution of the sensitivity and specificity.20, 21, 22 All effect measures were estimated with 95% confidence intervals (CIs). Diagnostic tests properties were interpreted as excellent when +LR ≥10.0 (to rule in the outcome) or −LR <0.10 (to rule in the outcome), good when +LR ≥5.0 or −LR <0.20, and fair hen +LR was between 2.0 and 4.9 or −LR was between 0.20 and 0.50.23
Publication bias for each main outcome was assessed when there were at least 10 relevant studies that reported on the outcome. Funnel plots were used to assess asymmetry visually, and if asymmetry were suggested, we performed exploratory analyses to investigate it using Egger’s test and, if necessary, the trim and fill method.24
Moderation was evaluated descriptively in subgroup analyses that accounted for potential differences in the study characteristics (such as quality or origin), baseline characteristics of the participants (such as body mass index [BMI] or comorbidities), potential co-interventions (such as aspirin), or outcome definitions.
All analyses were conducted using the meta25 and mada26 packages in R statistical software (R Core Team, Vienna, Austria).25,27
Results
Study selection and characteristics
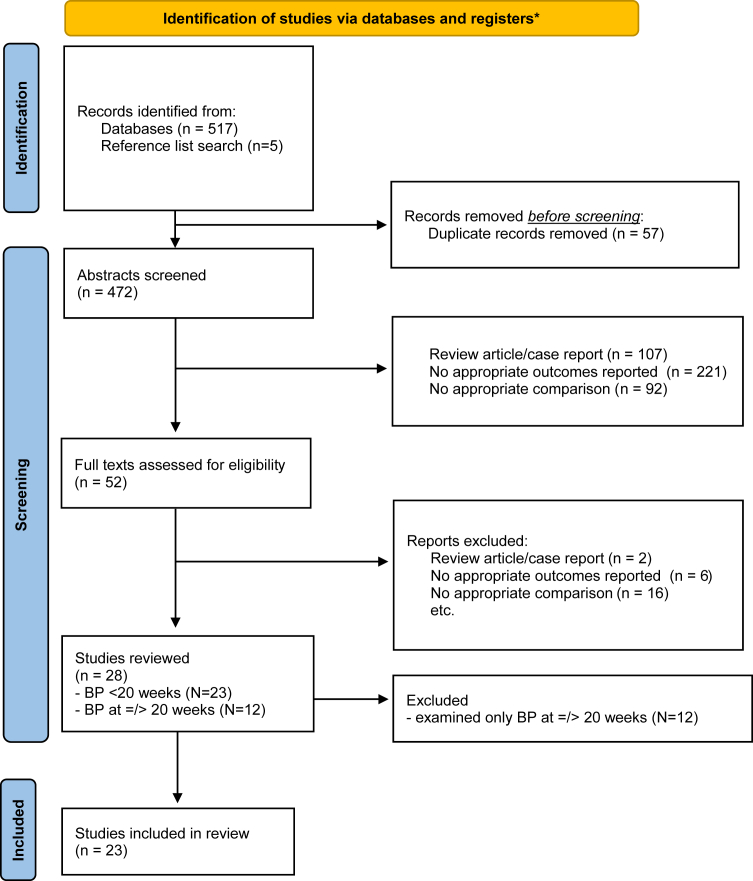
A total of 529 publications were identified in the literature search from January 1, 2017 to September 9, 2021, of which 57 duplicates were removed and 420 were excluded following abstract screening, because they were case reports or review articles (n=107), did not report the relevant outcomes (n=221), or had no appropriate comparison group (n=92). Of 52 articles selected for full-text review, further exclusions (including removal of duplicate publications28) left 23 studies that reported on the association between ACC-AHA BP categories based on BP measurements before 20 weeks gestation and adverse pregnancy outcomes.8, 9, 10, 11,13,14,29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45
Study characteristics and risk of bias
As shown in Table 1, approximately half the studies were retrospective observational designs, conducted in single centers, and primarily in high-income countries, mostly from America (12/23). Just more than half the studies were externally funded. All were included as full publications with a few supplemented with unpublished data. The majority of studies were at high risk of bias, based primarily on their patient selection; for details of the assessments based on the 4 domains of QUADAS-2, refer to Table S1. Each included study was reasonably large, reporting on a median of almost 10,000 pregnancies and collectively reporting on more than 700,000 pregnancies. Most participants were enrolled in the second trimester with only a few recruited in the first trimester. About one-third of studies stated their intention to enroll a low-risk cohort; however, almost all excluded women with a multiple pregnancy, half of the studies excluded women with known chronic hypertension, and in up to a quarter, women were excluded for other medical comorbidities. The rigor of BP measurement varied between studies (Table S2) with 13 of 23 using BP values collected under varied study conditions and the remainder using routinely recorded BP values from the medical record. Only 6 of 23 studies used an average of BP measurements as recommended,5 and 4 of 23 studies used a combination of multiple BP values across visits. No studies used home-based BP measurements.
Table 1.
Characteristics of the included studies and their participants
| Characteristics | <20 weeks gestation (N=23 studies) |
|---|---|
| Studies | |
| Type | |
| Observational retrospective controlled | 12 (52) |
| Observational prospective controlled | 2 (9) |
| Secondary analysis of randomized controlled trial | 9 (39) |
| Center status | |
| Single center | 11 (48) |
| Multiple centers <5 | 2 (10) |
| Multiple centers ≥5 | 11 (48) |
| Low- and middle-income country | 4 (17) |
| Funding reported | |
| None | 2 (10) |
| Not reported | 6 (29) |
| Externally funding reported | 13 (62) |
| Full publication | 23 (100) |
| Includes unpublished data | 4 (17) |
| QUADAS-2 overall risk of bias | |
| High risk | 15 (65) |
| Low risk | 4 (17) |
| Unclear | 4 (17) |
| Participants | |
| Total | 734,377 |
| Number per study | 9869 (2720–19,368) |
| Gestational age at study enrolmenta | |
| 1st trimester | 5 (22) |
| 2nd trimester | 18 (78) |
| 3rd trimester | Not applicable |
| Inclusion criteria | |
| Intention to enroll a low-risk cohort | 8 (35%) |
| Exclusion criteria | |
| Multiple pregnancy | 19 (83) |
| Chronic hypertension | 11 (48) |
| Diabetes mellitus | 5 (22) |
| Chronic kidney disease | 5 (22) |
| Systemic lupus erythematosus | 3 (13) |
| Demographics | |
| Maternal age reported | 20 (87) |
| Age (y), median of reported mean or median (IQR) | 29.6 (26.1–30.5) (20 studies) |
| Number of studies with ≥50% women aged ≥35 y | 2 (12) (9 studies) |
| Nulliparity reported | 21 (91) |
| Nulliparity, median % (IQR) | 43.2 (36.2–74.4) |
| Number of studies with ≥50% nulliparous participants | 9 (39) |
| BMI (kg/m2) reportedb | 20 (87) |
| BMI (kg/m2) (median of mean or median (IQR)) | 25.1 (23.4–26.2) (15 studies) |
| Overweight,c median % (IQR) | 11.5 (9.5–26.3) (8 studies) |
| Ethnicity reported, median % (IQR) | 19 (83) |
| Non-Hispanic White | 36.3 (25.0–50.7) (11 studies) |
| Non-Hispanic Black | 19 (10.6–44.0) (11 studies) |
| Hispanic | 16.4 (1.5–37.5) (11 studies) |
| Asiand | 73.4 (13.6–99.0) (14 studies) |
| Other (median % (IQR) women) | 2.9 (1.7–8.4) (8 studies) |
| N studies without predominance of any one ethnicity | 3/19 (16) |
| Aspirin use for preeclampsia prevention reportede | 10 (43) |
| Aspirin use (median % (IQR) women) | 12.7 (5.8–40.3) (10 studies) |
| BP measurementsf | |
| Nature of BP measurements used to define ACC-AHA level | |
| One measurement | 16 (70) |
| Multiple––at least 2 consecutive measurements | 4 (17) |
| Average of multiple measurements | 5 (22) |
| Normal BP compared with: | |
| Elevated BP | 9 (39) |
| Stage 1 hypertension | 9 (39) |
| Stage 2 hypertension | 7 (30) |
| BP cutoffs examined as new thresholds for abnormal BP: | |
| sBP 120 mmHg (with dBP <80 mmHg) | 8 (35) |
| sBP 130 mmHg or dBP 80 mmHg | 13 (57) |
| sBP 140 mmHg or dBP 90 mmHg | 13 (57) |
| Results presented adjusted for baseline characteristics | 16 (70) |
Data are presented as number (percentage) of pregnancies and median (interquartile range) unless otherwise stated).
ACC-AHA, American College of Cardiology-American Heart Association; BMI, body mass index; BP, blood pressure; dBP, diastolic BP; IQR, interquartile range.
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Not mutually exclusive
Institute of Medicine BMI criteria were used to define overweight (BMI, 25.0–29.9 kg/m2) and obesity (BMI, ≥30 kg/m2), unless ethnicity-refined norms were specified in the publication.11,34 BMI was recorded as a continuous value in 15 of 22 studies and as a cutoff for overweight or obesity in 8 of 22 studies with only 2 of 22 reporting both continuous and cutoff values
The definition of overweight was as defined by the study authors
Studies from China and Japan recorded as >90% Asian population without specific descriptors of study populations, because of low level of ethnic variation in these populations
Aspirin use was reported in studies that enrolled women at increased risk for preeclampsia
BP was categorized as normal (sBP <120 mmHg and dBP <80 mmHg), elevated BP (sBP 120–129 mmHg and dBP <80 mmHg), stage 1 hypertension (sBP 130–139 mmHg and/or dBP 80–89 mmHg), and stage 2 hypertension (sBP ≥140 mmHg and/or dBP ≥90 mmHg), which was also subdivided into nonsevere (sBP 140–159 mmHg and/or dBP 90–109 mmHg) and severe cases (sBP ≥160 mmHg and/or dBP ≥110 mmHg)2. A diagnosis of stage 2 hypertension was accepted when based on prescription of antihypertensive therapy (because there is no precedent for routine treatment of BP <140/90 mmHg).
Synthesis of results
On average, women were about 30 years of age and almost half were nulliparous (Table 1). Most studies reported participants’ BMI with a median of normal to overweight. Most studies did not report ethnicity directly, but if they did, less than half of women were White and approximately 20% were Black or Asian (based primarily on assumptions about where the studies were conducted) and approximately 10% were Hispanic. Data on aspirin use for preeclampsia prevention was reported by close to half of the studies with a median use of 13% of participants.
About two-thirds of studies categorized BP based on 1 measurement (Table 1). Although different studies compared different combinations of ACC-AHA BP categories against each other (Table S3), normal BP was compared with either elevated BP (n=9 studies, 159,573 women), stage 1 hypertension (n=9 studies, 159,573 women), or stage 2 hypertension (n=7 studies, 92,620 women). Only the Community-Level Interventions in Preeclampsia (CLIP) trials subdivided stage 2 hypertension into severe (≥160/110 mmHg) and nonsevere cases (140–159/90–109 mmHg) as reported previously.29,39,41 New BP cutoffs were examined at sBP ≥120 mmHg (regardless of dBP; n=8 studies, 159,573 women), sBP ≥130 mmHg or dBP ≥80 mmHg (n=13 studies, 696,533 women), and sBP ≥140 mmHg or dBP ≥90 mmHg (n=13 studies, 176,348 women).
Overall, 16 studies reported adjustment for maternal covariates, most commonly maternal age, prepregnancy BMI, parity, and/or race and ethnicity8,9,10,11,14,30,31,33,35, 36, 37, 38,42, 43, 44,46; 7 of these studies reported both adjusted and unadjusted analyses.8,9,31,42,43,46,47 In all analyses, adjustment for maternal confounders reduced the association between BP categories and adverse outcomes, most significantly for stage 2 hypertension when reported.
Preeclampsia
Preeclampsia was reported in 21 of 23 (91.0%) studies (661,828 women) at a median event rate of 4.0% (interquartile range [IQR], 2.4–6.3). Of these, 13 studies reported on all BP category comparisons (546,439 women). Most studies used the 2013 or 2019 ACOG definitions of preeclampsia, which did not require the presence of proteinuria for the diagnosis.
The Figure shows that when compared with normal BP, the risk for preeclampsia increased progressively with more advanced BP categories, based on BP measurements before 20 weeks gestation, from an RR of 1.9 (95% CI, 1.6–2.4; I2=87%) for elevated BP to an RR of 3.1 (95% CI, 2.4–3.9; I2=89%) for stage 1 hypertension and an RR of 8.0 for stage 2 hypertension (95% CI, 5.9–11.0; I2=91%). Although there was substantial between-study variation in the effects, it was not the presence of an association that differed between studies but rather the magnitude of the association that differed by more than could be expected by chance alone. A stronger relationship with preeclampsia was seen among studies at low risk of bias, those that were larger, and those with unselected populations for whom multiple routine (clinical) BP measurements were evaluated (Table S2).
Figure.
Relative risk for preeclampsia according to the ACC-AHA BP categories before 20 weeks gestation
ACC-AHA, American College of Cardiology-American Heart Association; BP, blood pressure; CI, confidence interval.
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table 2 shows that each cutoff with a sBP of 120 mmHg (with dBP <80 mmHg), an sBP 130 mmHg and/or a dBP of 80 mmHg, and an sBP of 140 mmHg and/or a dBP of 90 mmHg was associated with an increased risk for preeclampsia when compared with BP values below each of those cutoffs. However, neither an sBP <120/80 mmHg, a BP <130/80 mmHg, nor a BP <140/90 mmHg was useful to rule out development of preeclampsia, with −LR values all well above 0.2. In addition, neither an sBP ≥120 mmHg nor a BP ≥130/80 mmHg was useful to rule in development of preeclampsia; only a BP ≥140/90 mmHg was a good rule-in test for development of preeclampsia based on a pooled +LR of 5.95.
Table 2.
Pooled relative risk and mean likelihood ratios for preeclampsia according to BP cutoffs at <20 weeks gestation based on ACC-AHA BP categories
| Study |
Ref |
RR (95% CI); I2 (95% PI) |
−LR (95% CI) |
+LR (95% CI) |
|---|---|---|---|---|
| Diagnostic threshold: sBP 120 mmHg (and dBP <80 mmHg) | ||||
| Pooled | Normal (<120/80 mmHg) | 3.1 (2.6–4.0); I2=10% (1.1–8.4) |
0.69 (0.54–0.82) | 2.42 (2.07–2.82) |
| Bellad et al,29 2020 | 2.1 (1.7–2.6) | 0.94 (0.92–0.96) | 2.2 (1.73–2.68) | |
| Gonzalez-Valencia et al,32 2020 | 4.1 (1.9–8.9) | 0.55 (0.35–0.89) | 2.63 (1.72–4.02) | |
| Greenberg et al,9 2021 | 3.2 (2.8–3.5) | 0.60 (0.57–0.64) | 2.10 (1.99–2.22) | |
| Qureshi et al,39 2020 | 5.2 (4.1–6.5) | 0.61 (0.54–0.68) | 3.49 (3.04–4.00) | |
| Reddy et al,13 2020 | 3.8 (3.2–4.5) | 0.57 (0.51–0.63) | 2.27 (2.10–2.46) | |
| Rosner et al,40 2019 | 5.9 (2.1–16.0) | 0.39 (0.18–0.82) | 2.52 (1.81–3.50) | |
| Sevene et al,41 2020 | 0.9 (0.3–2.6) | 1.01 (0.90–1.13) | 0.94 (0.37–2.42) | |
| Sutton et al,43 2020 | 2.9 (2.6–3.2) | 0.67 (0.62–0.70) | 2.11 (1.98–2.24) | |
| Diagnostic threshold: sBP 130 mmHg or dBP 80 mmHg | ||||
|---|---|---|---|---|
| Pooled | <130/80 mmHg (normal BP + elevated BP) | 3.6 (2.4–5.6); I2=99% (1.4–9.9) |
0.66 (0.51–0.78) | 2.93 (2.32–3.67) |
| Bellad et al,29 2020 | 0.8 (0.6–0.9) | 0.95 (0.94–0.97) | 2.64 (2.00–3.48) | |
| Bello et al,30 2021 | 8.4 (7.9–8.9) | 0.44 (0.42–0.46) | 4.25 (4.14–4.37) | |
| Darwin et al,8 2021 | 4.7 (3.5–6.3) | 0.56 (0.47–0.66) | 2.98 (2.53–3.50) | |
| Duffy et al,31 2021 | 2.1 (2.0–2.2) | 0.79 (0.77–0.80) | 1.73 (1.69–1.77) | |
| Greenberg et al,9 2021 | 4.3 (3.9–4.8) | 0.67 (0.64–0.70) | 3.37 (3.12–3.64) | |
| Huai et al,35 2021 | 3.1 (2.0–5.0) | 0.36 (0.23–0.55) | 1.35 (1.24–1.46) | |
| McLaren et al,37 2021 | 2.6 (1.7–4.1) | 0.46 (0.32–0.68) | 1.79 (1.43–2.25) | |
| Qureshi et al,39 2020 | 6.0 (4.7–7.5) | 0.68 (0.62–0.75) | 4.71 (3.96–5.61) | |
| Reddy et al,13 2020 | 3.6 (3.0–4.3) | 0.73 (0.69–0.79) | 2.79 (2.46–3.16) | |
| Sabol et al,14 2021 | 4.5 (3.6–5.5) | 0.55 (0.49–0.63) | 3.15 (2.76–3.60) | |
| Sevene et al,41 2020 | 0.5 (0.1–3.3) | 1.03 (0.98–1.10) | 0.46 (0.07–3.25) | |
| Sutton et al,43 2020 | 4.2 (3.8–4.7) | 0.73 (0.70–0.76) | 3.67 (3.35–4.02) | |
| Diagnostic threshold: sBP 140 mmHg or dBP 90 mmHg | ||||
|---|---|---|---|---|
| Pooled | <140/90 mmHg (normal BP + elevated BP + stage 1 HTN) | 5.2 (4.1–6.5); I2=94% (1.7–15.10) | 0.80 (0.69, 0.89) | 5.95 (4.17, 8.12) |
| Bellad et al,29 2020 | 4.8 (3.3–6.9) | 0.98 (0.97–0.99) | 6.38 (3.77–10.79) | |
| Bello et al,30 2021 | 8.3 (7.8–8.8) | 0.73 (0.71–0.74) | 7.66 (7.27–8.07) | |
| Darwin et al,8 2021 | 4.3 (3.2–5.8) | 0.71 (0.63–0.80) | 3.53 (2.80–4.46) | |
| Greenberg et al,9 2021 | 5.6 (5.0–6.3) | 0.75 (0.72–0.78) | 5.49 (4.93–6.12) | |
| Huai et al,35 2021 | 2.9 (2.0–4.1) | 0.45 (0.34–0.60) | 1.61 (1.43–1.81) | |
| McLaren et al,37 2021 | 2.0 (1.4–2.9) | 0.84 (0.73–0.96) | 2.61 (1.41–4.83) | |
| Qureshi et al,39 2020 | 12.7 (9.6–16.8) | 0.88 (0.84–0.92) | 18.82 (12.28–28.83) | |
| Reddy et al,13 2020 | 6.5 (4.8–8.7) | 0.93 (0.90–0.95) | 7.22 (5.17–10.07) | |
| Rosner et al,40 2019 | 4.8 (1.7–13.4) | 0.82 (0.64–1.05) | 4.69 (1.76–12.52) | |
| Sabol et al,14 2021 | 5.3 (4.3–6.5) | 0.67 (0.61–0.73) | 5.24 (4.31–6.36) | |
| Sevene et al,41 2020 | 1.9 (0.3–13.0) | 0.99 (0.93–1.04) | 1.97 (0.26–14.70) | |
| Sutton et al,43 2020 | 5.5 (4.9–6.1) | 0.79 (0.77–0.82) | 5.84 (5.17–6.60) | |
ACC-AHA, American College of Cardiology-American Heart Association; BP, blood pressure; CI, confidence interval; −LR, negative likelihood ratio; +LR, positive likelihood ratio; PI, prediction interval; RR, relative risk.
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table 3 shows the associations and diagnostic test properties for BP cutoffs and other main and secondary outcomes; for details of individual studies, see Tables S4 to 15. There was a general pattern of significant associations between higher BP values measured before <20 weeks gestation and adverse pregnancy outcomes, usually with a dose-response relationship evident, and all adverse outcomes evaluated were associated with stage 2 hypertension. However, as for the outcome of preeclampsia (Table 2), the BP cutoffs for elevated BP or stage 1 hypertension was not useful in ruling out or ruling in adverse pregnancy outcomes. Although a BP <140/90 mmHg could not rule out adverse outcomes, a diagnosis of stage 2 hypertension was useful in identifying women at particular risk for eclampsia, stroke, and maternal ICU admission; these outcomes were informed primarily by trials from less developed countries with community-ascertained outcomes.29,39,41
Table 3.
Pooled relative risk and mean likelihood ratios for other main and secondary outcomes according to BP cutoffs at <20 weeks gestation based on ACC-AHA BP categories
| Outcome |
Ref |
Number of studies |
Number of women |
RR (95% CI); I2 (95% PI) |
−LR (95% CI) |
+LR (95% CI) |
|---|---|---|---|---|---|---|
| Diagnostic threshold: sBP 120 mmHg (with dBP <80 mmHg) | ||||||
| Serious maternal complications | 6a | 51,095 | 1.2 (0.9–1.8); I2=50%, (0.4–3.7) | 0.97 (0.89–1.04) | 1.19 (0.86–1.62) | |
| Preterm birth | 8 | 100,663 | 1.2 (1.0–1.5); I2=94%, (0.6–2.5) | 0.94 (0.89–1.00) | 1.21 (1.01–1.43) | |
| Perinatal death | 5 | 51,699 | 1.4 (1.2–1.6); I2=11%, (1.1–1.7) | 0.94 (0.87–0.97) | 1.34 (1.17–1.54) | |
| Stillbirth | 6 | 51,095 | 1.2 (0.9–1.8); I2=51%, (0.4–3.7) | 0.97 (0.89–1.04) | 1.18 (0.86–1.62) | |
| Newborn death | 5 | 50,410 | 1.4 (1.2–1.7); I2=0%, (1.0–1.9) | 0.94 (0.88–0.98) | 1.35 (1.14–1.59) | |
| SGA | 5 | 68,908 | 1.0 (0.9–1.1); I2=79%, (0.7–1.5) | 1.00 (0.96–1.04) | 1.00 (0.91–1.09) | |
| NICU admission | 3 | 34,401 | 1.5 (1.2–1.8); I2=45%, (0.2–10.15) | 0.87 (0.82–0.92) | 1.36 (1.21–1.52) | |
| Eclampsia | 4 | 38,586 | 2.2 (0.8–6.5); I2=40%, (UTD) | 0.89 (0.62–1.00) | 1.72 (0.97–2.60) | |
| Stroke | 3 | 19,387 | 2.1 (0.7–6.2); I2=63%, (UTD) | 0.88 (0.65–1.03) | 2.08 (0.74–4.39) | |
| Maternal ICU admission | 4 | 38,187 | 1.5 (1.1–2.0); I2=0%, (0.8–2.9) | 0.86 (0.79–0.92) | 2.02 (1.31–3.06) | |
| Placental abruption | 4 | 37,379 | 1.1 (0.9–1.3); I2=0%, (0.7–1.6) | 0.98 (0.93–1.03) | 1.05 (0.90–1.22) | |
| Cesarean | 4 | 19,752 | 1.3 (1.2–1.4); I2=0%, (1.0–1.6), | 0.96 (0.93–0.98) | 1.27 (1.13–1.45) | |
| Diagnostic threshold: sBP 130 mmHg or dBP 80 mmHg | ||||||
| Serious mat complications | 8 | 357,659 | 1.6 (1.3–1.9); I2=29%, (1.1–2.2) | 0.93 (0.89–0.96) | 1.47 (1.18–1.69) | |
| Preterm birth | 13 | 514,632 | 1.5 (1.3–1.8); I2=98%, (0.7–3.3) | 0.92 (0.84–0.96) | 1.49 (1.24–1.77 | |
| Perinatal death | 5 | 51,699 | 1.6 (1.4–1.9); I2=0%, (1.2–2.1) | 0.95 (0.92–0.97) | 1.59 (1.29–1.94) | |
| Stillbirth | 8 | 357,659 | 1.6 (1.3–1.9); I2=29%, (1.1–2.2) | 0.93 (0.89–0.96) | 1.47 (1.28–1.69) | |
| Newborn death | 5 | 50,410 | 1.6 (1.3–2.1); I2=14%, (1.0–2.7) | 0.96 (0.93–0.98) | 1.57 (1.19–2.05) | |
| SGA | 10 | 497,236 | 1.1 (1.0–1.2); I2=78%, (0.8–1.4) | 0.99 (0.96–1.00) | 1.06 (0.99–1.14) | |
| NICU admission | 6 | 462,080 | 1.4 (1.2–1.7); I2=96%, (1.1–1.8) | 0.92 (0.86–0.97) | 1.39 (1.11–1.72) | |
| Eclampsia | 5 | 342,275 | 2.5 (1.1–5.4); I2=66%, (0.1–48.6) | 0.85 (0.67–0.96) | 2.47 (1.39–4.32) | |
| Stroke | 4 | 323,076 | 2.1 (0.8–5.6); I2=76%, (0.0–105.9) | 0.86 (0.84–0.91) | 2.80 (1.40–5.20) | |
| Maternal ICU admission | 4 | 38,187 | 2.3 (1.7–3.1); I2=0%, (1.1–4.6) | 0.93 (0.84–0.99) | 1.78 (1.28–2.35) | |
| Placental abruption | 8 | 344,717 | 1.1 (1.0–1.2); I2=0%, (1.0–1.3) | 0.97 (0.94–0.99) | 1.10 (1.04–1.17) | |
| Cesarean delivery | 7 | 447,431 | 1.3 (1.1–1.6); I2=99%, (1.0–1.9) | 0.95 (0.90–0.97) | 1.45 (1.26–1.69) | |
| Diagnostic threshold: sBP 140 mmHg or dBP 90 mmHg | ||||||
|---|---|---|---|---|---|---|
| Serious maternal complications | 8 | 54,347 | 3.5 (2.5–4.9); I2=0%, (2.3–5.3) | 0.93 (0.86–0.97) | 3.33 (2.23–4.80) | |
| Preterm birth | 12 | 210,923 | 2.3 (2.0–2.6); I2=82%, (1.1–4.6) | 0.95 (0.89–0.98) | 2.51 (2.04–3.06) | |
| Perinatal death | 5 | 51,699 | 2.4 (1.8–3.1); I2=0%, (1.5–3.8) | 0.98 (0.95–0.99) | 2.54 (1.76–3.56) | |
| Stillbirth | 8 | 54,347 | 3.5 (2.5–4.0); I2=0%, (2.3–5.3) | 0.93 (0.86–0.97) | 3.26 (2.23–4.80) | |
| Newborn death | 5 | 50,410 | 1.9 (1.1–3.4); I2=0%, (0.4–9.4) | 0.99 (0.97–1.00) | 2.04 (1.00–3.73) | |
| SGA | 9 | 193,527 | 1.3 (1.2–1.4); I2=47%, (1.0–1.6) | 0.98 (0.96–0.99) | 1.32 (1.17–1.48) | |
| NICU admission | 6 | 158,768 | 1.8 (1.3–2.4); I2=93%, (0.4–9.0) | 0.95 (0.91–0.99) | 1.91 (1.18–3.15) | |
| Eclampsia | 4 | 38,586 | 7.3 (3.8–14.3); I2=0%, (0.1–560.9) | 0.89 (0.69–0.96) | 7.46 (4.16–13.3) | |
| Stroke | 3 | 19,387 | 8.6 (1.5–50.2); I2=0%, (UTD) | 0.90 (0.77–0.98) | 12.7 (2.11–41.10) | |
| Maternal ICU admission | 4 | 38,187 | 4.0 (2.8–5.6); I2=0%, (1.9–8.4) | 0.91 (0.84–0.96) | 6.34 (3.55–10.50) | |
| Placental abruption | 6 | 40,631 | 1.4 (1.0–1.9); I2=0%, (0.8–2.3) | 0.97 (0.91–1.00) | 1.40 (1.04–1.85) | |
| Cesarean delivery | 7 | 144,119 | 1.7 (1.6–1.8); I2=27%, (1.5–1.9) | 0.97 (0.93–0.98) | 2.30 (2.06–2.55) | |
ACC-AHA, American College of Cardiology-American Heart Association; BP, blood pressure; CI, confidence interval; dBP, diastolic blood pressure; ICU, intensive care unit; NICU, neonatal intensive care unit; PI, prediction interval; PPH, postpartum hemorrhage; sBP, systolic blood pressure; SGA, small for gestational age; UTD, unable to determine.
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
One additional study was not included, because complications such as gestational diabetes mellitus, cesarean delivery, and all forms of pregnancy hypertension were part of the composite.39
Other secondary maternal or neonatal outcomes that were reported on by the included studies, but at event rates too low for meaningful comparisons, were maternal postpartum hemorrhage (n=2/23), maternal death (n=3/23), HELLP syndrome (n=3/23), pulmonary edema (n=1/23 studies), acute kidney injury (n=1/23 studies), miscarriage (n=2/23 studies), newborn respiratory support (n=1/23), and neonatal seizures (n=2/23). The following maternal morbidities were not reported at all: intubation or ventilation, cortical blindness, retinal detachment, or liver capsule hematoma.
Discussion
Main findings
This systematic review demonstrated that higher BPs before 20 weeks gestation is associated with a greater risk for subsequent preeclampsia and most adverse pregnancy outcomes. In general, and in comparison with normal BP according to the ACC/AHA criteria, the risk for preeclampsia (and some other adverse outcomes) was greatest among participants with stage 2 hypertension, followed by those with stage 1 hypertension, and then by those with elevated BP. However, when the relevant cutoffs were examined, only the 140/90 mmHg cutoff for stage 2 hypertension when measured before 20 weeks gestation could accurately identify women at increased risk; our findings were similar for other adverse pregnancy outcomes. Neither the lower ACC/AHA BP cutoffs of 120/80 mmHg and 130/80 mmHg nor the currently used 140/90 mmHg cutoff demonstrated any ability to rule out preeclampsia or other adverse pregnancy outcomes. Taken together, these findings suggest that the definition of chronic hypertension in pregnancy, consistent with stage 2 hypertension, should not be revised.
Comparison with the literature
Our findings are consistent with literature reporting that chronic hypertension (ie, stage 2 hypertension) is a major risk factor for superimposed preeclampsia and other adverse pregnancy outcomes.48 By systematic review of 81 observational studies, chronic hypertension was associated with higher odds of developing preeclampsia (∼5-fold), maternal mortality (∼5-fold), cesarean delivery (∼2-fold), stillbirth (∼2-fold), preterm birth (∼2-fold), and SGA infants (∼2-fold).49
Our findings are consistent with the published association between higher BP levels (below 140/90 mmHg) and subsequent preeclampsia, a BP ≥140/90 mmHg being 1 of the criteria along with proteinuria or another manifestations of maternal end-organ dysfunction according to ACOG.50 A recent systematic review of prediction models for gestational hypertension and preeclampsia included 40 different models with varying ability to predict preeclampsia. Of 31 predictors, 17 were related to BP as a continuous measure in 12 studies, as the mean arterial pressure, as diastolic BP in 3, and as systolic BP in 251; only BMI was included more frequently in 19 of 40 models.
Strengths and limitations
Strengths of our analysis include inclusion of more than 700,000 women in diverse locations, from countries in Australasia, South America, South Asia, Africa, and East Asia, although most publications reported on women in America. The included studies reported on multiple populations at different risks for preeclampsia–1 at high risk, 3 using only nulliparous participants, and 7 using other low-risk women.
Although multiple pregnancy was not specifically addressed in this review, only 4 studies included women with multifetal gestations,29,33,39,41 and multiple pregnancy represented only a very small proportion of women.
Limitations included variable definitions of preeclampsia and variable preeclampsia incidence. We had different subsets of studies for evaluation of each ACC-AHA BP level, because only 7 studies reported on all 4 BP categories.9,11,13,29,39,41,43 Many studies combined categories to investigate the association between different BP thresholds instead of investigating the categories individually, which limited our analyses.10,14,31,32,35, 36, 37, 38,40,42,44,45 Although severe preeclampsia was reported in 13 of 23 studies, there was considerable heterogeneity between definitions, often specific to particular study authors; this prohibited use of severe preeclampsia as an outcome for meta-analysis.
We analyzed aggregate data sets, which precluded full exploration of interactions between BP level and other maternal or pregnancy characteristics, as well as use of BP as a continuous variable. Although BP is not used this way in clinical practice, multivariable models suggest that it has independent predictive power for preeclampsia when used in this fashion.52 There were limited possible comparisons for stage 2 hypertension with lower BP categories, and only 1 study reported stage 2 hypertension by severity, making impossible an analysis by severity of existing chronic hypertension.
The influence of demographic factors, particularly overweight and obesity, that compound the risk for adverse pregnancy outcomes is unclear from this analysis. Because this was not an individual participant data meta-analysis, we could not adjust for baseline risk factors; however, given that adjustment factors (eg, obesity) are confounders in the relationship between BP and adverse outcome, the unadjusted analyses would likely have overestimated the relationship between BP and adverse outcome.
Previous studies have not yet addressed whether treatment of hypertension at thresholds <140/90 mmHg in pregnancy is of benefit. However, the Control of Hypertension In Pregnancy Study (CHIPS) trial showed that control of BP (to a diastolic of 85 mmHg) reduced the incidence of severe maternal hypertension and severe features of preeclampsia (ie, platelet count <100×109/L and elevated liver enzymes with symptoms).53 In addition, the recent Control of Hypertension And Pregnancy (CHAP) trial showed a reduction in preeclampsia with severe features and medically indicated delivery at <35+0 weeks.54 In neither CHIPS nor CHAP was BP control associated with an increase in SGA neonates. Treatment for BPs below the current threshold for hypertension is not suggested by any major international guideline.55, 56, 57 Many studies in this review excluded women on antihypertensives for any other indication throughout their pregnancy.
Perspectives
BP measurements taken early in pregnancy contributes to delineating the most appropriate model of surveillance and care throughout pregnancy. Compared with women considered to have normal BP, women with chronic hypertension are seen more frequently and have ultrasound surveillance for fetal growth.56 Adjusting the threshold of chronic hypertension in pregnancy (to a level below 140/90 mmHg) based only on the association with poor outcomes and poor diagnostic test properties for their identification would significantly increase the workload associated with surveillance of these women without tangible benefits. Although also anticipated to increase costs, an economic analysis of such reclassifications still has to be undertaken.58
These data highlight the importance of ongoing monitoring of BP throughout pregnancy, because even normal BP (<120/80 mmHg) before 20 weeks gestation is not useful in ruling out the development of preeclampsia or related adverse pregnancy outcomes after 20 weeks.
Progress in the prediction of preeclampsia or other adverse outcomes from BP measurements is most likely to come from efforts focused on BP levels as a continuous variable or on other BP features (such as variability), specifically as part of multivariable models that include other aspects of maternal history, ultrasonographic assessment, and angiogenic markers.59
Conclusion and implications
This systematic review of publications examining the relationship between the 2017 ACC-AHA BP criteria and pregnancy outcomes has found no evidence that lowering the diagnostic threshold for chronic hypertension in pregnancy to below 140/90 mmHg would assist clinicians in identifying women more likely to develop preeclampsia or other adverse pregnancy outcomes.
Acknowledgments
The authors wish to acknowledge librarian Natalie Dempster, for her assistance with literature searching and associate professors Natalie Bello, MD, MPH, and Qi Li, MT, who kindly provided additional detail from their data for our analysis.
Footnotes
P.v.D. and L.A.M. contributed equally to this study.
The authors report no conflict of interest.
The Pregnancy Care Integrating Translational Science Everywhere (PRECISE) Network was funded by the United Kingdom Research and Innovation’s Grand Challenges Research Fund GROW Award scheme under award number MR/P027938/1.
This study was registered with the International Prospective Register of Systematic reviews (registration 2021 CRD42021229131).
Supplementary Data
Appendix
| Title | Page number | |
|---|---|---|
| Figures | ||
| Figure S1 | PRISMA flow diagram for study inclusion and exclusion | See separate |
| Tables | ||
| Table S1 | Details of QUADAS-2 assessment for included studies | 3-6 |
| Table S2 | Study characteristics arranged by strength of association with preeclampsia by highest BP category reported | 7-8 |
| Table S3 | ACC/AHA blood pressure categories reported by each study for measurements taken <20 weeks | 9 |
| Table S4 | Sensitivity and specificity of ACC/AHA BP categories for preeclampsia | 10 |
| Other main outcomes | ||
| Table S5 | Association of ACC/AHA BP levels at <20 weeks and serious maternal complications | 11 |
| Table S6 | Sensitivity and specificity of ACC/AHA BP categories for serious maternal outcomes | 12 |
| Table S7 | Association of ACC/AHA BP levels at <20 weeks and preterm birth | 13 |
| Table S8 | Sensitivity and specificity of ACC/AHA BP categories for preterm birth | 14 |
| Table S9 | Association of ACC/AHA BP levels at <20 weeks and perinatal death | 15 |
| Table S10 | Sensitivity and specificity of ACC/AHA BP categories for preterm birth | 16 |
| Table S11 | Association of ACC/AHA BP levels at <20 weeks and stillbirth | 17 |
| Table S12 | Sensitivity and specificity of ACC/AHA BP categories for stillbirth | 18 |
| Table S13 | Association of ACC/AHA BP levels at <20 weeks and newborn death | 19 |
| Table S14 | Sensitivity and specificity of ACC/AHA BP categories for newborn death | 20 |
| Table S15 | Association of ACC/AHA BP levels at <20 weeks and SGA infants | 21 |
| Table S16 | Sensitivity and specificity of ACC/AHA BP categories for SGA infants | 22 |
| Table S17 | Association of ACC/AHA BP levels at <20 weeks and NICU admission | 23 |
| Table S18 | Sensitivity and specificity of ACC/AHA BP categories for NICU admission | 24 |
| Other secondary outcomes | ||
| Table S19 | Association of ACC/AHA BP levels at <20 weeks and eclampsia | 25 |
| Table S20 | Sensitivity and specificity of ACC/AHA BP categories for eclampsia | 26 |
| Table S21 | Association of ACC/AHA BP levels at <20 weeks and stroke | 27 |
| Table S22 | Sensitivity and specificity of ACC/AHA BP categories for stroke | 28 |
| Table S23 | Association of ACC/AHA BP levels at <20 weeks and maternal admission to intensive care | 29 |
| Table S24 | Sensitivity and specificity of ACC/AHA BP categories for maternal admission to intensive care | 30 |
| Table S25 | Association of ACC/AHA BP levels at <20 weeks and placental abruption | 31 |
| Table S26 | Sensitivity and specificity of ACC/AHA BP categories for placental abruption | 32 |
| Table S27 | Association of ACC/AHA BP levels at <20 weeks and Cesarean | 33 |
| Table S28 | Sensitivity and specificity of ACC/AHA BP categories for Cesarean | 34 |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Figure S1.
PRISMA flow diagram for study inclusion and exclusion
From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S1.
Details of QUADAS-2 tool for risk-of-bias assessment of for included studies
| Paper | QUADAS domain |
Overall | ||||
|---|---|---|---|---|---|---|
| 1A | 1B | 2 | 3 | 4 | ||
| 29 | Low | Low | Low - thorough description, trained staff, semi-automated machine | Low | Low | Low |
| 30 | Low – singleton only, excluded only if no BP <20 weeks or medical comorbidity requiring antihypertensive use for indication other than lowering BP | Low | Unclear – no description of measurement | Unclear | Low | Unclear |
| 8 | Low – excluded lost to follow up and women given aspirin | Low | Low – single measurement, 5 mins rest, trained staff, automated sphygmomanometer, appropriately sized cuff | Low | Low | Low |
| 31 | Low - excluded <18 years old or fewer than 2 antenatal visits before 20 weeks of gestation | Low | Unclear – no description of measurement | Unclear | High | High |
| 32 | High - excluded chronic diseases including thrombophilia, heart disease, neuropathy, neurodegenerative disease, cancer or autoimmune disease, ART, fetal anomaly or aneuploidy, or delivery at different institution | Low | Unclear –aneroid machine but no other description of measurements | Unclear | Low | High |
| 9 | High – excluded maternal comorbidities – SLE, pre-existing diabetes, lack of maternal weight recorded or gestational weight gain, initiation of antihypertensive medication < 20 weeks without diagnosis of HDP | Low | Unclear – no description of measurement | Unclear | Low | High |
| 33 | High – nulliparous only. Excluded history of 3 or more spontaneous abortions, current pregnancy complicated by aneuploidy or fetal malformation, assisted reproduction with a donor oocyte, multifetal reduction or plans to terminate the pregnancy |
Low | Low – aneroid sphygmomanometer, trained staff, sized cuff, rested and seated, repeated x 3 | Low | Low | High |
| 10 | High – chronic hypertension, multiple pregnancy Included only those with pre-existing diabetes or history of previous PET |
Low | Low – mercury sphygmomanometer, seated 10 mins, trained study staff, cuff to size | Low | Low | High |
| 52 | High – excluded multiple pregnancy, multiparous women, chronic hypertension, missing variables – large proportion excluded | Low | Unclear – booking visit, right arm but no other specifications | Unclear | Low | High |
| 11 | High – excluded PET late pregnancy, birth defects, tobacco and alcohol use, chronic hypertension based on criteria <20 weeks, missing covariates and those who delivered more than once in the study period | Low | Low – seated, automated sphygmomanometer, repeated and averaged | Low | High | High |
| 35 | High – excluded those with missing BP data or chronic hypertension | Low | Low – mercury sphygmomanometer, trained staff, seated, resting, multiple measurements averaged | Low | Low | High |
| 36 | High – excluded multiple pregnancy, stillbirth, diabetes mellitus, thyroid disease, renal disease, chronic hypertension, PCOS, incomplete records | Low | Low – trained staff, mercury sphygmomanometer, upright, right arm, repeated and averaged | Low | Low | High |
| 37 | Low – excluded multiples, anomalies and lost to follow up <20 weeks | Low | Low – manual device, described technique 15 mins seated rest | Low | High – 1933 women met inclusion criteria but only 252 included overall∗ | High |
| 38 | High – excluded multiple pregnancy, miscarriage, stillbirth, chronic hypertension, missing data | Low | Low – automated device, described measurement technique arm at heart level | Low | Low | High |
| 39 | Low | Low | Low - thorough description, trained staff, semi-automated machine | Low | Low | Low |
| 13 | Low – multiple pregnancy, fetal anomalies and no BP measurements in specified gestations | Low | Unclear – trained staff, doesn’t specify which type of sphygmomanometer | Unclear | Low | Unclear |
| 3 | Low – excluded only multiple pregnancy and those entering care >12 weeks | Low | Unclear – BP left arm seated position but no other comments | Unclear | Low | Unclear |
| 14 | Low - excluded multiples, delivery <20 weeks, missing prenatal records or BP data | Low | Unclear – not described | Unclear | Low | Unclear |
| 41 | Low | Low | Low - thorough description, trained staff, semi-automated machine | Low | Low | Low |
| 43 | Low – excluded multiple pregnancy, incomplete records, second delivery in study period or miscarriage | Low | High – records from multiple practices, not regulated by research protocol | High | Low | High |
| 42 | High – cut off was 135/85, excluded chronic hypertension above that, renal disease, diabetes or anyone with proteinuria on dipstick | Low | Low – mercury sphygmomanometer, study staff, seated and rested | Low | Low | High |
| 44 | High – excluded multiples, renal disease, stillbirth, hypertension, diabetes, thyroid dysfunction in early pregnancy | Low | Low – trained nurses, mercury sphygmomanometer, comfortable seat, 2 measurements | Low | Low | High |
| 45 | High – excluded <2 BP measurements <20 weeks, chronic hypertension, cardiovascular or hepatic disease, diabetes, autoimmune disease, multiple gestation or fetal anomaly | Low | Low – automatic sphygmomanometer, at least 2 measurements, seated position, left arm, resting | Low | Low | High |
ACC (American College of Cardiology), AHA (American Heart Association), ART (assisted reproductive technologies), BP (blood pressure), HDP – hypertensive disorder of pregnancy, PCOS (polycystic ovarian syndrome), PET (preeclampsia), SLE (systemic lupus erythematosus)
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
For every patient placed into either the ACC-AHA group or the ACOG group, the next patient with normal blood pressures was placed in the control group.
Table S2.
Study characteristics arranged by strength of association with preeclampsia by highest BP category reported
| QUADAS2 summary | Av age | Av BMI | Ethnicity | MMR of country (per 100 000 live births) | PET definition | PET prevalence | BP device | BP gestation (weeks) | Proportion nulliparous | BP type | BP type – routine or study | Cohort | Total number participants | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 39 | Low | 28 | NS | S Asian | 289 | ISSHP 2018 | 2.5% | Automated | <20 | 23% | Av of 2 or 3 in 1 visit | Study∗ | Unselected | 10839 |
| 30 | Low | 30 | 27 | 52% H | 18 | ICD codes | 3.5% | NS | <20 | 41% | =/>2 visits in 30 days | Routine | Unselected | 132032 |
| 13 | Low | 31 | 30 | Mixed | 6 | ACOG 2019 | 2.9% | Mercury | Multiple | 40% | Single | Routine | Unselected | 18243 |
| 9 | High | 25% >35 | 25% >30 | 56% NHW | 18 | ACOG 2013 | 6.3% | NS | <20 | 43% | =/> 2 visits | Routine | Low risk | 18801 |
| 14 | Low | 28 | 36% >30 | Mixed | 18 | ACOG 2019 | 3.1% | NS | <20 | 41% | Single | Routine | Unselected | 30000 |
| 40 | Low | 34 | 23 | NR | 18 | ND | 3.4% | NS | <20 | 54% | Single | Routine | Unselected | 377 |
| 43 | High | 30 | 27 | 70% NHW | 19 | ICD codes | 6.9% | NS | <20 | 44% | =/> 2 visits | Routine | Unselected | 18162 |
| 29 | Low | 23 | NS | S Asian | 145 | ISSHP 2018 | 13.0% | Automated | <20 | 36% | Av 2 or 3 in 1 visit | Study∗ | Unselected | 6067 |
| 52 | High | 6% >35 | 9% >30 | Asian | 36 | ACOG 2013 | 2.1% | Mercury | 12 | 100% | Single ## | Routine | Nulliparous only | 58054 |
| 8 | Low | 30 | 26 | 51% NHB | 15 | ACOG 2019 | 5.4% | Automated | 11-14 | 74% | Single | Study | Unselected | 2976 |
| 32 | High | 24.2 | 24 | NR | 83 | 7.8% | Anaeroid | <20 | 42% | =/> 2, at least 4 hours apart | Routine | Low risk | 293 | |
| 36ˆ | High | 39 | 22 | Asian | 36 | ACOG 2019 | 1.7% | Mercury | <20 | Av of 3 in 1 visit | Study | Low risk | 6284 | |
| 37 | High | 30 | 26 | Mixed | 18 | ACOG 2013 | 30% | NS | <20 | 35% | Single | Routine | Unselected | 252 |
| 35Δδφ | High | 32 | 25 | Asian | 29 | ACOG 2013 | 18.1% | Mercury | <20 | 36% | Av of 2 in 1 visit | Study | Low risk | 838 |
| 44 | High | NS | 10% >30 | Asian | 29 | ISSHP 2018 | 8.2% | Mercury | <20 | 78% | Av of 2 in 1 visit | Routine | Low risk | 47874 |
| 31 | High | 30 | 26 | 52% H | 19 | ICD codes | 3.7% | NS | <20 | 29% | Single | Routine | Unselected | 303689 |
| 42δφ | Highδ | 21 | 23 | 50% NHB | 12 | ACOG 2003 | 7.8% | Mercury | (+ <20) | 100% | Single | Study | LRN only | 2947 |
| 45 | High | 32 | 21 | Asian | 97 | ACOG 2013 | 3.0% | Automated | <12 | 50% | =/> 2 visits | Routine | Low risk | 2039 |
| 10δφ | High | 25 | 28 | 58% NHB | 12 | ACOG 2003 | 17.9% | Mercury | (+ <20) | Single | Study | High risk | 1020 | |
| 33 | High | 27 | 26 | 61% NHW | 14 | ACOG 2013 | 8.3% | Anaeroid | 11-12 | 100% | Single | Study | Nulliparous only | 8899 |
| 41ˆ | Low | 23 | NS | African | 140 | ISSHP 2018 | 0.9% | Automated | <20 | 31% | Av of 2 or 3 in 1 visit | Study∗ | Unselected | 4163 |
ACOG (American College of Obstetricians and Gynaecologists), Av (average), BP (blood pressure), H (Hispanic), ICD (International Classification of Disease), ISSHP (International Society for Hypertension in Pregnancy), LRN (low risk nulliparous) ND (not defined), NHB (non Hispanic Black), NS (not stated), OPC (observational prospective controlled), ORC (observational retrospective controlled), PET (preeclampsia), S Asian (South Asian), SA (secondary analysis)ˆ includes unpublished data.
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
But used lower if multiple measurements done
Randomised trial
Aspirin trial
Study BP values for CLIP trials.
Table S3.
ACC/AHA blood pressure categories reported by each study
| Paper | Normal | Elevated | Stage 1 hypertension | Stage 2 hypertension |
|---|---|---|---|---|
| Bellad | X | |||
| Bello | X | |||
| Darwin | X | |||
| Duffy | X | |||
| Gonzalez-Valencia | ||||
| Hauspurg 19 | ||||
| Hauspurg 18 | ||||
| He | ||||
| Hu∗ | X | |||
| Huai | ||||
| Li | ||||
| McLaren | X | |||
| Nagao∗ | ||||
| Qureshi | X | |||
| Reddy | X | |||
| Rosner | X | |||
| Sabol | X | |||
| Sevene | X | |||
| Suttton 2020 | X | |||
| Sutton 2018 | ||||
| Wu | ||||
| Yang |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S4.
Sensitivity and Specificity of ACC/AHA BP categories for Preeclampsia
| COMPARATOR | |||
|---|---|---|---|
| BP measured at <20 weeks | Ref | Sensitivity | Specificity |
| ‘ELEVATED BP’ (as a new cut-off) | |||
| Pooled | Normal (<120/80mmHg) | 0.42 [0.25, 0.60] | 0.83 [0.74, 0.89] |
| Bellad | 0.11 [0.09, 0.13] | 0.95 [0.95, 0.95] | |
| Greenberg | 0.56 [0.53, 0.58] | 0.74 [0.73, 0.74] | |
| Qureshi | 0.47 [0.42, 0.53] | 0.86 [0.86, 0.87] | |
| Reddy | 0.57 [0.53, 0.62] | 0.75 [0.74, 0.75] | |
| Rosner | 0.72 [0.49, 0.88] | 0.71 [0.66, 0.76] | |
| Sevene | 0.11 [0.04, 0.25] | 0.88 [0.86, 0.90] | |
| Sutton 2020 | 0.49 [0.46, 0.52] | 0.77 [0.76, 0.77] | |
| ‘STAGE 1 HYPERTENSION’ (as a new cut-off) | |||
| Pooled | Normal + Elevated BP (<130/80mmHg) | 0.44 [0.29, 0.61] | 0.85 [0.74, 0.92] |
| Bellad | 0.07 [0.06, 0.09] | 0.97 [0.97, 0.98] | |
| Bello | 0.63 [0.61, 0.64] | 0.85 [0.85, 0.85] | |
| Darwin | 0.54 [0.47, 0.62] | 0.82 [0.80, 0.83] | |
| Duffy | 0.39 [0.38, 0.40] | 0.77 [0.77, 0.77] | |
| Huai | 0.88 [0.81, 0.92] | 0.35 [0.32, 0.39] | |
| Greenberg | 0.42 [0.39, 0.44] | 0.88 [0.87, 0.88] | |
| McLaren | 0.72 [0.61, 0.81] | 0.60 [0.52, 0.67] | |
| Qureshi | 0.37 [0.31, 0.43] | 0.92 [0.92, 0.93] | |
| Reddy | 0.36 [0.31, 0.43] | 0.87 [0.87, 0.88] | |
| Sabol | 0.54 [0.49, 0.60] | 0.83 [0.81, 0.84] | |
| Sevene | 0.03 [0.00, 0.14] | 0.94 [0.92, 0.95] | |
| Sutton 2020 | 0.34 [0.31, 0.37] | 0.91 [0.90, 0.91] | |
| ‘STAGE 2 HYPERTENSION’ (existing cut-off) | |||
| Pooled | Normal + Elevated BP + Stage 1 HTN (<140/90mmHg) | 0.22 [0.13, 0.36] | 0.96 [0.92, 0.98] |
| Bellad | 0.03 [0.02, 0.04] | 1.00 [0.99, 1.00] | |
| Bello | 0.30 [0.29, 0.31] | 0.96 [0.96, 0.96] | |
| Darwin | 0.36 [0.29, 0.44] | 0.90 [0.89, 0.91] | |
| Greenberg | 0.29 [0.27, 0.32] | 0.95 [0.94, 0.95] | |
| Huai | 0.76 [0.69, 0.82] | 0.53 [0.49, 0.56] | |
| McLaren | 0.24 [0.16, 0.34] | 0.91 [0.86, 0.94] | |
| Qureshi | 0.12 [0.09, 0.17] | 0.99 [0.99, 1.00] | |
| Reddy | 0.08 [0.06, 0.11] | 0.99 [0.99, 0.99] | |
| Sabol | 0.38 [0.33, 0.44] | 0.93 [0.92, 0.94] | |
| Rosner | 0.22 [0.09, 0.45] | 0.95 [0.93, 0.97] | |
| Sevene | 0.03 [0.00, 0.14] | 0.99 [0.98, 0.99] | |
| Sutton 2020 | 0.24 [0.22, 0.27] | 0.96 [0.96, 0.96] | |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S5.
Pooled relative risk and mean likelihood ratios for serious maternal complications, according to BP cut-offs at <20 weeks, determined by ACC/AHA BP categories
| COMPARATOR | ||||
|---|---|---|---|---|
| BP measured at <20 weeks | Ref | RR [95% CI] I2, (95% PI) | -LR | +LR |
| Diagnostic threshold: sBP 120mmHg (with dBP <80mmHg) | ||||
| Pooled | Normal (<120/80mmHg) | 1.2 [0.9, 1.8] I2=51%, (0.4, 3.7) | 0.97 [0.89, 1.04] | 1.19 [0.86, 1.62] |
| Bellad | 1.5 [1.0, 2.2] | 0.97 [0.95, 1.00] | 1.49 [1.02, 2.17] | |
| Qureshi | 1.6 [1.3, 2.1] | 0.91 [0.86, 0.96] | 1.55 [1.27, 1.89] | |
| Reddy | 0.7 [0.4, 1.3] | 1.07 [0.96, 1.20] | 0.79 [0.52, 1.22] | |
| Rosner | 0.4 [0.0, 9.3] | 1.21 [0.72, 2.01] | 0.54 [0.04, 6.79] | |
| Sevene | 0.4 [0.1, 2.8] | 1.05 [0.94, 1.18] | 0.57 [0.12, 2.73] | |
| Sutton 2020 | 2.3 [0.5, 10.1] | 0.75 [0.41, 1.38] | 1.76 [0.80, 3.86] | |
| Diagnostic threshold: sBP 130mmHg or dBP 80mmHg | ||||
| Pooled | Normal + Elevated BP (<130/80mmHg) | 1.6 [1.3, 1.9] I2=29%,(1.1, 2.2) | 0.93 [0.89, 0.96] | 1.47 [1.28, 1.69] |
| Bellad | 1.8 [1.1, 2.9] | 0.98 [0.95, 1.00] | 1.81 [1.12, 2.92] | |
| Duffy | 1.5 [1.3, 1.6] | 0.90 [0.87, 0.94] | 1.31 [1.21, 1.43] | |
| McLaren | 5.0 [0.6, 42.2] | 0.33 [0.05, 1.97] | 1.69 [1.16, 2.48] | |
| Qureshi | 1.8 [1.4, 2.4] | 0.93 [0.89, 0.97] | 1.75 [1.36, 2.27] | |
| Reddy | 0.7 [0.3, 1.5] | 1.04 [0.96, 1.12] | 0.75 [0.39, 1.45] | |
| Sabol | 2.9 [1.1, 7.8] | 0.71 [0.46, 1.10] | 2.10 [1.20, 3.67] | |
| Sevene | 0.8 [0.1, 5.7] | 1.01 [0.92, 1.11] | 0.79 [0.11, 5.45] | |
| Sutton 2020 | 1.4 [0.2, 11.2] | 0.96 [0.71, 1.30] | 1.30 [0.21, 8.00] | |
| Diagnostic threshold: sBP 140mmHg or dBP 90mmHg | ||||
| Pooled | Normal + Elevated BP + Stage 1 HTN (<140/90mmHg) | 3.5 [2.5, 4.9] I2=0%,(2.3, 5.3) | 0.93 [0.86, 0.97] | 3.33 [2.23, 4.80] |
| Bellad | 2.9 [1.3, 6.7] | 0.99 [0.98, 1.00] | 3.36 [1.39, 8.09] | |
| McLaren | 1.3 [0.2, 10.6] | 0.91 [0.62, 1.34] | 1.58 [0.37, 6.76] | |
| Qureshi | 4.3 [2.7, 6.6] | 0.96 [0.94, 0.99] | 5.17 [3.00, 8.90] | |
| Reddy | 1.9 [0.5, 7.7] | 0.98 [0.94, 1.02] | 2.33 [0.68, 7.96] | |
| Rosner | 3.3 [0.2, 66.9] | 0.88 [0.53, 1.47] | 2.91 [0.22, 37.83] | |
| Sabol | 2.8 [0.9, 8.8] | 0.82 [0.62, 1.09] | 2.54 [1.14, 5.64] | |
| Sevene | 2.5 [0.4, 17.7] | 0.95 [0.85, 1.06] | 3.58 [0.70, 18.28] | |
| Sutton 2020 | 2.8 [0.3, 23.6] | 0.86 [0.62, 1.20] | 3.39 [0.80, 14.36] | |
ACC (American College of Cardiology), AHA (American Heart Association), BP (blood pressure), CI (confidence interval), PI (prediction interval), dBP (diastolic BP), -LR (negative likelihood ratio), +LR (positive likelihood rate, sBP (systolic BP)
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S6.
Sensitivity and Specificity of ACC/AHA BP categories for serious maternal complications
| COMPARATOR | |||
|---|---|---|---|
| BP measured at <20 weeks | Ref | Sensitivity | Specificity |
| ‘ELEVATED BP’ (as a new cut-off) | |||
| Pooled | Normal (<120/80mmHg) | 0.19 [0.12, 0.31] | 0.84 [0.73, 0.91] |
| Bellad | 0.08 [0.05, 0.11] | 0.95 [0.95, 0.95] | |
| Qureshi | 0.22 [0.18, 0.27] | 0.86 [0.85, 0.87] | |
| Reddy | 0.21 [0.13, 0.31] | 0.74 [0.73, 0.74] | |
| Sevene | 0.07 [0.02, 0.24] | 0.89 [0.86, 0.91] | |
| Sutton 2020 | 0.44 [0.17, 0.74] | 0.75 [0.74, 0.76] | |
| Rosner | 0.17 [0.02, 0.69] | 0.69 [0.64, 0.73] | |
| ‘STAGE 1 HYPERTENSION’ (as a new cut-off) | |||
| Pooled | Normal + Elevated BP (<130/80mmHg) | 0.19 [0.11, 0.32] | 0.87 [0.76, 0.94] |
| Bellad | 0.05 [0.03, 0.08] | 0.97 [0.97, 0.98] | |
| Duffy | 0.31 [0.28, 0.33] | 0.77 [0.77, 0.77] | |
| McLaren | 0.83 [0.44, 0.97] | 0.51 [0.45, 0.57] | |
| Qureshi | 0.15 [0.11, 0.19] | 0.92 [0.91, 0.92] | |
| Reddy | 0.10 [0.05, 0.19] | 0.86 [0.86, 0.87] | |
| Sabol | 0.44 [0.23, 0.67] | 0.79 [0.78, 0.81] | |
| Sevene | 0.05 [0.01, 0.22] | 0.94 [0.92, 0.96] | |
| Sutton 2020 | 0.14 [0.03, 0.51] | 0.89 [0.89, 0.89] | |
| ‘STAGE 2 HYPERTENSION’ (existing cut-off) | |||
| Pooled | Normal + Elevated BP + Stage 1 HTN (<140/90mmHg) | 0.10 [0.04, 0.20] | 0.97 [0.93, 0.99] |
| Bellad | 0.02 [0.01, 0.03] | 1.00 [0.99, 1.00] | |
| McLaren | 0.21 [0.05, 0.58] | 0.86 [0.82, 0.90] | |
| Qureshi | 0.04 [0.03, 0.07] | 0.99 [0.99, 0.99] | |
| Reddy | 0.03 [0.01, 0.10] | 0.99 [0.98, 0.99] | |
| Rosner | 0.17 [0.02, 0.69] | 0.94 [0.91, 0.96] | |
| Sabol | 0.26 [0.11, 0.50] | 0.90 [0.86, 0.91] | |
| Sevene | 0.07 [0.02, 0.24] | 0.98 [0.97, 0.99] | |
| Sutton 2020 | 0.19 [0.03, 0.53] | 0.94 [0.94, 0.95] | |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S7.
Pooled relative risk and mean likelihood ratios for preterm birth, according to BP cut-offs at <20 weeks, determined by ACC/AHA BP categories
| COMPARATOR | ||||
|---|---|---|---|---|
| BP measured at <20 weeks | Ref | RR [95% CI] I2, (95% PI) | -LR | +LR |
| Diagnostic threshold: sBP 120mmHg (with dBP <80mmHg) | ||||
| Pooled | Normal (<120/80mmHg) |
1.2 [1.0, 1.5] I2=94%, (0.6, 2.5) |
0.95 [0.89, 1.00] | 1.21 [1.01, 1.43] |
| Bellad | 1.2 [1.0, 1.5] | 0.99 [0.97, 1.00] | 1.28 [1.03, 1.60] | |
| Greenberg | 1.6 [1.4, 1.8] | 0.84 [0.80, 0.88] | 1.41 [1.31, 1.52] | |
| Hu | 0.8 [0.7, 0.9] | 1.09[ 1.03, 1.15] | 0.86 [0.78, 0.96] | |
| Qureshi | 1.0 [0.9, 1.0] | 1.01 [0.99, 1.03] | 0.94 [0.83, 1.06] | |
| Reddy | 1.3 [1.1, 1.4] | 0.93 [0.89, 0.97] | 1.21 [1.10, 1.32] | |
| Rosner | 1.6 [0.9, 2.7] | 0.83 [0.65, 1.07] | 1.41 [0.96, 2.07] | |
| Sevene | 1.1 [0.8, 1.5] | 0.98 [0.93, 1.04] | 1.14 [0.74, 1.74] | |
| Sutton 2020 | 1.8 [1.6, 2.0] | 0.83 [0.79, 0.87] | 1.54 [1.42, 1.67] | |
| Diagnostic threshold: sBP 130mmHg or dBP 80mmHg | ||||
| Pooled LR | Normal + ElevatedBP (<130/80mmHg) |
1.5 [1.3, 1.8] I2=98%, (0.7, 3.3) |
0.91 [0.84, 0.96] | 1.49 [1.24, 1.77] |
| Bellad | 1.4 [1.1, 1.8] | 0.99 [0.98, 1.00] | 1.49 [1.11, 2.00] | |
| Bello | 2.0 [1.9, 2.1] | 0.85 [0.84, 0.86] | 1.83 [1.77, 1.90] | |
| Darwin | 2.3 [1.9, 2.8] | 0.77 [0.71, 0.84] | 2.04 [1.74, 2.40] | |
| Duffy | 1.2 [1.2, 1.3] | 0.95 [0.94, 0.95] | 1.18 [1.15, 1.21] | |
| Greenberg | 1.9 [1.7, 2.2] | 0.88 [0.85, 0.91] | 1.78 [1.59, 1.98] | |
| Hu | 0.8 [0.7, 1.0] | 1.05 [1.01, 1.09] | 0.86 [0.75, 0.99] | |
| Huai | 1.0 [0.6, 1.7] | 1.01 [0.82, 1.24] | 0.98 [0.66, 1.47] | |
| McLaren | 2.4 [1.2, 5.1] | 0.55 [0.31, 0.96] | 1.51 [1.16, 1.97] | |
| Qureshi | 1.0 [0.9, 1.2] | 1.00 [0.98, 1.01] | 1.04 [0.89, 1.22] | |
| Reddy | 1.4 [1.2, 1.7] | 0.94 [0.91, 0.97] | 1.38 [1.21, 1.58] | |
| Sabol | 2.2 [1.8, 2.6] | 0.78 [0.72, 0.84] | 1.99 [1.72, 2.30] | |
| Sevene | 1.1 [0.8, 1.7] | 0.99 [0.95, 1.03] | 1.21 [0.66, 2.22] | |
| Sutton 2020 | 2.3 [2.0, 2.6] | 0.87 [0.84, 0.90] | 2.12 [1.88, 2.40] | |
| Diagnostic threshold: sBP 140mmHg or dBP 90mmHg | ||||
| Pooled LR | Normal + Elevated BP +Stage 1 (<140/90mmHg) |
2.3 [2.0, 2.6] I2=82%, [1.1, 4.6] |
0.95 [0.89, 0.98] | 2.52 [2.04, 3.06] |
| Bello | 2.6 [2.5, 2.8] | 0.92 [0.91, 0.93] | 2.77 [2.60, 2.94] | |
| Bellad | 2.2 [1.4, 3.3] | 0.99 [0.99, 1.00] | 2.67 [1.46, 4.89] | |
| Darwin | 2.7 [2.2, 3.3] | 0.82 [0.77, 0.87] | 2.71 [2.20, 3.35] | |
| Greenberg | 2.5 [2.1, 2.9] | 0.90 [0.88, 0.93] | 2.46 [2.12, 2.85] | |
| Hu | 1.0 [0.7, 1.5] | 1.00 [0.98, 1.01] | 1.04 [0.73, 1.48] | |
| McLaren | 4.0 [2.2, 7.6] | 0.68 [0.51, 0.90] | 3.89 [2.15, 7.05] | |
| Qureshi | 1.6 [1.2, 2.0] | 0.99 [0.99, 1.00] | 2.14 [1.34, 3.43] | |
| Reddy | 2.4 [1.8, 3.3] | 0.98 [0.97, 0.99] | 2.66 [1.85, 3.82] | |
| Rosner | 2.1 [0.9, 4.7] | 0.94 [0.84, 1.04] | 2.25 [0.86, 5.85] | |
| Sabol | 2.7 [2.2, 3.2] | 0.83 [0.79, 0.87] | 2.93 [2.37, 3.62] | |
| Sevene | 1.3 [0.7, 2.4] | 0.99 [0.97, 1.01] | 1.48 [0.52, 4.21] | |
| Sutton 2020 | 3.2 [2.7, 3.7] | 0.89 [0.86, 0.91] | 3.19 [2.74, 3.72] | |
ACC (American College of Cardiology), AHA (American Heart Association), BP (blood pressure), dBP (diastolic BP), -LR (negative likelihood ratio), +LR (positive likelihood ratio), sBP (systolic BP), CI (confidence interval), PI (prediction interval)
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S8.
Sensitivity and Specificity of ACC/AHA BP categories for preterm birth
| COMPARATOR | |||
|---|---|---|---|
| BP measured at <20 weeks | Ref | Sensitivity | Specificity |
| ‘ELEVATED BP’ (as a new cut-off) | |||
| Pooled | Normal (<120/80mmHg) | 0.24 [0.14, 0.36] | 0.80 [0.70, 0.88] |
| Bellad | 0.06 [0.05, 0.08] | 0.95 [0.95, 0.96] | |
| Greenberg | 0.39 [0.36, 0.42] | 0.72 [0.72, 0.73] | |
| Hu | 0.34 [0.30, 0.37] | 0.61 [0.60, 0.62] | |
| Qureshi | 0.14 [0.13, 0.16] | 0.85 [0.84, 0.86] | |
| Reddy | 0.31 [0.29, 0.34] | 0.74 [0.73, 0.75] | |
| Sevene | 0.12 [0.08, 0.16] | 0.90 [0.87, 0.92] | |
| Sutton 2020 | 0.37 [0.34, 0.40] | 0.76 [0.75, 0.77] | |
| Rosner | 0.41 [0.28, 0.56] | 0.71 [0.66, 0.75] | |
| ‘STAGE 1 HYPERTENSION’ (as a new cut-off) | |||
| Pooled | Normal + Elevated BP (<130/80mmHg) | 0.22 [0.14, 0.33] | 0.85 [0.78, 0.90] |
| Bellad | 0.04 [0.03, 0.05] | 0.97 [0.97, 0.98] | |
| Bello | 0.28 [0.28, 0.29] | 0.84 [0.84, 0.85] | |
| Darwin | 0.37 [0.32, 0.42] | 0.82 [0.81, 0.83] | |
| Duffy | 0.27 [0.27, 0.28] | 0.77 [0.77, 0.77] | |
| Greenberg | 0.24 [0.22, 0.27] | 0.86 [0.86, 0.87] | |
| Hu | 0.22 [0.19, 0.35] | 0.75 [0.74, 0.75] | |
| Huai | 0.34 [0.23, 0.47] | 0.65 [0.60, 0.70] | |
| McLaren | 0.71 [0.53, 0.84] | 0.53 [0.46, 0.59] | |
| Qureshi | 0.09 [0.08, 0.10] | 0.91 [0.90, 0.92] | |
| Reddy | 0.18 [0.16, 0.21] | 0.87 [0.86, 0.87] | |
| Sabol | 0.36 [0.32, 0.41] | 0.82 [0.80, 0.83] | |
| Sevene | 0.06 [0.04, 0.10] | 0.95 [0.93, 0.95] | |
| Sutton 2020 | 0.22 [0.19, 0.24] | 0.90 [0.89, 0.90] | |
| ‘STAGE 2 HYPERTENSION’ (existing cut-off) | |||
| Pooled | Normal + Elevated BP +Stage 1 HTN (<140/90mmHg) | 0.08 [0.04, 0.16] | 0.97 [0.94, 0.98] |
| Bellad | 0.01 [0.01, 0.02] | 1.00 [0.99, 1.00] | |
| Bello | 0.12 [0.11, 0.13] | 0.96 [0.96, 0.96] | |
| Darwin | 0.26 [0.22, 0.31] | 0.90 [0.89, 0.91] | |
| Greenberg | 0.15 [0.13, 0.18] | 0.94 [0.93, 0.94] | |
| Hu | 0.04 [0.03, 0.06] | 0.96 [0.96, 0.96] | |
| McLaren | 0.39 [0.24, 0.56] | 0.90 [0.85, 0.93] | |
| Qureshi | 0.02 [0.01, 0.02] | 0.99 [0.99, 0.99] | |
| Reddy | 0.03 [0.02, 0.04] | 0.99 [0.99, 0.99] | |
| Rosner | 0.11 [0.05, 0.23] | 0.95 [0.92, 0.97] | |
| Sabol | 0.24 [0.20, 0.28] | 0.92 [0.91, 0.93] | |
| Sevene | 0.02 [0.01, 0.05] | 0.98 [0.97, 0.99] | |
| Sutton 2020 | 0.16 [0.14, 0.18] | 0.95 [0.95, 0.95] | |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S9.
Pooled relative risk and mean likelihood ratios for perinatal death, according to BP cut-offs at <20 weeks, determined by ACC/AHA BP categories
| COMPARATOR | ||||
|---|---|---|---|---|
| BP measured at <20 weeks | Ref | RR [95% CI] I2, (95% PI) |
-LR | +LR |
| Diagnostic threshold: sBP 120mmHg (with dBP <80mmHg) | ||||
| Pooled | Normal (<120/80 mmHg) |
1.4 [1.2, 1.6] I2=11%, (1.1, 1.7) |
0.94 [0.90, 0.97] | 1.34 [1.17, 1.54] |
| Bellad | 1.4 [1.1, 1.9] | 0.98 [0.95, 1.00] | 1.44 [1.06, 1.95] | |
| Greenberg | 1.7 [1.1, 2.5] | 0.84 [0.72, 0.99] | 1.40 [1.09, 1.80] | |
| Qureshi | 1.4 [1.2, 1.7] | 0.93 [0.90, 0.97] | 1.40 [1.20, 1.65] | |
| Reddy | 0.9 [0.6, 1.4] | 1.02 [0.91, 1.14] | 0.94 [0.67, 1.31] | |
| Sevene | 1.1 [0.5, 2.6] | 0.98 [0.88, 1.10] | 1.12 [0.52, 2.43] | |
| Diagnostic threshold: sBP 130mmHg or dBP 80mmHg | ||||
| Pooled | Normal + Elevated BP (<130/80 mmHg) |
1.6 [1.4, 1.9] I2=0%, (1.2, 2.1) |
0.95 [0.92, 0.97] | 1.59 [1.29, 1.94] |
| Bellad | 1.9 {1.4, 2.7] | 0.97 [0.96, 0.99] | 1.97 [1.36, 2.86] | |
| Greenberg | 1.8 [1.1, 2.9] | 0.90 [0.80, 1.00] | 1.62 [1.12, 2.35] | |
| Qureshi | 1.6 [1.3, 1.9] | 0.95 [0.92, 0.98] | 1.58 [1.28, 1.94] | |
| Reddy | 1.1 [0.6, 1.8] | 0.99 [0.92, 1.07] | 1.05 [0.65, 1.68] | |
| Sevene | 1.5 [0.5, 3.9] | 0.97 [0.89, 1.06] | 1.47 [0.55, 3.90] | |
| Diagnostic threshold: sBP 140mmHg or dBP 90mmHg | ||||
| Pooled | Normal + Elevated BP +Stage 1 HTN (<140/90 mmHg) |
2.4 [1.8, 3.1] I2=0%, (1.5, 3.8) |
0.98 [0.95, 0.99] | 2.54 [1.76, 3.56] |
| Bellad | 2.1 [1.2, 3.8] | 0.99 [0.98, 1.00] | 3.60 [1.75, 7.38] | |
| Greenberg | 3.2 [1.7, 5.7] | 0.93 [0.86, 1.00] | 2.00 [1.20, 3.32] | |
| Qureshi | 2.3 [1.5, 3.5] | 0.98 [0.97, 1.00] | 2.59 [1.52, 4.43] | |
| Reddy | 1.4 [0.3, 5.7] | 0.99 [0.97, 1.02] | 1.40 [0.35, 5.58] | |
| Sevene | 2.3 [0.6, 8.6] | 0.97 [0.92, 1.04] | 2.41 [0.56, 10.30] | |
ACC (American College of Cardiology), AHA (American Heart Association), BP (blood pressure), dBP (diastolic BP), -LR (negative likelihood ratio), +LR (positive likelihood ratio), sBP (systolic BP), CI (confidence interval), PI (prediction interval)
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S10.
Sensitivity and Specificity of ACC/AHA BP categories for perinatal death
| COMPARATOR | |||
|---|---|---|---|
| BP measured at <20 weeks | Ref | Sensitivity | Specificity |
| ‘ELEVATED BP’ (as a new cut-off) | |||
| Pooled | Normal (<120/80mmHg) | 0.20 [0.11, 0.33] | 0.85 [0.74, 0.92] |
| Bellad | 0.07 [0.05, 0.10] | 0.95 [0.95, 0.95] | |
| Greenberg | 0.40 [0.30, 0.50] | 0.72 [0.71, 0.72] | |
| Qureshi | 0.20 [0.17, 0.23] | 0.86 [0.85, 0.87] | |
| Reddy | 0.25 [0.17, 0.34] | 0.74 [0.73, 0.74] | |
| Sevene | 0.13 [0.06, 0.25] | 0.89 [0.86, 0.91] | |
| ‘STAGE 1 HYPERTENSION’ (as a new cut-off) | |||
| Pooled | Normal + Elevated BP (<130/80mmHg) | 0.12 [0.07, 0.20] | 0.92 [0.86, 0.96] |
| Bellad | 0.05 [0.04, 0.07] | 0.97 [0.97, 0.98] | |
| Greenberg | 0.23 [0.16, 0.32] | 0.86 [0.85, 0.86] | |
| Qureshi | 0.13 [0.11, 0.16] | 0.92 [0.91, 0.92] | |
| Reddy | 0.14 [0.09, 0.22] | 0.86 [0.86, 0.87] | |
| Sutton 2020 | 0.09 [0.03, 0.20] | 0.94 [0.92, 0.96] | |
| ‘STAGE 2 HYPERTENSION’ (existing cut-off) | |||
| Pooled | Normal + Elevated BP + Stage 1 HTN (<140/90mmHg) | 0.04 [0.02, 0.08] | 0.99 [0.96, 0.99] |
| Bellad | 0.01 [0.01, 0.02] | 1.00 [0.99, 1.00] | |
| Greenberg | 0.14 [0.08, 0.22] | 0.93 [0.93, 0.94] | |
| Qureshi | 0.02 [0.02, 0.04] | 0.99 [0.99, 0.99] | |
| Reddy | 0.02 [0.01, 0.07] | 0.99 [0.98, 0.99] | |
| Sevene | 0.04 [0.01, 0.14] | 0.98 [0.97, 0.99] | |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S11.
Pooled relative risk and mean likelihood ratios for stillbirth, according to BP cut-offs at <20 weeks, determined by ACC/AHA BP categories
| COMPARATOR | ||||
|---|---|---|---|---|
| BP measured at <20 weeks | Ref | RR [95% CI] I2, (95% PI) | -LR | +LR |
| Diagnostic threshold: sBP 120mmHg (with dBP <80mmHg) | ||||
| Pooled | Normal (<120/80mmHg) | 1.3 [0.9, 1.8] I2=51%, (0.4, 3.7) | 0.97 [0.89, 1.04] | 1.19 [0.86, 1.62] |
| Bellad | 1.5 [1.0, 2.2] | 0.97 [0.95, 1.00] | 1.49 [1.02, 2.17] | |
| Qureshi | 1.6 [1.3, 2.1] | 0.91 [0.86, 0.96] | 1.55 [1.27, 1.89] | |
| Reddy | 0.7 [0.4, 1.3] | 1.07 [0.96, 1.20] | 0.79 [0.52, 1.22] | |
| Rosner | 0.4 [0.0, 9.3] | 1.21 [0.72, 2.01] | 0.54 [0.04, 6.79] | |
| Sevene | 0.4 [0.1, 2.8] | 1.05 [0.94, 1.18] | 0.57 [0.12, 2.73] | |
| Sutton 2020 | 2.3 [0.5, 10.1] | 0.75 [0.41, 1.38] | 1.76 [0.80, 3.86] | |
| Diagnostic threshold: sBP 130mmHg or dBP 80mmHg | ||||
| Pooled | Normal + Elevated BP(<130/80mmHg) | 1.6 [1.3, 1.9] I2=29%, (1.1, 2.2) | 0.93 [0.89, 0.96] | 1.47 [1.28, 1.69] |
| Bellad | 1.8 [1.1, 2.9] | 0.98 [0.95, 1.00] | 1.81 [1.12, 2.92] | |
| Duffy | 1.5 [1.3, 1.6] | 0.90 [0.87, 0.94] | 1.31 [1.21, 1.43] | |
| McLaren | 5.0 [0.6, 42.2] | 0.33 [0.05, 1.97] | 1.69 [1.16, 2.48] | |
| Qureshi | 1.8 [1.4, 2.4] | 0.93 [0.89, 0.97] | 1.75 [1.36, 2.27] | |
| Reddy | 0.7 [0.3, 1.5] | 1.04 [0.96, 1.12] | 0.75 [0.39, 1.45] | |
| Sabol | 2.9 [1.1, 7.8] | 0.71 [0.46, 1.10] | 2.10 [1.20, 3.67] | |
| Sevene | 0.8 [0.1, 5.7] | 1.01 [0.92, 1.11] | 0.79 [0.11, 5.45] | |
| Sutton 2020 | 1.4 [0.2, 11.2] | 0.96 [0.71, 1.30] | 1.30 [0.21, 8.00] | |
| Diagnostic threshold: sBP 140mmHg or dBP 90mmHg | ||||
| Pooled | Normal + Elevated BP + Stage 1 HTN (<140/90mmHg) | 3.5 [2.5, 4.0] I2=0%, (2.3, 5.3) | 0.93 [0.86, 0.97] | 3.33 [2.23, 4.80] |
| Bellad | 2.9 [1.3, 6.7] | 0.99 [0.98, 1.00] | 3.36 [1.39, 8.09] | |
| McLaren | 1.3 [0.2, 10.6] | 0.91 [0.62, 1.34] | 1.58 [0.37, 6.76] | |
| Qureshi | 4.3 [2.7, 6.6] | 0.96 [0.94, 0.99] | 5.17 [3.00, 8.90] | |
| Reddy | 1.9 [0.5, 7.7] | 0.98 [0.94, 1.02] | 2.33 [0.68, 7.96] | |
| Rosner | 3.3 [0.2, 66.9] | 0.88 [0.53, 1.47] | 2.91 [0.22, 37.83] | |
| Sabol | 2.8 [0.9, 8.8] | 0.82 [0.62, 1.09] | 2.54 [1.14, 5.64] | |
| Sevene | 2.5 [0.4, 17.7] | 0.95 [0.85, 1.06] | 3.58 [0.70, 18.28] | |
| Sutton 2020 | 2.8 [0.3, 23.6] | 0.86 [0.62, 1.20] | 3.39 [0.80, 14.36] | |
ACC (American College of Cardiology), AHA (American Heart Association), BP (blood pressure), dBP (diastolic BP), -LR (negative likelihood ratio), +LR (positive likelihood ratio), sBP (systolic BP), CI (confidence interval), PI (prediction interval)
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S12.
Sensitivity and Specificity of ACC/AHA BP categories for stillbirth
| COMPARATOR | |||
|---|---|---|---|
| BP measured at <20 weeks | Ref | Sensitivity | Specificity |
| ‘ELEVATED BP’ (as a new cut-off) | |||
| Pooled | Normal (<120/80mmHg) | 0.19 [0.12, 0.31] | 0.84 [0.73, 0.91] |
| Bellad | 0.08 [0.05, 0.11] | 0.95 [0.95, 0.95] | |
| Qureshi | 0.22 [0.18, 0.27] | 0.86 [0.85, 0.87] | |
| Reddy | 0.21 [0.13, 0.31] | 0.74 [0.73, 0.74] | |
| Rosner | 0.17 [0.02, 0.69] | 0.69 [0.64, 0.73] | |
| Sevene | 0.07 [0.02, 0.24] | 0.89 [0.86, 0.91] | |
| Sutton 2020 | 0.44 [0.17, 0.74] | 0.69 [0.64, 0.73] | |
| ‘STAGE 1 HYPERTENSION’ (as a new cut-off) | |||
| Pooled | Normal + Elevated BP (<130/80mmHg) | 0.19 [0.11, 0.32] | 0.87 [0.76, 0.94] |
| Bellad | 0.05 [0.03, 0.08] | 0.97 [0.97, 0.98] | |
| Duffy | 0.31 [0.28, 0.33] | 0.77 [0.77, 0.77] | |
| McLaren | 0.83 [0.44, 0.97] | 0.51 [0.45, 0.57] | |
| Qureshi | 0.13 [0.11, 0.19] | 0.92 [0.91, 0.92] | |
| Reddy | 0.10 [0.05, 0.19] | 0.86 [0.86, 0.87] | |
| Sabol | 0.44 [0.23, 0.67] | 0.79 [0.78, 0.81] | |
| Sevene | 0.05 [0.01, 0.22] | 0.94 [0.92, 0.96] | |
| Sutton 2020 | 0.14 [0.03, 0.51] | 0.89 [0.89, 0.89] | |
| ‘STAGE 2 HYPERTENSION’ (existing cut-off) | |||
| Pooled | Normal + Elevated BP + Stage 1 HTN (<140/90mmHg) | 0.10 [0.04, 0.20] | 0.97 [0.93, 0.99] |
| Bellad | 0.02 [0.01, 0.03] | 1.00 [0.99, 1.00] | |
| McLaren | 0.21 [0.05, 0.58] | 0.86 [0.82, 0.90] | |
| Qureshi | 0.04 [0.03, 0.07] | 0.99 [0.99, 0.99] | |
| Reddy | 0.03 [0.01, 0.10] | 0.99 [0.98, 0.99] | |
| Rosner | 0.17 [0.02, 0.69] | 0.94 [0.91, 0.96] | |
| Sabol | 0.26 [0.11, 0.50] | 0.90 [0.88, 0.91] | |
| Sevene | 0.07 [0.02, 0.24] | 0.98 [0.97, 0.99] | |
| Sutton 2020 | 0.19 [0.04, 0.53] | 0.94 [0.94, 0.95] | |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S13.
Pooled relative risk and mean likelihood ratios for newborn death, according to BP cut-offs at <20 weeks, determined by ACC/AHA BP categories
| COMPARATOR | ||||
|---|---|---|---|---|
| BP measured at <20 weeks | Ref | RR [95% CI] I2, (95% PI) | -LR | +LR |
| Diagnostic threshold: sBP 120mmHg (with dBP <80mmHg) | ||||
| Pooled | Normal (<120/80 mmHg) | 1.4 [1.2, 1.7], I2=0% (1.0, 1.9) | 0.94 [0.88, 0.98] | 1.35 [1.14, 1.59] |
| Bellad | 1.4 [0.9, 2.2] | 0.98 [0.95, 1.01] | 1.44 [0.94, 2.20] | |
| Qureshi | 1.4 [1.1, 1.7] | 0.95 [0.90, 0.99] | 1.33 [1.07, 1.64] | |
| Reddy | 1.6 [0.8, 3.6] | 0.85 [0.64, 1.13] | 1.43 [0.88, 2.30] | |
| Sevene | 2.0 [0.9, 4.4] | 0.89 [0.74, 1.06] | 1.88 [0.97, 3.65] | |
| Sutton 2020 | 1.3 [0.8, 2.2] | 0.93 [0.79, 1.09] | 1.22 [0.85, 1.77] | |
| Diagnostic threshold: sBP 130mmHg or dBP 80mmHg | ||||
| Pooled | Normal + Elevated BP(<130/80mmHg) | 1.6 [1.3, 2.1] I2=15%, (1.0, 2.7) | 0.96 [0.93, 0.98] | 1.57 [1.19, 2.05] |
| Bellad | 2.2 [1.2, 3.5] | 0.97 [0.94, 1.00] | 2.17 [1.33, 3.55] | |
| Qureshi | 1.5 [1.1, 2.0] | 0.96 [0.92, 0.99] | 1.47 [1.12, 1.93] | |
| Reddy | 2.2 [0.9, 5.2] | 0.86 [0.69, 1.07] | 1.90 [1.00, 3.60] | |
| Sevene | 2.1 [0.8, 5.7] | 0.94 [0.83, 1.06] | 2.03 [0.78, 5.32] | |
| Sutton 2020 | 0.9 [0.4, 2.0] | 1.02 [0.94, 1.10] | 0.87 [0.40, 1.86] | |
| Diagnostic threshold: sBP 140mmHg or dBP 90mmHg | ||||
| Pooled | Normal + Elevated BP + Stage 1 HTN (<140/90mmHg) | 1.9 [1.1, 3.4] I2=22%, (0.4, 9.4) | 0.99 [0.99, 1.00] | 2.04 [1.00, 3.73] |
| Bellad | 3.9 [1.7, 8.9] | 0.98 [0.97, 1.00] | 4.54 [1.87, 10.98] | |
| Qureshi | 1.8 [0.9, 3.7] | 0.99 [0.98, 1.00] | 2.00 [0.94, 4.25] | |
| Reddy | 1.3 [0.1, 21.5] | 1.00 [0.95, 1.05] | 1.31 [0.08, 20.46] | |
| Sevene | 1.6 [0.2, 11.2] | 0.97 [0.91, 1.05] | 2.35 [0.45, 12.19] | |
| Sutton 2020 | 0.9 [0.3, 2.7] | 1.00 [0.94, 1.06] | 0.99 [0.36, 2.74] | |
ACC (American College of Cardiology), AHA (American Heart Association), BP (blood pressure), dBP (diastolic BP), -LR (negative likelihood ratio), +LR (positive likelihood ratio), sBP (systolic BP), CI (confidence interval), PI (prediction interval)
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S14.
Sensitivity and Specificity of ACC/AHA BP categories for newborn death
| COMPARATOR | |||
|---|---|---|---|
| BP measured at <20 weeks | Ref | Sensitivity | Specificity |
| ‘ELEVATED BP’ (as a new cut-off) | |||
| Pooled | Normal (<120/80 mmHg) | 0.19 [0.11, 0.33] | 0.89 [0.75, 0.92] |
| Bellad | 0.07 [0.05, 0.11] | 0.95 [0.95, 0.95] | |
| Qureshi | 0.19 [0.15, 0.23] | 0.86 [0.85, 0.87] | |
| Reddy | 0.37 [0.22, 0.56] | 0.74 [0.73, 0.74] | |
| Sevene | 0.21 [0.10, 0.37] | 0.89 [0.86, 0.91] | |
| Sutton 2020 | 0.30 [0.20, 0.42] | 0.75 [0.74, 0.76] | |
| ‘STAGE 1 HYPERTENSION’ (as a new cut-off) | |||
| Pooled | Normal + Elevated BP (<130/80mmHg) | 0.11 [0.07, 0.17] | 0.93 [0.87, 0.96] |
| Bellad | 0.06 [0.03, 0.09] | 0.97 [0.97, 0.98] | |
| Qureshi | 0.12 [0.09, 0.16] | 0.92 [0.91, 0.92] | |
| Reddy | 0.26 [0.13, 0.45] | 0.86 [0.86, 0.87] | |
| Sevene | 0.12 [0.05, 0.27] | 0.94 [0.92, 0.96] | |
| Sutton 2020 | 0.10 [0.04, 0.19] | 0.89 [0.89, 0.89] | |
| ‘STAGE 2 HYPERTENSION’ (existing cut-off) | |||
| Pooled | Normal + Elevated BP +Stage 1 HTN (<140/90mmHg) | 0.03 [0.02, 0.05] | 0.99 [0.97, 0.99] |
| Sutton 2020 | 0.05 [0.02, 0.14] | 0.94 [0.94 , 0.95] | |
| Reddy | 0.02 [0.00, 0.15] | 0.99 [0.98, 0.99] | |
| Bellad | 0.02 [0.01, 0.04] | 1.00 [0.99, 1.00] | |
| Qureshi | 0.02 [0.01, 0.04] | 0.99 [0.99, 0.99] | |
| Sevene | 0.04 [0.01, 0.17] | 0.98 [0.97, 0.99] | |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S15.
Pooled relative risk and mean likelihood ratios for SGA infants, according to BP cut-offs at <20 weeks, determined by ACC/AHA BP categories
| BP measured at <20 weeks | Ref | RR [95% CI] I2, (95% PI) | -LR | +LR |
|---|---|---|---|---|
| Diagnostic threshold: sBP 120mmHg (with dBP <80mmHg) | ||||
| Pooled | Normal (<120/80 mmHg) | 1.0 [0.9, 1.1] I2=79%, (0.7, 1.5) | 1.00 [0.96, 1.04] | 1.00 [0.91, 1.09] |
| Greenberg | 0.9 [0.9, 1.0] | 1.02 [1.00,1.05] | 0.94 [0.88, 1.01] | |
| Hu | 1.1 [1.0, 1.2] | 0.96 [0.92, 1.00] | 1.06 [1.00, 1.13] | |
| Reddy | 0.8 [0.7, 0.9] | 1.05 [1.02, 1.08] | 0.87 [0.78, 0.96] | |
| Rosner | 1.4 [0.7, 2.7] | 0.89 [0.68, 1.18] | 1.24 [0.77, 2.00] | |
| Sutton 2020 | 1.1 [1.0, 1.2] | 0.97 [0.94, 1.00] | 1.09 [1.00, 1.17] | |
| Diagnostic threshold: sBP 130mmHg or dBP 80mmHg | ||||
| Pooled | Normal + ElevatedBP (<130/80 mmHg) |
1.1 [1.0, 1.2] I2=78%, [0.8, 1.4] |
0.98 [0.96, 1.00] | 1.06 [0.99, 1.14] |
| Bello | 1.2 [1.1, 1.2] | 0.97 [0.96, 0.98] | 1.15 [1.10, 1.20] | |
| Darwin | 1.4 [1.1, 1.7] | 0.92 [0.86, 0.99] | 1.31 [1.07, 1.61] | |
| Duffy | 1.0 [1.0, 1.1] | 0.99 [0.99, 1.00] | 1.02 [1.00, 1.04] | |
| Greenberg | 1.0 [0.9, 1.2] | 0.99 [0.98, 1.01] | 1.04 [0.93, 1.15] | |
| Hu | 1.1 [1.0, 1.2] | 0.97 [0.95, 1.00] | 1.08 [0.99, 1.17] | |
| Huai | 0.9 [0.5, 1.7] | 1.03 [0.82, 1.30] | 0.94 [0.59, 1.50] | |
| McLaren | 1.2 [0.6, 2.6] | 0.88 [0.56, 1.36] | 1.13 [0.78, 1.62] | |
| Reddy | 0.9 [0.7, 1.0] | 1.02 [1.00, 1.04] | 0.87 [0.75, 1.01] | |
| Sabol | 0.9 [0.7, 1.1] | 1.03 [0.98, 1.08] | 0.90 [0.73, 1.11] | |
| Sutton 2020 | 1.2 [1.1, 1.4] | 0.97 [0.96, 0.99] | 1.21 [1.07, 1.37] | |
| Diagnostic threshold: sBP 140mmHg or dBP 90mmHg | ||||
| Pooled | Normal + Elevated BP +Stage 1 HTN (<140/90 mmHg) | 1.3 [1.2, 1.4] I2=47%, (1.0, 1.6) | 0.98 [0.96, 0.99] | 1.32 [1.17, 1.48] |
| Bello | 1.3 [1.2 ,1.4] | 0.98 [0.98, 0.99] | 1.35 [1.25, 1.46] | |
| Darwin | 1.2 [0.9, 1.7] | 0.97 [0.92, 1.02] | 1.24 [0.92, 1.66] | |
| Greenberg | 1.2 [1.0, 1.4] | 0.98 [0.97, 1.00] | 1.22 [1.05, 1.42] | |
| Hu | 1.3 [1.1, 1.6] | 0.99 [0.98, 1.00] | 1.31 [1.06, 1.62] | |
| Reddy | 0.7 [0.4, 1.2] | 1.00 [1.00, 1.01] | 0.72 [0.42, 1.24] | |
| Rosner | 2.4 [0.9, 6.3] | 0.92 [0.81, 1.05] | 2.54 [0.91, 7.09] | |
| McLaren | 1.8 [0.8, 4.2] | 0.89 [0.72, 1.09] | 1.79 [0.81, 3.92] | |
| Sabol | 1.1 [0.8, 1.5] | 0.99 [0.95, 1.02] | 1.12 [0.83, 1.50] | |
| Sutton 2020 | 1.6 [1.3, 1.8] | 0.97 [0.95, 0.98] | 1.61 [1.37, 1.89] | |
ACC (American College of Cardiology), AHA (American Heart Association), BP (blood pressure), (diastolic BP), -LR (negative likelihood ratio), +LR (positive likelihood ratio), sBP (systolic BP), SGA (small-for-gestational age), CI (confidence interval), PI (prediction interval)
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S16.
Sensitivity and Specificity of ACC/AHA BP categories for SGA infants
| COMPARATOR | |||
|---|---|---|---|
| BP measured at <20 weeks | Ref | Sensitivity | Specificity |
| ‘ELEVATED BP’ (as a new cut-off) | |||
| Pooled | Normal (<120/80mmHg) | 0.30 [0.24, 0.36] | 0.70 [0.65, 0.75] |
| Greenberg | 0.27 [0.25, 0.29] | 0.71 [0.71, 0.72] | |
| Hu | 0.41 [0.39, 0.43] | 0.61 [0.61, 0.62] | |
| Reddy | 0.23 [0.21, 0.25] | 0.73 [0.73, 0.74] | |
| Rosner | 0.38 [0.23, 0.55] | 0.70 [0.65, 0.74] | |
| Sutton | 0.27 [0.25, 0.29] | 0.75 [0.75, 0.76] | |
| ‘STAGE 1 HYPERTENSION’ (as a new cut-off) | |||
| Pooled | Normal + Elevated BP (<130/80mmHg) | 0.22 [0.17, 0.30] | 0.79 [0.72, 0.84] |
| Bello | 0.19 [0.18, 0.20] | 0.84 [0.83, 0.84] | |
| Darwin | 0.26 [0.21, 0.31] | 0.80 [0.79, 0.82] | |
| Duffy | 0.24 [0.23, 0.24] | 0.77 [0.77, 0.77] | |
| Greenberg | 0.15 [0.13, 0.16] | 0.86 [0.85, 0.86] | |
| Hu | 0.27 [0.25, 0.29] | 0.75 [0.74, 0.76] | |
| Huai | 0.32 [0.20, 0.48] | 0.65 [0.60, 0.70] | |
| McLaren | 0.56 [0.37, 0.72] | 0.51 [0.44, 0.57] | |
| Reddy | 0.12 [0.10, 0.14] | 0.86 [0.89, 0.90] | |
| Sabol | 0.19 [0.16, 0.23] | 0.79 [0.77, 0.80] | |
| Sutton 2020 | 0.13 [0.12, 0.15] | 0.89 [0.89, 0.90] | |
| ‘STAGE 2 HYPERTENSION’ (existing cut-off) | |||
| Pooled | Normal + Elevated BP + Stage 1 HTN (<140/90mmHg) | 0.08 [0.05, 0.13] | 0.94 [0.91, 0.96] |
| Hu | 0.05 [0.04, 0.06] | 0.96 [0.96, 0.96] | |
| Greenberg | 0.08 [0.07, 0.09] | 0.93 [0.93, 0.94] | |
| Sutton | 0.08 [0.07, 0.10] | 0.95 [0.94, 0.95] | |
| Reddy | 0.01 [0.01, 0.02] | 0.99 [0.98, 0.99] | |
| McLaren | 0.22 [0.11, 0.41] | 0.88 [0.83, 0.91] | |
| Darwin | 0.14 [0.11, 0.18] | 0.89 [0.87, 0.90] | |
| Bello | 0.06 [0.06, 0.07] | 0.95 [0.95, 0.95] | |
| Sabol | 0.12 [0.09, 0.15] | 0.90 [0.88, 0.91] | |
| Rosner | 0.12 [0.05, 0.28] | 0.95 [0.92, 0.97] | |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S17.
Pooled relative risk and mean likelihood ratios for NICU admission, according to BP cut-offs at <20 weeks, determined by ACC/AHA BP categories
| COMPARATOR | ||||
|---|---|---|---|---|
| BP measured at <20 weeks | Ref | RR [95% CI] I2, (95% PI) | -LR | +LR |
| Diagnostic threshold: sBP 120mmHg (with dBP <80mmHg) | ||||
| Pooled | Normal (<120/80 mmHg) | 1.5 [1.2, 1.8] I2=45%, (0.2, 10.15) | 0.87 [0.82, 0.92] | 1.36 [1.21, 1.52] |
| Greenberg | 1.3 [1.3, 1.4] | 0.90 [0.87, 0.92] | 1.27 [1.20, 1.35] | |
| Reddy | 1.6 [1.2, 2.1] | 0.87 [0.78, 0.96 | 1.38 [1.15, 1.86] | |
| Rosner | 2.1 [1.2, 3.5] | 0.73 [0.55, 0.96] | 1.70 [1.20, 2.39] | |
| Diagnostic threshold: sBP 130mmHg or dBP 80mmHg | ||||
| Pooled | Normal + ElevatedBP (<130/80 mmHg) | 1.4 [1.2, 1.7] I2=96%, (1.1, 1.8) | 0.92 [0.86, 0.97] | 1.39 [1.11, 1.72] |
| Bello | 1.7 [1.6, 1.7] | 0.89 [0.88, 0.90] | 1.56 [1.50, 1.62] | |
| Darwin | 2.2 [1.8, 2.7] | 0.78 [0.72, 0.85] | 1.97 [1.66, 2.32] | |
| Duffy | 1.2 [1.1, 1.3] | 0.96 [0.94, 0.98] | 1.14 [1.08, 1.19] | |
| Greenberg | 1.4 [1.3, 1.6] | 0.93 [0.92, 0.95] | 1.43 [1.31, 1.56] | |
| Reddy | 1.7 [1.2, 2.3] | 0.91 [0.85, 0.98] | 1.55 [1.18, 2.03] | |
| Sabol | 0.9 [0.8, 1.1] | 1.03 [0.98, 1.07] | 0.91 [0.76, 1.09] | |
| Diagnostic threshold: sBP 140mmHg or dBP 90mmHg | ||||
| Pooled | Normal + Elevated BP + Stage 1 HTN (<140/90 mmHg) | 1.8 [1.3, 2.4] I2=93%, (0.4, 9.0) | 0.95 [0.91, 0.99] | 1.98 [1.18, 3.15] |
| Bello | 2.0 [1.9, 2.1] | 0.95 [0.94, 0.96] | 2.06 [1.92, 2.20] | |
| Darwin | 2.4 [1.9, 3.0] | 0.84 [0.79, 0.90] | 2.40 [1.92, 2.99] | |
| Greenberg | 1.5 [1.4, 1.7] | 0.96 [0.95, 0.97] | 1.62 [1.43, 1.85] | |
| Reddy | 4.1 [2.3, 7.4] | 0.96 [0.93, 0.99] | 4.11 [2.28, 7.43] | |
| Rosner | 2.0 [0.9, 4.5] | 0.94 [0.85, 1.04] | 2.14 [0.82, 5.58] | |
| Sabol | 0.7 [0.6, 1.0] | 1.04 [1.01, 1.07] | 0.71 [0.53, 0.96] | |
ACC (American College of Cardiology), AHA (American Heart Association), BP (blood pressure), dBP (diastolic BP), -LR (negative likelihood ratio), +LR (positive likelihood ratio), NICU (neonatal intensive care unit), sBP (systolic BP), CI (confidence interval), PI (prediction interval)
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S18.
Sensitivity and Specificity of ACC/AHA BP categories for NICU admission
| COMPARATOR | |||
|---|---|---|---|
| BP measured at <20 weeks | Ref | Sensitivity | Specificity |
| ‘ELEVATED BP’ (as a new cut-off) | |||
| Pooled | Normal (<120/80 mmHg) | 0.36 [0.33, 0.39] | 0.73 [0.61, 0.74] |
| Greenberg | 0.35 [0.33, 0.37] | 0.73 [0.72, 0.73] | |
| Reddy | 0.36 [0.30, 0.43] | 0.74 [0.73, 0.75] | |
| Rosner | 0.48 [0.34, 0.62] | 0.72 [0.67, 0.76] | |
| ‘STAGE 1 HYPERTENSION’ (as a new cut-off) | |||
| Pooled | Normal + Elevated BP (<130/80mmHg) | 0.24 [0.20, 0.29] | 0.83 [0.79, 0.86] |
| Bello | 0.25 [0.24, 0.26] | 0.84 [0.84, 0.84] | |
| Darwin | 0.36 [0.31, 0.41] | 0.82 [0.80, 0.83] | |
| Duffy | 0.27 [0.25, 0.28] | 0.77 [0.77, 0.77] | |
| Greenberg | 0.19 [0.18, 0.21] | 0.87 [0.86, 0.87] | |
| Reddy | 0.21 [0.16, 0.27] | 0.86 [0.86, 0.87] | |
| Sabol | 0.19 [0.16, 0.23] | 0.79 [0.77, 0.80] | |
| ‘STAGE 2 HYPERTENSION’ (existing cut-off) | |||
| Pooled | Normal + Elevated BP + Stage 1 HTN (<140/90mmHg) | 0.10 [0.06, 0.16] | 0.95 [0.90, 0.97] |
| Bello | 0.09 [0.09, 0.10] | 0.95 [0.95, 0.96] | |
| Darwin | 0.24 [0.20, 0.29] | 0.90 [0.89, 0.91] | |
| Greenberg | 0.10 [0.09, 0.11] | 0.94 [0.93, 0.94] | |
| Reddy | 0.05 [0.03, 0.09] | 0.99 [0.99, 0.99] | |
| Rosner | 0.19 [0.05, 0.22] | 0.95 [0.92, 0.97] | |
| Sabol | 0.08 [0.06, 0.10] | 0.89 [0.88, 0.90] | |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S19.
Pooled relative risk and mean likelihood ratios for eclampsia, according to BP cut-offs at <20 weeks, determined by ACC/AHA BP categories
| COMPARATOR | ||||
|---|---|---|---|---|
| BP measured at <20 weeks | Ref | RR [95% CI] I2, (95% PI) | -LR | +LR |
| Diagnostic threshold: sBP 120mmHg (with dBP <80mmHg) | ||||
| Pooled | Normal (<120/80 mmHg) | 2.2 [0.8, 6.5] I2=40%, (UTD) | 0.87 [0.62, 1.00] | 1.73 [0.97, 2.60] |
| Bellad | 0.5 [0.1, 3.7] | 1.01 [0.95, 1.08] | 0.76 [0.16, 3.64] | |
| Greenberg | 2.7 [1.3, 5.5] | 0.68 [0.47, 0.97] | 1.82 [1.30, 2.55] | |
| Qureshi | 5.7 [0.8, 40.6] | 0.59 [0.24, 1.41] | 3.36 [1.40,8.09] | |
| Sevene | - | 0.57 [0.08, 4.05] | 4.07 [0.57, 29.11] | |
| Diagnostic threshold: sBP 130mmHg or dBP 80mmHg | ||||
| Pooled | Normal + Elevated BP(<130/80 mmHg) | 2.5 [1.1, 5.4] I2=66%, (0.1, 48.6) | 0.84 [0.67, 0.96] | 2.57 [1.39, 4.32] |
| Bellad | 0.9 [0.1, 6.7] | 0.99 [0.93, 1.06] | 1.35 [0.28, 6.51] | |
| Duffy | 1.5 [1.2, 5.4] | 0.89 [0.81, 0.97] | 1.37 [1.13, 1.65] | |
| Greenberg | 3.8 [1.9, 7.9] | 0.71 [0.54, 0.94] | 2.76 [1.79, 4.27] | |
| Qureshi | 10.2 [1.4, 72.2] | 0.55 [0.23, 1.32] | 5.60 [2.32, 13.50] | |
| Sevene | - | 0.53 [0.08, 3.79] | 7.75 [1.07, 55.88] | |
| Diagnostic threshold: sBP 140mmHg or dBP 90mmHg | ||||
| Pooled | Normal + Elevated BP + Stage 1 HTN (<140/90 mmHg) | 7.3 [3.8, 14.3] I2=0% (0.1, 560.9) | 0.87 [0.69, 0.96] | 7.79 [4.16, 13.30] |
| Bellad | 5.2 [0.7, 37.6] | 0.96 [0.90, 1.03] | 7.50 [1.53, 36.65] | |
| Greenberg | 7.5 [3.6, 15.7] | 0.69 [0.53, 0.89] | 5.31 [3.34, 8.64] | |
| Qureshi | 10.0 [0.5, 183.7] | 0.91 [0.68, 1.22] | 9.07 [0.65, 126.89] | |
| Sevene | - | 0.51 [0.07, 3.62] | 24.08 [3.22, 179.93] | |
ACC (American College of Cardiology), AHA (American Heart Association), BP (blood pressure), dBP (diastolic BP), -LR- (negative likelihood ratio), +LR (positive likelihood ratio), sBP (systolic BP), UTD (unable to determine), CI (confidence interval), PI (prediction interval)
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S20.
Sensitivity and Specificity of ACC/AHA BP categories for eclampsia
| COMPARATOR | |||
|---|---|---|---|
| BP measured at <20 weeks | Ref | Sensitivity | Specificity |
| ‘ELEVATED BP’ (as a new cut-off) | |||
| Pooled | Normal (<120/80 mmHg) | 0.23 [0.08, 0.52] | 0.89 [0.75, 0.94] |
| Bellad | 0.04 [0.01, 0.16] | 0.95 [0.94, 0.95] | |
| Greenberg | 0.52 [0.35, 0.68] | 0.72 [0.71, 0.72] | |
| Qureshi | 0.50 [0.17, 0.83] | 0.85 [0.84, 0.86] | |
| Sevene | 0.50 [0.05, 0.95] | 0.88 [0.85, 0.90] | |
| ‘STAGE 1 HYPERTENSION’ (as a new cut-off) | |||
| Pooled | Normal + Elevated BP (<130/80mmHg) | 0.23 [0.11, 0.42] | 0.91 [0.82, 0.96] |
| Bellad | 0.25 [0.24, 0.26] | 0.84 [0.84, 0.84] | |
| Greenberg | 0.39 [0.24, 0.56] | 0.86 [0.85, 0.86] | |
| Duffy | 0.32 [0.26, 0.38] | 0.77 [0.76, 0.77] | |
| Qureshi | 0.50 [0.17, 0.83] | 0.91 [0.90, 0.92] | |
| Sevene | 0.50 [0.05, 0.95] | 0.94 [0.92, 0.95] | |
| ‘STAGE 2 HYPERTENSION’ (existing cut-off) | |||
| Pooled | Normal + Elevated BP +Stage 1 HTN (<140/90mmHg) | 0.13 [0.04, 0.34] | 0.98 [0.95, 0.99] |
| Bellad | 0.04 [0.01, 0.16] | 0.99 [0.99, 1.00] | |
| Greenberg | 0.36 [0.22, 0.53] | 0.93 [0.93, 0.94] | |
| Qureshi | 0.10 [0.01, 0.54] | 0.99 [0.99, 0.99] | |
| Sevene | 0.50 [0.05, 0.95] | 0.98 [0.97, 0.99] | |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S21.
Pooled relative risk and mean likelihood ratios for stroke, according to BP cut-offs at <20 weeks, determined by ACC/AHA BP categories
| COMPARATOR | ||||
|---|---|---|---|---|
| BP measured at <20 weeks | Ref | RR [95% CI] I2, (95% PI) | -LR | +LR |
| Diagnostic threshold: sBP 120mmHg (with dBP <80mmHg) | ||||
| Pooled | Normal (<120/80 mmHg) | 2.1 [0.7, 6.2], I2= 63% (UTD) | 0.89 [0.65, 1.03] | 2.08 [0.74, 4.39] |
| Bellad | 3.5 [1.0, 12.2] | 0.88 [0.72, 1.08] | 3.13[1.11, 8.81] | |
| Qureshi | 3.4 [1.5, 7.8] | 0.73 [0.54, 1.00] | 2.52 [1.50, 4.23] | |
| Sevene | 0.6 [0.1, 2.4] | 1.05 [0.95, 1.17] | 0.59 [0.15, 2.28] | |
| Diagnostic threshold: sBP 130mmHg or dBP 80mmHg | ||||
| Pooled | Normal + ElevatedBP (<130/80mmHg) | 2.1 [0.8, 5.6] I2=76%, (0.0, 105.9) | 0.86 [0.84, 0.91] | 2.8 [1.4, 5.2] |
| Bellad | 6.5 [1.9, 22.2] | 0.84 [0.68, 1.04] | 6.18 [2.39, 16.01] | |
| Duffy | 1.3 [1.1, 1.4] | 0.94 [0.91, 0.97] | 1.19 [1.09, 1.29] | |
| Qureshi | 3.4 [1.4, 8.5] | 0.81 [0.64, 1.02] | 2.93 [1.50, 5.69] | |
| Sevene | 0.3 [0.0, 4.3] | 1.05 [1.00, 1.10] | 0.27 [0.02, 4.21] | |
| Diagnostic threshold: sBP 140mmHg or dBP 90mmHg | ||||
| Pooled | Normal + Elevated BP +Stage 1 HTN (<140/90 mmHg) | 8.6 [1.5, 50.2] I2=70%, (UTD) | 0.90 [0.77, 0.98] | 12.7 [2.11, 41.10] |
| Bellad | 22.8 [5.4, 97.3] | 0.87 [0.73, 1.04] | 24.72 [7.58, 80.60] | |
| Qureshi | 12.6 [3.8, 41.4] | 0.87 [0.74, 1.02] | 12.87 [4.75, 34.88] | |
| Sevene | 0.9 [0.1, 13.5] | 1.00 [0.96, 1.05] | 0.83 [0.05, 13.53] | |
ACC (American College of Cardiology), AHA (American Heart Association), BP (blood pressure), dBP (diastolic BP), -LR- (negative likelihood ratio), +LR (positive likelihood ratio), sBP (systolic BP), UTD (unable to determine), CI (Confidence interval), PI (prediction interval)
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S22.
Sensitivity and Specificity of ACC/AHA BP categories for stroke
| COMPARATOR | |||
|---|---|---|---|
| BP measured at <20 weeks | Ref | Sensitivity | Specificity |
| ‘ELEVATED BP’ (as a new cut-off) | |||
| Pooled | Normal (<120/80 mmHg) | 0.19 [0.06, 0.43] | 0.90 [0.82, 0.95] |
| Bellad | 0.17 [0.06, 0.39] | 0.95 [0.94, 0.95] | |
| Qureshi | 0.38 [0.21, 0.57] | 0.85 [0.84, 0.86] | |
| Sevene | 0.07 [0.02, 0.22] | 0.88 [0.86, 0.90] | |
| ‘STAGE 1 HYPERTENSION’ (as a new cut-off) | |||
| Pooled |
Normal + Elevated BP (<130/80mmHg) |
0.21 [0.17, 0.27] | 0.92 [0.82, 0.97] |
| Bellad | 0.25 [0.24, 0.26] | 0.84 [0.84, 0.84] | |
| Duffy | 0.28 [0.26, 0.30] | 0.77 [0.76, 0.77] | |
| Qureshi | 0.26 [0.13, 0.46] | 0.91 [0.90, 0.92] | |
| Sevene | 0.02 [0.00, 0.14] | 0.94 [0.92, 0.95] | |
| ‘STAGE 2 HYPERTENSION’ (existing cut-off) | |||
| Pooled | Normal + Elevated BP +Stage 1 HTN (<140/90mmHg) | 0.10 [0.04, 0.24] | 0.99 [0.98, 1.00] |
| Bellad | 0.13 [0.04, 0.35] | 0.99 [0.99, 1.00] | |
| Qureshi | 0.14 [0.05, 0.32] | 0.99 [0.99, 0.99] | |
| Sevene | 0.02 [0.00, 0.14] | 0.98 [0.97, 0.99] | |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S23.
Pooled relative risk and mean likelihood ratios for maternal ICU admission, according to BP cut-offs at <20 weeks, determined by ACC/AHA BP categories
| COMPARATOR | ||||
|---|---|---|---|---|
| BP measured at <20 weeks | Ref | RR [95%CI] I2, (95% PI) | -LR | +LR |
| Diagnostic threshold: sBP 120mmHg (with dBP <80mmHg) | ||||
| Pooled | Normal (<120/80 mmHg) | 1.5 [1.1, 2.0] I2= 0%, (0.8, 2.9) | 0.86 [0.79, 0.92] | 2.02 [1.31, 3.06] |
| Bellad | 2.5 [0.3, 20.5] | 0.92 [0.71, 1.20] | 2.34 [0.37, 14.66] | |
| Greenberg | 1.5 [1.1, 2.0] | 0.89 [0.79, 0.99] | 1.29 [1.06, 1.57] | |
| Qureshi | 3.8 [0.6, 22.6] | 0.71 [0.34, 1.44] | 2.67 [0.91, 7.83] | |
| Sevene | 2.6 [0.3, 24.4] | 0.85 [0.48, 1.49] | 2.81 [0.40, 12.04] | |
| Diagnostic threshold: sBP 130mmHg or dBP 80mmHg | ||||
| Pooled | Normal + ElevatedBP (<130/80mmHg) | 2.3 [1.7, 3.1] I2= 0%, (1.1, 4.6) | 0.94 [0.84, 0.99] | 1.78 [1.28, 2.35] |
| Bellad | 1.9 [0.1, 32.9] | 0.97 [0.83, 1.14] | 1.85 [0.12, 27.40] | |
| Greenberg | 2.3 [1.7, 3.2] | 0.84 [0.77, 0.92] | 1.98 [1.56, 2.51] | |
| Qureshi | 0.9 [0.1, 16.7] | 1.01 [0.79, 1.28] | 0.93 [0.07, 13.25] | |
| Sevene | 1.7 [0.1, 31.6] | 0.96 [0.72, 1.28] | 1.65 [0.12, 23.14] | |
| Diagnostic threshold: sBP 140mmHg or dBP 90mmHg | ||||
| Pooled | Normal + Elevated BP + Stage 1 HTN (<140/90 mmHg) | 4.0 [2.8, 5.6] I2= 0%, (1.9, 8.4) | 0.91 [0.84, 0.96] | 6.34 [3.55, 10.50] |
| Bellad | 3.9 [2.7, 5.5] | 0.83 [0.77, 0.90] | 3.34 [2.53, 4.41] | |
| Greenberg | 10.7 [0.6, 182.8] | 0.95 [0.81, 1.11] | 10.12 [0.68, 151.30] | |
| Qureshi | 8.0 [0.4, 143.0] | 0.93 [0.73, 1.18] | 7.39 [0.52, 105.91] | |
| Sevene | 5.6 [0.3, 100.3] | 0.92 [0.69, 1.23] | 5.14 [0.35, 74.41] | |
ACC (American College of Cardiology), AHA (American Heart Association), BP (blood pressure), dBP (diastolic BP), -LR- (negative likelihood ratio), +LR (positive likelihood ratio), sBP (systolic BP), CI (confidence interval), PI (prediction interval)
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S24.
Sensitivity and Specificity of ACC/AHA BP categories for maternal ICU admission
| COMPARATOR | |||
|---|---|---|---|
| BP measured at <20 weeks | Ref | Sensitivity | Specificity |
| ‘ELEVATED BP’ (as a new cut-off) | |||
| Pooled | Normal (<120/80mmHg) | 0.26 [0.17, 0.37] | 0.87 [0.75, 0.94] |
| Bellad | 0.12 [0.02, 0.47] | 0.95 [0.94, 0.95] | |
| Greenberg | 0.36 [0.30, 0.44] | 0.72 [0.71, 0.72] | |
| Qureshi | 0.40 [0.12, 0.77] | 0.85 [0.84, 0.86] | |
| Sevene | 0.25 [0.05, 0.70] | 0.89 [0.86, 0.91] | |
| ‘STAGE 1 HYPERTENSION’ (as a new cut-off) | |||
| Pooled | Normal + Elevated BP (<130/80mmHg) | 0.13 [0.05, 0.27] | 0.93 [0.87, 0.96] |
| Bellad | 0.06 [0.01, 0.37] | 0.97 [0.97, 0.97] | |
| Greenberg | 0.28 [0.22, 0.35] | 0.86 [0.85, 0.86] | |
| Qureshi | 0.08 [0.01, 0.48] | 0.91 [0.90, 0.92] | |
| Sevene | 0.10 [0.01, 0.54] | 0.94 [0.92, 0.95] | |
| ‘STAGE 2 HYPERTENSION’ (existing cut-off) | |||
| Pooled | Normal + Elevated BP +Stage 1 HTN (<140/90mmHg) | 0.10 [0.05, 0.20] | 0.98 [0.95, 0.99] |
| Bellad | 0.06 [0.01, 0.37] | 0.99 [0.99, 1.00] | |
| Greenberg | 0.22 [0.17, 0.29] | 0.93 [0.93, 0.94] | |
| Qureshi | 0.08 [0.01, 0.48] | 0.99 [0.99, 0.99] | |
| Sevene | 0.10 [0.01, 0.54] | 0.98 [0.97, 0.99] | |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S25.
Pooled relative risk and mean likelihood ratios for placental abruption, according to BP cut-offs at <20 weeks, determined by ACC/AHA BP categories
| COMPARATOR | ||||
|---|---|---|---|---|
| BP measured at <20 weeks | Ref | RR [95% CI] I2, (95% PI) | -LR | +LR |
| Diagnostic threshold: sBP 120mmHg (with dBP <80mmHg) | ||||
| Pooled LR | Normal (<120/80 mmHg) | 1.1 [0.9, 1.3] I2=0%, (0.7, 1.6) | 0.98 [0.93, 1.03] | 1.05 [0.90, 1.22] |
| Greenberg | 1.1 [0.8, 1.5] | 0.98 [0.89, 1.08] | 1.05 [0.84, 1.32] | |
| Qureshi | 1.0 [0.6, 1.7] | 1.00 [0.90. 1.10] | 1.02 [0.60, 1.74] | |
| Sevene | 0.8 [0.1, 10.1] | 1.20 [0.40, 3.62] | 0.67 [0.04, 10.05] | |
| Sutton 2020 | 1.1 [0.8, 1.5] | 0.97 [0.90, 1.05] | 1.08 [0.88, 1.32] | |
| Diagnostic threshold: sBP 130mmHg or dBP 80mmHg | ||||
| Pooled LR | Normal + ElevatedBP (<130/80 mmHg) | 1.1 [1.0, 1.2] I2=0%, (1.0, 1.3) | 0.97 [0.94, 0.99] | 1.10 [1.04, 1.17] |
| Duffy | 1.1 [1.1, 1.2] | 0.97 [0.95, 0.99] | 1.11 [1.04, 1.18] | |
| Huai | 1.0 [0.6, 1.9] | 0.99 [0.78, 1.25] | 1.03 [0.66, 1.59] | |
| Greenberg | 1.3 [0.9, 1.9] | 0.96 [0.89, 1.02] | 1.27 [0.92, 1.74] | |
| McLaren | 1.0 [0.1, 15.8] | 1.00 [0.32, 3.12] | 1.00 [0.32, 3.12] | |
| Qureshi | 1.2 [0.7, 2.1] | 0.97 [0.89, 1.06] | 1.28 [0.66, 2.47] | |
| Sabol | 1.0 [0.5, 2.1] | 0.99 [0.85, 1.16] | 1.03 [0.58, 1.81] | |
| Sevene | 0.8 [0.1, 10.1] | 1.20 [0.40, 3.62] | 0.67 [0.04, 10.05] | |
| Sutton 2020 | 0.8 [0.6, 1.3] | 1.02 [0.98, 1.06] | 0.87 [0.60, 1.28] | |
| Diagnostic threshold: sBP 140mmHg or dBP 90mmHg | ||||
| Pooled LR | Normal + Elevated BP +Stage 1 HTN (<140/90 mmHg) | 1.4 [1.0, 1.9] I2=0%, (0.8, 2.3) | 0.97 [0.91, 1.00] | 1.41 [1.04, 1.85] |
| Greenberg | 1.6 [1.0, 2.5] | 0.96 [0.91, 1.01] | 1.55 [1.00, 2.39] | |
| Sutton 2020 | 1.1 [0.7, 1.9] | 0.99 [0.96, 1.02] | 1.17 [0.73, 1.87] | |
| Qureshi | 1.9 [0.6, 5.7] | 0.98 [0.95, 1.02] | 2.65 [0.53, 13.18] | |
| Sevene | N/A | 0.86 [0.35, 2.07] | 2.00 [0.06, 68.48] | |
| McLaren | 6.4 [0.4, 100.1] | 0.58 [0.19, 1.79] | 3.75 [1.16, 12.13] | |
| Sabol | 1.1 [0.3, 2.8] | 0.98 [0.87, 1.09] | 1.19 [0.54, 2.62] | |
ACC (American College of Cardiology), AHA (American Heart Association), BP (blood pressure), dBP (diastolic BP), -LR (negative likelihood ratio), +LR (positive likelihood ratio), sBP (systolic BP) CI (confidence interval), PI (prediction interval)
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S26.
Sensitivity and Specificity of ACC/AHA BP categories for placental abruption
| COMPARATOR | |||
|---|---|---|---|
| BP measured at <20 weeks | Ref | Sensitivity | Specificity |
| ‘ELEVATED BP’ (as a new cut-off) | |||
| Pooled | Normal (<120/80 mmHg) | 0.25 [0.17, 0.34] | 0.77 [0.69, 0.83] |
| Greenberg | 0.30 [0.24, 0.37] | 0.72 [0.71, 0.72] | |
| Qureshi | 0.16 [0.10, 0.26] | 0.84 [0.80, 0.87] | |
| Sevene | 0.25 [0.03, 0.80] | 0.62 [0.22, 0.91] | |
| Sutton 2020 | 0.27 [0.22, 0.33] | 0.75 [0.74, 0.76] | |
| ‘STAGE 1 HYPERTENSION’ (as a new cut-off) | |||
| Pooled | Normal + Elevated BP (<130/80mmHg) | 0.24 [0.15, 0.36] | 0.79 [0.68, 0.86] |
| Duffy | 0.25 [0.24, 0.26] | 0.84 [0.84, 0.84] | |
| Greenberg | 0.18 [0.13, 0.24] | 0.86 [0.85, 0.86] | |
| Huai | 0.35 [0.23, 0.51] | 0.66 [0.60, 0.70] | |
| McLaren | 0.50 [0.13, 0.87] | 0.50 [0.44, 0.56] | |
| Qureshi | 0.12 [0.07, 0.20] | 0.91 [0.87, 0.93] | |
| Sabol | 0.26 [0.24, 0.28] | 0.77 [0.76, 0.77] | |
| Sevene | 0.25 [0.03, 0.80] | 0.62 [0.22, 0.91] | |
| Sutton 2020 | 0.10 [0.07, 0.14] | 0.89 [0.89, 0.89] | |
| ‘STAGE 2 HYPERTENSION’ (existing cut-off) | |||
| Pooled | Normal + Elevated BP +Stage 1 HTN (<140/90mmHg) | 0.10 [0.05, 0.19] | 0.93 [0.86, 0.96] |
| Greenberg | 0.11 [0.07, 0.16] | 0.93 [0.93, 0.94] | |
| McLaren | 0.36 [0.22, 0.53] | 0.93 [0.93, 0.94] | |
| Qureshi | 0.30 [0.01, 0.09] | 0.99 [0.97, 1.00] | |
| Sabol | 0.12 [0.06, 0.25] | 0.90 [0.88, 0.91] | |
| Sevene | 0.25 [0.03, 0.80] | 0.88 [0.40, 0.99] | |
| Sutton 2020 | 0.06 [0.04, 0.10] | 0.94 [0.94, 0.95] | |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S27.
Pooled relative risk and mean likelihood ratios for Cesarean, according to BP cut-offs at <20 weeks, determined by ACC/AHA BP categories
| COMPARATOR | ||||
|---|---|---|---|---|
| BP measured at <20 weeks | Ref | RR [95% CI] I2, (95% PI) | -LR | +LR |
| Diagnostic threshold: sBP 120mmHg (with dBP <80mmHg) | ||||
| Pooled | Normal (<120/80 mmHg) | 1.3 [1.2, 1.4] I2=0%, (1.0, 1.6) | 0.96 [0.93, 0.98] | 1.28 [1.13, 1.45] |
| Bellad | 1.3 [1.2, 1.5] | 0.98 [0.97, 0.99] | 1.44 [1.21, 1.71] | |
| Qureshi | 1.2 [1.1, 1.4] | 0.96 [0.94, 0.99] | 1.23 [1.08, 1.40] | |
| Rosner | 1.3 [0.9, 1.8] | 0.88 [0.75, 1.04] | 1.29 [0.95, 1.76] | |
| Sevene | 0.9 [0.3, 2.6] | 1.01 [0.90, 1.13] | 0.94 [0.37, 2.43] | |
| Diagnostic threshold: sBP 130mmHg or dBP 80mmHg | ||||
| Pooled | Normal + ElevatedBP (<130/80 mmHg) | 1.3 [1.1, 1.6] I2=99%, (1.0, 1.9) | 0.94 [0.90, 0.97] | 1.46 [1.26, 1.69] |
| Bellad | 1.5 [1.3, 1.8] | 0.98 [0.97, 0.99] | 1.66 [1.32, 2.08] | |
| Bello | 1.5 [1.5, 1.5] | 0.90 [0.89, 0.90] | 1.64 [1.60, 1.68] | |
| Darwin | 1.4 [1.3, 1.6] | 0.89 [0.85, 0.93] | 1.52 [1.32, 1.75] | |
| Duffy | 1.1 [1.1, 1.1] | 0.97 [0.96, 0.97] | 1.12 [1.10, 1.13] | |
| Qureshi | 1.2 [1.1, 1.4] | 0.98 [0.96, 0.99] | 1.26 [1.06, 1.49] | |
| Sabol | 1.4 [1.3, 1.6] | 0.88 [0.84, 0.92] | 1.57 [1.37, 1.80] | |
| Sevene | 0.2 [0.0, 3.5] | 1.05 [1.01, 1.09] | 0.22 [0.01, 3.43] | |
| Diagnostic threshold: sBP 140mmHg or dBP 90mmHg | ||||
| Pooled | Normal + Elevated BP +Stage 1 HTN (<140/90 mmHg) | 1.7 [1.6, 1.8] I2=27%, (1.5, 1.9) | 0.96 [0.93, 0.98] | 2.31 [2.06, 2.55] |
| Bellad | 2.1 [1.6, 2.8] | 0.99 [0.99, 1.00] | 2.89 [1.76, 4.74] | |
| Bello | 1.7 [1.7, 1.8] | 0.95 [0.95, 0.96] | 2.30 [2.18, 2.41] | |
| Darwin | 1.6 [1.4, 1.8] | 0.91 [0.88, 0.94] | 1.84 [1.51, 2.24] | |
| Qureshi | 1.5 [1.1, 2.1] | 0.99 [0.99, 1.00] | 1.77 [1.11, 2.81] | |
| Rosner | 1.1 [0.6, 2.1] | 0.99 [0.93, 1.05] | 1.22 [0.52, 2.86] | |
| Sabol | 1.6 [1.4, 1.8] | 0.91 [0.89, 0.94] | 2.07 [1.68, 2.55] | |
| Sevene | 0.8 [0.0, 11.9] | 1.00 [0.97, 1.04] | 0.74 [0.04, 12.12] | |
ACC (American College of Cardiology), AHA (American Heart Association), BP (blood pressure), dBP (diastolic BP), -LR (negative likelihood ratio), +LR (positive likelihood ratio), sBP (systolic BP), CI (confidence interval), PI (prediction interval)
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
Table S28.
Sensitivity and Specificity of ACC/AHA BP categories for caesarean
| COMPARATOR | |||
|---|---|---|---|
| BP measured at <20 weeks | Ref | Sensitivity | Specificity |
| ‘ELEVATED BP’ (as a new cut-off) | |||
| Pooled | Normal (<120/80mmHg) | 0.16 [0.08, 0.30] | 0.87 [0.75, 0.94] |
| Bellad | 0.07 [0.06, 0.08] | 0.95 [0.95, 0.95] | |
| Qureshi | 0.18 [0.16, 0.20] | 0.86 [0.85, 0.87] | |
| Rosner | 0.37 [0.28, 0.46] | 0.72 [0.66, 0.77] | |
| Sevene | 0.11 [0.04, 0.25] | 0.89 [0.86, 0.91] | |
| ‘STAGE 1 HYPERTENSION’ (as a new cut-off) | |||
| Pooled | Normal + ElevatedBP (<130/80mmHg) | 0.16 [0.09, 0.26] | 0.89 [0.82, 0.94] |
| Bellad | 0.04 [0.04, 0.05] | 0.97 [0.97, 0.98] | |
| Bello | 0.23 [0.22, 0.23] | 0.86 [0.86, 0.86] | |
| Darwin | 0.26 [0.24, 0.29] | 0.83 [0.81, 0.84] | |
| Duffy | 0.25 [0.25, 0.26] | 0.77 [0.77, 0.78] | |
| Qureshi | 0.11 [0.09, 0.12] | 0.92 [0.91, 0.92] | |
| Sabol | 0.27 [0.25, 0.30] | 0.83 [0.81, 0.84] | |
| Sevene | 0.01 [0.00, 0.11] | 0.94 [0.92, 0.95] | |
| ‘STAGE 2 HYPERTENSION’ (existing cut-off) | |||
| Pooled | Normal + Elevated BP +Stage 1 HTN (<140/90mmHg) | 0.06 [0.03, 0.13] | 0.97 [0.94, 0.99] |
| Bellad | 0.01 [0.01, 0.02] | 1.00 [0.99, 1.00] | |
| Bello | 0.08 [0.08, 0.09] | 0.96 [0.96, 0.97] | |
| Darwin | 0.17 [0.15, 0.20] | 0.91 [0.89, 0.92] | |
| Qureshi | 0.08 [0.01, 0.48] | 0.99 [0.99, 0.99] | |
| Rosner | 0.07 [0.03, 0.13] | 0.95 [0.91, 0.97] | |
| Sabol | 0.16 [0.14, 0.18] | 0.92 [0.91, 0.93] | |
| Sevene | 0.01 [0.00, 0.11] | 0.98 [0.97, 0.99] | |
Slade. The diagnostic accuracy of American College of Cardiology-American Heart Association blood pressure categories for identification of women and babies at risk. Am J Obstet Gynecol 2023.
References
- 1.Magee L.A., Nathan H.L., Shennan A.H., et al. Pregnancy outcomes and blood pressure visit-to-visit variability in three less-developed countries. BJOG. 2021;128(Suppl 2):171–172. [Google Scholar]
- 2.Davey D.A., MacGillivray I. The classification and definition of the hypertensive disorders of pregnancy. Am J Obstet Gynecol. 1988;158:892–898. doi: 10.1016/0002-9378(88)90090-7. [DOI] [PubMed] [Google Scholar]
- 3.Stone P., Cook D., Hutton J., Purdie G., Murray H., Harcourt L. Measurements of blood pressure, oedema and proteinuria in a pregnant population of New Zealand. Aust N Z J Obstet Gynaecol. 1995;35:32–37. doi: 10.1111/j.1479-828x.1995.tb01826.x. [DOI] [PubMed] [Google Scholar]
- 4.von Dadelszen P., Payne B., Li J., et al. Prediction of adverse maternal outcomes in pre-eclampsia: development and validation of the fullPIERS model. Lancet. 2011;377:219–227. doi: 10.1016/S0140-6736(10)61351-7. [DOI] [PubMed] [Google Scholar]
- 5.Magee L.A., Brown M.A., Hall D.R., et al. The 2021 International Society for the Study of Hypertension in Pregnancy classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2022;27:148–169. doi: 10.1016/j.preghy.2021.09.008. [DOI] [PubMed] [Google Scholar]
- 6.Whelton P.K., Carey R.M., Aronow W.S., et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. Hypertension. 2018;71:e13–e115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 7.Scott G., Gillon T.E., Pels A., von Dadelszen P., Magee L.A. Guidelines-similarities and dissimilarities: a systematic review of international clinical practice guidelines for pregnancy hypertension. Am J Obstet Gynecol. 2022;226:S1222–S1236. doi: 10.1016/j.ajog.2020.08.018. [DOI] [PubMed] [Google Scholar]
- 8.Darwin K.C., Federspiel J.J., Schuh B.L., Baschat A.A., Vaught A.J. ACC-AHA Diagnostic Criteria for Hypertension in Pregnancy identifies patients at intermediate risk of adverse outcomes. Am J Perinatol. 2021;38:e249–e255. doi: 10.1055/s-0040-1709465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenberg V.R., Silasi M., Lundsberg L.S., et al. Perinatal outcomes in women with elevated blood pressure and stage 1 hypertension. Am J Obstet Gynecol. 2021;224:521.e1–521.e11. doi: 10.1016/j.ajog.2020.10.049. [DOI] [PubMed] [Google Scholar]
- 10.Hauspurg A., Sutton E.F., Catov J.M., Caritis S.N. Aspirin effect on adverse pregnancy outcomes associated with stage 1 hypertension in a high-risk cohort. Hypertension. 2018;72:202–207. doi: 10.1161/HYPERTENSIONAHA.118.11196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hu J., Li Y., Zhang B., et al. Impact of the 2017 ACC/AHA guideline for high blood pressure on evaluating gestational hypertension-associated risks for newborns and mothers. Circ Res. 2019;125:184–194. doi: 10.1161/CIRCRESAHA.119.314682. [DOI] [PubMed] [Google Scholar]
- 12.Liu J., Tao L., Cao Y., et al. Stage 1 hypertension defined by the 2017 American College of Cardiology/American Heart Association guideline and risk of adverse birth outcomes in Eastern China. J Hypertens. 2020;38:1090–1102. doi: 10.1097/HJH.0000000000002380. [DOI] [PubMed] [Google Scholar]
- 13.Reddy M., Rolnik D.L., Harris K., et al. Challenging the definition of hypertension in pregnancy: a retrospective cohort study Am J Obstet Gynecol. 2020;222:606.e1–606.e21. doi: 10.1016/j.ajog.2019.12.272. [DOI] [PubMed] [Google Scholar]
- 14.Sabol B.A., Porcelli B., Diveley E., et al. Defining the risk profile of women with stage 1 hypertension: a time to event analysis. Am J Obstet Gynecol MFM. 2021;3:100376. doi: 10.1016/j.ajogmf.2021.100376. [DOI] [PubMed] [Google Scholar]
- 15.Brown M.A., Magee L.A., Kenny L.C., et al. The hypertensive disorders of pregnancy: ISSHP classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2018;13:291–310. doi: 10.1016/j.preghy.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 16.University of Bristol. Quadas-2 [Internet]. 2 | Bristol Medical School: Population Health Sciences | University of Bristol. University of Bristol; 2014. Available at: https://wwwbristolacuk/population-health-sciences/projects/quadas/quadas-2/ Accessed Feb 21 2021.
- 17.Whiting P.F., Rutjes A.W., Westwood M.E., et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 18.Greenland S., Robins J.M. Estimation of a common effect parameter from sparse follow-up data. Biometrics. 1985;41:55–68. [PubMed] [Google Scholar]
- 19.Higgins J.P., Altman D.G., Gøtzsche P.C., et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343 doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zwinderman A.H., Bossuyt P.M. We should not pool diagnostic likelihood ratios in systematic reviews. Stat Med. 2008;27:687–697. doi: 10.1002/sim.2992. [DOI] [PubMed] [Google Scholar]
- 21.Reitsma J.B., Glas A.S., Rutjes A.W., Scholten R.J., Bossuyt P.M., Zwinderman A.H. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005;58:982–990. doi: 10.1016/j.jclinepi.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 22.Harbord R.M., Deeks J.J., Egger M., Whiting P., Sterne J.A. A unification of models for meta-analysis of diagnostic accuracy studies. Biostatistics. 2007;8:239–251. doi: 10.1093/biostatistics/kxl004. [DOI] [PubMed] [Google Scholar]
- 23.Jaeschke R., Guyatt G.H., Sackett D.L. Users’ guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? Jama, Sierra Leone: The Evidence-Based Medicine Working Group. 1994;271(9):703–707. doi: 10.1001/jama.271.9.703. [DOI] [PubMed] [Google Scholar]
- 24.Duval S., Tweedie R.R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 25.Balduzzi S., Rücker G., Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22:153–160. doi: 10.1136/ebmental-2019-300117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Doebler P, Holling H. Meta-analysis of diagnostic accuracy with mada. 2020. Available at: https://cran.r-project.org/web/packages/mada/vignettes/mada.pdf. Accessed May 12, 2021.
- 27.mada DP. Meta-analysis of diagnostic accuracy. R package version 0.5.10. 2020. Available at: https://CRANR-projectorg/package=mada. Accessed May 12, 2021.
- 28.Rosner J.Y., Gutierrez M., Dziadosz M., et al. Prehypertension in early pregnancy: what is the significance? Am J Perinatol. 2017;34:117–122. doi: 10.1055/s-0036-1584542. [DOI] [PubMed] [Google Scholar]
- 29.Bellad M.B., Goudar S.S., Mallapur A.A., et al. Community level interventions for pre-eclampsia (CLIP) in India: a cluster randomised controlled trial. Pregnancy Hypertens. 2020;21:166–175. doi: 10.1016/j.preghy.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bello N.A., Zhou H., Cheetham T.C., et al. Prevalence of hypertension among pregnant women when using the 2017 American College of Cardiology/American Heart Association blood pressure guidelines and association with maternal and fetal outcomes. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.3808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duffy J.Y., Getahun D., Chen Q., Fong A. Pregnancy outcomes associated with a single elevated blood pressure before 20 weeks of gestation. Obstet Gynecol. 2021;138:42–50. doi: 10.1097/AOG.0000000000004422. [DOI] [PubMed] [Google Scholar]
- 32.González-Valencia D.P., Valero-Rubio S.Y., Fernando Grillo-Ardila C. Prehypertension as a risk factor for the development of perinatal complications: retrospective cohort study. Pregnancy Hypertens. 2020;21:203–207. doi: 10.1016/j.preghy.2020.04.016. [DOI] [PubMed] [Google Scholar]
- 33.Hauspurg A., Parry S., Mercer B.M., et al. Blood pressure trajectory and category and risk of hypertensive disorders of pregnancy in nulliparous women. Am J Obstet Gynecol. 2019;221:277.e1–277.e8. doi: 10.1016/j.ajog.2019.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang X., Chen D., He B., Cheng W. NRP1 and MMP9 are dual targets of RNA-binding protein QKI5 to alter VEGF-R/ NRP1 signalling in trophoblasts in preeclampsia. J Cell Mol Med. 2021;25:5655–5670. doi: 10.1111/jcmm.16580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huai J., Lin L., Juan J., et al. Preventive effect of aspirin on preeclampsia in high-risk pregnant women with stage 1 hypertension. J Clin Hypertens (Greenwich) 2021;23:1060–1067. doi: 10.1111/jch.14149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li Q., Zheng L., Gu Y., et al. Early pregnancy stage 1 hypertension and high mean arterial pressure increased risk of adverse pregnancy outcomes in Shanghai, China. J Hum Hypertens. 2022;36:917–924. doi: 10.1038/s41371-021-00523-6. [DOI] [PubMed] [Google Scholar]
- 37.McLaren R.A., Atallah F., Persad V.V.D., et al. Pregnancy outcomes among women with American College of Cardiology- American Heart Association defined hypertension. J Matern Fetal Neonatal Med. 2021;34:4097–4102. doi: 10.1080/14767058.2019.1704250. [DOI] [PubMed] [Google Scholar]
- 38.Nagao T., Saito K., Yamanaka M. Prehypertension in early pregnancy is a risk factor for hypertensive disorders during pregnancy: a historical cohort study in Japan. Hypertens Pregnancy. 2021;40:51–55. doi: 10.1080/10641955.2020.1864637. [DOI] [PubMed] [Google Scholar]
- 39.Qureshi R.N., Sheikh S., Hoodbhoy Z., et al. Community-level interventions for pre-eclampsia (CLIP) in Pakistan: a cluster randomised controlled trial. Pregnancy Hypertens. 2020;22:109–118. doi: 10.1016/j.preghy.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rosner J.Y., Gutierrez M., Dziadosz M., et al. Prehypertension in early versus late pregnancy. J Matern Fetal Neonatal Med. 2019;32:188–192. doi: 10.1080/14767058.2017.1374363. [DOI] [PubMed] [Google Scholar]
- 41.Sevene E., Sharma S., Munguambe K., et al. Community-level interventions for pre-eclampsia (CLIP) in Mozambique: a cluster randomised controlled trial. Pregnancy Hypertens. 2020;21:96–105. doi: 10.1016/j.preghy.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sutton E.F., Hauspurg A., Caritis S.N., Powers R.W., Catov J.M. Maternal outcomes associated with lower range stage 1 hypertension. Obstet Gynecol. 2018;132:843–849. doi: 10.1097/AOG.0000000000002870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sutton E.F., Rogan S.C., Lopa S., Sharbaugh D., Muldoon M.F., Catov J.M. Early pregnancy blood pressure elevations and risk for maternal and neonatal morbidity. Obstet Gynecol. 2020;136:129–139. doi: 10.1097/AOG.0000000000003885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wu D.D., Gao L., Huang O., et al. Increased adverse pregnancy outcomes associated with stage 1 hypertension in a low-risk cohort: evidence from 47 874 cases. Hypertension. 2020;75:772–780. doi: 10.1161/HYPERTENSIONAHA.119.14252. [DOI] [PubMed] [Google Scholar]
- 45.Yang S.W., Cho S.H., Kang Y.S., et al. Usefulness of uterine artery Doppler velocimetry as a predictor for hypertensive disorders in pregnancy in women with prehypertension before 20 weeks gestation. PLoS One. 2019;14 doi: 10.1371/journal.pone.0210566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.He D., Wu S., Zhao H., Zheng Z., Zhang W. High normal blood pressure in early pregnancy also contribute to early onset preeclampsia and severe preeclampsia. Clin Exp Hypertens. 2018;40:539–546. doi: 10.1080/10641963.2017.1407330. [DOI] [PubMed] [Google Scholar]
- 47.Bello N.A., Zhou H., Cheetham T.C., et al. Prevalence of hypertension among pregnant women when using the 2017 American College of Cardiology/American Heart Association blood pressure guidelines and association with maternal and fetal outcomes. Obstet Gynecol Surv. 2021;76:462–464. doi: 10.1001/jamanetworkopen.2021.3808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bramham K., Parnell B., Nelson-Piercy C., Seed P.T., Poston L., Chappell L.C. Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis. BMJ. 2014;348 doi: 10.1136/bmj.g2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Al Khalaf S.Y., O’Reilly É.J., Barrett P.M., et al. Impact of chronic hypertension and antihypertensive treatment on adverse perinatal outcomes: systematic review and meta-analysis. J Am Heart Assoc. 2021;10 doi: 10.1161/JAHA.120.018494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gestational hypertension and preeclampsia ACOG Practice Bulletin, Number 222. Obstet Gynecol. 2020;135:e237–e260. doi: 10.1097/AOG.0000000000003891. [DOI] [PubMed] [Google Scholar]
- 51.Antwi E., Amoakoh-Coleman M., Vieira D.L., et al. Systematic review of prediction models for gestational hypertension and preeclampsia. PLoS One. 2020;15 doi: 10.1371/journal.pone.0230955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wright D., Wright A., Nicolaides K.H. The competing risk approach for prediction of preeclampsia. Am J Obstet Gynecol. 2020;223:12–23.e7. doi: 10.1016/j.ajog.2019.11.1247. [DOI] [PubMed] [Google Scholar]
- 53.Magee L.A., von Dadelszen P., Singer J., et al. The CHIPS randomized controlled trial (control of hypertension in pregnancy study): is severe hypertension just an elevated blood pressure? Hypertension. 2016;68:1153–1159. doi: 10.1161/HYPERTENSIONAHA.116.07862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tita A.T., Szychowski J.M., Boggess K., et al. Treatment for mild chronic hypertension during pregnancy. N Engl J Med. 2022;386:1781–1792. doi: 10.1056/NEJMoa2201295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brown M.A., Magee L.A., Kenny L.C., et al. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension. 2018;72:24–43. doi: 10.1161/HYPERTENSIONAHA.117.10803. [DOI] [PubMed] [Google Scholar]
- 56.American College of Obstetricians and Gynecologists' Committee on Practice Bulletins—Obstetrics ACOG Practice Bulletin No. 203: chronic hypertension in pregnancy. Obstet Gynecol. 2019;133:e26–e50. doi: 10.1097/AOG.0000000000003020. [DOI] [PubMed] [Google Scholar]
- 57.National Collaborating Centre for Women’s and Children’s Health (UK). Hypertension in Pregnancy: The Management of Hypertensive Disorders During Pregnancy. London: RCOG Press; 2010. [PubMed]
- 58.Cluver C., Tong S. Revisiting blood pressure thresholds to define hypertension during pregnancy: is 140/90 mmHg too high? Lancet Glob Health. 2021;9:e1041–e1042. doi: 10.1016/S2214-109X(21)00285-0. [DOI] [PubMed] [Google Scholar]
- 59.Tan M.Y., Syngelaki A., Poon L.C., et al. Screening for pre-eclampsia by maternal factors and biomarkers at 11-13 weeks’ gestation. Ultrasound Obstet Gynecol. 2018;52:186–195. doi: 10.1002/uog.19112. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.