Abstract
Study Design
Systematic Review
Objectives
To conduct a meta-analysis on the survivorship of commonly performed cervical spine procedures to develop survival function curves for (i) second surgery at any cervical level, and (ii) adjacent level surgery.
Methods
A systematic review of was conducted following PRISMA guidelines. Articles with cohorts of greater than 20 patients followed for a minimum of 36 months and with available survival data were included. Procedures included were anterior cervical discectomy and fusion (ACDF), cervical disc arthroplasty (ADR), laminoplasty (LAMP), and posterior laminectomy and fusion (PDIF). Reconstructed individual patient data were pooled across studies using parametric Bayesian survival meta-regression.
Results
Of 1829 initial titles, 16 citations were included for analysis. 73 811 patients were included in the second surgery analysis and 2858 patients in the adjacent level surgery analysis. We fit a Log normal accelerated failure time model to the second surgery data and a Gompertz proportional hazards model to the adjacent level surgery data. Relative to ACDF, the risk of second surgery was higher with ADR and PDIF with acceleration factors 1.73 (95% CrI: 1.04, 2.80) and 1.35 (95% CrI: 1.25, 1.46) respectively. Relative to ACDF, the risk of second surgery was lower with LAMP with deceleration factor .06 (95% CrI: .05, .07). ADR decreased the risk of adjacent level surgery with hazard ratio .43 (95% CrI: .33, .55).
Conclusions
In cases of clinical equipoise between fusion procedures, our analysis suggests superior survivorship with anterior procedures. For all procedures, laminoplasty demonstrated superior survivorship.
Keywords: degenerative cervical myelopathy, anterior cervical discectomy and fusion, cervical disc arthroplasty, survivorship curve
Introduction
Approximately 150 000 American adults undergo cervical spine surgery each year.1,2 This represents a significant financial burden, with direct hospital costs ranging between $5000 and $30 000 depending on procedure and jurisdiction. 3 As cervical spine surgery utilization has increased 206% between 1992 and 2005,4,5 these procedures represent a prime target to optimize value in spine care. 6
An estimated 30-50% of adults will experience neck pain in any given year, 7 and 50-80% of these individuals will go on to develop chronic symptoms. 8 Though conservative care is the mainstay of treatment, 9 surgery does have a role in the treatment of cervical radiculopathy, 10 cervical myelopathy, 11 and cervical deformity. 11 However, there is significant variability in surgical approaches to the cervical spine, particularly in cervical myelopathy, where in approximately 50% of cases surgeons feel that there is equipoise in the surgical approach (anterior, posterior, vs both), number of levels to decompress, need for fusion, and need for fixation. 12
Given that surgeons regard a variety of surgeries as equivalent in many cases, other factors should be considered in decision-making. Durability of the chosen procedure is 1 such consideration. It is important to note that while the rate of primary cervical surgeries is increasing, rates of revision procedures are accelerating at a faster rate. 13 Revision procedures are more expensive, 14 carry a greater risk of complications, 15 and are less durable than primary procedures. 16 Granular data on future probabilities of revision surgery in treatment discussions could enhance patient counselling by surgeons. 17 Previously published systematic reviews and meta-analysis have been limited to risk factors for revision rather than actual probabilities of revision.18,19
In this paper we conduct the first meta-analysis of survival probabilities for commonly performed cervical spine procedures. We compute summary survival curves for (i) second surgery at the index level, and (ii) adjacent level surgery, which will allow surgeons to calculate the probability of revision surgery at any time-point of interest.
Methods
A systematic review was conducted in accordance with the Cochrane Prognosis Methods Group as well as the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA). 20 An electronic librarian-assisted search of Ovid MEDLINE, Ovid EMBASE, and CENTRAL from inception to February 22 2021 (Appendix 1) was performed. A validated DCM search filter with 100% sensitivity in MEDLINE was utilized and adapted for EMBASE.21,22 The highly sensitive Irvin filter, modified for occurrence of an event rather than death, was combined with the DCM filter to restrict results to DCM prognostic studies in MEDLINE and EMBASE.23,24 CENTRAL was searched using the strategy used in the Cochrane review for DCM treatment without the requirement for surgical treatment. 25 Reference lists of included papers were screened for additional manuscripts to ensure search completion.
Eligibility Criteria and Screening
Eligible studies included those written in English language with record of survivorship analysis for adult patients with degenerative cervical pathology treated with primary (not revision) surgery. We considered second surgery (at any cervical level, Analysis 1) and adjacent level surgery (Analysis 2) as survival endpoints. Both randomized controlled and cohort studies were eligible for inclusion. We required that a cohort of at least 20 patients be followed for at least 36 months. We required that survival be reported for at least 2 homogenous treatment group: (i) anterior cervical discectomy and fusion (ACDF), (ii) artificial disc replacement (ADR), (iii) laminoplasty (LAMP), or (iv) laminectomy and fusion, ie posterior decompression and instrumented fusion (PDIF). We required that studies report at least 2 groups to avoid bias introduced by single-arm studies. 26 We excluded cohorts focusing on a special population alone (eg smokers, patients on dialysis, or concomitant deformity) or cohorts undergoing a combination of procedures.
All titles and abstracts were independently screened for eligibility by 2 reviewers using the online platform Covidence (Melbourne, Australia). All discrepancies were resolved by consensus amongst authors. Duplicate articles were manually excluded. Two reviewers independently reviewed the full text of all studies identified by title and abstract screening to determine final eligibility.
Data Extraction and Quality Assessment
Two reviewers independently extracted study data using the CHARMS checklist and assessed the risk of bias using the QUIPS tool modified for overall prognosis studies. 27 All discrepancies were resolved by consensus amongst authors. A standardized electronic data collection form was used. Our primary outcome was probability of treatment failure reported with a survival curve.
Images of survival curves were saved from included studies and survival probabilities were extracted from survival curves using the computer program WebPlotDigitizer. 28
Statistical Analysis
We used the Guyot algorithm to simulate the individual patient data from published survival curves using the statistical programming language R.29,30 With the simulated individual patient data, we pooled survival curves across studies using a fixed effects approach of individual patient data meta-analysis. A parametric survival curve was fit to the pooled data using the framework outlined by Ishak et al. 31 We considered exponential, Weibull, Gompertz, Log-logistic, and Log-normal probability density functions in the model building exercise. Poorly fitting probability density functions were excluded using graphical exploratory analysis. Next, the probability density function with the lowest Akaike information criterion (AIC) and adequate fit of the pooled survival curve was used for further analysis.
Data from survival curves were used in a Bayesian meta-analysis using the statistical programming language R and the Bayesian modelling language Stan using the best fitting probability density function.30,32 Non-informative prior distributions were used. 33 Bayesian analysis was implemented using previously described techniques for meta-analysis. 34 We included treatment group as a categorical variable, and therefore only considered treatment group for which at least 2 survival curves were available. We assessed for heterogeneity through visual inspection of the published survival curves in relation to each other.
Results
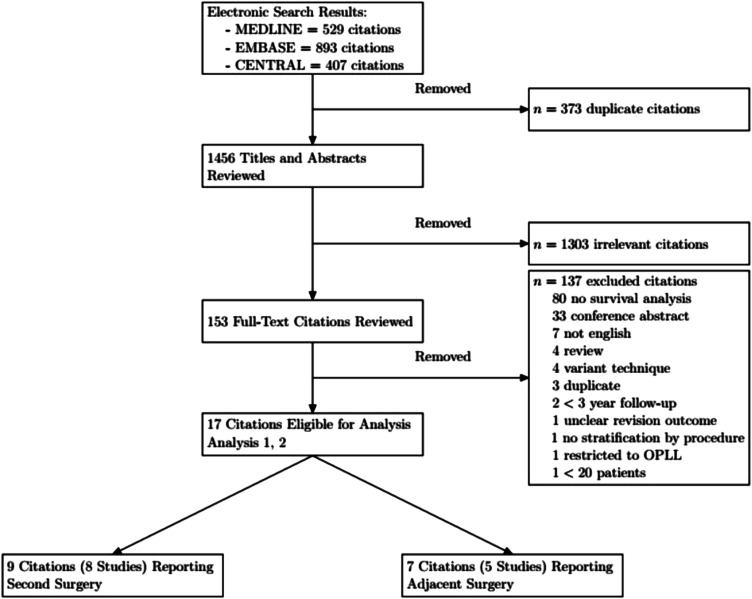
1829 studies were identified, and after excluding duplicates, 1456 remained. Through title and abstract screening, 1303 citations were excluded, resulting in 153 full-text citations for review. 137 citations were excluded yielding 16 citations that were included in our analysis (Figure 1).35‐40 For second surgery, 2 citations reported on the same dataset, therefore we considered 8 unique studies. 41‐49 For adjacent level surgery, 2 sets of citations reported on the same dataset, therefore we considered 5 unique studies.50‐56
Figure 1.
Study flow diagram.
For Analysis #1 (second surgery), the included studies were published between 2009 and 2020. For Analysis #2 (adjacent level surgery), the included studies were published between 2011 and 2019. Important study design and demographic characteristics are outlined in Table 1.
Table 1.
Characteristics of Studies Included in Second Surgery Analysis.
| Study | Study Design | Inclusion Criteria | Exclusion Criteria | Sponsor | Definition of Second Surgery | Arm | Sample Size | Technical Details | Age (mean and standard deviation unless otherwise stated) | Sex | NDI reported |
|---|---|---|---|---|---|---|---|---|---|---|---|
| NCT00578812 Phillips et al 41 | RCT | Single level degenerative disc disease with radiculopathy or myelopathy only affecting either levels C3-4 or C7-T1 | Trauma, prior fusion, 2 or more levels affected, tumor, osteoporosis, daily insulin, etc. | NuVasive | Any revision, removal, reoperation, or supplemental fixation | ACDF | 265 | Single level ACDF with allograft and plate | 43.9 range 22-73 | 46.0% male | Yes |
| ADR | 276 | PCM Cervical Disc | 43.3 range 25-72 | 46.4% male | Yes | ||||||
| ISRCTN44347115 Macdowall et al 42 | RCT | Patient 25-60yo with cervical radiculopathy (arm pain) for at least 3 months and correlating MRI findings in 1 or 2 levels | Previous surgery, >2 levels requiring treatment, severe facet arthropathy, myelopathy, etc. | Stockholm County Council, DePuy Synthes Spine, Uppsala County Council, Swedish Society of Spinal Surgeons | Not stated | ACDF | 70 | ACDF with autogenous iliac crest graft and plate | 47.0 ± 6.9 | 47.1% male | Yes |
| ADR | 81 | Discover ADR | 46.7 ± 6.7 | 50.6% male | Yes | ||||||
| Lin et al. 2015 43 | Retrospective cohort | Adult patients undergoing ACDF or laminoplasty diagnosed with multiple level cervical degenerative disease. From 2001 to 2011, query of Taiwan National Health Insurance Research Database (NHIRD), using diagnostic codes. Large national database including 99% of population according to paper. |
Single level disease, tumor, any who had both procedures. | Not reported | Defined as another ACDF or laminoplasty within 1 year (short term) or more than 1 year (long term) after the index | ACDF | 6605 | Not reported | 55.17 ± 14.18 | 65.42% male | No |
| Laminoplasty | 1578 | Not reported | 59.01 ± 14.05 | 66.29% male | No | ||||||
| Park et al. 201644,45 | Retrospective cohort | CSM or radiculopathy diagnoses treated with ACDF, corpectomy, posterior fusion, laminoplasty. Performed using diagnostic code search on national level HIRA database. | Trauma, tumor, infectious spondylitis, inflammatory spondylitis of gout, rheumatoid arthritis, ankylosing spondylitis, ossification of posterior longitudinal ligament | Hallym University Research Fund 2014 (HURF-2014-28) | Any cervical reoperation excluding third and subsequent reoperation events | ACDF | 8143 | Not reported | 51.44 ± 10.80 (all intervenions reported together) | 61.29% male | No |
| Laminoplasty | 391 | Not reported | No | ||||||||
| Laminectomy and Fusion | 537 | Not reported | No | ||||||||
| Puvanesarajah 2017 46 | Retrospective Cohort | ICD-9 diagnostic code database query for cervical spondylosis with myelopathy, subsequent query for surgical interventions of interest. Utilized fee-for-service patient database, PearlDiver Patient Records Database, which contains records for Medicare beneficiaries from 2005 to 2012. | Combined anterior posterior, revision, OC fusion, trauma, tumor, etc | No funding received | Revision surgery codes were searched in database including implant removal, revision fusion, incision and drainage, exploration, and hardware removal. | ACDF | 34 867 | 1 to 2 level ACDF | Not reported | 48.2% male (<65 years) 52.6% male (65-84 years) |
No |
| Laminectomy and Fusion | 16 167 | Not reported | Not reported | 57.8% 1-2 level PCF <65yrs 59.7% 1-2 PCF 65-84yrs 57.7% >3 level PCF <65yrs 56% >3 level PCF 65-84yrs |
No | ||||||
| Hashimoto et al. 2018 47 | Prospective cohort | Cervical myelopathy with radiographic compression between C2-C7, data source from national-level registry focusing on Miyagi prefecture in Japan since 1988. | Not stated | No funding | Analysis only included reoperation for ‘neurological complications.’ Though analyzed, Kaplan-Meier curve excluded revision for surgical site infection | Laminoplasty | 4208 | Midline splitting (French door) laminoplasty using hydroxyapatite spacer in split laminae and cross-multiplied non-absorbable threads are used to stabilize the laminae | 62 ± 11 | 68.75% male | No |
| Nakashima et al. 2020 49 | Retrospective case series | Adults with clinical myelopathy with either CSM or OPLL on MRI or CT, all who underwent laminoplasty. Unspecified surgical database searched from 2003-2016. | Revision, infection, tumor, or trauma | Nagoya Spine Group research funds | Surgeries for late-onset myelopathy, paralysis, or severe radicular pain (6 months after laminoplasty) Reoperation for infection, epidural hematoma, or C5 palsy conducted immediately after surgery (<6 months after surgery) |
Laminoplasty | 623 | Open door laminoplasty with gap bridged by local or artificial bone strut | Not reported | Not reported | No |
Analysis #1 considered 2 randomized controlled trials,41,42 3 large database studies,43‐46 and 2 single-center retrospective cohort studies.47‐49 At least 2 studies reported data for ACDF, ADR, LAMP, and PDIF. Overall, 49 950 patients underwent anterior cervical discectomy and fusion (ACDF), 357 underwent artificial disc replacement (ADR), 6800 laminoplasty, and 16 704 posterior laminectomy and instrumented fusion. One study limited patients to a diagnosis of radiculopathy, 42 2 included patients with either radiculopathy or myelopathy,41,44 3 included only patients with myelopathy,46,47,49 and 1 did not specify the clinical diagnosis, stating only that patients had multilevel cervical degenerative disease. 43 2 studies, both of which were RCTs comparing ACDF to ADR, included only single level disease.41,42 Two studies, both large database studies not including ADR, excluded single level disease, including only multi-level surgery.43,44 The remainder of studies in our second surgery analysis did not specify the number of operative levels.
Analysis #2 considered 4 randomized controlled trials,50‐54 and 1 single-center retrospective cohort study.55,56 Only 1 study reported survival curves for LAMP and PDIF, 55 therefore Analysis #2 only considered ACDF and ADR. The ADR data from Lee et al was excluded because hybrid ACDF-ADRs were included in their data. 55 All of these studies directly compared ACDF to ADR. Overall, 1710 patients underwent ACDF and 1148 patients underwent ADR. All studies included patients with either diagnoses of radiculopathy or myelopathy with radiographic evidence of degenerative disc disease. Two studies focused on single level degenerative disease51,52,54, 1 on 2 adjacent level disease, 53 and 1 on either single or 2 level disease. 50 One study did not restrict number of levels operated in the index procedure. 56
The QUIPS tool was used to assess bias in prognostic studies. All studies had an adequate description of baseline populations, recruitment strategy, and clearly stated inclusion and exclusion criteria and this is reported in Table 2. Table 1 outlines study sponsors as a source of funding, which was reported in all but 1 study. 43 All but 1 study included in our analysis of adjacent segment reoperation were industry sponsored. 55 Table 3 provides the full QUIPS score for each included study.
Table 2.
Risk of Bias Assessment for Included Studies.
| Study Author/ID | Study Participation | Study Attrition | Outcome Measurement | Statistical Analysis and Reporting | |
|---|---|---|---|---|---|
| Second surgery | |||||
| NCT0057881241 | L | L | L | L | |
| ISRCTN4434711542 | L | L | L | L | |
| Lin et al. 201543 | L | M | L | L | |
| Park et al. 201644,45 | L | L | L | L | |
| Puvanesarajah 201746 | M | L | L | L | |
| Hashimoto et al. 201847 | M | M | L | M | |
| Nakashima et al. 202059 | M | L | L | L | |
| Adjacent level surgery | |||||
| NCT0038959760 | L | L | L | L | |
| NCT0043719051,52 | M | L | L | L | |
| NCT0063715661 | L | L | L | L | |
| NCT0064287654 | L | L | L | L | |
| Lee et al. 201455,56 | L | L | L | L | |
L, low risk of bias; M, medium risk of bias, H, high risk of bias.
Table 3.
Characteristics of Studies Included in Adjacent Level Surgery Analysis.
| Study | Study Design | Inclusion Criteria | Exclusion Criteria | Sponsor | Definition of Adjacent Surgery | Arm | Sample Size | Technical Details | Age (mean and standard deviation unless otherwise stated) | Sex | NDI? | Reasons for adjacent surgery |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NCT00389597 50 |
RCT | Single or 2 level spondylosis with radiculopathy and/or myelopathy with levels involved C3-C7 | More than 2 levels, rigid segment, infection, osteoporosis, disc height <3mm, morbid obesity, Rheumatoid Arthritis, etc. | LDR Spine USA | Not reported | ACDF | 186 | ACDF with allograft and plate | 44.0 ± 8.2 1 level 46.2 ± 8.0 2 level |
44.4% male for 1-level, 57.1% male for 2-level | yes | Not fully reported, most common reason stated for both was “adjacent level disease or herniation” |
| ADR | 389 | Mobi-C ADR | 43.3 ± 9.2 1 level 45.3 ± 8.1 2 level |
47.6% male for 1-level, 50.2% male for 2-level | yes | |||||||
| NCT00437190 51,52 |
RCT | Single level degenerative disc disease with radiculopathy or myelopathy at levels between C3 and C7 | Deformity, diabetes requiring daily Insulin, morbid obesity, previous C-pine surgery, infection, steroid use. | Medtronic Spinal and Biologics | Surgery at adjacent level to index procedure | ACDF | 221 | Allograft Fusion and ATLANTIS™ Cervical Plate System | Not reported | Not reported | Yes | “Symptomatic adjacent level disease requiring surgery” |
| ADR | 242 | BRYAN Cervical Disc Prosthesis | Not reported | Not reported | Yes | “Symptomatic adjacent level disease requiring surgery” | ||||||
| NCT00637156 53 |
RCT | Intractable radiculopathy and/or myelopathy with degenerative disc disease at 2 adjacent cervical levels from C3-C7 | Other condition, smokers, pregnant patients, osteoporotic patients | Medtronic Spinal and Biologics | Any surgery at adjacent levels | ACDF | Historical Control from NCT00642876 5 | |||||
| ADR | 209 | PRESTIGE LP device at 2 adjacent levels | 47.1 (8.3) | 44.0% male | Yes | Not reported | ||||||
| NCT00642876 54 |
RCT | Single-level cervical disc disease and at least 1 additional confirmatory neuroradiographic study, such as MRI or CT-enhanced myelography that showed findings consistent with clinical findings | -Cervical spinal conditions other than single-level symptomatic degenerative disc disease or evidence of instability. -Symptomatic disc disease at level C2–3 or C7–T1, a history of discitis, or a medical condition that required medication, such as steroids or nonsteroidal anti-inflammatory medications that could interfere with fusion. |
Medtronic Spinal and Biologics | Any secondary surgery including revision at initial site that involved an adjacent level | ACDF | 265 | Allograft Fusion and ATLANTIS™ Cervical Plate System | 43.9 (22-73) | 46.0% male | Yes | Not reported |
| ADR | 276 | PRESTIGE® Cervical Disc | 43.3 (25-72) | 46.4% male | Yes | Not reported | ||||||
| Lee et al. 2014 55,56 | Retrospective series | Cervical spine surgery performed by the senior author (K.D.R.) for radiculopathy, myelopathy, or myeloradiculopathy between January 1999 and December 2010 | Contiguous or mixed OPLL, patients undergoing revision within 12 months. | Soonchunhyang University Research Fund (No. 20150000) | Any surgery at adjacent level | ACDF | 1038 | One level arthrodesis were performed on 353 patients; 2 levels on 374 patients; 3 levels on 228 patients; 4 levels on 70 patients; 5 levels on 12 patients; and 6 levels on 1 patient | 50 (22–89) | 49.5% male | No | New radiographically correlated symptoms at a segment adjacent to previous anterior arthrodesis minimum 1 year after the index operation |
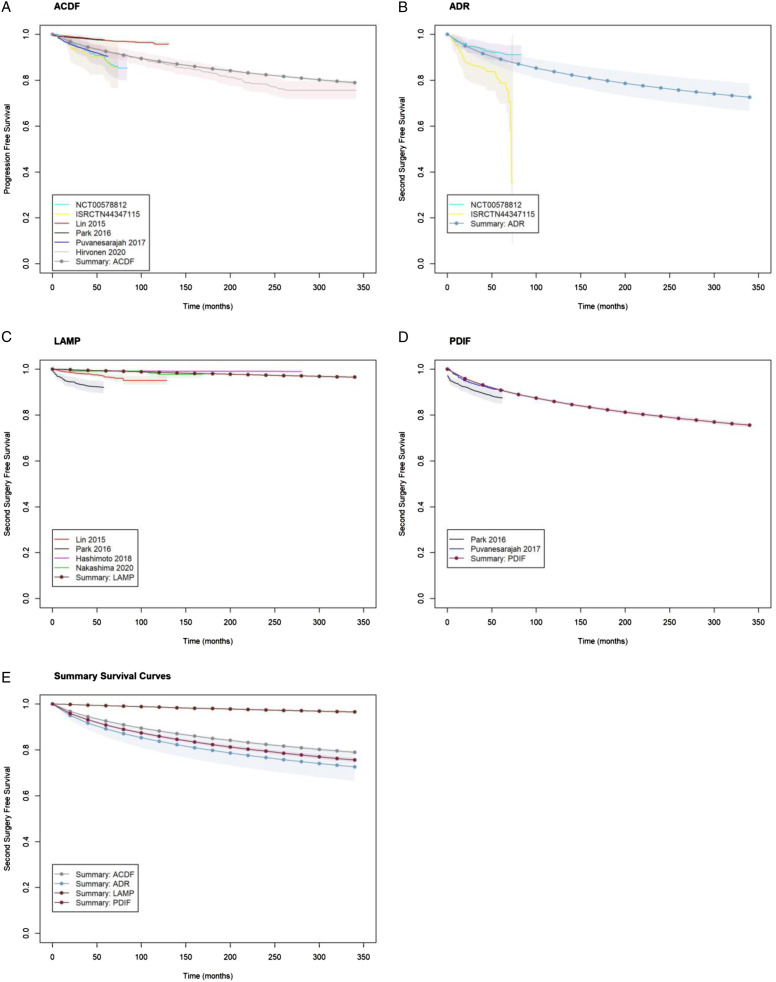
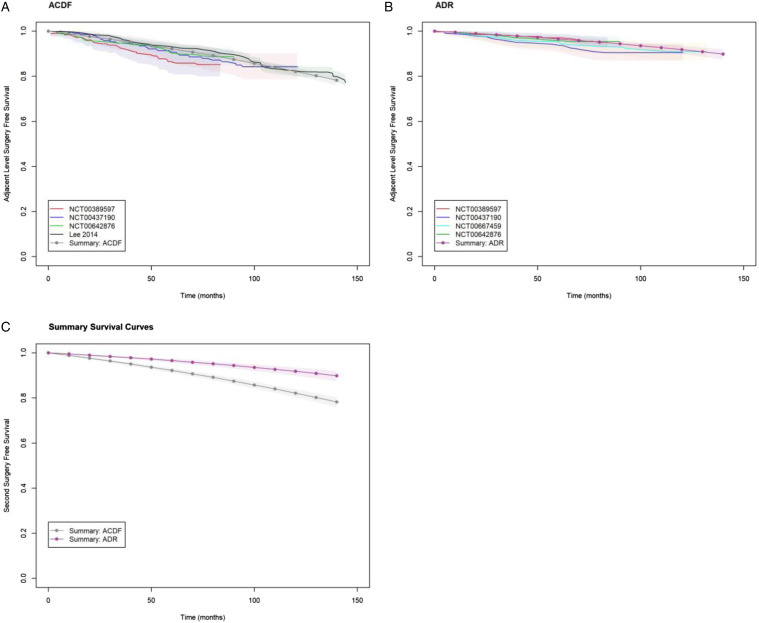
Individual study survival results for second surgery and adjacent level surgery are shown in Figures 2 and 3 respectively. In Analysis #1 (second surgery), we noted little heterogeneity in survival curves reported by studies on ACDF, LAMP and PDIF. There was substantial heterogeneity between the 2 studies on ADR.41,42 ISRCTN44347115 42 included patients undergoing 1 or two-level ADR, whereas NCT00578812 41 was restricted to single-level ADR. We also note ISRCTN44347115 42 recruited a smaller sample than NCT00578812 41 resulting in wide confidence intervals for the former which overlap with the latter. In Analysis #2 (adjacent level surgery), we noted consistent results between studies for ACDF and ADR.
Figure 2.
Individual study survival curves, and parametric summary survival curve for second surgery.
Figure 3.
Individual study survival curves, and parametric summary survival curve for adjacent level surgery.
Exploratory plots for the appropriate probability density function for the pooled Kaplan-Meier data are shown in Figure A1. The exponential, Weibull and Log-logistic distributions showed a lack of linearity at early and late times and thus poor for the pooled data. Based on AIC, the Gompertz model provided the best fit, and further supported by the similarity between observed and predicted survival probabilities shown in Figure A2.
The summary survival curve generated by the meta-analysis for second surgery (Analysis #1) is shown in Figure 2. The pooled second surgery free survival estimates for ACDF, ADR, LAMP and PDIF are shown in Table 4. Relative to ACDF, the risk of second surgery was higher with ADR and PDIF with acceleration factors 1.73 (95% CrI: 1.04, 2.80) and 1.35 (95% CrI: 1.25, 1.46) respectively. Relative to ACDF, the risk of second surgery was lower with LAMP with deceleration factor .06 (95% CrI: .05, .07). Despite statistically significant acceleration factors, survival estimates for ACDF, ADR and PDIF were not significantly different from each which indicates a lack of clinical significance (Table 3e).
Table 4.
Second Surgery Free Survival Estimates from Meta-Regression.
| Time (years) | ACDF | ADR | LAMP | PDIF |
|---|---|---|---|---|
| 1 | .98 (.98, .98) | .97 (.95, .98) | 1 (1, 1) | .97 (.97, .97) |
| 2 | .96 (.96, .96) | .94 (.92, .96) | 1 (1, 1) | .95 (.95, .96) |
| 3 | .95 (.95, .95) | .92 (.89, .95) | 1 (1, 1) | .94 (.93, .94) |
| 4 | .94 (.93, .94) | .91 (.87, .93) | .99 (.99, 1) | .92 (.92, .93) |
| 5 | .93 (.92, .93) | .89 (.86, .92) | .99 (.99, .99) | .91 (.9, .91) |
| 10 | .88 (.88, .89) | .84 (.79, .88) | .99 (.98, .99) | .86 (.85, .87) |
95% CrI in parentheses
The summary survival curve generated by the meta-analysis for adjacent level surgery (Analysis #2) is shown in Figure 3. The pooled adjacent level free survival estimates for ACDF and ADR are shown in Table 5. ADR decreased the risk of adjacent level surgery with hazard ratio .43 (95% CrI: .33, .55). Survival estimates for ADR were greater than those for ACDF at all time points (Figure 3C).
Table 5.
Adjacent-Level Surgery Free Survival Estimates from Meta-Regression.
| Time (years) | ACDF | ADR |
|---|---|---|
| 1 | .99 (.98, .99) | .99 (.99, 1) |
| 2 | .97 (.97, .98) | .99 (.98, .99) |
| 3 | .96 (.95, .96) | .98 (.98, .99) |
| 4 | .94 (.93, .95) | .97 (.97, .98) |
| 5 | .92 (.91, .93) | .97 (.96, .97) |
| 10 | .82 (.8, .84) | .92 (.9, .93) |
95% CrI in parentheses.
Discussion
This systematic review and meta-analysis is the first quantitative synthesis of published data on the long-term survivorship of the most commonly performed surgeries for degenerative cervical spine pathologies.
The parameteric summary survival curve for second surgery is shown in Figure 2 (log-normal) and for adjacent level surgery in Figure 3 (Gompertz). Our analysis shows a higher risk of second surgery for ADR and PDIF (acceleration factors 1.73 (95% CrI: 1.04, 2.80) and 1.35 (95% CrI: 1.25, 1.46) respectively), and a lower risk of second surgery for LAMP relative to ACDF (.06 (95% CrI: .05, .07)). The increased risk of second surgery for ADR and PDIF did not translate into significantly different survival probabilities suggesting a lack of clinical significance (Table 4). While our analysis showed that the risk of adjacent level surgery was lower for ADR relative ACDF with hazard ratio .43 (95% CrI: .33, .55).
Zhong et al. have published the only other meta-analysis on the risk of second surgery in ACDF vs ADR incorporating data from 12 RCTs. 56 They conducted a random-effects meta-analysis of pooled second surgery rates at various follow-up times. Notably 50% of studies only followed patients to 2 years. They found that the risk of second surgery was lower with ADR compared to ACDF (Risk Ratio .54 (95%CI: .36-.80). Zhong et al.’s findings differ from ours that ADR carries a higher risk of surgery with an acceleration factor 1.35 (95% CrI: 1.25, 1.46), albeit with no difference in actual survivorship (Figure 2E). This discrepancy stems from the fact that, in the Zhong et al. meta-analysis, the pooled second surgery rate for ACDF was 11.6% which contrasts with our findings of a 4% second surgery rate at 2-years (Table 4). It is interesting that second surgery rates for ADR are similar in our and Zhong et al.’s meta-analysis (6% and 6.1% respectively). There are several potential reasons for differences in estimates of in ACDF second surgery rates. First, 75% of studies in the Zhong meta-analysis were industry funded, whereas only 50% were industry- funded in our ACDF vs ADR comparisons for second surgery. Second, the majority of studies in the Zhong et al meta-analysis reported index and adjacent level surgery separately, and second surgery was simply calculated as the sum of both event rates. This approach assumes that second and index level surgery are mutually exclusive. Such an assumption will overestimate second surgery rates if patients undergo both an index and adjacent level surgery in the same second surgery. Third, Zhong et al. were not able to account for observation time and censoring in their analyses. Our meta-analysis of actual second surgery time-to-event data addresses the methodological limitations of the Zhong et al meta-analysis.
Our findings agree with previously published meta-analyses on the risk of adjacent-level surgery. Deng et al. conducted a meta-analysis on the risk of adjacent-level surgery in ACDF vs ADR with 8 randomized controlled trials. 19 Their finding that ADR carried a lower risk of adjacent level surgery at 4-5 years, 7 years, and 9-10 years of follow-up agree with our findings. Badhiwala et al. conducted a meta-analysis on the risk of adjacent level surgery ACDF vs ADR. 57 They included 11 RCTs reporting with follow-up to 2 years, 4 years, 5 years, or 7 years. They report 5-year adjacent level surgery free survival rates of 91.9 (95% CI: 88.9-94.1) and 97.1 (95% CI: 95.2-98.2) for ACDF and ADR respectively which closely agree with our estimates shown in Table 5.
Our study incorporates an important methodological advancements over Zhong et al.’s, Deng et al.’s and Bhadiwala et al.’s meta-analyses.18,19,57 The analytical approach used in these papers was restricted to fixed follow-up times. We instead digitized published survival curves and reconstructed individual patient data using recently developed algorithms. This is a less restrictive requirement and allowed us to include the totality of longitudinal data in 1 meta-analysis. This approach allowed us to include very large sample sizes in our paper: 73 811 patients for second surgery, and 2858 patients for adjacent level surgery and therefore confidence intervals around summary survival curves are relatively precise.
Several limitations are important to consider. First, we are unaware of any sample size calculations for survival meta-regression and therefore are unable to formally evaluate the power of our analysis. A commonly cited rule-of-thumb that linear regression requires 10 to 20 subjects per variable. 58 In Analysis #1 (second surgery), we used 3 variables (surgery as a categorical variable) with a minimum of 759 observations for the LAMP variable. In Analysis #2 (adjacent level surgery), we used 1 variable (surgery as a categorical variable) with a minimum of 357 observations for the ADR variable. Therefore, we feel our analysis is statistically viable. Second, inclusion/exclusion criteria were variable across studies. Some studies included patients with myelopathy, while this was an exclusion criterion in others. In particular, trials were restricted to 1 or 2 operative levels, while observational studies considered greater levels. Despite this methodological heterogeneity, we noted a low level of heterogeneity.
Lastly, we cannot report demographic homogeneity between groups. It is critical to note that the main purpose of this study is to produce individual survival curves for each of these procedures and that this is not a direct comparative study. Although the incidence of different pathologies is not specifically reported, we suspect that the 2 papers producing the bulk of the laminoplasty patients in our study contained more patients with OPLL, as this was not an exclusion criterion for them, and rates of OPLL are known to be higher in East Asia, with both papers focussing on a Japanese population. However, to our knowledge, there is no literature to suggest that OPLL is protective against reoperation. In fact, large cohorts such as those produced by Fujiwara et al. suggest higher rates of complication and reoperation in patients with OPLL compared to Cervical Spondylotic Myelopathy (CSM) 60 . Additionally, laminoplasty is usually preferred for multi-level disease, as opposed to single level disease 61 , thereby increasing surgical time, dissection, and presumably complications. If anything, these factors would bias our results against the survivorship of laminoplasty. Nevertheless, an important caveat of this study is demographic heterogeneity.
Our survival curves can aid patients and surgeons during the shared decision-making process. Parametric survival data can be used to more concretely discuss the risk of additional surgery when planning treatment. Furthermore, in cases of clinical equipoise between cervical procedures for a specific patient, our analysis can be used to include durability as a factor in the decision-making process.
Conclusion
Herein we present survival and reoperation curves for the most performed cervical spine procedures for myelopathy and radiculopathy. We incorporated all available long-term survival data from high-quality publications. We found no significant difference in adjacent segment surgery between ACDF and ADR. We found posterior laminectomy and fusion to have a significantly higher risk of secondary surgery when compared to ventral approaches or posterior laminoplasty. This allows a pragmatic patient-centred discussion regarding expectations and outcomes of surgery. Second, in cases of clinical equipoise between fusion procedures, particularly between single or 2 level ACDF and posterior laminectomy and fusion, our analysis suggests superior survivorship with the anterior procedure.
Supplemental Material
Supplemental Material for Long-Term Survivorship of Cervical Spine Procedures; A Survivorship Meta-Analysis and Meta-Regression by Mohamed Sarraj, Philip Hache, Farid Foroutan, Colby Oitment, Travis E. Marion, Daipayan Guha, and Markian Pahuta in Global Spine Journal
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Mohamed Sarraj https://orcid.org/0000-0002-3879-0445
Colby Oitment https://orcid.org/0000-0003-1351-9410
Markian Pahuta https://orcid.org/0000-0002-4808-5459
References
- 1.Liu CY, Zygourakis CC, Yoon S, et al. Trends in utilization and cost of cervical spine surgery using the national inpatient sample database, 2001 to 2013. Spine. 2017;42(15):E906-E913. doi: 10.1097/BRS.0000000000001999 [DOI] [PubMed] [Google Scholar]
- 2.Oglesby M, Fineberg SJ, Patel AA, Pelton MA, Singh K. Epidemiological trends in cervical spine surgery for degenerative diseases between 2002 and 2009. Spine. 2013;38(14):1226-1232. doi: 10.1097/BRS.0b013e31828be75d [DOI] [PubMed] [Google Scholar]
- 3.Alvin MD, Miller JA, Lubelski D, et al. Variations in cost calculations in spine surgery cost-effectiveness research. Neurosurgical focus. 2014;36(6):E1. doi: 10.3171/2014.3.FOCUS1447 [DOI] [PubMed] [Google Scholar]
- 4.Fehlings MG, Kwon BK, Tetreault LA. Guidelines for the management of degenerative cervical myelopathy and spinal cord injury: An introduction to a focus issue. Global Spine Journal. 2017;7(3_supplement):6S-7S. doi: 10.1177/2192568217701714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fehlings MG, Tetreault LA, Riew KD, et al. A clinical practice guideline for the management of patients with degenerative cervical myelopathy: Recommendations for patients with mild, moderate, and severe disease and nonmyelopathic patients with evidence of cord compression. Global Spine Journal. 2017;7(3_supplement):70S-83S. doi: 10.1177/2192568217701914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Safiri S, Kolahi AA, Hoy D, et al. Global, regional, and national burden of neck pain in the general population, 1990-2017: systematic analysis of the Global Burden of Disease Study 2017. BMJ (Clinical research ed). 2020;368:m791. doi: 10.1136/bmj.m791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hogg-Johnson S, van der Velde G, Carroll LJ, et al. The burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Journal of manipulative and physiological therapeutics. 2009;32(2 Suppl):S46-60. doi: 10.1016/j.jmpt.2008.11.010 [DOI] [PubMed] [Google Scholar]
- 8.Carroll LJ, Hogg-Johnson S, van der Velde G, et al. Course and prognostic factors for neck pain in the general population: Results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33(4 Suppl):S75-82. doi: 10.1097/BRS.0b013e31816445be [DOI] [PubMed] [Google Scholar]
- 9.Hurwitz EL, Carragee EJ, van der Velde G, et al. Treatment of neck pain: Noninvasive interventions: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33(4 Suppl):S123-S152. doi: 10.1097/BRS.0b013e3181644b1d [DOI] [PubMed] [Google Scholar]
- 10.Bono CM, Ghiselli G, Gilbert TJ, et al. An evidence-based clinical guideline for the diagnosis and treatment of cervical radiculopathy from degenerative disorders. The spine journal : official journal of the North American Spine Society. 2011;11(1):64-72. doi: 10.1016/j.spinee.2010.10.023 [DOI] [PubMed] [Google Scholar]
- 11.Fehlings MG, Tetreault LA, Riew KD, et al. A clinical practice guideline for the management of patients with degenerative cervical myelopathy: Recommendations for patients with mild, moderate, and severe disease and nonmyelopathic patients with evidence of cord compression. Global spine journal. 2017;7(3 Suppl):70S-83S. doi: 10.1177/2192568217701914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghogawala Z, Coumans JV, Benzel EC, Stabile LM, Barker FG. Ventral versus dorsal decompression for cervical spondylotic myelopathy: surgeons’ assessment of eligibility for randomization in a proposed randomized controlled trial: Results of a survey of the Cervical Spine Research Society. Spine. 2007;32(4):429-436. doi: 10.1097/01.brs.0000255068.94058.8a [DOI] [PubMed] [Google Scholar]
- 13.Rajaee SS, Kanim LEA, Bae HW. National trends in revision spinal fusion in the USA: Patient characteristics and complications. The bone & joint journal. 2014;96-B(6):807-816. doi: 10.1302/0301-620X.96B6.31149 [DOI] [PubMed] [Google Scholar]
- 14.Kim EJ, Chotai S, Wick JB, Stonko DP, Sivaganesan A, Devin CJ. Patient-Reported Outcomes and Costs Associated With Revision Surgery for Degenerative Cervical Spine Diseases. Spine. 2018;43(7):E423-E429. doi: 10.1097/BRS.0000000000002361 [DOI] [PubMed] [Google Scholar]
- 15.Neifert SN, Martini ML, Yuk F, et al. Predicting trends in cervical spinal surgery in the United States from 2020 to 2040. World neurosurgery. 2020;141:e175-e181. doi: 10.1016/j.wneu.2020.05.055 [DOI] [PubMed] [Google Scholar]
- 16.Xu R, Bydon M, Macki M, et al. Adjacent segment disease after anterior cervical discectomy and fusion: clinical outcomes after first repeat surgery versus second repeat surgery. Spine. 2014;39(2):120-126. doi: 10.1097/BRS.0000000000000074 [DOI] [PubMed] [Google Scholar]
- 17.Pahuta MA, Werier J, Wai EK, Patchell RA, Coyle D. A technique for approximating transition rates from published survival analyses. Cost Effectiveness and Resource Allocation. 2019;17(1). doi: 10.1186/s12962-019-0182-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhong ZM, Zhu SY, Zhuang JS, Wu Q, Chen JT. Reoperation after cervical disc arthroplasty versus anterior cervical discectomy and fusion: A meta-analysis. Clin Orthop Relat Res. 2016;474(5):1307-1316. doi: 10.1007/s11999-016-4707-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deng Y, Li G, Liu H, Hong Y, Meng Y. Mid- to long-term rates of symptomatic adjacent-level disease requiring surgery after cervical total disc replacement compared with anterior cervical discectomy and fusion: a meta-analysis of prospective randomized clinical trials. J Orthop Surg Res. 2020;15(1):468. doi: 10.1186/s13018-020-01957-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moons KG, Hooft L, Williams K, Hayden JA, Damen JA, Riley RD. Implementing systematic reviews of prognosis studies in Cochrane. The Cochrane database of systematic reviews. 2018;10:ED000129. doi: 10.1002/14651858.ED000129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davies BM, Goh S, Yi K, Kuhn I, Kotter MRN. Development and validation of a MEDLINE search filter/hedge for degenerative cervical myelopathy. BMC Medical Research Methodology. 2018;18(1):1-8. doi: 10.1186/s12874-018-0529-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pope DH, Davies BM, Mowforth OD, Bowden AR, Kotter MRN. Genetics of degenerative cervical myelopathy: A systematic review and meta-analysis of candidate gene studies. Journal of clinical medicine. 2020;9(1). doi: 10.3390/jcm9010282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boulos L, Ogilvie R, Hayden JA. Search methods for prognostic factor systematic reviews: A methodologic investigation. Journal of the Medical Library Association. 2021;109(1). doi: 10.5195/jmla.2021.939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riva JJ, Noor ST, Wang L, et al. Predictors of prolonged opioid use after initial prescription for acute musculoskeletal injuries in adults: A systematic review and meta-analysis of observational studies. Annals of internal medicine. 2020;173(9):721-729. doi: 10.7326/M19-3600 [DOI] [PubMed] [Google Scholar]
- 25.Nikolaidis I, Fouyas IP, Sandercock PA, Statham PF. Surgery for cervical radiculopathy or myelopathy. Cochrane Database of Systematic Reviews. Published online 2010. doi: 10.1002/14651858.cd001466.pub3 [DOI] [PMC free article] [PubMed]
- 26.Singh J, Abrams KR, Bujkiewicz S. Incorporating single-arm studies in meta-analysis of randomised controlled trials: a simulation study. BMC Med Res Methodol. 2021;21(1):114. doi: 10.1186/s12874-021-01301-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moons KGM, de Groot JAH, Bouwmeester W, et al. Critical appraisal and data extraction for systematic reviews of prediction modelling studies: The CHARMS checklist. PLoS Medicine. 2014;11(10):e1001744. doi: 10.1371/journal.pmed.1001744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rohatgi A. WebPlotDigitizer. Published online 2020.
- 29.Guyot P, Ades AE, Ouwens MJNM, Welton NJ. Enhanced secondary analysis of survival data: Reconstructing the data from published Kaplan-Meier survival curves. BMC Medical Research Methodology. 2012;12(1):9. doi: 10.1186/1471-2288-12-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.R Core Team . R: A language and environment for statistical computing. Published online 2018.
- 31.Ishak KJ, Kreif N, Benedict A, Muszbek N. Overview of parametric survival analysis for health-economic epplications. PharmacoEconomics. 2013;31(8):663-675. doi: 10.1007/s40273-013-0064-3 [DOI] [PubMed] [Google Scholar]
- 32.Stan Development Team . Stan: A C++ Library for probability and sampling, Version 2.2. Published online 2014.
- 33.Brilleman SL, Elci EM, Novik JB, Wolfe R. Bayesian survival analysis using the rstanarm R package. arXiv. Published online 2020.
- 34.Pahuta M, Smolders JM, van Susante JL, Peck J, Kim PR, Beaule PE. Blood metal ion levels are not a useful test for adverse reactions to metal debris: A systematic review and meta-analysis. Bone & joint research. 2016;5(9):379-386. doi: 10.1302/2046-3758.59.BJR-2016-0027.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kadaňka Z, Mareš M, Bednařík J, et al. Predictive factors for spondylotic cervical myelopathy treated conservatively or surgically. European Journal of Neurology. 2005;12(1):55-63. doi: 10.1111/j.1468-1331.2004.00896.x [DOI] [PubMed] [Google Scholar]
- 36.Sumi M, Miyamoto H, Suzuki T, Kaneyama S, Kanatani T, Uno K. Prospective cohort study of mild cervical spondylotic myelopathy without surgical treatment: Clinical article. Journal of Neurosurgery: Spine. 2012;16(1):8-14. doi: 10.3171/2011.8.SPINE11395 [DOI] [PubMed] [Google Scholar]
- 37.Oshima Y, Seichi A, Takeshita K, et al. Natural course and prognostic factors in patients with mild cervical spondylotic myelopathy with increased signal intensity on T2-weighted magnetic resonance imaging. Spine. 2012;37(22):1909-1913. doi: 10.1097/BRS.0b013e318259a65b [DOI] [PubMed] [Google Scholar]
- 38.Allam AFA, Abotakia TAA, Koptan W. Role of Cerebrolysin in cervical spondylotic myelopathy patients: a prospective randomized study. The spine journal: official journal of the North American Spine Society. 2018;18(7):1136-1142. doi: 10.1016/j.spinee.2017.11.002 [DOI] [PubMed] [Google Scholar]
- 39.Feng X, Hu Y, Ma X. Progression prediction of mild cervical spondylotic myelopathy by somatosensory-evoked potentials. Spine. 2020;45(10):E560-E567. doi: 10.1097/BRS.0000000000003348 [DOI] [PubMed] [Google Scholar]
- 40.Martin AR, Kalsi-Ryan S, Akbar MA, et al. Clinical outcomes of nonoperatively managed degenerative cervical myelopathy: An ambispective longitudinal cohort study in 117 patients. Journal of Neurosurgery: Spine. 2021;34(6):821-829. doi: 10.3171/2020.9.SPINE201395 [DOI] [PubMed] [Google Scholar]
- 41.Phillips FM, Geisler FH, Gilder KM, Reah C, Howell KM, McAfee PC. Long-term outcomes of the US FDA IDE prospective, randomized controlled clinical trial comparing PCM cervical disc arthroplasty with anterior cervical discectomy and Fusion. Spine. 2015;40(10):674-683. doi: 10.1097/BRS.0000000000000869 [DOI] [PubMed] [Google Scholar]
- 42.MacDowall A, Canto Moreira N, Marques C, et al. Artificial disc replacement versus fusion in patients with cervical degenerative disc disease and radiculopathy: A randomized controlled trial with 5-year outcomes. Journal of neurosurgery Spine. 2019;30(3):323-331. doi: 10.3171/2018.9.SPINE18659 [DOI] [PubMed] [Google Scholar]
- 43.Lin JH, Chien LN, Tsai WL, Chen LY, Hsieh YC, Chiang YH. Reoperation rates of anterior cervical discectomy and fusion versus posterior laminoplasty for multilevel cervical degenerative diseases: A population-based cohort study in Taiwan. The spine journal: official journal of the North American Spine Society 2016;16(12):1428-1436. doi: 10.1016/j.spinee.2016.08.017 [DOI] [PubMed] [Google Scholar]
- 44.Park MS, Ju YS, Moon SH, et al. Reoperation rates after surgery for degenerative cervical spine disease according to different surgical procedures: National population-based cohort study. Spine. 2016;41(19):1484-1492. doi: 10.1097/BRS.0000000000001581 [DOI] [PubMed] [Google Scholar]
- 45.Park MS, Ju YS, Moon SH, et al. Reoperation Rates After Anterior Cervical Discectomy and Fusion for Cervical Spondylotic Radiculopathy and Myelopathy: A National Population-based Study. Spine. 2016;41(20):1593-1599. doi: 10.1097/BRS.0000000000001590 [DOI] [PubMed] [Google Scholar]
- 46.Puvanesarajah V, Jain A, Cancienne JM, et al. Complication and Reoperation Rates Following Surgical Management of Cervical Spondylotic Myelopathy in Medicare Beneficiaries. Spine. 2017;42(1):1-7. doi: 10.1097/BRS.0000000000001639 [DOI] [PubMed] [Google Scholar]
- 47.Hashimoto K, Aizawa T, Ozawa H, et al. Reoperation Rates after Laminoplasty for Cervical Disorders: A 26-Year Period Survival Function Method Analysis. Spine surgery and related research. 2019;3(4):304-311. doi: 10.22603/ssrr.2019-0028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hirvonen T, Siironen J, Marjamaa J, Niemelä M, Koski-Palkén A. Anterior cervical discectomy and fusion in young adults leads to favorable outcome in long-term follow-up. The spine journal : official journal of the North American Spine Society. 2020;20(7):1073-1084. doi: 10.1016/j.spinee.2020.03.016 [DOI] [PubMed] [Google Scholar]
- 49.Nakashima H, Kanemura T, Satake K, et al. Reoperation for Late Neurological Deterioration After Laminoplasty in Individuals With Degenerative Cervical Myelopathy: Comparison of Cases of Cervical Spondylosis and Ossification of the Posterior Longitudinal Ligament. Spine. 2020;45(15):E909-E916. doi: 10.1097/BRS.0000000000003408 [DOI] [PubMed] [Google Scholar]
- 50.Radcliff K, Davis RJ, Hisey MS, et al. Long-term Evaluation of Cervical Disc Arthroplasty with the Mobi-C© Cervical Disc: A Randomized, Prospective, Multicenter Clinical Trial with Seven-Year Follow-up. International journal of spine surgery. 2017;11:31. doi: 10.14444/4031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sasso RC, Anderson PA, Riew KD, Heller JG. Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. The Journal of bone and joint surgery American volume. 2011;93(18):1684-1692. doi: 10.2106/JBJS.J.00476 [DOI] [PubMed] [Google Scholar]
- 52.Ghobrial GM, Lavelle WF, Florman JE, Riew KD, Levi AD. Symptomatic Adjacent Level Disease Requiring Surgery: Analysis of 10-Year Results From a Prospective, Randomized, Clinical Trial Comparing Cervical Disc Arthroplasty to Anterior Cervical Fusion. Neurosurgery. 2019;84(2):347-354. doi: 10.1093/neuros/nyy118 [DOI] [PubMed] [Google Scholar]
- 53.Gornet MF, Lanman TH, Burkus JK, et al. Two-level cervical disc arthroplasty versus anterior cervical discectomy and fusion: 10-year outcomes of a prospective, randomized investigational device exemption clinical trial. Journal of neurosurgery Spine. 2019:1-11. doi: 10.3171/2019.4.SPINE19157 [DOI] [PubMed] [Google Scholar]
- 54.Burkus JK, Traynelis VC, Haid RW, Mummaneni P V. Clinical and radiographic analysis of an artificial cervical disc: 7-year follow-up from the Prestige prospective randomized controlled clinical trial: Clinical article. Journal of neurosurgery Spine. 2014;21(4):516-528. doi: 10.3171/2014.6.SPINE13996 [DOI] [PubMed] [Google Scholar]
- 55.Lee JC, Lee SH, Peters C, Riew KD. Risk-factor analysis of adjacent-segment pathology requiring surgery following anterior, posterior, fusion, and nonfusion cervical spine operations: survivorship analysis of 1358 patients. The Journal of bone and joint surgery American volume. 2014;96(21):1761-1767. doi: 10.2106/JBJS.M.01482 [DOI] [PubMed] [Google Scholar]
- 56.Lee JC, Lee SH, Peters C, Riew KD. Adjacent segment pathology requiring reoperation after anterior cervical arthrodesis: the influence of smoking, sex, and number of operated levels. Spine. 2015;40(10):E571-E577. doi: 10.1097/BRS.0000000000000846 [DOI] [PubMed] [Google Scholar]
- 57.Badhiwala JH, Platt A, Witiw CD, Traynelis VC. Cervical disc arthroplasty versus anterior cervical discectomy and fusion: a meta-analysis of rates of adjacent-level surgery to 7-year follow-up. J Spine Surg. 2020;6(1):217-232. doi: 10.21037/jss.2019.12.09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Green SB. How Many Subjects Does It Take To Do A Regression Analysis. Multivariate Behavioral Research. 1991;26(3):499-510. doi: 10.1207/s15327906mbr2603_7 [DOI] [PubMed] [Google Scholar]
- 59.Nakashima H, Kanemura T, Satake K, et al. Reoperation for Late Neurological Deterioration After Laminoplasty in Individuals With Degenerative Cervical Myelopathy: Comparison of Cases of Cervical Spondylosis and Ossification of the Posterior Longitudinal Ligament. Spine. 2020;45(15):E909. doi: 10.1097/BRS.0000000000003408 [DOI] [PubMed] [Google Scholar]
- 60.Morishita S, Yoshii T, Inose H, et al. Perioperative Complications of Laminoplasty in Degenerative Cervical Myelopathy -A Comparative Study Between Ossification of Posterior Longitudinal Ligament and Cervical Spondylotic Myelopathy Using a Nationwide Inpatient Database. Global Spine Journal. 2021:21925682211063868. doi: 10.1177/21925682211063867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kwok SSS, Cheung JPY. Surgical decision-making for ossification of the posterior longitudinal ligament versus other types of degenerative cervical myelopathy: anterior versus posterior approaches. BMC Musculoskeletal Disorders. 2020;21(1):823. doi: 10.1186/s12891-020-03830-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Long-Term Survivorship of Cervical Spine Procedures; A Survivorship Meta-Analysis and Meta-Regression by Mohamed Sarraj, Philip Hache, Farid Foroutan, Colby Oitment, Travis E. Marion, Daipayan Guha, and Markian Pahuta in Global Spine Journal