Abstract
Congenital anomalies are distressing events for future parents/parents when a foetal anomaly is detected during pregnancy or when the infant is born with a disability or a congenital disorder. Maternal health services in India do not provide information on these disorders as part of routine activities. The objective is to understand women's knowledge and attitude on causes, prevention, rights; attituted towards disability; and knowledge on medical care, rehabilitation, and welfare services in Pune district, India, with the goal of identifying the contents of birth defects education resources. The study used a qualitative descriptive design. Six focus group discussions were conducted with 24 women from Pune district. Qualitative content analysis was used to identify emergent themes. Three themes emerged. Firstly, women’s knowledge on congenital anomalies was limited. These conditions were discussed generally with other adverse pregnancy experiences, and with reference to children with disabilities. Secondly, pregnancy termination for conditions considered untreatable was majorly advocated by most women. Directive counselling for pregnancy termination by doctors was common. Thirdly, stigmatizing attitudes were responsible for children with disabilities being considered a burden, for maternal blaming, and for the stigma and isolation of families. Knowledge on rehabilitation was limited. The study identified that participants. Three target groups and contents for birth defects education were identified. Women’s resources should include knowledge on preconception and antenatal opportunities for reducing risks, available medical care, and legal rights. Parents’ resources should provide information on treatment, rehabilitation, legal provisions, and rights of disabled children. Resources for the general community should additionally include disability sensitization messages to ensure the inclusion of children with congenital disabilities.
Supplementary information
The online version contains supplementary material available at 10.1007/s12687-023-00654-y.
Keywords: Congenital anomalies, Disability, Children, Maternal health services, India, Qualitative research
Introduction
Congenital anomalies (congenital malformations, birth defects) include common disabling childhood conditions like congenital heart defects (CHD), orofacial clefts (OFC), congenital talipes equinovarus (CTEV) or clubfoot, developmental dysplasia of the hip (DDH), and neural tube defects (NTD). While several common disorders can be corrected, a lack of services results in disability, progressive medical complications, and higher than normal usage of health (Arth et al. 2017), rehabilitation, and social welfare services (Kamenov et al. 2019; Shooshtari et al. 2017). Congenital anomalies cause distress when women are confronted with the diagnosis of a foetal anomaly during pregnancy, a stillbirth, or a premature born infant with a malformation. Global estimates indicate that congenital anomalies are the third largest cause of neonatal deaths (Perin et al. 2022). Prevention, a major public health function, is challenged by limited specific interventions as the causes of the majority of congenital anomalies are not determined (Taruscio et al. 2015). Preconception folic acid supplementation and rubella immunization are two possible available specific protection measures. Secondary prevention, that is, detection of a foetal anomaly followed by pregnancy termination (Termination of Pregnancy for Foetal Anomaly, ToPFA), remains an ethically difficult but common strategy for severe congenital anomalies in some places like India. Tertiary prevention, that is, medical treatment, can correct disability among survivors, and physical and social rehabilitation can improve the quality of life of children and caregivers.
Congenital anomalies are under-prioritized in maternal and child health services of low- and middle-income countries (LMIC) (Darmstadt et al. 2016) where healthcare is not universal and assured to all. The focus of global agendas like the Sustainable Development Goal 3 is to prioritize activities to reduce preventable child mortality. Childhood disability remains under-recognized, and services are fragmented.
The need to prioritize congenital anomalies is especially urgent in India, which has an annual birth cohort of 25 million. Estimates suggest that congenital anomaly birth prevalence in the country ranges from 184.48 (95% CI 164.74–204.21) to 230.51 (95%CI 170.99–310.11) per 10,000 live births, accounting for 472,177 to 530,208 affected pregnancies annually (Bhide et al. 2016; Bhide and Kar 2018; Kar and Ujagare 2021). Global Burden of Disease data indicate that 16% of global neonatal deaths caused by congenital anomalies occur in India (Ujagare and Kar 2021). Global child mortality trends (Liu et al. 2019; Fadel et al. 2017) and data on child mortality at the sub-national level in India (Dandona et al. 2020) identify changes in the cause composition of neonatal deaths and an increase in congenital anomaly mortality in several parts of the country. A nationwide disability survey identified that 30% of people with disabilities in India (about 7.74 million) reported disability since birth (Ministry of Statistics and Programme Implementation 2018). These data are indicative of the invisible magnitude of congenital anomalies and congenital disabilities in India.
Maternal and child health services in India do not include awareness messages on congenital anomalies. This increases individual responsibility in adopting preventive measures, taking informed decisions in case of prenatal detection of a foetal malformation, and being empowered to access appropriate treatment and rehabilitation services. The purpose of this study was to understand women’s knowledge and attitudes on congenital anomalies, sources of knowledge, local language words to refer to these conditions, understanding of causation and prevention, knowledge about legal provisions for termination of malformation-affected pregnancies, knowledge on availability of medical care and rehabilitation therapies, and attitudes towards children with disabilities. The underlying purpose was to use the evidence from this study to develop a birth defects education resource.
The limited number of studies that have reported women’s knowledge on congenital anomalies from (LMIC) have used quantitative methods (Unusan 2004; Bello et al. 2013; Lawal et al. 2015; De Silva et al. 2019). Quantitative methods may not truly capture women’s understanding of these conditions. This study used a qualitative approach, which permits a deeper understanding of awareness, opinions, perspectives, and understanding of phenomena.
Methods
Study design and setting
The study used a qualitative descriptive approach, which has been used in healthcare and nursing studies to uncover poorly understood phenomenon (Kim et al. 2017). Unlike other types of qualitative methods, qualitative descriptions are not necessarily anchored in a theory, but are used to provide a clear-cut description of an inadequately characterized phenomenon. In health and nursing studies, qualitative description provides useful information for the development of interventions or for refining questionnaires (Kim et al. 2017). The study used focus group discussion (FGD) (Wong 2008), which is a type of group discussion about a topic under the guidance of a trained moderator. The FGD uncovers people’s understanding, perceptions, and values. The study was conducted in Pune city and Talegaon Dhamdhere, a village 40 km from the city, located in Pune district. The study settings were selected based on the convenience of the researchers. The Consolidated Criteria for Reporting Qualitative Research (COREQ) (Tong et al. 2007) was used during reporting of this study (Supplementary Table 1).
Recruitment and sampling
A purposive sample of women were invited through an audio-video recording, that was widely shared via social messaging groups of colleagues, friends, and relatives. The audio-video presentation was in Marathi language and provided details about the research organization, the researchers, the purpose of the study, the role of the participant, eligibility criteria, and issues relating to confidentiality. Eligibility for inclusion was women of age less than 45 years, having one or more living child/children without a congenital disorder or a disability, not reporting a history of prenatal detection of a congenital malformation, having a telephone, being familiar with the use of social messaging, and being conversant in the local language (Marathi). In order to ensure diversity, both rural and urban women were included in the study. Thirteen rural women expressed interest, of whom twelve consented to participate. Among the 16 urban women who initially expressed interest, twelve participated in the FGD. The reason for non-participation was scheduling difficulties. Each woman was telephoned to establish rapport, re-explain the study and the process of FGD, obtain informed consent, answer any queries or concerns, and schedule the date and time for the discussion. The latter required contacting and adjusting the timing, providing an opportunity for further rapport establishment. A set of questions was used to collect demographic data from participants at this time. The women were informed that there were no financial incentives for participation, but that their views would be used to design educational material for women considering pregnancy.
Data collection
FGDs were conducted by two female researchers (DiD and AM) who were trained in qualitative research and were fluent in Marathi and English. None of the urban women knew each other, but some rural women discovered common acquaintances during the group discussion. FDGs were conducted in spaces with assured privacy, and were guided by a topic guide (Table 1). This guide was developed on the basis of general literature on congenital anomalies and the field experiences of the researchers. It investigated (1) familiarity with these conditions, their causes, knowledge about prevention, and the local language term for birth defects; (2) awareness about available options for detection of a foetal anomaly; and (3) awareness about available services in case of an affected birth, including attitudes towards disabled children. The topic guide was refined through two pilot discussions with an independent group that consisted of clinicians and women who shared the same eligibility characteristics. The term ‘birth defects’ (janmajata apangatva) was used in both the audio-visual presentation and while introducing the group discussion. Brief examples of orofacial clefts (a child born with a cut lip), congenital heart defects (a hole in the heart), or congenital malformations that affected pregnancies were provided to introduce women to the topic. The researchers used probing and engaged with all participants in order to ensure that all opinions were included. Each FDG ranged from 1 and a half to 2 h. All discussions were recorded. Field notes were made immediately after the interview. The within-method of data triangulation was done by informal discussions with participants to clarify and validate the data obtained from the analysis.
Table 1.
Topic guide
| - Knowledge about congenital anomalies, sources of knowledge, and the local language term for congenital anomalies |
| - Knowledge about the causes and prevention of congenital anomalies |
| - Knowledge about legal options and opinions on termination of pregnancy for a foetal anomaly |
| - Knowledge on treatment and rehabilitation, including available government schemes |
| - Impact on mother, the support needs of families with a child with a disability, and attitudes towards children with disabilities |
Data analysis
Qualitative content analysis, using an inductive thematic approach, was used to understand the data (Forman and Damschroder 2007; Vaismoradi et al. 2016). The interviews were transcribed and translated by one author (AM or DiD) and the translations were checked by another author (AK). After the finalization of translations, the interviews were independently coded by all three researchers. Both a priori and inductive coding were used in the analysis of each FGD. Codes were reconciled, and a codebook was created. The interviews were revisited, and sub-themes and themes were evolved from the codes, which were then analyzed in context with the research questions.
Ethics
The study was approved by the Institutional Ethics Committee. Participants were women who were not pregnant at the time of the FDG, and did not have a child with a congenital anomaly or a disability, and did not report a history of prenatal diagnosis of a congenital malformation. Participants were invited to the FDG only after obtaining written informed consent, which included consent to record the interview.
Results
Demographic characteristics of participants
Twenty-four women participated in the FGD. Urban women were more educated, and several were employed (Table 2). Rural women were homemakers with lower education levels.
Table 2.
Demographic details
| FGD* | Respondent | Age | Education (degree/years of education) | Number of children | Current occupation |
|---|---|---|---|---|---|
| FGD1 | U1 | 36 | Post-graduate | 2 | Homemaker |
| FGD1 | U2 | 37 |
Double post-graduate |
2 | Homemaker |
| FGD1 | U3 | 38 | Post-graduate | 2 | Homemaker |
| FGD1 | U4 | 27 | Under-graduate degree in engineering | 1 | Software engineer |
| FGD2 | U5 | 30 | Under-graduate | 1 | Self-employed |
| FGD2 | U6 | 36 | High school | 1 | Employed |
| FGD2 | U7 | 37 | Under-graduate degree in engineering | 1 | Employed |
| FGD2 | U8 | 33 | Post-graduate degree computer application | 2 | Employed |
| FGD3 | U9 | 35 | Post-graduate degree in business administration | 1 | Employed |
| FGD3 | U10 | 35 | PhD | 1 | Teacher |
| FGD3 | U11 | 38 | Under-graduate | 2 | Homemaker |
| FGD3 | U12 | 35 | 10 years | 2 | Self-employed |
| FGD4 | R13 | 35 | 10 years | 2 | Homemaker |
| FGD4 | R14 | 33 | 12 years | 2 | Homemaker |
| FGD4 | R15 | 35 | 12 years | 3 | Homemaker |
| FGD4 | R16 | 26 | 1 year of college education | 2 | Homemaker |
| FGD5 | R17 | 34 | 10 years | 2 | Homemaker |
| FGD5 | R18 | 30 | 1 year of college education | 2 | Homemaker |
| FGD5 | R19 | 26 | 12 years | 2 | Homemaker |
| FGD5 | R20 | 25 | One year of college education | 1 | Homemaker |
| FGD6 | R21 | 30 | 12 years (+ 1 year nursing course) | 2 | Homemaker |
| FGD6 | R22 | 36 | 10 years | 2 | Homemaker |
| FGD6 | R23 | 39 | 12 years | 3 | Homemaker |
| FGD6 | R24 | 38 | 8 years | 2 | Farm labourer |
*FGD1–3 were discussions with urban women, and FGD4–6 were discussions with rural women
Knowledge on congenital anomalies
The analysis revealed three overarching themes: (1) limited knowledge on congenital anomalies, (2) termination of pregnancy was suggested for all conditions considered to be untreatable, and (3) children with disabilities were viewed as a burden.
Theme 1. Knowledge on congenital anomalies
Subtheme 1.1: Congenital anomalies were considered one of several adverse pregnancy outcomes
Women were familiar with the Marathi language equivalent of ‘congenital’ (janmajat), but required probing to recall specific examples of congenital anomalies. Sixty-one different conditions were discussed as congenital anomalies, which included lay descriptions of different anomalies, examples of maternal pregnancy complications, other adverse outcomes (miscarriage, foetal demise), and descriptions of children with congenital and acquired disabilities and developmental disabilities (DD) (Supplementary Table 2). Sources of knowledge were unclear, but direct or indirect experiences of relatives, neighbours, and friends were mentioned (Supplementary Table 2). Rural participants additionally mentioned receiving information from health programs on television. Only two urban women who had experienced pregnancy complications reported receiving information on congenital anomalies from healthcare professionals during pregnancy.
Subtheme 1.2: Knowledge of causation and prevention was limited
There was some knowledge on causation, but this was discussed in the context of general pregnancy practices like good nutrition during pregnancy, a supportive environment, and respect for women during pregnancy (Table 3). Nearly all women mentioned marriage among relatives and self-medication as causes. Other factors mentioned were family history of a birth defect, maternal general health status, maternal mental health, need for respect during pregnancy, supportive family environment, one mention of anxiety about COVID-19 during pregnancy, physical exposures (specifically chemical and pesticides in food), poor diet during pregnancy (including ‘hybrid’ food implying inferior nutrient content), falling during pregnancy, assisted reproductive methods, abortion medication, alcohol consumption, and repeated use of ultrasound during pregnancy (Table 3).
Table 3.
Women’s opinion on causes of congenital anomalies
| Causes of congenital anomalies | |
|---|---|
| Heredity | “People say the culprit of this condition is heredity and the tablets and tonics that were taken during pregnancy” #R13, FGD4 |
| Consanguineous marriages | “You will also see a lot of congenital anomalies in endogamous marriages in south India. It’s not uncommon to see a lot of albino’s, people who are blind or have deformities in their extremities” #U2, FGD1 |
| Medicines | “Taking medicine for headache causes the child to become handicapped” #R14, FGD4 |
| “For abortion, she took pills in one, one and a half months. But that was not aborted, means they did sonography, but nothing was told to them (that is, unsuccessful abortion).” #R16, FGD4 | |
| Maternal health, diet, environment | “Sometimes mothers become anaemic due to low blood, also if you don’t get proper sunlight then for the first month the baby will be yellowish in colour” #U10, FGD3 |
| “Food quality is not good because of all the hybrid food and the pesticides that are used” #U9, FGD3 | |
| “Endosulfan was sprayed on trees. That caused many birth defects” #U10, FGD3 | |
| “The lifestyle, that is daily chores at home, office, everyday exertion, the surrounding environment, work related stress, all these things (cause) a lot of mental stress” # U7, FGD2 | |
| Fall | “So may be when she falls down, the disability happens” #U9,FGD3 |
| Ultrasonography | “Nowadays doctors ask us to do more sonography. Due to that diseases of uterus and abortion, or child is born defected” #R23, FGD6 |
| Beliefs | “I have heard that the family is cursed because for past three to four generations a boy or girl is born normal, but later develops some psychological problems” #U1, FGD1 |
| “Elderly people tell us not to go out after 6–7 pm, especially pregnant ladies” #U6, FGD2 | |
| “No, God never does bad things to anyone. Whatever it is, it belongs to what we do” #R17, FGD5 | |
| “We should hear good things, say good things, pray to God. We don’t follow this and they are the reasons” #U10, FGD3 | |
| Alcohol | “My mother assumes that because my dad was an alcoholic when she was pregnant, that’s what caused it (fused, low lying kidneys with short ureter) but I have no idea, honestly”. #U2, FGD1 |
| Assisted reproduction | “it was a IVF baby” #U1, FGD1 |
Subtheme 1.3: Lay beliefs predominated views on causation
Lay beliefs predominated understanding of causation. The association between maternal activities during an eclipse and congenital anomalies like ‘cut lips’, ‘crooked legs’, or a missing body part was mentioned by all women. Rural women mentioned God’s will and destiny.
How God decides, it happens. It is part of everyone’s destiny (Participant R21, FGD6).
Karma (the consequences of one’s deeds) was mentioned.
The (intellectually impaired) son …. knocks on the door continuously, and when he is hungry, he gives the bowl. When asked, the Brahman (religious man) said these are fruits of our past karma (Participant R23, FGD6).
Past sins were also cited as causes of congenital anomalies.
Then he says (father of a child with a severe disability), what sins have I done? No one does any sin. It is the effect of sins in a previous life (Participant R23, FGD6).
The majority of participants were undecided about the truth behind these beliefs, but were hesitant to not follow these practices, in fear of an adverse outcome.
Beliefs are carried on from generation to generation. We can’t do anything about it (Participant U4, FGD1).
The two urban participants who had pregnancy complications mentioned prenatal tests (quadruple marker test, genetic tests), and a rural woman mentioned “colour Doppler” tests. The risks of repeated ultrasound as a cause of congenital anomalies were stated by both urban and rural women.
Sometimes, by exposure to X-rays (ultrasound), the child can be born mentally retarded. So, it depends on one’s destiny, how much to take advantage of, and how much to lose (Participant R23, FGD6).
Several participants believed that by requesting multiple ultrasonographic examinations, medical professionals were responsible for causing congenital anomalies. There was no mention of preconception care, use of folic acid supplementation, or rubella immunization. Several women were of the opinion that these conditions could not be prevented.
Whenever such a child is born, is it in anyone’s hands? (Participant R23, FGD6).
Theme 2. Values on termination of pregnancy
Discontinuation of an affected pregnancy was strongly advocated by majority of participants.
Subtheme 2.1: Decision to advocate for abortion was dependent on whether the condition was treatable or not
Participants had a positive opinion/attitude on termination of pregnancy when the child had an untreatable condition. According to participants, the decision to terminate a pregnancy would be dependent on whether the condition could be treated or not, on the financial status of the family, and on the doctor’s advice. The term untreatable implied any condition that would lead to the birth of a child with a disability.
If there is defect in the legs, and if that is going to be alright after treatment, then (gestures indicating pregnancy should be continued). But if the child is blind, or not mentally developed, then in such situations, there is no point in giving birth to such a child. Abortion will be the correct advice in that situation (Participant R17, FGD5).
The decision to recommend discontinuation of the pregnancy was based on the belief that a child with a disability was a lifelong burden.
A disability is a disability. If the baby is born, the baby will also face a lot of difficulties in surviving. It is a crime, abortion, we shouldn’t do that or tell someone to do it. But still, in my personal opinion, I think if in the beginning we come to know, we should not bring the baby to the world to make him or her suffer (Participant U10, FGD3).
Termination of pregnancy was also justified as it would prevent maternal emotional distress (there will be a lot of mental pressure throughout her life, Participant U1, FGD1) and maternal blaming.
Everyone will blame the woman…. What the baby wants--nobody is going to be involved. They will only blame the mother, who will be doing all the work (of caregiving) (Participant U8, FGD2).
Another reason that was cited was that there was a lack of knowledge about raising a child with a disability, so that discontinuation of the pregnancy would be a more convenient decision.
We don’t have the information available to treat them, how they grow, how to take care. You can’t just give birth and leave them. You have to raise the child; he is going to grow, so what to do about it…. the entire family should think about this (Participant U2, FGD1).
Most participants believed that the decision to terminate or continue the pregnancy should rest with the mother, although one group of participants believed that it was necessary to involve the whole family in the decision. There was a minority view that abortion was wrong.
But mistakes are also God’s creation, good or bad, is it in our hands? This (child) is given to us for taking care (Participant R23, FGD6).
Subtheme 2.2: Limited knowledge on legal provision for ToPFA
There was limited knowledge on legal provisions for ToPFA. Due to highly publicized advertisements on the penalties for sex-selective abortion in India, women were aware that there was a legal gestation limit beyond which discontinuation of a pregnancy was not permitted. However, none of the participants was aware that there were special legal provisions for ToPFA. Lack of such knowledge was the source of apprehension among participants in one group as the FGD was being recorded.
Participant R23: “That covering, or shield (of the skull) was not there. They got to know in the 5th month, and they did the abortion in the 6th month. It was a baby boy”
Participant R22: “That is not good, knowing the sex of the child, whether a girl or boy. Will there be any legal problems for us?” (pointing at the recorder, FGD6).
Subtheme 2.3: Directive counselling for pregnancy termination by medical professionals
Directive counselling by medical professionals appeared to be commonplace.
When I was three months pregnant, one doctor directly told me, if you are thinking about abortion, only then come to me, otherwise, don’t (Participant U8, FGD2, participant with diabetes).
Parents’ decisions appeared to be of little consequence.
His ureter and anus were not developed, and doctor told them from the sonography report that there was a problem, so, don’t go for the baby, do an abortion. But she did not want to do the abortion. (At the time of delivery) after seeing all those reports, xxx hospital was not ready to admit her as they (parents/family) had already been told (to not continue the pregnancy), as the baby would not survive. The baby died after five days (Participant R16, FGD4).
Several participants stated that they would follow their doctor’s advice, but not all participants were willing to accept directive counselling.
All those doctors… the way they treated me …. I feel like going and showing them, look, this is my (healthy) baby. In our family, we were assertive. But suppose a family takes this decision (to terminate the pregnancy) because of the advice given by doctors? (Participant U8, FGD2, diabetic woman, directed not to continue the pregnancy).
Theme 3. Impact of living with a child with a disability
Subtheme 3.1: Stigmatizing attitudes towards children with disabilities
Children with disabilities were viewed as a burden. Some participants believed that a child with a disability had to be accepted. Shared caregiving (‘His grandmother sits with him. Yes, someone is always there for him’, Participant R14, FGD4) was mentioned by several participants. Inclusion of children in social activities was also cited. The majority opinion was, however, that a child with a disability would be ‘trouble’ for the family. ‘Investment’ in terms of treatment and special schooling was questioned, as several participants believed that there was likely to be little improvement even after treatment (‘exactly why invest in something like this?’, Participant U2, FGD1). Stigmatizing attitudes towards children with disabilities were apparent, as they were perceived to be aesthetically displeasing.
People passing by would look at him with revulsion, look how he is drooling, look at his hands and legs (Participant U7, FGD2).
They were also perceived as being dangerous.
These children, who are not bed ridden, are very aggressive (Participant U12, FGD3).
Another stigmatizing attitude was pity for the mother and the family.
I really pity them and pray that this should not happen to any mother (Participant U1, FGD1).
Stigmatizing attitudes were cited as being responsible for the isolation of disabled children and their families. Examples were a child not being brought out of his room for 19–20 years (Participant U1, FGD1), and parents feeling ashamed to present the child in public.
They don’t take him anywhere. They say they can’t take him, but I think there is a certain degree of - what other people will say” (Participant U2, FGD1).
The extreme consequences of stigma were evident from the description of the death by suicide of a family of a child with congenital hearing impairment, who were distant relatives of a participant (Punekar News 2021).
People from their village and surrounding areas would say, you are a doctor, and you can’t cure your (hearing impaired) child? He (the doctor who died by suicide) said (in a suicide note) we know it is wrong, but we are not able to tolerate our son’s insult (Participant R23, FGD6).
Subtheme 3.2: Limited knowledge on medical options and rehabilitation
Knowledge about treatment and rehabilitation for children with congenital anomalies was minimal. Surgery for congenital heart defects, club foot, and orofacial clefts was mentioned by women who had relatives or neighbours with these conditions. While it was believed that surgery could cure the defect, there was also the opinion that some conditions could not be treated.
There are conditions when there is no treatment even though a person has money (Participant R14, FGD4).
There was significantly more knowledge about government medical and disability services among rural women (free medical services, financial assistance for people with disabilities, assistive devices like three-wheeled cycles for children with locomotor disabilities, hearing aids for hearing impaired children, reservations in employment, and special schools). Women’s knowledge on rehabilitation was obtained through interaction with the families of persons with disabilities and from community-based health and social welfare service information sources.
Several participants felt strongly that rehabilitation, including special schooling, must be provided to children with disabilities. There was mention of several instances of encouraging children with disabilities to be independent, for example by selling incense sticks in the neighbourhood. Most participants agreed that the decision to provide rehabilitation therapy and special schooling would depend on the family’s awareness of these services and its financial situation. The perceived benefits of providing rehabilitation care were also cited as influencing the decision to provide therapies.
If there is not going to be any income from this child, then they will think, let the child be as it was born, let him be at home, they are not going to get any returns (Participant U1, FGD1).
Rehabilitation of children with disabilities was reported to be difficult, as participants cited instances where special schools expressed their inability to manage children with special needs. (These children disturb children who are getting better. So, the school said take your child home, Participant R17, FGD5).
Other reasons cited for discontinuation of special education were the parental perception that there was no improvement in the child, difficulty in transporting the disabled child, or due to parental concerns that children were not properly cared for at school (Participant R17, FGD5).
Discussion
Main findings
The findings of this study identify that there was limited knowledge on congenital anomalies, their causation, and prevention. Common conditions were recalled only after probing, and discussed with other adverse pregnancy outcomes like miscarriage, stillbirths, premature birth, or the birth of a child with a disability. Lay beliefs, such as the association between maternal practices during an eclipse and congenital anomalies, a well-documented phenomenon in ethnocultural studies on congenital anomalies (Cohen et al. 1998) was widespread. Strikingly, there was no mention of preconception folic acid supplementation, the most effective measure for prevention of folate-susceptible NTDs. There was widespread advocacy for ToPFA. Without a clear understanding on congenital anomalies, this recommendation also included any condition considered to be untreatable. This was because childhood disability was viewed as a burden, that imposed additional maternal caregiving activities, maternal blaming, and a financial burden on families. Stigmatizing attitudes towards children with disabilities were evident. Knowledge about medical care, rehabilitation, and early intervention services was minimal. There was limited knowledge on women’s rights to ToPFA (Ministry of Law 2021).
There were some differences between urban and rural women. In contrast to urban women, rural women could provide more descriptions of pregnancy complications (including congenital anomalies) and disabilities from larger social networks of friends, neighbours, and close and distant relatives. They were better informed about government maternal and child health and disability schemes due to the visits by community health workers. Rural women were unable to use medical terms but could give verbatim descriptions of what was mentioned by the doctor. Urban women used medical terminologies and looked up pregnancy-related information on the internet. More superstitions or misconceptions were identified among rural women. Urban women used more disability-sensitive terminologies as compared to rural women.
A recent European study investigated parental experiences of having a child with a congenital anomaly (Holm et al.2021). Unlike India, European parents are assured access to high cost medical services like surgery for congenital heart defects or cleft palate. Despite availability of services, maternal experiences of guilt and blame, stigmatizing attitudes, difficulty in negotiating access to welfare support were identified, which was comparable to the findings of our study. However, unlike our study, European parents welcomed the birth of the child (Holm et al.2021), as they were prepared by a supportive information and counselling services. This key finding underlines the need for developing educational resources on birth defects.
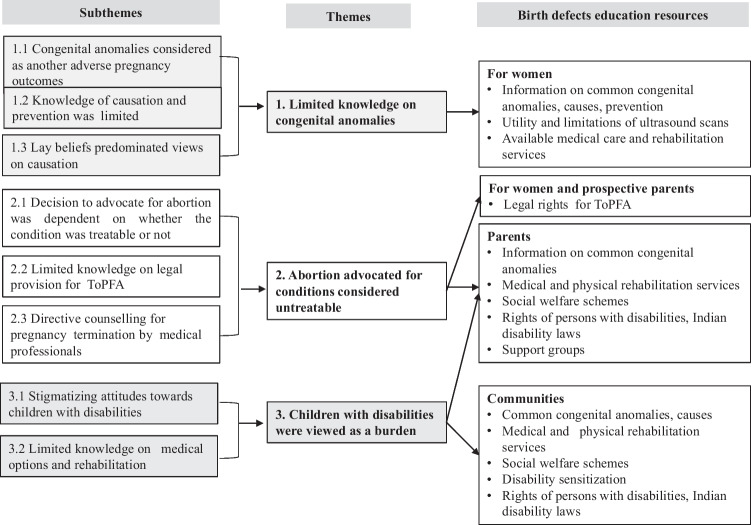
Implications for practice
The data from this study can be mapped to frame a conceptual framework that utilizes the sub-themes and themes to identify the target audience, content, and timing of birth defects education. As depicted in Fig. 1, women need to be the primary targets, with information on common congenital anomalies, their causes and prevention, the utility and limitations of ultrasound scans, and the legal rights to decide about discontinuation of a pregnancy diagnosed with a foetal malformation. For women, in addition to the contents, the timing of delivering the information is important. Enhancing awareness in the preconception period provides the opportunity to treat/manage existing risk factors, practice healthy behaviours (Atrash and Jack 2020), and also learn about the causes, risk factors, and methods of prevention of adverse maternal and foetal outcomes. Preconception education on pregnancy complications becomes advantageous for obstetricians, as it makes it less difficult to break the bad news of an adverse event (Greiner and Conklin 2015).
Fig. 1.
Conceptual framework to inform target audience and contents of birth defects education
The findings of the study identified that while women are the primary targets of birth defects education, two other groups need to be targeted. The second target for birth defects awareness is prospective parents and parents, as there was limited knowledge on available options after prenatal diagnosis of a malformation and legal provisions for ToPFA. Such information is imperative to ensure independence in decision making, as participants cited several instances of directive counselling. Parents’ resources should provide information about medical and early intervention services, government social welfare schemes for children born with disabilities, and the rights of children and adults with disabilities. In India, different services are already in place, but there is no centralized information source and the services are not connected through clearly defined referral pathways (Kar 2021a).
The study identified the need for a birth defects awareness for general communities, as stigmatizing attitudes were evident (Kar 2021b). Information for communities should aim at disability sensitization, highlighting the capabilities and rights of people with disabilities, as well as providing information on congenital anomalies and their causes to prevent maternal blaming. Information for all these three groups of target audiences can be packaged into a larger ‘birth defects education’ resource within the maternal and child health service.
Limitations
We acknowledge the limitations of the study. The findings are based on a small group of urban and rural women from Pune district. Like all qualitative studies, the findings from this study may not be applicable to other areas. Furthermore, the views expressed by the participants may reflect their own attitudes towards women with an unsuccessful pregnancy or a child with a disability.
Conclusions
The observations from this study underline the need for birth defects services. It identified the content and target audience for birth defects education that can build on, correct, and clarify knowledge on common congenital anomalies, their causation, prevention, and care. The study identified the need for resources for prospective parents and parents, as well as resources for communities, so that they are equipped with correct information on available choices, medical care, rehabilitation, and the rights of children with disabilities.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We acknowledge the participants in the FGDs, the informants in the pilot studies, Aarti Nagarkar, Supriya Phadnis, Charuta Gokhale, and especially Prajkta Bhide for comments on the manuscript.
Author contribution
AK conceived and designed the study, supervised data collection, verified translation, conducted data analysis, and wrote the manuscript. AM and DD participated in developing the objectives and methodology, conducted the focus group discussions, transcribed, translated and coded the data, and commented and added to the analysis and manuscript drafts.
Data availability
Available on request.
Declarations
Ethics approval
Granted by Institutional Ethics Committee.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dipali Dhamdhere and Aishwarya Medhekar contributed equally to the study.
References
- Arth AC, Tinker SC, Simeone RM, Ailes EC, Cragan JD, Grosse SD. Inpatient hospitalization costs associated with congenital anomalies among persons of all ages—United States, 2013. Morb Mortal Wkly Rep. 2017;66:41–46. doi: 10.15585/mmwr.mm6602a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atrash H, Jack B. Preconception care to improve pregnancy outcomes: clinical practice guidelines. J Human Growth Dev. 2020;30:407–416. doi: 10.7322/jhgd.v30.11075. [DOI] [Google Scholar]
- Bello AI, Acquah AA, Quartey JN, Hughton A. Knowledge of pregnant women about congenital anomalies. BMC Pregnancy Childbirth. 2013;13:1–7. doi: 10.1186/1471-2393-13-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhide P, Kar A. A national estimate of the birth prevalence of congenital anomalies in India: systematic review and meta-analysis. BMC Pediatr. 2018;18:175. doi: 10.1186/s12887-018-1149-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhide P, Gund P, Kar A. Prevalence of congenital anomalies in an Indian maternal cohort: healthcare, prevention, and surveillance implications. PLoS ONE. 2016;11:e0166408. doi: 10.1371/journal.pone.0166408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen LH, Fine BA, Pergament E. An assessment of ethnocultural beliefs regarding the causes of congenital anomalies and genetic disorders. J Genet Couns. 1998;7:15–29. doi: 10.1023/A:1022812027511. [DOI] [PubMed] [Google Scholar]
- Dandona R, Kumar GA, Henry NJ, Joshua V, Ramji S, Gupta SS, et al. Subnational mapping of under-5 and neonatal mortality trends in India: The Global Burden of Disease Study 2000–17. The Lancet. 2020;395:1640–1658. doi: 10.1016/S0140-6736(20)30471-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darmstadt GL, Howson CP, Walraven G, Armstrong RW, Blencowe HK, Christianson AL, et al. Prevention of congenital disorders and care of affected children: a consensus statement. JAMA Pediatr. 2016;170:790–793. doi: 10.1001/jamapediatrics.2016.0388. [DOI] [PubMed] [Google Scholar]
- De Silva J, Amarasena S, Jayaratne K, Perera B. Correlates of knowledge on congenital anomalies and associated factors among antenatal mothers in Galle, Sri Lanka: a cross-sectional analytical study. BMC Pregnancy Childbirth. 2019;19:1–9. doi: 10.1186/s12884-018-2163-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fadel SA, Rasaily R, Awasthi S, Begum R, Black RE, Gelband H, et al. Changes in cause-specific neonatal and 1–59-month child mortality in India from 2000 to 2015: a nationally representative survey. The Lancet. 2017;390:1972–1980. doi: 10.1016/S0140-6736(17)32162-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman J, Damschroder L (2007) Qualitative content analysis. In Empirical methods for bioethics: a primer (Vol. 11, pp. 39–62). Emerald Group Publishing Limited
- Greiner AL, Conklin J. Breaking bad news to a pregnant woman with a fetal abnormality on ultrasound. Obstet Gynecol Surv. 2015;70:39–44. doi: 10.1097/OGX.0000000000000149. [DOI] [PubMed] [Google Scholar]
- Holm KG, Neville AJ, Pierini A, Latos Bielenska A, Jamry-Dziurla A, Cavero-Carbonell C, et al. The voice of parents of children with a congenital anomaly–a EUROlinkCAT study. Front Pediatr. 2021;29(9):654883. doi: 10.3389/fped.2021.654883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamenov K, Mills J-A, Chatterji S, Cieza A. Needs and unmet needs for rehabilitation services: a scoping review. Disabil Rehabil. 2019;41:1227–1237. doi: 10.1080/09638288.2017.1422036. [DOI] [PubMed] [Google Scholar]
- Kar A. Birth defects in India. Singapore: Springer; 2021. Medical, rehabilitation and social welfare services for children with birth defects and developmental disabilities in India; pp. 275–296. [Google Scholar]
- Kar A. Birth defects in India. Singapore: Springer; 2021. Birth defects stigma; pp. 317–333. [Google Scholar]
- Kar A, Ujagare D. Birth defects in India. Singapore: Springer; 2021. Magnitude of congenital anomalies in India; pp. 143–167. [Google Scholar]
- Kim H, Sefcik JS, Bradway C. Characteristics of qualitative descriptive studies: a systematic review. Res Nurs Health. 2017;40:23–42. doi: 10.1002/nur.21768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawal TA, Yusuf B, Fatiregun AA. Knowledge of congenital anomalies among nursing mothers in a developing country. Afr Health Sci. 2015;15:180–187. doi: 10.4314/ahs.v15i1.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, Chu Y, Oza S, Hogan D, Perin J, Bassani DG, et al. National, regional, and state-level all-cause and cause-specific under-5 mortality in India in 2000–15: a systematic analysis with implications for the Sustainable Development Goals. Lancet Glob Health. 2019;7:e721–e734. doi: 10.1016/S2214-109X(19)30080-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Law and Justice (Legislative Department) (2021) The Medical Termination of Pregnancy (Amendment) Act, 2021 Available at https://egazette.nic.in/WriteReadData/2021/226130.pdf. Accessed May 31st 2021
- Ministry of Statistics and Programme Implementation. (2018). Persons with disabilities in India NSS 76th Round July to August 2018 Available at http://www.mospi.gov.in/sites/default/files/publication_reports/Report_583_Final_0.pdf. Accessed 26 May 2020
- Perin J, Mulick A, Yeung D, Villavicencio F, Lopez G, Strong KL, et al. Global, regional, and national causes of under-5 mortality in 2000–19: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet Child Adolesc Health. 2022;6:106–115. doi: 10.1016/S2352-4642(21)00311-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punekar News (2021). Doctor commits suicide after giving poisonous injection to wife and children – writes in suicide note. Available at https://www.punekarnews.in/doctor-commits-suicide-after-giving-poisonous-injection-to-wife-and-children-writes-in-suicide-note/. Accessed 30 May,2021
- Shooshtari S, Brownell M, Mills RS, Dik N, Yu DC, Chateau D, et al. Comparing health status, health trajectories and use of health and social services between children with and without developmental disabilities: a population-based longitudinal study in Manitoba. J Appl Res Intellect Disabil. 2017;30:584–601. doi: 10.1111/jar.12253. [DOI] [PubMed] [Google Scholar]
- Taruscio D, Mantovani A, Carbone P, Barisic I, Bianchi F, Garne E, et al. Primary prevention of congenital anomalies: recommendable, feasible and achievable. Public Health Genomics. 2015;18:184–191. doi: 10.1159/000379739. [DOI] [PubMed] [Google Scholar]
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- Ujagare D, Kar A. Birth defect mortality in India 1990–2017: estimates from the Global Burden of Disease data. J Community Genet. 2021;12:81–90. doi: 10.1007/s12687-020-00487-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unusan N. Assessment of Turkish women’s knowledge concerning folic acid and prevention of congenital anomalies. Public Health Nutr. 2004;7:851–855. doi: 10.1079/PHN2004615. [DOI] [PubMed] [Google Scholar]
- Vaismoradi M, Jones J, Turunen H, Snelgrove S. Theme development in qualitative content analysis and thematic analysis. J Nurs Educ Pract. 2016;6:100–110. [Google Scholar]
- Wong LP. Focus group discussion: a tool for health and medical research. Singapore Med J. 2008;49:256–260. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Available on request.