Abstract
Purpose
Burnout has been well examined among physicians and other high-wage, high-autonomy healthcare positions. However, lower-wage healthcare workers with less workplace autonomy (e.g., medical assistants, nurses’ aides) represent a substantial proportion of the workforce, but remain understudied. We aimed to examine the effects of burnout on psychotropic medication use and misuse and whether these effects differed by occupational level.
Methods
In March 2022, we collected data from a diverse sample of US healthcare workers (N = 200) and examined the cross-sectional relationship between burnout and changes in prescribed psychotropic medication (i.e., starting, stopping, and/or having a change in the dose/frequency) during the COVID-19 pandemic. We also separately examined the relationship between burnout and psychotropic medication misuse (i.e., without a prescription, in greater amounts, more often, longer than prescribed, and/or for a reason other than prescribed). We stratified models by occupational level (prescribers/healthcare administrators vs. other healthcare workers).
Results
Greater burnout was associated with higher odds of changes in prescribed psychotropic medication among prescribers/healthcare administrators (aOR = 1.23, 95% CI 1.01, 1.48), but not among other healthcare workers (aOR = 1.04, 95% CI 0.98, 1.10). Greater burnout was not associated with psychotropic medication misuse among prescribers/healthcare administrators (aOR = 0.96, 95% CI 0.82, 1.12) but was associated with increased odds of psychotropic medication misuse among other healthcare workers (aOR = 1.07, 95% CI 1.01, 1.14).
Conclusions
Potential disparities in help-seeking and healthcare access might manifest in non-medical use of prescription drugs among some healthcare workers, which has implications for worker safety and well-being.
Keywords: Burnout, Healthcare workers, Psychotropic medication, Non-medical use
Introduction
Over 20 million people in the United States (US) are employed in the Healthcare and Social Assistance sector [1]. Although people working in this sector have always been susceptible to occupational burnout (i.e., a state of mental exhaustion, depersonalization, and decreased sense of personal accomplishment) [2], the COVID-19 pandemic has exacerbated these experiences to unprecedented levels [3]. Numerous studies published in the post-pandemic era have demonstrated that burnout is a prevalent and systemic issue among healthcare workers around the world [4-10]. Indeed, a recent study demonstrated that healthcare workers experienced greater burnout during the COVID-19 pandemic than those working in other high-stress occupations, like first responders and volunteer disaster relief workers, in addition to experiencing greater burnout than the general population [10]. The US has experienced a series of healthcare resource shortages and continues to have one of the highest COVID-19 mortality rates per capita [11], resulting in substantial strains on the US healthcare workforce. Moreover, a recent Surgeon General’s Advisory highlights a critical call to action to better understand and address burnout among US healthcare workers [12].
Research has shown that burnout is a common problem among physicians [2, 13-16] and is associated with $4.6 billion in costs related to turnover and reduced clinical hours each year [17]. Physician burnout has also been associated with increased mental health symptomatology [18], reduced help-seeking [19], increased medical errors, and other negative sequelae [20]. While some research suggests that burnout is also prevalent among nurses [21], much less is known about other types of healthcare occupations, particularly lower-wage healthcare support roles characterized by high job demands and low autonomy in the workplace. Importantly, a Mercer Health Care Market Analysis report projected a national shortage of more than 3 million low-wage health workers within the next 5 years [22], and burnout among this population has been identified as a critical problem expected to exacerbate this labor shortage [12].
A recent study of healthcare workers in critical care units of English hospitals [23] suggests that nearly half of hospital-based healthcare workers experience clinically significant symptoms of problem drinking, anxiety, depression, or PTSD. Importantly, findings from this study demonstrated that physicians had significantly better mental health than other healthcare occupations working in the same healthcare settings, suggesting that there may be important differences according to occupational level that have not been well explored. Further, research conducted by Prins and colleagues [24] examined more than 12,000 full-time workers and demonstrated that occupations characterized by higher authority, autonomy, and expertise were associated with lower odds of a range of psychiatric symptomatology. Despite the compelling evidence that work-related stressors have a deleterious effect on physicians, those working in lower-wage healthcare positions characterized by high demands and low autonomy may be at even greater risk.
The mental exhaustion, depersonalization, and decreased sense of personal accomplishment experienced by healthcare workers can result in a number of mental and physical responses [2], which can be understood within the context of stress and coping. Stress has been hypothesized to be a transactional process (i.e., involves a transaction between an individual and their environment), and coping is thought to be informed by both cognitive appraisal of the stressor and the resulting emotional response [25]. The use and misuse of substances as an external way to modify emotions have long been hypothesized as a coping mechanism in response to stress (i.e., self-medication theory) [26].
A recent systematic review of coping and burnout during the COVID-19 pandemic demonstrates that healthcare workers employ a variety of coping mechanisms [27]. However, research suggests that healthcare workers may be more likely to employ maladaptive coping strategies (e.g., self-distraction) over other more adaptive approaches [28] to cope with burnout. For example, an examination of the behaviors of a sample of Kenyan healthcare workers before and during the COVID-19 pandemic suggests that there was an increase in the prevalence self-medication [29]. Moreover, a study of physicians practicing medicine in European countries showed that greater burnout was associated with a higher likelihood of psychotropic medication use [30], suggesting that psychotropic medications may be used as a coping mechanism in this occupational context. Given the self-medication theory and that psychotropic medication use is highly prevalent among adults in the US [31, 32], it is possible that burnout among healthcare workers might manifest in both prescribed psychotropic medication use and misuse (i.e., non-medical use). However, the extent to which burnout affects these outcomes among non-physician healthcare workers is largely unknown. Further, there may be important differences in the effects of burnout on psychotropic medication use and misuse among different occupational levels.
Current study
To begin to address some of the identified gaps in the literature, the current study examines the effects of burnout on prescribed psychotropic medication use and misuse (i.e., non-medical use) among a sample of US healthcare workers during the COVID-19 pandemic. Given the varying levels of job demands, autonomy, wages, and social supports associated with different healthcare occupations and findings from prior research regarding the varying psychiatric symptomatology of different occupational levels [23, 24], we hypothesized that there might be differential effects of burnout on psychotropic medication use and misuse by occupational level (i.e., prescriber/healthcare administrator vs. other healthcare workers).
Methods
Participants and procedure
In March 2022, we recruited a diverse sample of US healthcare workers (N = 200) using targeted social media recruitment methods. To be eligible for the study, participants needed to be at least 18 years of age and currently working for wages in one or more of the following healthcare settings in the US: hospital, ambulatory or outpatient clinic, nursing or residential facility, social assistance program, and/or home healthcare. Participants also needed to be able to read and understand the English language and be willing and able to participate. Participants completed one online survey at a place of their choosing, which took approximately 60 min to complete. Upon completion, participants were compensated in the form of an electronic $50 gift card. The study protocol was approved by the Institutional Review Board of the University of Illinois Urbana-Champaign. A total of 284 individuals were eligible for inclusion in the study. Of those, 200 (70.4%) agreed to participate and completed the survey. We conducted sensitivity analyses and did not find any statistically significant differences in age, gender identity, or work setting between participants, who were eligible and participated and participants who were eligible but did not participate.
Our sample included a broad range of healthcare occupations, including low-wage healthcare support roles (e.g., nursing assistants, dietary aides, administrative support staff), licensed practical nurses, registered nurses, psychologists, case managers, social workers, physical therapists, mid-level providers (e.g., nurse practitioners, physician assistants), both resident and attending physicians, pharmacists, dentists, as well as healthcare administrators. The sample worked in a variety of healthcare settings, including ambulatory/outpatient clinics, home healthcare, hospitals, social assistance programs, and nursing/residential facilities. Additional details about the study sample are shown in Table 1.
Table 1.
Sample characteristics (N = 200 healthcare workers)
| Overall sample (N = 200) % (n) or mean (± SD) | Prescriber/administrator (n = 49) % (n) or mean (± SD) | Other healthcare worker (n = 151) % (n) or mean (± SD) | |
|---|---|---|---|
| Age, years | 30.8 (± 7.3) | 31.5 (± 4.2) | 30.6 (± 8.1) |
| Gender identity | – | – | – |
| Man | 32.5% (65) | 53.1% (26) | 25.8% (39) |
| Woman | 66.5% (133) | 46.9% (23) | 72.9% (110) |
| Non-binary/genderqueer | 1.0% (2) | 0.0% (0) | 1.3% (2) |
| Race/ethnicity | – | – | – |
| Non-Hispanic White | 54.5% (109) | 42.9% (21) | 58.3% (88) |
| Non-Hispanic Black | 17.5% (35) | 12.2% (6) | 19.2% (29) |
| Non-Hispanic Asian | 14.0% (28) | 34.7% (17) | 7.3% (11) |
| Non-Hispanic American Indian or Alaska Native | 1.0% (2) | 2.0% (1) | 0.7% (1) |
| Hispanic or Latinx | 10.0% (20) | 4.1% (2) | 11.9% (18) |
| Other | 3.0% (6) | 4.1% (2) | 2.7% (4) |
| Education | – | – | – |
| High school diploma or equivalent (GED) | 3.0% (6) | 0.0% (0) | 4.0% (6) |
| Some college (no degree) | 5.0% (10) | 0.0% (0) | 6.6% (10) |
| Associate’s/other technical 2-year degree | 14.0% (28) | 0.0% (0) | 18.5% (28) |
| Bachelor’s/other 4-year degree | 35.5% (71) | 0.0% (0) | 47.0% (71) |
| Graduate or professional degree | 42.5% (85) | 100.0% (49) | 23.8% (36) |
| Family income | – | – | – |
| Less than $10,000 | 0.5% (1) | 0.0% (0) | 0.7% (1) |
| $10,000–$19,999 | 3.5% (7) | 0.0% (0) | 4.6% (7) |
| $20,000–$29,999 | 2.5% (5) | 0.0% (0) | 3.3% (5) |
| $30,000–$39,999 | 4.5% (9) | 0.0% (0) | 6.0% (9) |
| $40,000–$49,999 | 10.0% (20) | 4.1% (2) | 11.9% (18) |
| $50,000–$74,999 | 19.5% (39) | 20.4% (10) | 19.2% (29) |
| $75,000–$99,999 | 20.0% (40) | 12.2% (6) | 22.5% (34) |
| $100,000–$149,999 | 24.0% (48) | 30.6% (15) | 21.9% (33) |
| $150,000 or more | 15.5% (31) | 32.7% (16) | 9.9% (15) |
| Years in job | – | – | – |
| Less than 1 year | 14.5% (29) | 10.2% (5) | 15.9% (24) |
| 1–5 years | 61.0% (122) | 77.6% (38) | 55.6% (84) |
| 6–10 years | 17.5% (35) | 8.2% (4) | 20.5% (31) |
| 11–20 years | 6.0% (12) | 4.1% (2) | 6.6% (10) |
| More than 20 years | 1.0% (2) | 0.0% (0) | 1.3% (2) |
| Hospital setting | – | – | – |
| No | 46.0% (92) | 14.3% (7) | 56.3% (85) |
| Yes | 54.0% (108) | 85.7% (42) | 43.7% (66) |
SD standard deviation
Measures
Burnout
We assessed burnout with the English version of the Oldenburg Burnout Inventory (OLBI) [34, 35], a 16-item measure of occupational burnout severity. The OLBI assesses two core dimensions of burnout: exhaustion and disengagement (from work), by asking respondents to rate their level of agreement on a 4-point Likert scale (from strongly disagree to strongly agree) with a series of statements related to their work experience. Total scores range from 16 to 64, with higher scores indicating greater burnout. Example items include “Lately, I tend to think less at work and do my job almost mechanically”; “During my work, I often feel emotionally drained”; and “After my work, I usually feel worn out and weary.” The OLBI has been shown to be a valid and reliable measure of burnout across a diverse range of occupations and populations [34, 36] and had good internal consistency in our sample (α = 0.86). Total OLBI was parameterized as a count variable in all analyses.
Changes in psychotropic medication
To assess changes in prescribed psychotropic medication use among this sample of healthcare workers, we used the following lead-in: “Many people are prescribed psychiatric medications. These are medications are for your mental health, including anti-depressant medications, anti-anxiety medications, anti-psychotic medications, mood stabilizer medications, and stimulant medications for conditions like ADHD. Answer the following questions about your use of prescribed psychiatric medications.” Participants were asked a series of questions related to their medication use, including “Are you currently prescribed any psychiatric medication(s) by a healthcare provider?”; “During the COVID-19 pandemic, did you start taking any new psychiatric medication(s)?”; “During the COVID-19 pandemic, did you stop taking any psychiatric medication(s)?” and “During the COVID-19 pandemic, did your dose or frequency of psychiatric medication(s) change?” Participants were also allowed to specify which medications they were currently taking and those that they had started, stopped, or changed during the COVID-19 pandemic. Given that finding the appropriate type(s) and dose(s) of psychotropic medication(s) to treat a patient’s mental health symptomatology can require trial and error [37-40], we generated a dichotomous variable that characterized any changes to psychotropic medications based on a medical provider’s recommendation. We coded all participants who reported starting, stopping, and/or having a change in the dose/frequency of any of their prescribed psychiatric medication during the COVID-19 pandemic as “Yes” and those who did not as “No.”
Psychotropic medication misuse
We assessed healthcare workers’ psychotropic medication misuse in the past three months with the National Institute on Drug Abuse (NIDA) Modified Alcohol, Smoking and Substance Involvement Screening Test (ASSIST), which has been shown to be valid and reliable across a diverse range of settings and cultures [41]. Psychotropic medication misuse was defined as the (non-medical) use of prescription stimulants (e.g., Ritalin, Concerta, Dexedrine, Adderall), sedatives and sleeping medications (e.g., Valium, Serepax, Ativan, Xanax), or other psychotropic medications “on your own, that is either without a doctor’s prescription, in greater amounts, more often, or longer than prescribed, or for a reason other than a doctor said you should use them” [41]. Psychotropic medication misuse was assessed with the following question: “In the past three months, how often have you used [substance]?” Any use in the past three months was considered a positive screen for psychotropic medication misuse and was dichotomized (no/yes) in our analyses.
Occupational level
Participants reported their type of occupation in the healthcare sector. To differentiate between high-earning high-autonomy positions from other roles, we first grouped together healthcare administrators and prescribers (e.g., physicians, nurse practitioners, physician assistants) and then grouped other healthcare professionals together (e.g., registered nurses, nursing assistants, dietary aides, administrative support staff), resulting in a dichotomous occupational level variable (healthcare administrator/prescriber vs. other healthcare worker).
Covariates
Age Participants self-reported their age in years. Given that burnout is more prevalent among younger healthcare workers [5] and that there are notable age differences in the rates of psychotropic medication use [31, 42, 43] and misuse [44], we included age in years as a covariate in all adjusted models.
Gender identity All participants self-reported their gender identity (i.e., man, woman, non-binary, genderqueer, or other gender). Rates of psychological symptomatology and substance use are high among gender minorities [45], and there are significant differences in substance use patterns [44] and the prevalence of psychiatric medication use between men and women [43]. Additionally, some evidence suggests that there may be gender-specific differences in the effects of burnout among healthcare workers [46, 47]. As such, we included gender identity in all of our adjusted models to account for its potential confounding effects.
Years worked in current job Participants were asked to indicate the number of years that they had been working in their current healthcare job at the time of their survey. Findings regarding the length of time in job and burnout are mixed. Some studies suggest that burnout tends to be more prevalent among early-career workers [48], while others suggest that those with a longer length of service are at greater risk [49]. Years in job was included as an ordinal variable (i.e., less than 1 year, 1–5 years, 6–10 years, 11–20 years) in all adjusted models.
Type of healthcare setting Although burnout is prevalent across all healthcare settings [50], there is substantial evidence suggesting that those working in hospital settings may be especially vulnerable [51-53]. In order to address these potential differences in the effects of burnout on psychotropic medication use and misuse, we included type of healthcare setting (i.e., hospital setting vs. non-hospital setting) in all adjusted regression models.
Data analysis
First, we used descriptive statistics to characterize our overall sample and by occupation type (i.e., prescriber or healthcare administrator vs. other healthcare workers). Second, to examine the cross-sectional effects of burnout on starting, stopping, or having a change in dose and/or frequency of psychotropic medication, we ran separate logistic regression models stratified by occupation type. Next, we also examined the cross-sectional effects of burnout on psychotropic medication misuse by running separate logistic regression models stratified by occupation type. Odds ratios (ORs) and 95% confidence intervals (CIs) are reported. We then added age, gender identity, years worked in current job, and type of healthcare setting as covariates to all regression models and report adjusted odds ratios (aORs) and 95% CIs.
Results
Descriptive results
This sample of healthcare workers represented 28 different US states plus Washington, DC, ranged in age from 19 to 58 years, included men (n = 65), women (n = 133), and non-binary/genderqueer people (n = 2), and the sample was racially and ethnically diverse. Although the sample comprised predominantly of women (66.5%), this is consistent with demographic estimates of healthcare workers nationally [33]. Among this sample of healthcare workers, the mean (± SD) OLBI score was 41.4 (± 7.0). Prescribers/healthcare administrators had a significantly lower mean total burnout score, exhaustion subscale score, and disengagement subscale score than other healthcare workers (Fig. 1). More than 1 in 5 healthcare workers (21.0%) reported currently being prescribed psychotropic medication(s). Overall, the prevalence of starting, stopping, and/or having a change in the dose/frequency of prescribed psychotropic medication during the COVID-19 pandemic was 22.5% (Table 2) and did not significantly differ by occupational level (prescriber/healthcare administrators: 20.4% vs. other healthcare workers: 23.2%; p > 0.10). Participants indicated that these prescriptions included anti-anxiety, anti-depressant, mood stabilizer, and sleeping medications. The overall prevalence of psychotropic medication misuse (i.e., non-medical use) was 21.0%, with a trend-level difference between prescribers/healthcare administrators (12.2%) and other healthcare workers (23.8%; p < 0.10). Among those reporting psychotropic medication misuse (n = 42), 78.6% reported non-medical use of prescription sedatives and sleeping medications (e.g., Valium, Serepax, Ativan, Xanax), 26.2% reported non-medical use of prescription stimulants (e.g., Ritalin, Concerta, Dexedrine, Adderall), and 7.1% reported non-medical use of other psychotropic medications (e.g., Zoloft, Trazodone, Lamictal, Seroquel).
Fig. 1.
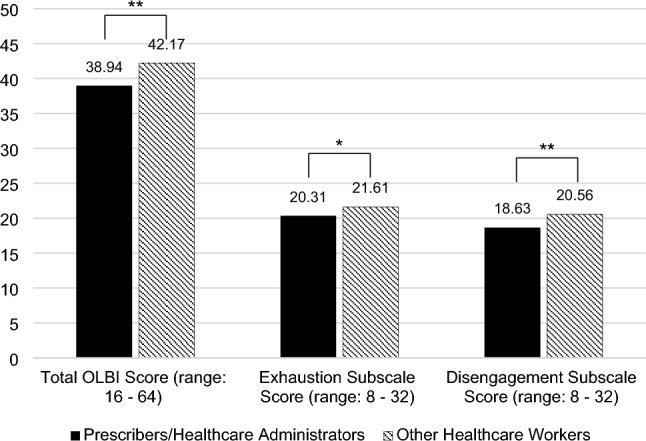
Mean Oldenburg Burnout Inventory scores by occupation. **p < 0.01, *p < 0.05; OLBI Oldenburg Burnout Inventory
Table 2.
Overall sample prevalence of outcomes
| % (n) | |
|---|---|
| Any change in prescribed psychotropic medication | 22.5% (45) |
| Started new psychotropic medication | 18.5% (37) |
| Stopped psychotropic medication | 4.0% (8) |
| Change in the dose/frequency of psychotropic medication | 13.0% (26) |
| Any psychotropic medication misuse | 21.0% (42) |
| Prescription stimulant misuse | 5.5% (11) |
| Prescription sedative or sleeping medication misuse | 16.0% (32) |
| Other psychotropic medication misuse | 1.5% (3) |
Effect of burnout on starting, stopping, or having a change in dose/frequency of psychotropic medication
Among healthcare prescribers and administrators, greater burnout was associated with higher odds of starting, stopping and/or having a change in their prescribed psychotropic medication (OR = 1.21, 95% CI 1.03, 1.42; Table 3). This association remained statistically significant after controlling for age, gender identity, years worked in job, and whether they worked in a hospital setting (aOR = 1.23, 95% CI 1.01, 1.48). However, among other healthcare workers, there was no association between burnout and the odds of starting, stopping and/or having a change in prescribed psychotropic medication in unadjusted (OR = 1.04, 95% CI 0.99, 1.10) and adjusted models (aOR = 1.04, 95% CI 0.98, 1.10).
Table 3.
Effect of burnout on starting, stopping, or having a change in dose/frequency of psychotropic medication by occupation type
| Starting, stopping, or changing psychotropic medication, prescriber/administrator (n = 49) | Starting, stopping, or changing psychotropic medication, other healthcare worker (n = 151) | |||
|---|---|---|---|---|
| OR (95% CI) | aOR (95% CI) | OR (95% CI) | aOR (95% CI) | |
| Oldenburg Burnout Inventory score | 1.21 (1.03, 1.42)* | 1.23 (1.01, 1.48)* | 1.04 (0.99, 1.10) | 1.04 (0.98, 1.10) |
| Age | 0.94 (0.76, 1.15) | 1.01 (0.96, 1.07) | ||
| Gender identity | – | – | ||
| Man | Referent | Referent | ||
| Woman | 6.13 (0.90, 41.87) | 1.17 (0.45, 3.10) | ||
| Non-binary/genderqueer | NAa | NAb | ||
| Years in job | 0.82 (0.19, 3.55) | 1.04 (0.60, 1.80) | ||
| Hospital setting | – | – | ||
| No | Referent | Referent | ||
| Yes | 1.07 (0.12, 9.76) | 0.59 (0.26, 1.35) | ||
OR odds ratio, aOR adjusted odds ratio, CI confidence interval, NA not applicable (omitted from model)
*p < 0.05
aNo prescribers or healthcare administrators identified as non-binary or genderqueer
bBoth participants who identified as non-binary, genderqueer, or other gender reported starting, stopping, or having a change in dose/frequency of psychotropic medication
Boldface text indicates statistically significant
Effect of burnout on psychotropic medication misuse
There was no association between the severity of burnout and the odds of psychotropic medication misuse among prescribers/healthcare administrators (OR = 0.97, 95% CI 0.85, 1.10; Table 4). The effect remained non-significant after controlling for relevant covariates (aOR = 0.96, 95% CI 0.82, 1.12). However, among other healthcare workers, greater burnout was associated with higher odds of psychotropic medication misuse (OR = 1.06, 95% CI 1.01, 1.14), and this effect remained statistically significant in our adjusted model (aOR = 1.07, 95% CI 1.01, 1.14).
Table 4.
Effect of burnout on psychotropic medication misuse
| Psychotropic medication misuse, prescriber/administrator (n = 49) | Psychotropic medication misuse, other healthcare worker (n = 151) | |||
|---|---|---|---|---|
| OR (95% CI) | aOR (95% CI) | OR (95% CI) | aOR (95% CI) | |
| Oldenburg Burnout Inventory score | 0.97 (0.85, 1.10) | 0.96 (0.82, 1.12) | 1.06 (1.01, 1.12)* | 1.07 (1.01, 1.14)* |
| Age | 0.80 (0.59, 1.09) | 1.00 (0.95, 1.06) | ||
| Gender identity | – | – | ||
| Man | Referent | Referent | ||
| Woman | 3.32 (0.44, 24.91) | 0.43 (0.18, 1.05) | ||
| Non-binary/genderqueer | NAa | NAb | ||
| Years in job | 2.63 (0.40, 17.51) | 1.59 (0.92, 2.75) | ||
| Hospital setting | – | – | ||
| No | Referent | Referent | ||
| Yes | 1.31 (0.11, 16.20) | 0.96 (0.43, 2.15) | ||
OR odds ratio, aOR adjusted odds ratio, CI confidence interval, NA not applicable (omitted from model)
*p < 0.05
aNo prescribers or healthcare administrators identified as non-binary or genderqueer
bNeither participant who identified as non-binary, genderqueer, or other gender reported psychotropic medication misuse
Boldface text indicates statistically significant
Discussion
The current study provides compelling evidence that not only is burnout a prevalent and systemic issue in healthcare settings, but that greater burnout is associated with a greater likelihood of psychotropic medication use and misuse among healthcare workers. Notably, these effects differed by occupational level. While greater burnout was associated with starting, stopping, and/or having a change in prescribed psychotropic medication among healthcare prescribers and administrators, greater burnout was associated with psychotropic medication misuse among other healthcare workers. Consistent with other research that demonstrated less mental health symptomatology among higher-wage occupations [23, 24], findings from the current study suggest that, on average, healthcare prescribers and administrators experience significantly lower levels of burnout than other healthcare workers.
While poverty and substance misuse are inextricably and bidirectionally related, differences may not be explained by social stratification based on individual attributes alone (e.g., socioeconomic status). Rather, mechanisms that produce social stratification may increase the risk for problematic substance use. For example, a study examining data from the 1983 to 2017 waves of the Panel Study of Income Dynamics [54] showed that greater labor exploitation (i.e., working unpaid hours) was associated with greater psychological distress. Thus, despite the compelling evidence that work-related stressors have a deleterious effect on physicians, those working in lower-wage healthcare positions characterized by high demands and low autonomy may be at even greater risk.
Although self-medication theory posits that people use substances as an external way to modify their emotions [26], self-medication theory has been criticized for oversimplifying the underlying causes of substance use and misuse [55]. The differential effects of burnout on psychotropic medication use and misuse by occupational level observed in the current study might be explained by barriers to help-seeking and access to care, particularly among lower-wage healthcare workers. A national examination of low-income adults in the US with psychological distress shows that although the prevalence of health insurance among this population has increased over time, mental health service use has not changed and structural barriers have increased [56]. It is possible that the psychotropic medication misuse observed in the current study might be a manifestation of these barriers. Many physicians report that they would be reluctant to seek professional care for a serious emotional problem due to fear of stigma and professional consequences [19]. However, recent population data suggests that the COVID-19 pandemic was associated with a substantial increase in accessing mental health services among physicians [57]. This aligns with our finding of increased burnout among physicians and healthcare administrators being associated with higher odds of starting, stopping, and/or having a change in their prescribed psychotropic medication.
Research also suggests that there are systematic differences in the demographic characteristics of people who are and are not prescribed certain psychotropic medications, which may also affect the results observed in this study. For example, one study suggests that people who are older and non-Hispanic White are more likely to be prescribed benzodiazepines than people who are younger or minoritized [58]. Additionally, studies suggest that benzodiazepine prescribing is also likely to be influenced by the gender of both the prescriber and the patient. Some research suggests that men are more likely to prescribe benzodiazepines [59, 60], while women are more likely to be prescribed benzodiazepines [60]. Given these prescribing patterns, it is possible that the prescribers/healthcare administrators in the current study may be more likely to be prescribed psychotropic medications for their psychological distress than other healthcare workers.
While some research suggests that personality trait characteristics, like psychological hardiness (i.e., dispositional resilience) may be appropriate intervention targets for reducing burnout [10], systemic workplace contributors to burnout should also be acknowledged and addressed. For example, low perceived safety in the workplace and redeployment to an unfamiliar work environment have both been associated with increased burnout among healthcare workers from various countries [16]. Likewise, chronic understaffing is associated with higher levels of burnout [61], and in the context in the of scarce medical resources, some healthcare workers have been faced with having to prioritize the care of patients who are more likely to survive, resulting in intense ethical dilemmas [62]. Moreover, women are overrepresented in the low-wage healthcare workforce [33] and are more likely to be exposed to biological risks and experience work-related stress and burnout [63]. Coupled with barriers to help-seeking and access to care, lower-wage healthcare workers may be especially vulnerable to these systemic issues.
Limitations
Our findings should be interpreted within the context of this study’s limitations. First, all data are cross-sectional, so we are limited in our ability to draw causal conclusions from these data. It is possible that there are additional factors which might partially explain the associations observed in this study that should be examined in future research (e.g., hours worked, mental health, social support). Second, all data were self-reported and as such, are susceptible to social desirability bias. However, confidential computer-assisted interviewing has been shown to produce valid estimates of substance use, mental health symptomatology, and other sensitive topics [64-68] and is generally preferred by research participants over face-to-face interview methods [64, 69]. Third, although our sample of healthcare workers was diverse with respect to demographic characteristics, data were collected using non-probability sampling methods and our findings may not necessarily be representative of healthcare workers nationally. Our sample was relatively young, and prior research shows that burnout is more prevalent among younger healthcare workers [5] and young adults are more likely to misuse prescription medications than their older counterparts [44]. Additionally, given that our sample was recruited via social media and participants were given an incentive, the current study is subject to selection bias. However, social media has been shown to be advantageous for observational study recruitment [70] and is frequently more effective than traditional methods (e.g., print, e-mail) [71]. Moreover, appropriate research payment amounts have been shown to be non-coercive and increase participant satisfaction [72]. Fourth, our sample size may have limited our statistical power to detect significant effects, increasing the probability of a Type II error. However, given the findings of the current study, it is possible that the true effect of burnout on psychotropic medication use and misuse may be even stronger than what is observed here. Future research should examine these effects longitudinally and among a larger sample of healthcare workers to better understand how burnout may affect these outcomes over time.
Strengths
Despite these limitations, our study has several strengths that should also be noted. First, we examined a critically important and timely issue among a large and growing population [1]. Second, the inclusion of a broad range of healthcare occupations is important, given that much of the research on occupational burnout in healthcare settings tends to focus on physicians [e.g., 2, 13–16]. Specifically, healthcare workers in lower-wage positions that are characterized by high demands and low autonomy remain understudied and experience unique occupational hazards. Finally, findings from the current study are bolstered by the use of a validated measure of non-medical use of psychotropic mediations [41] and a diverse sample recruited from across the US that is demographically comparable to healthcare workers nationally [33].
Conclusions and future directions
Results from the current study suggest that occupational burnout is not only prevalent among a broad range of healthcare workers, but that it is associated with both psychotropic medication use and misuse on the basis of occupational level. These results point to potential disparities in help-seeking and healthcare access among lower-wage healthcare workers and have implications for the safety and well-being of this population. In addition to addressing systemic drivers of occupational burnout, universal screening for burnout, robust employee assistance programs, and workplace interventions are recommended.
Acknowledgements
This research was supported by the Mary Jane Neer Fund of the College of Applied Health Sciences at the University of Illinois Urbana-Champaign. The authors would like to thank the following research assistants who helped to collect the data presented in the current study: Jaqueline Carrillo, Nivin George, Michael Knipp, Susana Lopez, Wendy Marinez, Yasmeen Scott, Ja’Resa Stockdale, and Eshana Vora.
Author contributions
RH: conceived of and designed the study, conducted the formal analysis, and wrote the first draft of the manuscript with sections contributed by SL and RS. All authors reviewed and approved the final manuscript.
Data availability
The data that support the findings of this study are available on request from the corresponding author, RAH.
Declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
References
- 1.U.S. Bureau of Labor Statistics (2021) Workforce Statistics. https://www.bls.gov/iag/tgs/iag62.htm#workforce. Accessed 13 Jan 2022
- 2.Lacy BE, Chan JL. Physician burnout: the hidden health care crisis. Clin Gastroenterol Hepatol. 2018;16(3):311–317. doi: 10.1016/j.cgh.2017.06.043. [DOI] [PubMed] [Google Scholar]
- 3.Restauri N, Sheridan AD. Burnout and posttraumatic stress disorder in the coronavirus disease 2019 (COVID-19) pandemic: intersection, impact, and interventions. J Am Coll Radiol. 2020;17(7):921–926. doi: 10.1016/j.jacr.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raudenská J, Steinerová V, Javůrková A, Urits I, Kaye AD, Viswanath O, Varrassi G. Occupational burnout syndrome and post-traumatic stress among healthcare professionals during the novel coronavirus disease 2019 (COVID-19) pandemic. Best Pract Res Clin Anaesthesiol. 2020;34(3):553–560. doi: 10.1016/j.bpa.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses' burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J Adv Nurs. 2021;77(8):3286–3302. doi: 10.1111/jan.14839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manzano García G, Ayala Calvo JC. The threat of COVID-19 and its influence on nursing staff burnout. J Adv Nurs. 2021;77(2):832–844. doi: 10.1111/jan.14642. [DOI] [PubMed] [Google Scholar]
- 7.Barello S, Palamenghi L, Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020;290:113129. doi: 10.1016/j.psychres.2020.113129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tan BYQ, Kanneganti A, Lim LJH, Tan M, Chua YX, Tan L, Sia CH, Denning M, Goh ET, Purkayastha S, Kinross J, Sim K, Chan YH, Ooi SBS. Burnout and associated factors among health care workers in singapore during the COVID-19 pandemic. J Am Med Dir Assoc. 2020;21(12):1751–1758.e1755. doi: 10.1016/j.jamda.2020.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sriharan A, West KJ, Almost J, Hamza A. COVID-19-related occupational burnout and moral distress among nurses: a rapid scoping review. Nurs Leadersh (Tor Ont) 2021;34(1):7–19. doi: 10.12927/cjnl.2021.26459. [DOI] [PubMed] [Google Scholar]
- 10.Vagni M, Maiorano T, Giostra V, Pajardi D, Bartone P. Emergency stress, hardiness, coping strategies and burnout in health care and emergency response workers during the COVID-19 pandemic. Front Psychol. 2022;13:918788. doi: 10.3389/fpsyg.2022.918788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Our World in Data (2022) Coronavirus Source Data. https://ourworldindata.org/coronavirus-source-data. Accessed 11 July 2022
- 12.U.S. Department of Health and Human Services PHS, Office of the Surgeon General, (2022) Addressing Health Worker Burnout: The U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce. https://www.surgeongeneral.gov/burnout. Accessed 15 July 2022 [PubMed]
- 13.West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516–529. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- 14.Yates SW. Physician stress and burnout. Am J Med. 2020;133(2):160–164. doi: 10.1016/j.amjmed.2019.08.034. [DOI] [PubMed] [Google Scholar]
- 15.Lancet T. Physician burnout: a global crisis. Lancet. 2019;394(10193):93. doi: 10.1016/S0140-6736(19)31573-9. [DOI] [PubMed] [Google Scholar]
- 16.Denning M, Goh ET, Tan B, Kanneganti A, Almonte M, Scott A, Martin G, Clarke J, Sounderajah V, Markar S, Przybylowicz J, Chan YH, Sia CH, Chua YX, Sim K, Lim L, Tan L, Tan M, Sharma V, Ooi S, Winter Beatty J, Flott K, Mason S, Chidambaram S, Yalamanchili S, Zbikowska G, Fedorowski J, Dykowska G, Wells M, Purkayastha S, Kinross J. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the Covid-19 pandemic: a multinational cross-sectional study. PLoS One. 2021;16(4):e0238666. doi: 10.1371/journal.pone.0238666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Han S, Shanafelt TD, Sinsky CA, Awad KM, Dyrbye LN, Fiscus LC, Trockel M, Goh J. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170(11):784–790. doi: 10.7326/m18-1422. [DOI] [PubMed] [Google Scholar]
- 18.Hyman SA, Shotwell MS, Michaels DR, Han X, Card EB, Morse JL, Weinger MB. A survey evaluating burnout, health status, depression, reported alcohol and substance use, and social support of anesthesiologists. Anesth Analg. 2017;125(6):2009–2018. doi: 10.1213/ane.0000000000002298. [DOI] [PubMed] [Google Scholar]
- 19.Dyrbye LN, Leep Hunderfund AN, Winters RC, Moeschler SM, Vaa Stelling BE, Dozois EJ, Satele DV, West CP. The relationship between burnout and help-seeking behaviors, concerns, and attitudes of residents. Acad Med. 2021;96(5):701–708. doi: 10.1097/acm.0000000000003790. [DOI] [PubMed] [Google Scholar]
- 20.Menon NK, Shanafelt TD, Sinsky CA, Linzer M, Carlasare L, Brady KJS, Stillman MJ, Trockel MT. Association of physician burnout with suicidal ideation and medical errors. JAMA Netw Open. 2020;3(12):e2028780. doi: 10.1001/jamanetworkopen.2020.28780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bakhamis L, Paul DP, 3rd, Smith H, Coustasse A. Still an epidemic: the burnout syndrome in hospital registered nurses. Health Care Manag (Frederick) 2019;38(1):3–10. doi: 10.1097/hcm.0000000000000243. [DOI] [PubMed] [Google Scholar]
- 22.Mercer (2021) U.S. Healthcare Labor Market Report.
- 23.Greenberg N, Weston D, Hall C, Caulfield T, Williamson V, Fong K. Mental health of staff working in intensive care during Covid-19. Occup Med (Lond) 2021;71(2):62–67. doi: 10.1093/occmed/kqaa220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prins SJ, McKetta S, Platt J, Muntaner C, Keyes KM, Bates LM. Mental illness, drinking, and the social division and structure of labor in the United States: 2003–2015. Am J Ind Med. 2019;62(2):131–144. doi: 10.1002/ajim.22935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer publishing company; 1984. [Google Scholar]
- 26.Khantzian EJ. The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. The cocaine crisis. Springer; 1987. pp. 65–74. [DOI] [PubMed] [Google Scholar]
- 27.Rossi MF, Gualano MR, Magnavita N, Moscato U, Santoro PE, Borrelli I. Coping with burnout and the impact of the COVID-19 pandemic on workers’ mental health: a systematic review. Front Psych. 2023;14:1139260. doi: 10.3389/fpsyt.2023.1139260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McKinley N, McCain RS, Convie L, Clarke M, Dempster M, Campbell WJ, Kirk SJ. Resilience, burnout and coping mechanisms in UK doctors: a cross-sectional study. BMJ Open. 2020;10(1):e031765. doi: 10.1136/bmjopen-2019-031765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Onchonga D, Omwoyo J, Nyamamba D. Assessing the prevalence of self-medication among healthcare workers before and during the 2019 SARS-CoV-2 (COVID-19) pandemic in Kenya. Saudi Pharm J. 2020;28(10):1149–1154. doi: 10.1016/j.jsps.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Soler JK, Yaman H, Esteva M. Burnout in European general practice and family medicine. Soc Behav Personal Int J. 2007;35(8):1149–1150. doi: 10.2224/sbp.2007.35.8.1149. [DOI] [Google Scholar]
- 31.Brody DJ, Gu Q. Antidepressant use among adults: United States, 2015–2018. NCHS Data Brief. 2020;377:1–8. [PubMed] [Google Scholar]
- 32.Blanco C, Han B, Jones CM, Johnson K, Compton WM. Prevalence and correlates of benzodiazepine use, misuse, and use disorders among adults in the United States. J Clin Psychiatry. 2018 doi: 10.4088/JCP.18m12174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.U.S. Census Bureau (2021) 2020 American Community Survey Subject Table: Class of Worker by Sex and Median Earnings in the Past 12 Months for the Civilian Employed Population 16 Years and Over. https://www.census.gov/acs/www/data/data-tables-and-tools/subject-tables/. Accessed 28 Apr 2022
- 34.Halbesleben JRB, Demerouti E. The construct validity of an alternative measure of burnout: investigating the English translation of the Oldenburg Burnout Inventory. Work Stress. 2005;19(3):208–220. doi: 10.1080/02678370500340728. [DOI] [Google Scholar]
- 35.Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol. 2001;86(3):499. doi: 10.1037/0021-9010.86.3.499. [DOI] [PubMed] [Google Scholar]
- 36.Demerouti E, Bakker AB (2008) The Oldenburg Burnout Inventory: A good alternative to measure burnout and engagement. Handbook of stress and burnout in health care 65(7):1–25
- 37.Desmarais JE, Beauclair L, Margolese HC. Switching from brand-name to generic psychotropic medications: a literature review. CNS Neurosci Ther. 2011;17(6):750–760. doi: 10.1111/j.1755-5949.2010.00210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Holsboer F. How can we realize the promise of personalized antidepressant medicines? Nat Rev Neurosci. 2008;9(8):638–646. doi: 10.1038/nrn2453. [DOI] [PubMed] [Google Scholar]
- 39.Wade M, Tai S, Awenat Y, Haddock G. A systematic review of service-user reasons for adherence and nonadherence to neuroleptic medication in psychosis. Clin Psychol Rev. 2017;51:75–95. doi: 10.1016/j.cpr.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 40.Watts M, Murphy E, Keogh B, Downes C, Doyle L, Higgins A. Deciding to discontinue prescribed psychotropic medication: a qualitative study of service users’ experiences. Int J Ment Health Nurs. 2021;30:1395–1406. doi: 10.1111/inm.12894. [DOI] [PubMed] [Google Scholar]
- 41.WHO Assist Working Group The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- 42.Olfson M, King M, Schoenbaum M. Benzodiazepine use in the United States. JAMA Psychiat. 2015;72(2):136–142. doi: 10.1001/jamapsychiatry.2014.1763. [DOI] [PubMed] [Google Scholar]
- 43.Johansen ME. Psychiatric medication users by age and sex in the United States, 1999–2018. J Am Board Fam Med. 2021;34(4):732–740. doi: 10.3122/jabfm.2021.04.200596. [DOI] [PubMed] [Google Scholar]
- 44.SAMHSA (2020) Results from the 2019 National Survey on Drug Use and Health: Detailed Tables. https://www.samhsa.gov/data/report/2019-nsduh-detailed-tables. Accessed 1 July 2022
- 45.Newcomb ME, Hill R, Buehler K, Ryan DT, Whitton SW, Mustanski B. High burden of mental health problems, substance use, violence, and related psychosocial factors in transgender, non-binary, and gender diverse youth and young adults. Arch Sex Behav. 2020;49(2):645–659. doi: 10.1007/s10508-019-01533-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Low ZX, Yeo KA, Sharma VK, Leung GK, McIntyre RS, Guerrero A, Lu B, Sin Fai Lam CC, Tran BX, Nguyen LH, Ho CS, Tam WW, Ho RC. Prevalence of burnout in medical and surgical residents: a meta-analysis. Int J Environ Res Public Health. 2019 doi: 10.3390/ijerph16091479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lu PW, Columbus AB, Fields AC, Melnitchouk N, Cho NL. Gender differences in surgeon burnout and barriers to career satisfaction: a qualitative exploration. J Surg Res. 2020;247:28–33. doi: 10.1016/j.jss.2019.10.045. [DOI] [PubMed] [Google Scholar]
- 48.Galaiya R, Kinross J, Arulampalam T. Factors associated with burnout syndrome in surgeons: a systematic review. Ann R Coll Surg Engl. 2020;102(6):401–407. doi: 10.1308/rcsann.2020.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Miller E. The prevalence of stress and burnout in UK emergency ambulance service workers and its impact on their mental health and well-being. Br Paramed J. 2021;5(4):62–63. doi: 10.29045/14784726.2021.3.5.4.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Green S, Markaki A, Baird J, Murray P, Edwards R. Addressing healthcare professional burnout: a quality improvement intervention. Worldviews Evid Based Nurs. 2020;17(3):213–220. doi: 10.1111/wvn.12450. [DOI] [PubMed] [Google Scholar]
- 51.Sanghera J, Pattani N, Hashmi Y, Varley KF, Cheruvu MS, Bradley A, Burke JR. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting-a systematic review. J Occup Health. 2020;62(1):e12175. doi: 10.1002/1348-9585.12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lasalvia A, Amaddeo F, Porru S, Carta A, Tardivo S, Bovo C, Ruggeri M, Bonetto C. Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: a cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open. 2021;11(1):e045127. doi: 10.1136/bmjopen-2020-045127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Buran F, Altın Z. Burnout among physicians working in a pandemic hospital during the COVID-19 pandemic. Leg Med (Tokyo) 2021;51:101881. doi: 10.1016/j.legalmed.2021.101881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Prins SJ, McKetta S, Platt J, Muntaner C, Keyes KM, Bates LM. The serpent of their agonies: exploitation as structural determinant of mental illness. Epidemiology. 2021;32(2):303–309. doi: 10.1097/ede.0000000000001304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hall DH, Queener JE. Self-medication hypothesis of substance use: testing Khantzian's updated theory. J Psychoactive Drugs. 2007;39(2):151–158. doi: 10.1080/02791072.2007.10399873. [DOI] [PubMed] [Google Scholar]
- 56.Mojtabai R. U.S. health care reform and enduring barriers to mental health care among low-income adults with psychological distress. Psychiatr Serv. 2021;72(3):338–342. doi: 10.1176/appi.ps.202000194. [DOI] [PubMed] [Google Scholar]
- 57.Myran DT, Cantor N, Rhodes E, Pugliese M, Hensel J, Taljaard M, Talarico R, Garg AX, McArthur E, Liu CW, Jeyakumar N, Simon C, McFadden T, Gerin-Lajoie C, Sood MM, Tanuseputro P. Physician health care visits for mental health and substance use during the COVID-19 pandemic in Ontario, Canada. JAMA Netw Open. 2022;5(1):e2143160. doi: 10.1001/jamanetworkopen.2021.43160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jessell L, Stanhope V, Manuel JI, Mateu-Gelabert P. Factors associated with benzodiazepine prescribing in community mental health settings. J Subst Abuse Treat. 2020;109:56–60. doi: 10.1016/j.jsat.2019.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lui LMW, Lee Y, Lipsitz O, Rodrigues NB, Gill H, Ma J, Wilkialis L, Tamura JK, Siegel A, Chen-Li D, Rosenblat JD, Mansur RB, McPherson MA, McIntyre RS. The influence of prescriber and patient gender on the prescription of benzodiazepines: results from the Florida Medicaid Dataset. CNS Spectr. 2022;27(3):378–382. doi: 10.1017/S1092852921000055. [DOI] [PubMed] [Google Scholar]
- 60.McIntyre RS, Chen VC-H, Lee Y, Lui LM, Majeed A, Subramaniapillai M, Mansur RB, Rosenblat JD, Yang Y-H, Chen Y-L. The influence of prescriber and patient gender on the prescription of benzodiazepines: evidence for stereotypes and biases? Soc Psychiatry Psychiatr Epidemiol. 2021;56(6):1083–1089. doi: 10.1007/s00127-020-01989-4. [DOI] [PubMed] [Google Scholar]
- 61.Lasater KB, Aiken LH, Sloane DM, French R, Martin B, Reneau K, Alexander M, McHugh MD. Chronic hospital nurse understaffing meets COVID-19: an observational study. BMJ Qual Saf. 2021;30(8):639–647. doi: 10.1136/bmjqs-2020-011512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mannelli C. Whose life to save? Scarce resources allocation in the COVID-19 outbreak. J Med Ethics. 2020;46(6):364–366. doi: 10.1136/medethics-2020-106227. [DOI] [PubMed] [Google Scholar]
- 63.Santoro PE, Borrelli I, Gualano MR, Amantea C, Tumminello A, Daniele A, Rossi MF, Moscato U. Occupational hazards and gender differences: a narrative review. Ital J Gend Specif Med. 2022;8(3):154–162. [Google Scholar]
- 64.Waruru AK, Nduati R, Tylleskär T. Audio computer-assisted self-interviewing (ACASI) may avert socially desirable responses about infant feeding in the context of HIV. BMC Med Inform Decis Mak. 2005;5:24. doi: 10.1186/1472-6947-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gerbert B, Bronstone A, Pantilat S, McPhee S, Allerton M, Moe J. When asked, patients tell: disclosure of sensitive health-risk behaviors. Med Care. 1999;37(1):104–111. doi: 10.1097/00005650-199901000-00014. [DOI] [PubMed] [Google Scholar]
- 66.Kumar PC, Cleland CM, Gourevitch MN, Rotrosen J, Strauss S, Russell L, McNeely J. Accuracy of the audio computer assisted self interview version of the alcohol, smoking and substance involvement screening test (ACASI ASSIST) for identifying unhealthy substance use and substance use disorders in primary care patients. Drug Alcohol Depend. 2016;165:38–44. doi: 10.1016/j.drugalcdep.2016.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Spear SE, Shedlin M, Gilberti B, Fiellin M, McNeely J. Feasibility and acceptability of an audio computer-assisted self-interview version of the alcohol, smoking and substance involvement screening test (ASSIST) in primary care patients. Subst Abus. 2016;37(2):299–305. doi: 10.1080/08897077.2015.1062460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.McNeely J, Strauss SM, Rotrosen J, Ramautar A, Gourevitch MN. Validation of an audio computer-assisted self-interview (ACASI) version of the alcohol, smoking and substance involvement screening test (ASSIST) in primary care patients. Addiction. 2016;111(2):233–244. doi: 10.1111/add.13165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Perlis TE, Des Jarlais DC, Friedman SR, Arasteh K, Turner CF. Audio-computerized self-interviewing versus face-to-face interviewing for research data collection at drug abuse treatment programs. Addiction. 2004;99(7):885–896. doi: 10.1111/j.1360-0443.2004.00740.x. [DOI] [PubMed] [Google Scholar]
- 70.Topolovec-Vranic J, Natarajan K. The use of social media in recruitment for medical research studies: a scoping review. J Med Internet Res. 2016;18(11):e286. doi: 10.2196/jmir.5698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ellington M, Connelly J, Clayton P, Lorenzo CY, Collazo-Velazquez C, Trak-Fellermeier MA, Palacios C. Use of Facebook, Instagram, and Twitter for recruiting healthy participants in nutrition-, physical activity-, or obesity-related studies: a systematic review. Am J Clin Nutr. 2022;115(2):514–533. doi: 10.1093/ajcn/nqab352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Festinger DS, Dugosh KL. Paying substance abusers in research studies: where does the money go? Am J Drug Alcohol Abuse. 2012;38:43–48. doi: 10.3109/00952990.2011.563337. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, RAH.


