Abstract
Objective
In the United States (US), the health and financial consequences of COVID-19 have disproportionately impacted women and minoritized racial-ethnic groups. Yet, few US studies have investigated financial hardship during the COVID-19 pandemic and sleep health disparities. Our objective was to investigate associations between financial hardship and sleep disturbances during the COVID-19 pandemic by gender and race and ethnicity in the United States.
Methods
We used the nationally representative COVID-19′s Unequal Racial Burden cross-sectional survey data collected among 5339 men and women from 12/2020 to 2/2021. Participants reported financial hardship (eg, debt, employment/work loss) since the pandemic began and completed the Patient-Reported Outcomes Management Information System Short Form 4a for sleep disturbances. Prevalence ratios (PRs) and 95% confidence intervals were estimated using adjusted, weighted Poisson regression with robust variance.
Results
Most (71%) participants reported financial hardship. Prevalence of moderate to severe sleep disturbances was 20% overall, higher among women (23%), and highest among American Indian/Alaska Native (29%) and multiracial adults (28%). Associations between financial hardship and moderate to severe sleep disturbances (PR = 1.52 [95% confidence interval: 1.18, 1.94]) did not differ by gender but varied by race and ethnicity: associations were strongest among Black/African American (PR = 3.52 [1.99,6.23]) adults.
Conclusions
Both financial hardship and sleep disturbances were prevalent, and their relationships were strongest among certain minoritized racial-ethnic groups, particularly Black/African American adults. Interventions that alleviate financial insecurity may reduce sleep health disparities.
Keywords: COVID-19, Financial stress, Sleep quality, Health status disparities, Racial groups
Introduction
According to the World Health Organization, the COVID-19, or SARS-CoV-2 pandemic started around December 2019 in Wuhan, China and quickly spread to 114 countries, including the United States (US) by March 2020.1, 2 In response to the outbreak, states across the US hastily implemented preventive measures to reduce transmission of the virus. Most people were advised to shelter in place at their dwelling, thus halting usual daily activities or routines due to, for instance, the temporary closure of nonessential businesses. Reverberations of the abrupt, widespread change in lifestyle included impacts on the social environment, such as increased physical isolation and loneliness as well as disruption of supply chains (eg, shortages of essential items) and unprecedented, widespread unemployment, among other adverse consequences (eg, poor mental health).3, 4 The unemployment rate in the US rose from 3.6% in 2019 to 13% by mid-2020, and approximately 46% of US households reported serious financial hardships, such as increasing debt and inability to pay bills.3, 5
The impacts of the COVID-19 pandemic were not evenly distributed.3, 6 At the onset of the pandemic, women compared to men and minoritized racial-ethnic groups compared to non-Hispanic White people, among other sociodemographic groups (eg, lower income), were disproportionately financially impacted as demonstrated by the higher unemployment rates (eg, 14% among women vs. 12% among men) and higher burden of financial hardship among these groups.3 It is also likely that racially and ethnically minoritized women may have been more disproportionately impacted but data are sparse.
Unlike sparse data on financial hardship, gender and racial-ethnic sleep disparities prior to the pandemic are well-documented.7, 8 Although both sleep disorders, which are estimated to affect 50-70 million US adults, and short habitual sleep duration, affecting approximately one-third of adults, are prevalent,9, 10 indicators of poor sleep health (eg, taking ≥30 minutes to fall asleep) have consistently been recognized as more prevalent among women versus men and among most minoritized racial-ethnic groups (eg, Black and/or African American [BAA], non-Mexican Hispanic/Latino) compared to non-Hispanic White adults with trends suggesting widening disparities.7, 11 Social determinants of health, including economic stability, have been identified as fundamental causes of sleep disparities.7, 8, 12 Both preexisting sleep health disparities and financial hardship during the COVID-19 pandemic may contribute to exacerbation of widening sleep health disparities. Financial hardship during the COVID-19 pandemic can contribute to poor sleep health and sleep health disparities through, for example, impacting psychological (eg, stress, physiological arousal) and lifestyle (eg, hunger due to food insecurity) factors.13, 14, 15 Further, impacts of disease outbreaks on health are increasingly recognized as persistent,4 suggesting the possibility of chronic, enduring sleep health consequences. Thus, elucidating associations between financial hardship and sleep health among racially and ethnically diverse populations may help guide long-term intervention development necessary to avoid exacerbation of sleep health disparities.
While prior studies have suggested negative impacts of financial hardship on sleep health (eg, insomnia symptoms, poor sleep quality),16, 17, 18, 19, 20, 21, 22, 23 to our knowledge, nationally representative US studies to date have yet to investigate potentially differential relationships between financial hardship and sleep during the COVID-19 pandemic by important social determinants of health.16 To fill this gap in the literature, our aim was to investigate associations between financial hardship and sleep disturbances during the pandemic among a nationally representative sample of US adults and to determine whether associations were modified by gender, race-ethnicity, and both gender and race-ethnicity. We hypothesized that financial hardship would be associated with more severe sleep disturbance and that associations would be stronger among women compared to men and among minoritized racial-ethnic groups compared to non-Hispanic White adults. Further, we hypothesized that associations would be strongest among women belonging to minoritized racial-ethnic groups.
Participants and methods
Data source
For this analysis, we used data from the COVID-19′s Unequal Racial Burden (CURB) survey, which is a nationally representative, online survey led by the National Institute on Minority Health and Health Disparities that was designed to investigate the impacts of the COVID-19 pandemic among a diverse cohort of US adults. The cross-sectional survey was offered in both English and Spanish from December 8, 2020 to February 17, 2021. YouGov, a consumer research firm, created a theoretical sample using the 2018 American Community Survey and then matched eligible participants from their survey panel (∼1.8 million adults) to the theoretical sample by sociodemographic characteristics. To participate in CURB, respondents had to complete a double opt-in procedure (to the survey panel and CURB) to confirm their consent. YouGov protocol was approved for Federal-wide Assurance by the Department of Health and Human Services (FWA00010960). Further details are elsewhere.24
Overall, 5500 participants who self-identified their race and ethnicity were recruited (response rate: 20%): 500 American Indian/Alaska Native (AIAN), 1000 Asian, 1000 non-Hispanic BAA, 500 English-speaking Hispanic/Latino (hereafter, Latino), 500 Spanish-speaking Latino, 500 multiracial, 500 Native Hawaiian/Pacific Islander (NHPI), and 1000 non-Hispanic White (hereafter, White) adults aged 18 years and older. Survey weights were then generated to create nationally representative cohorts within each racial-ethnic group. Due to the use of de-identified data provided by YouGov, the National Institutes of Health Office of Internal Review Board Operations did not consider CURB human subjects research and waived consent (IRB #000166).
Study participants
CURB participants were eligible for inclusion in this analysis if they identified as a man or woman (due to the small sample size of nonbinary or transgender persons, n = 128, 2.3%) and if they had no missing data for financial hardship, potential confounders, or potential modifiers (n = 33; 0.7% missing data). As a result, the analytic sample comprised 5339 men and women. Compared to men and women in the analytic sample, excluded men and women were more likely to be married, have a lower socioeconomic status and children in the household, report fair or poor general health, and have more severe sleep disturbances; however, they were no more likely to report financial hardships (Supplemental Table 1).
Exposures: Financial hardship (FH)
All participants responded to twelve questions related to economic and financial hardship during the first year of the pandemic, most were adapted from questions in the All of Us Study.25 After examination of correlations, these questions were consolidated into 6 domains of financial hardship: 1) debt (ie, lost savings or increased debt); 2) lost income (ie, lost job or income or hours reduced); 3) unmet expenses (ie, did not have enough money to pay bills or meet daily needs); 4) unmet healthcare expenses (ie, did not have enough money to pay for healthcare or lost health insurance); 5) housing insecurity (ie, did not have enough money to pay rent, mortgage, or other housing costs); and 6) food insecurity (ie, were hungry but did not have enough money for food). A financial hardship index was created by assigning each domain a value of 1 if reported and summing the domains where higher scores indicate higher financial hardship (range 0-6). For this analysis, we assessed ordinal financial hardship categories that capture increasing severity—including the approximately highest quintile—of hardship (ie, substantial hardship (4-6), some hardship (2-3), little hardship (1), and no hardship (0)) and a dichotomized financial hardship measure (any [≥1] vs. none [0]).
Outcomes: Sleep disturbances (SDs)
The previously validated 4-item Patient-Reported Outcomes Management Information System (PROMIS) Short Form v1.0—Sleep Disturbance 4a captured SDs in the past 7 days.26 Using a five-point Likert scale, participants reported sleep quality, refreshing sleep, problems with sleep, and difficulty falling asleep in the past 7 days. All items were then summed to create a SDs score ranging from 4 to 20 where higher scores indicated more severe SDs (Cronbach’s α = 0.86 within CURB). In accordance with the PROMIS scoring guidelines,27 total raw scores were converted to a standardized PROMIS T-score for each participant by using the Health Measures Scoring Service (https://www.assessmentcenter.net/ac_scoringservice). In addition to measuring SDs continuously using the PROMIS T-score, we categorically assessed SDs as ‘severe’ (T-score > 70), ‘moderate’ (60-70), ‘mild’ (55-60), and ‘within normal limits’ (<55 [reference]) based on scoring guidelines.28 Due to the relatively low prevalence of severe sleep disturbances (3.5%), moderate and severe were collapsed into a single category for analysis.
Potential confounders
Sociodemographic characteristics included categorical age (18-34 years, 35-49 years, 50-64 years, ≥65 years), gender identity (man, woman), and race-ethnicity (categories aligned with the US Census Bureau collection of race-ethnicity data in the 2020 Census: AIAN, Asian, BAA, Latino, Multiracial, NHPI, White). Latino participants were further stratified by survey language preference (English-speaking, Spanish-speaking). Other sociodemographic characteristics were citizenship status (US-born, foreign-born, undocumented), marital status (married/domestic partnership, single/separated/divorced/widowed), current full- or part-time employment, current telework most to all of the time (yes, no), educational attainment (<high school, high school/general education diploma, some college/technical school, ≥college), annual household income (<$20,000, $20,000-$59,000, $60,000-$99,000, ≥$100,000), children in the household (yes, no), and region of residence (Northeast, Midwest, South, West). Health behaviors included alcohol consumption before and during the pandemic (drinker vs. nondrinker) and physical activity in the past month (inactive [none, once/month], underactive [several times/month to 3 times/week], active [≥4 times/week]). Financial hardship-related characteristics included receipt of financial assistance (ie, unemployment benefits, paid time off from employer) or COVID-19 stimulus checks (yes, no). Participants self-rated fair or poor physical health (yes, no). Emotional well-being included 2 mental health measures: self-rated or perceived mental health and psychological distress as measured by the Patient Health Questionnaire-4.29 Participants who self-rated poor or fair versus good, very good, or excellent mental health or with a Patient Health Questionnaire-4 score ≥3 (indicating psychological distress) met the criteria for poor emotional well-being (yes, no).29 Lastly, participants were asked, “In the past month, how often have you felt lonely and isolated?”. Any loneliness was dichotomized as yes (fairly or very often, sometimes, almost never) versus no (never).
Potential modifiers
Potential modifiers included self-identified gender as well as race and ethnicity.
Statistical analysis
Post-survey weights obtained from matching and propensity score weighting were applied to all analyses to obtain nationally representative estimates for US adults.24 Weighted descriptive statistics included frequencies (proportions) and means ± standard deviations among the total population and by FH, gender, race-ethnicity, and categorical SDs. Using multivariate linear regression, we estimated betas and 95% confidence intervals (CIs) for PROMIS T-scores. Poisson regression with robust variance estimators assessed prevalence ratios (PRs) and 95% CIs for 2 SD categories, separately (moderate to severe and mild vs. within normal limits).
Models among the overall population were adjusted in a sequential manner for potential confounders that were selected based on prior literature, our construction of directed acyclic graphs, and subsequently, an assessment of multicollinearity.30 We then combined categories of confounders in which<10% of participants comprised one category (see Table 1) to increase model stability when stratifying by potential modifiers. Model 1 was age-adjusted; Model 2 was additionally adjusted for sociodemographic characteristics (gender, race-ethnicity, marital status, educational attainment, children in household, region of residence, and receipt of assistance); and Model 3 was additionally adjusted for health behaviors or characteristics (alcohol consumption, physical activity, self-rated physical health, and poor emotional well-being). We then stratified the fully adjusted Model 3 by gender and race-ethnicity, separately, and performed Wald tests for two-way interaction terms (eg, gender*FH). We also further stratified by both gender and race-ethnicity if either gender or race-ethnicity was identified as a modifier in prior steps.
Table 1.
Study population characteristics, COVID-19′s Unequal Racial Burden (CURB) Survey, December 2020-February 2021, N = 5339
| Overall | Financial hardship |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any | Ordinal categories within any financial hardship |
None | ||||||||||
| Substantial | Some | Little | ||||||||||
| N or n (%) | 5339 | (100) | 3813 | (71) | 1160 | (22) | 1501 | (28) | 1152 | (22) | 1526 | (29) |
| n or mean | (%) or±SD | n or mean | (%) or±SD | n or mean | (%) or±SD | n or mean | (%) or±SD | n or mean | (%) or±SD | n or mean | (%) or±SD | |
| Sociodemographic characteristics | ||||||||||||
| Age, yearsa,b | ||||||||||||
| 18-34 years | 1922 | (36.0) | 1466 | (38.4) | 511 | (44.1) | 563 | (37.5) | 392 | (34.0) | 456 | (29.9) |
| 35-49 years | 1604 | (30.0) | 1206 | (31.6) | 428 | (36.9) | 449 | (29.9) | 329 | (28.6) | 398 | (26.1) |
| 50-64 years | 1497 | (28.0) | 1006 | (26.4) | 209 | (18.0) | 438 | (29.2) | 359 | (31.2) | 491 | (32.2) |
| ≥65 years | 316 | (5.9) | 135 | (3.5) | 12 | (1.0) | 51 | (3.4) | 72 | (6.3) | 181 | (11.9) |
| Gendera,b | ||||||||||||
| Men | 2450 | (45.9) | 1666 | (43.7) | 481 | (41.5) | 645 | (43.0) | 540 | (46.9) | 784 | (51.4) |
| Women | 2889 | (54.1) | 2147 | (56.3) | 679 | (58.5) | 856 | (57.0) | 612 | (53.1) | 742 | (48.6) |
| Race-ethnicitya,b | ||||||||||||
| American Indian/Alaska Native | 473 | (8.9) | 363 | (9.5) | 128 | (11.0) | 140 | (9.3) | 95 | (8.2) | 110 | (7.2) |
| Asian | 983 | (18.4) | 573 | (15.0) | 119 | (10.3) | 209 | (13.9) | 245 | (21.3) | 410 | (26.9) |
| Black/African American | 982 | (18.4) | 775 | (20.3) | 245 | (21.1) | 306 | (20.4) | 224 | (19.4) | 207 | (13.6) |
| Hispanic/Latino- English Speaking | 491 | (9.2) | 361 | (9.5) | 119 | (10.3) | 143 | (9.5) | 99 | (8.6) | 130 | (8.5) |
| Hispanic/Latino- Spanish Speaking | 486 | (9.1) | 422 | (11.1) | 162 | (14.0) | 198 | (13.2) | 62 | (5.4) | 64 | (4.2) |
| Multiracial | 467 | (8.7) | 325 | (8.5) | 91 | (7.8) | 123 | (8.2) | 111 | (9.6) | 142 | (9.3) |
| Native Hawaiian/Pacific Islander | 476 | (8.9) | 387 | (10.1) | 157 | (13.5) | 136 | (9.1) | 94 | (8.2) | 89 | (5.8) |
| White | 981 | (18.4) | 607 | (15.9) | 139 | (12.0) | 246 | (16.4) | 222 | (19.3) | 374 | (24.5) |
| US citizenship statusa,b | ||||||||||||
| US-born | 4128 | (77.3) | 2925 | (76.7) | 888 | (76.6) | 1123 | (74.8) | 914 | (79.3) | 1203 | (78.8) |
| Foreign-born | 948 | (17.8) | 681 | (17.9) | 189 | (16.3) | 286 | (19.1) | 206 | (17.9) | 267 | (17.5) |
| Undocumented | 263 | (4.9) | 207 | (5.4) | 83 | (7.2) | 92 | (6.1) | 32 | (2.8) | 56 | (3.7) |
| Marital statusa,b | ||||||||||||
| Married/domestic partnership | 2525 | (47.3) | 1694 | (44.4) | 468 | (40.3) | 705 | (47.0) | 521 | (45.2) | 831 | (54.5) |
| Single/separated/divorced/ widowed | 2814 | (52.7) | 2119 | (55.6) | 692 | (59.7) | 796 | (53.0) | 631 | (54.8) | 695 | (45.5) |
| Current full or part-time employment (yes) | 2697 | (50.5) | 1799 | (47.2) | 496 | (42.8) | 719 | (47.9) | 584 | (50.7) | 898 | (58.8) |
| Current telework (yes)a,b | 1070 | (20.0) | 623 | (16.3) | 133 | (11.5) | 241 | (16.1) | 249 | (21.6) | 447 | (29.3) |
| Educational attainmenta,b | ||||||||||||
| <High school | 388 | (7.3) | 333 | (8.7) | 130 | (11.2) | 125 | (8.3) | 78 | (6.8) | 55 | (3.6) |
| High school/GED | 1424 | (26.7) | 1137 | (29.8) | 383 | (33.0) | 447 | (29.8) | 307 | (26.6) | 287 | (18.8) |
| Some college/technical school | 1789 | (33.5) | 1346 | (35.3) | 455 | (39.2) | 523 | (34.8) | 368 | (31.9) | 443 | (29.0) |
| ≥College | 1738 | (32.6) | 997 | (26.1) | 192 | (16.6) | 406 | (27.0) | 399 | (34.6) | 741 | (48.6) |
| Annual household incomea, b, c | ||||||||||||
| < $20,000 | 1006 | (18.8) | 916 | (24.0) | 370 | (31.9) | 338 | (22.5) | 208 | (18.1) | 90 | (5.9) |
| $20,000-$59,000 | 1838 | (34.4) | 1431 | (37.5) | 497 | (42.8) | 607 | (40.4) | 327 | (28.4) | 407 | (26.7) |
| $60,000-$99,000 | 964 | (18.1) | 628 | (16.5) | 151 | (13.0) | 236 | (15.7) | 241 | (20.9) | 336 | (22.0) |
| ≥ $100,000 | 894 | (16.7) | 409 | (10.7) | 61 | (5.3) | 144 | (9.6) | 204 | (17.7) | 485 | (31.8) |
| Children in household (yes)a, b | 2004 | (37.5) | 1563 | (41.0) | 568 | (49.0) | 622 | (41.4) | 373 | (32.4) | 441 | (28.9) |
| Region of residencea, b | ||||||||||||
| Northeast | 850 | (15.9) | 601 | (15.8) | 160 | (13.8) | 237 | (15.8) | 204 | (17.7) | 249 | (16.3) |
| Midwest | 832 | (15.6) | 573 | (15.0) | 177 | (15.3) | 231 | (15.4) | 165 | (14.3) | 259 | (17.0) |
| West | 1941 | (36.4) | 1429 | (37.5) | 458 | (39.5) | 562 | (37.4) | 409 | (35.5) | 512 | (33.6) |
| South | 1716 | (32.1) | 1210 | (31.7) | 365 | (31.5) | 471 | (31.4) | 374 | (32.5) | 506 | (33.2) |
| Health behaviors | ||||||||||||
| Alcohol consumption (before and during COVID)a, b | ||||||||||||
| Drinker | 3766 | (70.5) | 2770 | (72.6) | 917 | (79.1) | 1128 | (75.1) | 725 | (62.9) | 996 | (65.3) |
| Nondrinker | 1573 | (29.5) | 1043 | (27.4) | 243 | (20.9) | 373 | (24.9) | 427 | (37.1) | 530 | (34.7) |
| Physical activity (past month)a, b | ||||||||||||
| Inactive | 1659 | (31.1) | 1313 | (34.4) | 432 | (37.2) | 497 | (33.1) | 384 | (33.3) | 346 | (22.7) |
| Underactive | 2449 | (45.9) | 1758 | (46.1) | 532 | (45.9) | 711 | (47.4) | 515 | (44.7) | 691 | (45.3) |
| Active | 1231 | (23.1) | 742 | (19.5) | 196 | (16.9) | 293 | (19.5) | 253 | (22.0) | 489 | (32.0) |
| Financial Loss/Hardship | ||||||||||||
| Financial hardship | ||||||||||||
| Debt | 3106 | (58.2) | 3106 | (81.5) | 1151 | (99.2) | 1350 | (89.9) | 605 | (52.5) | - | - |
| Lost income | 2462 | (46.1) | 2462 | (64.6) | 1020 | (87.9) | 990 | (66.0) | 452 | (39.2) | - | - |
| Unmet expenses | 1828 | (34.2) | 1828 | (47.9) | 1104 | (95.2) | 683 | (45.5) | 41 | (3.6) | - | - |
| Unmet healthcare expenses | 1234 | (23.1) | 1234 | (32.4) | 785 | (67.7) | 403 | (26.8) | 46 | (4.0) | - | - |
| Housing insecurity | 997 | (18.7) | 997 | (26.1) | 811 | (69.9) | 181 | (12.1) | 5 | (0.4) | - | - |
| Food insecurity | 679 | (12.7) | 679 | (17.8) | 573 | (49.4) | 103 | (6.9) | 3 | (0.3) | - | - |
| Received financial assistance (yes) | 3869 | (72.5) | 2801 | (73.5) | 869 | (74.9) | 1100 | (73.3) | 832 | (72.2) | 1068 | (70.0) |
| Physical and mental health characteristics | ||||||||||||
| Fair/poor self-rated physical health (yes)a, b | 1358 | (25.4) | 1115 | (29.2) | 390 | (33.6) | 447 | (29.8) | 278 | (24.1) | 243 | (15.9) |
| Fair/poor self-rated mental health (yes) | 1551 | (29.1) | 1275 | (33.4) | 488 | (42.1) | 474 | (31.6) | 313 | (27.2) | 276 | (18.1) |
| Psychological distress (yes)a, b, d | 2661 | (49.8) | 2171 | (56.9) | 829 | (71.5) | 840 | (56.0) | 502 | (43.6) | 490 | (32.1) |
| Poor emotional well-being (yes)a, b, e | 2914 | (54.6) | 2350 | (61.6) | 866 | (74.7) | 919 | (61.2) | 565 | (49.0) | 564 | (37.0) |
| Any loneliness (yes)a, b | 3319 | (62.2) | 2588 | (67.9) | 917 | (79.1) | 1013 | (67.5) | 658 | (57.1) | 731 | (47.9) |
| Sleep disturbancea, b | ||||||||||||
| PROMIS T-score | 51.8 | ±9.6 | 53.3 | ±9.0 | 57.1 | ±8.4 | 52.8 | ±8.4 | 50.9 | ±9.3 | 48.8 | ±10.2 |
| Severe (PROMIS T-score >70) | 187 | (3.5) | 171 | (4.5) | 104 | (9.0) | 51 | (3.4) | 16 | (1.4) | 16 | (1.0) |
| Moderate (PROMIS T-score 60-70) | 902 | (16.9) | 739 | (19.4) | 320 | (27.6) | 261 | (17.4) | 158 | (13.7) | 163 | (10.7) |
| Mild (PROMIS T-score 55-60) | 850 | (15.9) | 672 | (17.6) | 219 | (18.9) | 282 | (18.8) | 171 | (14.8) | 178 | (11.7) |
| Within normal limits (PROMIS T-score <55) |
3400 | (63.7) | 2231 | (58.5) | 517 | (44.6) | 907 | (60.4) | 807 | (70.1) | 1169 | (76.6) |
GED, general education diploma; PROMIS, Patient-Reported Outcomes Management Information System.
p < 0.05 for Chi-Square or t-test for differences between any versus no financial hardship.
p < 0.05 for Chi-Square or analysis of variance (ANOVA) for differences between financial hardship categories.
n = 637 missing values for annual household income.
Psychological distress defined as a score ≥3 on the Patient Health Questionnaire-4.
Poor emotional well-being defined as either fair/poor self-rated mental health or psychological distress.
In post-hoc analyses, we investigated associations with each of the mutually adjusted 6 domains of FH to determine which FH domains may drive associations. Results were stratified by gender or race-ethnicity if interaction was present. A two-sided p-value of 0.05 was used to determine statistical significance. All analyses were performed using SAS, 9.4 (Cary, NC).
Results
Study population characteristics
Among the 5339 included participants, 66% were aged 49 years or younger and 54% were women (Table 1). Most participants reported FH (71%) since the pandemic began with 22% reporting substantial, 28% some, and 22% little. The most frequently endorsed hardships related to debt (58%), lost income (46%), and unmet expenses (34%). Mean ± standard deviation PROMIS T-score was 52 ± 10, and approximately 4% of adults reported severe, 17% moderate, and 16% mild SDs while most had SDs within normal limits (64%).
Socioeconomic characteristics and FH varied by gender, race-ethnicity, and SDs (Supplementary Tables 2-5). Compared to men, women reported lower household income, were more likely to have children in the household (40% vs. 34%) and were more likely to report both any (74% vs. 68%) and substantial FH (24% vs. 20%). Women also had a higher prevalence of moderate to severe SDs compared to men (23% vs. 17%). Annual household income was lowest while moderate to severe SDs were most prevalent among AIAN, BAA, Spanish-speaking Latino, and NHPI adults.
BAA (79%), Spanish-speaking Latino (80%), and NHPI (81%) adults were most likely to report any FH, while White (62%) and Asian (58%) adults were least likely. There were also gender differences in FH that varied by race-ethnicity. For instance, the prevalence of any FH was higher among Spanish-speaking Latino men than women, but the prevalence of any FH was higher among NHPI and BAA women than men (eg, BAA: 81% among women vs. 77% among men).
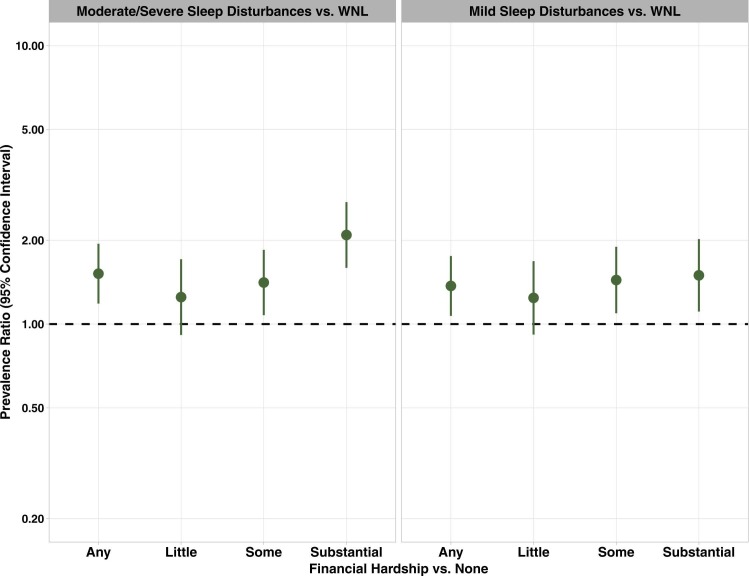
FH and SDs among adults
We present results for all models (ie, for the continuous (PROMIS T-score) and categorical SD measures) in Supplementary Material (Supplementary Tables 6-9b) and display the results for categorical SDs ( Fig. 1, Fig. 2, Fig. 3). Among the total population, any FH was associated with a 52% higher prevalence of moderate to severe SDs (PR = 1.52 [95% CI: 1.18, 1.94]). By FH severity, substantial (PR = 2.09 [95% CI: 1.59, 2.74]) and some (PR = 1.41 [95% CI: 1.08, 1.85]) FH were associated with a two-times higher and 41% higher prevalence of moderate to severe SDs, respectively (Fig. 1).
Fig. 1.
Fully adjusted prevalence ratios and 95% confidence intervals for associations between financial hardship during the pandemic and sleep disturbances, CURB Survey, December 2020 to February 2021, N = 5339. Note: Models are adjusted for age (18-34 years, 35-49 years, ≥50 years), gender (man, woman), race-ethnicity (American Indian/Alaska Native, Asian, Black/African American, Hispanic/Latino- English Speaking, Hispanic/Latino- Spanish Speaking, Multiracial, Native Hawaiian/Pacific Islander, White), marital status (married/domestic partnership, single/separated/divorced/ widowed), educational attainment (≤high school, some college, ≥college), receipt of financial assistance or COVID relief (yes, no), region of residence (Northeast, Midwest, West, South), children in the household (yes, no), alcohol consumption (drinker, nondrinker), physical activity (inactive, underactive, active), fair or poor self-rated physical health (yes, no), and poor emotional well-being (yes, no). WNL, within normal limits.
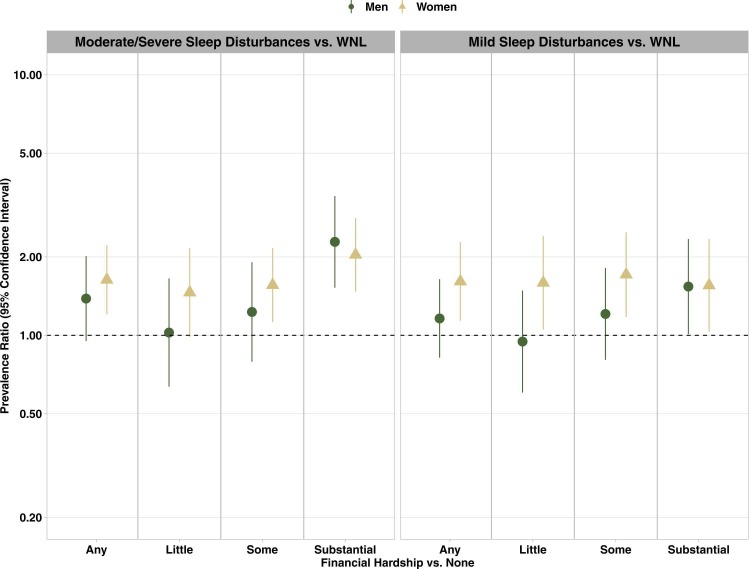
Fig. 2.
Fully adjusted prevalence ratios and 95% confidence intervals for associations between financial hardship during the pandemic and sleep disturbances by gender, CURB Survey, December 2020 to February 2021, N = 5339. Note: Models are adjusted for age (18-34 years, 35-49 years, ≥50 years), race-ethnicity (American Indian/Alaska Native, Asian, Black/African American, Hispanic/Latino- English Speaking, Hispanic/Latino- Spanish Speaking, Multiracial, Native Hawaiian/Pacific Islander, White), marital status (married/domestic partnership, single/separated/divorced/ widowed), educational attainment (≤high school, some college, ≥college), receipt of financial assistance or COVID relief (yes, no), region of residence (Northeast, Midwest, West, South), children in the household (yes, no), alcohol consumption (drinker, nondrinker), physical activity (inactive, underactive, active), fair or poor self-rated physical health (yes, no), and poor emotional well-being (yes, no). WNL, within normal limits.
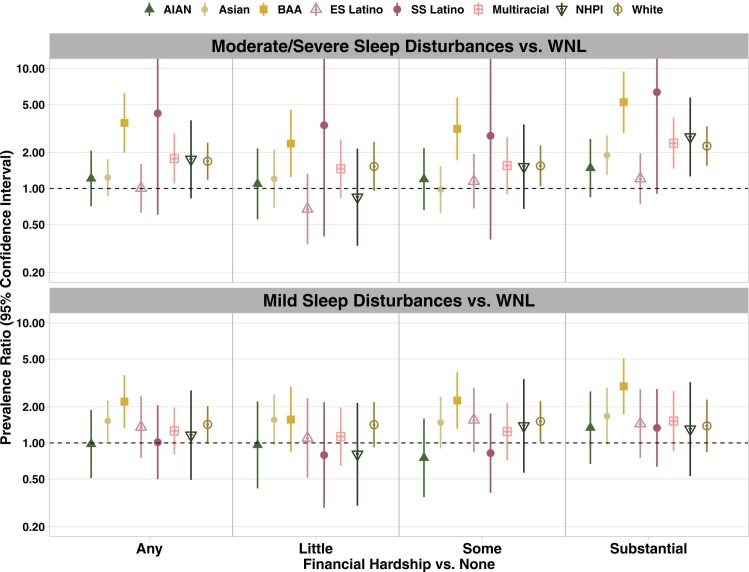
Fig. 3.
Fully adjusted prevalence ratios and 95% confidence intervals for associations between financial hardship during the pandemic and sleep disturbances by race-ethnicity, CURB Survey, December 2020 to February 2021, N = 5339. Note: Models are adjusted for age (18-34 years, 35-49 years, ≥50 years), gender (man, woman), marital status (married/domestic partnership, single/separated/divorced/ widowed), educational attainment (≤high school, some college, ≥college), receipt of financial assistance or COVID relief (yes, no), region of residence (Northeast, Midwest, West, South), children in the household (yes, no), alcohol consumption (drinker, nondrinker), physical activity (inactive, underactive, active), fair or poor self-rated physical health (yes, no), and poor emotional well-being (yes, no). Upper confidence limits for moderate to severe sleep disturbances among Spanish-Speaking Latino adults extended beyond the range displayed in the figure. For upper confidence limits, see Supplementary Table 8. WNL, within normal limits; AIAN, American Indian/Alaska Native; BAA, Black/African American; ES, English-speaking; SS, Spanish-speaking; NHPI, Native Hawaiian/Pacific Islander.
FH and SDs by gender
Only associations between categories of FH and PROMIS T-scores varied by gender, suggesting stronger associations among women compared to men (Supplementary Table 7). However, associations between FH and SDs categories did not vary by gender (Fig. 2).
FH and SDs by race-ethnicity
Associations between any FH and a higher prevalence of moderate to severe SDs were stronger among BAA adults than among other racial-ethnic groups (pFH*race-ethnicity = 0.03). BAA adults with any versus no FH had over three times the prevalence (PR = 3.52 [95% CI: 1.99, 6.23]) of moderate to severe SDs (range of PRs among the other racial-ethnic groups: 1.00 [English-speaking Latino]-1.77 [multiracial]). Like among BAA adults, PRs for moderate to severe SDs were also high among Spanish-speaking Latinos (eg, PRany vs. none = 4.23 [95% CI: 0.60, 29.58]); however, CIs were wide. Results were similar for categories of FH (ie, substantial, some, and little vs. none; pFH*race-ethnicity = 0.06). For example, BAA adults with substantial versus no FH had over five times the prevalence (PR = 5.24 [95% CI: 2.91, 9.43] of moderate to severe SDs, which was stronger than associations among AIAN adults (PR = 1.48 [95% CI: 0.85, 2.59]), Asian adults (PR = 1.90 [95% CI: 1.30, 2.77), and English-speaking Latino adults (PR = 1.21 [95% CI: 0.74, 1.96]).
Individual hardships and SDs
Overall, individual hardship domains including unmet expenses, housing insecurity, and food insecurity were associated with a 23%-73% higher prevalence of moderate to severe SDs (Supplementary Tables 9a-9b). Further, associations between food insecurity and moderate to severe SDs were suggestively stronger among men (PR = 2.03 [95% CI: 1.54, 2.69]) compared to women (PR = 1.50 [95% CI: 1.21, 1.86]; pinteraction< 0.10). By race-ethnicity, associations between housing insecurity and moderate to severe SDs were suggestively strongest among BAA, Spanish-speaking Latino, and NHPI adults (pinteraction< 0.10). While PRs ranged between 1.09 and 1.40 among other racial or ethnic groups, BAA, Spanish-speaking Latino, and NHPI adults reporting versus not reporting housing insecurity had approximately 80% higher prevalence of moderate to severe SDs (PR range = 1.79-1.83).
Discussion
In this nationally representative study of US adults, financial hardship during the COVID-19 pandemic was associated with higher sleep disturbance severity, the linear relationship was stronger among women compared to men, and relationships were generally strongest among BAA adults, which was consistent with our hypotheses. For instance, BAA adults with financial hardship had over three times the prevalence of moderate to severe sleep disturbances compared to within-race counterparts without financial hardship. There were either nonsignificant associations or up to 77% higher prevalence among adults with versus without financial hardship in other racial-ethnic groups. All relationships were observed even after adjustment for sociodemographic, household, health behavior, and mental health characteristics, supporting the robustness of our results. Also, women compared to men reported more financial hardship and more sleep disturbances. Further, minoritized racial-ethnic groups except Asians (particularly, BAA, Spanish-speaking Latino, and NHPI adults) had the largest burdens of financial hardship and AIAN, multiracial, and NHPI adults had more severe sleep disturbances.
While our results are consistent with the limited prior literature on financial hardship during COVID in relation to sleep health, it also extends the literature. The few prior non-nationally representative studies reported that either summary measures of financial hardship or individual hardships (eg, food insecurity, financial strain) were associated with various measures of sleep health (ie, objectively measured poorer sleep, poor sleep quality, and insomnia symptoms), which is consistent with our findings.16, 17, 18, 19, 20, 21, 22, 23, 31 The 1 nationally representative US study reported a comparable high prevalence of job loss and loss of income/work hours (∼40% vs. 46% in CURB) as well as job loss, loss of income or work hours, and childcare difficulties as cross-sectionally associated with trouble sleeping among US adults from March to April 2020.16 We expanded upon the literature on this topic by demonstrating associations with additional domain-specific financial hardships (eg, unmet expenses) as well as gender and racial-ethnic disparities in these associations after the second (and highest peak) versus first wave of the pandemic in the US (ie, December 2020 to February 2021).
Our observations of associations between financial hardship and sleep disturbances may be explained by stress response pathways as well as reduced access to health-promoting resources.13, 14, 15, 17, 18 Overall, both worry about finances and material financial hardship have been previously associated with poorer sleep among adults during the pandemic.17, 18 Financial hardship and related worry may impact one’s ability to engage in a healthy sleep cycle by, for example, triggering biological stress responses, thus contributing to dysregulation of hypothalamic adrenal axis functioning, and physiological arousal.13, 14 Financial hardship also negatively impacts access to health-promoting resources (eg, adequate nutrition) that are associated with healthy sleep.15
Our observations of disparities by gender and race-ethnicity may be explained by intersectional lived experiences (ie, experiences related to membership in multiple marginalized groups) in the context of societal conditions.7, 8 Studies have shown that women and minoritized adults were more financially vulnerable prior to COVID-19 compared to men and White adults. Prior to the pandemic, the prevalence of financial health, an indicator of financial resilience in times of crises, was 40% among men and 28% among women in the US.32 With regard to race-ethnicity, estimates ranged between 15% and 34% among BAA, Hispanic or Latino, and multiracial adults, compared to 39% among non-Hispanic White adults.32 Relatedly, racial-ethnic and gender gaps in pay exist. For instance, national data suggests that White men have the highest hourly rate of pay followed by Black men, White women, and then Black women, and that the racial pay gap is higher among women ($0.82) compared to men ($0.69).33 Women and minoritized racial-ethnic groups also reported disproportionate burdens of financial hardships during the pandemic.5, 32 Further, within racial-ethnic groups, women often had even larger burdens of financial hardship compared to men (eg, BAA and NHPI adults) in our study. As populations that also displayed disparate, poorer sleep health prior to COVID,7, 11 stronger relationships between financial hardship and higher sleep disturbance severity were expected among these groups. Lived experiences including, for instance, factors related to structural racism that contribute to lack of access to material and social resources as well as racial-ethnic discrimination concurrent with the pandemic also contribute to poorer sleep, potentially further contributing to disparities.34, 35, 36 Women who are primarily responsible for caregiving were also more likely to have children in the household, which may cause additional stress and has also been associated with poorer sleep during the pandemic.16 Intersectional identities (eg, racially minoritized women) and financial hardship during the pandemic may synergistically contribute to poorer sleep health.
Our findings should be considered in the context of our study limitations. First, our data were cross-sectional, which precludes our ability to infer causal associations. Recall bias is also possible. The prevalence of reported financial hardship was high, and due to differences in measurement, is not directly comparable to observations in other nationally representative studies. However, the questions surveyed specific, salient stressors that occurred within 12 months prior to data collection, which may limit bias related to reporting. Nonetheless, data were limited to the frequency of hardships although the duration and intensity of hardships are undoubtedly important. Data were self-reported; however, sleep disturbances were ascertained using a validated measure with good internal consistency. Nevertheless, further study using objective sleep measures is warranted. Related to our assessment of sleep disturbances, our focus on categories—although of public health significance—results in a loss of information regarding linear relationships between financial hardship and sleep disturbance severity and may mask associations within groups. Due to the observational nature of our study and less refined categories of confounder assessment (eg, dichotomous alcohol drinking), residual confounding is possible. Using the internet survey modality may have also introduced sampling bias. Further, our sample size was reduced with stratification for certain groups, which resulted in limited power to detect associations that may exist. Concomitantly, we could not further examine variations by citizenship status due to small proportions of persons who were non-US-born within some races-ethnicities. Relatedly, we were unable to investigate within-group differences beyond language among Latino adults and associations among gender minorities. However, it is important to have an adequate representation of all populations at risk of being disproportionately impacted by the pandemic due to intersectional identities and nuances of lived experiences in future studies.37 Lastly, inflation of type 1 error is possible due to multiple statistical tests; however, all tests for associations between financial hardship and sleep disturbances were a priori and central to the study hypotheses. Further, adjustment for multiple comparisons could inflate type 2 error thus reducing power and contributing to missing possibly true findings worthy of future study.38
Our study also has several noteworthy strengths. This nationally representative study of major racial-ethnic groups in the US comprised a large sample size that allowed for sufficiently robust stratification by gender and race-ethnicity. Further, we had adequate sample sizes to investigate understudied racial-ethnic groups including AIAN, Asian, and NHPI adults in the US. We also measured financial hardship across six domains to capture sources of financial strain beyond most measures in prior literature. Our assessment of sleep disturbances included a validated scale that is often used in clinical studies. This study also contributes to the COVID-19 literature by, to our knowledge, being the first nationally representative US study to capture the potential of chronic sleep disturbances related to financial hardship since sleep disturbances were reported approximately nine months after the shutdowns imposed in March 2020, although longitudinal assessments are warranted.
Conclusions
In this nationally representative study of US adults, financial hardship was prevalent, disproportionately high among women and certain minoritized racial-ethnic groups, and people who reported experiencing financial hardship during COVID-19 were more likely to also report more severe sleep disturbances. The strongest associations were generally among Black/African American adults. Our study captures relationships between financial hardship and sleep disturbances from late 2021 to early 2022. While the US government provided some economic relief by this timepoint, more economic relief followed, employment increased, and there were economic gains, all of which may impact associations. However, economic uncertainty and threats of economic recession linger. It will be important to assess changes in both financial hardship and sleep health over time. Although longitudinal studies using objective sleep measures are warranted, US adults who were and remain financially insecure may best be prioritized for targeted financial assistance, resource allocation to address the consequences of financial insecurity (eg, food insecurity), and sleep interventions by policy makers, public health practitioners, and healthcare professionals. Moreover, due to disproportionate burdens, tailored interventions may be especially beneficial among women and minoritized racial-ethnic groups, particularly Black/African American adults, who were disproportionately burdened by financial hardship.
Financial Disclosure
None.
CRediT authorship contribution statement
Symielle A. Gaston, Paula Strassle, Dana M. Alhasan, Eliseo J. Pérez-Stable, Anna M. Nápoles, Chandra L. Jackson, Conceptualization: CL Jackson, SA Gaston, Data curation: P Strassle, Formal Analysis: SA Gaston, Funding Acquisition: AM Nápoles, CL Jackson, Methodology: SA Gaston, CL Jackson, P Strassle, AM Nápoles, Project administration: P Strassle, CL Jackson, Resources: CL Jackson, Supervision: CL Jackson, Writing – original draft: SA Gaston, Writing – reviewing and editing: SA Gaston, P Strassle, DM Alhasan, EJ Pérez-Stable, AM Nápoles, CL Jackson.
Declaration of conflict of interest
The authors have no conflicts of interest to declare.
Acknowledgments
The authors wish to thank the CURB participants. The authors also wish to thank the NIEHS library staff, Stacey Mantooth and Erin Knight, for conducting a literature search for this manuscript as well as W. Braxton Jackson II and Jesse Wilkerson of DLH, Corp for performing quality control of the data analysis.
The results of the study were presented, in part, at the SLEEP 2022 Meeting (Charlotte, North Carolina) on June 6–7, 2022.
Funding support
This work was funded, in part, by the Division of Intramural Research at the NIH, National Institute of Environmental Health Sciences (Z1AES103325 (CLJ)) and by the Division of Intramural Research at the NIH, National Institute on Minority Health and Health Disparities.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.sleh.2023.04.007.
Appendix A. Supplementary material
Supplementary material
.
References
- 1.WHO Director-General's opening remarks at the media briefing on COVID-19- 11 March 2020 [press release]. 2020.
- 2.World Health Organization. Origins of SARS-CoV-2. March 26 2020.
- 3.Smith S.M., Edwards R., Duong H.C. Unemployment rises in 2020, as the country battles the COVID-19 pandemic. June 2021.
- 4.O'Regan D., Jackson M.L., Young A.H., Rosenzweig I. Understanding the impact of the COVID-19 pandemic, lockdowns and social isolation on sleep quality. Nat Sci Sleep. 2021;13:2053–2064. doi: 10.2147/NSS.S266240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NPR-RWJF TH. Harvard Chan School of Public Health. The impact of coronavirus on household across America September 2020.
- 6.Isasi C.R., Gallo L.C., Cai J., et al. Economic and psychosocial impact of COVID-19 in the hispanic community health study/study of latinos. Health Equity. 2023;7(1):206–215. doi: 10.1089/heq.2022.0211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson D.A., Jackson C.L., Williams N.J., Alcantara C. Are sleep patterns influenced by race/ethnicity—a marker of relative advantage or disadvantage? Evidence to date. Nat Sci Sleep. 2019;11:79–95. doi: 10.2147/NSS.S169312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jackson C.L., Walker J.R., Brown M.K., Das R., Jones N.L. A workshop report on the causes and consequences of sleep health disparities. Sleep. 2020;43(8):zsaa037. doi: 10.1093/sleep/zsaa037. PMID: 32154560; PMCID: PMC7420527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Institute of Medicine Committee on Sleep M, Research . In: Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Colten H.R., Altevogt B.M., editors. National Academies Press (US) National Academy of Sciences; Washington (DC): 2006. The national academies collection: reports funded by national institutes of health. [PubMed] [Google Scholar]
- 10.Sheehan C.M., Frochen S.E., Walsemann K.M., Ailshire J.A. Are U.S. adults reporting less sleep?: Findings from sleep duration trends in the National Health Interview Survey, 2004–2017. Sleep. 2018;42(2) doi: 10.1093/sleep/zsy221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caraballo C., Mahajan S., Valero-Elizondo J., et al. Evaluation of temporal trends in racial and ethnic disparities in sleep duration among US adults, 2004-2018. JAMA Netw Open. 2022;5(4):e226385. doi: 10.1001/jamanetworkopen.2022.6385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Billings M.E., Hale L., Johnson D.A. Physical and social environment relationship with sleep health and disorders. Chest. 2020;157(5):1304–1312. doi: 10.1016/j.chest.2019.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim E.-J., Dimsdale J.E. The effect of psychosocial stress on sleep: a review of polysomnographic evidence. Behav Sleep Med. 2007;5(4):256–278. doi: 10.1080/15402000701557383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buckley T.M., Schatzberg A.F. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J Clin Endocrinol Metab. 2005;90(5):3106–3114. doi: 10.1210/jc.2004-1056. [DOI] [PubMed] [Google Scholar]
- 15.Lee S., Deason K., Rancourt D., Gray H.L. Disentangling the relationship between food insecurity and poor sleep health. Ecol Food Nutr. 2021;60(5):580–595. doi: 10.1080/03670244.2021.1926245. [DOI] [PubMed] [Google Scholar]
- 16.Cobb R.J., Sheehan C.M., Nguyen A.W., Johnson D. COVID-19 hardships and self-reported sleep quality among American adults in March and April 2020: Results from a nationally representative panel study. Sleep Health. 2022;8(3):288–293. doi: 10.1016/j.sleh.2022.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wright L., Steptoe A., Fancourt D. Are adversities and worries during the COVID-19 pandemic related to sleep quality? Longitudinal analyses of 46,000 UK adults. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0248919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yuksel D., McKee G.B., Perrin P.B., et al. Sleeping when the world locks down: correlates of sleep health during the COVID-19 pandemic across 59 countries. Sleep Health. 2021;7(2):134–142. doi: 10.1016/j.sleh.2020.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Samuel L.J., Dwivedi P., Hladek M., et al. The effect of COVID-19 pandemic-related financial challenges on mental health and well-being among U.S. older adults. J Am Geriatr Soc. 2022;70(6):1629–1641. doi: 10.1111/jgs.17808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baird M.D., Dubowitz T., Cantor J., Troxel W.M. Examining the impact of employment status on sleep quality during the COVID-19 pandemic in two low-income neighborhoods in Pittsburgh, PA. Sleep. 2022;45(3) doi: 10.1093/sleep/zsab303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Antino M., Ruiz-Zorrilla P., Sanz-Vergel A.I., Leon-Perez J.M., Rodriguez-Munoz A. The role of job insecurity and work-family conflict on mental health evolution during COVID-19 lockdown. Eur J Work Organ Psychol. 2022;18:667–684. [Google Scholar]
- 22.Lima M.G., Barros M.B.A., Szwarcwald C.L., et al. Association of social and economic conditions with the incidence of sleep disorders during the COVID-19 pandemic. Cad Saude Publica. 2021;37(3) doi: 10.1590/0102-311X00218320. [DOI] [PubMed] [Google Scholar]
- 23.Simonelli G., Petit D., Delage J.P., et al. Sleep in times of crises: a scoping review in the early days of the COVID-19 crisis. Sleep Med Rev. 2021;60 doi: 10.1016/j.smrv.2021.101545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Strassle P.D., Stewart A.L., Quintero S.M., et al. COVID-19–related discrimination among racial/ethnic minorities and other marginalized communities in the United States. Am J Public Health. 2022;112(3):453–466. doi: 10.2105/AJPH.2021.306594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.All of Us Research Program, Denny JC, Rutter JL, Goldstein DB, Philippakis A, Smoller JW, et al. N Engl J Med. 2019; 381(7):668-676. [DOI] [PMC free article] [PubMed]
- 26.Cella D., Choi S.W., Condon D.M., et al. PROMIS(®) adult health profiles: efficient short-form measures of seven health domains. Value Health. 2019;22(5):537–544. doi: 10.1016/j.jval.2019.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cella D., Riley W., Stone A., et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.PROMIS Score Cut Points. Available at: https://www.healthmeasures.net/score-and-interpret/interpret-scores/promis/promis-score-cut-points. Accessed March 3, 2023.
- 29.Kroenke K., Spitzer R.L., Williams J.B., Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 30.Tennant P.W.G., Murray E.J., Arnold K.F., et al. Use of directed acyclic graphs (DAGs) to identify confounders in applied health research: review and recommendations. Int J Epidemiol. 2020;50(2):620–632. doi: 10.1093/ije/dyaa213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Borrescio-Higa F., Droller F., Valenzuela P. Financial distress and psychological well-being during the COVID-19 pandemic. Int J Public Health. 2022;67 doi: 10.3389/ijph.2022.1604591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garon T., Dunn A., Celik N., Robb H. 2020 Trends report. October 2020.
- 33.Budig M.J., Lim M., Hodges M.J. Racial and gender pay disparities: the role of education. Soc Sci Res. 2021;98 doi: 10.1016/j.ssresearch.2021.102580. [DOI] [PubMed] [Google Scholar]
- 34.Shi L., Zhang D., Martin E., et al. Racial discrimination, mental health and behavioral health during the COVID-19 pandemic: a national survey in the United States. J Gen Intern Med. 2022;37(1):2496–2504. doi: 10.1007/s11606-022-07540-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gaston S.A., Feinstein L., Slopen N., Sandler D.P., Williams D.R., Jackson C.L. Everyday and major experiences of racial/ethnic discrimination and sleep health in a multiethnic population of U.S. women: findings from the Sister Study. Sleep Med. 2020;71:97–105. doi: 10.1016/j.sleep.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bailey Z.D., Krieger N., Agénor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- 37.Duran D.G., Pérez-Stable E.J. Novel approaches to advance minority health and health disparities research. Am J Public Health. 2019;109(S1):S8–s10. doi: 10.2105/AJPH.2018.304931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rothman K.J. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43–46. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material