To The Editor,
Malaria is a tropical disease carried by Anopheles mosquitos, whose bites inject the gametes of a protozoan parasite of the genus Plasmodium [1]. There are five different malaria-inducing Plasmodium species. Among them, Plasmodium falciparum is the most fatal and responsible for the most deaths worldwide [2]. Plasmodium falciparum infection leads to fatal complications such as acute renal failure, cerebral malaria, blackwater fever, and acute respiratory distress syndrome [3]. The primary methods for diagnosing P. falciparum are thick and thin smears of peripheral blood examined under a microscope and detection of malarial antigens by rapid immunochromatographic assay. However, the most precise and sensitive method is molecular analysis using polymerase chain reaction techniques [4]. Environmental factors and socioeconomic conditions play direct roles in malaria epidemiology through the support of vector development, resulting in the enhancement of parasite-host relationships, which are especially prominent in developing countries like Pakistan [5]. The hemozoin pigment is formed by the parasite through the breakdown of hemoglobin, which can easily be detected under a microscope. Its presence in more than 5% of neutrophils correlates with severe malaria [6].
A 55-year-old man with no known comorbidities presented to the emergency room with a history of high-grade fever accompanied by chills, rigor, generalized weakness, and shortness of breath for 2 weeks. He had no travel history in the recent past. He had a temperature of 39 °C, blood pressure of 60/40 mmHg, respiratory rate of 26 breaths per minute, and heart rate of 120 beats per minute. On physical examination, he was found to be pale and icteric, with normal vesicular breathing, and no signs of organomegaly were found. Initial laboratory findings revealed hemoglobin of 8 g/dL, erythrocyte count of 3.2x1012/L, mean corpuscular volume of 93 fL, mean corpuscular hemoglobin of 27 pg, white blood cell count of 4.6x109/L, 73% neutrophils, 20% lymphocytes, 0.5% monocytes, 0.2% eosinophils, 0.0% basophils, platelet count of 16x109/L, indirect bilirubin level of 4 mg/dL, prothrombin time of 12 s, international normalized ratio of 0.9, activated partial thromboplastin time of 52.7 s, and creatine of 1.9 mg/dL. Peripheral blood film evaluation showed heavy parasitemia with 60% of red blood cells having single or double ring-shaped trophozoites of Plasmodium falciparum (Figure 1, arrows A and B) and 10% of neutrophils showing intracytoplasmic malarial pigmentation or hemozoin (Figure 1, arrow C). A diagnosis of severe falciparum malaria was made, and supportive care and intravenous quinidine were started. Unfortunately, the patient died within hours due to circulatory collapse.
Figure 1.
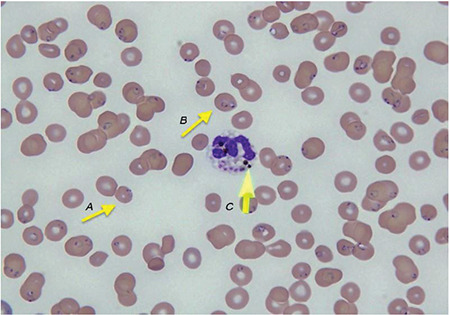
Peripheral smear at 100x, Leishman stain. Arrows A and B: trophozoites of Plasmodium falciparum; arrow C: hemozoin pigment.
Among all possible malarial species, Plasmodium falciparum causes the most lethal complications due to high levels of parasitemia, and more than 5% of neutrophils containing hemozoin pigment correlates with the severity of the disease as it infects red blood cells of all ages [6]. According to the World Health Organization, manifestations of severe malaria include impaired consciousness, prostration, multiple convulsions, acidosis, hypoglycemia, severe anemia, renal impairment, jaundice, pulmonary edema, significant bleeding, shock, and hyperparasitemia. Our patient presented with 10% of neutrophils containing hemozoin pigment, hyperparasitemia, severe anemia, and jaundice, which were all indicative of severe malaria [7]. As most of the deaths caused by malaria are due to Plasmodium falciparum, prompt action must be taken for early diagnosis and treatment with parenteral therapy in cases of severe malaria due to the risk of mortality [8].
In conclusion, severe malaria caused by Plasmodium falciparum can cause life-threatening symptoms if it is not managed early. Thus, early access to medical care, prompt diagnosis, and appropriate management of severe malaria are of utmost importance in reducing the mortality rates of these patients.
Footnotes
Ethics
Informed Consent: Obtained.
Authorship Contributions
Surgical and Medical Practices: H.Q., M.M.B., M.D.O., M.A., A.A.; Concept: H.Q.; Analysis or Interpretation: M.D.O.; Literature Search: M.A., A.A.; Writing: M.M.B.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
- 1.Milner DA Jr. Malarial pathogenesis. Cold Spring Harb Perspect Med. 2018;8:a025569. doi: 10.1101/cshperspect.a025569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maier AG, Matuschewski K, Zhang M, Rug M. Plasmodium falciparum. Trends Parasitol. 2019;35:481–482. doi: 10.1016/j.pt.2018.11.010. [DOI] [PubMed] [Google Scholar]
- 3.Balaji SN, Deshmukh R, Trivedi VJ. Severe malaria: biology, clinical manifestation, pathogenesis and consequences. Vector Borne Dis. 2020;57:1–13. doi: 10.4103/0972-9062.308793. [DOI] [PubMed] [Google Scholar]
- 4.Rehman A, Abbas N, Saba T, Mehmood Z, Mahmood T, Ahmed KT. Microscopic malaria parasitemia diagnosis and grading on benchmark data sets. Res Tech. 2018;81:1042–1058. doi: 10.1002/jemt.23071. [DOI] [PubMed] [Google Scholar]
- 5.Umer MF, Zofeen S, Majeed A, Hu W, Qi X, Zhuang G. Spatiotemporal clustering analysis of malaria infection in Pakistan. Int J Environ Res Public Health. 2018;15:1202. doi: 10.3390/ijerph15061202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pittai L, Howard CC, Zheng Y, Bernabeu M. Binding of Plasmodium falciparum-infected red blood cells to engineered 3D microvessels. Methods Mol Biol. 2022;2470:557–585. doi: 10.1007/978-1-0716-2189-9_43. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Guidelines for Malaria. Geneva, WHO, 2022. Available online at. [Internet] https://apps.who.int/iris/handle/10665/351995.
- 8.Kenangalem E, Poespoprodjo JR, Douglas NM, Burdam FH, Gdeumana K, Chalfein F, Thio F, Devine A, Marfurt J, Waramori G, Yeung S, Noviyanti R, Penttinen P, Bangs MJ, Sugiarto P, Simpson JA, Soenarto Y, Anstey NM, Price RN. Malaria morbidity and mortality following introduction of a universal policy of artemisinin-based treatment for malaria in Papua, Indonesia: a longitudinal surveillance study. PLoS Med. 2019;16:e1002815. doi: 10.1371/journal.pmed.1002815. [DOI] [PMC free article] [PubMed] [Google Scholar]


