Abstract
Introduction: The COVID-19 vaccine is the most essential tool for altering the pandemic's trajectory. The pandemic's control is complicated by society's unwillingness to vaccinate. The aim of this cross-sectional study was to assess patients with hematological malignancies and their attitudes regarding COVID-19 immunization and to investigate COVID-19 anxiety in this susceptible population.
Methods: In this cross-sectional study, 165 patients with hematological malignancies were included. COVID-19 anxiety was evaluated with the coronavirus anxiety scale (CAS), and COVID-19 vaccine attitude was evaluated with the Vaccine Attitudes Review (VAX) scale.
Results: The mean CAS score was 2.42 (0-17). There were 22 (13%) participants with a mean CAS score of ≥ 9. Half of the participants had a CAS score of 0. The CAS score was higher in females (p = 0.023). Similarly, it was significantly higher in patients who were not in remission for hematological malignancy and who received active chemotherapy (p = 0.010). The mean VAX score was 49.07 ± 8.76 (27-72). Most of the participants (64%) had a neutral attitude toward the COVID-19 vaccination. In a survey of 165 patients, 55% said that they were skeptical about vaccination safety, and 58% said that they were concerned about unintended side effects. In addition, 90% expressed moderate concerns about commercial profiteering. Natural immunity was preferred by 30% of the participants. There was no statistically significant correlation between CAS scores and the Vaccine Attitudes Review (VAX) scale.
Conclusion: This study draws attention to the level of anxiety in patients with hematological malignancies during the COVID-19 pandemic. Negative attitudes toward the COVID-19 vaccine are worrisome for at-risk patient groups. We think that patients with hematological malignancies should be informed to eliminate their hesitations about COVID-19 vaccines.
Keywords: coronavirus disease, covid 19, vaccination attitudes, coronavirus anxiety scale, sars-cov-2, hematological malignancy, covid-19 vaccination
Introduction
The COVID-19 virus was detected in December 2019 and spread extensively over the world; the World Health Organization designated it a pandemic in March 2020 [1]. From the start of the pandemic to March 6, 2022, more than six million deaths were reported [2]. Many studies have demonstrated that COVID-19 is related to higher mortality rates in patients with cancer [3-6].
There is a lot of negative news about the pandemic on the internet, television, and social media, often including the number of cases and deaths. This causes the development of coronaphobia in society [7]. Similarly, the prevalence of fear, anxiety, and depression associated with COVID-19 is high in cancer patients [8-10]. One of the best public health measures for preventing and controlling infectious diseases is vaccination [11]. Due to concerns about the safety of vaccines developed against a new virus, the possibility of side effects, and uncertainty about protection, individuals are cautious about vaccines [12]. Vaccine hesitancy is the delay in accepting a vaccine or the rejection of a vaccine despite its availability. This is an increasing threat to both national and global health [13].
It has been shown in studies that patients, especially those with hematological malignancies, should be evaluated for COVID-19 vaccination in very high-risk categories and should be vaccinated primarily [14]. There are very few studies that determine the attitudes of patients with hematological malignancies toward COVID-19 vaccines.
This study's objective was to assess the attitudes of patients with hematological malignancies towards vaccination and determine the relationships between vaccination hesitancy and patient characteristics. The secondary aim was to identify the pandemic-related anxiety level of this patient group and to investigate whether anxiety influences vaccination propensity.
This article was previously presented as a meeting abstract at the XIII Eurasian Hematology-Oncology Congress in Istanbul, Turkey, on October 6, 2022.
Materials and methods
Population data
This cross-sectional study was conducted with hematologically malignant patients at the Hematology Clinic of the Erciyes University Hospital, in Kayseri, Turkey, from May 1 to December 1, 2021. Patients who (1) were at least 18 years old, (2) willingly accepted to participate in the survey, and (3) could understand and answer the questionnaire met the inclusion criteria.
Consent and ethical approval
Patients were briefed about the study's purpose and outcomes, and after all of their questions were answered, they signed a written informed consent form. The study protocol was reviewed and approved by the Institutional Review Board at Erciyes University. The Erciyes University Scientific Ethics Committee approved the study on September 22, 2021, with approval number 2021/625.
Research instruments
The questionnaire consisted of three parts. In the first section of the study, questions regarding the patients' sociodemographic characteristics, including age, gender, diagnosis, disease, hematopoietic stem cell transplantation (HSCT) history, educational status, marital status, and place of residence, were asked. Participants' histories of vaccinations and COVID-19 infection status were questioned on a yes-or-no basis. Two questions were used to assess previous vaccination histories: "Have you ever been vaccinated against seasonal flu in the last two years?" and "Have you ever been vaccinated against COVID-19?"
Coronavirus anxiety scale (CAS)
The second instrument was the COVID-19 pandemic-related anxiety scale or coronavirus anxiety scale (CAS) [15], which is standardized. The five items on the coronavirus anxiety scale range from 0 (not at all) to four (nearly every day over the last two weeks) on a five-point Likert-type scale. An individual was classified as having anxiety if their score was nine or greater. The CAS has good diagnostic viability and construct validity. The validity and reliability study of the scale's Turkish version was carried out by Evren et al. The scale's internal dependability was good (Cronbach's alpha = 0.80) [16].
Vaccination attitudes examination scale (VAX)
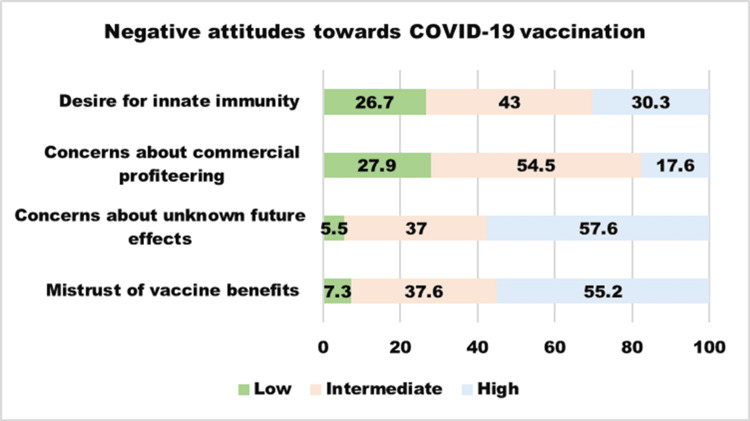
The 12-item Vaccine Attitudes Review (VAX) scale [17] was employed in the third section to assess general attitudes regarding vaccines. "Mistrust of vaccine benefits," "concerns about unknown future effects," "concerns about commercial profiteering," and "desire for innate immunity" are the four subscales on this scale. While answering the questions, participants were instructed to concentrate on the COVID-19 vaccination. The responses were graded on a six-point Likert scale ranging from one to six, with one indicating "strongly agree" and six indicating "strongly disagree." The scores for each subscale of the VAX instrument were categorized into three levels of negative attitudes toward vaccines: high (score of five to six), intermediate (score of three to four), and low (score of one to two). A higher VAX total score indicates a higher intensity of anti-vaccination attitudes. Yıldız et al. conducted content validity and reliability research in Turkey. R = 0.818 was the Cronbach alpha coefficient [18].
Statistical analysis
The IBM Statistical Package for Social Sciences (SPSS) was used to examine the study's data (version 25 for Windows, IBM Corp., Armonk, NY, USA). When using the mean and standard deviation for continuous data, absolute and percentage values were used for categorical variables. To evaluate the parameters' distribution, the Shapiro-Wilk test was used. Chi-square tests were used to make statistical comparisons on categorical data. Continuous numerical data were compared using the Student t-test for two independent samples. The relationship among quantitative data was evaluated using the Spearman correlation analysis. Values of p<0.05 were considered to indicate statistical significance.
Results
Characteristics of the study group
The basic demographics of the study group are shown in Table 1.
Table 1. Demographic and clinical characteristics of the study group (n = 165).
| Descriptive statistics n (%) | |
| Age (in years) | 48 (18 - 86) |
| 18 – 39 | 53 (32) |
| 40-59 | 62 (38) |
| >60 | 50 (30) |
| Gender, n (%) | |
| Female | 61 (37) |
| Male | 104 (63) |
| Diagnosis, n (%) | |
| Acute myeloid leukemia | 61 (37) |
| Acute lymphoblastic leukemia | 14 (9) |
| Multiple myeloma | 22 (13) |
| Hodgkin's lymphoma | 15 (9) |
| Non-Hodgkin's lymphoma | 49 (30) |
| Other | 4 (2) |
| Hematopoietic stem cell transplantation, n (%) | |
| No | 120 (73) |
| Yes | 45 (27) |
| Autologous | 18 (11) |
| Allogeneic | 27 (16) |
| Disease status, n (%) | |
| Active | 117(71) |
| Remission | 48(29) |
| Comorbidities, n (%) | |
| No | 130(79) |
| Yes | 35(21) |
| Education level, n (%) | |
| Primary school | 61 (37) |
| Middle school | 33 (20) |
| High school | 38 (23) |
| University | 33 (20) |
| Marital status, n (%) | |
| Married | 130 (79) |
| Unmarried | 35 (821) |
| Place of residence, n (%) | |
| Rural | 49 (30) |
| Urban | 116 (70) |
| Have you ever tested positive for COVID-19? n (%) | |
| No | 116 (70) |
| Yes | 49 (30) |
| Have you ever been vaccinated against COVID-19? n (%) | |
| No | 93 (56) |
| Yes | 72 (44) |
| Have you ever been vaccinated against seasonal flu in the last two years? n (%) | |
| No | 128 (77) |
| Yes | 37 (23) |
After removing those who did not complete the questionnaires (n = 12), the study comprised a total of 165 participants. The median age was 48 (18-86) years, 61 (37%) of whom were female. Most of the participants (37%) were diagnosed with acute myeloid leukemia and were undergoing chemotherapy. In addition, 21% of the patients reported having comorbidities. For educational levels, 37% (n = 61) attended primary school, 20% (n = 33) had middle school instruction, 23% (n = 38) received high school education, and 20% (n = 33) obtained university education. In terms of marital status, 79% (n = 130) of the patients were married. When the participants were evaluated according to their place of residence, 70% (n = 116) lived in urban areas and 30% (n = 49) lived in rural areas. At the time of the survey, 70% of the patients had not been infected with COVID-19, whereas 44% had been vaccinated. Furthermore, 23% had been vaccinated for the seasonal flu in the previous two years.
Outcomes of VAX
The mean VAX score was 49.07 ± 8.76 (27-72). Most of the participants (68%) had a neutral attitude towards the COVID-19 vaccination. Of the 165 participants, 55% reported high distrust of vaccine safety, while 38% were unsure about their level of confidence. Furthermore, 58% reported severe concerns about unexpected adverse effects, while 37% reported moderate concerns. Additionally, 18% expressed serious doubts about commercial profiteering. Natural immunity was highly desired by around 30% of the participants, whereas natural immunity was thought to be superior to vaccination by 43% (Figure 1).
Figure 1. A proportion of the sample reporting high, intermediate, and low negative attitudes towards vaccines.
The average of the three items each in the "mistrust of vaccine benefit," "concerns about unknown future effects", "concerns about commercial profiteering", and "desire for innate immunity" subscales were used as the outcome measure, and the average participant scores were 4.66, 4.72, 3.2, and 3.75, respectively. The results are recorded in Table 2.
Table 2. Scores of the coronavirus anxiety scale (CAS) and Vaccination Attitudes Examination (VAX) scale .
| Variables | Mean / Standard deviation / Range | Items |
| CAS | 2.42 ± 3.46 (0-17) | 1-5 |
| VAX | 49.07± 8.76 (27-72) | 1-12 |
| Mistrust of vaccine benefits | 4.66 ± 1.26 | 1-3 |
| Concerns about unknown future effects | 4.72±1.19 | 4-6 |
| Concerns about commercial profiteering | 3.22±1.24 | 7-9 |
| Desire for innate immunity | 3.75±1.54 | 10-12 |
| Total | 4.08±0.73 | 1-12 |
Outcomes of CAS
The sample’s overall CAS mean score was 2.42 (SD = 3.47) (0-17). There were 22 (13%) participants with a mean CAS score of ≥ 9. Half of the participants had a CAS score of 0. Eighty-two (50%) patients had some level of anxiety (CAS score 1-20). By gender, women expressed a higher CAS score than men (p = 0.023). The mean score for women on the CAS was 3.39, while the mean score for men was 1.85. Similarly, it was significantly higher in patients who were not in remission for a hematological malignancy and who had received active chemotherapy (p=0.010) (Table 3).
Table 3. Investigation of the relationship between demographic and clinical characteristics and CAS and VAX scores.
| Variables | CAS | p-value | VAX | p-value |
| Age (in years) | ||||
| 18 – 39 | 1.58±3.26 | 0.079 | 50.7 ±9.18 | 0.174 |
| 40-59 | 2.82±3.74 | 48.9 ±7.69 | ||
| >60 | 2.80±3.22 | 47.52 ±9.39 | ||
| Gender | ||||
| Female | 3.39±4.08 | 0.023 | 50.6±8.60 | 0.073 |
| Male | 1.85±2.82 | 48.14±8.75 | ||
| Diagnosis | ||||
| Acute myeloid leukemia | 2.64±3.49 | 0.894 | 49.83±7.93 | 0.898 |
| Acute lymphoblastic leukemia | 1.71±2.73 | 50.85±8.55 | ||
| Multiple myeloma | 1.55±2.87 | 47.53±11.45 | ||
| Hodgkin's lymphoma | 2.27±4.35 | 47.68±7.10 | ||
| Non-Hodgkin's lymphoma | 2.86±2.87 | 48.6±9.52 | ||
| Other | 1.62±2.63 | 45.7±10.37 | ||
| Disease status | ||||
| Active | 2.83±3.67 | 0.010 | 48.41±8.65 | 0.131 |
| Remission | 1.42±2.68 | 50.68±8.88 | ||
| Comorbidities | ||||
| Yes | 2.86±3.11 | 0.108 | 47.80±8.43 | 0.563 |
| No | 2.30±3.55 | 49.42±8.85 | ||
| Hematopoietic stem cell transplantation | ||||
| Yes | 1.87±3.2 | 0.086 | 49.22±8.76 | 0.963 |
| No | 2.63±3.52 | 49.02±8.80 | ||
| Education level | 0.115 | 0.699 | ||
| Primary school | 3.41±3.95 | 48.91±8.42 | ||
| Middle school | 2.03±2.54 | 48±10.18 | ||
| High school | 1.74±2.91 | 50.4±7.26 | ||
| University | 1.76±3.59 | 48.8±9.59 | ||
| Marital status | ||||
| Unmarried | 1.91±3.64 | 0.160 | 51±10.53 | 0.051 |
| Married | 2.55±3.41 | 48.56±8.19 | ||
| Place of residence | ||||
| Rural | 2.51±3.44 | 0.645 | 49.51±8.62 | 0.68 |
| Urban | 2.38±3.49 | 48.89±8.84 | ||
| Have you ever tested positive for COVID-19? | ||||
| Yes | 2.8±3.95 | 0.872 | 50.28±9.32 | 0.251 |
| No | 2.26±3.24 | 48.56±8.50 | ||
| Have you ever been vaccinated against COVID-19? | ||||
| Yes | 2.72±3.74 | 0.232 | 47.69±8.71 | 0.074 |
| No | 2.18±3.23 | 50.15±8.69 |
Evaluation of CAS relationship with the VAX scale
There was no statistically significant correlation between CAS scores and the Vaccine Attitudes Review (VAX) scale (Table 4).
Table 4. Investigation of the correlation between CAS scores and the Vaccine Attitudes Review (VAX) scale.
| VAX | CAS>9 | Cas<9 | p-value |
| Mistrust of vaccine benefit (items 1–3) | |||
| Low | 1 (0.6) | 11 (7) | 0.404 |
| İntermediate | 6 (3.6) | 56 (34) | |
| High | 15 (9) | 76 (46) | |
| Concerns about unknown future effects (items 4-6) | |||
| Low | 1 (0.6) | 8 (5) | 0.974 |
| İntermediate | 8 (4.8) | 53 (32) | |
| High | 13 (8) | 82 (50) | |
| Concerns about commercial profiteering (items 7-9) | |||
| Low | 5 (3) | 41(24.8) | 0.649 |
| Intermediate | 14 (8.5) | 76 (46) | |
| High | 3 (1.8) | 26(15.8) | |
| Desire for innate immunity (items 10–12) | |||
| Low | 4 (2.4) | 40 (24.2) | 0.591 |
| İntermediate | 11 (6.7) | 60 (36.4) | |
| High | 7 (4.2) | 43 (26.1) | |
| Total (items 1–12) | |||
| Low | 0 (0) | 2 (1.2) | 0.748 |
| İntermediate | 15 (9.1) | 97 (58.8) | |
| High | 7 (4.2) | 44 (26.7) |
Discussion
Our study, to our knowledge, is the first to assess how patients with hematological malignancies think about COVID-19 vaccines and their anxiety associated with COVID-19. When we reviewed the literature, there was a gap in studies evaluating COVID-19 anxiety and attitudes toward vaccines in patients with hematological malignancies. This included a large number of patients with hematological malignancies, representing a vulnerable population most affected by the pandemic. According to research conducted on cancer patients, COVID-19 caused them great dread and distress [10, 19-21]. In our study, it was found that the mean CAS score of the patients was 2.42 ± 3.47. Half of the participants had a CAS score of 0. While conducting our study, we expected a high level of COVID-19-related anxiety in patients. However, we found low anxiety scores in our study. Our findings were not compatible with the literature's findings. Studies have shown that a high level of knowledge among cancer patients is associated with decreased anxiety [22].
Since the beginning of the pandemic, we have informed our patients in detail about COVID-19 and tried to address their concerns. We think that our patients have a high level of knowledge about the COVID-19 infection and its management. Anxiety was significantly higher in female patients and those with active disease. In a study analyzing the psychological distress of lymphoma patients during the COVID-19 pandemic, women were revealed to be at higher risk, which is similar to our data. [23]. This may be due to cultural differences. In Turkish society, men may not express their feelings as much as women. In a study of cancer patients, 34.3% of patients rated cancer as more dangerous than COVID-19, while 59% thought that COVID-19 was more severe in cancer patients. In the same study, 45.6% of the patients reported that the pandemic negatively affected their cancer care [24].
In our study, a statistically higher rate of anxiety was found in cancer patients receiving active chemotherapy than in patients in remission. The COVID-19 pandemic has caused problems, such as not being able to receive treatment due to the lack of health resources among individuals, who have to apply to the hospital regularly for follow-up and treatment. In addition, the thought that there may be a delay in diagnosis and treatment for cancer patients receiving active treatment may have created more anxiety.
This study showed an intermediate vaccine hesitancy score (M = 4.08). In a study of 3960 people who expressed their hesitation about the COVID-19 vaccine, the most frequently expressed reason was concerns about the novelty of the vaccine. At the same time, general distrust was widespread due to concerns about the safety of the vaccine [25]. Our findings suggest that patients with hematological malignancies have a distrust of the benefits of COVID-19 vaccines and concerns about their unpredictable effects. Studies have shown that the groups with the highest mistrust of vaccines are women, children, and individuals with low education levels and low socioeconomic status [26-30]. We found no association between demographic and clinical characteristics and vaccination acceptance.
However, it provides important data for evaluating factors associated with vaccine hesitancy in patients with hematological malignancies. Vaccination is the most important strategy in the fight against COVID-19. Emphasizing the importance of vaccination, especially in vulnerable patient groups, may facilitate the acceptance of COVID-19 vaccines.
Due to its cross-sectional design and small sample size, this study has some limitations. Our study's lack of a control group made up of healthy adults is another drawback.
Conclusions
This study showed that patients with active cancer have a relatively higher rate of COVID-19 anxiety. Our findings are important in terms of demonstrating the mistrust of the usefulness of the vaccine in patients with hematological malignancies, concerns about side effects, and commercial concerns. One of the biggest barriers to vaccination is misinformation, especially on the Internet. Increasing knowledge about vaccination and promoting trust among health authorities can help reduce vaccination hesitancy. Hematologists and oncologists should promote the COVID-19 vaccine for patients with cancer.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. Erciyes University Institutional Review Board issued approval 2021/625
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Who declares COVID-19 a pandemic. Cucinotta D, Vanelli M. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coronavirus case. 2023. https://www.worldometers.info/coronavirus/. https://www.worldometers.info/coronavirus/.
- 3.Factors associated with COVID-19-related death using OpenSAFELY. Williamson EJ, Walker AJ, Bhaskaran K, et al. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Analyses of risk, racial disparity, and outcomes among US patients with cancer and COVID-19 infection. Wang Q, Berger NA, Xu R. JAMA Oncol. 2021;7:220–227. doi: 10.1001/jamaoncol.2020.6178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Risk factors and outcome of COVID-19 in patients with hematological malignancies. Piñana JL, Martino R, García-García I, et al. Exp Hematol Oncol. 2020;9:21. doi: 10.1186/s40164-020-00177-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: a multicentre, retrospective, cohort study. Yang K, Sheng Y, Huang C, et al. Lancet Oncol. 2020;21:904–913. doi: 10.1016/S1470-2045(20)30310-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coronaphobia: fear and the 2019-nCoV outbreak. Asmundson GJ, Taylor S. J Anxiety Disord. 2020;70:102196. doi: 10.1016/j.janxdis.2020.102196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Depression and anxiety among patients with cancer during COVID-19 pandemic: a systematic review and meta-analysis. Ayubi E, Bashirian S, Khazaei S. J Gastrointest Cancer. 2021;52:499–507. doi: 10.1007/s12029-021-00643-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anxiety and depression in patients with advanced cancer during the COVID-19 pandemic. Obispo-Portero B, Cruz-Castellanos P, Jiménez-Fonseca P, et al. Support Care Cancer. 2022;30:3363–3370. doi: 10.1007/s00520-021-06789-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Effect of COVID-19 fear and COVID-19 anxiety on sleep quality of breast cancer patients. Runida D, Menekli T. https://www.proquest.com/scholarly-journals/effect-covid-19-fear-anxiety-on-sleep-quality/docview/2595143025/se- Int J Caring Sci. 2021;14:1248–1257. [Google Scholar]
- 11.Mandatory and recommended vaccination in the EU, Iceland and Norway: results of the VENICE 2010 survey on the ways of implementing national vaccination programmes. Haverkate M, D'Ancona F, Giambi C, Johansen K, Lopalco PL, Cozza V, Appelgren E. Euro Surveill. 2012;17:20183. doi: 10.2807/ese.17.22.20183-en. [DOI] [PubMed] [Google Scholar]
- 12.Primary care clinicians as COVID-19 vaccine ambassadors. Katzman JG, Katzman JW. J Prim Care Community Health. 2021;12:21501327211007026. doi: 10.1177/21501327211007026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bibliometric analysis of global scientific literature on vaccine hesitancy in peer-reviewed journals (1990-2019) Sweileh WM. BMC Public Health. 2020;20:1252. doi: 10.1186/s12889-020-09368-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Priority COVID-19 vaccination for patients with cancer while vaccine supply is limited. Ribas A, Sengupta R, Locke T, et al. Cancer Discov. 2021;11:233–236. doi: 10.1158/2159-8290.CD-20-1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coronavirus anxiety scale: A brief mental health screener for COVID-19 related anxiety. Lee SA. Death Stud. 2020;44:393–401. doi: 10.1080/07481187.2020.1748481. [DOI] [PubMed] [Google Scholar]
- 16.Measuring anxiety related to COVID-19: a Turkish validation study of the coronavirus anxiety scale. Evren C, Evren B, Dalbudak E, Topcu M, Kutlu N. Death Stud. 2022;46:1052–1058. doi: 10.1080/07481187.2020.1774969. [DOI] [PubMed] [Google Scholar]
- 17.Understanding the dimensions of anti-vaccination attitudes: the vaccination attitudes examination (VAX) scale. Martin LR, Petrie KJ. Ann Behav Med. 2017;51:652–660. doi: 10.1007/s12160-017-9888-y. [DOI] [PubMed] [Google Scholar]
- 18.Assessment of validity and reliability of the Turkish version of the vaccination attitudes examination (VAX) scale. Yildiz E, Gungormus Z, Dayapoglu N. https://www.proquest.com/scholarly-journals/assessment-validity-reliability-turkish-version/docview/2537156898/se-2 Int J Caring Sci. 2021;14:261–268. [Google Scholar]
- 19.Perspectives, knowledge, and fears of cancer patients about COVID-19. Guven DC, Sahin TK, Aktepe OH, Yildirim HC, Aksoy S, Kilickap S. Front Oncol. 2020;10:1553. doi: 10.3389/fonc.2020.01553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Understanding the psychological impact of COVID-19 pandemic on patients with cancer, their caregivers, and health care workers in Singapore. Ng KY, Zhou S, Tan SH, et al. JCO Glob Oncol. 2020;6:1494–1509. doi: 10.1200/GO.20.00374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sleep disturbances, fear, and generalized anxiety during the COVID-19 shut down phase in Germany: relation to infection rates, deaths, and German stock index DAX. Hetkamp M, Schweda A, Bäuerle A, et al. Sleep Med. 2020;75:350–353. doi: 10.1016/j.sleep.2020.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Satisfaction with information and unmet information needs in men and women with cancer. Faller H, Koch U, Brähler E, et al. J Cancer Surviv. 2016;10:62–70. doi: 10.1007/s11764-015-0451-1. [DOI] [PubMed] [Google Scholar]
- 23.Psychological distress in outpatients with lymphoma during the COVID-19 pandemic. Romito F, Dellino M, Loseto G, et al. Front Oncol. 2020;10:1270. doi: 10.3389/fonc.2020.01270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Understanding COVID-19 vaccine hesitancy and resistance: another challenge in cancer patients. Mejri N, Berrazega Y, Ouertani E, Rachdi H, Bohli M, Kochbati L, Boussen H. Support Care Cancer. 2022;30:289–293. doi: 10.1007/s00520-021-06419-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.COVID-19 vaccine hesitancy and acceptance among individuals with cancer, autoimmune diseases, or other serious comorbid conditions: cross-sectional, Internet-based survey. Tsai R, Hervey J, Hoffman K, et al. JMIR Public Health Surveill. 2022;8:0. doi: 10.2196/29872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. The COCONEL Group. Lancet Infect Dis. 2020;20:769–770. doi: 10.1016/S1473-3099(20)30426-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Sherman SM, Smith LE, Sim J, et al. Hum Vaccin Immunother. 2021;17:1612–1621. doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: outlining evidence-based and theoretically informed future intervention content. Williams L, Gallant AJ, Rasmussen S, et al. https://doi.org/10.1111/bjhp.12468. Br J Health Psychol. 2020;25:1039–1054. doi: 10.1111/bjhp.12468. [DOI] [PubMed] [Google Scholar]
- 29.Public perceptions of COVID-19 in Australia: perceived risk, knowledge, health-protective behaviors, and vaccine intentions. Faasse K, Newby J. Front Psychol. 2020;11:551004. doi: 10.3389/fpsyg.2020.551004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.A systematic review of the sex and gender reporting in COVID-19 clinical trials. Heidari S, Palmer-Ross A, Goodman T. Vaccines (Basel) 2021;9:1322. doi: 10.3390/vaccines9111322. [DOI] [PMC free article] [PubMed] [Google Scholar]