Abstract
The current coronavirus disease 2019 (COVID-19) pandemic has led Cameroon’s government to implement public health measures aimed at preventing its spread. This paper investigates how community health education on the virus was being carried out, what gaps exist and what further action could be taken. A survey instrument was used to gather data among a total of 179 Cameroonians recruited via opportunistic and snowball sampling methods. According to our findings, gaps exist. These include the need for adequate community health education on COVID-19, maximising multilingualism and indigenous cultural assets and disbanding misconceptions on the pandemic, as well as stigmatisation. The paper culminates by underlining the significance of an integrated approach to confront the pandemic. This approach captures the need to frame but also firm up community health education architecture on COVID-19 that captures inputs from different stakeholders, including indigenous knowledge holders, for collective wellbeing.
Keywords: community health education, COVID-19, Cameroon, integrated approach
The outbreak of the coronavirus (COVID-19) in 2019 in Wuhan China which soon assumed pandemic proportions has brought about unprecedented outcomes across the entire globe, not least because of a growing death toll. Following the first reported case of COVID-19 in Africa, in Egypt on Feb 14, 2020, just few days after World Health Organization (WHO) had declared the outbreak a pandemic, 1 a total of 47 African countries have been affected by the virus, with 77,087 deaths recorded as at the 27th of March, 2021. 2 This pales in comparison with global and other regional cases and total deaths. 3 Maeda and Nkengasong 4 assert that from the onset of the COVID-19 pandemic, earlier predictions suggested Africa would be worst hit, with about 70 million Africans infected and 3 million deaths. According to the author, the predicted surge was predicated on the “continent’s overstrained and weak health systems, inadequate financing of health care, paucity in human resources, and challenges posed by existing endemic diseases—including HIV, tuberculosis, and malaria.” 4 (p1) Whilst the gap between the predicted and current number of recorded COVID-19 cases and deaths in Africa can be ascertained as a puzzle, a number of factors have been advanced to deconstruct it. Writing for the BBC, Soy 3 posits five reasons why Covid-19 has been less deadly in Africa than other regions. These include the drastic actions taken by many nations to halt or slow the spread of the virus, wide public support for different measures, the characteristic of the population being mostly young people, favourable climate and good community health systems. In addition to some of these factors, Maeda and Nkengasong 4 also capture limited testing regime, preexisting immunity and genetic factors. Tembo et al. 5 also suggest there is evidence of possible under-reporting.
Whilst some of these factors may raise eyebrows and beckons for more interrogation, the COVID-19 pandemic continues to have far reaching impact on Africa, beyond the number of infections and death toll. For instance, a number of authors have opined the negative impact the pandemic is having on the economic growth of member states, the livelihood of the citizenry, as well as threatening gains made in achieving the UN sustainable development goals.6–8 Other wider impacts of the pandemic can be evident in literature. The case of restrictions and lockdown of entire countries and practice of social distancing continue to have detrimental consequence on the mental health of some people.9–11 Furthermore, with children not going to school over a prolonged period and members of the same family constrained to live together within a finite space as a result of lockdown, the real possibility of child abuse and domestic violence cannot be underestimated.11,12
Although it can be ascertained that the first wave of the COVID-19 pandemic and its impact in Africa has not progressed as predicted, there is evidence that the continent is having a more severe second wave, with many more cases. 1 Mwai 13 posits that Africa’s new variants of the virus are causing growing concerns with experts believing “the emergence of new coronavirus variations in Africa have contributed to an increase in the number of both cases and deaths reported in many countries on the continent.” 13 (p1) This highlights the need to rethink existing strategies being implemented to stop or slow the spread of the virus. To this end, a consideration is given to community health education. While the role of education in managing a health crisis at public level is foregrounded in literature,14–19 there is paucity of research that examines its usefulness in the management of the current COVID-19 pandemic, specifically within local community contexts. This paper therefore sets out to address this gap and is organised as follows: The next section provides a conceptual framework. Then, we contextualise the study, and outline our methodology. We subsequently present and discuss our empirical findings and provide concluding remarks.
Conceptualising Community Health Education
Before unveiling what we mean by community health education, it is expedient to look into the notion of community. The word community is characterised by a lack of precision and determined by the specific circumstances in which it is being alluded. 20 It means different things to different people in different fields such as geography, psychology, demography, history, medicine, women’s studies, political sciences and social policy, with each conveying a contextualised understanding of community rather than assigning a blanket meaning which might not be relevant to the context being referred to. Whilst there are different types of communities such as shared interest, function, identity, virtual and distant communities, our focus is on place based or geographical communities, which can be considered spatial locations, inhabited by people with similar needs and values. 21 They are bounded territories where individuals, people and families reside, meet most of their daily needs and interact with one another in a variety of social groups, organisations, institutions, and businesses. This community context is inclusive of other forms of communities and several frameworks operate within it such as community health education. In conceptualising community health education, we focus on the intersection between community education and public health education. Whilst community education brings to the fore the role of community educators, the same is applicable to the role of health educators.
Drawing on the work of Lev Vygosyky, we conceptualise community/health educator as the more knowledgeable other, 22 with the role of helping the less knowledgeable or informed navigate the zone of proximal acquisition of knowledge on a particular subject such as the pathology of COVID-19, its transmission, ways of mitigation or adaptation to its spread. The role of the more knowledgeable other can be actualised through a process of scaffolding of knowledge 23 or direct communication of new and helpful information to the recipient.
Different forms of community education abound but our interest lies with the radical model. Whereas the radical model can be defined as an educational attempt aimed at eliminating major inequalities all together from the society or significantly reduce the current scale,24,25 we contend that inequality can take different forms. As COVID-19 has exacerbated economic, educational, health and social class inequalities in the society,26–28 the place of a radical form of community education as a possible panacea cannot be overlooked. Community education within the context of a health crisis also captures public health education. Although the words “community” and “public” can be used interchangeably, health education defines the educational context and gives it a focus. Whitehead 29 posits different functions and actions related to health education including impartation with health related information that influences values, beliefs, attitudes and motivations; achievement of health or illness-related learning through knowledge acquisition, assimilation and dissemination; skills development and lifestyle/behaviour modification.
Community health education has been used in the past to address a number of health related challenges in the society such as Stroke, 14 Cardiovascular Disease, 15 Ebola Virus, 16 Cervical Cancer 17 and HIV Transmission.18,19 Community health education can be formal or informal, structured or unstructured, controlled or uncontrolled and leading to a conscientized empowerment of the community or members of the public to act on an acquired information or knowledge. In addition to the work of Lev Vygostky, we consider the usefulness of Habermas’ theory of communicative action and Freire’s idea of conscientization. Whilst Habermas’ 30 theory of communicative action points to the need for society’s stakeholders, actors or educators to operate in a collective and integrated context to frame the architecture of community health education, this can ultimately lead to a conscientized community. According to Freire’s 31 notion of conscientization, the community or public can be critically conscious of different health related issues that underpin the COVID-19 pandemic, and which could lead to praxis. Through praxis, instigated via community health education, local people can acquire the needed critical awareness of the state of the spread of the virus in their community and take action to mitigate or adapt to it as the new ‘normal’ dictates.
Contextual Background
The context of Cameroon was chosen for this study, primarily because of accessibility by the research team. Cameroon, with an estimated population of 25 million, shares borders with Nigeria, Gabon, Equatorial Guinea, Congo, Chad and the Central African Republic. The country is bilingual, having come under French and British colonial administrations, with eight of the ten administrative regions predominantly French speaking and the remaining two English speaking.
Whilst COVID-19 is a global phenomenon that has affected every continent, following the first occurrence in December 2019 in Wuhan China, Cameroon recorded its first case in March 2020 32 and have since then seen a upsurge in the number of people infected with the virus. As of August 22, 2020, there were 18,762 confirmed cases of COVID-19 with 408 deaths in Cameroon, 33 making it one of the hardest affected countries in Africa and the epicentre of the virus in central Africa. 34 To manage the spread of the virus, an inter-ministerial consultation was held on the 17th of March 2020 led by the prime minister, to assess the situation and identify appropriate actions to be implemented. 35 Consequently, Cameroon’s land, air and sea borders were closed, all operations of educational institutions from nursery to universities were suspended, gathering of more than 50 persons were prohibited, social venues such as bars, restaurants and entertainment spots were closed and a toll-free number set up for mobilization of a rescue team in the event of an emergency amongst others. Furthermore, and consistent with WHO guidelines, the public was urged to strictly observe hygienic measures such as regular hand washing with soap, covering the mouth when sneezing and maintaining social distancing. Isolation and care centres for COVID-19 patients were also created and the gravity of the spread of the virus necessitated the cancellation of Hajj pilgrimage for Cameroonian Muslims.36,37 After the implementation of the 3T Strategy of Track, Test and Treat, the government announced the launch of a pilot phase of mobile caravans in private companies, schools, universities and markets in Yaoundé. 36 These measures yielded some fruits and this was evidenced by the Minister of Public Health, stating on July 22nd 2020 on the State owned television channel (CRTV) that the country has succeeded in stabilizing the epidemic curve and that the peak of the pandemic has been reached. However, measures to fight COVID-19 have also had a damaging impact on the economy of the country, in addition to other social ills such as an increase in domestic violence. 36 Despite the positive and negative impact that accompanied measures put in place to halt the spread of the virus, gaps still exist in its handling. These gaps need to be addressed, because the pandemic has not been eradicated at the time of preparing this paper and some countries are noticing a second wave.38,39 As at 28 March 2021, Cameroon has 47,669 confirmed cases and 721 deaths, and this shows a significant increase from previous reports. 40 Forku 41 asserts that the second wave of COVID-19 has boosted this increase in the country's figures, with Manaouda Malachiem, Cameroon’s Minister of Public Health urging a return to the measures issued by the government in early 2020. This may be essential as the decisive move across the globe to get people vaccinated against the virus faces certain challenges in Africa, ranging from access to a COVID-19 vaccine to lack of willingness to take it. 42
Some of the gaps in Cameroon’s COVID-19 management captured in different grey literature include poor involvement and motivation of the public to comply with measures to impede the spread of the virus. 36 Ammassari 34 (p1) also asserts the ‘lack of adequate capacity to scale up testing and expand contact tracing and the provision of intensive care unit/ventilation support for the seriously ill, as well as limited personal protective equipment for medical staff” are some of the limitations. The author also maintains that the rapid implementation of community education programmes, emphasizing hand hygiene and social distancing, is also an ongoing challenge, especially in poor, often overcrowded, urban areas. Given the potential of community health education to give local people critical consciousness to reflect and act through praxis, to overcome a health crisis, we examine its role in COVID-19 handling in Cameroon.
Methodology
We nested the research that underpins this paper in a case study design, for an in-depth understanding of a complex issue. 43 Data collection occurred from June 9 – August 22, 2020. Given that multiple types of case study abound, that which is applicable to this study is an instrumental case study. 44 This was chosen because the case can provide an insight into similar cases in the developing world context. As case studies typically employ different methods to collect data, we used questionnaires to make the most of the available opportunity. Whilst questionnaires are typically used for quantitative oriented research projects, they have also been employed for qualitative studies 45 and in the case of this research, the questionnaires captured both closed and open-ended responses. Questions asked included participants’ view on trainings and guidelines provided to manage COVID-19, channels of communication about the pandemic, effort made to educate or inform the community on the risks posed by COVID-19 and challenges faced during the pandemic with regards to access to healthcare. The questionnaires were designed and administered via online means.
Two sets of participants were approached for the study, namely health workers such as doctors, nurses, medical lab technicians amongst others and local people in different residential communities. In total, 179 people participated in the study, that is, 39 health workers and 140 local community members. Participants came from eight of the ten regions that make up the administrative structure of Cameroon, with the most recruited from the Centre, Southwest, Northwest and Littoral regions of the country. The specific city, town or village location of participants was not captured by the data. Opportunistic sampling through existing networks and snowball methods were used to recruit participants and following their voluntary acceptance to participate in the study which adhered to standard ethical protocol.
Whereas the two sets of participants responded to bespoke questionnaires, the open-ended responses were analysed thematically, 46 while the closed ended responses provided simple descriptive outputs in the form of statistical graphs or charts.
Findings and Discussion
Findings from the data touch on the need for adequate community health education to combat the spread of the virus by maximising multilingualism and other cultural assets. It also depicted that community health education can be considered a two-edged sword to disband misconception and stigmatisation that underpin the virus. Insight into these themes will be covered in the ensuing part:
The Need for Adequate Community Health Education on COVID-19 Acknowledged
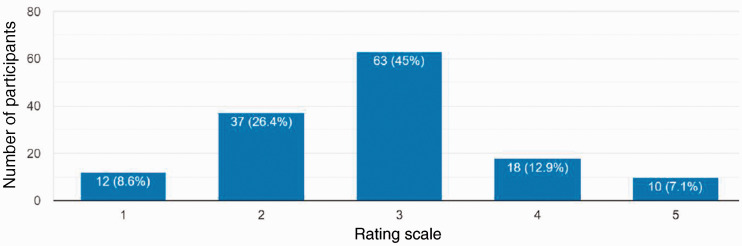
Both sets of participants, namely, health workers and local people were prompted to assess the adequacy of community health education on COVID-19, taking into consideration their role in the society and communities they reside in. Whilst it was largely acknowledged that community education on COVID-19 is ongoing, with the participation of different stakeholders, this was not adequate. Of the local community participants (n = 140) who were asked to rate the adequacy of community education on COVID-19 on a scale of 1 to 5, only 10 indicated it was very adequate as depicted by Figure 1.
Figure 1.
Participants’ Perception of the Adequacy of Community Health Education.
The shortcomings associated with community education programmes intended to slow the spread of the virus and reduce its impact are underlined by different factors – some of these touch on politics, access, and training. To cast more light on these, a female health worker from the North West region asserts that “the educational measures are politicized and done mostly by politicians with no involvement of health workers, so I do not think that the measures are adequate”. Whilst some politicians of ruling parties are using the pandemic to secure political points or scores, 47 those in the opposition could be said to be involved in premature post mortems on the government’s response to COVID-19 for party political gains. 48 Apart from playing politics, the inadequacy of community health education is compounded by the fact that some residential communities are in very remote and restive or conflict areas which impede access. A male health worker from the North West Region posits that “there are still gaps to reach to the population especially those living in conflict affected areas with barriers to accessing health education on COVID-19”. This is particularly the case in the ongoing conflict in the English speaking zone of Cameroon where separatists have taken up arms and are clamouring for an independent state. 49 Given the urgent need to create an awareness and wage a fight in every community against COVID-19 and its impact, the UN Secretary-General António Guterres “urged warring parties across the world to lay down their weapons in support of the bigger battle against COVID-19.” 50 Whilst this is a laudable demand, research data reveals that most of the warring factions in the Anglophone crisis in Cameroon were not heeding to it. We argue that the call for a collective and integrated approach to fight the common enemy known as COVID-19 needs to be heeded by different stakeholders for a sustainable outcome.
Given that our idea of ‘community’ in community health education was inclusive, we were not limited to sensitization of lay people on COVID-19 but did also capture information on training of relevant health personnel to combat the spread of the virus. A male health worker from the North West Region asserts:
Most District Medical Officers and hospital directors have resorted to using online contents from various sources like WHO and CDC to auto-build their own capacities and subsequently that of their staff. Some senior level district staff like myself have been briefed on COVID-19 through regional meetings but an actual capacity-building workshop has not been done as in the case at the central level or Yaounde. The training of health actors is not extensively done. Only district management team members and certain regions/towns have benefited from such training.
This lack of extensive or adequate training among health workers to combat COVID-19 at different health facilities could mean that instead of being on the offensive to defeat the virus, some of them can become victims and subsequently in need of care. A male health worker from the Centre Region maintains that “since health professionals are not also adequately protected, some are scared to manage patients with COVID-19”. Although a recurrent theme among challenges in the architecture of COVID-19 management in Cameroon is the lack of personal protection equipment, education on their proper use and other necessities associated with curbing the spread of the virus were also identified. The acute shortage of resources and poor stakeholder coordination 51 may have exacerbated these challenges, including the lack of rapid implementation of community education programmes.
Maximising Multilingualism and Indigenous Cultural Assets for Community Health Education on COVID-19
By multilingualism, the reference is on variety of languages spoken in a given setting. In addition to Cameroon’s two official languages of English and French and a lingua franca known as pidgin, Cameroon has over 270 indigenous languages. 52 A significant number of participants attributed the lack of adequate education or sensitisation of the public on COVID-19 to little or no inclusion of native languages and pidgin as mediums of communication, given that they are widely spoken, compared to English and French. The following participants assert:
The mother tongues or indigenous languages of the different local communities should be used since most of the indigenes don’t understand the official languages. (A female community member from the West Region)
Pidgin English should be used because most ‘buyam sellams’ and IDPs from the North West and South West regions understand the language better. (A male community member from the Centre Region)
The uneducated population speaks and understands pidgin better than any other language and therefore it should be used. (A female community member from the centre region)
COVID-19 attacks mostly old persons and most of them don't understand pidgin either, so native language or vernacular will be the best language to make them understand. (A male community member from the South West Region)
The COVID-19 treatment protocol available for my facility is the one provided by the government via the National Scientific Committee. It is unfortunately in French and so adoption is limited to those who can comprehend French. Translating such documents must be done via professional schemes, which are too expensive for individuals at their facilities to adopt. (A male health worker from the North West Region)
Considering these assertations, it can be argued that for the community or public to be sensitized or well informed about COVID-19 and prevention mechanisms for instance, the information must be conveyed via the right language for optimal impact. Where necessary, translators or interpreters can be sought to aid communication. It can be further argued that using an appropriate native language can give expression to a people’s cultural capital or habitus.53,54 Not only is a native language instrumental in enhancing community health education on COVID-19, research data also reveals the significance of capturing indigenous knowledge or knowhow. A male health worker from the Centre Region noted that ‘treatment protocols were copied from the West and indigenous knowhow which proved to be quite potent was not given deserved attention’. The demand to include indigenous knowledge holders and their insights in community health education on COVID-19 points to an integrated approach. It can be argued that interventions designed for community health education on COVID-19 should adopt a collaborative approach that would capture and incorporate the views of those living within that community if such an intervention would not be considered cultural invasion or intrusion. 31 Although COVID-19 is having a global impact, and its management has a predominantly western steerage via WHO, headquartered in Geneva, a hybrid approach to dealing with the virus, inclusive of indigenous knowledge can have a sustainable impact in a developing world context such as Cameroon. Various indigenous interventions have been employed to impede the spread or deadly impact of COVID-19 in many resource constraint communities, with some claims of success. 55 Whilst the veracity of such claims can be questioned, it can also be argued that there are useful assets in African indigenous architectures that can be advantageous to the fight against COVID-19 and should be captured in any community health education framework.
Community Health Education, a Two-Edged Sword to Disband Misconception on COVID-19 and Stigmatisation
Research data revealed that little or no community health education on COVID-19 can be devastating as it can provide a fertile ground for misconceptions and fake news to flourish. This can lead to people becoming complacent with obeying guidelines, as well as being vulnerable to transmission, infection and even death. The following participants captured some of the misconceptions about COVID-19 in their responses:
Some people still don’t believe COVID-19 is real and some say that the medical personnel are injecting patients with the virus. (A female health worker from North West Region)
Some people don’t believe in the existence of COVID-19 and others consider it as a political instrument maliciously designed to eliminate adversaries. (A male community from the North West Region)
Most people think the virus doesn’t exist and that the government is just inflating figures in order to get money from donor organizations. (A female health worker from the North West Region)
Some people think COVID-19 is an issue of the white man that only minimally affects the black man. (A male health worker from the Centre Region)
Widespread misinformation about a health crisis is foregrounded in literature16,56 including those related to COVID-19.57–63 Drawing on Brennen et al., 57 some of the misinformation underpinning COVID-19 touch on public authority action, community spread, prominent actors, conspiracy theories, virus origin, and vaccine development. Twitter, YouTube, and Facebook are commonly used channels. Larson 64 asserts that the biggest pandemic risk is viral misinformation. It can be posited that to counter a viral misinformation on COVID-19, a robust and aggressive form of community health education is needed, one with an integrated approach.
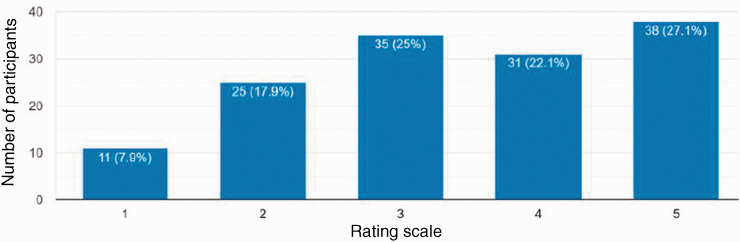
In addition to the subject of misinformation about COVID-19, a key theme that emerged from the data is stigmatisation. It is a good thing that not everyone is peddling misinformation about the virus. However, a number of persons who believe COVID-19 exists were on the other hand stigmatising patients or health facilities for fear of contamination. Stigmatisation during a health crisis is also not uncommon.65,66 Out of the 140 local community participants prompted to rate the extent to which COVID-19 patients are stigmatised – with 5 being most stigmatised, Figure 2 reveals an interesting finding.
Given the displayed figures in Figure 2, it can be ascertained that a vast majority of community participants felt COVID-patients are experiencing some forms of stigmatisation with only 11 members revealing they were not. This reveals a worrying sign of the ineffectiveness of relevant measures put in place to manage the spread of the virus and impact of the pandemic.
Figure 2.
Participants’ Rating of the Extent to Which COVID-19 Patients Were Stigmatised.
The following accounts from health participants support the claim of stigmatisation in the local community:
Many myths and misinformation have led to the stigmatization of health workers and institutions that manage COVID-19. (A male health worker from the North West Region)
Stigma still runs strong. This is the reason some patients with symptoms deny seeking medical attention. (A female health worker from the Centre Region)
Yes, patients feel stigmatised. Even in my centre many staff members kept away from COVID-19 patients. (A male health worker from the Centre Region)
There is serious self-stigma and social/public stigma has been a major challenge in COVID-19 testing and management of patients. There is a lot of distrust of the community on health facilities, especially, the public facilities. (A male health worker from the North West Region)
Even health facilities designated to treat COVID-19 patients have been shunned by the general public for fear of getting contaminated. You must have head over the media that the routine vaccination coverage has dropped by over 20% in the last quarter in Cameroon as a result. (A male health worker from the Centre Region)
Interestingly, research data also reveals that not only are COVID-19 patients stigmatised by the public but also by some health workers charged with administering treatment. Health facilities are shunned and while in normal times there will be routine visits to hospitals for other health matters by members of the public, the rate has dropped. It is the case that in some parts of the world routine visits to the hospitals were limited to prioritise COVID-19 patients due to limited capacity – For instance, the NHS in England stated on its website that “to help stop the spread of coronavirus, most hospitals have stopped or significantly limited visits.” 67 (p1) However, the context of abstaining from hospitals mentioned in the research that underpins this paper is that of stigmatisation. Stigmatisation of COVID-19 patients can lead to depression, post-traumatic stress disorder and a negative impact on their mental health.9–12 We argue that through an integrated intervention of community health education on COVID-19, misconceptions and stigmatisation can be squashed.
Conclusion: Towards an Integrated Approach to Community Health Education on COVID-19
The study at the nexus of this paper sets out to investigate how the COVID-19 pandemic in Cameroon was being managed, with particular focus on community health education. Following data analysis, it can be acknowledged that the current state of community health education to combat a pandemic in Cameroon such as the COVID-19 is not adequate. In order to address the gaps, we argued for the need to maximise multilingualism and indigenous cultural assets for an effective community health education on COVID-19. We also posited that community health education can be positioned as a two-edged sword to disband misconception on COVID19 and stigmatisation.
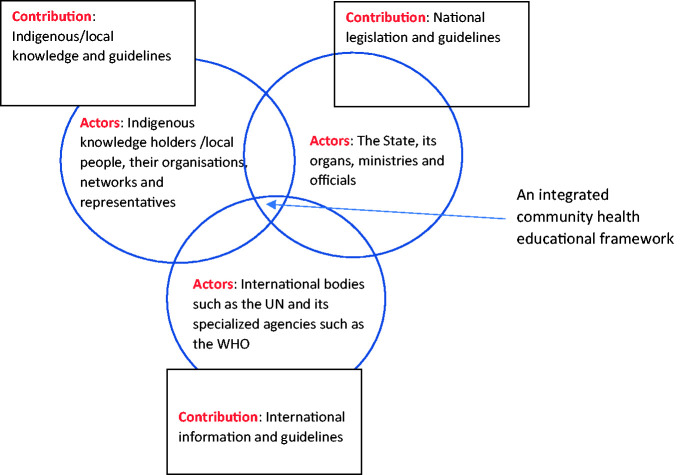
Whilst COVID-19 is an emergent pandemic and a lot is still being discovered about the virus, which means some mistakes in management were made globally, from the onset,48,68,69 it has nevertheless exposed gaps in the health systems of many countries including Cameroon.47,48,70 COVID-19 has proven to Cameroon how weak and regressive its health system is in the context of pandemic preparedness and response that needs to be strengthened and rendered more resilient in the advent of any future public health crisis. To address the gaps in the ongoing COVID-19 management in Cameroon and any eventual pandemic outbreak, research data points to the need for an integrated approach to community health education. Whilst there are different integrated approaches to health,71,72 we draw on Berkes and Ross 73 to maintain that an integrated approach is concerned with how different stakeholders with their resources combine to produce the architecture and process of community health education to combat COVID-19 in a given geographical context such as Cameroon. In this case, adaptive capacity and shared agency are both highly significant.
In the framework for an integrated approach to community health education to halt the spread of COVID-19 (see Figure 3), we identify three key stakeholders, namely the global community represented by relevant international organisations, the State, and the citizenry who may also be indigenous knowledge holders.
Figure 3.
A Framework for an Integrated Community Health Education on a Global Pandemic.
The suggested integrated approach, predicated on mutual trust and respect, calls for collective responsibility, contribution, coordination and participation of all stakeholders as this can play an important role in generating and galvanising useful ideas in developing and taking effective actions to frame and firm up community health education on COVID-19. This approach can be most effective in leading to behavioural change across different sectors and segments of the wider community that will halt the spread of the virus. As existing and prospective international guidelines against COVID-19 are translated into national guidelines, these also need to capture indigenous/local realities for optimal understanding and sustainable compliance. Whilst this hinges on Habermas insight into communicative rationality that brings to the fore the interconnection between language, reason and action, 74 we also argue that communicative relationality is very vital. Linkages should be established between indigenous knowledge holders or local people, their networks and representatives such as their traditional rulers with the State, its organs, ministries, and officials for a concerted, integrated and inclusive educational framework to fight COVID-19. This inclusivity embedded in an integrated approach to community health education can enhance social capital and a conscientized participation of all stakeholder. Through praxis, the citizenry can collectively take action to educate themselves and every member of the community on COVID-19, and for collective wellbeing by being each other’s keeper. This is also consistent with the spirits of solidarity and shared humanity that underpin the African communal way of life. Furthermore, this integrated approach brings to the fore the relational networks and cultural assets which are valuable for infrastructural provision 75 and can also be useful in fostering community health education in resource constraint regions.
Whilst the study unveils some interesting findings, it also has some limitations. Firstly, the research instrument was solely in the English language, due to the additional cost of securing a translator. Given that Cameroon is bilingual, with the vast population French speaking, a number of potential participants could have been alienated as a result of language barrier. Secondly, we were constrained by time and limited resources not to recruit participants from all regions, towns and villages of the country and had to make the most of available opportunities. Thirdly, government officials were not targeted as we felt we needed to capture the voices of local people and health professionals who are at the forefront of combating the COVID-19 pandemic. However, on reflecting, it would have been worthwhile to capture the opinions of policy makers and compare, as well as contrast with others. Irrespective of these limitations, we argue that the study and findings articulated in this paper present an opportunity for the country to rethink community health education as a viable strategy in confronting COVID-19 and any future pandemic.
Author Biographies
Marcellus Forh Mbah is a senior lecturer at Institute of Education, Nottingham Trent University, Nottingham, UK. His Research interests touch on the following overarching themes: education and international development, university community engagement, climate change education, community-based service learning, community health education and indigenous knowledge systems.
Henry Ngenyam Bang is a research fellow at Disaster Management Centre, Bournemouth University, Poole, UK. He has interdisciplinary research interests in disaster risk reduction/management & International Development related themes like governance/institutional frameworks, climate change-induced risks and natural/anthropogenic hazards. Of peculiar interest, are the trajectories of vulnerability/resilience including implications for sustainable development particularly in developing countries.
Humphrey Ngala Ndi is an associate professor at Department of Geography, Higher Teacher Training College, University of Yaounde I, Yaounde, Cameroon. His research interests are situated within the discipline of human geography in general, but health geography in particular. In this wise, his specific interest is in studying the impact of different types of human environments and health. These include the health implications of urban and rural landscapes, and industrial, agricultural landscapes among others.
Judwin Alieh Ndzois a paediatrician at Nottingham University Hospitals NHS Trust, Nottingham, UK.She is passionate about improving nutritional statuses of children in Africa and has formerly worked with Medicines Sans Frontières and the French Red Cross.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Marcellus Mbah https://orcid.org/0000-0002-4199-0819
Henry Bang https://orcid.org/0000-0002-1850-857X
References
- 1.Salyer JS, Maeda J, Sembuche S, et al. The first and second waves of the COVID-19 pandemic in Africa: a cross-sectional study. Lancet 2021; 397: 1265–1275. www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00632-2/fulltext (accessed 28 March 2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. WHO African Region numbers at a glance, www.afro.who.int/health-topics/coronavirus-covid-19 (2021, accessed 28 March 2021).
- 3.Soy A. Coronavirus in Africa: five reasons why Covid-19 has been less deadly than elsewhere. BBC News, 2020, www.bbc.co.uk/news/world-africa-54418613 (accessed 28 March 2021).
- 4.Maeda JM, Nkengasong JN.The puzzle of the COVID-19 pandemic in Africa. Science 2021; 371: 27–28. [DOI] [PubMed] [Google Scholar]
- 5.Tembo J, Maluzi K, Egbe F, et al. Covid-19 in Africa. BMJ 2021; 372: n457. https://www.bmj.com/content/372/bmj.n457 (accessed on the 28 March 2021). [DOI] [PubMed]
- 6.Ataguba JE.COVID-19 pandemic, a war to be won: understanding its economic implications for Africa. Appl Health Econ Health Policy 2020; 18: 325–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lone SA, Ahmad A.COVID-19 pandemic—an African perspective. Emerg Microbes Infect 2020; 9: 1300–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ekwebelem OC, Ofielu ES, Nnorom-Dike OV, et al. Threats of COVID-19 to achieving United Nations sustainable development goals in Africa. Am J Trop Med Hygiene 2021; 104: 457–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Armitage R, Nellums LB.COVID-19 and the consequences of isolating the elderly. Lancet Public Health 2020; 5: e256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jiménez-Pavón D, Carbonell-Baeza A, Lavie CJ.Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: special focus in older people. Prog Cardiovasc Dis 2020; 63: 386–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bradbury‐Jones C, Isham L.The pandemic paradox: the consequences of COVID‐19 on domestic violence. J Clin Nurs 2020; 29: 2047–2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galea S, Merchant RM, Lurie N.The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med 2020; 180: 817–818. [DOI] [PubMed] [Google Scholar]
- 13.Mwai P.Coronavirus: Africa’s new variants are causing growing concern. BBC News, 2021, www.bbc.co.uk/news/world-africa-53181555 (accessed 28 March 2021).
- 14.Stern EB, Berman M, Thomas JJ, et al. Community education for stroke awareness: an efficacy study. Stroke 1999; 30: 720–723. [DOI] [PubMed] [Google Scholar]
- 15.Luepker RV, Murray DM, Jacobs DR, Jr, et al. Community education for cardiovascular disease prevention: risk factor changes in the Minnesota heart health program. Am J Public Health 1994; 84: 1383–1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kpanake L, Gossou K, Sorum PC, et al. Misconceptions about Ebola virus disease among lay people in Guinea: Lessons for community education. J Public Health Policy 2016; 37: 160–172. [DOI] [PubMed] [Google Scholar]
- 17.Abiodun OA, Olu-Abiodun OO, Sotunsa JO, et al. Impact of health education intervention on knowledge and perception of cervical cancer and cervical screening uptake among adult women in rural communities in Nigeria. BMC Public Health 2014; 14: 814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aggleton P, Yankah E, Crewe M.Education and HIV/AIDS—30 years on. AIDS Educ Prev 2011; 23: 495–507. [DOI] [PubMed] [Google Scholar]
- 19.Mukandavire Z, Garira W, Tchuenche JM.Modelling effects of public health educational campaigns on HIV/AIDS transmission dynamics. Appl Math Modell 2009; 33: 2084–2095. [Google Scholar]
- 20.Elliott J, Francis H, Humphreys R. (edset al. Communities and their universities: the challenge of lifelong learning. London: Lawrence & Wishart Limited, 1996. [Google Scholar]
- 21.Wallace A.We have had nothing for so long that we don’t know what to ask’: new deal for communities and the regeneration of socially excluded terrain. Soc Policy Soc 2007; 6: 1–12. [Google Scholar]
- 22.Chaiklin S.The zone of proximal development in Vygotsky’s analysis of learning and instruction. Vygotsky’s Educ Theory Cult Context 2003; 1: 39–64. [Google Scholar]
- 23.Sanders D, Welk DS.Strategies to scaffold student learning: applying Vygotsky’s zone of proximal development. Nurse Educ 2005; 30: 203–207. [DOI] [PubMed] [Google Scholar]
- 24.Baker J, Lynch K, Cantillon S, et al. 2004. Equality, from theory to action. London: Palgrave MacMillan. [Google Scholar]
- 25.Fitzsimons C.2017. Rekindling community education in neoliberal times. In: Community education and neoliberalism. Cham: Palgrave Macmillan, pp.227–245.
- 26.Patel JA, Nielsen FBH, Badiani AA, et al. Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health 2020; 183: 110–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Obeng-Odoom F.COVID-19, inequality, and social stratification in Africa. Afr Rev Econ Finance 2020; 12: 3–37. [Google Scholar]
- 28.Bowleg L. We’re not all in this together: on COVID-19, intersectionality, and structural inequality. Am J Public Health 2020; 110: 917. [DOI] [PMC free article] [PubMed]
- 29.Whitehead D.Health promotion and health education: advancing the concepts. J Adv Nurs 2004; 47: 311–320. [DOI] [PubMed] [Google Scholar]
- 30.Habermas J.The theory of communicative action: lifeworld and systems, a critique of functionalist reason. Hoboken: John Wiley & Sons, 2015, vol. 2. [Google Scholar]
- 31.Freire P.Pedagogy of the oppressed (Ramos MB, Trans.). New York: Continuum, 2007 (Original work published 1970).
- 32.Kouagheu J. Cameroon, Togo confirm first cases of coronavirus, www.reuters.com/article/us-health-coronavirus-cameroon-idUSKBN20T10Z (2020, accessed 22 August 2020).
- 33.WHO. Cameroon Covid 19 situation, https://covid19.who.int/region/afro/country/cm (2020, accessed 22 August 2020).
- 34.Ammassari S.Dealing with COVID-19 in Cameroon, www.unaids.org/en/resources/presscentre/featurestories/2020/may/20200511_covid19-cameroon (2020, accessed 22 August 2020).
- 35.Services of the Prime Minister. Government response strategy to the coronavirus pandemic (COVID-19), www.spm.gov.cm/site/?q=en/content/government-response-strategy-coronavirus-pandemic-covid-19 (2020, accessed 22 August 2020).
- 36.OCHA. Cameroon COVID-19 Emergency Situation Report No. 05, www.humanitarianresponse.info/sites/www.humanitarianresponse.info/files/documents/files/covid19_emergency_sitrep_ndeg5.pdf (2020, accessed 22 August 2020).
- 37.UNICEF. Cameroon: COVID-19 Situation Report #16, 23 July–06 August 2020, https://reliefweb.int/report/cameroon/cameroon-covid-19-situation-report-16-23-july-06-august-2020 (2020, accessed 22 August 2020).
- 38.Badcock J.Coronavirus: why Spain is seeing second wave, www.bbc.co.uk/news/world-europe-53832981 (2020, accessed 22 August 2020).
- 39.Newey S, Gilbert D, Clark A.Is a second wave beginning to sweep through Europe?, www.telegraph.co.uk/global-health/science-and-disease/second-wave-coronavirus-covid-19-cases-rising-europe/ (2020, accessed 22 August 2020).
- 40.WHO. Cameroon Covid 19 situation, https://covid19.who.int/region/afro/country/cm (2021, accessed 29 March 2021).
- 41.Forku R. Cameroon minister urges respect of virus measures. AA, www.aa.com.tr/en/africa/cameroon-minister-urges-respect-of-virus-measures/2153694 (2021, accessed 29 March 2021).
- 42.Samarasekera U. Feelings towards COVID-19 vaccination in Africa. Lancet 2021; 21: P324. https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(21)00082-7/fulltext (accessed 29 March 2021). [DOI] [PMC free article] [PubMed]
- 43.Crowe S, Cresswell K, Robertson A, et al. The case study approach. BMC Med Res Methodol 2011; 11: 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stake RE.The art of case study research. Thousand Oaks, CA: SAGE, 1995.
- 45.McGuirk PM, O’Neill P. Using questionnaires in qualitative human geography. In: Hay I (ed.) Qualitative research methods in human geography. Don Mills: Oxford University Press, 2016, pp. 246–273.
- 46.Braun V, Clarke V.Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 47.Ojong N.The COVID-19 pandemic and the pathology of the economic and political architecture in Cameroon. Healthcare 2020; 8: 176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oliver D.David Oliver: Covid-19—recriminations and political point scoring must wait. BMJ 2020; 368. [DOI] [PubMed] [Google Scholar]
- 49.Chothia F (2018) Cameroon's Anglophone crisis: Red Dragons and Tigers – the rebels fighting for independence. BBC NEWS. Available at: https://www.bbc.co.uk/news/world-africa-45723211 (accessed August 22 2020)
- 50.UN, 2020.
- 51.Kingue S, Rosskam E, Bela AC, et al. Strengthening human resources for health through multisectoral approaches and leadership: the case of Cameroon. Bull World Health Organ 2013; 91: 864–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ndille R.English and French as official languages in Cameroon: the intentionality of colonial representations and the failure of a Cameroon-centric identity; 1884 and after. Eur J Lang Stud 2016; 3(2). [Google Scholar]
- 53.Lareau A, Weininger EB.Cultural capital in educational research: a critical assessment. Theory Soc 2003; 32: 567–606. [Google Scholar]
- 54.Bourdieu P.The genesis of the concepts of habitus and field. Sociocriticism 1985; 1: 11–24. [Google Scholar]
- 55.Oben J, Bigoga J, Takuissu G, et al. The acceptability of ‘star yellow,’ a Cameroonian functional food that could curb the spread of the COVID-19 via feces. Funct Foods Health Dis 2020; 10: 324–330. [Google Scholar]
- 56.Wang Y, McKee M, Torbica A, et al. Systematic literature review on the spread of health-related misinformation on social media. Soc Sci Med 2019; 240: 112552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brennen JS, Simon F, Howard PN, et al. Types, sources, and claims of COVID-19 misinformation. Reuters Inst 2020; 7: 3–1. [Google Scholar]
- 58.Roozenbeek J, Schneider CR, Dryhurst S, et al. Susceptibility to misinformation about COVID-19 around the world. R Soc Open Sci 2020; 7: 201199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kouzy R, Abi Jaoude J, Kraitem A, et al. Coronavirus goes viral: quantifying the COVID-19 misinformation epidemic on Twitter. Cureus 2020; 12(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shahi GK, Dirkson A, Majchrzak TA.An exploratory study of covid-19 misinformation on twitter. Online Soc Netw Media 2021; 22: 100104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gupta L, Gasparyan AY, Misra DP, et al. Information and misinformation on COVID-19: a cross-sectional survey study. J Korean Med Sci 2020; 35: e256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ihekweazu C, Agogo E.Africa’s response to COVID-19. BMC Med 2020; 18: 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Islam MS, Sarkar T, Khan SH, et al. COVID-19–related infodemic and its impact on public health: a global social media analysis. Am J Trop Med Hygiene 2020; 103: 1621–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Larson HJ.The biggest pandemic risk? Viral misinformation. Nature 2018; 562: 309–310. [DOI] [PubMed] [Google Scholar]
- 65.Holloway I, Sofaer-Bennett B, Walker J.The stigmatisation of people with chronic back pain. Disabil Rehabil 2007; 29: 1456–1464. [DOI] [PubMed] [Google Scholar]
- 66.Aggleton P, Wood K, Malcolm A, Parker R and Maluwa M. HIV-related stigma, discrimination and human rights violations: case studies of successful programmes. Joint United Nations Programme on HIV/AIDS. Available at: https://repository.library.georgetown.edu/handle/10822/984894 (Accessed August 22, 2020)
- 67.NHS. Visiting someone in hospital, www.nhs.uk/using-the-nhs/nhs-services/hospitals/visiting-someone-in-hospital/ (2020, accessed 24 August 2020).
- 68.Miller A.Did the WHO mishandle the global coronavirus pandemic? www.cbc.ca/news/health/coronavirus-who-china-canada-pandemic-1.5549836 (2020, accessed 24 August 2020).
- 69.Peston R. What was the government’s biggest coronavirus mistake? www.itv.com/news/2020-07-17/what-was-the-governments-biggest-coronavirus-mistake (2020, accessed 24 August 2020).
- 70.Chetterje P.Gaps in India’s preparedness for COVID-19 control. Lancet Infect Dis 2020; 20: 544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rüegg SR, Häsler B, Zinsstag J.Integrated approaches to health: a handbook for the evaluation of One Health. Wageningen: Wageningen Academic Publishers, 2018.
- 72.Baron SL, Beard S, Davis LK, et al. Promoting integrated approaches to reducing health inequities among low‐income workers: applying a social ecological framework. Am J Ind Med 2014; 57: 539–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Berkes F, Ross H.Community resilience: toward an integrated approach. Soc Nat Resour 2013; 26: 5–20. [Google Scholar]
- 74.Habermas J.On the pragmatics of social interaction: preliminary studies in the theory of communicative action. Cambridge: MIT Press, 2002.
- 75.Fonchingong CC. Re-inventing community development: Utilizing relational networking and cultural assets for infrastructure provision. Societies 2018; 8(3): 84.