Abstract
Introduction:
Smoking prevalence has decreased considerably in Brazil from 34.8% in 1989 to 12.6% in 2019 owing to the implementation of strong tobacco control policies. However, recent data show that the downward trend may be stagnating. Detailed analyses of historical smoking patterns by birth cohort could guide tobacco control decision making in Brazil.
Methods:
Using the 2008 Global Adult Tobacco Survey and the 2013 and 2019 National Health Surveys, historical smoking patterns in Brazil were estimated, supplemented with data from the 2006‒2019 Surveillance System of Risk Factors for Chronic Diseases by Telephone Interviews. Age‒period‒cohort models with constrained natural splines were applied to estimate the annual probabilities of smoking initiation and cessation, current smoker prevalence, and mean cigarettes smoked per day by age, gender, and birth cohort. Analysis was conducted in 2021‒2022.
Results:
Current smoker prevalence has declined considerably since the 1950 and 1955 birth cohorts for males and females, respectively, reflecting decreased smoking initiation and increased smoking-cessation probabilities over time. Among female cohorts born on or after 2000, smoking initiation may be increasing even as their smoking cessation has increased considerably. Mean cigarettes smoked per day has remained relatively constant across period and cohorts, showing only a minor decrease among males.
Conclusions:
These detailed cohort-specific smoking parameters can be used to inform models that evaluate the impact of tobacco use and policies on long-term health outcomes and guide public health decision making in Brazil. Stagnant mean cigarettes smoked per day, increasing female smoking initiation, and limited improvement in male cessation among recent cohorts present challenges to tobacco control.
INTRODUCTION
Brazil is considered a global leader in tobacco control because of its exemplary domestic tobacco policies1,2: prohibitions on many forms of tobacco advertising dating back to the 1980s; a National Program to Control Tobacco Use launched in 1989; ratification and implementation of the WHO Framework Convention on Tobacco Control in 2005 and 2006; and comprehensive legislation in 2011 ensuring nationwide smoke-free air law, increased tobacco taxes, and large graphic health warnings on cigarette packs.1 A law banning flavors in tobacco products, including menthol, was passed in 2012 but has yet to be implemented.3 Because of these hard-won policies, smoking declined from 34.8% in 1989 to 12.6% in 2019.4–8 However, smoking-attributable deaths still make up 14.9% of all deaths among males.9 Further study of smoking patterns in Brazil is still necessary for several reasons.
First, recent surveillance estimates suggest that past declines are stagnating or possibly reversing for youth, and detailed data could help explain their underlying drivers. From 2015 to 2019, adolescent male smoking prevalence remained constant, whereas adolescent female smoking prevalence increased from 6.0% to 6.5%,10–13 although the change was not statistically significant. Other recent analyses indicate widespread non-compliance with laws prohibiting cigarette sales to minors.14 Analyses of trends for Brazil are key to understanding historical patterns and what that means for future projections of smoking in a country whose policies affect over 200 million people.
Second, monitoring national smoking prevalence and its underlying components—initiation, cessation, intensity—allows a comprehensive picture of smoking dynamics across the population. Previous research on trends in smoking in Brazil has focused almost exclusively on smoking prevalence using data from an annual non-nationally representative survey of residents in state capitals (Surveillance System of Risk Factors for Chronic Diseases by Telephone Interviews [VIGITEL]).15–17 Most also examine smoking by age and period (calendar year), with one recent exception that analyzed smoking prevalence by birth cohort.18 These studies do not specifically analyze initiation and cessation behaviors, the underlying drivers of overall smoking prevalence. Initiation and cessation are addressed differently by tobacco control policies and programs (preventing smoking initiation among youth versus promoting successful cessation among adult smokers) and should therefore be examined separately. The omission of smoking intensity in trend analyses also precludes the evaluation of changing consumption patterns within the smoking population, although some studies have attempted to do so.5,19 Understanding smoking intensity is critical to assess the risk of lung cancer and chronic obstructive pulmonary disease, which varies as a function of intensity and duration.20,21
Third, recent historical smoking trend analyses have not been nationally representative. To date, studies have relied on data from VIGITEL, an annual cross-sectional survey conducted since 2006. However, VIGITEL participants are exclusively based in state capitals capturing only those aged ≥18 years representing ~25% of the total urban population, 20% of Brazil’s total adult population, and 17% of the smoking population.22,23 Moreover, VIGITEL surveys participants with landlines, but landline coverage has been decreasing and typically belong to those at higher income levels. Therefore, low-income populations are underrepresented and may differ in ways that sampling and poststratification weights cannot correct for. Other health surveys are considered nationally representative, such as the Global Adult Tobacco Survey (GATS) and the Brazilian National Survey of Health (PNS), but smoking data are collected through these surveys only sporadically.
Finally, detailed historical smoking analyses provide important information when evaluating the effectiveness of past and present tobacco control policies and facilitate the development of tools that could support future decision making. The Cancer Interventional and Surveillance Modeling Network (CISNET) has produced detailed analyses of smoking histories by age, gender, and birth cohort for the U.S. population.24,25 CISNET smoking histories characterize not only smoking prevalence but also smoking initiation, cessation, and intensity (mean cigarettes smoked per day [CPD]). These estimates are used for surveillance and evaluation of the impact of tobacco control interventions on population health.26–30 The fitted models use the linear logistic framework for estimating age, period, and cohort effects on temporal trends. Hence, one important scientific contribution of this application of statistical modeling is that it explicitly estimates and accounts for birth cohort effects, that is, the generational trends for each type of smoking behavior. An earlier model of smoking in Brazil quantified the public health benefit of its tobacco control policies but did not use parameters specific to Brazil’s unique smoking initiation and cessation trajectories.4 This study extends the CISNET methodology24 to characterize histories of smoking initiation, cessation, prevalence, and intensity for the population of Brazil by age, gender, and birth cohort. These detailed estimates of historical smoking patterns by birth cohort across the population can inform future tobacco control and public health decision making in Brazil.
METHODS
Study Sample
Nationally representative smoking data were available through the 2008 GATS that was embedded in the National Household Sample Survey (n=39,425; response rate=94.0%), the 2013 PNS (n=222,385; 86.0%), and the 2019 PNS (n=293,725; 93.6%).3,12 All the 3 were cross-sectional surveys designed to conduct individual interviews on tobacco use, with similar questions on smoking behaviors, employing a complex probabilistic sample with several selection stages (e.g., census tracts, households, and individuals). These data were pooled into 1 national data set and were used to estimate smoking initiation, cessation, and intensity. However, because of selection bias, these parameters require adjustment on the basis of analysis of ever-smoker prevalence, for which detailed age patterns over time are necessary. Although the VIGITEL data have limitations, they are collected annually and provide a good resolution for such age patterns. Therefore, age patterns were separately analyzed from the annual 2006−2019 VIGITEL (n=730,309; response rates ranged from 64.9% to 76.5%). The VIGITEL age effects were then used as inputs to estimate period and cohort effects from the national (GATS and PNS) data. Details about the sampling designs for these surveys have been reported previously.31–33
Information regarding never, current, and former smoking status as well as information on the age of smoking initiation and cessation were extracted from each survey. GATS and PNS data were analyzed accounting for their sample weights. This study used public, deidentified data.
Measures
This analysis defines smoking status on the basis of the use of combustible tobacco. Survey questions refer to smoking any tobacco product, which may include other noncigarette combustible tobacco products such as bidis, pipes, cigars, cigarillos, and water pipes. However, cigarette smoking remains the dominant form of combustible tobacco used in Brazil representing 97.6% of overall smoking prevalence in 2019.8
Current smokers were those who smoked >100 cigarettes in their lifetime and self-reported currently smoking any tobacco products at the time of the survey. Former smokers smoked >100 cigarettes in their lifetime and reported that they smoked in the past but currently do not smoke any tobacco products. Never smokers were participants indicating that they never used tobacco products or had not reached the lifetime 100 cigarettes use threshold. Smoking intensity was obtained through questions ascertaining daily or weekly cigarette use; cigarettes smoked per week were converted into an average daily cigarette equivalent where 7 per week would be considered 1 per day. Participants with smoking histories self-reported age at initiation and cessation (Appendix Table 1, available online).
Statistical Analysis
Age‒period‒cohort (APC) models were used to estimate the following age-specific smoking parameters by birth cohort (1950 −2000) and gender: smoking initiation and cessation probabilities; the prevalence of ever, current, and former smoking; and CPD (i.e., smoking intensity) among adults who were currently smoking.24,34 CPD smoked were categorized as (approximate mean CPD within a category): CPD≤5 (3), 5<CPD≤15 (10), 15<CPD≤25 (20), 25<CPD≤35 (30), 35<CPD≤45 (40), and 45<CPD (60).
VIGITEL covered a longer time span than the national data, which provided better estimates of age trend patterns for ever-smoker prevalence. However, the national surveys provided better coverage for the country, so the analytical approach sought to capture the strengths of each set of surveys. First, an age-cohort logistic regression model using only the VIGITEL data for ever-smoker prevalence was used to estimate age and cohort effects. Second, a model was fitted using the national data set to estimate cohort effects, but the age effects from the VIGITEL analysis were used by including these as an offset for the model. This assumes that the VIGITEL surveys better capture the effect of age while at the same time using the national to better summarize results for the country. Finally, APC logistic regression models were used to estimate the probabilities of smoking initiation, cessation, and intensity in the national data set because both period and cohort effects are important to explain the temporal trends of these smoking parameters. Because these analyses expand the time frame using retrospectively collected information, it was possible to obtain these estimates using only the national data. All analyses accounted for sample weights using the survey package logistic regression in R (Version 4.0).35 Initiation probabilities by cohort were adjusted to produce predictions of ever-smoking prevalence consistent with estimated ever-smoker prevalence at age 30 years (Appendix, available online, provides details).
RESULTS
Results are presented for selected birth cohorts by gender from 1950 to 2000 in 5-year intervals from 1955 to 2019. Results for additional birth cohorts are available and can be downloaded at https://apps.cisnetsmokingparameters.org/Brazil/.
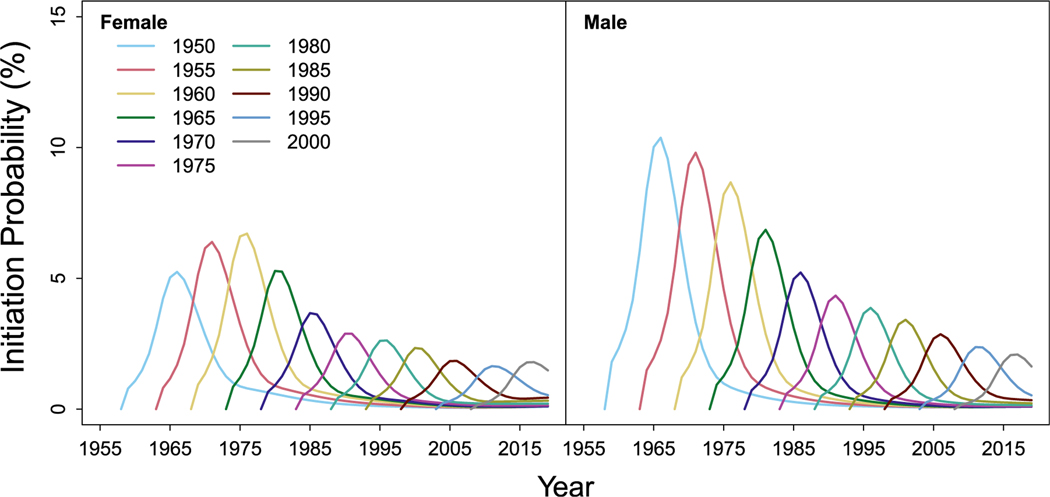
Figure 1 shows age-specific smoking initiation probabilities. Within each birth cohort, initiation probabilities generally peak during adolescence and early adulthood before declining thereafter. For all cohorts, initiation probabilities are higher for males than for females. Initiation probabilities have been decreasing by birth cohort for males, with a rapid decrease from the 1960 to 1965 birth cohorts and the 1965 to 1970 birth cohorts. Females showed similar patterns, except with slight increases in initiation among the oldest (1950−1955) and most recent (1995−2000) birth cohorts.
Figure 1.
Age-specific smoking initiation probabilities (percentage) for selected 1950−2000 birth cohorts by gender in Brazil.
Note: An interactive version of this figure’s data can be found at https://apps.cisnetsmokingparameters.org/Brazil/.
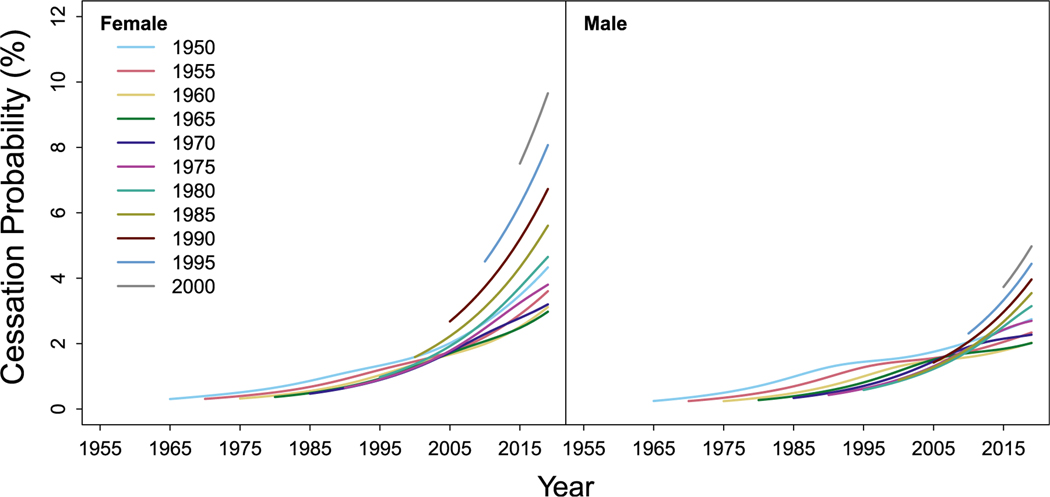
Figure 2 shows age-specific smoking-cessation probabilities. Across all cohorts and genders, the likelihood of cessation generally increases with age. Females show higher cessation probabilities than males, especially in recent birth cohorts. Among 1950−1955 male birth cohorts, a slight bump occurs around ages 35−45 years, which does not appear in more recent birth cohorts. Cessation probabilities have been increasing in recent cohorts. Female cessation shows dramatic increases among birth cohorts born from 1990 onward. Among males, there are similar increases in cessation but without the larger changes exhibited by females.
Figure 2.
Age-specific smoking-cessation probabilities (percentage) for selected 1950−2000 birth cohorts by gender in Brazil.
Note: An interactive version of this figure’s data can be found at https://apps.cisnetsmokingparameters.org/Brazil/.
Figure 3 shows age-specific current smoking prevalence. Prevalence remains higher among males than among females and generally increases and peaks during adolescence and young adulthood (maximum around age 20 years) before declining through later adulthood. Among males, current smoker prevalence was highest in the 1950 birth cohort, declining consistently across birth cohorts, with the lowest observed prevalence in the 2000 birth cohort. Females had a notable increase in smoking from the 1950−1960 birth cohorts, before declining hereafter. Although smoking among the 1960 female birth cohort is quite the same as that among the 1955 cohort, substantial decreases occur in the 1965−1970 birth cohorts, reflecting a rapid decrease in initiation for these birth cohorts.
Figure 3.
Age-specific current smoking prevalence for selected 1950−2000 birth cohorts by gender in Brazil.
Note: An interactive version of this figure’s data can be found at https://apps.cisnetsmokingparameters.org/Brazil/.
Figure 4 shows age-specific mean CPD. Males have higher estimated smoking intensity than females across cohorts. Across all cohorts, smoking intensity increases with age through middle adulthood, peaking around age 45 years. For females, only moderate declines in CPD are observed at later ages, whereas males show noticeably steeper decreases in intensity at older ages, although a minor second bump is observed in the 1950 birth cohort. Peaks in mean CPD have remained constant across female birth cohorts, but show a slight decline with more recent male birth cohorts. Results for ever-smoking prevalence, mean smoking duration, and pack-years are shown in Appendix Figures 2−4 (available online).
Figure 4.
Age-specific mean CPD for selected 1950−2000 birth cohorts by gender in Brazil.
Note: An interactive version of this figure’s data can be found at https://apps.cisnetsmokingparameters.org/Brazil/. CPD, cigarettes smoked per day.
DISCUSSION
The smoking parameters generated by this study improve the existing understanding of historical patterns in Brazil by leveraging nationally representative surveys. Current smoker prevalence has declined over the last several decades, reflecting both decreased initiation and increased cessation. Female smoking patterns show slightly lower but rising initiation and higher cessation probabilities than males, especially in the 2000 birth cohort. However, female smoking initiation is stagnant or even worsening for the most recent birth cohorts, with an increase between the 1995−2000 cohorts, bringing female initiation closer to that of males. Male smoking initiation shows minor improvements in more recent cohorts. This is consistent with adolescent smoking data from school-based surveys that suggest stagnation among males and possible increases among females.10–13
The results also suggest that cessation probabilities could be increasing among more recent birth cohorts, especially for females. Societal changes, such as increases in smoke-free workplaces and homes or devaluation of Brazilian currency from 2017 to 2019 (reduced cigarette purchasing power), may be contributing factors.36–38 Although these data may signal encouraging trends, they appear to conflict with 2013 and 2019 surveys showing that the proportion of young adult women who made a quit attempt decreased from 60.1% to 52.7%, and the proportion who reported quitting in the past 2 years decreased from 48.2% to 20.6%.22,39 It is not clear what could cause this discrepancy. Estimates for more recent birth cohorts are based on fewer years of data and younger respondents, making the estimates less reliable than for cohorts with more information available across the life course, but survey data on self-reported quit attempts are also not directly comparable with APC estimates of annual cessation probabilities. Future research should determine the relationship between policy changes, quit attempts, and long-term smoking cessation among recent birth cohorts in Brazil.
Although other metrics of smoking prevalence, initiation, and cessation have generally shown major improvements over time and across birth cohorts, mean CPD has remained stagnant for females and shown only minor decreases for males. The absence of improvements in smoking intensity may reflect the stagnant policy environment in Brazil. In recent years, no major changes in tobacco control policies have occurred at the national level, and some consumers may be migrating to cheaper illicit cigarettes. The share of illicit cigarette consumption as a proportion of total cigarette consumption has fluctuated over the years, from 16.6% in 2008 to 31.1% in 2013 and then 42.8% in 2016. Since 2016, the share has decreased; however, Brazil has one of the highest proportions of illicit cigarette consumption in the world at ~39%.37,40–42 In addition, cigarette minimum prices and specific excise tax rates in Brazil remain unchanged since 2016. Because the price of tobacco products has not been adjusted for inflation or the increased buying power of Brazilian consumers, the real price of a pack of cigarettes has decreased for 4 consecutive years since 2017, making them more affordable.37,41,43 Rising cigarette affordability could similarly influence initiation and cessation behaviors, either by directly worsening trends or by slowing the pace of progress. However, the methods used in this study preclude direct causal inferences between policies and smoking outcomes.
Although E-cigarettes are banned in Brazil, 0.6% of the population (~1 million people) reported current E-cigarette use in 2019, the majority of whom were young adults.44 It is unclear how E-cigarettes may influence future smoking among young people. However, the current ban limits the potential for E-cigarettes to alter smoking trajectories among young people.
This is the first study to offer a comprehensive historical account of smoking behaviors by birth cohort across Brazil’s population. Cohort analyses of smoking require historical data covering a long period with samples that include older and recent birth cohorts. High-income nations benefit from long historical time-series data; for example, the U.S. began collecting smoking data as early as 1965.45 Many low- and middle-income countries (LMICs), including Brazil, have data limitations that preclude such historical analyses. Although Brazil has a nationwide surveillance system tracking tobacco use—which many LMICs lack—when data are not collected annually or with set frequencies, the absence of information presents challenges for time-series analyses and forecasting. The validated APC methodology pioneered by CISNET, already extended to numerous U.S. populations,24,25,28,34,46–50 has been adapted for Brazil, allowing a thorough investigation of trends in smoking because they have varied across cohorts and time.
The data generated from this study can be applied to simulation models that aim to project the long-term health outcomes associated with tobacco use and policies in Brazil.51 Recent work has estimated price elasticities of tobacco consumption,52 the market effects of tobacco tax reforms,53 and the effects of smoke-free air laws on young adult smoking initiation and cessation.54 Future evaluations could similarly quantify the separate effects on initiation and cessation so that the impact of policies on smoking prevention versus cessation is better understood. These types of studies offer policy parameters that could be combined with the smoking histories produced in this paper and collectively serve as inputs to models of tobacco use and policy in Brazil.
This methodology can be similarly applied to LMICs. However, other challenges remain. Unlike many LMICs with scarcer resources, Brazil has comparatively more data that can be used for smoking trend analyses. Researchers may wish to explore creative ways to solve such challenges. For example, the International Agency for Research on Cancer estimates the burden of cancer for countries with missing data by borrowing information from nearby regions with similar health profiles.55 Another data challenge is the absence of consistent, repeated measures of smoking over long periods. Even in resource-rich countries, survey design changes can present challenges for trend analysis. Researchers with such data limitations will need to explore ways to harmonize across data sources when necessary, whereas government health agencies must be careful to preserve consistent measures in national surveys over time.
Future research should explore Brazilian smoking trends and disparities as they relate to income, education, race, and location. Geographic disparities reflect variations in cigarette prices and smoking prevalence across Brazilian states and are worthy of analysis.8,16 The study tells the history of smoking behaviors in Brazil but does not identify which factors led to observed changes. Other research methods should ascertain the effects of policy changes on the trends revealed by this study. Although this study precludes causal inference, the recently observed stagnation in smoking patterns suggests the potential need for increased tobacco control efforts.
Limitations
This analysis is strengthened by its use of nationally representative surveys on adult smoking in Brazil. However, GATS and PNS surveys offer only 3 data collection periods, over 11 years. The study is also limited by its need to combine data across surveys with different designs, samples, and questions. To the extent possible, smoking measures were harmonized across data sources. The absence of consecutive years of survey data also limits the number of observations included. To mitigate this, information from the VIGITEL data on the effects of age on smoking was integrated into the process of estimating ever-smoker prevalence (Appendix, available online). This assumes that age patterns of ever smoking in Brazilian capitals are generalizable to the rest of the country. Differences between the GATS and PNS were relatively minor because they share similar complex sampling designs and smoking questions, but the VIGITEL uses a different survey design and sample entirely.31–33 Although available data sources do not stretch back farther into time, this is typical of many LMICs with less epidemiologic infrastructure.
CONCLUSIONS
Brazil already meets many existing benchmarks for tobacco control policies.56 However, there have been no changes in cigarette minimum prices or specific excise tax rates since 2016.41 Substantial evidence indicates that high cigarette taxes indexed to adjust for inflation and rising incomes can reduce the affordability of cigarette packs and increase government revenue while benefiting public health.57–61 Implementing the 2012 flavor ban also has the potential for public health benefits but has yet to be realized.3 The data presented by this study reflect historical patterns, but future smoking trends will be shaped by policymakers’ willingness to take action and maintain Brazil’s status as a tobacco control leader on the global stage.
Supplementary Material
ACKNOWLEDGMENTS
This project was funded through National Cancer Institute (NCI) grants U01CA199284 and U01CA253858. The study sponsor had no role in the study design; collection, analysis, and interpretation of data; writing of the report; or the decision to submit the report for publication.
JT, DL, JJ, TH, and RM acknowledge support from National Cancer Institute grant U54CA229974.
No financial disclosures were reported by the authors of this paper.
This article is part of a supplement entitled Patterns of Birth Cohort-Specific Smoking Histories by Sociodemographic Group in the U.S., sponsored by the National Cancer Institute (Grants U01CA199284, U01CA253858, U54CA229974).
SUPPLEMENT NOTE
This article is part of a supplement entitled Patterns of Birth Cohort-Specific Smoking Histories by Sociodemographic Group in the U.S., which is sponsored by the National Cancer Institute (NCI) Grants U01CA199284 and U01CA253858. Authors also acknowledge support from NCI grant U54CA229974. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of NCI.
Footnotes
CREDIT AUTHOR STATEMENT
Jamie Tam: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing − original draft, Writing − review & editing. Mohammed A. Jaffri: Data curation, Investigation, Software, Writing − original draft, Writing − review & editing. Yoonseo Mok: Formal analysis, Investigation, Methodology, Software, Visualization, Writing − review & editing. Jihyoun Jeon: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing − review & editing. André S. Szklo: Conceptualization, Methodology, Investigation, Writing − review & editing. Mirian C. Souza: Conceptualization, Methodology, Investigation, Writing − review & editing. Theodore R. Holford: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Software, Writing − review & editing. David T. Levy: Conceptualization, Funding acquisition, Investigation, Writing − review & editing. Pianpian Cao: Methodology, Writing − review & editing. Luz M. Sánchez-Romero: Writing − review & editing. Rafael Meza: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Software, Supervision, Visualization, Writing − review & editing.
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2022.12.002.
REFERENCES
- 1.Portes LH, Machado CV, Turci SRB, Figueiredo VC, Cavalcante TM, Silva VLDCE. Tobacco Control Policies in Brazil: a 30-year assessment [A Política de Controle do Tabaco no Brasil: um balanç o de 30 anos]. Cien Saúde Colet. 2018;23(6):1837–1848. 10.1590/1413-81232018236.05202018. [DOI] [PubMed] [Google Scholar]
- 2.Lee K, Chagas LC, Novotny TE. Brazil and the framework convention on tobacco control: global health diplomacy as soft power. PLoS Med. 2010;7(4):e1000232. 10.1371/journal.pmed.1000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kyriakos CN, Fong GT, de Abreu Perez C, et al. Brazilian smokers are ready for the ban on flavour additives in tobacco to be implemented. Prev Med. 2022;160:107074. 10.1016/j.ypmed.2022.107074. [DOI] [PubMed] [Google Scholar]
- 4.Levy D, de Almeida LM, Szklo A. The Brazil SimSmoke policy simulation model: the effect of strong tobacco control policies on smoking prevalence and smoking-attributable deaths in a middle income nation. PLoS Med. 2012;9(11):e1001336. 10.1371/journal.pmed.1001336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Szklo AS, Levy D, Souza MC, et al. Changes in cigarette consumption patterns among Brazilian smokers between 1989 and 2008. Cad Saude Publica. 2012;28(11):2211–2215. . [DOI] [PubMed] [Google Scholar]
- 6.Szklo AS, Yuan Z, Levy D. Update and extension of the Brazil SimSmoke model to estimate the health impact of cigarette smoking by pregnant women in Brazil. Cad Saude Publica. 2017;33(12): e00207416. . [DOI] [PubMed] [Google Scholar]
- 7.Monteiro CA, Cavalcante TM, Moura EC, Claro RM, Szwarcwald CL. Population-based evidence of a strong decline in the prevalence of smokers in Brazil (1989−2003). Bull World Health Organ. 2007;85 (7):527–534. 10.2471/blt.06.039073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malta DC, Gomes CS, Andrade FMD, et al. Tobacco use, cessation, secondhand smoke and exposure to media about tobacco in Brazil: results of the National Health survey 2013 and 2019. Rev Bras Epidemiol. 2021;24(suppl 2):e210006. 10.1590/1980-549720210006.supl.2. [DOI] [PubMed] [Google Scholar]
- 9.Institute for Health Metrics and Evaluation (IHME). Compare GBD. Seattle, WA: IHME, University of Washington. https://vizhub.healthdata.org/gbd-compare/. Published October 15, 2020. Accessed July 19, 2022. [Google Scholar]
- 10.Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional de Saúde do Escolar 2012. Rio de Janeiro, Brazil: Instituto Brasileiro de Geografia e Estatística (IBGE); 2013. https://www.ibge.gov.br/en/statistics/social/education/16837-national-survey-of-school-health-editions.html?edicao=19298&t=resultados. Accessed July 20, 2022 [Google Scholar]
- 11.Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional de Saúdedo Escolar 2015. Rio de Janeiro, Brazil: Instituto Brasileiro de Geografia e Estatística (IBGE); 2016. https://www.ibge.gov.br/en/statistics/social/education/16837-national-survey-of-school-health-editions.html?edicao=16842&t=resultados. Accessed July 20, 2022 [Google Scholar]
- 12.Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional de Saúdedo Escolar 2019. Rio de Janeiro, Brazil: Instituto Brasileiro de Geografia e Estatística (IBGE); 2021. https://www.ibge.gov.br/en/statis-tics/social/education/16837-national-survey-of-school-health-editions.html?edicao=31649&t=resultados. Accessed July 20, 2022 [Google Scholar]
- 13.PeNSE - Pesquisa nacional de Saude do escolar. Instituto Brasileiro de Geografiae Estatística (IBGE). https://www.ibge.gov.br/en/statistics/social/health/16837-national-survey-of-school-health-editions.html?=&t=resultados. Accessed July 20, 2022.
- 14.Szklo AS, Cavalcante TM. Noncompliance with the law prohibiting the sale of cigarettes to minors in Brazil: an inconvenient truth. J Bras Pneumol. 2018;44(5):398–404. 10.1590/S1806-37562017000000359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Szklo AS, de Almeida LM, Figueiredo VC, et al. A snapshot of the striking decrease in cigarette smoking prevalence in Brazil between 1989 and 2008. Prev Med. 2012;54(2):162–167. 10.1016/j.ypmed.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Souza LE, Rasella D, Barros R, Lisboa E, Malta D, McKee M. Smoking prevalence and economic crisis in Brazil. Rev Saude Publica. 2021;55 (3). 10.11606/s1518-8787.2021055002768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maia EG, Stopa SR, de Oliveira Santos R, Claro RM. Trends in prevalence of cigarette smoking in Brazil: 2006−2019. Am J Public Health. 2021;111(4):730–738. 10.2105/AJPH.2020.306102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Malta DC, Flor LS, Machado ÍE, et al. Trends in prevalence and mortality burden attributable to smoking, Brazil and federated units, 1990 and 2017. Popul Health Metr. 2020;18(suppl 1):24. 10.1186/s12963-020-00215-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Szklo AS, de Souza MC, Szklo M, de Almeida LM. Smokers in Brazil: who are they? Tob Control. 2016;25(5):564–570. 10.1136/tobaccocontrol-2015-052324. [DOI] [PubMed] [Google Scholar]
- 20.Tammemägi MC, Katki HA, Hocking WG, et al. Selection criteria for lung-cancer screening [published correction appears in N Engl J Med. 2013;369(4):394]. N Engl J Med. 2013;368(8):728–736. 10.1056/NEJMoa1211776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chang JT, Meza R, Levy DT, Arenberg D, Jeon J. Prediction of COPD risk accounting for time-varying smoking exposures. PLoS One. 2021;16(3):e0248535. 10.1371/journal.pone.0248535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.IBGE, Pesquisa nacional de Saúde2019: percepção do estado de saúde, estilos de vida, doenças crônicas e Saúdebucal [National health survey 2019: perception of health status, lifestyles, chronic diseases and oral health], IBGE, 2020, 113. https://biblioteca.ibge.gov.br/index.php/biblioteca-catalogo?view=detalhes&id=2101764. Accessed July 25, 2022. [Google Scholar]
- 23.da Saúde Ministério, de Vigilância em Saúde Secretaria, Departamento de Análise em Saúdee Vigilância de Doenças não Transmissíveis, Brasília Brasil V.: da Saúde Ministério. 2020; 2019: vigilância de fatores de risco e proteção para doenç as crônicas por inquérito telefônico: estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteçãopara doenç as crônicas nas capitais dos 26 estados brasileiros e no Distrito Federal [2019: Surveillance of risk and protective factors for chronic diseases by telephone survey: estimates on the frequency and sociodemographic distribution of risk and protective factors for chronic diseases in the capitals of the 26 Brazilian states and the Federal District]. https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/publicacoes-svs/vigitel/vigitel-brasil-2019-vigilancia-fatores-risco.pdf/view. Accessed August 30, 2022.
- 24.Holford TR, Levy DT, McKay LA, et al. Patterns of birth cohort-specific smoking histories, 1965−2009. Am J Prev Med. 2014;46(2):e31–e37. 10.1016/j.amepre.2013.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jeon J, Holford TR, Levy DT, et al. Smoking and lung cancer mortality in the United States from 2015 to 2065: a Comparative Modeling Approach. Ann Intern Med. 2018;169(10):684–693. 10.7326/M18-1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holford TR, Meza R, Warner KE, et al. Tobacco control and the reduction in smoking-related premature deaths in the United States, 1964−2012. JAMA. 2014;311(2):164–171. 10.1001/jama.2013.285112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tam J, Jeon J, Thrasher JF, et al. Estimated prevalence of smoking and smoking-attributable mortality associated with graphic health warnings on cigarette packages in the U.S. from 2022 to 2100. JAMA Health Forum. 2021;2(9):e212852. 10.1001/jamahealthforum.2021.2852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tam J, Levy DT, Jeon J, et al. Projecting the effects of tobacco control policies in the USA through microsimulation: a study protocol. BMJ Open. 2018;8(3):e019169. 10.1136/bmjopen-2017-019169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meza R, Cao P, Jeon J, et al. Impact of joint lung cancer screening and cessation interventions under the new recommendations of the U.S. Preventive Services Task Force. J Thorac Oncol. 2022;17(1):160–166. 10.1016/j.jtho.2021.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Apelberg BJ, Feirman SP, Salazar E, et al. Potential public health effects of reducing nicotine levels in cigarettes in the United States. N Engl J Med. 2018;378(18):1725–1733. 10.1056/NEJMsr1714617. [DOI] [PubMed] [Google Scholar]
- 31.Souza Júnior PRB, Szwarcwald CL, Almeida WDS, et al. Comparison of sampling designs from the two editions of the Brazilian National Health Survey, 2013 and 2019. Cad Saúde Publ. 2022;38(suppl 1): e00164321. 10.1590/0102-311X00164321. [DOI] [PubMed] [Google Scholar]
- 32.Instituto Nacional de Câncer (Brasil). Global adult tobacco survey - Brazil 2008. Rio de Janeiro, Brazil: Instituto Nacional de Câncer; https://www.paho.org/hq/dmdocuments/2010/GATS-2010-Brazil-Report-en.pdf. Published 2010. Accessed November 21, 2022. [Google Scholar]
- 33.Enes CC, Nucci LB. A telephone surveillance system for noncommunicable diseases in Brazil. Public Health Rep. 2019;134(4):324–327. 10.1177/0033354919848741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holford TR, Levy DT, Meza R. Comparison of smoking history patterns among African American and white cohorts in the United States born 1890 to 1990. Nicotine Tob Res. 2016;18(suppl 1):S16–S29. 10.1093/ntr/ntv274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; https://www.R-project.org/. Published April 24, 2020. Accessed August 5, 2022. [Google Scholar]
- 36.Szklo AS, Cavalcante TM, Reis NBD, Souza MC. Tobacco denormalization at home”: the contribution of the smoking ban in enclosed workplaces in Brazil. Cad Saude Publica. 2022;38(suppl 1):e00107421. 10.1590/0102-31100107421. [DOI] [PubMed] [Google Scholar]
- 37.Szklo AS, Iglesias RM. Interferência da indústria do tabaco sobre os dados do consumo de cigarro no Brasil [Interference by the tobacco industry in data on cigarette consumption in Brazil]. Cad Saude Publica. 2020;36(12):e00175420. 10.1590/0102-311X00175420. [DOI] [PubMed] [Google Scholar]
- 38.Szklo AS, Iglesias RM. Decrease in the proportion of illicit cigarette use in Brazil: what does it really mean? Tob Control. 2020;29 (suppl 4):s287–s288. 10.1136/tobaccocontrol-2018-054846. [DOI] [PubMed] [Google Scholar]
- 39.IBGE. Pesquisa nacional de Saúde. 2013: percepção do estado de saúde, estilos de vida e doenç as crônicas [National Health Survey. 2013: perception of health status, lifestyles and chronic diseases]. IBGE; 2014. https://biblioteca.ibge.gov.br/index.php/biblioteca-cata-logo?view=detalhes&id=291110. Accessed October 18, 2022 [Google Scholar]
- 40.Szklo A, Iglesias RM, Carvalho de Souza M, Szklo M, Maria de Almeida L. Trends in illicit cigarette use in Brazil estimated from legal sales, 2012−2016. Am J Public Health. 2018;108(2):265–269. 10.2105/AJPH.2017.304117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tobacconomics, National Cancer Institute of Brazil, World Health Organization. Cigarette Tax Policy in Brazil: Recent Trends, Current Challenges, and Ways Forward. Tobacconomics Policy Note. Health Policy Center, Institute for Health Research and Policy, University of Illinois at Chicago; 2021. https://tobacconomics.org/research/ciga-rette-tax-policy-in-brazil/. Accessed July 20, 2022 [Google Scholar]
- 42.Iglesias RM, Szklo AS, Souza MC, de Almeida LM. Estimating the size of illicit tobacco consumption in Brazil: findings from the global adult tobacco survey. Tob Control. 2017;26(1):53–59. 10.1136/tobaccocontrol-2015-052465. [DOI] [PubMed] [Google Scholar]
- 43.Sóñora G, Reynales-Shigematsu LM, Barnoya J, Llorente B, Szklo AS, Thrasher JF. Achievements, challenges, priorities and needs to address the current tobacco epidemic in Latin America. Tob Control. 2022;31(2):138–141. 10.1136/tobaccocontrol-2021-057007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bertoni N, Cavalcante TM, Souza MC, Szklo AS. Prevalence of electronic nicotine delivery systems and waterpipe use in Brazil: where are we going? Rev Bras Epidemiol. 2021;24(suppl 2):e210007. 10.1590/1980-549720210007.supl.2. [DOI] [PubMed] [Google Scholar]
- 45.National health interview survey. Centers for Disease Control and Prevention (CDC). 2022. https://www.cdc.gov/nchs/nhis/index.htm. [Google Scholar]
- 46.Tam J, Levy DT, Feuer EJ, Jeon J, Holford TR, Meza R. Using the past to understand the future of U.S. and global smoking disparities: a birth cohort perspective. Am J Prev Med. 2023;64(4S):S1–S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jeon J, Cao P, Fleischer NL, et al. Birth cohort-specific smoking patterns by family income in the U.S. Am J Prev Med. 2023; 64(4S1):S32–S41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cao P, Jeon J, Tam J, et al. Smoking disparities by level of educational attainment and birth cohort in the U.S. Am J Prev Med. 2023;64(4S1): S22–S31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Meza R, Cao P, Jeon J, et al. Patterns of birth cohort-specific smoking histories by race and ethnicity in the U.S. Am J Prev Med. 2023; 64(4S1):S11–S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Holford TR, McKay L, Jeon J, et al. Smoking histories by state in the U.S. Am J Prev Med. 2023;64(4S1):S42–S52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carvalho de Souza M, Giunta DH, Szklo AS, Almeida LM, Szklo M. The tobacco epidemic curve in Brazil: where are we going? Cancer Epidemiol. 2020;67:101736. 10.1016/j.canep.2020.101736. [DOI] [PubMed] [Google Scholar]
- 52.Divino JA, Ehrl P, Candido O, Valadao MAP. Extended cost-benefit analysis of tobacco taxation in Brazil. Tob Control. 2022;31(suppl 2): s74–s79. 10.1136/tobaccocontrol-2021-056806. [DOI] [PubMed] [Google Scholar]
- 53.Divino JA, Ehrl P, Candido O, Valadao MAP. Effects of the Brazilian tax reform plans on the tobacco market. Tob Control. 2022;31(suppl 2):s65–s73. 10.1136/tobaccocontrol-2021-056822. [DOI] [PubMed] [Google Scholar]
- 54.Steffens C, Pereda P. Dynamic effects of smoking bans on addictive behavior among young adults. SSRN Journal. 2022. Preprint. Online February 28. 10.2139/ssrn.4027079. [DOI] [Google Scholar]
- 55.Data & methods. International Agency for Research on Cancer (IARC), Cancer Today. https://gco.iarc.fr/today/data-sources-methods. Accessed July 20, 2022.
- 56.Tobacco control policies. tobaccocontrollaws.org. https://www.tobac-cocontrollaws.org/legislation/factsheet/policy_status/brazil. Updated September 17, 2019. Accessed July 25, 2022.
- 57.Blecher E, Bouw A, Goodchild M, et al. WHO technical manual on tobacco tax policy and administration. Geneva, Switzerland: WHO. https://www.who.int/publications/i/item/9789240019188. Published April 12, 2021. Accessed July 26, 2022. [Google Scholar]
- 58.WHO. Health taxes: a primer. Geneva, Switzerland: WHO. https://apps.who.int/iris/rest/bitstreams/1259486/retrieve. Published 2019. Accessed September 30, 2022. [Google Scholar]
- 59.The economics of tobacco and tobacco control. U.S. National Cancer Institute tobacco control monograph 21. Bethesda, MD: National Cancer Institute. https://cancercontrol.cancer.gov/brp/tcrb/monographs/monograph-21. Published 2016. Accessed July 21, 2022. [Google Scholar]
- 60.Marquez PV, Moreno-Dodson B. Tobacco tax reform at the crossroads of health and development: a multisectoral perspective. Washington, DC: World Bank Group, 2017. Published. 10.1596/28494. [DOI] [Google Scholar]
- 61.WHO. WHO report on the global tobacco epidemic, 2015: raising taxes on tobacco. Geneva, Switzerland: WHO. https://apps.who.int/iris/handle/10665/178574. Published 2015. Accessed July 21, 2022. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.