Abstract
Background and objectives
In this systematic review, we carried out an assessment of perioperative costs of local or regional anesthesia versus general anesthesia in the ambulatory setting.
Methods
A systematic literature search was conducted to find relevant data on costs and cost-effectiveness analyses of anesthesia regimens in outpatients, regardless of the medical procedure they underwent. The hypothesis was that local or regional anesthesia has a lower economic impact on hospital costs in the outpatient setting. The primary outcome was the average total cost of anesthesia calculated on perioperative costs (drugs, staff, resources used).
Results
One-thousand-six-hundred-ninety-eight records were retrieved, and 28 articles including 27,581 patients were selected after reviewing the articles. Data on the average total costs of anesthesia and other secondary outcomes (anesthesia time, recovery time, time to home readiness, hospital stay time, complications) were retrieved. Taken together, these findings indicated that local or regional anesthesia is associated with lower average total hospital costs than general anesthesia when performed in the ambulatory setting. Reductions in operating room time and postanesthesia recovery time and a lower hospital stay time may account for this result.
Conclusions
Despite the limitations of this systematic review, mainly the heterogeneity of the studies and the lack of cost-effectiveness analysis, the economic impact of the anesthesia regimes on healthcare costs appears to be relevant and should be further evaluated.
Keywords: Anesthesia, Outpatients, Costs and Cost Analysis, Economics
Introduction
In recent decades, industrialized countries have witnessed a significant increase in medical care costs.1 In the current times of resource constraints, the financial sustainability of healthcare systems has become of paramount importance. This increased the relevance of economic criteria in decision-making processes, thus fostering the diffusion of economic evaluations in healthcare.
With regard to surgery, the majority of overall costs are represented by fixed costs and are highly dependent on hospitalization and the length of stay.2 Incentives toward a leaner and cheaper perioperative process have led to a continuous increase in ambulatory surgery over recent years.3 However, the assumption that ambulatory surgery is always cheaper than inpatient surgery is not always true: the outpatient perioperative process should be well conceived and optimized to minimize its own fixed costs, as inefficiencies are multiplied by a high turnover.4
The main factors affecting ambulatory surgery process fixed costs are the operating room time, the occupancy of the postoperative care unit and the time to discharge. Indeed, the cost-effectiveness of the outpatient perioperative process depends on its ability to optimize these most labor-intensive and resource-consuming phases.5
Regional anesthesia has been increasingly employed in the outpatient setting, given its unique characteristics of selectivity and efficacy in the control of acute postoperative pain. Outpatient regional anesthesia economic externalities have been investigated by some studies, which have associated its systematic adoption with a decrease in anesthesia-controlled operating room time and thus in the operating room fixed costs, potentially translating into a significant increase in patient turnover and ultimately hospital revenues.5, 6 Moreover, regional anesthesia is associated with a very high postoperative care unit bypass rate and with a lower incidence of postoperative anesthesia-related side effects, such as nausea and vomiting, excessive sedation and dizziness, which, in the ambulatory setting, may significantly prolong the day-hospital length of stay, jeopardize the meeting of discharge criteria or even cause unscheduled hospital readmissions.5, 6
On the other hand, the recent evolution of general anesthesia techniques has led some to challenge a supposed superiority of regional anesthesia techniques in the outpatient setting with regard to their safety and side-effect profile. The extensive use of laryngeal masks and anesthetic drugs with a more favorable pharmacokinetic profile has actually led to a reduction in the incidence of postoperative complications, an increase in the postanesthesia care unit (PACU) bypass rate and a potential reduction in the average anesthesia-controlled operating room time.7 If, following these recent developments, a difference in cost-effectiveness between the two anesthesia regimens still persists, it is not clear.
Despite the importance of the topic for the future development of our profession, in a context where ambulatory surgery is continuously growing and has been estimated to account for the vast majority of all surgical procedures in the near future,1 a systematic review of all the contrasting evidence on this theme is still lacking.
The aim of this work is to provide a systematic review of the recent literature to test the hypothesis that the use of local or regional anesthesia is associated with significantly lower average total hospital costs than general anesthesia when applied in the ambulatory setting.
Methods
Search strategy
A literature search of the electronic PubMed/MEDLINE, Cochrane Central Register of Controlled Trials (CENTRAL), Web of Science, and Google Scholar databases was carried out to find relevant data on the costs or cost-effectiveness of general and local or regional anesthesia performed in an ambulatory setting. The primary outcome was the average total cost of anesthesia. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were applied in carrying out this systematic review.8
The search algorithm was based on the clinicoeconomic question coded into the PICO framework and constructed combining a set of terms referring to outpatient setting (Patient), regional anesthesia (Intervention), general anesthesia (Comparator), cost or cost-effectiveness analysis (Outcome). To formulate the best query for the literature search, many attempts were made to be sure to include all terms relevant for our clinico-economic question. The final search query was ((outpatient*) OR (out-patient*) OR (ambulatory) OR (day-surgery) OR (day surgery) OR (day-case) OR (day case)) AND ((anaesthesia) OR (anesthesia) OR (anaesthetic*) OR (anesthetic*)) AND (general) AND ((block*) OR (local) OR (regional) OR (loco-regional) OR (locoregional) OR (nerve) OR (spinal) OR (epidural)) AND ((cost-effective) OR (cost*) OR (cost-efficacy) OR (cost-effectiveness) OR (cost-utility) OR (economic*)).
The last literature search was performed on 10th May 2021 in all databases. No specific study design was defined. Search was without language restriction. Reference lists of the retrieved articles were also screened for additional data.
Eligibility criteria
Studies were included in the systematic review when they met each of the following inclusion criteria: a) original article published in peer-reviewed journal; b) the study includes adults only; c) the study compares regional and general anesthesia in outpatient setting; d) the study reports data on cost or cost-effectiveness analysis. Anesthesia was considered general anesthesia whenever loss of consciousness was achieved, and arousal was not achievable at verbal command. With regional anesthesia was meant any technique aimed at achieving a reversible loss of sensation of a limb or a body area through the administration of a local anesthetic in close proximity of a peripheral nerve, a plexus or the spinal nerve roots or the spinal cord. Local anesthesia was considered a reversible loss of sensation of a body wall area achieved through the infiltration of a local anesthetic directly into tissues. An outpatient setting was defined as a surgery or medical treatment for which the patient was discharged the same day (less than 24 hours) regardless of whether it required or not to occupy a hospital bed. The average total cost of anesthesia per case encompassed the perioperative costs of drugs, staff labor and resources used. Readmissions and complications were excluded from the cost calculation.
The exclusion criteria were a) articles not within the field of interest of this review (for example, medical procedures not in ambulatory setting); b) review articles, letters, or editorials; c) case reports or case series (less than 10 patients included); and d) articles published prior to 2000 to restrict the search to the recent literature to retrieve updated costs.
Study selection
Titles and abstracts of the retrieved records were independently reviewed by three researchers (MP, GT, FM) applying the inclusion and exclusion criteria mentioned above. Full texts of the selected articles were retrieved and read to determine their eligibility for inclusion. Any disagreement between authors was resolved by discussion.
Quality assessment
The quality of the studies included in the systematic review was critically assessed using the Consensus on Health Economic Criteria (CHEC) list.9 The assessment tool had 19 indicators, and each indicator was assessed for every study using yes or no depending on whether the required information was reported. The quality assessment was performed by two independent authors; any disagreement between the authors was resolved in a consensus meeting.
Data extraction and analysis
For each included study, two authors (MP, FM) extracted information concerning basic data (authors, year of publication, country of origin, type of study, medical procedure, number of patients, mean age, gender), methods (type of anesthesia, anesthetic drug), and outcomes (average total costs and main findings regarding the cost analysis). Another author checked all extracted data independently (GT). During data extraction from the selected studies, the following secondary outcomes were judged interesting for the topic and were also included: anesthesia time, recovery time, time to home readiness, hospital stay time, and complications.
All currencies of the included studies were converted to United States dollars (USD) according to CCEMG – EPPI-Centre Cost Converter v.1.6 (last update: 29th March 2021, http://eppi.ioe.ac.uk/costconversion/default.aspx).
Results
Literature search
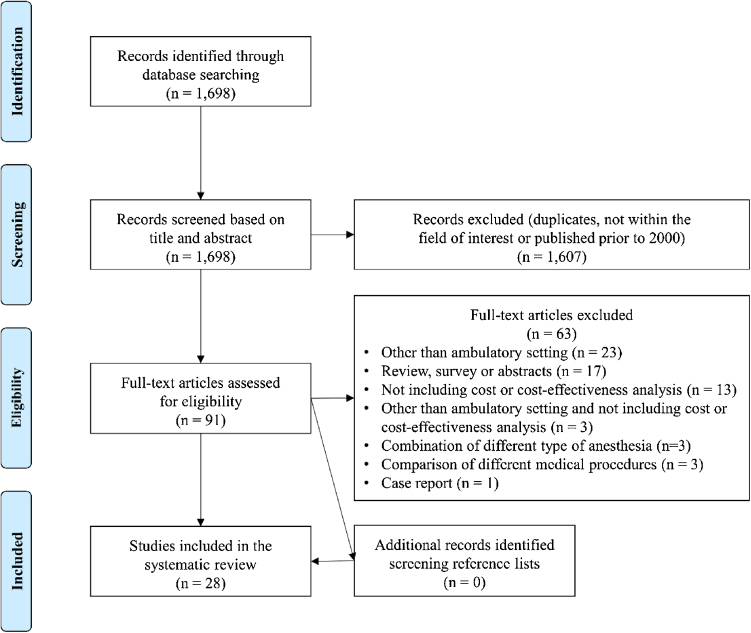
The literature search from the PubMed/MEDLINE, Cochrane CENTRAL, Web of Science, and Google Scholar databases yielded a total of 1,698 records. After reviewing titles and abstracts and excluding those published prior to 2000 and not related to the clinicoeconomic question, 91 articles were selected. The full text was retrieved for all. Following the eligibility assessment, 63 articles did not meet the inclusion criteria and were excluded from the systematic review. Of these, 23 were excluded because not in the outpatient setting, 17 were reviews, surveys, or abstracts, 16 did not include data on costs, 6 reported sparse data on different anesthesia types and medica procedures and 1 article was a case report. Manual searches of the reference lists of the selected articles did not yield any additional records. Finally, 28 studies including 27,581 patients were identified as potentially relevant and were selected for the systematic review.10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 All of the included studies were published in English. These studies covered the period from January 2000 to May 2021. Search results and article selection are displayed in a PRISMA flow chart (Fig. 1).
Figure 1.
PRISMA flow chart of the retrieved, excluded and analyzed studies.
Selected studies
The characteristics of the selected studies are reported in Table 1. They were conducted in various countries across the world (Europe, North America, Oceania, Africa). The sample size of the included studies ranged from 20 to 14,713 adults who underwent various medical procedures under general and local or regional anesthesia in an outpatient setting. General anesthesia was compared to local anesthesia in 15 studies,10, 13, 14, 16, 17, 18, 19, 20, 21, 22, 23, 24, 27, 30, 33 to spinal anesthesia in 7 studies,12, 15, 25, 31,32, 34, 35 and to both in 5 studies.26, 28, 29, 36,37 Medical procedures were different and included laryngoplasty, knee arthroscopy, biopsy, hernia repair, hysteroscopy, and others. Studies were included irrespective of the induction method of anesthesia (inhalation, infusion, topical). Regional anesthetic techniques encompassed axillary brachial plexus block,33 ilioinguinal-hypogratric37 or paracervical18 or peripheral24 or sciatic-femoral23, 28, 30 nerve block, and epidural26 or spinal15, 25, 28, 29,31, 32, 34, 35, 36, 37 or intravenous regional33 anesthesia. Thirteen studies were randomized controlled trials,12, 22, 23, 25,26, 28, 29, 30, 31, 32, 34, 36, 37 2 of which were double-blinded,23, 25 and 15 were observational with a prospective16, 27, 33 or a retrospective10, 11, 13, 14, 15, 17, 18, 19, 20, 21, 24, 35 design. The overall quality of the included studies was assessed with the CHEC list (Appendix A). None of the studies satisfied at least 80% of the CHEC list criteria, and 11 studies met less than 50% of the criteria. Thus, overall, the methodological quality was judged to be moderate.
Table 1.
Included studies comparing costs of general and local or regional anesthesia regimen for different outpatient medical procedures in an outpatient setting.
| Authors | Year | Country | Study design | Medical procedure | Number of patients evaluated | Mean age (years) | % Male |
|---|---|---|---|---|---|---|---|
| Li et al.10 | 2020 | USA | Retrospective, observational | Anterior shoulder stabilization surgery | 7,103 | NR | 69.4 |
| Bokshan et al.11 | 2019 | USA | Retrospective analysis | Anterior Cruciate Ligament Reconstruction | 14,713 | <20 years: 30.4% | 59.3 |
| 20−29 years: 27.6% | |||||||
| 30−39 years: 19.1% | |||||||
| >40 years: 22.9% | |||||||
| Gebhardt et al.[12] | 2018 | Germany | Prospective, RCT | Knee arthroscopy | 50 | 48.5 | 64 |
| Hamilton et al.13 | 2018 | Canada | Retrospective cohort study | Shoulder surgery | 1,623 | 50.5 | 66.7 |
| Chandran et al.14,a | 2018 | Australia | Retrospective, observational | Injection laryngoplasty | 20 | 63.08 | 70 |
| Camponovo et al.15 | 2014 | Switzerland | Retrospective, observational | Knee arthroscopy | 56 | 50 | 55.3 |
| Penketh et al.16,b | 2014 | Canada | Prospective,c comparative, observational | Hysteroscopy | 118d | 56.7d | – |
| Sivalingam et al.17 | 2013 | USA | Retrospective, observational | Ureteral stent placement for obstructing stones | 119 | 53.11 | 44.54 |
| Ahonkallio et al.18,e | 2012 | Finland | Retrospective, observational | Endometrial thermal ablation with Novasure | 36 | NR | – |
| Covarelli et al.19,a | 2012 | Italy | Retrospective, observational | Sentinel lymphnodes biopsy | 153 | 50 | 52 |
| Stoffels, et al.20 | 2011 | Germany | Retrospective, observational | Sentinel lymphnodes excision | 300 | 57.7 | 60.7 |
| Mitchell et al.21,a | 2011 | UK | Retrospective, observational | Sacral nerve stimulation | 111 | 56.68 | 3.33 |
| Kushawaha et al.22 | 2008 | United Kingdom | Prospective, RCT | Open hemorrhoidectomy | 41 | 52.68 | 60.97 |
| Mostafa et al.23 | 2008 | Egypt | Prospective, | Knee arthroscopy | 60 | 48.33 | 41.67 |
| Double, blind, RCT | |||||||
| Horn et al.24,a | 2007 | USA | Retrospective, observational | Upper extremity surgical procedures | 213 | 41.59 | 55.39 |
| Nishikawa et al.25 | 2007 | Japan | Prospective, | Prostate biopsy | 80 | 72 | – |
| Double, blind, RCT | |||||||
| Nordin et al.26,a | 2007 | Sweden | Prospective, multicenter | Inguinal hernia repair | 616 | 56 | 98 |
| RCT | |||||||
| Spanknebel et al.27 | 2006 | USA | Prospective, observational | Thyroidectomy | 1,194 | 49.57 | 41.09 |
| Casati et al.28 | 2004 | Italy | Prospective, | Knee arthroscopy | 120 | 43.5 | 54.2 |
| RCT | |||||||
| Forssblad et al.29 | 2004 | Sweden | Prospective, | Knee arthroscopy | 343 | NR | NR |
| RCT | |||||||
| Casati et al.30 | 2002 | Italy | Prospective, | Knee arthroscopy | 40 | 48.5 | 60 |
| RCT | |||||||
| Danelli et al.31 | 2002 | Italy | Prospective, | Hysteroscopic ablation of endometrial neoplasm | 40 | 52.50 | – |
| RCT | |||||||
| Lennox et al.32 | 2002 | Canada | Prospective, | Gynecologycal laparoscopy | 20 | 34.5 | – |
| RCT | |||||||
| Chan et al.33 | 2001 | Canada | Prospective, observational | Hand surgery | 126 | 39.67 | 62.7 |
| Martikainen et al.34 | 2001 | Finland | Prospective, | Knee arthroscopy | 60 | 40.3 | 55 |
| RCT | |||||||
| Chilvers et al.35 | 2000 | Canada | Retrospective, comparative | Gynecologycal laparoscopic sterilisation | 52 | 34.46 | – |
| Li et al.36 | 2000 | USA | Prospective, | Anorectal surgery | 93 | 41.33 | 72.04 |
| RCT | |||||||
| Song et al.37 | 2000 | USA | Prospective, | Unilateral inguinal herniorrhaphy | 81 | 39 | 86.42 |
| RCT |
NR, not reported; RCT, randomized controlled trial.
Day-case setting.
Day-case setting in the operating room for general and local anesthesia, outpatient setting for local anesthesia.
Cost analysis is retrospective.
Refers only to group of patients underwent local anesthesia in outpatient setting.
Day-case setting for general anesthesia and outpatient setting for paracervical block.
Cost analysis
The main findings of the cost analysis are summarized in Table 2. The average total cost of anesthesia per case encompassed the perioperative costs of drugs, staff labor and resources used, except four studies that also included the cost of room management.19, 22 Readmissions and complications were excluded from the cost calculation. Ten studies10, 11, 14, 16, 17, 18, 21, 24, 26,27 not reporting the average total costs of anesthesia were also included, as they compared the average total costs of the entire medical procedure on the basis of the costs of the anesthetic regimen used. None of the selected studies reported data on cost-effectiveness analysis. Regardless of the medical procedure, the total costs were significantly higher for general anesthesia than local14, 16, 17, 19, 20, 21, 22, 27 or regional11, 12, 15, 18,24, 25, 28, 32, 33, 34, 37 anesthetic techniques in almost all included studies, other than five studies that reported no statistically significant difference between loco-regional and general anesthesia.13, 23, 30, 31,35 Only one study reported higher costs in patients who received the loco-regional anesthesia.10 Furthermore, three studies comparing all three types of anesthesia26, 29, 36 confirmed the lowest costs for medical procedures under local anesthesia and similar costs between general and spinal or epidural anesthesia,26, 29 except one showing higher costs under general anesthesia.36 Major cost savings for medical procedures under local anesthesia were reported for ureteral stent placement (74%),17 hysteroscopic resection (67% if performed in the office and 50% in the operating room),16 and anorectal surgery under local anesthesia with sedation (52%)36; this last study also included a group undergoing anorectal surgery under spinal anesthesia, for which cost savings of only 18% were reported with respect to general anesthesia. Thus, anorectal surgery under local anesthesia was associated with the lowest costs, mainly due to the ability of patients to bypass phase 1 recovery units.36 Cost savings of nearly 40% were reported for injection laryngoplasty under local anesthesia,14 knee arthroscopy under spinal anesthesia12, 15 and endometrial thermal ablation under paracervical nerve block18 compared to general anesthesia. Significant cost savings in respect to general anesthesia were also reported in anterior cruciate ligament reconstruction11 under loco-regional anesthesia and in sentinel lymphnodes biopsy/excision under local anesthesia.19, 20 Reduced staff costs16, 33, 36 and drugs or supplies,18, 20, 25, 26,32, 33, 37 ability to bypass the postoperative PACU or phase 1 recovery unit,15, 24, 36 and shorter recovery time12, 22, 26, 28,29, 37 are the main anesthetic procedure factors associated with health care cost reductions.
Table 2.
Main findings of the selected studies about cost analysis and secondary outcomes.
| General anesthesia |
Local/Regional anesthesia |
Outcomes |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Authors | Anesthetic | No. of patients | Average total costs (USD) | Type | Anesthetic | No. of patients | Average total costs (USD) | Main findings about cost analysis (primary outcome)) | Other study findings (secondary outcomes) | Resources included for the calculation of costs |
| Li et al.10 | NR | 3,903 | 15,670 | Loco-regional anesthesia | NR | 1,576 | 19,929 | Average total costs were significantly higher in patients undergoing regional anesthesia. | Several other contributors to higher costs are described. | Medical procedure costs |
| Bokshan et al.11 | NR | 3,737 | 19,249 | Loco-regional anesthesia | NR | 10,976 | 17,469 | Average total costs were significantly lower in patients undergoing regional anesthesia. | General anesthesia, Hispanic ethnicity, Chronic medical condition, male gender, operative time and age are predictors of increased costs. | Medical procedure costs |
| Gebhardt et al.12 | Sulfentanil and Propofol | 25 | 71.92 | SA | Chloroprocaine 1% | 25 | 41.02 | Anesthesia costs are inferior in case of regional anesthesia. | Spinal had faster recovery with patients reaching discharge earlier (117 vs. 142 min)*. Pain occurred earlier in the general anesthesia group. Patients felt significantly more uncomfortable after general anesthesia. | Anesthesia costs |
| Hamilton et al.13 | Volatile anesthetics or intravenous with propofol | 241 | 60 | Interscalene brachial plexus single shot block, or catheter | 20–40 mL of 0.5% ropivacaine with 1:400,000 epinephrine | 1,382 | 82 | No statistically significant difference between groups. | Increased risk of an emergency department visit within 30 days for patients who received a regional anesthesia. | Costs incurred after surgery |
| Chandran et al.14,a | NR | 6 | 2071 | LA | NR | 14 | 1251 | Average total costs of injection laryngoplasty under LA are significantly lower than under GA with cost savings of 40%. Major contributors are direct and indirect operating theater costs. | Length of stay (h): 8.8 GA vs 6.4 LA* | Medical procedure costs |
| Camponovo et al.15 | Intravenous propofol and fentanyl | 28 | 104 | SA | Chloroprocaine 1% | 28 | 63 | SA for knee arthroscopy is associated with cost reductions per patient compared with GA. Cost reductions in the SA group are due to: the ability to systematically bypass the PACU, faster discharge time, the lower incidence of pain and postoperative nausea and vomiting. | Anesthesia time: 64 vs. 62 min. | Anesthesia supplies, drugs, staff |
| Discharge time: 326 (GA) vs 203 min (SA)* | ||||||||||
| Penketh et al.16 | NR | NR | 1,485 | LA in operatory room | NR | NR | LA in operatory room: 716 | Operative hysteroscopic resection under LA is less expensive than under GA, especially if performed in the office compared to the OR. Reduced staff costs are the primary reason for saving. | NR | Medical procedure costs |
| LA in office | LA in office: 482 | |||||||||
| Sivalingam et al.17 | NR | 73 | 30,060 | LA | Lidocaine 1%b | 46 | 7,770 | Average total cost is nearly 4 times greater for the GA group compared to LA. Ureteral stent placement can be safely and effectively performed under LA in the office. | No difference in complications between GA and LA. | Medical procedure costs |
| Ahonkallio et al.18,c | NR | 20 | 2,333 | Peripheral block | 20 mL ropivacaine 2 mg mL−1,d | 16 | 1,333 | Endometrial thermal ablation under PB is cheaper than GA and results in significantly reduced health service costs. The difference is due to lower costs of the hospital ward and anesthesia, and partly to overhead costs. | NR | Medical procedure costs |
| Covarelli et al.19,a | NR | 41 | 373 | LA | 10−25 mL 1% mepivacaine and 0.5% L-bupicavaine in equal parts | 112 | 258 | Average total costs for groin and axillary sentinel lymph node biopsy under GA are significantly higher than those under LA. | No differences in the number of complications. | Operating room management, personnel, drugs, instruments |
| Stoffels et al.20 | NR | 89 | 500 | LA | 450 mL physiological solution, 50 mL Lidocain 1%, 0.5 mg Epinephrin | 211 | 47 | The costs were significantly less in a procedures room performed under local anesthesia compared to general anesthesia in an operating room. | No differences in the number of postoperative complications nor in oncological outcomes. | Anesthesia costs |
| Mitchell et al.21,a | NR | 64 | 1,244 | LA | NR | 47 | 1,026 | Sacral nerve stimulation under LA is associated with reduced costs compared to GA. | LA is associated with shorter hospital staye and quicker recovery. | Medical procedure costs |
| Similar symptom score and success rate for both anesthesia. | ||||||||||
| Kushwaha et al.22 | Propofol 1.5−2 mg kg−1 and fentanyl 10 μg kg−1 with sevofluranef | 22 | 714 | LA | 20 mL 1% lidocaine with 1:10,000 epinephrine | 19 | 503 | Excluding the cost of post-operative follow-up, LA was 1.5 times cheaper than GA. This difference is due to the saving in GA and recovery room costs. | LA is associated with similar tolerance and clinical outcome compared to GA. | Suture materials, drugs, day surgery bed, staff costs, recovery room, post-operative medication. |
| Mostafa et al.23 | Intravenous remifentanil 0.5 μg kg−1 min−1 or alfentanil 2 μg kg−1 min−1 and propofol 9 mg kg−1 h−1 | 40 | 492 for remifentanil | Sciatic-femoral nerve block | 25 mL ropivacaine | 20 | 393 | Costs of disposals, pre-operative and post-operative times are higher for the sciatic-femoral block group, however average total costs (including also drugs) are insignificant between GA and sciatic-femoral nerve block. | Length of stay in PACU: 28 min for remifentanil GA vs 25 min for alfentanil GA vs 28 for sciatic-femoral nerve block | Disposal, drugs, staff |
| 541 for alfentanil | ||||||||||
| Horn et al.24,a | Propofol with sevoflurane or desflurane, fentanyl or sufentanyl | 121 | 4,780 | Peripheral nerve block | Mepivacaine 1.5% with 10% sodium bicarbonate | 92 | 3,656 | Perioperative costs in the peripheral nerve block group are significantly lower than in the GA group. | PACU time: 49 min (GA) vs 15 min (PNB)* | Medical procedure costs |
| The use of peripheral nerve block in upper extremity surgery is feasible and associated to significant cost savings. | Postoperative complications: 11.7% (GA) vs 3.3% (PNB)* | |||||||||
| Nishikawa et al.25 | Intravenous fentanyl 1 μg kg−1 and propofol 6 mg kg−1 h−1 | 40 | 74 | SA | Lidocaine 1% 1 m L | 40 | 49 | Average total costs are significantly lower in the SA group. Costs of drugs and supplies used in the operatory room are reduced for the SA, whereas the labor costs are higher in both operatory room and recovery unit. | Time to home-readiness: 30 min (GA) vs 38 min (SA)* | Drugs, equipment, staff |
| No pain in the recovery unit for 75% patients in GA vs 80% patients SA groups. * | ||||||||||
| SA may be a suitable cost-effective alternative to GA for elderly ambulatory prostate biopsy. | No adverse events at home. | |||||||||
| Nordin et al.26,a | NR | 199 | 2,964 | SA/epidural anesthesia | SA/epidural anesthesia: NR | SA/epidural anesthesia: 164/35 = 199 | SA/epidural anesthesia: 3,010 | Average total costs of LA are significantly lower than the other two groups. Intra-operative (anesthetic equipment, duration of surgery and anesthesia) and post-operative (time in recovery room, unplanned overnight admission) costs are reduced for LA compared to SA/epidural anesthesia and GA. No difference between SA/epidural anesthesia and GA. | NR | Medical procedure costs |
| LA | LA: 50:50 mixture of 1% mepivacaine and 0.5% bupicavaine | LA: 205 | LA: 2,508 | |||||||
| Spanknebel et al.27 | NR | 85 | 3,153 | LA | Lidocaine and bupicavaine | 217 | 2,760 | Average total costs are significantly higher for GA than LA. Extensive procedures and increased operating room times impact significantly on costs. | Thyroidectomy under LA results in similar outcome and morbidity rate to GA with reduced costs. | Medical procedure costs |
| Casati et al.28 | Intravenous remifentanil 0.1−0.3 μg kg−1 min−1 and propofol 2−4 μg mL−1 | 40 | 317 | sciatic-femoral nerve block SA | sciatic-femoral nerve block: 25 mL 2% mepivacaine | sciatic-femoral nerve block: 40 | sciatic-femoral nerve block: 220 | The use of sciatic-femoral nerve block results in the lowest total costs. Costs of drugs and disposable material required for anesthesia are lower in the SA group than the others. | Regional anesthesia techniques reduce the rate of admission and the duration of stay in the PACU as compared with GA. | Drugs, devices, staff |
| SA: 8 mg 0.5% bupicavaine | SA: 40 | SA: 308 | The time readiness for home discharge are shorter in the GA group than regional anesthesia. | |||||||
| Forssblad et al.29 | Propofol and alfentanil | 88 | 236 | LA | LA: 30 mL 0.5% prilocaine with 4 μg mL−1 adrenaline | LA: 181 | LA: 76 | The knee arthroscopy in LA is associated with lower cost than knee arthroscopy in SA and GA, because of the shorter recovery time of LA that reduces the need for recovery beds and postoperative care. | Recovery time: 139.1 min (GA) vs 33.6 min (LA) vs 230.1 min (SA). | Drugs, devices, staff |
| SA | SA: 60−90 mg 5% lidocaine with 5−10 mg ephedrine | SA: 74 | SA: 219 | Time in hospital: 280.4 min (GA) vs 130.4 min (LA) vs 350.3 min (SA) | ||||||
| Casati et al.30 | Intravenous remifentanil 0.1−0.3 μg kg−1 min−1 and propofol 2−4 μg mL−1 | 20 | 291 | Sciatic-femoral nerve block | 25 mL 2% mepivacaine | 20 | 288 | Average total costs between GA group and sciatic-femoral block group in patients undergoing knee arthroscopy are not statistically significant. Costs related to the time spent in the PACU are statistically significant lower for the sciatic-femoral block group (USD 2.0) compared with the GA group (USD 55.7). | Time in the hospital: 170 min (GA) vs 277 min (Sciatic-femoral block)* | Disposable materials, drugs, staff |
| Length of stay in PACU: 23 min (GA) vs 5 min* | ||||||||||
| VAS pain: 7 (GA) vs 0* | ||||||||||
| Danelli et al.31 | Intravenous remifentanil 0.25 μg kg−1 min−1 and propofol 4 μg mL−1 | 20 | 260 | SA | 10 mg 0.5% bupivacaine | 20 | 282 | No differences in average total costs between the two groups. | Hospital discharge time: 156 min (GA) vs 296 min (SA)* | Disposable materials, drugs, staff |
| Pain control is similar. | ||||||||||
| Lennox et al.32 | Fentanyl 2 μg kg−1 and propofol 2 mg kg−1, 65% nitrous oxide | 10 | 127 | SA | 3 mL 10 mg lidocaine and 10 μg sufentanil | 10 | 94 | Average total cost of anesthesia and recovery is significantly less for patients in the SA group than the GA group. Recovery costs are similar, whereas mean costs of anesthesia is significantly less in the SA group. Cost savings are due to lower cost of anesthetic supplies, sterilization, drugs. | Anesthesia time: 6.6 min (GA) vs 6.6 min (SA) | Supplies, drugs, staff |
| PACU time: 112 min (GA) vs 101 min (SA) | ||||||||||
| Postoperative pain: 50% (GA) vs 0% (SA)* | ||||||||||
| Nausea/vomiting: 0% (GA) vs 30% (SA) | ||||||||||
| Chan et al.33 | Propofol, fentanyl, with isoflurane (up to 1.5%), 60% nitrous oxide | 39 | 718 | Intravenous regional anesthesia | Intravenous regional anesthesia: 35−45 mL 0.5% lidocaine | Intravenous regional anesthesia: 45 | Intravenous regional anesthesia: 513 | The intra- and post-operative costs are the least in the intravenous regional anesthesia group than GA and axillary block, reflecting cost savings of approximately 30% in both cases. intravenous regional anesthesia is associated with short induction time, lower anesthetic drug and equipment costs in the operatory room, and with less demand on nursing time and lower drug and supply costs in the PACU. | Total hospital stay time: 240 min (GA) vs 180 min (intravenous regional anesthesia)*vs 244 min (axillary block) | Disposable materials, drugs, staff |
| Axillary block | Axillary block: 40−50 mL 3% chloroprocaine and 2% or 1.5% lidocaine with 1:200,000 epinephrine | Axillary block: 42 | Axillary block: 755 | Anesthesia time: 83 min (GA) vs 72 min (intravenous regional anesthesia)*vs 106 min (axillary block) | ||||||
| PACU recovery time: 70 min (GA) vs 45 min (intravenous regional anesthesia)*vs 63 min (axillary block) | ||||||||||
| Martikainen et al.34 | Intravenous propofol 2 mg kg−1 and alfentanil 1 mg with sevoflurane (up to 8%) | 30 | 333 | SA | 3 mL 2% lidocaine | 30 | 293 | Average total costs are significantly reduced for SA. However, GA is more cost-effective than SA in ambulatory knee surgery, if a short recovery unit time is required. | Recovery unit time: 218 min (GA) vs 224 min (SA) | Disposable materials, drugs, staff |
| Time to home-readiness: 96.4 min (GA) vs 140.8 min (SA)* | ||||||||||
| Post-operative pain low (VAS < 4 in 100% patients in SA vs in 86.7% in GA groups). | ||||||||||
| Chilvers et al.35 | Propofol, fentanyl or sufentanil, and mivacurium or succinylcholine, with isoflurane nitrous oxide | 28 | 99 | SA | 2−2.5 mL 1% lidocaine and 10−25 μg fentanyl | 24 | 107 | Average total costs for anesthesia and recovery are similar between the two groups. Use of SA in alternative to GA does not reduce costs or improve efficacy of anesthesia and recovery for outpatient laparoscopy. | Anesthesia time: 10 min (GA) vs 18 min (SA)* | Disposable materials, drugs, staff |
| PACU recovery time: 94 min (GA) vs 123 min (SA)* | ||||||||||
| Time to discharge: 124 min (GA) vs 150 min (SA) | ||||||||||
| Li et al.36 | Intravenous propofol 2.5 mg kg−1, fentanyl 1−2 μg kg−1 with 0.5−2% sevoflurane, 65% nitrous oxide | 31 | 289 | SA | SA: 30 mg lidocaine and 20 μg fentanylg | SA: 31 | SA: 208 | Average total costs are significantly decreased for LA than SA and GA because both intraoperative and recovery costs are the lowest. Patients in the LA group are able to by-pass phase 1 recovery unit requiring less nursing labor (thus less costs). GA is associated to the highest costs. | Anesthesia time: 40 min (LA) vs 72 min (SA)* vs 75 min (GA)* | Drugs, supplies, staff |
| LA with sedation | LA: 31 | LA: 138 | Phase 1 stay: 0 (LA) vs 52 min (SA)*vs 44 min (GA)* | |||||||
| LA: topical 2% lidocaine gel and sedation-analgesia with propofol 75 μg kg−1 min−1 and 0.5 μg kg−1 fentanyl. 15 mL 2% lidocaine, 15 mL 0.5% bupicavaine, 0.5% epinephrine (1:200,000) | Time to home-readiness: 76 min (LA) vs 193 min (SA)*vs 171 min (GA)* | |||||||||
| Hospital stay: 116 min (LA) vs 266 min (SA)*vs 247 min (GA)* | ||||||||||
| No differences in post-operative side effects or unanticipated hospitalizations. | ||||||||||
| Song et al.37 | Propofol 2.5 mg kg−1 min−1 1% sevoflurane, 65% nitrous oxide | 28 | 369 | SA | SA: 1.2−1.5 mL 0.75% bupicavaine and 25 μg fentanyl | SA: 25 | SA: 330 | Average total costs are the lowest for the ilioinguinal-hypogastric nerve block group (reduced supplies during the intraoperative period, reduced labor during post-operative period). No difference between GA and SA. | Anesthesia time: 109 min (ilioinguinal block) vs 119 (GA) vs 116 (SA) | Drugs, staff, resources |
| Ilioinguinal-hypogastric nerve block | Ilioinguinal-hypogastric nerve block: 30 mL of 0.25% bupivacaine, 1% lidocaine and propofol 25−150 μg kg−1 min−1 | Ilioinguinal-hypogastric nerve block: 28 | Ilioinguinal-hypogastric nerve block: 288 | Ilioinguinal-hypogastric nerve block is the most cost-effective techniques for outpatients undergoing unilateral herniorrhaphy with respect to recovery, patient comfort, and associated incremental costs. | Phase 1 PACU: 5 min (ilioinguinal block) vs 40 (GA)*vs 35 (SA)* | |||||
| Phase 2 unit: 153 min (ilioinguinal block) vs 168 (GA) vs 276 (SA)* | ||||||||||
| Time to home-readiness: 133 min (ilioinguinal block) vs 171 (GA)*vs 280 (SA)* | ||||||||||
| Time to actual discharge: 158 min (ilioinguinal block) vs 208 (GA)*vs 309 (SA)* | ||||||||||
| Maximum pain VAS: 15 (ilioinguinal block) vs 39 (GA)*vs (34) SA* | ||||||||||
| Maximum nausea VAS: 1 (ilioinguinal block) vs 27 (GA)*vs 4 (SA)* | ||||||||||
NR, not reported; PACU, post-operative anesthesia care unit. Currency is expressed with United States dollars (USD). Type of anesthesia: GA, general anesthesia; LA, local anesthesia; SA, spinal anesthesia.
Day-case setting.
Four patients received also i.v. midazolam.
Day-case setting (8 h) for general anesthesia and outpatient setting (4 h) for paracervical block.
When necessary also Alfentanil 0.5 mg.
Overnight stay for 38% of patients of the GA group due to adverse effects of the anesthesia.
This group received also a perianal block as for the LA group.
Patients received also 1−2 mg midazolam i.v. for sedation.
Statistically significant.
Among studies comparing different types of regional anesthesia, two randomized trials found spinal anesthesia to be more expensive than both sciatic-femoral nerve blocks in patients undergoing knee arthroscopy,28 even if the costs of drugs and disposables were lower, and ilioinguinal-hypogastric nerve block for unilateral inguinal herniorrhaphy37 and reduced PACU costs were the primary reasons for this difference for both surgeries. Chan et al.33 found that intravenous regional anesthesia decreased costs of 30% compared to axillary brachial plexus block due to shorter induction time and lower drug and supply requirements. Two studies which used treatment codes for patient selection did not specify the type of peripheral block performed.10, 11
Contrasting results were achieved by analyzing the costs of a subgroup of studies focusing on knee arthroscopy, which was investigated in 6 randomized clinical trials12, 23, 28, 29, 30, 34 and in one retrospective observational study.15 Cost advantages were demonstrated for regional anesthesia12, 15, 28, 34 in half of the studies, but similar costs were found in the other two trials.23, 30 The remaining study29 confirmed that there was no statistically significant difference between spinal and general anesthesia but found reduced costs only for knee arthroscopy under local anesthesia. Reduced drugs and/or disposable materials and recovery time were associated with cost savings, further supporting the overall results of this systematic review.
Secondary outcomes
Twelve trials12, 14, 15, 21,28, 29, 30, 31, 33, 35, 36, 37 reported data on the duration of hospital stay; all studies found a shorter length of stay for local14, 21, 29, 36 or regional12, 15, 30, 31,33, 37 anesthesia, except one that did not reveal any difference.35
Postanesthesia recovery time was investigated in 12 studies.12, 21, 23, 24,28, 29, 30, 32, 33, 34, 35, 37 Local or regional anesthesia techniques significantly decreased the PACU time.12, 21, 24, 28, 29, 30, 33, 35, 37 In particular, Song et al.37 showed that patients undergoing ilioinguinal-hypogastric nerve block spent less time in the phase 1 PACU (5 minutes) compared to patients operated on under general anesthesia (40 minutes) but also than patients undergoing spinal (35 minutes) anesthesia; moreover, these latter techniques required more time to recover in the phase 2 unit than the other two techniques. Thus, ilioinguinal-hypogastric nerve block was associated with lower costs than the spinal technique as regional anesthesia for unilateral herniorrhaphy. No difference in the duration of recovery stay was found in three studies.23, 32, 34 Time readiness for home discharge was significantly shorter for general anesthesia in 325, 28, 34 out 5 studies reporting this datum.25, 28, 34, 36,37
Data on anesthesia time conflicted with three studies reporting lower times for local and regional techniques33, 35, 36 and three15, 32, 37 finding no statistically significant difference.
The overall rates of complications or side effects and clinical outcomes were similar12, 13, 17, 19, 20, 21, 22, 25, 36 or more favorable15, 24, 30, 32,37 for medical procedures under local or regional anesthesia.
Discussion
The vast majority of the studies included in this systematic review were concordant in showing an association between local or regional anesthesia and lower perioperative costs, regardless of the surgical procedure.11, 12, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 32, 33, 34, 36, 37 This is consistent with data identifying in the operating room time the major fixed cost incurred during the perioperative process.2 The anesthesia-controlled operating room time was defined as the portion of this time required by the anesthesiologist to perform the anesthesia technique of choice. When this time is reduced, overall hospital costs decrease. We know that regional anesthesia is associated with a reduction in anesthesia-controlled operating room time, fastening both the induction and postoperative phases.5 Our main finding is that local anesthesia is associated with a greater reduction in total costs further confirms the hypothesis of a reduction in anesthesia-controlled operating room time as the main factor affecting the overall total cost reduction observed, as local infiltrative anesthesia requires, on average, less time to be performed.
Only two studies23, 30 found the cost profile of peripheral nerve block-based anesthesia to be similar to that of general anesthesia regarding sciatic nerve block. A possible explanation can be that sciatic nerve block is a so-called “deep block”, i.e., an advanced block, requiring more skills and possibly more time to be performed than other peripheral nerve blocks usually applied in the outpatient setting. Marhofer et al.38 describes well the relative difficulty in the localization of the nerve and the surrounding anatomical structures due to their depth. However, Ehlers et al.39 and Marhofer40 have also shown that this block may be associated with a faster onset and higher efficacy when ultrasound-guided compared to nerve stimulation guidance. It remains to be demonstrated that these advantages actually translate into increased cost-effectiveness when compared to general anesthesia or other techniques in the ambulatory setting.
The second factor with a known impact on the perioperative process total costs is the PACU bypass rate or the recovery time when the patient requires postoperative supervision. The PACU is a highly work-intensive environment whose fixed cost is relevant.2 Total cost reduction may be achieved in case of a consistently high PACU bypass rate by a reduction in nurses equivalent staff required.23, 30 Our results confirm regional and local anesthesia techniques to be associated with a higher PACU bypass rate and a lower recovery time in comparison to general anesthesia.
The third factor that affects average total costs is the time to readiness for discharge, directly affecting the day-hospital length of stay. As discussed above, the overall day-hospital length of stay represents a significant fixed cost in the ambulatory perioperative process.4 Regional anesthesia has been associated with a lower incidence of postoperative anesthesia-related complications and side effects, translating into a quicker functional recovery and a lower time to discharge.3
In general, we can conclude that local and regional anesthesia is associated with lower total hospital costs when performed in the ambulatory setting. It is likely due to three factors: a reduction in total anesthesia-controlled operating room time, a reduction in postanesthesia recovery time and an overall shorter length of stay. These results apply to contexts where regional anesthesia can be performed regularly and systematically and where dedicated pathways are in place to enhance patient turnover in the outpatient setting, which is often the case in ambulatory surgical centers. Indeed, as stated by Philip and colleagues, a higher PACU bypass rate will only generate cost savings if utilization actually increases or staffing actually decreases.23, 30 Moreover, the reduction in anesthesia-controlled operating room time per procedure is a few minutes and thus becomes significant only if many ambulatory procedures are performed in a given program and if an induction room allows for performing the following block while the previous patient is still undergoing surgery.5 Cost-effectiveness comparisons of different anesthesia techniques are dependent on the surgical duration of the case.41, 42 Schuster et al.,41 in 2005, performing a regression function, demonstrated that the advantage of spinal anesthesia over general anesthesia in terms of operating room total fix costs reduction can be estimated to be 13% for a 50 minutes case, 9% for a 100 minutes case, and 5% for a 200 minutes case.23, 30 These data highlight the fact that regional anesthesia cost-effectiveness depends on patient turnover and is higher in contexts characterized by high turnover and high case load per operating room, such as ambulatory surgery.
Our systematic review has some limitations. Heterogeneity among studies may represent a potential source of bias in a systematic review. This heterogeneity is likely to arise through baseline differences among the patients in the included studies, diversity in methodological aspects between different studies, and different study quality. We detected significant heterogeneity and poor quality of design among several studies in our systematic review. However, we used the CHEC list to assess the methodological robustness of the studies, and some of the criteria were not properly applicable to all studies since most of them were cost-minimization analyses. The meta-analysis was substantially hampered by the presence of this heterogeneity, which would make it challenging to compare the studies. Heterogeneity was also present in estimates of savings, which vary widely and may be explained by several reasons, such as implementation differences, hospital setting, and patient mix. These analyses are often not comparable among published studies due to variations in the type of cost data and accounting practices used. Such limitations preclude the possibility to estimate an effect size.
Our literature search was carried out on four major medical databases that should provide robust and reliable search results. The inclusion of other sources might refine our search strategy, specifically the inclusion of specialized databases (i.e., NHS Economic Evaluation Database). Moreover, we selected studies published since 2000 to be sure to include only the most recent and updated data about costs. However, problems with the breadth of costs and outcomes considered exist in all the studies. Last, none of the included studies was a cost-effectiveness analysis; thus, comparing the relative costs and outcomes of the two different anesthesia regimens and estimating the possible healthcare gains were not feasible. This means that the robustness of the results and conclusions about the impact of the anesthesia regimen on the average total costs is uncertain. Hence, a cost-effective analysis is necessary to undertake an assessment of both costs and effectiveness and to determine which anesthesia regimen is the most cost-effective procedure for ensuring that resources are being used wisely.
Conclusions
Despite the limitations of this systematic review, mainly the heterogeneity of the studies and the lack of cost-effectiveness analysis, the economic impact of the anesthesia regimes on healthcare costs appears to be relevant and should be further evaluated.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgements
This work was carried out in collaboration with the Clinical Trial Unit of Ente Ospedaliero Cantonale (Ticino, Switzerland).
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:10.1016/j.bjane.2021.09.012.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.OECD . OECD Publishing; Paris: 2015. Ambulatory surgery. Health at a Glance 2015: OECD Indicators. [DOI] [Google Scholar]
- 2.Macario A., Vitez T.S., Dunn B., et al. Where are the costs in perioperative care? Analysis of hospital costs and charges for inpatient surgical care. Anesthesiology. 1995;83:1138–1144. doi: 10.1097/00000542-199512000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Chung F., Ritchie E., Su J. Postoperative pain in ambulatory surgery. Anesth Analg. 1997;85:808–816. doi: 10.1097/00000539-199710000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Saporito A., Anselmi L., Borgeat A., et al. Can the choice of the local anesthetic have an impact on ambulatory surgery perioperative costs? Chloroprocaine for popliteal block in outpatient foot surgery. J Clin Anesth. 2016;32:119–126. doi: 10.1016/j.jclinane.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 5.Dexter F., Macario A., Manberg P.J., et al. Computer simulation to determine how rapid anesthetic recovery protocols to decrease the time for emergence or increase the phase I postanesthesia care unit bypass rate affect staffing of an ambulatory surgery center. Anesth Analg. 1999;88:1053–1063. doi: 10.1097/00000539-199905000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Williams B.A., Kentor M.L., Vogt M.T., et al. Economics of nerve block pain management after anterior cruciate ligament reconstruction: potential hospital cost savings via associated postanesthesia care unit bypass and same-day discharge. Anesthesiology. 2004;100:697–706. doi: 10.1097/00000542-200403000-00034. [DOI] [PubMed] [Google Scholar]
- 7.Gupta A., Stierer T., Zuckerman R., et al. Comparison of recovery profile after ambulatory anesthesia with propofol, isoflurane, sevoflurane and desflurane: a systematic review. Anesth Analg. 2004;98:632–641. doi: 10.1213/01.ane.0000103187.70627.57. table of contents. [DOI] [PubMed] [Google Scholar]
- 8.Moher D., Liberati A., Tetzlaff J., et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Evers S., Goossens M., de Vet H., et al. Criteria list for assessment of methodological quality of economic evaluations: Consensus on Health Economic Criteria. Int J Technol Assess Health Care. 2005;21:240–245. [PubMed] [Google Scholar]
- 10.Li L.T., Bokshan S.L., Levins J.G., et al. Cost Drivers Associated With Anterior Shoulder Stabilization Surgery. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120926465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bokshan S.L., Mehta S., DeFroda S.F., et al. What Are the Primary Cost Drivers of Anterior Cruciate Ligament Reconstruction in the United States? A Cost-Minimization Analysis of 14,713 Patients. Arthroscopy. 2019;35:1576–1581. doi: 10.1016/j.arthro.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 12.Gebhardt V., Zawierucha V., Schöffski O., et al. Spinal anaesthesia with chloroprocaine 1% versus total intravenous anaesthesia for outpatient knee arthroscopy: A randomised controlled trial. Eur J Anaesthesiol. 2018;35:774–781. doi: 10.1097/EJA.0000000000000794. [DOI] [PubMed] [Google Scholar]
- 13.Hamilton G.M., Ramlogan R., Lui A., et al. Association of peripheral nerve blocks with postoperative outcomes in ambulatory shoulder surgery patients: a single-centre matched-cohort study. Can J Anaesth. 2019;66:63–74. doi: 10.1007/s12630-018-1234-8. [DOI] [PubMed] [Google Scholar]
- 14.Chandran D., Woods C.M., Schar M., et al. Cost analysis of injection laryngoplasty performed under local anaesthesia versus general anaesthesia: an Australian perspective. J Laryngol Otol. 2018;132:168–172. doi: 10.1017/S0022215117001384. [DOI] [PubMed] [Google Scholar]
- 15.Camponovo C. Spinal 1% 2-Chloroprocaine versus general anesthesia for ultra-short outpatient procedures: a retrospective analysis. Acta Biomed. 2014;85:265–268. [PubMed] [Google Scholar]
- 16.Penketh R.J., Bruen E.M., White J., et al. Feasibility of resectoscopic operative hysteroscopy in a UK outpatient clinic using local anesthetic and traditional reusable equipment, with patient experiences and comparative cost analysis. J Minim Invasive Gynecol. 2014;21:830–836. doi: 10.1016/j.jmig.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 17.Sivalingam S., Tamm-Daniels I., Nakada S.Y. Office-based ureteral stent placement under local anesthesia for obstructing stones is safe and efficacious. Urology. 2013;81:498–502. doi: 10.1016/j.urology.2012.10.021. [DOI] [PubMed] [Google Scholar]
- 18.Ahonkallio S., Santala M., Valtonen H., et al. Cost-minimisation analysis of endometrial thermal ablation in a day case or outpatient setting under different anaesthesia regimens. Eur J Obstet Gynecol Reprod Biol. 2012;162:102–104. doi: 10.1016/j.ejogrb.2012.01.025. [DOI] [PubMed] [Google Scholar]
- 19.Covarelli P., Badolato M., Tomassini G.M., et al. Sentinel lymph node biopsy under local anaesthesia versus general anaesthesia: reliability and cost-effectiveness analysis in 153 patients with malignant melanoma. In Vivo. 2012;26:315–318. [PubMed] [Google Scholar]
- 20.Stoffels I., Dissemond J., Körber A., et al. Reliability and cost-effectiveness of sentinel lymph node excision under local anaesthesia versus general anaesthesia for malignant melanoma: a retrospective analysis in 300 patients with malignant melanoma AJCC Stages I and II. J Eur Acad Dermatol Venereol. 2011;25:306–310. doi: 10.1111/j.1468-3083.2010.03786.x. [DOI] [PubMed] [Google Scholar]
- 21.Mitchell P.J., Cattle K., Saravanathan S., et al. Insertion under local anaesthetic of temporary electrodes for sacral nerve stimulation testing is reliable and cost effective. Colorectal Dis. 2011;13:445–448. doi: 10.1111/j.1463-1318.2010.02211.x. [DOI] [PubMed] [Google Scholar]
- 22.Kushwaha R., Hutchings W., Davies C., et al. Randomized clinical trial comparing day-care open haemorrhoidectomy under local versus general anaesthesia. Br J Surg. 2008;95:555–563. doi: 10.1002/bjs.6113. [DOI] [PubMed] [Google Scholar]
- 23.Mostafa H., el-Shamaa H., el-Refaai N., et al. Randomized double blind comparison between sciatic-femoral nerve block and propofol-remifentanil, propofol-alfentanil general anesthetics in out-patient knee arthroscopy. Pak J Biol Sci. 2008;11:359–365. doi: 10.3923/pjbs.2008.359.365. [DOI] [PubMed] [Google Scholar]
- 24.Horn J.L., Swide C., Gaebel B.A., et al. Comparison of efficiency, recovery profile and perioperative costs of regional anaesthesia vs. general anaesthesia for outpatient upper extremity surgery. Eur J Anaesthesiol. 2007;24:557–559. doi: 10.1017/s0265021506002195. [DOI] [PubMed] [Google Scholar]
- 25.Nishikawa K., Yoshida S., Shimodate Y., et al. A comparison of spinal anesthesia with small-dose lidocaine and general anesthesia with fentanyl and propofol for ambulatory prostate biopsy procedures in elderly patients. J Clin Anesth. 2007;19:25–29. doi: 10.1016/j.jclinane.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 26.Nordin P., Zetterström H., Carlsson P., et al. Cost-effectiveness analysis of local, regional and general anaesthesia for inguinal hernia repair using data from a randomized clinical trial. Br J Surg. 2007;94:500–505. doi: 10.1002/bjs.5543. [DOI] [PubMed] [Google Scholar]
- 27.Spanknebel K., Chabot J.A., DiGiorgi M., et al. Thyroidectomy using monitored local or conventional general anesthesia: an analysis of outpatient surgery, outcome and cost in 1,194 consecutive cases. World J Surg. 2006;30:813–824. doi: 10.1007/s00268-005-0384-3. [DOI] [PubMed] [Google Scholar]
- 28.Casati A., Cappelleri G., Aldegheri G., et al. Total intravenous anesthesia, spinal anesthesia or combined sciatic-femoral nerve block for outpatient knee arthroscopy. Minerva Anestesiol. 2004;70:493–502. [PubMed] [Google Scholar]
- 29.Forssblad M., Jacobson E., Weidenhielm L. Knee arthroscopy with different anesthesia methods: a comparison of efficacy and cost. Knee Surg Sports Traumatol Arthrosc. 2004;12:344–349. doi: 10.1007/s00167-004-0523-7. [DOI] [PubMed] [Google Scholar]
- 30.Casati A., Cappelleri G., Berti M., et al. Randomized comparison of remifentanil-propofol with a sciatic-femoral nerve block for out-patient knee arthroscopy. Eur J Anaesthesiol. 2002;19:109–114. doi: 10.1017/s0265021502000194. [DOI] [PubMed] [Google Scholar]
- 31.Danelli G., Berti M., Casati A., et al. Spinal block or total intravenous anaesthesia with propofol and remifentanil for gynaecological outpatient procedures. Eur J Anaesthesiol. 2002;19:594–599. doi: 10.1017/s0265021502000960. [DOI] [PubMed] [Google Scholar]
- 32.Lennox P.H., Chilvers C., Vaghadia H. Selective spinal anesthesia versus desflurane anesthesia in short duration outpatient gynecological laparoscopy: a pharmacoeconomic comparison. Anesth Analg. 2002;94:565–568. doi: 10.1097/00000539-200203000-00016. table of contents. [DOI] [PubMed] [Google Scholar]
- 33.Chan V.W., Peng P.W., Kaszas Z., et al. A comparative study of general anesthesia, intravenous regional anesthesia, and axillary block for outpatient hand surgery: clinical outcome and cost analysis. Anesth Analg. 2001;93:1181–1184. doi: 10.1097/00000539-200111000-00025. [DOI] [PubMed] [Google Scholar]
- 34.Martikainen M., Kangas-Saarela T., Löppönen A., et al. Two percent lidocaine spinal anaesthesia compared with sevoflurane anaesthesia in ambulatory knee surgery - cost-effectiveness, home readiness and recovery profiles. Ambul Surg. 2001;9:77–81. doi: 10.1016/s0966-6532(01)00074-9. [DOI] [PubMed] [Google Scholar]
- 35.Chilvers C.R., Goodwin A., Vaghadia H., et al. Selective spinal anesthesia for outpatient laparoscopy. V: pharmacoeconomic comparison vs general anesthesia. Can J Anaesth. 2001;48:279–283. doi: 10.1007/BF03019759. [DOI] [PubMed] [Google Scholar]
- 36.Li S., Coloma M., White P.F., et al. Comparison of the costs and recovery profiles of three anesthetic techniques for ambulatory anorectal surgery. Anesthesiology. 2000;93:1225–1230. doi: 10.1097/00000542-200011000-00015. [DOI] [PubMed] [Google Scholar]
- 37.Song D., Greilich N.B., White P.F., et al. Recovery profiles and costs of anesthesia for outpatient unilateral inguinal herniorrhaphy. Anesth Analg. 2000;91:876–881. doi: 10.1097/00000539-200010000-00020. [DOI] [PubMed] [Google Scholar]
- 38.Marhofer P., Harrop-Griffiths W., Kettner S.C., et al. Fifteen years of ultrasound guidance in regional anaesthesia: part 1. Br J Anaesth. 2010;104:538–546. doi: 10.1093/bja/aeq069. [DOI] [PubMed] [Google Scholar]
- 39.Ehlers L., Jensen J.M., Bendtsen T.F. Cost-effectiveness of ultrasound vs nerve stimulation guidance for continuous sciatic nerve block. Br J Anaesth. 2012;109:804–808. doi: 10.1093/bja/aes259. [DOI] [PubMed] [Google Scholar]
- 40.Marhofer P., Harrop-Griffiths W., Willschke H., et al. Fifteen years of ultrasound guidance in regional anaesthesia: Part 2-recent developments in block techniques. Br J Anaesth. 2010;104:673–683. doi: 10.1093/bja/aeq086. [DOI] [PubMed] [Google Scholar]
- 41.Schuster M., Gottschalk A., Berger J., et al. A retrospective comparison of costs for regional and general anesthesia techniques. Anesth Analg. 2005;100:786–794. doi: 10.1213/01.ANE.0000148685.73336.70. table of contents. [DOI] [PubMed] [Google Scholar]
- 42.Schuster M., Standl T. Cost drivers in anesthesia: manpower, technique and other factors. Curr Opin Anaesthesiol. 2006;19:177–184. doi: 10.1097/01.aco.0000192790.78139.82. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.