Abstract
Use of nanoparticles have established benefits in a wide range of applications, however, the effects of exposure to nanoparticles on health and the environmental risks associated with the production and use of nanoparticles are less well-established. The present study addresses this gap in knowledge by examining, through a scoping review of the current literature, the effects of nanoparticles on human health and the environment. We searched relevant databases including Medline, Web of Science, ScienceDirect, Scopus, CINAHL, Embase, and SAGE journals, as well as Google, Google Scholar, and grey literature from June 2021 to July 2021. After removing duplicate articles, the title and abstracts of 1495 articles were first screened followed by the full-texts of 249 studies, and this resulted in the inclusion of 117 studies in the presented review.
In this contribution we conclude that while nanoparticles offer distinct benefits in a range of applications, they pose significant threats to humans and the environment. Using several biological models and biomarkers, the included studies revealed the toxic effects of nanoparticles (mainly zinc oxide, silicon dioxide, titanium dioxide, silver, and carbon nanotubes) to include cell death, production of oxidative stress, DNA damage, apoptosis, and induction of inflammatory responses. Most of the included studies (65.81%) investigated inorganic-based nanoparticles. In terms of biomarkers, most studies (76.9%) used immortalised cell lines, whiles 18.8% used primary cells as the biomarker for assessing human health effect of nanoparticles. Biomarkers that were used for assessing environmental impact of nanoparticles included soil samples and soybean seeds, zebrafish larvae, fish, and Daphnia magna neonates.
From the studies included in this work the United States recorded the highest number of publications (n = 30, 25.64%), followed by China, India, and Saudi Arabia recording the same number of publications (n = 8 each), with 95.75% of the studies published from the year 2009. The majority of the included studies (93.16%) assessed impact of nanoparticles on human health, and 95.7% used experimental study design. This shows a clear gap exists in examining the impact of nanoparticles on the environment.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-023-15958-4.
Keywords: Biomarkers, Cytotoxicity; Environmental health, Genotoxicity, Human health, Impact, Nanoparticles, Scoping review, Toxicity
Highlights
• While nanoparticles are beneficial in a range of applications, they pose significant threats to humans and the environment.
• Immortalised cell lines are mostly used as biomarkers to assess human health effect of nanoparticles.
• Biomarkers such as soil samples and zebrafish larvae are used to investigate the environmental effect of nanoparticles.
• This work has revealed the toxic effects of nanoparticles to include production of oxidative stress, DNA damage, apoptosis, cell death, and induction of inflammatory responses.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-023-15958-4.
Introduction
Importance and meaning
Nanoparticles are small particles ranging from 1 to 100 nm (nm) in size [1]. They are used in a wide range of applications and can be grouped into four types: 1) inorganic-based nanoparticles, 2) carbon-based nanoparticles, 3) organic/polymer nanoparticles, and 4) composite-based nanoparticles [2]. Inorganic-based nanoparticles are made up of different metal and metal oxides. Examples of metal-based inorganic nanoparticles include aluminium, silver, gold, zinc, lead, iron, cadmium, and copper, whereas examples of metal oxide-based inorganic nanoparticles include aluminium oxide, copper oxide, iron oxide, silica, zinc oxide, titanium oxide, and magnesium aluminium oxide. Carbon-based nanoparticles include fullerene, graphene, multi- and single-walled carbon nanotubes, carbon black, and carbon fibres. Organic-based nanoparticles are derived from organic materials without carbon, for example, liposome, dendrimers, cyclodextrin, and micelle, whereas composite nanoparticles are made from combinations of metal oxide-based, metal-based, organic-based, and/or carbon-based nanoparticles.
In recent years, nanoparticles have gained increasing attention due to their use in consumer products, medicine, soil, and aquatic environments. For example, nanoparticles have been used for textiles [3], water treatment [4], environmental remediation [5–7], cancer therapy [8], radiology [9], and cosmetics [10]. This growing attention and extensive usage of nanoparticles is due to specific novel characteristics exhibited by such particles, which results from their small size and large surface area [11]. These unique qualities, while advantageous, pose certain risks to living organisms.
The harmful effects of nanoparticles
The small sizes of nanoparticles give them the ability to permeate physiological barriers of living organisms, causing harmful biological reactions. Nanoparticles are known to enter the human body through the lung, intestinal tract, or skin, and can be toxic to the brain, cause lung inflammation and cardiac problems [12]. In fact, certain nanoparticles have been found to cause permanent cell damage through organ injury and oxidative stress, due to their size and composition. In a study by Magrez et al. [13] to assess the toxic effect of carbon-based nanoparticles on lung cancer cells, the authors reported findings suggesting that carbon-based nanoparticles cause size-dependent cytotoxicity. The level of toxicity of nanoparticles is suggested to be dependent on factors such as composition of the nanoparticle, size, surface functionality, crystallinity, and aggregation [14]. Moreover, the toxicity of a nanoparticle in an individual is dependent on the genetic make-up of that individual, which is determined by the individual's ability to adapt and respond to toxic substances.
The gaps of previous studies
There are growing concerns regarding the toxicologic effects of nanoparticles, and frequent exposure to nanoparticles is regarded as a public health threat [15]. While there is extensive evidence about the benefits of nanoparticles, as well as the potential health and environmental risks associated with its production and use, current understanding of the impact of nanoparticles exposure to human health and the environment is limited. The current review seeks to explore, through a scoping review of the current literature, the effects of nanoparticles on human health and the environment. This review is unique as it adopts a systematic scoping approach to explore the current literature on the health risks posed by the manufacture, distribution, and use of nanoparticles. Published studies in this area have mainly used a narrative literature review approach [2, 16, 17].
Objective and research questions
The objective of this review is to map the distribution of the current literature on the human and environmental impacts of nanotoxicity. Specifically, this scoping review will be guided by the following research questions:
What is the relative distribution of the current literature on the human and environmental impact of nanotoxicity?
Which exposure pathways and nanoparticles have been researched and which have not?
What biomarkers have been used in assessing the human and environmental impact of exposure to nanoparticles?
Methods
This scoping review was conducted and reported in accordance with the Joanna Briggs Institute Reviewers Manual [18]. The following steps were followed:
Defining and aligning the objectives and research questions
Developing and aligning the inclusion criteria with the objectives and research questions
Describing the planned approach to evidence searching and selection
Searching for the evidence
Extracting the evidence
Charting the evidence
Summarising the evidence in relation to the objectives and research questions
The Preferred Reporting of Items for Systematic Reviews and Meta-Analysis (PRISMA) statement was used to summarise the screening process. The protocol of this review has been registered with the Open Science Framework [19].
Search strategy
The aim of the search strategy was to find both published and unpublished studies that have examined the effect of nanotoxicity on human health and the environment. Search terms consisted of a combination of key terms and concepts in the objective and research questions, using the Boolean operators, 'AND', and 'OR' as follows:
(nanomaterials OR nanoparticles OR nanostructures) AND (toxicity OR health) AND (“biomarker* of exposure” OR biomarker OR exposure) AND (human OR environment).
The search was limited to peer-reviewed articles published from the year 2000. This was to enable us to study the current literature (research conducted over the last 2 decades). The search was limited to primary studies published in the English language due to difficulties with language translation.
Table 1 below presents a list of the databases, grey literature, and search engines that were searched for eligible papers. The reference list of all included papers was also searched for additional papers on the subject matter.
Table 1.
Sources of literature
| Database sources | Grey Literature | Search Engines |
|---|---|---|
|
ScienceDirect Sage Journals Online Campbell Collaboration Cochrane collaboration Embase Medline CINAHL Web of Science Scopus |
OpenGrey NICE Evidence Search The Grey Literature Report Bielefeld Academic Search Engine (BASE) Australian Bureau of Statistics (ABS) |
Google Scholar |
For the database searches, a master search strategy was first developed using the Medline database, this was then modified for the other databases. The supplementary material file presents the Medline search history. The literature search was conducted between 1st June 2021 and 31st July 2021.
Reference management
All search results were imported into an Endnote library to help manage references and to remove duplicate articles. Once duplicates were removed, the search results were exported from Endnote into Covidence (a web-based software platform that streamlines the production of scoping/systematic reviews) for screening. The Covidence software was also useful in identifying and deduplicating articles that could not be identified by Endnote.
Selection criteria
The following criteria were used to identify eligible articles for inclusion in the review.
Inclusion criteria
Types of participants
Studies that have assessed the human and environmental impacts of nanotoxicity were considered for inclusion in this review. Human participants included children and/or adults of any age, gender, or ethnicity. Studies involving the use of animals as biomarkers for assessing the environmental impact of nanotoxicity were also considered for inclusion.
Concept
Studies that have examined the impacts of nanotoxicity as well as the biomarkers for assessing exposure to nanoparticles were eligible for inclusion in this review. While all types of nanoparticles were considered for inclusion, attention was given to studies involving metallic (oxides, pure metal) and carbonaceous (fullerenes, carbon nanotubes, and graphene) nanoparticles. This is mainly due to these particles being widely produced and used [20], therefore, they are considered the most relevant for public health.
Context
Studies from any geographical location aimed at assessing the human and/or environmental impact of nanotoxicity were considered eligible for inclusion. Studies whose full texts were in a language other than English were excluded because there were no available translators.
Study types
We included all original primary research (both quantitative and qualitative), including, but not limited to randomised controlled studies, quasi-experimental studies, surveys, retrospective and prospective cohort studies, case studies, and phenomenological studies.
Exclusion criteria
The following exclusion criteria were applied to the title and abstract, as well as the full-text review stage:
Irrelevant problem/focus: studies that have not examined the human and/or environmental impact of nanotoxicity, or the biomarkers for assessing exposure to nanoparticles
Irrelevant type of study: review reports or studies that did not contain any original research
Selection of studies
We employed a two-step screening process to assess search results for eligible studies. The first level involved screening of the titles and abstracts and was done independently by two reviewers (EK and RF). The next step was carried out independently by three reviewers (EK, RF, and SH) and involved screening of the full-texts of potentially eligible papers. Disagreements between reviewers were resolved through discussions and consensus. Where disagreements persisted, a third reviewer (TP or FVZ) was consulted.
Data charting
We developed a standardised data extraction form in the Covidence software for data extraction. The form was designed to collect the following information from included studies: year of publication, aim/objective of study, study design, country, type of nanoparticle, application of the nanoparticle, major exposure route(s), biomarker/model used, how biomarker was obtained, and study outcome(s).
The developed data extraction form was pilot-tested using 10% of the included articles before beginning the actual data extraction. Data extraction was done by one reviewer (PB, RF, or SH) and verified by another (EK, TP, or FVZ), using the Covidence software.
Data synthesis
The extracted data was first exported into Excel for editing and to check for accuracy. The edited data was then exported from Excel into SPSS (version 26) to aid with data synthesis. Descriptive statistics was used to report included studies by their characteristics and outcome measures, described below.
Characteristics of included studies
Year of publication: studies were grouped based on their year of publication. As stated earlier, this included studies published from the year 2000 to July 2021 (the date of completion of literature searches).
Country in which study was conducted: to assess the distribution of the current literature on human and environmental impact of nanotoxicity, the countries in which eligible studies were conducted were classified into six regions based on the World Bank’s classification of countries. This included: East Asia and Pacific, Europe and Central Asia, Latin America and Caribbean, Middle East and North Africa, North America, South Asia, and Sub-Saharan Africa (World Bank Group, 2018).
Study design: randomised controlled trial, non-randomised controlled trial, cohort study, experimental study, case control study, longitudinal study, uncontrolled before and after studies.
Impact/effect assessed: human health and/or environment
Outcome measures
Type of nanoparticle: This was divided into four groups: 1) inorganic-based nanoparticles, 2) carbon-based nanoparticles, 3) organic nanoparticles, and 4) composite-based nanoparticles two groups, metallic (oxides, pure metal) and carbonaceous (fullerenes and carbon nanotubes) particles.
Biomarker or model used in assessing human and/or environmental exposure: primary cell or immortalised cell line
Effect/impact on human health and/or the environment
A narrative synthesis was then used to further explore findings.
Results
Search results
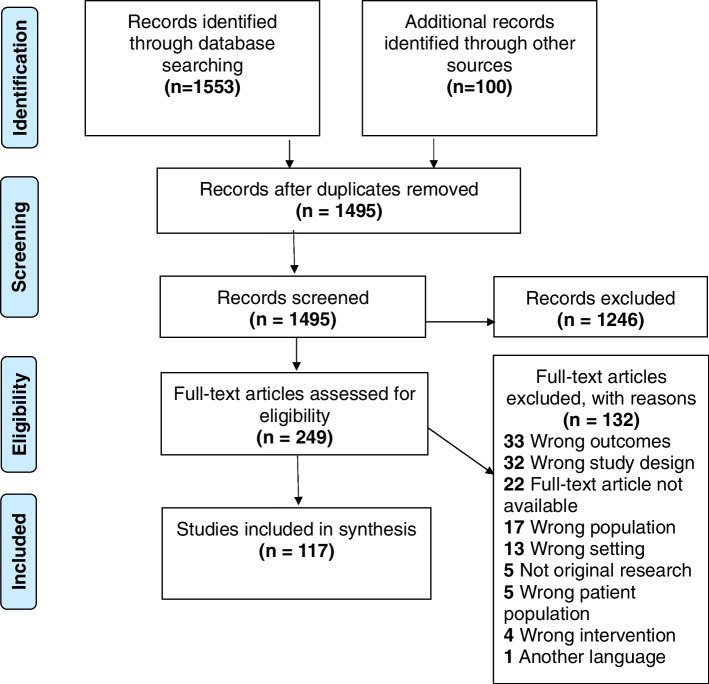
The database searches resulted in 1553 papers (presented in Fig. 1): Medline (n = 1,381); ScienceDirect (n = 0); Sage Journals Online (n = 50); Campbell Collaboration (n = 0); Cochrane Collaboration (n = 0); Embase (n = 5); Scopus (n = 6); Web of Science (n = 50); CINAHL (n = 61). Google and Google Scholar searches yielded 100 results, and no article was obtained from grey literature searches. Following removal of duplicate articles, the titles and abstracts of 1495 articles were screened to assess their eligibility for inclusion, which resulted in the exclusion of a total of 1246 articles as they did not meet the inclusion criteria. As such, the full texts of 249 articles were assessed for eligibility. Following this stage, a total of 132 articles were excluded for several reasons (see Fig. 1), whereas 117 studies qualified for inclusion in the review.
Fig. 1.
Study flow diagram (adapted from Moher et al., 2009)
Characteristics of included studies
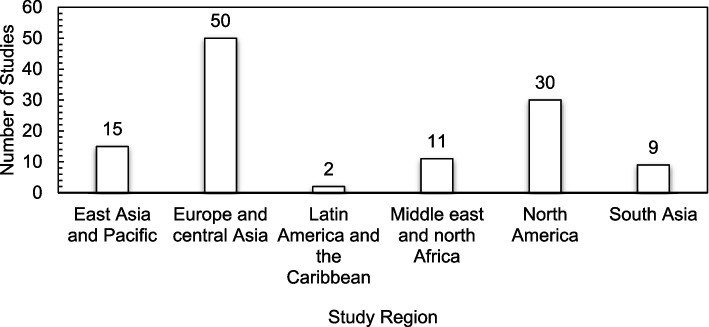
The studies included in this review originated from 23 countries across several continents, with the majority of the studies originating from Europe and Central Asia (n = 50). Nevertheless, the United Sates recorded the highest number of publications (n = 30), followed by China, India, and Saudi Arabia recording the same number of publications (n = 8). The lowest number of studies (n = 1 each) originated from Argentina, Czech Republic, Egypt, Mexico, Pakistan, Poland, and Russia. There were no studies recorded from Sub-Saharan Africa. Figure 2 presents a classification of the included studies by region.
Fig. 2.
Classification of Studies by Region
Included studies were published between the year 2006 and 2021, with a high proportion of the articles (95.75%) published from the year 2009. However, the year 2020 recorded the highest number of publications (n = 15; 12.82%), followed by 2016 (n = 14; 11.97%). Table 2 below presents the number of publications per year.
Table 2.
Number of publications per year (n = 117)
| Year | Number | Percent |
|---|---|---|
| 2006 | 1 | 0.85 |
| 2007 | 1 | 0.85 |
| 2008 | 3 | 2.56 |
| 2009 | 10 | 8.55 |
| 2010 | 5 | 4.27 |
| 2011 | 6 | 5.13 |
| 2012 | 11 | 9.40 |
| 2013 | 6 | 5.13 |
| 2014 | 10 | 8.55 |
| 2015 | 5 | 4.27 |
| 2016 | 14 | 11.97 |
| 2017 | 6 | 5.13 |
| 2018 | 9 | 7.69 |
| 2019 | 8 | 6.84 |
| 2020 | 15 | 12.82 |
| 2021 | 7 | 5.98 |
| Total | 117 | 100 |
The majority of the studies used an experimental study design (n = 112, 95.7%), with only 5 (4.3%) studies employing a cross-sectional design. Regarding the type of impact/effect of nanoparticle assessed, a vast majority of the studies assessed impact on human health (n = 109), 5 of the studies assessed effects on the environment, with only 3 studies assessing both human and environmental health impact (Fig. 3).
Fig. 3.
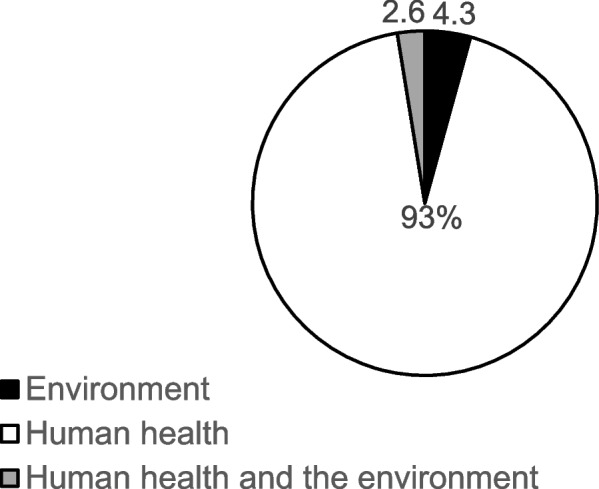
Effect/impact of nanoparticles on human/environmental health
Outcome measures
Just over 65% (n = 77) of the included studies investigated the human and/or environmental effect of inorganic-based nanoparticles. The inorganic-based nanoparticles that were investigated include, but not limited to, bismuth oxide (Bi2O3), silicon dioxide (SiO2), copper oxide (CuO), zinc oxide (ZnO), titanium dioxide (TiO2), silver (Ag), gold (Au), platinum (Pt), iron oxide (Fe2O3), cerium oxide (CeO2), cobalt oxide (Co3O4), aluminium oxide (Al2O3), molybdenum trioxide (MoO3), magnesium oxide (MgO), nickel oxide (NiO), chromium oxide (Cr2O3), tungsten oxide (WO3), yttrium oxide (Y2O3), and manganese oxide (Mn2O3).
Thirty-five (29.9%) studies reported on carbon-based nanoparticles (including single and multi-walled carbon nanotubes (SWCNTs/MWCNTs), graphene oxide (GO), and graphene nanoplatelets, GNP). Three studies [21–23] reported on both inorganic- and carbon-based nanoparticles; one study [24] reported on both inorganic-based and polymer nanoparticles (i.e., Titanium dioxide, terbium-doped gadolinium, and polylactic-co-glycolic acid, PLGA), whereas another study [25] investigated the effect of Poly lactic-co-glycolic acid (a polymer) nanoparticle on the environment.
The most investigated nanoparticles were ZnO (n = 25), followed by MWCNTs (n = 20), TiO2 (n = 16), CeO (n = 15), SWCNTs and Fe2O3 (n = 14), and SiO2 (n = 12). The least studied nanoparticles include Pt, Au, MgO, MoO3, WO3, Carbon Black (CB), and GNP with only one report available.
A significant number (n = 90, 76.9%) of the included studies used immortalised cell lines as the biomarker for assessing the human health effect of nanoparticles. Examples of the immortalised cell lines that were used include the human hepatocarcinoma cell line (HepG2), human (alveolar) epithelial A549 cell line with human monocyte-derived dendritic cells (MDDCs) and macrophages (MDMs), Melanoma cells and human foreskin fibroblasts, human airway epithelial (BEAS-2B) cells, human bronchial epithelium (BEAS-2B) cells, human neuroblastoma SHSY5Y cell line, human keratinocyte (HaCaT) cell line, and MCF-7 cell line, which is a human breast cancer cell line with oestrogen, progesterone and glucocorticoid receptors. Immortalised cell lines were mostly purchased/obtained from organisations such as the American Type Culture Collection (ATCC, Manassas, VA, USA).
Twenty-two studies used primary cells obtained from study participants/volunteers. Examples of the primary cells that were used as biomarkers by included studies are human bone marrow mesenchymal stem cells (hBMMSCs) taken from the iliac crest of human donors, human lymphocytes (blood), and human dermal fibroblasts which were isolated by the outgrowth method using infant foreskins obtained after circumcision. Workplace air samples have also been used to investigate workplace exposures to graphene nanoplatelets [26]. Five studies [25, 27–30] that reported on the environmental effect of nanoparticles used a variety of biomarkers, including soil samples and soybean seeds, Allium cepa bulbs, zebrafish larvae, seedlings of buckwheat, Nitrosomonas europaea KCTC 12270 bacterium (an ammonia-oxidizing bacterium) and Nitrospira moscoviensis (a nitrite-oxidizing bacterium), as well as aquatic species including Daphnia magna neonates, fish, and Carp (Cyprius carpio). The studies included in this review reported several toxicities associated with the production and application of nanoparticles. The most reported health impact of nanoparticles was found to be decreased cell viability and/or cell death (observed by twenty-nine studies). Twenty-eight studies also noted reactive oxygen species generation as a result of exposure to nanoparticles, especially to CNT (n = 7), ZnO (n = 7), SiO2 (n = 5), and TiO2 (n = 4). The third commonly observed health impact was dose-dependent oxidative stress in the biomarkers (n = 25), particularly, in cases of exposure to SiO2 (n = 5), ZnO (n = 5), Fe3O4 (n = 4), CeO2 (n = 3), and CuO (n = 3). In addition, there were sixteen reports regarding DNA damage after exposure to nanoparticles, mainly for ZnO (n = 4) and MWCNTs (n = 3). Table 3 presents a comprehensive outline of the effects (human health and the environment) reported by each of the included studies. These are further explored in the ensuing section.
Table 3.
Studies on effect (human health and environment) of various types of nanoparticles
| Reference | Type of nanoparticle | Biomarker/model used | Toxicity/harmful impacts of nanoparticle |
|---|---|---|---|
| Inorganic-based Nanoparticles | |||
| Ahamed et al. [31] | Bismuth oxide (Bi2O3) | MCF-7 cell line (a human breast cancer cell line with estrogen, progesterone, and glucocorticoid receptors) |
• Reduces cell viability • Induces membrane damage Dose-dependently • Oxidative stress • Reactive Oxygen Species generation |
| Eom & Choi [32] | Fumed and porous Silicon dioxide (SiO2) | Human bronchial epithelial cell (Beas-2) |
• Oxidative stress • Induction of heme oxygenase-1 (HO-1) |
| Bengalli et al. [33] | Copper (CuO) and Zinc oxide (ZnO) | Reconstructed human epidermis model and fibroblast monolayer | • Deeply affect the epidermal tissue and the underlying dermal cells upon trans-epidermal permeation |
| Ferraro et al. [34] | Titanium dioxide (TiO2) | Human neuroblastoma (SH-SY5Y) cell line |
• Reactive Oxygen Species generation • Apoptosis • Induction of endoplasmic (ER) stress • Neurotoxicity |
| Gambardella et al. [35] | Silicon dioxide (SiO2) | Sea urchin Paracentrotus lividus sperms |
• Reduced toxicity • Neurotoxic damage • Decrease of acetylcholinesterase (AChE) expression • No effect on fertilization capability • Induced of toxic effect on the offspring |
| Yusefi-Tanha et al. [30] | Zinc oxide (ZnO) | Soil samples and Soybean seeds |
• Oxidative stress • Significant particle size-, morphology-, and concentration-dependent influence on seed yield and lipid peroxidation |
| Oh et al. [36] | Citrate-coated silver (Ag) | Human embryonic stem cell (hESC) |
• Oxidative stress • Dysfunctional neurogenesis |
| Zhao et al. [37] | Silicon dioxide (SiO2) | Lung bronchial epithelial cells (BEAS-2B) |
• Disturbs global metabolism • Oxidative stress • Generation of reactive oxygen species • Significantly perturbs mitochondrial dysfunction-related GSH metabolism and pantothenate and coenzyme A (CoA) biosynthesis • Causes abnormality in mitochondrial structure and mitochondrial dysfunction |
| Ying et al. [38] | Superparamagnetic Iron oxide (SPIO) | A3 human T lymphocytes | • Causes concentration-dependent nanotoxicity |
| Jing et al. [39] | Copper oxide (CuO) | Lung adenocarcinoma cells (A549 cells) and human bronchial epithelial cells (HBEC) |
• Significantly reduced cell viability • Increased lactate dehydrogenase (LDH) release • Reactive Oxygen species and IL-8 generation |
| Lojk et al. [40] | Silicon dioxide (SiO2), Titanium dioxide (TiO2), Silver (Ag), Polyacrylic acid (PAA) coated cobalt ferrite (CoFe2O4) | Human neuroblastoma (SH-SY5Y) cell |
• Neurotoxicity • Reactive Oxygen species formation • Membrane damage • Autophagy dysfunction for TiO2 P25 NPs • Decrease of cell viability for TiO2 FG NPs |
| Tsai et al. [41] | Titanium dioxide (TiO2) and Cerium dioxide (CeO2) | BEAS-2B epithelial cell |
• TiO2 induces apoptosis and hypersecretion of mucus • CeO2 NPs reduce cytosolic Ca2+ changes and mitochondrial damage caused by TiO2 NPs |
| Sramkova et al. [42] | Titanium dioxide (TiO2), Silicon dioxide (SiO2), magnetite (Fe3O4) and gold (Au) | Human renal proximal tubule epithelial TH1 cell line |
• None of the NPs induced any DNA strand breaks and oxidative DNA lesions regardless of the exposure (static and dynamic conditions) • No cytotoxicity was observed, except for Fe3O4NPs |
| Bell et al. [43] | Silicon dioxide (SiO2) |
SH-SY5Y human neuroblastoma (ATCC CRL-2266) Human epithelial type-2 (HEp-2) cells (ATCC CCL-23) |
• Destabilizes mitochondrial membrane potential • stimulates reactive oxygen species production • Promotes cytotoxicity |
| Akhtar et al. [44] | Silicon dioxide (SiO2) | Human lung epithelial cells (A549 cells) |
• Lower concentration: o Induction of reactive oxygen species o Membrane damage • Higher concentration: o Reactive oxygen species generation o GSH depletion |
| Gaiser et al. [27] | Silver (Ag) and cerium oxide (CeO2) |
Aquatic species: Daphnia magna neonates, fish, Carp (Cyprius carpio) Human model: C3A human hepatocyte cell line and caco-2 human intestinal epithelial cells |
• Ag is more cytotoxic than CeO2 • Both particles when in diet have the potential to enter the body following ingestion |
| Dankers et al. [45] | CeO2, Mn2O3, CuO, ZnO, Co3O4, and WO3 | Lung epithelium and dendritic cells | • Metal oxide NPs elicit minimal proinflammatory effects |
| Chen et al. [46] | Zinc oxide (ZnO) | Human umbilical vein endothelial cells (HUVECs) |
• ZnO induces significant cellular ER stress • Higher doses of ZnO induces apoptosis |
| Patil et al. [47] | Titanium dioxide (TiO2) and zinc oxide (ZnO) | Lung fibroblast (MRC5) | • Impedes genomic DNA hypomethylation |
| Mohamed et al. [48] | Silicon dioxide (SiO2) | Human monocytic leukemia cell line THP-1 and human alveolar epithelial (A549) cell line |
• Low degree of cytotoxicity at all concentrations • Stress-related cellular response at high concentrations |
| Mancuso & Cao [14] | Copper oxide (CuO) | Human bone marrow mesenchymal stem cells (hBMMSCs) |
• Bigger sizes exhibit significant cytotoxicity at all concentrations • Micro-sized particles exhibit very low cytotoxicity at the same concentration |
| Alshatwi et al. [49] | Aluminium oxide (Al2O3) | Human mesenchymal stem cells (hMSCs) |
• Dose-dependent decreased cell viability • Decreased mitochondrial membrane potential with increasing concentrations after 24 exposures • Down-regulation in the expression of the antioxidant enzyme SOD • Did not induce apoptosis • Dose-dependent oxidative stress |
| Baber et al. [50] | Two amorphous silica coated (MagSilica 85, MagSilica 50) and uncoated iron oxide NPs (Fe3O4) | BEAS-2B (immortalized normal human bronchial epithelium) |
• Little to no indications of cytotoxicity • No induction of inflammatory response/oxidative stress |
| Corbalan et al. [51] | Amorphous Silicon dioxide (SiO2) | Blood |
• Induced an upregulation of selectin P expression and glycoprotein IIb/IIIa activation on the platelet surface membrane • Platelet aggregation |
| Branica et al. [52] | Zinc oxide (ZnO) | Blood (Human lymphocyte) | • Higher concentrations increase cytogenetic damage and intracellular Zn2+ levels in lymphocytes |
| Gurunathan et al. [53] | Platinum (Pt) | Human acute monocytic leukemia (THP-1) macrophages |
• Decreased cell viability and proliferation • Induces cell death • Oxidative stress • Mitochondrial dysfunction • Endoplasmic reticulum stress (ERS) • Proinflammatory responses |
| Hussain et al. [54] | Cerium dioxide (CeO2) | Human peripheral blood monocytes | • CeO2 NPs at non-cytotoxic concentrations neither modulate pre-existing inflammation nor prime for subsequent exposure to lipopolysaccharides in human monocytes from healthy subjects |
| Zerboni et al. [55] | Zinc oxide (ZnO) and Cupper oxide (CuO) | Human alveolar epithelial cells, A549 | • The presence of diesel exhaust particles (DEP) introduces new physicochemical interactions able to increase the cytotoxicity of ZnO and to reduce that of CuO NPs |
| Zielinska et al. [56] | Silver (Ag) | Human fetal osteoblast cells (hFOB 1.19) |
• Cell death • Reactive oxygen species production |
| Rajiv et al. [57] | Cobalt (II, III) oxide (Co3O4); Iron (III) oxide (Fe2O3), Silicon dioxide (SiO2), and Aluminium oxide (Al2O3) | Human lymphocytes |
• Co3O4 NPs showed a decrease in cellular viability and an increase in cell membrane damage followed by Fe2O3, SiO2, and Al2O3 NPs in a dose-dependent manner • Oxidative stress • Lipid peroxidation • Depletion of catalase • Reduced glutathione • Superoxide dismutase |
| Alarifi et al. [58] | Copper oxide (CuO) | Human skin epidermal cell line (HaCaT; passage no. 20) |
• Decrease in cell viability • Reduction in glutathione and induction in lipid peroxidation, catalase, and superoxide dismutase • Apoptosis • Necrosis • Induces DNA damage mediated by oxidative stress |
| Sun et al. [59] | Zinc oxide (ZnO), Fe2O3, Iron (II, III) oxide (Fe3O4), Magnesium oxide (MgO), Aluminium oxide (Al2O3), Copper (II) oxide (CuO) | Human cardiac microvascular endothelial cells (HCMECs) |
• Fe2O3, Fe3O4, and Al2O3 NPs did not have significant effects on cytotoxicity, permeability, and inflammation response • ZnO, CuO, and MgO NPs produced cytotoxicity at a concentration-dependent and time-dependent manner and elicited permeability and inflammation response in HCMECs |
| Tolliver et al. [60] | Titanium dioxide – (TiO2), Zinc oxide – (ZnO), Copper oxide – (CuO), Manganese oxide (Mn2O3), Iron oxide – (Fe2O3), Nickel oxide – (NiO), Chromium oxide – (Cr2O3) | Human lung cancer cell model (A549) |
• All NPs aside from Cr2O3 and Fe2O3 showed a time- and dose-dependent decrease in viability • All NPs significantly inhibited cellular proliferation • Apoptosis • Cell cycle alteration in the most toxic NPs |
| Rothen-Rutishauser et al. [61] | Cerium oxide (CeO2) | Adenocarcinomic human alveolar basal epithelial (A549) cell line |
• Generation of oxidative DNA damage • Causes tightness of the lung cell monolayer • Dose-dependent cellular response |
| Benameur et al. [62] | Cerium Oxide (CeO2) | Human dermal fibroblasts |
• Genotoxicity • Reactive oxygen species production • Lower doses of CeO2 did not induce significant cytotoxicity • Induces lipid peroxidation and decline of cellular glutathione level at concentrations above 0.00006 M |
| Gojova et al. [63] | Cerium oxide (CeO2) | Human aortic endothelial cells (HAECs) | • Causes very little inflammatory response even at higher doses |
| Lee et al. [29] | Zinc oxide (ZnO) |
Natural soil and seedlings of buckwheat |
• The effect of ZnO NPs on soil bacterial depends on the presence of plants • The soil–plant interactive system helps to decrease the toxic effects of ZnO nanoparticles on the rhizobacteria population relative to soil systems not containing plants |
| Hildebrand et al. [64] | Magnetite (Fe3O4) and palladium magnetite (Pd/Fe3O4) |
1) Human cell lines: Colon adenocarcinoma cells, CaCo-2 (HTB-37), Human keratinocyte cells, (HaCaT) 2) Fish cell line: Rainbow trout gills (RTgill-W1) cell line |
• No initiation of reactive oxygen species production • Little impact on the viability of colon adenocarcinoma cells, human keratinocyte cells, and the rainbow trout gills cell line • No toxic effect was found |
| Lai et al. [65] | Titanium dioxide (TiO2) | Human astrocytoma and human fibroblasts |
• Induces cell death • Apoptosis • Necrosis |
| Ahamed et al. [66] | Copper oxide (CuO) | Human lung epithelial cells (A 459) |
• Dose-dependent reduction in cell viability • Induces oxidative stress • Depletion of glutathione • Induction of lipid peroxidation, Catalase and superoxide dismutase • Induces cellular damage (indicated by the expression of Hsp70, the first tier biomarker of cellular damage) |
| Vergaro et al. [67] | Titanium dioxide (TiO2) | Human bronchial epithelial cells (BEAS-2B) | • Induces a low photo reactivity and a toxic effect lower than Aeroxide P25 of the nano-TiO2 powders |
| Dávila-Grana et al. [68] | Zinc oxide (ZnO), Titanium dioxide (TiO2), Cerium dioxide (CeO2), Aluminium oxide (Al2O3), Yttrium (III) oxide (Y2O3) | Jurkat cell line |
• The combination of nanoparticles induces changes in cell signalling mediated by the MAPKs and nuclear factor-κB (NF-κB) • Al2O3 NPs had a protective effect when combined with the ZnO NPs • CeO2 and Y2O3 Nps induced a synergistic effect on the toxicity and p38 activation • TiO2 nanoparticles increase the toxicity induced by ZnO nanoparticles but reduced the phosphorylation of the signalling proteins |
| Pierscionek et al. [69] | Cerium oxide (CeO2) | Human lens epithelial cells |
• Epithelial cells can sustain normal growth when exposed to lower concentrations of nanoceria • Induces genotoxicity when exposed for longer periods |
| Rafieepour et al. [70] | Magnetite iron oxide (Fe3O4), polymorphous silicon dioxide (P-SiO2) | Adenocarcinomic human alveolar basal epithelial (A549) cell line |
• Reduces cell viability • Reduces cellular glutathione content and mitochondrial membrane potential • Increases reactive oxygen species generation in both single and combined exposures of Fe3O4 and P-SiO2 • The toxic effects of combined exposure to these NPs were less than the single exposures |
| Ickrath et al. [71] | Zinc oxide (ZnO) | Human mesenchymal stem cells (hMSC) |
• Induces cytotoxic effect at higher concentrations of 50mcg/mL • Induces genotoxic effects in hMSC exposed to between 1 and 10mcg/mL ZnO-NP |
| Radeloff et al. [72] | Iron oxide (Fe3O4) | Human adipose tissue derived stromal cells (hASCs) | • No effect on the physiological functions of human adipose tissue derived stromal cell (hASCs) |
| Jin et al. [73] | Zinc oxide (ZnO) | Zebrafish larvae and human neuroblastoma cells SH-SY5Y |
• Smaller sizes of ZnO showed slightly higher toxicity than the larger sizes • Long ZnO NRs (l-ZnO NRs) harbours a remarkably potential risk for the onset and development of Parkinson’s disease at relatively high doses |
| Kumari et al. [74] | Cerium oxide (CeO2) | Human neuroblastoma cell line (IMR32) |
• Induces size- and dose-dependent toxicity (oxidative stress and genotoxicity) • CeO2 did not induce toxicity below 100 mg/mL concentration • IMR32 cells are less sensitive to CeO2 NPs |
| Fernández-Bertólez et al. [75] | Silica-coated iron oxide nanoparticles (SiO2) | Human glioblastoma A172 cells |
• Cytotoxicity (cell cycle disruption and cell death induction) • Rarely induces genotoxic effects • No alteration in the DNA repair process |
| Gliga et al. [76] | Nickel (Ni), nickel oxide (NiO) | Human bronchial epithelial cell line (BEAS-2B) |
• Long-term exposures (six weeks) changes gene expressions • Induces DNA strand breaks and alter cell cycle after six weeks of repeated exposure • Nickel causes no effect on cell transformation (ability to form colonies in soft agar) or cell motility |
| Kennedy et al. [77] | Iron oxide (Fe3O4), zinc oxide (ZnO), Yttrium oxide (Y2O3), and cerium oxide (CeO2) | Human aortic endothelial cells (HAECs) |
• Induces oxidative stress • Zinc oxide more toxic than yttrium oxide • No effect on HAECs when exposed to Iron oxide and cerium oxide |
| Schanen et al. [78] | Titanium dioxide and cerium dioxide (TiO2 and CeO2) | PBMC blood product | • Low dose exposures modulate human innate and adaptive immunity (i.e., dendritic cells activation and primary CD4 T helper cell differentiation state) |
| Seker et al. [79] | Zinc oxide (ZnO) | Human periodontal ligament fibroblast cells (hPDLFs) |
• Causes cell index decrease at concentrations of 50 to 100lg/mL • Induces changes in cell morphology • Induces harmful effects on cell viability and membrane integrity • Necrosis • Cell death (in terms of morphological change or cellular shrinkage) at doses higher than 50lg/mL • Cytotoxicity depends on duration of exposure and concentration |
| Könen-Adıgüzel & Ergenel [80] | Cerium dioxide (CeO2) | Human blood lymphocytes | • Induces genotoxicity even at 3–24 h exposure under in vitro conditions |
| Henson et al. [81] | Cupric (II) oxide (CuO), Polyvinylpyrrolidone (PVP) coated NPs | A three-dimensional model of the human small intestine, EpiIntestinalTM(SMI-100) | • Induces dose- and time-dependent viability of human cells |
| Gojova et al. [82] | Iron oxide (Fe2O3), Yttrium oxide (Y2O3), and Zinc oxide (ZnO) | Human aortic endothelial cells (HAECs) |
• All three types of nanoparticles are internalized into HAECs and are often found within intracellular vesicles • No inflammatory response after exposure to Fe2O3 • Y2O3 and ZnO nanoparticles elicit pronounced inflammatory response |
| Alarifi et al. [83] | Zinc Oxide (ZnO) | Human skin melanoma (A375) cells |
• Decrease in cell viability • Causes morphological changes • Induces oxidative stress • Reactive oxygen species generation • Depletion of the antioxidant, glutathione • Induces DNA damage at higher concentrations |
| Ãkerlund et al. [84] | Nickel (Ni) and nickel oxide (NiO) | Human bronchial epithelial cells (HBEC) | • Causes a release of inflammatory cytokines from exposed macrophages |
| Jiménez-Chávez et al. [85] | Titanium dioxide and Zinc oxide (TiO2 and ZnO) | Human alveolar epithelial cells (A549) |
TiO2: • Shows a higher persistence in cell surface and uptake • Induces sustained inflammatory response (by means of TNF-Î ± , IL-10, and IL-6 release) • Induces reactive oxygen species generation ZnO: • Shows a modest response and low number in cell surface Both TiO2 and ZnO: • Concentration-dependent reduction in SP-A levels at 24 h of exposure to both TiO2 and ZnO • Cellular damage • Loss of lung function |
| Hussain & Garantziotis [86] | Cerium dioxide (CeO2) | Primary human monocytes |
• Apoptosis (involving mitochondrial damage) • Causes a loss in membrane potential • Induces mitochondrial relocation of BAX • Induces modulation in autophagic events |
| Abudayyak et al. [87] | Bismuth Oxide—Bi (III) oxide (Bi2O3) |
a) HepG2 human hepatocarcinoma cells (ATCC HB-8065) b) Caco-2 human colorectal adenocarcinoma cells (ATCC HTB-37) c) A549 human lung carcinoma cells (ATCC CCL-185) |
• Induces apoptosis in HepG2 • Induces necrosis in A549 and Caco-2 cells • Causes significant changes in the levels of glutathione (GSH), malondialdehyde (MDA), and 8-hydroxydeoxyguanine (8-OHdG) in HepG2 and Caco-2 cells, except A549 cell |
| Fahmy et al. [88] | Copper/copper oxide (Cu/CuO) | Human diploid lung fibroblast normal cell lines (WI-38 cell) and human epithelial lung carcinoma cell lines (A549 cells) |
• Suppresses proliferation and cell viability • Cause DNA damage • Induces generation of reactive oxygen species • Induces oxidative stress |
| Božinović et al. [89] | Molybdenum trioxide (MoO3) | Human keratinocyte (HaCaT) cell line | • Short exposure (up to 1 h) of keratinocytes to MoO3 has no significant impact on cell survival |
| Ahamed et al. [90] | Iron oxide (Fe3O4) | Skin epithelial A431 and lung epithelial A549 cell lines |
• Induces dose-dependent cytotoxicity (indicated by reduction in cell viability lactate dehydrogenase leakage assays) • Induces dose-dependent oxidative stress • Induces reactive oxygen species • Induces lipid peroxidation • Causes DNA damage in high concentrations • Up-regulates the protein expression level of cleaved caspase-3 |
| Pelclova et al. [91] | Titanium dioxide (TiO2) | Exhaled breath condensate (EBC) and urine |
• Induces elevation of Leukotrienes (LT) levels • Induces inflammation and potential fibrotic changes in the lungs |
| Valdiglesias et al. [92] | Zinc oxide (ZnO) | Human neuroblastoma SHSY5Y cell line |
• Apoptosis • Decreases cell viability • Induces cell cycle alterations • Induces micronuclei production • Induces H2AX phosphorylation and DNA damage |
| Verdon et al. [93] | Silver (Ag), Zinc oxide (ZnO), Copper oxide (CuO), Titanium dioxide (TiO2) |
1) Human acute myeloid leukemia suspension cell line, HL-60 2) Primary neutrophils from human blood |
• Ag and CuO nanoparticles stimulate neutrophil activation • TiO2 do not induce neutrophil response in either cell type • ZnO induces activation of HL-60 cells but does not activate primary cells |
| Siddiqui et al. [94] | Nickel oxide (NiO) | Cultured human airway epithelial (HEp-2) and human breast cancer (MCF-7) cells |
• Apoptosis • Cytotoxicity • Reactive Oxygen species generation • Oxidative stress • generation and oxidative stress • Dietary antioxidant curcumin can effectively abrogate NiO NP-induced toxicity |
| Park et al. [95] | Cerium oxide (CeO2) | Human lung epithelial cells (BEAS-2B) |
• Causes cell death • Reactive oxygen species production • Glutathione (GSH) decrease • Induces oxidative stress-related genes (e.g., heme oxygenase-1, catalase, glutathioneS-transferase, and thioredoxin reductase) • Apoptosis |
| Fakhar-e-Alam et al. [96] | Zinc oxide (ZnO) | Melanoma cells and human foreskin fibroblasts |
• Induces reactive oxygen species production after UV-A-irradiation • Causes loss of mitochondrial membrane potential • Induces significant loss of cell viability |
| Hackenberg et al. [97] | zinc oxide (ZnO) | Human mucosa of the inferior nasal turbinate | • Repetitive exposure to low concentrations of ZnO-NPs results in persistent or ongoing DNA damage |
| Andujar et al. [98] | Welding-related NPs (essentially, Iron (Fe), Manganese (Mn), Chromium (Cr) oxide) | The lung of arc welders exposed to fume-issued NPs |
• Induce the production of a pro-inflammatory secretome • All, but magnetite NPs, induce an increased migration of macrophages • NP-exposed macrophage secretome has no effect on human primary lung fibroblasts differentiation |
| Sharma et al. [99] | Zinc oxide (ZnO) | Human hepatocarcinoma cell line (HepG2) |
• Decreases cell viability • Apoptosis • Induces DNA damage • Production of reactive oxygen species • Decreases mitochondria membrane potential • Activates JNK and p38 • Induces p53-Ser15 phosphorylation |
| Senapati et al. [100] | Zinc oxide (ZnO) | Human monocytic cell line, THP-1 |
• Induces oxidative and nitrosative stress • Causes an increase in inflammatory response (via activation of redox sensitive NF-kB and MAPK signalling pathways) |
| Carbon-based Nanoparticles | |||
| Vlaanderen et al. [101] | Multi-walled carbon nanotubes (MWCNTs) | Breathing zone measurement of inhalable particulate matter, whole blood samples, and assessment of lung function of workers |
• Significant upward trends for immune markers C–C motif ligand 20 (p = .005), basic fibroblast growth factor (p = .05), and soluble IL-1 receptor II (p = .0004) with increasing exposure to MWCNTs • Effect on lung health and immune system |
| Asghar et al. [102] | Carbon Nanotubes (CNT), Graphene Oxide (GO) | Human sperm |
• Both SWCNT-COOH and reduced GO Causes no effect to sperm viability at lower concentrations • SWCNT-COOH generates significant reactive superoxide species at a higher concentration • Reduced graphene oxide does not initiate reactive species in human sperm |
| Periasamy et al. [103] | Carbon nanoparticles (CNPs) | Human mesenchymal stem cells (hMSCs) | • Reduces cell viability |
| Beard et al. [104] | Carbon nanotubes and nanofibers (CNT/F) | Sputum and blood |
Inhalable rather than respirable CNT/F associated with: • Fibrosis • Inflammation • Oxidative stress • Cardiovascular biomarkers |
| Zhang et al. [105] | Single Wall Carbon nanotube (SWCNT) | Human ovarian cancer cell line OVCAR3 |
• Sensitises OVCAR3 cells to the chemotherapeutic compound paclitaxel (PTX) resulting in increased cell death • Apoptosis |
| de Gabory et al. [106] | Double-Walled Carbon Nanotubes (DWCNTs) | Human nasal epithelial cells (HNEpCs) |
• Dose-dependent decrease in cell metabolic activity and cell growth • Stimulation of mucus production • Significant increase in Reactive Oxygen Species • Increased effect after 12-day exposure |
| Eldawud et al. [107] | Single Wall Carbon nanotubes (SWCNTs) | Immortalised human lung epithelial cell (BEAS-2B) |
• Reducing cell viability • Changes cell structure, cycle and cell–cell interactions |
| Pacurari et al. [108] | Multi-walled carbon nanotubes (MWCNTs) | Human microvascular endothelial cells (HMVEC) |
• Increase in endothelial monolayer permeability and migration in HMVEC • Induces endothelial cell permeability • Production of reactive oxygen species • Actin filament remodelling |
| Reamon-Buettner et al. [109] | Multi-walled carbon nanotubes (MWCNTs) | Human peritoneal mesothelial cells LP9 |
• Inhibition of cell division • Induces premature cellular senescence |
| Phuyal et al. [110] | Multi-walled carbon nanotubes (MWCNTs) | Human bronchial epithelial 3-KT (HBEC-3KT) cells | • Alters both the proteome and the lipidome profiles of the target epithelial cells in the lung |
| Witzmann & Monteiro-Riviere [111] | Multi-walled carbon nanotubes (MWCNTs) | Cryopreserved neonatal human epidermal keratinocytes |
• Alters the protein expression in epithelial cells • Significant effect on the expression of cytoskeletal elements |
| Snyder et al. [112] | Multi-walled carbon nanotubes (MWCNTs) | Human bronchial epithelial primary cells |
• Negatively impacts the ability of human airway epithelium to form a monolayer barrier • Altered cell morphology • Cytoskeletal disruption |
| Snyder et al. [113] | Multi-walled carbon nanotube (MWCNTs) | Human bronchial epithelial cells (BECs) | • Causes mitochondrial dysfunction that leads to mitophagy |
| Ghosh et al. [28] | Multi-walled carbon nanotubes (MWCNTs) | Allium cepa bulbs |
• Cyto-genotoxicity • Induces significant DNA damage • Induces micronucleus formation • Chromosome aberration • Internucleosomal fragments formation, indicative of apoptotic cell death |
| Yu et al. [114] | Multi-walled carbon nanotubes (MWCNTs) | Immortalized human mesothelial cell line (Met-5A) |
• Causes significant cytotoxic effects on Met-5A cells • Higher concentrations induce cellular membrane permeability and disturbance of mitochondrial metabolism • No significant toxic effect at low concentrations • Reactive oxygen species formation |
| Rizk et al. [115] | Multi-walled carbon nanotube (MWCNTs) | Normal human dermal fibroblast (NHDF) cells |
• Induces induced massive loss of cell viability • DNA damage • Programmed cell death |
| Jos et al. [116] | Single wall carbon nanotubes (SWCNTs) | Human Caucasian colon adenocarcinoma (Caco-2) cell line |
• Increase in Lactate dehydrogenase (LDH) leakage • Cytotoxicity • Protein content only modified at higher concentrations |
| Vankoningsloo et al. [117] | Multi-walled carbon nanotubes (MWCNTs) |
1) Immortalised human keratinocytes (IHK) 2) SZ95 sebocytes 3) Reconstructed human epidermises (RHE) |
• Induces cytotoxicity in human keratinocytes • No cytotoxic effects in SZ95 sebocytes or in stratified epidermises reconstructed in vitro |
| Herzog et al. [118] | Single-walled carbon nanotubes (SWCNTs), Carbon black (CB) |
1) Human lung epithelial cells (A549) 2) Normal human primary bronchial epithelial cells (NHBE) |
• Low oxidative stress • Cell responses are strongly dependent on the vehicle used for dispersion • The presence of dipalmitoyl phosphatidylcholine (DPPC) increased intracellular reactive oxygen species (ROS) formation |
| Müller et al. [119] | Single-walled carbon nanotubes (SWCNTs) and Titanium dioxide (TiO2) | Human epithelial lung cells (A549), human monocyte-derived macrophages (MDMs) and monocyte-derived dendritic cells (MDDCs) |
• SWCNTs and TiO2 can penetrate into A549, MDMs, and MDDCs • Induces the production of reactive oxygen species |
| Baktur et al | Single-walled Carbon nanotubes (SWCNTs) | Human alveolar epithelial cells (A549) |
• Enhances Interleukin-8 (IL-8) expression in the presence of serum • Induces changes in IL-8 expression |
| Basak et al. [120] | Multi-walled carbon nanotubes (MWCNTs) and TiO2 nanobelts (TiO2-NB) | Human colorectal adenocarcinoma cells | • Cytotoxicity |
| Patlolla et al. [121] | Multi-walled carbon nanotubes (MWCNTs) | Normal human dermal fibroblast cells (NHDF) |
• Dose-dependent toxicity • Massive loss of cell viability through DNA damage • Cell death |
| Dahm et al. [122] | Carbon nanotubes and nanofibers (CNT/F) |
Sputum samples Scanning electron microscopy (SEM) |
• Industrial workers are exposed to the toxic effect of carbon nanotubes at the workplace |
| Fatkhutdinova et al. [123] | Multi-walled carbon nanotubes (MWCNTs) | Blood and sputum samples from workers |
• Induction of pro-inflammatory cytokines (IL-6, TNF-α, and IL-1β) • Induction of KL-6 (a serological biomarker for interstitial lung disease) • Accumulation of inflammatory and fibrotic biomarkers in biofluids of workers manufacturing MWCNTs |
| Zhao et al. [124] |
Multi-walled carbon nanotubes (MWCNTs) i.e., three commercially available MWCNTs, namely XFM4, XFM22, and XFM34 (diameters XFM4 < XFM22 < XFM34) |
Human umbilical vein endothelial cells (HUVECs) |
• XFM4 induced a significantly higher level of cytotoxicity than XFM22, and XFM34 • HUVECs internalized more XFM4 • XFM4 induces cytokine release, monocyte adhesion, and intracellular reactive oxygen species level • XFM4 exposure reduces the expression of autophagic genes autophagy-related 7 (ATG7), autophagy-related 12 (ATG12), and beclin 1 (BECN1) • Causes autophagy dysfunction and endoplasmic reticulum stress |
| Öner et al. [125] | Multi-walled carbon nanotubes (MWCNTs) and Single-walled carbon nanotubes (SWCNTs) | Human bronchial epithelial cells (16HBE) |
• MWCNTs induce a single hypomethylation at a CpG site and gene promoter region • No change in DNA methylation after the recovery period for MWCNTs • SWCNTs or amosite induce hypermethylation at CpG sites after sub-chronic exposure |
| Luanpitpong et al. [126] | Carbon nanotubes (CNT) | Non-tumorigenic human lung epithelial cells |
• Induces Cancer Stem-like cells (CSC) in lung epithelial cells • Induces specific stem cell surface markers CD24 low and CD133 high that are associated with SWCNT-induced CSC formation and tumorigenesis |
| Shvedova et al. [127] | Carbon nanotubes (CNT)—Multi-walled carbon nanotubes (MWCNTs) |
Air Sample Peripheral whole blood |
• Causes significant changes in the non-coding RNAs (ncRNA) and coding messenger RNAs (mRNA) expression profiles • Cell cycle regulation/progression/control • Apoptosis and proliferation • Potential to trigger pulmonary and cardiovascular effects • Potential to induce carcinogenic outcomes in humans |
| Domenech et al. [128] | Carbon-based nanoparticles: Graphene oxide (GO), Graphene nanoplatelets (GNPs) | Human colorectal adenocarcinomas (Caco-2, ATCC HTB-37) |
• No oxidative damage induction was detected, either by the DCFH-DA assay or the FPG enzyme in the comet assay • Both GO and GNPs induce DNA breaks • Induces weak anti-inflammatory response |
| Wang et al. [129] | Single-walled carbon nanotubes (SWCNT) and multi-walled carbon nanotubes (MWCNTs) | Primary human Small Airway epithelial Cells (SAECs) |
• Increases cell proliferation • Induces anchorage-independent growth • Causes cell invasion and angiogenesis |
| Mukherjee et al. [130] | Graphene oxide (GO) | human bronchial epithelium (BEAS-2B) cells |
• Causes mitochondrial dysfunction after a 48-h exposure • Causes engagement of apoptosis pathways after longer exposure periods (i.e., 28 days) • Causes down regulation of genes belonging to the inhibitor of apoptosis protein (IAP) family |
| Pérez et al. [131] | Reduced graphene oxide (rGO) | Human airway epithelial (BEAS-2B) cells | • Medium-term rGO exposure does not have significant effects on the DNA methylation patterns of human lung epithelial cells |
| Xu et al. [132] | Single-walled carbon nanotubes (SWCNT) | Pulmonary surfactant monolayer (PSM) |
• Inhalation toxicity of SWCNTs is largely affected by their lengths • Short SWCNTs increases inflammatory response • Longer SWCNTs causes severe lipid depletion and PSM-rigidifying effect |
| Gasser et al. [133] | Multi-walled carbon nanotubes (MWCNTs) |
Human monocyte derived macrophages (MDM) monocultures A sophisticated in vitro model of the human epithelial airway barrier |
• Increases reactive oxygen species levels • Decreases intracellular glutathione depletion in MDM • Decreases the release of Tumour necrosis factor alpha (TNF-Î ±) • Induces apoptosis • Increases the release of the release of Interleukin-8 (IL-8) |
| Di Cristo et al. [134] | Graphene Oxide (GO) | EpiAirway™ tissues (AIR-100, PE6-5), a 3D mucociliary tissue model of the primary human bronchial epithelium |
• Elicits proinflammatory response after 2 weeks exposure • Causes moderate barrier impairment • Induces autophagosome accumulation (resulting from blockade of autophagy flux) • Prolonged exposures increase the risk of pulmonary infections and/or lung diseases |
| Chortarea et al. [135] | Carbon nanotubes (CNTs) | Human (alveolar) epithelial A549 cell line with human monocyte-derived dendritic cells (MDDCs) and macrophages (MDMs) | • Repeated exposures to lung cell cultures at the Air–Liquid Interface, elicit a limited biological impact over a three-day period |
| Lee et al. [26] | Graphene oxide (GO) | Workplace air samples |
• Minimum release of graphene or other particles during manufacturing based on real-time aerosol monitoring • Negligible exposure to graphene based on personal and area sampling for the Total Suspended Particles (TSP) and elemental carbon (EC) |
| Both Inorganic-based and Carbon-based Nanoparticles | |||
| Phuyal et al. [21] | Titanium dioxide (TiO2) and multi-walled carbon nanotubes (MWCNTs) | Human bronchial epithelial (HBEC-3KT) cell line |
• Low cytotoxicity in short-term tests • Cell proliferation affected in long-term exposure |
| Shalini et al. [22] | Zinc oxide (ZnO) and nanorods | Human peripheral blood lymphocytes (HPBL) |
• Genotoxicity in smaller ZnO NPs • Cytotoxic effect in larger microparticles and microrods • Higher level of oxidative potential and reactive oxygen species generation capacity in ZnO NPs and nanorods |
| Simon-Deckers et al. [23] | Aluminium oxide (Al2O3), Titanium dioxide – (TiO2), Multi-walled carbon nanotubes (MWCNTs) | A549 human type II lung epithelium cell line |
• Carbon nanotubes are more toxic than metal oxide NPs • Both nanotubes and NPs rapidly enter into cells, and distribute in the cytoplasm and intracellular vesicles |
| Inorganic-based and Polymer Nanoparticles | |||
| Setyawati et al. [24] | Titanium dioxide (TiO2), Terbium-doped gadolinium oxide (Tb-Gd2O3), and Poly (lactic-co-glycolic acid) (PLGA) | Human neonatal foreskin fibroblast cell line (BJ) |
TiO2 and Tb-Gd2O3: • Dose-dependent cytotoxicity • Promotes genotoxicity via DNA damage PLGA nanoparticles: • Did not induce significant cytotoxic or genotoxic effects on BJ |
| Polymer Nanoparticles | |||
| Nishu et al. [25]., 2020 | Poly lactic-co-glycolic acid (PLGA) |
Nitrosomonas europaea KCTC 12270 bacterium Nitrospira moscoviensis bacterium |
• Reduce nitrification in both cultures of nitrifying strains and in microbial communities in soil samples |
Discussion
The objective of this scoping review was to ascertain the distribution of the current literature on the human and environmental impacts of nanoparticles. Specifically, in this review, we synthesised evidence regarding the exposure pathways and types of nanoparticles that have been researched and the ones that have not, as well as the biomarkers that have been used in assessing human and environmental impact of exposure to nanoparticles.
Characteristics of included studies
While the majority of studies originated from Europe and Central Asia, the United States of America (USA) alone recorded the highest number of publications. This finding is not surprising, as the USA has continuously fostered the development of nanotechnology through significant investments in research and development in this area. In 2016, the USA was projected to account for almost one-third of total global nanotechnology research funding [136]. Moreover, the USA and the European Union have over the years taken a committed approach towards enhancing the health and safety of nanoparticles [137]. As part of this commitment, annual meetings are held, where researchers discuss topics relating to nano-safety, as well as funding priorities and research needs.
While there have been some investments in nanotechnology research in African countries (including Egypt and South Africa), a recent publication by the United Nations Economic Commission for Africa (UNECA) indicates that the African continent, relative to other continents, is lagging behind with regards to nanotechnology research [138]. This assertion is consistent with the findings of this review, which found only one study originating from North Africa (Egypt), with no study conducted in Sub-Saharan Africa.
Over the past two decades, there have been increasing public awareness of nanotechnology and a growing concern about its commercial applications [139]. This has led to rapidly increasing scientific publications in this field, especially from early 2000s [140]. It is, therefore, not surprising that the studies included in this scoping review were published from the year 2006. Indeed, a literature search of nanotechnology publications by Huang et al. [140] revealed over 50,000 publications for the year 2006.
Although the included studies investigated a wide range of nanoparticles, most of them focused on inorganic-based nanoparticles (e.g., zinc oxide, titanium dioxide, copper oxide, and silica), followed by carbon-based nanoparticles (e.g., carbon-nanotubes, fullerenes, and graphene) (Table 3). This finding is consistent with previous reviews that have reported extensive investigation into the impact of inorganic-based and/or carbon-based nanoparticles [141, 142]. These nanoparticles may have gained attention due to their extensive production and usage. In addition to their use for cancer treatment, inorganic and carbon-based nanoparticles provide significant benefits in photothermal therapy, diagnosis, tissue engineering, imaging contrast agents, and sensing applications [143]. This is due to their unique physical and chemical properties (such as electrical, thermal, structural, mechanical, and optical diversity), which make them stronger, flexible, and more electrically conductible towards several biological entities [141, 144]. The advantages of, for example inorganic-based nanoparticles, including their high reactivity, small size and good capacity have been found to induce adverse harmful effects in both humans and the environment.
In this review, a number of approaches were used by included studies to assess the toxicity of nanoparticles. However, the majority of the studies applied the in vitro method, perhaps because in vitro studies are time saving and cost-effective. Nonetheless, the in vitro approach has been criticised by researchers (e.g., Bahadar et al. [145]) for producing varying results in different laboratories.
The included studies used differing methods in assessing cytotoxicity and genotoxicity: cell membrane integrity was assessed with Lactate dehydrogenase (LDH) assays [44, 57, 116]; cell viability was assessed using tetrazolium reduction assays [82, 83, 90, 116]; apoptosis was assessed using immunohistochemistry biomarkers [60, 65, 86]; electron microscopy was used to assess intracellular localisation of nanoparticles [34, 106]; and cell inflammation was estimated using chemokines biomarkers (i.e., IL-8, TNF- α, and IL-6) [146]. Compounds such as MTT, XTT, MTS, and WST-1 are used to detect viable cells [147]. However, in the current review, most of the studies employed MTT tetrazolium assays for investigating cell toxicity [47, 49, 50, 58, 116]. Similar findings have been reported by Bahadar et al. [145] who conducted a review on the toxicity of nanoparticles.
The human impact of nanoparticles
Most of the studies in this review focused on assessing the characteristics of nanoparticles, as well as the impact of nanoparticles on, particularly, human health. In recent years, there have been promising results from the application of nanoparticles to human health, especially in cancer treatment. This is due to the potential of nanoparticles to provide innovative solutions to curb the limitations of traditional treatment methods, including radiotherapy and chemotherapy [148]. Relative to conventional cancer treatment methods, nanoparticle-based drug delivery systems have been shown to have significant advantages in a) drug resistance, b) correctly targeting tumour cells, c) having good pharmacokinetics, and d) reduction of treatment side effects [149]. Notwithstanding these benefits, however, nanoparticles have potential harmful effects, and there are controversies about their safe use in humans [139]. This has undoubtedly led to the rapidly growing number of studies investigating the human health impact of nanoparticles, as was revealed in this review.
The majority of the studies (n = 90) in this review used immortalised cell lines as the biomarker for assessing human health impact of nanoparticles, and only 22 studies used primary cells as biomarkers. Immortalised cell lines have mostly been used for nano-safety studies because, relative to primary cells, they are generally less expensive, readily accessible, and easier to cultivate [150]. However, the type of cell that is used as biomarker for nano-safety studies is of great importance since this may have an impact on the general outcome of studies [151]. Cancer cell lines, for example, have a disturbed anti-apoptotic balance, and have undergone transformation in metabolism, which impacts their ability to sustain their high rate of proliferation [152]. As such, using these cells may have an impact on study findings. Nonetheless, the use of primary cells in nano-safety studies, are not without limitations. Primary cells have limited lifespan in vitro and can suffer from clonal changes.
In using immortalised cell lines, several studies [153, 154]) have reported variations in findings regarding nanoparticle-induced effects in cell lines obtained from different species or tissues. For example, Zhang et al. [153] and Mukherjee et al. [154] investigated the effect of exposure to silver nanoparticle on mammalian cells. Zhang et al. [153] used epithelial cells and microphages, and Mukherjee et al. [154] used the human dermal and cervical cell lines as biomarkers. Mukherjee et al. [154] reported nanoparticle-induced cytotoxicity such as elevated levels of oxidative stress, cell membrane damage, and glutathione depletion, whereas Zhang et al. [153] reported effects including changes in antioxidant defence and metallothionein. Moreover, while Ekstrand-Hammarstrom et al. [155] and Kermanizadeh et al. [156] have compared the effect of nanoparticles on immortalised cell lines versus primary cells of the same species and tissues, available data regarding the relative effectiveness of these two types of cells are unclear. Therefore, it is difficult to make explicit conclusions as to which of these two types of cells can be used as a reliable biomarker for nano-safety studies.
This review has revealed that humans are exposed to nanoparticles through inhalation, ingestion, or dermal route. After their exposure, nanoparticles induce toxic effects such as production of oxidative stress at the exposure site, inflammation, DNA damage, and cell death [87, 88]. For instance, exposure of human neuroblastoma (Sh-sy5y) cells to inorganic nanoparticles, such as titanium dioxide, silica dioxide, and silver are associated with induction of neurotoxicity, membrane damage, reaction oxygen specie formation, decrease in cell viability, and autophagy dysfunction [40]. Similarly, exposure to carbon-based nanoparticles such as single and multi-walled carbon nanotubes reduce cell viability, as well as induce changes in cell structure, cell cycle, and cell-to-cell interactions in human lung epithelial cells (BEAS-2B) [107].
The environmental impact of nanoparticles
The findings of this scoping review indicate a gap in the literature regarding environmental impact of nanoparticles. Out of the 117 included studies, only 5 had assessed the environmental impact of exposure to nanoparticles. This significant gap in the scientific literature has been highlighted by authors such as Bundschuh et al. [157]. The growing production and usage of nanoparticles has undoubtedly led to a diversification of emission sources into both the aquatic and soil environment. Nanoparticles enter the environment mainly through three emission scenarios: a) released during production of nano-enabled products and raw materials, b) during application, and c) following disposal of products containing nanoparticles [158]. These emissions occur either indirectly through systems such as landfills or wastewater treatment plants, or directly to the environment. Nonetheless, nanoparticles are mostly released during the application phase and following disposal [159]. Indeed, during production, only about 2% of the production volume is emitted [160]. The studies in this review used biomarkers such as soil samples and soybean seeds, zebrafish larvae, fish, and Daphnia magna neonates. This finding is in line with a previous review by Bundschuh et al. [157], which explored the effects of nanoparticles on the environment.
Limitations of the review
In this review, every effort was made to reduce bias. The search strategy was developed by experts of the review team with many years of experience in conducting systematic/scoping reviews. A comprehensive search of multiple relevant databases and other resources was conducted by one review author (EAK) and a rerun of the searches was done after 4 weeks of the initial search. Two authors (EAK and RF or PB and SH) independently screened the search results, and disagreements between reviewers were resolved by FVZ or TP.
The main limitation of this review is that the searches were limited to studies published in the English language. This may have led to the exclusion of potentially relevant papers published in other languages. Also, searches were restricted to studies published from the year 2000, which may have led to the omission of potentially relevant papers.
Conclusions
This review has provided an extensive synthesis of the current literature on the effects of nanoparticles on human health and the environment. The review has shown that while nanoparticles are beneficial in a range of applications, they pose significant threats to humans and the environment. Through the use of several biological models and biomarkers (e.g., human bronchial epithelial cells (Beas-2), soil samples, and soybean seeds), the included studies revealed the toxic effects of nanoparticles, with the most investigated nanoparticles being Zinc Oxide, MWCNTs, Titanium Dioxide, Cerium Oxide, SWCNTs, Ferric Oxide, and Silicon Dioxide. The main health impacts of nanoparticles identified in this review are decreased cell viability, cell death, reactive oxygen species generation, production of oxidative stress (dose-dependent), DNA damage, apoptosis, and induction of inflammatory responses.
This review has revealed a significant gap in the scientific literature regarding environmental impact of nanoparticles of all types. Future studies should be directed at investigating the impact of the various types of nanoparticles on the aquatic, terrestrial, and soil environment. The findings from this review have also shown limited data regarding the relative effectiveness of immortalised cell lines and primary cells as biomarkers in nano-safety studies. Future research should focus on evaluating the effectiveness of these two types of cells, in order to determine the cell that can be used as a reliable biomarker for nano-safety studies. There is also the need for future studies in this area to focus on exploring the toxic effects of Platinum, Gold, Magnesium Oxide, Molybdenum Trioxide, Tungsten trioxide, and Carbon Black nanoparticles, as findings from this review has shown that these nanoparticles are least researched. The findings of this review will be useful to policy makers and stakeholders in assessing the potential effects of nanoparticles.
Supplementary Information
Additional file 1. MEDLINE Search History.
Acknowledgements
We would like to thank Daphne Silva Pino and Romana Petry for their contribution at the initial stages of this research.
Authors’ contributions
Elizabeth Adjoa Kumah: Conceptualization, Methodology, Investigation, Formal analysis, Validation, Supervision, Writing—Original Draft, Writing—Review & Editing, Raoul Djou Fopa: Investigation, Data Curation, Saeed Harati: Investigation, Data Curation, Paul Boadu: Investigation, Data Curation, Formal analysis, Fatemeh Vida Zohoori: Conceptualization, Methodology, Validation, Supervision, Writing—Review & Editing, Funding acquisition, Tannaz Pak: Conceptualization, Methodology, Validation, Supervision, Writing—Review & Editing, Funding acquisition. The author(s) read and approved the final manuscript.
Funding
This research was funded through the GRUN project (Towards the first implementation of groundwater remediation using nanotechnology in Brazil) as part of UKRI’s Global Challenges Research Fund (GCRF) and a grant from the São Paulo Research Foundation (FAPESP) (Grant 17/20308–0).
Availability of data and materials
All data generated or analysed during this study are included in this published article and in the presented supplementary material file.
Declarations
Ethics approval and consent to participate
The research presented in this article is a scoping review, as such, no ethical approval was needed.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jiao H, Barakat N. Balanced depth and breadth in a new interdisciplinary nanotechnology course. J Educ Technol Syst. 2012;40(1):75–87. doi: 10.2190/ET.40.1.g. [DOI] [Google Scholar]
- 2.Khan I, Saeed K, Khan I. Nanoparticles: properties, applications and toxicities. Arab J Chem. 2017;12(7):908–931. doi: 10.1016/j.arabjc.2017.05.011. [DOI] [Google Scholar]
- 3.Som C, Wick P, Krug H, Nowack B. Environmental and health effects of nanomaterials in nanotextiles and facade coatings. Environ Int. 2011;37:1131–1142. doi: 10.1016/j.envint.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 4.Bottero JY, Rose J, Wiesner MR. Nanotechnologies: Tools for sustainability in a new wave of water treatment processes. Integr Environ Assess Manag. 2006;2:391–395. doi: 10.1002/ieam.5630020411. [DOI] [PubMed] [Google Scholar]
- 5.Pak T, Archilha NL, de Lima Luz, LF. Nanotechnology-Based Remediation of Groundwater. In: Kumar C, editor. Nanotechnology Characterization Tools for Environment, Health, and Safety. Berlin, Heidelberg: Springer; 2019. p. 145–65.
- 6.Pak T, Archilha NL, Al-Imari R. Application of nanotechnology in removal of NAPLs from contaminated aquifers: a source clean-up experimental study. Clean Technol Environ Pol. 2018;20:427–33. doi: 10.1007/s10098-018-1487-5. [DOI] [Google Scholar]
- 7.Pak T, Luz LFDL, Tosco T, Costa GSR, Rosa PRR, Archilha NL. Pore-scale investigation of the use of reactive nanoparticles for in situ remediation of contaminated groundwater source. Proc Natl Acad Sci. 2020;117(24):13366–73. doi: 10.1073/pnas.1918683117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lammers T, Hennink WE, Storm G. Tumour-targeted nanomedicines: Principles and practice. Br J Cancer. 2008;99:392–397. doi: 10.1038/sj.bjc.6604483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta AK, Gupta M. Synthesis and surface engineering of iron oxide nanoparticles for biomedical applications. Biomaterials. 2006;26:3995–4021. doi: 10.1016/j.biomaterials.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 10.Botta C, Labille J, Auffan M, Borschneck D, Miche H, Cabie M, et al. TiO2-based nanoparticles released in water from commercialized sunscreens in a life-cycle perspective: structures and quantities. Environ Pollut. 2011;159:1543–1550. doi: 10.1016/j.envpol.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Auffan M, Bottero JY, Chaneac C, Rose J. Inorganic manufactured nanoparticles: How their physicochemical properties influence their biological effects in aqueous environments. Nanomed Nanotechnol Biol Med. 2010;5:999–1007. doi: 10.2217/nnm.10.61. [DOI] [PubMed] [Google Scholar]
- 12.Oberdorster G, Oberdorster E, Oberdorster J. Nanotoxicology: an emerging discipline evolving from studies of ultrafine particles. Environ Health Perspect. 2005;113:823–839. doi: 10.1289/ehp.7339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Magrez A, Kasas S, Salicio V, Pasquier N, Seo JW, Celio M, et al. Cellular toxicity of carbon-based nanomaterials. Nano Lett. 2006;6(6):1121–1125. doi: 10.1021/nl060162e. [DOI] [PubMed] [Google Scholar]
- 14.Mancuso L, Cao G. Acute toxicity test of CuO nanoparticles using human mesenchymal stem cells. Toxicol Mech Methods. 2014;24(7):449–454. doi: 10.3109/15376516.2014.928920. [DOI] [PubMed] [Google Scholar]
- 15.Yokel RA, MacPhail RC. Engineered nanomaterials: exposures, hazards, and risk prevention. J Occup Med Toxicol. 2011;6:7. doi: 10.1186/1745-6673-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jeevanandam J, Barhoum A, Chan YS, Dufresne A, Danquah MK. Review on nanoparticles and nanostructured materials: history, sources, toxicity and regulation. Beilstein J Nanotechnol. 2018;9:908–931. doi: 10.3762/bjnano.9.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sahu SC, Hayes AW. Toxicity of nanomaterials found in human environment: a literature review. Toxicol Res Appl. 2017;1:2397847317726352. [Google Scholar]
- 18.Aromataris E, Munn Z (Editors). JBI Manual for Evidence Synthesis. Joanna Briggs Institute. 2020. Available from: 10.46658/JBIMES-20-01
- 19.Kumah EA, Zohoori V, Pak T, Harati S, Raoul FD, Boadu P. Effects of nanotechnology: A scoping review of the current literature. OSF; 2021. Available from: osf.io/w67m9.
- 20.Boczkowski J, Hoet P. What’s new in nanotechnology? Implications for public health from a brief review of the 2008 literature. Nanotoxicology. 2010;4(1):1–14. doi: 10.3109/17435390903428844. [DOI] [PubMed] [Google Scholar]
- 21.Phuyal S, Kasem M, Rubio L, Karlsson HL, Marcos R, Skaug V, et al. Effects on human bronchial epithelial cells following low-dose chronic exposure to nanomaterials: A 6-month transformation study. Toxicol Vitro : Int J Publishe Assoc BIBRA. 2017;44:230–240. doi: 10.1016/j.tiv.2017.07.016. [DOI] [PubMed] [Google Scholar]
- 22.Shalini D, Senthilkumar S, Rajaguru P. Effect of size and shape on toxicity of zinc oxide (ZnO) nanomaterials in human peripheral blood lymphocytes. Toxicol Mech Methods. 2018;28(2):87–94. doi: 10.1080/15376516.2017.1366609. [DOI] [PubMed] [Google Scholar]
- 23.Simon-Deckers A, Gouget B, Mayne-L'hermite M, Herlin-Boime N, Reynaud C, Carrière M. In vitro investigation of oxide nanoparticle and carbon nanotube toxicity and intracellular accumulation in A549 human pneumocytes. Toxicology. 2008;253(1–3):137–146. doi: 10.1016/j.tox.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 24.Setyawati MI, Khoo PKS, Eng BH, Xiong S, Zhao X, Das GK, et al. Cytotoxic and genotoxic characterization of titanium dioxide, gadolinium oxide, and poly(lactic-co-glycolic acid) nanoparticles in human fibroblasts. J Biomed Mater Res, Part A. 2013;101(3):633–640. doi: 10.1002/jbm.a.34363. [DOI] [PubMed] [Google Scholar]
- 25.Nishu SD, Park S, Ji Y, Han I, Key J, Lee TK. The effect of engineered PLGA nanoparticles on nitrifying bacteria in the soil environment. J Ind Eng Chem. 2020;84:297–304. doi: 10.1016/j.jiec.2020.01.011. [DOI] [Google Scholar]
- 26.Lee JH, Han JH, Kim JH, Kim B, Bello D, Kim JK, et al. Exposure monitoring of graphene nanoplatelets manufacturing workplaces. Inhalation Toxicol. 2016;28(6):281–291. doi: 10.3109/08958378.2016.1163442. [DOI] [PubMed] [Google Scholar]
- 27.Gaiser BK, Fernandes TF, Jepson M, Lead JR, Tyler CR, Stone V, et al. Assessing exposure, uptake and toxicity of silver and cerium dioxide nanoparticles from contaminated environments. Environ Health. 2009;8(1):S2. doi: 10.1186/1476-069X-8-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ghosh M, Bhadra S, Adegoke A, Bandyopadhyay M, Mukherjee A. MWCNT uptake in Allium cepa root cells induces cytotoxic and genotoxic responses and results in DNA hyper-methylation. Mutat Res. 2015;774:49–58. doi: 10.1016/j.mrfmmm.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 29.Lee S, Kim S, Kim S, Lee I. Effects of soil-plant interactive system on response to exposure to ZnO nanoparticles. J Microbiol Biotechnol. 2012;22(9):1264–1270. doi: 10.4014/jmb.1203.03004. [DOI] [PubMed] [Google Scholar]
- 30.Yusefi-Tanha E, Fallah S, Rostamnejadi A, Pokhrel LR. Zinc oxide nanoparticles (ZnONPs) as a novel nanofertilizer: Influence on seed yield and antioxidant defense system in soil grown soybean (Glycine max cv. Kowsar) Sci Total Enviro. 2020;738:140240. doi: 10.1016/j.scitotenv.2020.140240. [DOI] [PubMed] [Google Scholar]
- 31.Ahamed M, Akhtar MJ, Khan MAM, Alrokayan SA, Alhadlaq HA. Oxidative stress mediated cytotoxicity and apoptosis response of bismuth oxide (Bi2O3) nanoparticles in human breast cancer (MCF-7) cells. Chemosphere. 2019;216:823–831. doi: 10.1016/j.chemosphere.2018.10.214. [DOI] [PubMed] [Google Scholar]
- 32.Eom H-J, Choi J. Oxidative stress of silica nanoparticles in human bronchial epithelial cell, Beas-2B. Toxicol In Vitro. 2009;23(7):1326–1332. doi: 10.1016/j.tiv.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 33.Bengalli R, Colantuoni A, Perelshtein I, Gedanken A, Collini M, Mantecca P, et al. In vitro skin toxicity of CuO and ZnO nanoparticles: Application in the safety assessment of antimicrobial coated textiles. NanoImpact. 2021;21:100282. doi: 10.1016/j.impact.2020.100282. [DOI] [PubMed] [Google Scholar]
- 34.Ferraro SA, Domingo MG, Etcheverrito A, Olmedo DG, Tasat DR. Neurotoxicity mediated by oxidative stress caused by titanium dioxide nanoparticles in human neuroblastoma (SH-SY5Y) cells. J Trace Elem Med Biol. 2020;57:126413. doi: 10.1016/j.jtemb.2019.126413. [DOI] [PubMed] [Google Scholar]
- 35.Gambardella C, Morgana S, Bari GD, Ramoino P, Bramini M, Diaspro A, et al. Multidisciplinary screening of toxicity induced by silica nanoparticles during sea urchin development. Chemosphere. 2015;139:486–495. doi: 10.1016/j.chemosphere.2015.07.072. [DOI] [PubMed] [Google Scholar]
- 36.Oh JH, Son MY, Choi MS, Kim S, Choi AY, Lee HA, Kim KS, Kim J, Song CW, Yoon S. Integrative analysis of genes and miRNA alterations in human embryonic stem cells-derived neural cells after exposure to silver nanoparticles. Toxicol Appl Pharmacol. 2016;299:8-23. 10.1016/j.taap.2015.11.004. [DOI] [PubMed]
- 37.Zhao L, Yu C, Lv J, Cui Y, Wang Y, Hou C, et al. Fluoride exposure, dopamine relative gene polymorphism and intelligence: A cross-sectional study in China. Ecotoxicol Environ Saf. 2021;209:111826. doi: 10.1016/j.ecoenv.2020.111826. [DOI] [PubMed] [Google Scholar]
- 38.Ying E, Hwang H-M. In vitro evaluation of the cytotoxicity of iron oxide nanoparticles with different coatings and different sizes in A3 human T lymphocytes. Sci Total Environ. 2010;408(20):4475–4481. doi: 10.1016/j.scitotenv.2010.07.025. [DOI] [PubMed] [Google Scholar]
- 39.Jing X, Park JH, Peters TM, Thorne PS. Toxicity of copper oxide nanoparticles in lung epithelial cells exposed at the air–liquid interface compared with in vivo assessment. Toxicol In Vitro. 2015;29(3):502–511. doi: 10.1016/j.tiv.2014.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lojk J, Repas J, Veranič P, Bregar VB, Pavlin M. Toxicity mechanisms of selected engineered nanoparticles on human neural cells in vitro. Toxicology. 2020;432:152364. doi: 10.1016/j.tox.2020.152364. [DOI] [PubMed] [Google Scholar]
- 41.Tsai S-M, Duran-Robles E, Goshia T, Mesina M, Garcia C, Young J, et al. CeO2 nanoparticles attenuate airway mucus secretion induced by TiO2 nanoparticles. Sci Total Environ. 2018;631–632:262–269. doi: 10.1016/j.scitotenv.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sramkova M, Kozics K, Masanova V, Uhnakova I, Razga F, Nemethova V, et al. Kidney nanotoxicity studied in human renal proximal tubule epithelial cell line TH1. Mut Res/Gen Toxicol Environ Mutagen. 2019;845:403017. doi: 10.1016/j.mrgentox.2019.01.012. [DOI] [PubMed] [Google Scholar]
- 43.Bell KJ, Lansakara TI, Crawford R, Monroe TB, Tivanski AV, Salem AK, et al. Mechanical cues protect against silica nanoparticle exposure in SH-SY5Y neuroblastoma. Toxicol In Vitro. 2021;70:105031. doi: 10.1016/j.tiv.2020.105031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Akhtar MJ, Ahamed M, Kumar S, Siddiqui H, Patil G, Ashquin M, et al. Nanotoxicity of pure silica mediated through oxidant generation rather than glutathione depletion in human lung epithelial cells. Toxicology. 2010;276(2):95–102. doi: 10.1016/j.tox.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 45.Dankers ACA, Kuper CF, Boumeester AJ, Fabriek BO, Kooter IM, Gröllers-Mulderij M, et al. A practical approach to assess inhalation toxicity of metal oxide nanoparticles in vitro. J Appl Toxicol : JAT. 2018;38(2):160–171. doi: 10.1002/jat.3518. [DOI] [PubMed] [Google Scholar]
- 46.Chen R, Huo L, Shi X, Bai R, Zhang Z, Zhao Y, et al. Endoplasmic reticulum stress induced by zinc oxide nanoparticles is an earlier biomarker for nanotoxicological evaluation. ACS Nano. 2014;8(3):2562–2574. doi: 10.1021/nn406184r. [DOI] [PubMed] [Google Scholar]
- 47.Patil NA, Gade WN, Deobagkar DD. Epigenetic modulation upon exposure of lung fibroblasts to TiO 2 and ZnO nanoparticles: alterations in DNA methylation. Int J Nanomed. 2016;11:4509–4519. doi: 10.2147/IJN.S110390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mohamed BM, Verma NK, Prina-Mello A, Williams Y, Davies AM, Bakos G, et al. Activation of stress-related signalling pathway in human cells upon SiO2 nanoparticles exposure as an early indicator of cytotoxicity. J Nanobiotechnol. 2011;9:29. doi: 10.1186/1477-3155-9-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Alshatwi AA, Subbarayan PV, Ramesh E, Al-Hazzani AA, Alsaif MA, Alwarthan AA. Aluminium oxide nanoparticles induce mitochondrial-mediated oxidative stress and alter the expression of antioxidant enzymes in human mesenchymal stem cells. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2013;30(1):1–10. doi: 10.1080/19440049.2012.729160. [DOI] [PubMed] [Google Scholar]
- 50.Baber O, Jang M, Barber D, Powers K. Amorphous silica coatings on magnetic nanoparticles enhance stability and reduce toxicity to in vitro BEAS-2B cells. Inhalation Toxicol. 2011;23(9):532–543. doi: 10.3109/08958378.2011.592869. [DOI] [PubMed] [Google Scholar]
- 51.Corbalan JJ, Medina C, Jacoby A, Malinski T, Radomski MW. Amorphous silica nanoparticles aggregate human platelets: potential implications for vascular homeostasis. Int J Nanomed. 2012;7:631–639. doi: 10.2147/IJN.S28293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Branica G, Mladinić M, Omanović D, Želježić D. An alternative approach to studying the effects of ZnO nanoparticles in cultured human lymphocytes: combining electrochemistry and genotoxicity tests. Arh Hig Rada Toksikol. 2016;67(4):277–288. doi: 10.1515/aiht-2016-67-2910. [DOI] [PubMed] [Google Scholar]
- 53.Gurunathan S, Jeyaraj M, La H, Yoo H, Choi Y, Do JT, et al. Anisotropic platinum nanoparticle-induced cytotoxicity, apoptosis, inflammatory response, and transcriptomic and molecular pathways in human acute monocytic leukemia cells. Int J Mol Sci. 2020;21(2):440. doi: 10.3390/ijms21020440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hussain S, Al-Nsour F, Rice AB, Marshburn J, Ji Z, Zink JI, et al. Cerium dioxide nanoparticles do not modulate the lipopolysaccharide-induced inflammatory response in human monocytes. Int J Nanomed. 2012;7:1387–1397. doi: 10.2147/IJN.S29429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zerboni A, Bengalli R, Baeri G, Fiandra L, Catelani T, Mantecca P. Mixture effects of diesel exhaust and metal oxide nanoparticles in human lung a549 cells. Nanomaterials (Basel, Switzerland) 2019;9(9):1302. doi: 10.3390/nano9091302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zielinska E, Tukaj C, Radomski MW, Inkielewicz-Stepniak I. Molecular mechanism of silver nanoparticles-induced human osteoblast cell death: protective effect of inducible nitric oxide synthase inhibitor. PLoS ONE. 2016;11(10):e0164137. doi: 10.1371/journal.pone.0164137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rajiv S, Jerobin J, Saranya V, Nainawat M, Sharma A, Makwana P, et al. Comparative cytotoxicity and genotoxicity of cobalt (II, III) oxide, iron (III) oxide, silicon dioxide, and aluminum oxide nanoparticles on human lymphocytes in vitro. Hum Exp Toxicol. 2016;35(2):170–183. doi: 10.1177/0960327115579208. [DOI] [PubMed] [Google Scholar]
- 58.Alarifi S, Ali D, Verma A, Alakhtani S, Ali BA. Cytotoxicity and genotoxicity of copper oxide nanoparticles in human skin keratinocytes cells. Int J Toxicol. 2013;32(4):296–307. doi: 10.1177/1091581813487563. [DOI] [PubMed] [Google Scholar]
- 59.Sun J, Wang S, Zhao D, Hun FH, Weng L, Liu H. Cytotoxicity, permeability, and inflammation of metal oxide nanoparticles in human cardiac microvascular endothelial cells: cytotoxicity, permeability, and inflammation of metal oxide nanoparticles. Cell Biol Toxicol. 2011;27(5):333–342. doi: 10.1007/s10565-011-9191-9. [DOI] [PubMed] [Google Scholar]
- 60.Tolliver LM, Holl NJ, Hou FYS, Lee H-J, Cambre MH, Huang Y-W. Differential cytotoxicity induced by transition metal oxide nanoparticles is a function of cell killing and suppression of cell proliferation. Int J Mol Sci. 2020;21(5):1731. doi: 10.3390/ijms21051731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rothen-Rutishauser B, Grass RN, Blank F, Limbach LK, Mühlfeld C, Brandenberger C, et al. Direct combination of nanoparticle fabrication and exposure to lung cell cultures in a closed setup as a method to simulate accidental nanoparticle exposure of humans. Environ Sci Technol. 2009;43(7):2634–2640. doi: 10.1021/es8029347. [DOI] [PubMed] [Google Scholar]
- 62.Benameur L, Auffan M, Cassien M, Liu W, Culcasi M, Rahmouni H, et al. DNA damage and oxidative stress induced by CeO2 nanoparticles in human dermal fibroblasts: Evidence of a clastogenic effect as a mechanism of genotoxicity. Nanotoxicology. 2015;9(6):696–705. doi: 10.3109/17435390.2014.968889. [DOI] [PubMed] [Google Scholar]
- 63.Gojova A, Lee J-T, Jung HS, Guo B, Barakat AI, Kennedy IM. Effect of cerium oxide nanoparticles on inflammation in vascular endothelial cells. Inhalation Toxicol. 2009;21(Suppl 1):123–130. doi: 10.1080/08958370902942582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hildebrand H, Kühnel D, Potthoff A, Mackenzie K, Springer A, Schirmer K. Evaluating the cytotoxicity of palladium/magnetite nano-catalysts intended for wastewater treatment. Environ Pollut (Barking, Essex 1987) 2010;158(1):65–73. doi: 10.1016/j.envpol.2009.08.021. [DOI] [PubMed] [Google Scholar]
- 65.Lai JCK, Lai MB, Jandhyam S, Dukhande VV, Bhushan A, Daniels CK, et al. Exposure to titanium dioxide and other metallic oxide nanoparticles induces cytotoxicity on human neural cells and fibroblasts. Int J Nanomed. 2008;3(4):533–545. doi: 10.2147/ijn.s3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ahamed M, Siddiqui MA, Akhtar MJ, Ahmad I, Pant AB, Alhadlaq HA. Genotoxic potential of copper oxide nanoparticles in human lung epithelial cells. Biochem Biophys Res Commun. 2010;396(2):578–583. doi: 10.1016/j.bbrc.2010.04.156. [DOI] [PubMed] [Google Scholar]
- 67.Vergaro V, Aldieri E, Fenoglio I, Marucco A, Carlucci C, Ciccarella G. Surface reactivity and in vitro toxicity on human bronchial epithelial cells (BEAS-2B) of nanomaterials intermediates of the production of titania-based composites. Toxicol Vitro : Int J Publish Assoc BIBRA. 2016;34:171–178. doi: 10.1016/j.tiv.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 68.Dávila-Grana Á, Diego-González L, González-Fernández Á, Simón-Vázquez R. Synergistic effect of metal oxide nanoparticles on cell viability and activation of MAP Kinases and NFκB. Int J Mol Sci. 2018;19(1):246. doi: 10.3390/ijms19010246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pierscionek BK, Li Y, Schachar RA, Chen W. The effect of high concentration and exposure duration of nanoceria on human lens epithelial cells. Nanomed Nanotechnol Biol Med. 2012;8(3):383–390. doi: 10.1016/j.nano.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 70.Rafieepour A, Azari MR, Khodagholi F, Jaktaji JP, Mehrabi Y, Peirovi H. The effect of single and combined exposures to magnetite and polymorphous silicon dioxide nanoparticles on the human A 549 cell line: in vitro study. Environ Sci Pollut Res Int. 2019;26(31):31752–31762. doi: 10.1007/s11356-019-06229-0. [DOI] [PubMed] [Google Scholar]
- 71.Ickrath P, Wagner M, Scherzad A, Gehrke T, Burghartz M, Hagen R, et al. Time-dependent toxic and genotoxic effects of zinc oxide nanoparticles after long-term and repetitive exposure to human mesenchymal stem cells. Int J Environ Res Public Health. 2017;14(12):1590. doi: 10.3390/ijerph14121590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Radeloff K, Radeloff A, Ramos Tirado M, Scherzad A, Hagen R, Kleinsasser NH, et al. Toxicity and Functional Impairment in Human Adipose Tissue-Derived Stromal Cells (hASCs) following long-term exposure to Very Small Iron Oxide Particles (VSOPs) Nanomaterials (Basel, Switzerland) 2020;10(4):741. doi: 10.3390/nano10040741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jin M, Li N, Sheng W, Ji X, Liang X, Kong B, et al. Toxicity of different zinc oxide nanomaterials and dose-dependent onset and development of Parkinson's disease-like symptoms induced by zinc oxide nanorods. Environ Int. 2021;146:106179. doi: 10.1016/j.envint.2020.106179. [DOI] [PubMed] [Google Scholar]
- 74.Kumari M, Singh SP, Chinde S, Rahman MF, Mahboob M, Grover P. Toxicity study of cerium oxide nanoparticles in human neuroblastoma cells. Int J Toxicol. 2014;33(2):86–97. doi: 10.1177/1091581814522305. [DOI] [PubMed] [Google Scholar]
- 75.Fernández-Bertólez N, Costa C, Brandão F, Kiliç G, Duarte JA, Teixeira JP, et al. Toxicological assessment of silica-coated iron oxide nanoparticles in human astrocytes. Food Chem Toxicol : Int J Publish Bri Industr Biol Res Assoc. 2018;118:13–23. doi: 10.1016/j.fct.2018.04.058. [DOI] [PubMed] [Google Scholar]
- 76.Gliga AR, Di Bucchianico S, Åkerlund E, Karlsson HL. Transcriptome profiling and toxicity following long-term, low dose exposure of human lung cells to Ni and NiO nanoparticles-comparison with NiCl 2. Nanomaterials (Basel, Switzerland) 2020;10(4):649. doi: 10.3390/nano10040649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kennedy IM, Wilson D, Barakat AI. Uptake and inflammatory effects of nanoparticles in a human vascular endothelial cell line. Res Rep (Health Effects Institute) 2009;136:3–32. [PubMed] [Google Scholar]
- 78.Schanen BC, Das S, Reilly CM, Warren WL, Self WT, Seal S, et al. Immunomodulation and T helper TH1/TH2 response polarization by CeO2 and TiO2 nanoparticles. PLoS ONE. 2013;8(5):e62816. doi: 10.1371/journal.pone.0062816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Seker S, Elçin AE, Yumak T, Sınağ A, Elçin YM. In vitro cytotoxicity of hydrothermally synthesized ZnO nanoparticles on human periodontal ligament fibroblast and mouse dermal fibroblast cells. Toxicol Vitro : Int J Publish Assoc BIBRA. 2014;28(8):1349–1358. doi: 10.1016/j.tiv.2014.06.016. [DOI] [PubMed] [Google Scholar]
- 80.Könen-Adıgüzel S, Ergene S. In vitro evaluation of the genotoxicity of CeO 2 nanoparticles in human peripheral blood lymphocytes using cytokinesis-block micronucleus test, comet assay, and gamma H2AX. Toxicol Ind Health. 2018;34(5):293–300. doi: 10.1177/0748233717753780. [DOI] [PubMed] [Google Scholar]
- 81.Henson TE, Navratilova J, Tennant AH, Bradham KD, Rogers KR, Hughes MF. In vitro intestinal toxicity of copper oxide nanoparticles in rat and human cell models. Nanotoxicology. 2019;13(6):795–811. doi: 10.1080/17435390.2019.1578428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gojova A, Guo B, Kota RS, Rutledge JC, Kennedy IM, Barakat AI. Induction of inflammation in vascular endothelial cells by metal oxide nanoparticles: effect of particle composition. Environ Health Perspect. 2007;115(3):403–409. doi: 10.1289/ehp.8497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Alarifi S, Ali D, Alkahtani S, Verma A, Ahamed M, Ahmed M, et al. Induction of oxidative stress, DNA damage, and apoptosis in a malignant human skin melanoma cell line after exposure to zinc oxide nanoparticles. Int J Nanomed. 2013;8:983–993. doi: 10.2147/IJN.S42028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Åkerlund E, Islam MS, McCarrick S, Alfaro-Moreno E, Karlsson HL. Inflammation and (secondary) genotoxicity of Ni and NiO nanoparticles. Nanotoxicology. 2019;13(8):1060–1072. doi: 10.1080/17435390.2019.1640908. [DOI] [PubMed] [Google Scholar]
- 85.Jiménez-Chávez A, Solorio-Rodríguez A, Escamilla-Rivera V, Leseman D, Morales-Rubio R, Uribe-Ramírez M, et al. Inflammatory response in human alveolar epithelial cells after TiO 2 NPs or ZnO NPs exposure: Inhibition of surfactant protein A expression as an indicator for loss of lung function. Environ Toxicol Pharmacol. 2021;86:103654. doi: 10.1016/j.etap.2021.103654. [DOI] [PubMed] [Google Scholar]
- 86.Hussain S, Garantziotis S. Interplay between apoptotic and autophagy pathways after exposure to cerium dioxide nanoparticles in human monocytes. Autophagy. 2013;9(1):101–103. doi: 10.4161/auto.22266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Abudayyak M, Öztaş E, Arici M, Özhan G. Investigation of the toxicity of bismuth oxide nanoparticles in various cell lines. Chemosphere. 2017;169:117–123. doi: 10.1016/j.chemosphere.2016.11.018. [DOI] [PubMed] [Google Scholar]
- 88.Fahmy HM, Ebrahim NM, Gaber MH. In-vitro evaluation of copper/copper oxide nanoparticles cytotoxicity and genotoxicity in normal and cancer lung cell lines. J Trace Elem Med Biol. 2020;60:126481. doi: 10.1016/j.jtemb.2020.126481. [DOI] [PubMed] [Google Scholar]
- 89.Božinović K, Nestić D, Centa UG, Ambriović-Ristov A, Dekanić A, de Bisschop L, et al. In-vitro toxicity of molybdenum trioxide nanoparticles on human keratinocytes. Toxicology. 2020;444:152564. doi: 10.1016/j.tox.2020.152564. [DOI] [PubMed] [Google Scholar]
- 90.Ahamed M, Alhadlaq HA, Alam J, Khan MAM, Ali D, Alarafi S. Iron oxide nanoparticle-induced oxidative stress and genotoxicity in human skin epithelial and lung epithelial cell lines. Curr Pharm Des. 2013;19(37):6681–6690. doi: 10.2174/1381612811319370011. [DOI] [PubMed] [Google Scholar]
- 91.Pelclova D, Zdimal V, Kacer P, Fenclova Z, Vlckova S, Komarc M, et al. Leukotrienes in exhaled breath condensate and fractional exhaled nitric oxide in workers exposed to TiO2 nanoparticles. J Breath Res. 2016;10(3):036004. doi: 10.1088/1752-7155/10/3/036004. [DOI] [PubMed] [Google Scholar]
- 92.Valdiglesias V, Costa C, Kiliç G, Costa S, Pásaro E, Laffon B, et al. Neuronal cytotoxicity and genotoxicity induced by zinc oxide nanoparticles. Environ Int. 2013;55:92–100. doi: 10.1016/j.envint.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 93.Verdon R, Gillies SL, Brown DM, Henry T, Tran L, Tyler CR, et al. Neutrophil activation by nanomaterials in vitro : comparing strengths and limitations of primary human cells with those of an immortalized (HL-60) cell line. Nanotoxicology. 2021;15(1):1–20. doi: 10.1080/17435390.2020.1834635. [DOI] [PubMed] [Google Scholar]
- 94.Siddiqui MA, Ahamed M, Ahmad J, Majeed Khan MA, Musarrat J, Al-Khedhairy AA, et al. Nickel oxide nanoparticles induce cytotoxicity, oxidative stress and apoptosis in cultured human cells that is abrogated by the dietary antioxidant curcumin. Food Chem Toxicol : Int J Publish Bri Industr Biol Res Assoc. 2012;50(3–4):641–647. doi: 10.1016/j.fct.2012.01.017. [DOI] [PubMed] [Google Scholar]
- 95.Park E-J, Choi J, Park Y-K, Park K. Oxidative stress induced by cerium oxide nanoparticles in cultured BEAS-2B cells. Toxicology. 2008;245(1–2):90–100. doi: 10.1016/j.tox.2007.12.022. [DOI] [PubMed] [Google Scholar]
- 96.Fakhar-e-Alam M, Kishwar S, Willander M. Photodynamic effects of zinc oxide nanowires in skin cancer and fibroblast. Lasers Med Sci. 2014;29(3):1189–1194. doi: 10.1007/s10103-013-1501-4. [DOI] [PubMed] [Google Scholar]
- 97.Hackenberg S, Zimmermann F-Z, Scherzed A, Friehs G, Froelich K, Ginzkey C, et al. Repetitive exposure to zinc oxide nanoparticles induces dna damage in human nasal mucosa mini organ cultures. Environ Mol Mutagen. 2011;52(7):582–589. doi: 10.1002/em.20661. [DOI] [PubMed] [Google Scholar]
- 98.Andujar P, Simon-Deckers A, Galateau-Sallé F, Fayard B, Beaune G, Clin B, et al. Role of metal oxide nanoparticles in histopathological changes observed in the lung of welders. Part Fibre Toxicol. 2014;11:23. doi: 10.1186/1743-8977-11-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sharma V, Anderson D, Dhawan A. Zinc oxide nanoparticles induce oxidative DNA damage and ROS-triggered mitochondria mediated apoptosis in human liver cells (HepG2) Apoptosis. 2012;17(8):852–870. doi: 10.1007/s10495-012-0705-6. [DOI] [PubMed] [Google Scholar]
- 100.Senapati VA, Kumar A, Gupta GS, Pandey AK, Dhawan A. ZnO nanoparticles induced inflammatory response and genotoxicity in human blood cells: a mechanistic approach. Food Chem Toxicol. 2015;85:61–70. doi: 10.1016/j.fct.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 101.Vlaanderen J, Pronk A, Rothman N, Hildesheim A, Silverman D, Hosgood HD, et al. A cross-sectional study of changes in markers of immunological effects and lung health due to exposure to multi-walled carbon nanotubes. Nanotoxicology. 2017;11(3):395–404. doi: 10.1080/17435390.2017.1308031. [DOI] [PubMed] [Google Scholar]
- 102.Asghar W, Shafiee H, Velasco V, Sah VR, Guo S, El Assal R, et al. Toxicology study of single-walled carbon nanotubes and reduced graphene oxide in human sperm. Sci Rep. 2016;6:30270. doi: 10.1038/srep30270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Periasamy VS, Athinarayanan J, Alfawaz MA, Alshatwi AA. Carbon nanoparticle induced cytotoxicity in human mesenchymal stem cells through upregulation of TNF3, NFKBIA and BCL2L1 genes. Chemosphere. 2016;144:275–284. doi: 10.1016/j.chemosphere.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 104.Beard JD, Erdely A, Dahm MM, de Perio MA, Birch ME, Evans DE, et al. Carbon nanotube and nanofiber exposure and sputum and blood biomarkers of early effect among U.S. workers. Environ Int. 2018;116:214–28. doi: 10.1016/j.envint.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zhang W, Zhang D, Tan J, Cong H. Carbon nanotube exposure sensitize human ovarian cancer cells to paclitaxel. J Nanosci Nanotechnol. 2012;12(9):7211–7214. doi: 10.1166/jnn.2012.6506. [DOI] [PubMed] [Google Scholar]
- 106.de Gabory L, Bareille R, Daculsi R, L’Azou B, Flahaut E, Bordenave L. Carbon nanotubes have a deleterious effect on the nose: the first in vitro data. Rhinology. 2011;49(4):445–52. doi: 10.4193/Rhino10.256. [DOI] [PubMed] [Google Scholar]
- 107.Eldawud R, Wagner A, Dong C, Stueckle TA, Rojanasakul Y, Dinu CZ. Carbon nanotubes physicochemical properties influence the overall cellular behavior and fate. NanoImpact. 2018;9:72–84. doi: 10.1016/j.impact.2017.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pacurari M, Qian Y, Fu W, Schwegler-Berry D, Ding M, Castranova V, et al. Cell permeability, migration, and reactive oxygen species induced by multiwalled carbon nanotubes in human microvascular endothelial cells. J Toxicol Environ Health A. 2012;75(2):112–128. doi: 10.1080/15287394.2011.615110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Reamon-Buettner SM, Hackbarth A, Leonhardt A, Braun A, Ziemann C. Cellular senescence as a response to multiwalled carbon nanotube (MWCNT) exposure in human mesothelial cells. Mech Ageing Dev. 2021;193:111412. doi: 10.1016/j.mad.2020.111412. [DOI] [PubMed] [Google Scholar]
- 110.Phuyal S, Kasem M, Knittelfelder O, Sharma A, Fonseca DDM, Vebraite V, et al. Characterization of the proteome and lipidome profiles of human lung cells after low dose and chronic exposure to multiwalled carbon nanotubes. Nanotoxicology. 2018;12(2):138–52. doi: 10.1080/17435390.2018.1425500. [DOI] [PubMed] [Google Scholar]
- 111.Witzmann FA, Monteiro-Riviere NA. Multi-walled carbon nanotube exposure alters protein expression in human keratinocytes. Nanomedicine. 2006;2(3):158–168. doi: 10.1016/j.nano.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 112.Snyder RJ, Hussain S, Rice AB, Garantziotis S. Multiwalled carbon nanotubes induce altered morphology and loss of barrier function in human bronchial epithelium at noncytotoxic doses. Int J Nanomed. 2014;9:4093–4105. doi: 10.2147/IJN.S65567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Snyder RJ, Verhein KC, Vellers HL, Burkholder AB, Garantziotis S, Kleeberger SR. Multi-walled carbon nanotubes upregulate mitochondrial gene expression and trigger mitochondrial dysfunction in primary human bronchial epithelial cells. Nanotoxicology. 2019;13(10):1344–1361. doi: 10.1080/17435390.2019.1655107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Yu M, Chen R, Jia Z, Chen J, Lou J, Tang S, et al. MWCNTs Induce ROS Generation, ERK Phosphorylation, and SOD-2 expression in human mesothelial cells. Int J Toxicol. 2016;35(1):17–26. doi: 10.1177/1091581815591223. [DOI] [PubMed] [Google Scholar]
- 115.Rizk MZ, Ali SA, Kadry MO, Fouad GI, Kamel NN, Younis EA, et al. C-reactive protein signaling and chromosomal abnormalities in nanotoxicity induced via different doses of TiO 2 (80 nm) boost liver function. Biol Trace Elem Res. 2020;198(1):157–167. doi: 10.1007/s12011-020-02030-0. [DOI] [PubMed] [Google Scholar]
- 116.Jos A, Pichardo S, Puerto M, Sánchez E, Grilo A, Cameán AM. Cytotoxicity of carboxylic acid functionalized single wall carbon nanotubes on the human intestinal cell line Caco-2. Toxicol Vitro : Int J Published Assoc BIBRA. 2009;23(8):1491–1496. doi: 10.1016/j.tiv.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 117.Vankoningsloo S, Piret J-P, Saout C, Noel F, Mejia J, Zouboulis CC, et al. Cytotoxicity of multi-walled carbon nanotubes in three skin cellular models: effects of sonication, dispersive agents and corneous layer of reconstructed epidermis. Nanotoxicology. 2010;4(1):84–97. doi: 10.3109/17435390903428869. [DOI] [PubMed] [Google Scholar]
- 118.Herzog E, Byrne HJ, Davoren M, Casey A, Duschl A, Oostingh GJ. Dispersion medium modulates oxidative stress response of human lung epithelial cells upon exposure to carbon nanomaterial samples. Toxicol Appl Pharmacol. 2009;236(3):276–281. doi: 10.1016/j.taap.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 119.Müller L, Riediker M, Wick P, Mohr M, Gehr P, Rothen-Rutishauser B. Oxidative stress and inflammation response after nanoparticle exposure: differences between human lung cell monocultures and an advanced three-dimensional model of the human epithelial airways. J R Soc Interface. 2010;7(Suppl 1):S27–S40. doi: 10.1098/rsif.2009.0161.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Basak SC, Vracko M, Witzmann FA. Mathematical nanotoxicoproteomics: quantitative characterization of effects of Multi-walled Carbon Nanotubes (MWCNT) and TiO2 Nanobelts (TiO2-NB) on protein expression patterns in human intestinal cells. Curr Comput Aided Drug Des. 2016;12(4):259–264. doi: 10.2174/1573409912666160824145722. [DOI] [PubMed] [Google Scholar]
- 121.Patlolla A, Patlolla B, Tchounwou P. Evaluation of cell viability, DNA damage, and cell death in normal human dermal fibroblast cells induced by functionalized multiwalled carbon nanotube. Mol Cell Biochem. 2010;338(1–2):225–232. doi: 10.1007/s11010-009-0356-2. [DOI] [PubMed] [Google Scholar]
- 122.Dahm MM, Schubauer-Berigan MK, Evans DE, Birch ME, Bertke S, Beard JD, et al. Exposure assessments for a cross-sectional epidemiologic study of US carbon nanotube and nanofiber workers. Int J Hyg Environ Health. 2018;221(3):429–440. doi: 10.1016/j.ijheh.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 123.Fatkhutdinova LM, Khaliullin TO, Vasil'yeva OL, Zalyalov RR, Mustafin IG, Kisin ER, et al. Fibrosis biomarkers in workers exposed to MWCNTs. Toxicol Appl Pharmacol. 2016;299:125–131. doi: 10.1016/j.taap.2016.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhao X, Chang S, Long J, Li J, Li X, Cao Y. The toxicity of multi-walled carbon nanotubes (MWCNTs) to human endothelial cells: The influence of diameters of MWCNTs. Food Chem Toxicol : Int J Publish Bri Industr Biol Res Assoc. 2019;126:169–177. doi: 10.1016/j.fct.2019.02.026. [DOI] [PubMed] [Google Scholar]
- 125.Öner D, Ghosh M, Coorens R, Bové H, Moisse M, Lambrechts D, et al. Induction and recovery of CpG site specific methylation changes in human bronchial cells after long-term exposure to carbon nanotubes and asbestos. Environ Int. 2020;137:105530. doi: 10.1016/j.envint.2020.105530. [DOI] [PubMed] [Google Scholar]
- 126.Luanpitpong S, Wang L, Castranova V, Rojanasakul Y. Induction of stem-like cells with malignant properties by chronic exposure of human lung epithelial cells to single-walled carbon nanotubes. Part Fibre Toxicol. 2014;11:22. doi: 10.1186/1743-8977-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Shvedova AA, Yanamala N, Kisin ER, Khailullin TO, Birch ME, Fatkhutdinova LM. Integrated analysis of dysregulated ncRNA and mRNA expression profiles in humans exposed to carbon nanotubes. PLoS ONE. 2016;11(3):e0150628. doi: 10.1371/journal.pone.0150628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Domenech J, Hernández A, Demir E, Marcos R, Cortés C. Interactions of graphene oxide and graphene nanoplatelets with the in vitro Caco-2/HT29 model of intestinal barrier. Sci Rep. 2020;10(1):2793. doi: 10.1038/s41598-020-59755-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wang L, Stueckle TA, Mishra A, Derk R, Meighan T, Castranova V, et al. Neoplastic-like transformation effect of single-walled and multi-walled carbon nanotubes compared to asbestos on human lung small airway epithelial cells. Nanotoxicology. 2014;8(5):485–507. doi: 10.3109/17435390.2013.801089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Mukherjee SP, Gupta G, Klöditz K, Wang J, Rodrigues AF, Kostarelos K, et al. Next-generation sequencing reveals differential responses to acute versus long-term exposures to graphene oxide in human lung cells. Small. 2020;16(21):e1907686. doi: 10.1002/smll.201907686. [DOI] [PubMed] [Google Scholar]
- 131.Pérez RF, Soto Fernández AY, Bousquets Muñoz P, Sierra MI, Tejedor JR, Morales-Sánchez P, et al. No genome-wide DNA methylation changes found associated with medium-term reduced graphene oxide exposure in human lung epithelial cells. Epigenetics. 2020;15(3):283–293. doi: 10.1080/15592294.2019.1666650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Xu Y, Luo Z, Li S, Li W, Zhang X, Zuo YY, et al. Perturbation of the pulmonary surfactant monolayer by single-walled carbon nanotubes: a molecular dynamics study. Nanoscale. 2017;9(29):10193–10204. doi: 10.1039/C7NR00890B. [DOI] [PubMed] [Google Scholar]
- 133.Gasser M, Wick P, Clift MJD, Blank F, Diener L, Yan B, et al. Pulmonary surfactant coating of multi-walled carbon nanotubes (MWCNTs) influences their oxidative and pro-inflammatory potential in vitro. Part Fibre Toxicol. 2012;9:17. doi: 10.1186/1743-8977-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Di Cristo L, Grimaldi B, Catelani T, Vázquez E, Pompa PP, Sabella S. Repeated exposure to aerosolized graphene oxide mediates autophagy inhibition and inflammation in a three-dimensional human airway model. Materials Today Bio. 2020;6:100050. doi: 10.1016/j.mtbio.2020.100050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Chortarea S, Clift MJD, Vanhecke D, Endes C, Wick P, Petri-Fink A, et al. Repeated exposure to carbon nanotube-based aerosols does not affect the functional properties of a 3D human epithelial airway model. Nanotoxicology. 2015;9(8):983–993. doi: 10.3109/17435390.2014.993344. [DOI] [PubMed] [Google Scholar]
- 136.Sargent JF. Nanotechnology: a policy primer. Congres Res Serv. 2011;4(3/4):191–203. [Google Scholar]
- 137.Duschl A, Windgasse G. A survey on the state of nanosafety research in the European Union and the United States. J Nanoparticles Res. 2018;20(12):335. doi: 10.1007/s11051-018-4434-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.UNECA. Towards African nanotechnology future: trends, impacts and opportunities. Addis Ababa: United Nations. Economic Commission for Africa; 2020. Available from: https://archive.uneca.org/publications/towards-african-nanotechnology-future-trendsimpacts-and-opportunities.
- 139.Bayda S, Adeel M, Tuccinardi T, Cordani M, Rizzolio F. The history of nanoscience and nanotechnology: from chemical-physical applications to nanomedicine. Molecules. 2019;25(1):112. doi: 10.3390/molecules25010112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Huang Q, Yu H, Ru Q. Bioavailability and delivery of nutraceuticals using nanotechnology. J Food Sci. 2010;75(1):R50–R57. doi: 10.1111/j.1750-3841.2009.01457.x. [DOI] [PubMed] [Google Scholar]
- 141.Maiti D, Tong X, Mou X, Yang K. Carbon-based nanomaterials for biomedical applications: a recent study. Front Pharmacol. 2019;9:1401. doi: 10.3389/fphar.2018.01401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Pandey P, Dahiya M. A brief review on inorganic nanoparticles. J Crit Rev. 2016;3(3):18. [Google Scholar]
- 143.Lohse SE, Murphy CJ. Applications of colloidal inorganic nanoparticles: from medicine to energy. J Am Chem Soc. 2012;134(38):15607–15620. doi: 10.1021/ja307589n. [DOI] [PubMed] [Google Scholar]
- 144.Wang P, Lombi E, Zhao FJ, Kopittke PM. Nanotechnology: a new opportunity in plant sciences. Trends Plant Sci. 2016;21(8):699–712. doi: 10.1016/j.tplants.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 145.Bahadar H, Maqbool F, Niaz K, Abdollahi M. Toxicity of nanoparticles and an overview of current experimental models. Iran Biomed J. 2016;20(1):1–11. doi: 10.7508/ibj.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Baktur R, Patel H, Kwon S. Effect of exposure conditions on SWCNT-induced inflammatory response in human alveolar epithelial cells. Toxicol Vitro : Int J Published Assoc BIBRA. 2011;25(5):1153–1160. doi: 10.1016/j.tiv.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 147.Liu G, Gao J, Ai H, Chen X. Applications and potential toxicity of magnetic iron oxide nanoparticles. Small. 2013;9–10:1533–1545. doi: 10.1002/smll.201201531. [DOI] [PubMed] [Google Scholar]
- 148.Yao Y, Zhou Y, Liu L, Xu Y, Chen Q, Wang Y, et al. Nanoparticle-based drug delivery in cancer therapy and its role in overcoming drug resistance. Front Mol Biosci. 2020;7:193. doi: 10.3389/fmolb.2020.00193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Dadwal A, Baldi A, Narang RK. Nanoparticles as carriers for drug delivery in cancer. Artificial Cells, Nanomed Biotechnol. 2018;46(Sup2):295–305. doi: 10.1080/21691401.2018.1457039. [DOI] [PubMed] [Google Scholar]
- 150.Kermanizadeh A, Lohr M, Roursgaard M, Messner S, Gunness P, Kelm JM, et al. Hepatic toxicology following single and multiple exposure of engineered nanomaterials utilising a novel primary human 3D liver microtissue model. Part Fibre Toxicol. 2014;11:56. doi: 10.1186/s12989-014-0056-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Joris F, Valdepérez D, Pelaz B, Soenen SJ, Manshian BB, Parak WJ, et al. The impact of species and cell type on the nanosafety profile of iron oxide nanoparticles in neural cells. J Nanobiotechnol. 2016;14:69. doi: 10.1186/s12951-016-0220-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Wang Y, Chen S, Yan Z, Pei M. A prospect of cell immortalization combined with matrix microenvironmental optimization strategy for tissue engineering and regeneration. Cell Biosci. 2019;9:7. doi: 10.1186/s13578-018-0264-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Zhang S, Zhang X, Liu H, Qu W, Guan Z, Zeng Q, et al. Modifying effect of COMT gene polymorphism and a predictive role for proteomics analysis in children's intelligence in endemic fluorosis area in Tianjin, China. Toxicol Sci J Soc Toxicol. 2015;144(2):238–245. doi: 10.1093/toxsci/kfu311. [DOI] [PubMed] [Google Scholar]
- 154.Mukherjee SG, O’Claonadh N, Casey A, Chambers G. Comparative in vitro cytotoxicity study of silver nanoparticle on two mammalian cell lines. Toxicol In Vitro. 2012;26(2):238–251. doi: 10.1016/j.tiv.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 155.Ekstrand-Hammarström B, Akfur CM, Andersson PO, Lejon C, Österlund L, Bucht A. Human primary bronchial epithelial cells respond differently to titanium dioxide nanoparticles than the lung epithelial cell lines A549 and BEAS-2B. Nanotoxicology. 2011;6(6):623–634. doi: 10.3109/17435390.2011.598245. [DOI] [PubMed] [Google Scholar]
- 156.Kermanizadeh A, Pojana G, Gaiser BK, Birkedal R, Bilanicová D, Wallin H, et al. In vitro assessment of engineered nanomaterials using a hepatocyte cell line: cytotoxicity, pro-inflammatory cytokines and functional markers. Nanotoxicology. 2013;7(3):301–313. doi: 10.3109/17435390.2011.653416. [DOI] [PubMed] [Google Scholar]
- 157.Bundschuh M, Filser J, Lüderwald S, McKee MS, Metreveli G, Schaumann GE, et al. Nanoparticles in the environment: where do we come from, where do we go to? Environ Sci Eur. 2018;30(1):6. doi: 10.1186/s12302-018-0132-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Tolaymat T, Genaidy A, Abdelraheem W, Dionysiou D, Andersen C. The effects of metallic engineered nanoparticles upon plant systems: An analytic examination of scientific evidence. Sci Total Environ. 2017;579(1):93–106. doi: 10.1016/j.scitotenv.2016.10.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Keller AA, McFerran S, Lazareva A, Suh S. Global life cycle releases of engineered nanomaterials. J Nanopart Res. 2013;15:1692. doi: 10.1007/s11051-013-1692-4. [DOI] [Google Scholar]
- 160.Gottschalka F, Nowack B. The release of engineered nanomaterials to the environment. J Environ Monitor. 2011;13:1145–1155. doi: 10.1039/c0em00547a. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. MEDLINE Search History.
Data Availability Statement
All data generated or analysed during this study are included in this published article and in the presented supplementary material file.