Abstract
Background:
Advances in pediatric intensive care have dramatically improved the prognosis for critically ill patients. The study aimed to determine the survival status and predictors of mortality among patients admitted to the pediatric intensive care unit at selected tertiary care hospitals in Ethiopia.
Methods:
A health facility-based prospective observational study from October 2020 to May 30, 2021, was conducted in a selected tertiary care hospital in Ethiopia. Kaplan Meier was used to compare patient survival experiences and Cox regression was used to identify independent predictors of ICU mortality. The hazard ratio was used as a measure of the strength of the association, and a P-value of <.05 was considered to declare statistical significance.
Results:
Of 206 study participants, 59 (28.6%) patients died during follow-up time, and the incidence of mortality was 3.6 deaths per 100 person-day observation (95% CI: 2.04-5.04 deaths per 100 person-days). Respiratory failure 19 (32.2%) was the commonest cause of death followed by septic shock 11(18.6). In-ICU complications (AHR: 2.13; 95% CI: 1.02, 4.42; P = .04), sepsis diagnosis (AHR: 2.43; 95% CI: 1.24, 4.78; P = .01), GCS < 8 (AHR: 1.96; 95% CI: 1.12, 3.43; P = .02), use of sedative drugs (AHR: 2.40; 95% CI: 1.16, 4.95; P = .02) were linked with increased risk of in-ICU mortality. In contrast, the use of mechanical ventilation was associated with decreased mortality (AHR: 0.45; 95% CI: 0.21, 0.92; P = .03).
Conclusion:
The study found a high incidence of in-ICU mortality among admitted pediatric patients in selected Ethiopian tertiary care hospitals. In-ICU complications, sepsis diagnosis, GCS < 8, and patient use of sedative drugs were independent predictors of in-ICU mortality. Prudent follow-up is warranted for those patients with the aforementioned risk factors.
Keywords: Survival status, predictors of mortality, pediatric intensive care unit, Ethiopia
Introduction
Intensive care is a multi-disciplinary and inter-professional specialty committed to the management of patients with serious organ dysfunction. 1 The pediatric intensive care unit (PICU) is a specifically staffed, separate, and independent area in the health care facilities dedicated to the broad management of patients with critical illnesses to reduce mortality by strictly monitoring and treating severely ill patients who are considered to be at high risk of death.1,2
Regardless of significant improvements in decreasing child mortality, worldwide childhood mortality rates remain high, and children continue to face extensive regional disparities in their chances of existence. 3 The World Health Organization (WHO) report shows that the major causes of pediatric death in developing countries are preventable and curable diseases if treatment is optimized.4,5 The prevalence of intensive care unit (ICU) pediatric mortality was varied in developed and developing countries and was very high in low-income countries6-10 as compared to high-income countries.11-13 In the United States (US), the primary causes of mortality among under-five children were congenital anomalies and accidental injuries, but in unindustrialized countries, most childhood mortality was due to infections such as pneumonia, diarrhea, and severe malaria. 2
Advances in pediatric intensive care have radically enhanced the prognosis for critically ill patients, but pediatric critical care services were reasonably inadequate in developing countries, and children’s mortality remains a major health problem, particularly in Sub-Saharan Africa (SSA), with varying qualities and quantities of the infrastructure necessary for the provision of suitable critical care services. 14 In 2020 alone, SSA will remain the region with the highest under-5 mortality rate, which accounts for 53% of all under-five deaths globally.3,15 Studies conducted in Mozambique, Rwanda, and Eritrea showed that mortality rates in the ICU were found to be high, which were 25%, 50%, and 25.3%, respectively.9,16,17
Ethiopia is one of the top 5 countries with the world’s highest under-5 mortality rates, which account for 59 deaths per 1000 live births.5,18 Based on available findings, the pediatric ICU is where the highest number of deaths occur in most hospitals in Ethiopia. The studies conducted in Ethiopia reported that the overall mortality rate of patients admitted to the PICU was 8.5%, 32.6%, and 39.8%, with the most common causes of death being neurologic disorders, infections, and cardiovascular disease, respectively.6,10,19
As a result of the high burden of critically ill children in developing countries, the pediatric ICU is an essential area of service to save the lives of patients with acutely life-threatening conditions. Organizational details of pediatric ICUs and available data on pediatric intensive care, specifically on the incidence of mortality and its predictors among patients admitted to PICUs in Ethiopia, remain insufficient. Also, most of the existing evidence of mortality in the pediatric ICUs was limited to single-center, revised patient medical charts retrospectively.6,8,10,19,20
In Ethiopia, there are a small number of pediatric ICUs established for pediatric patients, and in addition to that; there is an inadequate resource to provide care for critically ill patients. This makes the establishment of adequate service and the enhancement of outcomes difficult. So, there is a great need to conduct an extensive study on the hospital basis, particularly the ICU basis, to obtain reliable information in this area. Therefore, the aim of the study was to determine the incidence of mortality and its predictors among patients admitted to selected tertiary health care hospitals in Ethiopia.
Methods and Participants
Study design, period, and setting
An institutional-based prospective observational study was conducted among pediatric patients admitted to the PICU at Jimma Medical Center (JMC), and St. Paul’s Hospital Millenium Medical College (SPHMMC) from October 2020 to May 2021. JMC is the teaching and referral hospital in south-west Ethiopia, located in Jimma City, which provides services for more than 20 million people. Currently, the hospital has more than 600-beds, including 4 PICU beds.
SPHMMC is a tertiary care hospital located in Addis Ababa, the capital city of Ethiopia. It is one of the largest government hospitals in the nation, and its core services include the provision of medical care, teaching, and research. The hospital provides services to patients coming from Addis Ababa and all over Ethiopia. Currently, the hospital has more than 750 beds, and of these, the PICU has 6 beds with electronic monitors and mechanical ventilators for patients admitted to the PICU.
Source and study population
All pediatric patients admitted to the pediatric ICUs at JMC and SPHMMC were our source population. Pediatric patients admitted to the pediatric ICU during the study period who met the inclusion criteria comprised the study populations.
Study variables
Dependent variables
Time to death (ICU mortality).
Independent variables
The independent variables were age, gender, residence, weight, patient category, nutritional status, vaccination status, source of admission, frequency of admission, reason for admission, presence of comorbid illness, mental status, organ dysfunction, and intervention during ICU stay, PIM2 score, and length of ICU stay, as well as caregiver-related factors.
Eligibility criteria
All pediatric patients who were admitted to the PICU of JMC and SPHMMC during the study period were included, while those who died on arrival or died within 2 hours of admission were excluded.
Sample size determination and sampling procedures
The sample size for this study was calculated using a single population proportion formula where, No = minimal sample size required, z = 1.96 (normal deviate corresponding to 95% confidence interval), w = 0.05 (degree of precision of 5%), P = .326 (a mortality rate of 32.6%; from the study conducted in Ethiopia (10).
Since the target population was less than 10 000, the exact sample size was adjusted as; nf = No/1 + No/N, where nf is the corrected sample size and N is obtained from the previous admission data from 2 hospitals (SPMMC = 229, JMC = 186), which was 415.
Then, by adding a 10% contingency value, the final sample size was 206 patients. Based on the previous admissions, this number was proportionally divided for both hospitals by the ratio of 1:1.24. Accordingly, 92 and 114 patients were allocated for JMC and SPHMMC, respectively. A consecutive sampling technique was used, and all consecutively admitted patients to the PICU from October 2020 to May 2021 were included based on the inclusion criteria.
Data collection tools and procedures
To ensure content validity, the data collection tool was adapted from previous related studies21,22 and patient charts were reviewed in accordance with the study’s objectives. The data were collected by 1 bachelor nurse and 1 clinical pharmacist recruited from each department who were working at SPHMMC and JMC after taking assent from the caregivers. Before beginning the data collection, data collectors received training on data collection. Clinical characteristics such as SBP, pupillary light reflex, oxygen saturation, and need for mechanical ventilation (MV) were assessed within the first hour and entered into an electronic application to calculate the Pediatric Index of Mortality 2 (PIM2) score. 23
Data quality assurance
Before the actual data collection, the questionnaire adapted from previous studies was translated to the local official languages (Amharic and Afan Oromo), and then back to the English version to ensure the data content. A pretest was done on 5% of a sample before the actual data collection to check the consistency and validity of the structured data collection format. The collected data were double-checked by the data collectors and principal investigator for completeness, accuracy, and clarity.
Data processing and analysis
Data were manually checked for completeness before being entered into Epi-data Manager version 4.6 and then into SPSS version 23 for statistical and survival analysis. Descriptive analysis was performed to recap baseline characteristics, and results were presented by the text, tables, and figures. Kaplan-Meier curves were computed to compare the survival status of patients. Bi-variable analysis was conducted, and variables having a P-value <.25 were considered candidates for multi-variable regression. A multi-variable cox proportional hazard model was performed to identify factors associated with in-ICU mortality. The hazard ratio was used to assess the strength of the association, and variables with a P-value of .05 were considered statistically significant.
Results
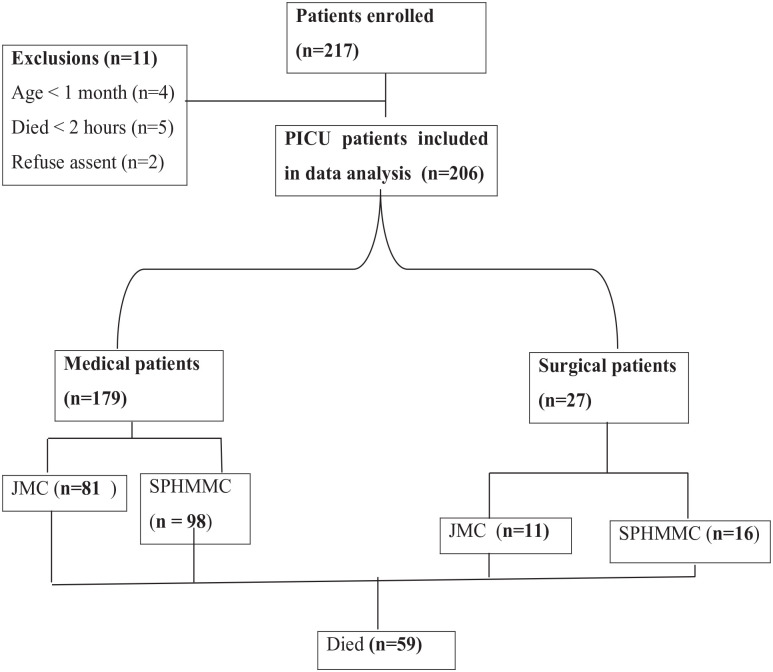
Out of 217 consecutive patients admitted to the pediatric ICU at JMC and SPHMMC over an 8 month period, 206 patients were included. Of these patients enrolled, 11 patients were excluded (age < 1 month = 4, died < 2 hours of ICU admission = 5, parent’s reject assent = 2). Finally, data from 206 patients were included in the study. A majority, 114 (55.3%) of the patients were from SPHMMC. Of the study participants, 179 (86.9%) were medical, and 27 (13.1%) were surgical admissions (Figure 1).
Figure 1.
Study flow chart (overview of the study participants).
Socio-demographic characteristics
Of the patients admitted, 113 (54.9%) were female, giving a male-to-female ratio of 1:1.2. The mean ± SD age of the patients admitted to the ICU was 55.9 ± 54.9 months. More than half, 124 (60.2%) of the patients were from a rural area, and 94 (45.6%) were admitted from the pediatric emergency department. Of all the patients analyzed, 38 (18.4%) were severely malnourished (<3 Z-score). The majority of patients were medical patients, which accounted for 179 (86.9%) and 157 (76.2%) new admissions. Regarding the vaccination status, 120 (58.3%) were fully vaccinated. The majority, 185 (89.8%) of the caregivers were parents and 80 (38.8%) had no formal education; and around 94 (45.6%) of them were farmers (Table 1).
Table 1.
Socio-demographic characteristics among patients admitted to PICU of selected tertiary care hospitals in Ethiopia, 2021 (N = 206).
| Socio demographic variables | Outcome n (%) | Frequency (%) | |
|---|---|---|---|
| Died | Survived | ||
| Study site | |||
| JMC | 27 (29.3) | 65 (70.7) | 92 (44.7) |
| SPHMMC | 32 (28.1) | 82 (71.9) | 114 (55.3) |
| Sex | |||
| Female | 30 (26.5) | 83(73.5) | 113 (54.9) |
| Male | 29 (31.2) | 64 (68.8) | 93 (45.1) |
| Age in months | |||
| 1-12 | 24 (33.8) | 47 (66.2) | 71 (34.5) |
| 13-60 | 15 (25.9) | 43 (74.1) | 58 (28.2) |
| 61-120 | 9 (20.9) | 34 (79.1) | 43 (20.9) |
| 121-168 | 11 (32.4) | 23 (67.6) | 34 (16.5) |
| Residence | |||
| Rural | 32 (25.8) | 92 (74.2) | 124 (60.2) |
| Urban | 27 (32.9) | 55 (67.1) | 82 (39.8) |
| Weight (kg) | |||
| (Mean ± SD) | 13.54 ± 10.6 | 15.3 ± 10.2 | |
| Patient category | |||
| Medical patient | 51 (28.5) | 128 (71.5) | 179 (86.9) |
| Surgical patient | 8 (29.6) | 19 (70.4) | 27 (13.1) |
| Source of admission | |||
| Pediatric EOPD | 24 (25.5) | 70 (74.5) | 94 (45.6) |
| Pediatric ward | 24 (30.4) | 55 (69.6) | 79 (38.3) |
| Surgical ward | 8 (32) | 17 (68) | 25 (12.1) |
| Referral | 3 (37.5) | 5 (62.5) | 8 (3.9) |
| Nutritional status | |||
| Normal | 47 (29.9) | 110 (70.1) | 157 (76.2) |
| Malnourished | 12 (24.5) | 37 (75.5) | 49 (23.8) |
| Vaccination status | |||
| Fully vaccinated | 38 (31.7) | 82 (68.3) | 120 (58.3) |
| Not vaccinated | 21 (24.4) | 65 (75.6) | 86 (41.7) |
| Frequency admission | |||
| Frist admission | 44 (28) | 113 (72) | 157 (76.2) |
| Readmission(⩾2) | 15 (30.6) | 34 (69.4) | 49 (23.8) |
| Caregiver’s | |||
| Parents | 55 (29.7) | 130 (70.3) | 185 (89.8) |
| Siblings | 2 (16.7) | 10 (83.3) | 12 (5.8) |
| Grandparents | 2 (22.2) | 7 (77.8) | 9 (4.4) |
| Caregiver’s education | |||
| No formal education | 25 (31.3) | 55 (68.7) | 80 (38.8) |
| Primary school (1-8) | 7 (19.4) | 29 (80.6) | 36 (17.5) |
| Secondary school (9-12) | 8 (25) | 24 (75) | 32 (15.5) |
| College/University | 19 (32.8) | 39 (67.2) | 58 (28.2) |
| Caregiver’s occupation | |||
| Farmer | 26 (27.7) | 68 (72.3) | 94 (45.6) |
| Merchant/labor work | 14 (29.8) | 33 (70.2) | 47 (22.8) |
| Employee (Govt./private) | 14 (31.8) | 30 (68.2) | 44 (21.4) |
| Others | 5 (23.8) | 16 (76.2) | 21 (10.2) |
Abbreviations: EOPD, emergency outpatient department; Govt., governmental; JMC, Jimma Medical Center; others, unemployed, students, and housewife; SD, standard deviation; SPHMMC, St. Paul’s Hospital Millenium Medical College.
Clinical profile of admitted patients
The most common cause of ICU admission was severe pneumonia, 35 (17%), followed by septic shock 32 (15.5%), and complicated meningitis 25 (12.1%) (Table 2). Regarding the consciousness level of patients at arrival at the ICU, 52 (25.2%) patients presented with severe impairment of consciousness. About 122 (59.2%) patients had oxygen saturation <90% at ICU admission. The mean ± SD of the PIM-2 score was 7.1 ± 5.93 with the majority of them, 135 (65.5%) being >5 scores. More than two-thirds, 142 (68.9%) of patients were mechanically ventilated. The median length of stay in the PICU was 5 (IQR: 3-9) days and the majority, 104 (50.5) of patients died within 7 days of ICU admission. About 48 patients (23.3%) developed complications during their ICU stay (Table 3).
Table 2.
Reason for admission among the study participants admitted to PICU of selected tertiary care hospitals in Ethiopia, 2021 (N = 206).
| Variables | Outcome n (%) | Frequency (%) | |
|---|---|---|---|
| Died | Survived | ||
| Reason for admission | |||
| Infectious | 37 (33) | 75 (67) | 112 (54.4) |
| Non-infectious | 22 (23.4) | 72 (76.6) | 94 (45.6) |
| Primary diagnosis | |||
| Severe pneumonia | 13 (37.1) | 22 (62.9) | 35 (17) |
| Severe sepsis/septic shock | 12 (37.5) | 20 (62.5) | 32 (15.5) |
| Complicated meningitis | 9 (36) | 16 (64) | 25 (12.1) |
| Congestive heart failure | 3 (13) | 20 (87) | 23 (11.2) |
| Post-operative | 3 (23.1) | 10 (76.9) | 13 (6.3) |
| Guillen Barrie syndrome | 3 (23.1) | 10 (76.9) | 13 (6.3) |
| Severe asthma | 1 (11.1) | 8 (88.9) | 9 (4.4) |
| Upper airway obstruction | 1 (14.3) | 6 (85.7) | 7 (3.4) |
| Traumatic brain injury | 2 (33.3) | 4 (66.7) | 6 (2.9) |
| Acute glomerulonephritis | 1 (16.7) | 5 (83.3) | 6 (2.9) |
| Disseminated tuberculosis | 2 (33.3) | 4 (66.7) | 6 (2.9) |
| Cardiogenic shock | 2 (40) | 3 (60) | 5 (2.4) |
| Diabetic ketoacidosis | 1 (20) | 4 (80) | 5 (2.4) |
| Status epileptics | 2 (40) | 3 (60) | 5 (2.4) |
| Miscellaneous conditions a | 4 (25) | 12 (75) | 16 (7.9) |
Miscellaneous conditions: bronchiolitis, down syndrome, hepatic failure, generalized tetanus, corpulmonale, severe malaria, and organophosphate poisoning.
Table 3.
Clinical characteristics of the study participants admitted to PICU of selected tertiary care hospitals in Ethiopia, 2021 (N = 206).
| Variables | Outcome n (%) | Frequency (%) | P-value | |
|---|---|---|---|---|
| Died | Survived | |||
| Organ dysfunction | ||||
| Yes | 51 (33.1) | 103 (66.9) | 154 (74.8) | .20 |
| No | 8 (15.4) | 44 (84.6) | 52 (25.2) | |
| Level of consciousness | ||||
| GCS > 8 | 36 (23.4) | 118 (76.6) | 154 (74.8) | .02 |
| GCS ⩽ 8 | 23 (44.2) | 29 (55.8) | 52 (25.2) | |
| Oxygen saturation (%) | ||||
| <90% | 45 (36.9) | 77 (63.1) | 122 (59.2) | .02 |
| 90%-100% | 14 (16.7) | 70 (83.3) | 84 (40.8) | |
| Use of MV | ||||
| Yes | 49 (34.5) | 93 (65.5) | 142 (68.9) | .05 |
| No | 10 (15.6) | 54 (84.4) | 64 (31.1) | |
| Patient’s access to airway | ||||
| ETT | 42 (35.3) | 77 (64.7) | 119 (83.8) | .65 |
| Tracheotomy | 7 (30.4) | 16 (70.6) | 23 (16.2) | |
| PIM2 score | ||||
| >5 | 45 (33.3) | 90 (66.7) | 135 (65.5) | .75 |
| ⩽5 | 14 (19.7) | 57 (80.3) | 71 (34.5) | |
| Length of stay on MV in days | ||||
| <2 | 22 (39.3) | 34 (60.7) | 56 (39.4) | .26 |
| 2-7 | 20 (33.3) | 40 (66.7) | 60 (42.3) | |
| >7 | 7 (26.9) | 19 (73.1) | 26 (18.3) | |
Abbreviations: ETT, endotracheal tube; GCS, Glasgow coma scale; MV, mechanical ventilation; PIM2, pediatric index of mortality 2.
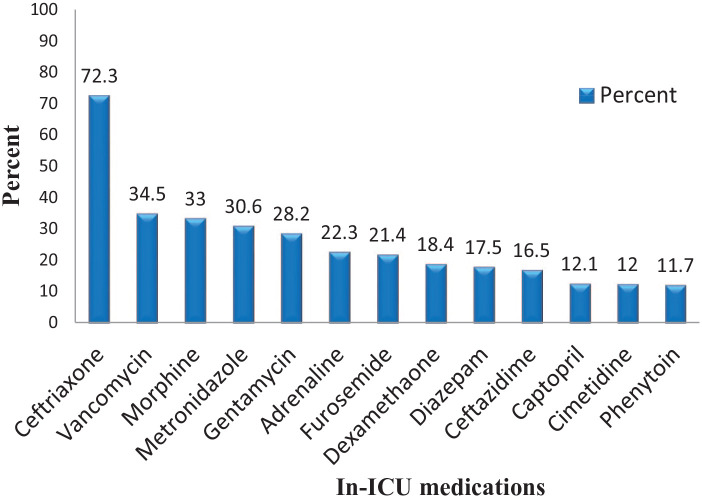
Type of treatment given during PICU Stay
Of medication prescribed in pediatric ICU, almost all patients were treated with different types of antibiotics 185 (89.8%), followed by fluid resuscitation 158 (76.7%), analgesics, 109 (52.9%), and nutritional treatments (Table 4). The majority, 149 (72.3%) of the patients were treated with ceftriaxone followed by vancomycin 71 (34.5%), morphine 68 (33%), and metronidazole 63 (30.6%) (Figure 2).
Table 4.
Distribution of type of treatments given during ICU stays among patients admitted to PICU of selected tertiary care hospitals in Ethiopia, 2021 (N = 206).
| Type of treatments given during ICU stays | Outcome n (%) | Frequency (%) | |
|---|---|---|---|
| Yes | No | ||
| Antibiotics | 56 (30.3) | 129 (69.7) | 185 (89.8) |
| Fluid therapy | 40 (25.3) | 118 (74.7) | 158 (76.7) |
| Analgesics | 28 (25.7) | 81 (74.3) | 109 (52.9) |
| Nutritional treatments | 20 (27.8) | 52 (72.2) | 72 (35) |
| Steroids | 11 (16.7) | 55 (83.3) | 66 (32) |
| Diuretics | 15 (23.6) | 42 (73.7) | 57 (27.7) |
| Sedatives | 9 (16.7) | 45 (83.3) | 54 (26.2) |
| Inotropes use | 15 (29.4) | 36 (70.6) | 51 (24.8) |
| Anticonvulsants | 11(30.6) | 25 (69.4) | 36 (17.5) |
| Stress-ulcer prophylaxis | 10 (28.6) | 25 (71.4) | 35 (17) |
| ACE-inhibitors | 2 (7.4) | 25 (92.6) | 27 (13.1) |
| Anti-asthmatic | 2 (10) | 18 (90) | 20 (9.7) |
| Anti-malarial | 4 (21.1) | 15 (78.9) | 19 (9.2) |
| Miscellaneous drug class a | 18 (26.9) | 49 (73.1) | 67 (32.5) |
Miscellaneous drug class: insulin, blood transfusion, thrombosis prophylaxis, antifungal, beta-blockers, anti-hypertensive, and anti-helminthics.
Figure 2.
Commonly prescribed specific medications during ICU stay among patients admitted to JMC and SPHMMC, from October 1 to May 30, 2021.
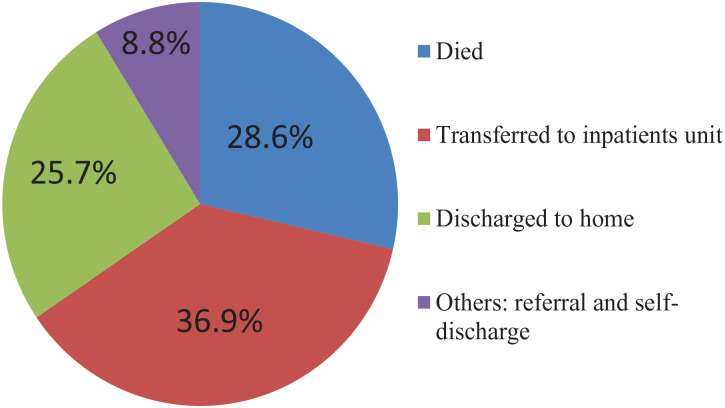
ICU outcomes and incidence of mortality
During the study period, 59 (28.6%) patients died in the PICU, however, 147 (71.4%) patients survived, and among them, the majority 76 (51.7%) were improved and transferred to the wards (Figure 3). Respiratory failure (32.2%) was the leading immediate cause of death in the PICU followed by septic shock (18.6%), cardiac arrest (11.9%), multi-organ failure (11.9%), and complicated meningitis (10.1%). Study subjects were followed during the study period, which gave a total of 1625 person-day observations (54.2 person-months), and the median LOS in the ICU was 3 (IQR: 1-9) days. Of the 206 participants, 59 (28.6%) died during the follow-up period. The incidence of mortality was 3.6 deaths per 100 person-day observations (95% CI: 2.04-5.04 deaths per 100 person-days). Among deaths reported, more than two-thirds (76.3%) died within 7 days, 13 (15.3%) died between 7 and 14 days and the remaining died after 2 weeks of admission (Table 5).
Figure 3.
Outcome at discharge among patients admitted to JMC and SPHMMC, from October 1 to May 30, 2021.
Table 5.
Causes of death among patients admitted to PICU of selected tertiary care hospitals in Ethiopia, 2021 (N = 206).
| Causes of death | Frequency (n = 59, %) |
|---|---|
| Respiratory failure | 19 (32.2) |
| Septic shock | 11 (18.6) |
| Cardiac arrest | 9 (15.3) |
| Multi organ failure | 7 (11.9) |
| Complicated meningitis | 6 (10.1) |
| Brain death | 5 (8.5) |
| GBS | 2 (3.4) |
| Total | 59 (100) |
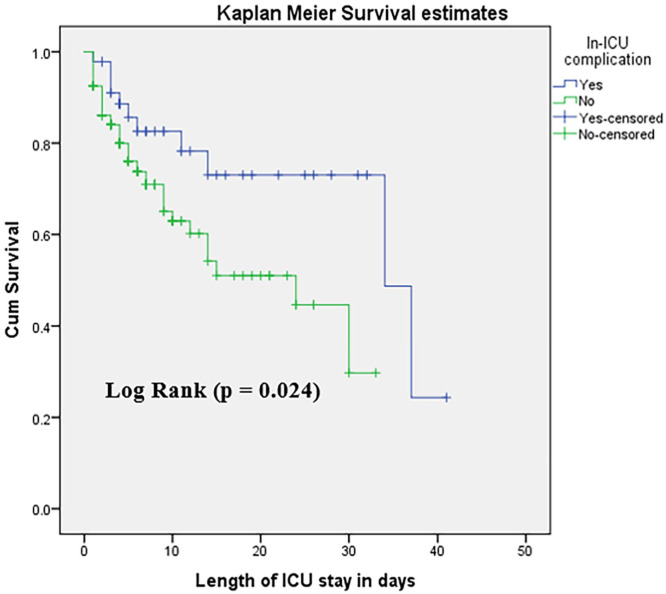
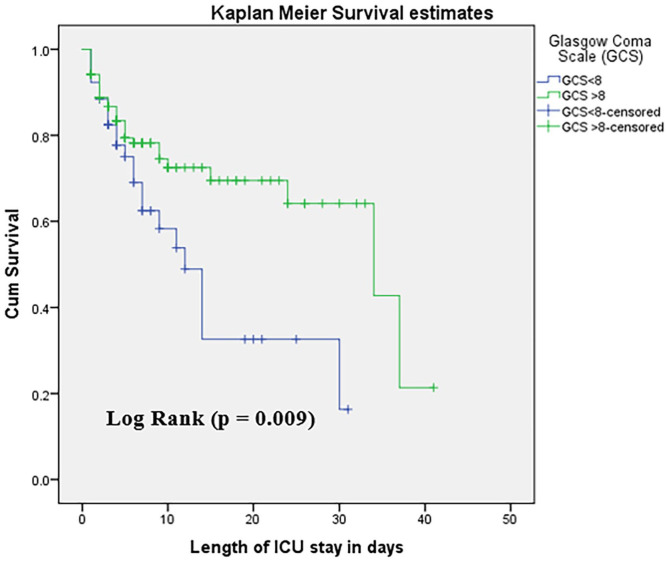
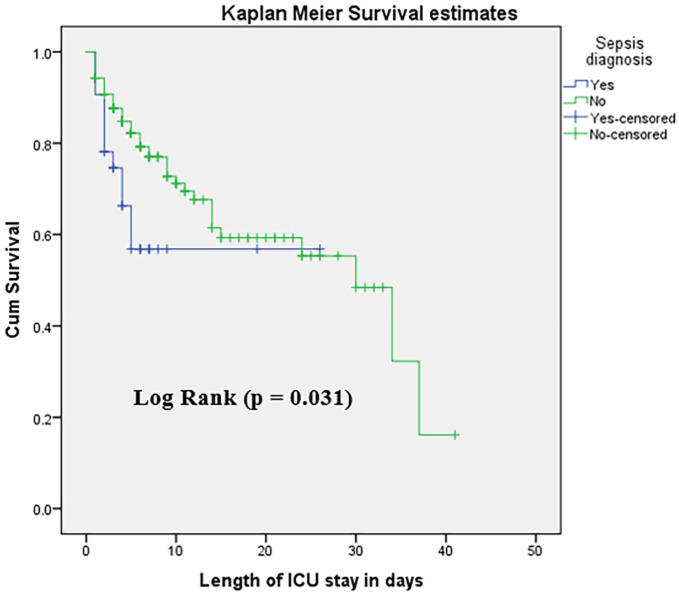
The (median ± SD) survival times among patients who develop complications and non-complicated were 34.0 ± 9.8, and 24.0 ± 6.5 days respectively (log-rank P = .024) (Figure 4). The (median ± SD) survival times among patients with GCS < 8 and GCS > 8 were 12 ± 1.8, and 34 ± 8.5 days respectively (log-rank P = .009) (Figure 5). The (median ± SD) survival times among patients with sepsis diagnosis and without sepsis diagnosis were 30 ± 3.76, and 30 ± 6.03 days respectively (log-rank P = .031) (Figure 6).
Figure 4.
Survival estimates for patients with complication and non-complicated after ICU admissions at JMC and SPHMMC, from October 1 to May 30, 2021.
Figure 5.
Survival estimates for patients with GCS < 8 and GCS > 8 in ICU admissions at JMC and SPHMMC, from October 1 to May 30, 2021.
Figure 6.
Survival estimates for patients with sepsis and non-sepsis diagnosis after at ICU of JMC and SPHMMC, from October 1 to May 30, 2021.
Generally, the differences in all variables at baseline between strata were determined using the log-rank (χ2) test, and the equality of hazard was assessed for the different explanatory variables. Kaplan Meier survival curve was plotted for ICU complications (P-value = .024), and GCS < 8 (P-value = .009) and sepsis diagnosis (P-value = .031) shows a significant difference (Figures 3–5).
Predictors of in-ICU mortality
Cox regression was done to identify the association between baseline characteristics and in-ICU mortality. Accordingly, sepsis diagnosis, sex, infectious disease, organ dysfunction, need for a mechanical ventilator, PIM2 score, patient use of sedative drugs, Oxygen saturation at admission, antibiotics use, GCS at admission, and complications in the ICU had a P-value of <.25. With a multivariate cox proportional hazard regression modeling, complications in the ICU (AHR: 2.13; 95% CI: 1.02, 4.42; P = .04), sepsis diagnosis (AHR: 2.43; 95% CI: 1.24, 4.78; P = .01), GCS < 8 (AHR: 1.96; 95% CI: 1.12, 3.43; P = .02), use of sedative drugs (AHR: 2.40; 95% CI: 1.16, 4.95; P = .02) were linked with increased risk of in-ICU mortality. The use of mechanical ventilation was associated with decreased mortality (AHR: 0.45; 95% CI: 0.21, 0.92; P = .04). Then, the hazard of mortality was 2 times higher for patients who developed complications in pediatric ICU (AHR: 2.13; 95% CI: 1.02, 4.42; P = .04) as compared with non-complicated patients. Also, the hazard of mortality was 2.40 times higher in patients who used sedative drugs (AHR: 2.40; 95% CI: 1.16, 4.95; P = .01) as compared with non-users of sedative drugs. Mortality was 55% lower for those who use mechanical ventilators during their ICU stay than for non-users of MV (AHR: 0.45; 95% CI: 0.21, 0.92) (Table 6).
Table 6.
Bivariate and multivariable Cox proportional hazard regression to identify predictors of in-ICU mortality at PICU of selected tertiary care hospitals in Ethiopia, 2021 (N = 206).
| Variables | Outcome | CHR (95% CI) | AHR (95% CI) | P-value | |
|---|---|---|---|---|---|
| Died | Survived | ||||
| Sex | |||||
| Female | 30 (26.5) | 83 (73.5) | 1.38 (0.82, 2.33) | 1.14 (0.65, 1.99) | .65 |
| Male | 29 (31.2) | 64 (68.8) | 1 | 1 | |
| Infectious disease | |||||
| Yes | 37 (33) | 75 (67) | 0.52 (0.28, 0.94) | 1.06 (0.57, 1.97) | .86 |
| No | 22 (23.4) | 71 (76.6) | 1 | 1 | |
| Sepsis diagnosis | |||||
| Yes | 12 (37.5) | 20 (62.5) | 0.50 (0.27, 0.96) | 2.43 (1.24, 4.78) | .01 |
| No | 47 (27) | 127 (73) | 1 | ||
| Organ dysfunction | |||||
| Yes | 51 (33.1) | 103 (66.9) | 0.60 (0.28, 1.26) | 1.06 (0.29, 3.98) | .94 |
| No | 8 (15.4) | 44 (84.6) | 1 | 1 | |
| GCS | |||||
| ⩽8 | 23 (44.2) | 29 (55.8) | 0.51 (0.30, 0.86) | 1.96 (1.12, 3.43) | .02 |
| >8 | 36 (23.4) | 118 (76.6) | 1 | 1 | |
| Oxygen saturation | |||||
| ⩽90% | 45 (36.9) | 77 (63.1) | 0.52 (0.28, 0.94) | 1.29 (0.62, 2.71) | .49 |
| >90% | 14 (16.7) | 70 (83.3) | 1 | 1 | |
| PIM2 score | |||||
| ⩾5 | 45 (33.3) | 90 (66.7) | 0.67 (0.37, 1.22) | 1.27 (0.53, 3.04) | .59 |
| >5 | 14 (19.7) | 57 (80.3) | 1 | 1 | |
| Antibiotics use | |||||
| Yes | 56 (30.3) | 129 (69.7) | 0.49 (0.15, 1.56) | 0.56 (0.17, 1.84) | .34 |
| No | 3 (14.3) | 18 (85.7) | 1 | 1 | |
| Use of MV | |||||
| Yes | 49 (34.5) | 93 (65.5) | 0.58 (0.29, 1.15) | 0.45 (0.21, 0.92) | .03 |
| No | 10 (15.6) | 56 (84.4) | 1 | 1 | |
| Sedative drugs use | |||||
| Yes | 9 (16.7) | 45 (83.3) | 2.41 (1.18, 4.92) | 2.40 (1.16, 4.95) | .02 |
| No | 50 (32.9) | 102 (67.1) | 1 | 1 | |
| In-ICU complications | |||||
| Yes | 11 (23.9) | 35 (76.1) | 2.13 (1.08, 4.57) | 2.13 (1.02, 4.42) | .04 |
| No | 48 (30) | 112 (70) | 1 | 1 | |
Abbreviations: AHR, adjusted hazard ratio; CHR, crude hazard ratio; CI, confidence interval; GCS, Glasgow coma scale; ICU, intensive care unit; MV, mechanical ventilation; PIM, pediatric index of mortality. Bold Variables with significant association.
Discussion
This study looked at the survival status and predictors of patients admitted to pediatric intensive care units at 2 Ethiopian tertiary care hospitals. The study is the first report from a 2-center prospective observational study in a PICU in Ethiopia that demonstrates that the mortality rate is high and identifies predictors of mortality such as complications in the ICU, use of sedative drugs, sepsis diagnosis, GCS < 8, and use of a mechanical ventilator.
In this study, the overall in-ICU mortality was 28.6%, with an incidence of 3.63 deaths per 100 person-day observations. This finding is consistent with the mortality rate in the studies conducted in Pakistan, (26.6%), 24 Egypt, (33.1%), 25 Mozambique, (25%), 7 Eritrea, (25.3%), 16 and Gonder (Ethiopia), (32.6%). 10 However, it is lower than the finding of a retrospective cross-sectional study done in Jimma (Ethiopia) from 2009 to 2013 (40%). 8 The difference could be attributed to the higher proportion of trauma patients admitted to their PICU compared with the present study. From the trauma, the head injury was the highest 8 with high risk of death. 26 Furthermore, the proportion of mortality in PICU in the present study was higher than the finding of a study conducted in Ayder Referral Hospital (Ethiopia), Iran, Pakistan, Nepal, and India (8.5%, 16.5%, 11.9%, 12.6%, and 14%), respectively.6,11,27-29
The higher proportion of deaths in our setting could be explained by the fact that this is a tertiary center, which accepts referrals from distant locations, resulting in delayed presentation, and most of the patients were seriously ill when admitted to the setting. This may also be due to the insufficient mechanical ventilator in the present setting for those in need. Furthermore, the lack of a high dependency unit in the study area could be one of the factors contributing to the higher rate of ICU mortality.
A higher proportion of death was reported among patients with infectious diseases (17.9%) versus non-infectious (10.7%). This finding is in line with most of the studies conducted in developing countries, in which more than half of deaths were attributed to infectious diseases.7,9,10,27 This could be because of low socioeconomic levels, 30 poor hygiene, 31 and the inaccessibility of health care facilities in developing settings. However, several findings from developed countries reported non-infectious disease as the most common cause of death.11-13
The present study showed that respiratory failure was the leading cause of death, accounting for (32.2%) of total deaths, followed by septic shock (18.6%), and cardiac arrest (11.9%), and complicated meningitis (10.1%). This finding is comparable with the study conducted in Mozambique, Gonder (Ethiopia), Iran, Bangladesh, and India.7,10,11,32,33 Contrary to our findings, the leading cause of death was the withdrawal of life-sustaining treatments in the study done in the US, 13 trauma in a study done in Jimma, 8 and renal failure in the study conducted in Eritrea. 16 This disparity could be attributed to differences in the reason for admission, and in the current study, severe pneumonia was the primary reason for admission, which causes respiratory failure. 34
The mean (±SD) length of stay in PICU was 7.87 ± 7.86 days with (59.7%) of patients staying within 2 to 7 days of ICU admission in our study. This finding is consistent with the study conducted in Rwanda (6.8 ± 8.5 days), 9 and Nepal (6.3 days), 35 but on contrary to a study done in Pakistan (4.11 ± 1.88 day). 24 The difference in mean length of stay might be due to variation in admission patterns; the quality of care delivered to the patients in the ICU, and in-ICU complications, which might be one of the contributing factors to the higher length of ICU stay.
This study also identified the independent predictors of in-ICU mortality. Hence, the presence of in-ICU complications, a sepsis diagnosis, a GCS < 8, and the use of sedative drugs were found to be independent predictors of mortality at the PICU, while the use of a mechanical ventilator was associated with a lower risk of mortality. Patients who developed complications during their ICU stay were 2 times more likely to die than those without complications (P = .04). There is no published study for comparison purposes. However, this could be because complications are associated with an increased probability of death because of the double burden on initial illnesses. This study indicated that the mortality risk was 2.40 times higher in patients taking sedatives (P = .02). This is comparable to the study conducted in Rwanda, 9 Greece, 11 and Harvard Children’s Hospital, Boston 36 ; in which the use of the sedative drug was correlated with an increased risk of in-ICU mortality. This might be due to sedation leaving the patient at risk of needing prolonged respiratory support, specifically mechanical ventilator, prolonged ICU stays, and also putting critically ill patients at high risk of developing ICU-acquired complications.9,11,36
Children admitted with a reduced level of consciousness (GCS < 8) had a nearly 2-fold increased risk of mortality than those admitted with a higher level. This is consistent with the findings of studies done in Iran. 11 The child who was diagnosed with sepsis had a higher risk of mortality than those who were not. This finding was consistent with other studies conducted in Iran. 37 This could be because patients with severe sepsis have a low reserve of physiologic function.
The in-ICU mortality was 55% lower for those who use a mechanical ventilator during their ICU stay than non-users. This finding was in contrast with a study conducted in TASH, 19 and Gonder (Ethiopia), 10 in which the use of a mechanical ventilator was significantly correlated with an increased risk of in-ICU mortality. The possible justification could be related to the most common cause of admission in the present study which was severe pneumonia and could lead to acute respiratory distress syndrome (ARDS). Most patients with ARDS benefit from MV. 38
Though this study is a prospective 2-center study conducted in a resource-limited country, it has some limitations. First, the income of caregivers that might influence the survival status of pediatric patients was not assessed because it was difficult to ascertain since the majority of admissions were from rural areas and caregivers usually underreported the assets they had. Second, the PIM2 score was based on 8 out of 10 parameters because there was no arterial blood gas analyzer in our PICU during the study period. Finally, the sample size is small, which may affect the power of the study.
Conclusion
The study found a high incidence of in-ICU mortality among pediatric patients in selected Ethiopian tertiary care hospitals. Respiratory failure, septic shock, and cardiac arrest were the common causes of admission and death. In-ICU complications, sepsis diagnosis, GCS < 8, and use of sedative drugs were linked with an increased risk of in-ICU mortality in contrast to the use of a mechanical ventilator. Therefore, prudent follow-up is warranted for those patients with the forementioned risk factors.
Acknowledgments
The authors would like to acknowledge Jimma University and St. Paul’s Hospital Millennium Medical College for the support during this study.
Footnotes
ORCID iDs: Mesay Dechasa Gudeta  https://orcid.org/0000-0002-3222-1049
https://orcid.org/0000-0002-3222-1049
Tamirat Bekele Beressa  https://orcid.org/0000-0001-9497-3388
https://orcid.org/0000-0001-9497-3388
Getandale Zeleke Negera  https://orcid.org/0000-0002-0178-5888
https://orcid.org/0000-0002-0178-5888
Declarations
Ethics Approval and Consent to Participate: The study was done in accordance with the Declaration of Helsinki. An ethical clearance letter was obtained from the institutional review board of Jimma University (reference No: IRB000234/2012) and St. Paul’s Hospital Millennium Medical College (reference No: PM23/200). Then, a letter of cooperation was taken from each pediatrics and child health department of the hospital. Informed verbal consent was obtained from the caretakers. The name of the patient was not recorded on the data collection form, and all information taken from the chart was kept strictly confidential, and the data retrieved was used only for the study.
Consent for publication: Not applicable.
Authors’ contributions: AJB contributed to the conceptualization, methodology, investigation, data curation, formal analysis, and drafting of the original manuscript. DAG, MDG, and TBB contributed to data curation, formal analysis, and the writing of the original draft. GZN has contributed to the conceptualization, formal analysis, methodology, and supervision of the study. All authors read and approved the final manuscript.
Funding: None
The authors declare that they have no competing interests.
Availability of Data and Materials: All the data have been included in the study, and if any raw data is needed, it will be obtained by contacting the corresponding author.
References
- 1.Marshall JC, Bosco L, Adhikari NK, et al. What is an intensive care unit? A report of the task force of the World Federation of Societies of intensive and Critical Care Medicine. J Crit Care. 2017;37:270-276. [DOI] [PubMed] [Google Scholar]
- 2.Klieg R.M., GEME J. S.Overview of pediatrics. Nelson Textbook of Pediatrics. 21st ed. Elsevier Saunders; 2020:1-9. [Google Scholar]
- 3.Ezbakhe F, Pérez-Foguet A.Child mortality levels and trends. Demogr Res. 2020;43:1263-1296. [Google Scholar]
- 4.Vincent J-L, Marshall JC, Namendys-Silva SA, et al. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014;2:380-386. [DOI] [PubMed] [Google Scholar]
- 5.Riviello ED, Letchford S, Achieng L, Newton MW.Critical care in resource-poor settings: lessons learned and future directions. Crit Care Med. 2011;39:860-867. [DOI] [PubMed] [Google Scholar]
- 6.Haftu H, Hailu T, Medhaniye A, G/Tsadik T. Assessment of pattern and treatment outcome of patients admitted to pediatric intensive care unit, Ayder referral hospital, Tigray, Ethiopia, 2015. BMC Res Notes. 2018;11:339-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Punchak M, Hall K, Seni A, et al. Epidemiology of disease and mortality from a PICU in Mozambique. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2018;19:e603-e610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abebe T, Girmay M, Tesfaye M.The epidemiological profile of pediatric patients admitted to the general intensive care unit in an Ethiopian university hospital. Int J Gen Med. 2015;8:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nyirasafari R, Corden MH, Karambizi AC, et al. Predictors of mortality in a paediatric intensive care unit in Kigali, Rwanda. Paediatr Int Child Health. 2017;37:109-115. [DOI] [PubMed] [Google Scholar]
- 10.Teshager NW, Amare AT, Tamirat KS.Incidence and predictors of mortality among children admitted to the pediatric intensive care unit at the University of Gondar comprehensive specialised hospital, northwest Ethiopia: a prospective observational cohort study. BMJ Open. 2020;10:e036746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Valavi E, Aminzadeh M, Shirvani E, Jaafari L, Madhooshi S.The main causes of mortality in pediatric intensive care unit in south west of Iran. Zahedan J Res Med Sci. 2018;20:1-4 [Google Scholar]
- 12.Volakli E, Sdougka M, Tamiolaki M, Tsonidis C, Reizoglou M, Giala M.Demographic profile and outcome analysis of pediatric intensive care patients. Hippokratia. 2011;15:316-322. [PMC free article] [PubMed] [Google Scholar]
- 13.Burns JP, Sellers DE, Meyer EC, Lewis-Newby M, Truog RD.Epidemiology of death in the PICU at five U.S. teaching hospitals. Crit Care Med. 2014;42:2101-2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adedokun ST, Yaya S.Childhood morbidity and its determinants: evidence from 31 countries in sub-Saharan Africa. BMJ Glob Health. 2020;5:e003109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. Newborns: Improving Survival and Well-Being. Geneva: World Health Organization; 2020. [Google Scholar]
- 16.Mohammed M.Patterns and treatment outcomes of pediatric intensive care unit admissions in 2013, Orotta national referral hospital, Asmara, Eritrea. [Google Scholar]
- 17.Ongóndi M, Mwachiro M, Ranketi S.Predictors of mortality in a critical care unit in south western Kenya. Ann Afr Surg. 2016;13:1-4. [Google Scholar]
- 18.Institute EPH and ICF. Ethiopia mini demographic and health survey 2019: key indicators. J Chem Inf Model. 2019;53:1689-1699. [Google Scholar]
- 19.Abebe A, Adal O, Noah Y. Disease pattern, outcome, and associated factor of patient admitted in pediatric intensive care unit at Tikur Anbessa specialized hospital, 2022: retrospective study. 2022. [Google Scholar]
- 20.Tazebew AA, Cahkilu B, Bacha T.Admission pattern and outcome in a pediatric intensive care unit of Gondar university hospital. Ethiop Med J. 2019;57: 111-115. [Google Scholar]
- 21.Abate SM, Assen S, Yinges M, Basu B.Survival and predictors of mortality among patients admitted to the intensive care units in southern Ethiopia: a multi-center cohort study. Ann Med Surg. 2021;65:102318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yeshaneh A, Tadele B, Dessalew B, et al. Incidence and predictors of mortality among neonates referred to comprehensive and specialized hospitals in Amhara regional state, North Ethiopia: a prospective follow-up study. Ital J Pediatr. 2021;47:186-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shukla V, Nimbalkar S, Phatak AG, Ganjiwale JD.Critical analysis of PIM2 score applicability in a tertiary care PICU in Western India. Int J Pediatr. 2014;20144:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Basheer F, Nayyar ZA, Butt AI.Clinical profile and outcome in a paediatric intensive care unit of a tertiary care hospital in Pakistan. PAFMJ. 2020;70:1657-1661. [Google Scholar]
- 25.Rady HI.Profile of patients admitted to pediatric intensive care unit, Cairo University Hospital: 1-year study. Ain Shams J Anaesthesiol. 2014;7:500. [Google Scholar]
- 26.McMillan TM, Teasdale GM, Weir CJ, Stewart E.Death after head injury: the 13 year outcome of a case control study. J Neurol Neurosurg Psychiatry. 2011;82:931-935. [DOI] [PubMed] [Google Scholar]
- 27.Haque A, Siddiqui NR, Jafri SK, Hoda M, Bano S, Mian A.Clinical profiles and outcomes of children admitted to the pediatric intensive care unit from the emergency department. Pak J Coll Physicians Surg Pakistan. 2015;25:301. [PubMed] [Google Scholar]
- 28.Shah GS, Shah BK, Thapa A, Shah L, Mishra O.Admission patterns and outcome in a pediatric intensive care unit in Nepal. Br J Med Med Res. 2014;4:4939-4945. [Google Scholar]
- 29.Roy SM, Basu S, Roy BC, Datta S.Clinical profile and outcome of patients admitted to pediatric intensive care unit of a tertiary care teaching hospital in Eastern India. J Med Sci Clin Res. 2018;6:1071-1075. [Google Scholar]
- 30.Andrist E, Riley CL, Brokamp C, Taylor S, Beck AF.Neighborhood poverty and pediatric intensive care use. Pediatrics. 2019;144:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Freeman MC, Garn JV, Sclar GD, et al. The impact of sanitation on infectious disease and nutritional status: a systematic review and meta-analysis. Int J Hyg Environ Health. 2017;220:928-949. [DOI] [PubMed] [Google Scholar]
- 32.Hoque MS, Masud M, Ahmed A.Admission pattern and outcome in a paediatric intensive care unit of a tertiary care paediatric hospital in Bangladesh–a two-year analysis. DS (Child) HJ. 2012;28:14-19. [Google Scholar]
- 33.Mukhija DG, Chandra DS, Prasad DP.Clinical profile of patients admitted to the PICU of a tertiary care teaching hospital. Pediatr Rev Int J Pediatr Res. 2017;4:125-127. [Google Scholar]
- 34.Confalonieri M, Potena A, Carbone G, Porta RD, Tolley EA, Umberto Meduri G.Acute respiratory failure in patients with severe community-acquired pneumonia: a prospective randomized evaluation of noninvasive ventilation. Am J Respir Crit Care Med. 1999;160:1585-1591. [DOI] [PubMed] [Google Scholar]
- 35.Shrestha AK, Bhattarai S, Paudel P, Basel PL.Morbidity and mortality pattern of patients admitted into paediatric intensive care unit of tertiary level hospital of Nepal. J Nepal Paediatr Soc. 2020;40:28-33. [Google Scholar]
- 36.Egbuta C, Mason KP.Current state of analgesia and sedation in the pediatric intensive care unit. J Clin Med. 2021;10:1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aljabari S, Balch A, Larsen GY, Fluchel M, Workman JK.Severe sepsis-associated morbidity and mortality among critically ill children with cancer. J Pediatr Intensive Care. 2019;8:122-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rittayamai N, Brochard L.Recent advances in mechanical ventilation in patients with acute respiratory distress syndrome. Eur Respir Rev. 2015;24:132-140. [DOI] [PMC free article] [PubMed] [Google Scholar]