Take Home Message
Day-case surgery can help the English National Health Service achieve net-zero carbon emissions. The change in the proportion of transurethral resection of bladder tumour procedures performed as day cases between 2013–2014 and 2021–2022 is estimated to have saved enough carbon to power 2716 homes for 1 yr.
Keywords: Urology, Transurethral resection of bladder tumour, Day case, Carbon footprint, Sustainable health care
Abstract
Background
The National Health Service (NHS) in England has set a net-zero target for carbon emissions by 2040. Increasing use of day-case surgery pathways may help in meeting this target.
Objective
To investigate the estimated difference in carbon footprint between day-case and inpatient transurethral resection of bladder tumour (TURBT) surgery in England.
Design, setting, and participants
This was a retrospective analysis of administrative data extracted from the Hospital Episode Statistics database for all TURBT procedures conducted in England from April 1, 2013 to March 31, 2022.
Outcome measurements and statistical analysis
Day-case and inpatient TURBT procedures were identified and the carbon footprint for key elements of the surgical pathway was estimated using data from Greener NHS and the Sustainable Healthcare Coalition.
Results and limitations
Of 209 269 TURBT procedures identified, 41 583 (20%) were classified as day-case surgery. The day-case rate increased from 13% in 2013–2014 to 31% in 2021–2022. The move from inpatient stays to day-case surgery between 2013–2014 and 2021–2022 demonstrates a trend toward a lower-carbon pathway, with an estimated saving of 2.9 million kg CO2 equivalents (equivalent to powering 2716 homes for 1 yr) in comparison to no change in practice. We calculated that potential carbon savings for the financial year 2021–2022 would be 217 599 kg CO2 equivalents (equivalent to powering 198 homes for 1 yr) if all hospitals in England not already in the upper quartile were able to achieve the current upper-quartile day-case rate. Our study is limited in that estimates are based on carbon factors for generic surgical pathways.
Conclusions
Our study highlights potential NHS carbon savings that could be achieved by moving from inpatient stays to day-case surgery. Reducing variation in care across the NHS and encouraging all hospitals to adopt day-case surgeries, where clinically appropriate, would lead to further carbon savings.
Patient summary
In this study we estimated the potential for carbon savings if patient undergoing bladder tumour surgery were admitted and discharged on the same day. We estimate that increasing use of day-case surgery between 2013–2014 and 2021–2022 has saved 2.9 million kg CO2 equivalents. If all hospitals were to achieve day case-rates comparable to those in the highest quarter of hospitals in England in 2021–2022, then the carbon equivalent to powering 198 homes for 1 year could have been saved.
1. Introduction
Climate change is one of the greatest health threats of the 21st century, and we are already seeing the effects of the climate emergency in the UK. Extreme weather events such as heatwaves, floods, and storms are increasing in intensity [1]. Together with deaths from air pollution, these events account for 1 in 20 deaths in the UK [2]. In addition to these direct effects on health, extreme weather events will impact our ability to deliver health care [3].
Health care is a contributor to climate change. Globally, the health care sector is responsible for almost 5% of carbon emissions [4] The UK National Health Service (NHS) has a significant carbon footprint that accounts for 4.6% of all UK emissions [5], [6].
In the Delivering a ‘Net Zero’ National Health Service report published in October 2022 [5], NHS England committed to delivering the world’s first net-zero health service by 2040. This report provided a target for reaching net-zero carbon for emissions that the NHS controls directly by 2040, and by 2045 for those it can influence, such as its supply chain. Through work on carbon hotspots such as anaesthetic gases and asthma inhalers, NHS estates and facilities, and travel and transport over 1 yr (2020–2021), the NHS reduced its emissions by 1.26 megatons of CO2 equivalents (CO2e), which would power 1.1 million homes with electricity for 1 yr [5]. However, to achieve the long-term goal of a net-zero health care system, more environmentally sustainable models of care need to be designed and delivered. Initiatives such as boosting “out-of-hospital” care, empowering patients to have more control over their health, digitally enabled care, and delivering streamlined efficient care pathways that minimise unnecessary travel, waste, and duplication are a key part of achieving net-zero status [5], [7], [8], [9].
Understanding the carbon impact of models of care in detail is a key step to implementing lower-carbon pathways and helps in identifying pockets of good practice. In England, improving clinical care by spreading best practice falls within the remit of the Getting it Right First Time (GIRFT) programme. GIRFT has a remit to reduce unwarranted variation in health care provision across the NHS in England that negatively impacts patient outcomes or service efficiency. For the urology specialty, the 2018 GIRFT national report identified that day-case rates for transurethral resection of bladder tumour (TURBT) varied substantially across NHS trusts and recommended that day-case surgery rates be increased to the level of the best-performing providers [10], and there is evidence that this is happening [11], [12]. Increasing the provision of day-case surgery, where clinically appropriate, has potential for reducing the carbon footprint of that care pathway by removing the need for high-resource, carbon-intensive inpatient hospital stays [6].
The aim of this study was to estimate the difference in carbon footprint between day-case and inpatient TURBT, estimate the amount of carbon saved by changes in day-case TURBT rates over the last decade, and estimate the potential further carbon reductions for TURBT procedures if all trusts achieved the day-case rates of NHS trusts in the upper quartile.
2. Patients and methods
2.1. Study design
This was a retrospective analysis of administrative data from the Hospital Episode Statistics (HES) database for England. The HES database is collected by NHS Digital and includes data for all NHS hospital activity in England. This includes patients admitted to non-NHS hospitals but funded by the NHS.
2.2. Ethics
The presentation of data follows current NHS Digital guidance for use of HES data for research purposes [13]. Consent from individuals involved in this study was not required for analysis of this administrative data set.
2.3. Data collection
The data presented here are for TURBT procedures performed during the period from April 1, 2013 to March 31, 2022 (inclusive). The period was chosen to be recent enough to reflect current practice but long enough to allow investigation of temporal trends. TURBT procedures were identified by extracting all data for which the main specialty code was listed as “urology services” or the treatment function code was “urology services” or “paediatric urology services” and the first listed procedure during the hospital spell was TURBT (Office of Populations Censuses and Surveys Classification of Interventions and Procedures version 4 [OPCS-4] code M421, in the absence of code Y082). Data were extracted at a spell level and no patients were excluded on the basis of age.
Data were then extracted for these procedures in relation to the NHS trust providing the care, date of admission, date of operation, date of discharge, age, sex, Index of Multiple Deprivation (IMD) score, and Hospital Frailty Risk Score (HFRS) [14]. IMD scores were categorised into quintiles on the basis of national percentiles for lower super output areas in England [15]. HFRS values were categorised as none, mild, moderate, and severe frailty on the basis of established cutoffs [14]. Follow-up data were available from the HES database for emergency return to hospital within 30 d of hospital discharge.
2.4. Quantifying the carbon footprint
We assessed the difference in carbon footprint between day-case and inpatient TURBT procedures. The carbon footprint of day-case and inpatient TURBT procedures was calculated using Sustainable Healthcare Coalition (SHC) carbon footprint data [16]. SHC data estimate the carbon footprint of an “average” surgical procedure as 35.1 kg CO2e [17]. This figure is a generic estimate and includes items covering consumables, equipment, medical gases, staff travel, energy, water use, and waste; it was used in this study as a proxy for the carbon footprint for TURBT. More detailed data specific to TURBT are not yet available. The same carbon factor was applied to day-case and inpatient procedures. The average carbon footprint of a low-intensity inpatient bed day was estimated as 37.9 kg CO2e [18]. For postprocedural emergency readmissions within 30 d, the carbon footprint was estimated as 13.8 kgCO2e for an emergency department attendance [19] and 126.0 kg CO2e for a short emergency inpatient stay [19]. The emergency attendance figure was used when there was no overnight stay and both figures summed when the patient was admitted. The methodology used to derive these estimates has been published [16], [17], [18], [19].
We only considered the carbon footprint of the operative TURBT procedure, immediate postoperative stay, and emergency readmissions as, these are likely to be the key points of difference between a day-case and inpatient TURBT pathway. The pathway activities that are likely to be constant (ie, those unlikely to change whether on a day-case or inpatient pathway) such as preoperative pathway components (eg, outpatient appointment, diagnostics [flexible cystoscopy and imaging]) and postoperative follow-up were therefore not considered.
2.5. Data management and statistical analysis
All data were analysed on a secure server controlled by NHS England using standard statistical software: Microsoft Excel (Microsoft Corp., Redmond, WA, USA), Stata (Stata Corp. LLC, College Station, TX, USA), and Alteryx (Alteryx Inc., Irvine, CA, USA). The data were summarised using standard descriptive statistics, depending on the data level. Carbon factors were calculated at a patient level and then aggregated for day-case and overnight-stay patients and per financial year, as appropriate. Total carbon saved was calculated using 2013–2014 as a baseline. To provide context, CO2e emissions were converted to CO2e to power an average UK home with electricity for 1 yr using a conversion factor of 1098.9 kg CO2e per home per year [20], [21].
Day-case rates for each hospital trust were adjusted for demographic factors using multivariable logistic regression modelling. The models were adjusted for age, sex, IMD quintile, and HFRS category. Age was modelled as a continuous variable (there was no evidence of nonlinearity in the relationship between the log odds of day-case surgery and age) and sex, IMD quintile, and HFRS category as categorical variables as described above. Adjusted day-case rates were derived using the margins command in Stata. Marginal values were calculated by adding hospital trust to the model as a fixed effect and holding its value constant across all cases and then repeating this for all trusts. This allowed estimation of adjusted day-case rates based on the sample distribution of all the covariates within the model.
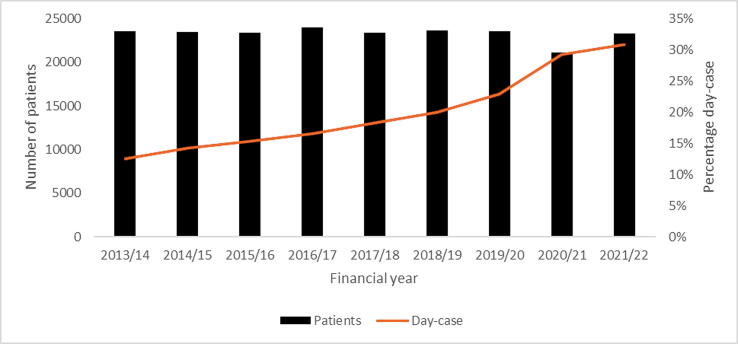
3. Results
Data were available for 209 269 patients undergoing TURBT during the study period, of which 41 583 (20%) were day cases. The demographic characteristics of the patients are shown in Table 1. Day-case patients were younger and less frail than inpatients. The day-case rate increased from 13% in 2013–2014 to 23% in 2019–2020, the last pre-COVID-19 year (Fig. 1). By 2021–2022, activity levels had broadly returned to prepandemic levels, but with a large increase in the day-case rate to 31%.
Table 1.
Characteristics of and outcomes for patients with and without an overnight stay for a transurethral resection of bladder tumour procedure
| Day cases | Inpatient cases | |
|---|---|---|
| Patients, n (%) | 41 583 (20) | 167 686 (80) |
| Age group, n (%) | ||
| <50 yr | 2633 (6.3) | 5057 (3) |
| 50–59 yr | 5032 (12) | 12 427 (7) |
| 60–69 yr | 10487 (25) | 33 895 (20) |
| 70–79 yr | 15522 (37) | 61 721 (37) |
| ≥80 yr | 7909 (19) | 54 586 (33) |
| Female, n (%) | 10 804 (26) | 36 817 (22) |
| HFRS category, n (%) | ||
| None | 25 194 (61) | 79 093 (47) |
| Mild | 12 056 (29) | 57 039 (34) |
| Moderate | 3987 (9.6) | 27 616 (17) |
| Severe | 346 (0.82) | 3938 (2.3) |
| IMD quintile, n (%) | ||
| 1 (most deprived) | 6298 (15) | 28 965 (17) |
| 2 | 7626 (19) | 31 014 (19) |
| 3 | 8966 (22) | 34 845 (21) |
| 4 | 9134 (22) | 36 560 (22) |
| 5 (least deprived) | 9206 (22) | 34 716 (21) |
| Emergency readmission within 30 d, n (%)a | 2599 (6.3) | 15 339 (9.1) |
| Median length of stay, d (IQR) | 0 | 1 (1–2) |
HFRS = Hospital Frailty Risk Score; IMD = Index of Multiple Deprivation; IQR = interquartile range.
Emergency readmissions were only recorded when there was an overnight stay
Fig. 1.
Patient numbers and rates of day-case surgery across the 9-yr study period.
For the treatment pathway components studied, the change in carbon footprint for all TURBT procedures conducted for each year is summarised in Table 2. From 2013–2014 to 2021–2022, the increase in day-case surgery reduced the carbon footprint of TURBT by 24 kg CO2e per patient. The estimated cumulative saving across the study period from the baseline of 2013–2014 was approximately 2.9 million kg CO2e (2.9 kilotons; Table 2). This is equivalent to powering 2716 UK homes with electricity for 1 yr.
Table 2.
Carbon footprint per patient per year
| Financial year | Patients (n) | Day-case rate (%) | MCF per patient for items included in the calculation (kg CO2) | Estimated CCS (kg CO2)a |
|---|---|---|---|---|
| 2013–2014 | 23 521 | 13 | 116.4 | – |
| 2014–2015 | 23 454 | 14 | 111.8 | −115 687 |
| 2015–2016 | 23 407 | 15 | 109.3 | −179 459 |
| 2016–2017 | 23 946 | 17 | 106.6 | −185 200 |
| 2017–2018 | 23 341 | 18 | 105.1 | −284 705 |
| 2018–2019 | 23 659 | 20 | 101.9 | −326 992 |
| 2019–2020 | 23 545 | 23 | 100.1 | −380 990 |
| 2020–2021 | 21 144 | 29 | 91.0 | −813 740 |
| 2021–2022 | 23 252 | 31 | 92.4 | −589 359 |
| Total | 209 269 | – | – | −2 876 132 |
CCS = cumulative carbon saving; MCF = mean carbon footprint.
Estimated CCS based on the rounded estimates for the MCF per patient in comparison to 2013–2014.
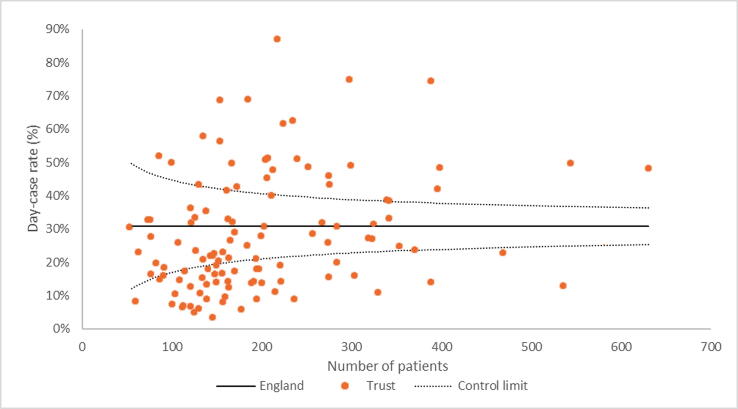
The model-adjusted day-case rates for 2021–2022 for NHS hospital trusts performing more than 50 TURBT procedures during the year are summarised in Figure 2. There was substantial variation in adjusted day-case rates across the 116 trusts included. The highest day-case rate was 87% and 13 trusts had day-case rates above 50%. The lowest day-case rate was 3.5% and 14 trusts had a day-case rate below 10%.
Fig. 2.
Funnel plot of adjusted day-case rate for the financial year 2021–2022 for all trusts conducting transurethral resection of bladder tumour procedures for more than 50 patients.
For the financial year 2021–2022, the average carbon footprint was 41.5 kg CO2e for a pathway involving day-case surgery and 115.0 kg CO2e for a pathway with inpatient surgery. The adjusted upper-quartile value was 39% day-case surgery. If all 87 trusts below the upper-quartile for the day-case surgery rate had met this target, the total carbon saving would be 217 599 kg CO2e (equivalent to powering 198 homes for 1 yr). The adjusted upper-decile value was 51% day-case surgery. If all 104 trusts below the upper-decile for the day-case surgery rate had met this target, the total carbon saving would be 372 127 kg CO2e (equivalent to powering 339 UK homes with electricity for 1 yr). The 30-d emergency readmission (with an overnight stay) rate was 6.4% for the 29 trusts in the upper quartile for day-case rates and 6.5% for the trusts in the lower three quartiles. These rates were 6.3% for the top decile and 6.5% for the lower nine deciles.
4. Discussion
Day-case rates more than doubled over the 9-yr study period, with the majority of the increase arising from 2018–2019 onwards. Reassuringly, trusts with very high rates of day-case surgery have very similar 30-d emergency readmission rates to trusts with lower day-case rates. Although day-case surgery will not be suitable for all, our results support previous evidence that day-case surgery, as part of a streamlined best-practice procedure pathway, is safe for patients who do not have complicating underlying disease [11].
Our findings highlight that comparisons of different ways of delivering care can identify carbon-saving opportunities. Further carbon savings could be made by reducing variation between hospitals in day-case delivery. Minimising hospital stays while maintaining levels of care and patient outcomes is one way to reduce carbon emissions, and there is evidence that day-case and outpatient surgery is as safe and effective as inpatient surgery for many procedures across a range of specialties [11], [22], [23], [24], [25].
However, the estimated emissions reductions associated with a day-case pathway will not be enough to achieve net-zero status. More detailed analysis of existing and alternative treatment pathways will be needed to support the net-zero goal. Research on the carbon footprint of surgical care pathways has predominantly focused on in-theatre carbon emissions, a known carbon hotspot in surgery [26]. A recent study attributed 42% of the carbon footprint of surgical care to anaesthetic gases and 23% to the surgical procedure itself. However, 29% of the carbon footprint was from inpatient bed-days and 5.5% from patient travel [27]. Our study considers aspects of the wider patient pathway and could be extended to include preoperative and postoperative outpatient and primary care contacts and travel. In this context, initiatives such as one-stop haematuria clinics, virtual appointments (where appropriate), patient-initiated follow-up, and the promotion of patient self-management in a way that improves health and negates the need for complex acute care could also help in reducing carbon emissions.
In the case of bladder tumour management, emerging treatments such as transurethral laser ablation (TULA), which can be performed as an outpatient procedure under local anaesthetic, may be part of the solution [28]. Anaesthetic gases make up 2% of the overall NHS carbon footprint and are one of the key carbon hotspots of surgery [5]. Innovative models of care that build on moves to day-case or outpatient surgery (such as TULA) could reduce anaesthetic gas emissions via the use of safe, low-carbon alternatives such as spinal/regional anaesthesia or local anaesthetic where appropriate. Likewise, alternative management options should be considered as a way to decarbonise bladder tumour pathways. For non–muscle-invasive bladder cancer, flexible cystoscopy and tumour ablation can offer a safe and less resource-intensive treatment option for selected cases, depending on patient and tumour factors [29]. For carefully selected patients there could even be a role for active surveillance [30]. More broadly, the role of preventative programmes in reducing the need for surgery should also be evaluated.
Although our study did not seek to identify possible causes of the increase in day-case surgery observed over the study period, there are a number of possible drivers for the changes seen. These include increasing recognition that day-case TURBT is technically feasible and safe in a high proportion of patients [11] and increasing use of bipolar technology (although in many circumstances good intraoperative haemostasis with monopolar energy can also facilitate safe day-case TURBT). The GIRFT programme now advocates day-case TURBT by default on the basis that this provides a more efficient pathway that decreases inpatient bed pressures and allows patients to recover at home. Promotion of day-case surgery in England by GIRFT and other stakeholders will also have driven some of the changes seen.
In England, the GIRFT High Volume Low Complexity (HVLC) programme is seen as a key element in the recovery of elective surgical services following the COVID-19 pandemic [31]. The programme focuses on addressing the large proportion of patients waiting for noncomplex surgery to free up other services to manage patients on more complex surgery pathways. To achieve this, the GIRFT-HVLC programme is driving efficiencies in six high-volume specialities via the establishment of dedicated GIRFT-HVLC surgical hubs and the adoption of best-practice procedure pathways and theatre efficiency principles. The GIRFT-HVLC programme offers an opportunity to design low-carbon pathways for future surgical care.
Carbon savings identified in this study should be viewed as savings per patient rather than an actual reduction in emissions at a system level. In the short term at least, bed capacity released by moving to a day-case surgery model will often be taken up by other patients rather than resulting in a reduction in carbon emissions because of reductions in hospital activity. Only at a point at which supply matches or exceeds demand will these particular carbon savings be realised.
4.1. Strengths and limitations
A strength of our study is that we had a large data set of all TURBT procedures conducted within an entire health care system over a number of years. Cases included in the data set should be representative of all patients undergoing TURBT in England, and will be broadly similar to patients seen in many countries with a similar health care model to England.
A key limitation of our work is that we did not investigate the entire surgical pathway, but just the key differences between day-case and overnight stay pathways. Our estimates should not be interpreted as the carbon footprint of the pathway. Some data entry inconsistencies have been noted in the HES data set, mostly with regard to differences in coding practice for procedures across different trusts [10]. However, there are likely to be fewer errors for high-volume procedures, such as TURBT, than for less common procedures, for which coders may be less familiar with how to record the episode. We also acknowledge that our estimates will only be as accurate as the carbon factors applied to each part of the pathway. The carbon factors used were for generic procedures and admissions and are not specific to TURBT. Thus, we were unable to differentiate between different surgical approaches to TURBT (eg, monopolar vs bipolar vs laser). Having reliable carbon-factor data for specific procedures and admission types will be an important next step if the work is to be expanded to other procedures and other parts of the surgical pathway. More broadly, as day-case TURBT rates increase, the occurrence of early emergency readmissions and other adverse events should be closely monitored to ensure that patient outcomes are not being compromised. Our findings and earlier research indicate that, so far, this is not the case [11].
5. Conclusions
We estimated that there has been a substantial reduction in the carbon footprint related to TURBT surgery in England as a result of the progressive increase in day-case rates. There appears to be scope to increase TURBT day-case rates in many trusts, which would help in improving efficiency and assisting the transition to net-zero health care.
Author contributions: William K. Gray had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Gray, van Hove, Briggs, Phull, McGrath, Begum.
Acquisition of data: Gray, Begum.
Analysis and interpretation of data: Gray, Begum, John, Phull, van Hove.
Drafting of the manuscript: Gray, Begum, John, Phull, van Hove.
Critical revision of the manuscript for important intellectual content: Gray, Begum, John, Phull, van Hove, Briggs, O’Flynn.
Statistical analysis: Gray, Begum.
Obtaining funding: None.
Administrative, technical, or material support: Gray.
Supervision: O’Flynn, McGrath.
Other: None.
Financial disclosures: William K. Gray certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor: None.
Acknowledgments: We acknowledge NHS Digital for permission to use their data in this report. The GIRFT programme is providing a framework for examining contemporary clinical practice in unprecedented detail and breadth. We also thank all staff within individual NHS trusts who collected and entered the data used in this study.
Ethics considerations: Ethical approval was not sought for the study because it did not directly involve human participants. Informed consent was not sought for the study because it was an analysis of routine clinical data. The study was completed in accordance with the Helsinki Declaration as revised in 2013.
Data sharing statement: This report does not contain identifiable patient data. Data in this report are anonymised. The underlying HES data cannot be made available directly by the authors as the data were obtained under licence/a data sharing agreement from NHS Digital. HES data are available from NHS Digital on application.
Associate Editor: M. Carmen Mir
Statistical Editor: Melissa Assell
References
- 1.Pörtner H-O, Roberts DC, Tignor M, et al, editors. Climate change 2022: impacts, adaptation and vulnerability. Working Group II contribution to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK: Cambridge University Press; 2022. https://report.ipcc.ch/ar6/wg2/IPCC_AR6_WGII_FullReport.pdf.
- 2.Public Health England. Public Health England publishes air pollution evidence review. London, UK: Public Health England; 2019. https://www.gov.uk/government/news/public-health-england-publishes-air-pollution-evidence-review.
- 3.Romanello M., Di Napoli C., Drummond P., et al. The 2022 report of the Lancet Countdown on health and climate change: health at the mercy of fossil fuels. Lancet. 2022;400:1619–1654. doi: 10.1016/S0140-6736(22)01540-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Health Care Without Harm. Health care climate footprint report. Brussels, Belgium: Health Care Without Harm Europe; 2022. https://noharm-europe.org/ClimateFootprintReport.
- 5.Greener NHS. Delivering a ‘net zero’ NHS. London, UK: NHS England; 2022. https://www.england.nhs.uk/greenernhs/a-net-zero-nhs/.
- 6.Tennison I., Roschnik S., Ashby B., et al. Health care’s response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health. 2021;5:e84–e92. doi: 10.1016/S2542-5196(20)30271-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sustainable Healthcare Coalition. Guidance and tools. London, UK: Sustainable Healthcare Coalition; 2022. https://shcoalition.org/download-area/.
- 8.MacNeill A.J., McGain F., Sherman J.D. Planetary health care: a framework for sustainable health systems. Lancet Planet Health. 2021;5:e66–e68. doi: 10.1016/S2542-5196(21)00005-X. [DOI] [PubMed] [Google Scholar]
- 9.Rizan C., Reed M., Mortimer F., Jones A., Stancliffe R., Bhutta M.F. Using surgical sustainability principles to improve planetary health and optimise surgical services following the COVID-19 pandemic. Bull R Coll Surg Engl. 2020;102:177–181. [Google Scholar]
- 10.Harrison S. Urology: GIRFT programme national specialty report. London, UK: GIRFT; 2018. https://gettingitrightfirsttime.co.uk/wp-content/uploads/2018/07/Urology-June18-M.pdf.
- 11.Gray W.K., Day J., Briggs T.W.R., Harrison S. Transurethral resection of bladder tumour as day-case surgery: evidence of effectiveness from the UK Getting it Right First Time (GIRFT) programme. J Clin Urol. 2020;13:221–227. [Google Scholar]
- 12.Gray W.K., Day J., Briggs T.W.R., Harrison S. To what extent have key recommendations from the Getting It Right First Time programme for urology in England been implemented? J Clin Urol. 2022;15:96–102. doi: 10.1177/20514158211010651. [DOI] [Google Scholar]
- 13.Digital N.H.S. NHS Digital; London, UK: 2018. Hospital Episode Statistics (HES) analysis guide. [Google Scholar]
- 14.Gilbert T., Neuburger J., Kraindler J., et al. Development and validation of a hospital frailty risk score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet. 2018;391:1775–1782. doi: 10.1016/S0140-6736(18)30668-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Office for National Statistics. Lower layer Super Output Area population estimates. London, UK: ONS; 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/lowersuperoutputareamidyearpopulationestimates.
- 16.Coalition for Sustainable Pharmaceuticals and Medical Devices. Care pathways: guidance on appraising sustainability, main document. Newton Abbot, UK: Sustainable Healthcare Coalition; 2015. https://shcoalition.org/wp-content/uploads/2019/10/Sustainable-Care-Pathways-Guidance-Main-Document-Oct-2015.pdf.
- 17.Coalition for Sustainable Pharmaceuticals and Medical Devices. Care pathways: guidance on appraising sustainability, surgical procedure module. Newton Abbot, UK: Sustainable Healthcare Coalition; 2015. https://shcoalition.org/wp-content/uploads/2019/10/Sustainable-Care-Pathways-Guidance-Surgical-Procedure-Module-Oct-2015.pdf.
- 18.Coalition for Sustainable Pharmaceuticals and Medical Devices. Care pathways: guidance on appraising sustainability, inpatient bed day module. Newton Abbot, UK: Sustainable Healthcare Coalition; 2015. https://shcoalition.org/wp-content/uploads/2019/10/Sustainable-Care-Pathways-Guidance-Inpatient-Bed-Day-Module-Oct-2015.pdf.
- 19.Coalition for Sustainable Pharmaceuticals and Medical Devices. Care pathways: guidance on appraising sustainability, emergency department visit module. Newton Abbot, UK: Sustainable Healthcare Coalition; 2015. https://shcoalition.org/wp-content/uploads/2019/10/6_3.-Sustainable-Care-Pathways-Guidance-Emergency-Department-Visit-Module-Oct-2015.pdf.
- 20.Department for Business Energy & Industrial Strategy. National statistics. Energy consumption in the UK 2020. London, UK: UK Government; 2020. https://www.gov.uk/government/statistics/energy-consumption-in-the-uk-2020.
- 21.Department for Energy Security and Net Zero, Department for Business Energy & Industrial Strategy. Research and analysis. Greenhouse gas reporting: conversion factors 20London, UK: UK Government; 2022. https://www.gov.uk/government/publications/greenhouse-gas-reporting-conversion-factors-2021.
- 22.Gray W.K., Takhar A.S., Navaratnam A.V., et al. Safety of day-case paediatric tonsillectomy in England: an analysis of administrative data for the Getting It Right First Time programme. Anaesthesia. 2022;77:277–285. doi: 10.1111/anae.15562. [DOI] [PubMed] [Google Scholar]
- 23.Duignan M., Lao C., Lawrenson R., Wood A.J. A policy of day-case sinonasal surgery is safe, well tolerated and cost-effective. J Laryngol Otol. 2021;135:341–343. doi: 10.1017/S0022215121000803. [DOI] [PubMed] [Google Scholar]
- 24.Oker N., Dupuch V., Herman P., et al. Outcomes of endoscopic ethmoidectomy performed on a day-case basis: a prospective bi-centric study. Eur Arch Otorhinolaryngol. 2017;274:305–310. doi: 10.1007/s00405-016-4263-3. [DOI] [PubMed] [Google Scholar]
- 25.Gray WK, Day J, Briggs TWR, Hutton M. Safety of same-day discharge posterior lumbar decompression and/or discectomy: an observational study using administrative data from England. Global Spine J. In press. 10.1177/21925682221131764. [DOI] [PMC free article] [PubMed]
- 26.MacNeill A.J., Lillywhite R., Brown C.J. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health. 2017;1:e381–e388. doi: 10.1016/S2542-5196(17)30162-6. [DOI] [PubMed] [Google Scholar]
- 27.Whiting A., Tennison I., Roschnik S., Collins M. Surgery and the NHS carbon footprint. Bull R Coll Surg Engl. 2020;102:182–185. [Google Scholar]
- 28.Malde S., Grover S., Raj S., et al. A Systematic Review of the Efficacy and Safety of Outpatient Bladder Tumour Ablation. Eur Urol Focus. 2022;8:141–151. doi: 10.1016/j.euf.2021.01.019. [DOI] [PubMed] [Google Scholar]
- 29.Herr H.W., Donat S.M., Reuter V.E. Management of low grade papillary bladder tumors. J Urol. 2007;178:1201–1205. doi: 10.1016/j.juro.2007.05.148. [DOI] [PubMed] [Google Scholar]
- 30.Petrelli F., Giannatempo P., Maccagnano C., Contieri R., Hurle R. Active surveillance for non-muscle invasive bladder cancer: a systematic review and pooled-analysis. Cancer Treat Res Commun. 2021;27 doi: 10.1016/j.ctarc.2021.100369. [DOI] [PubMed] [Google Scholar]
- 31.Getting It Right First Time programme. High volume, low complexity (HVLC) surgery. London, UK: GIRFT; 2022. https://gettingitrightfirsttime.co.uk/hvlc/hvlc-programme/.