Abstract
Introduction
The advent of digital systems and global mobile phone availability presents an opportunity for better healthcare access and equity. However, the disparity in the usage and availability of mHealth systems between Europe and Sub-Saharan Africa (SSA) has not been explored in relation to current health, healthcare status, and demographics.
Objective
This study aimed to compare mHealth system availability and use in SSA and Europe in the above-mentioned context.
Methods
The study analyzed health, healthcare status, and demographics in both regions. It assessed mortality, disease burden, and universal health coverage. A systematic narrative review was conducted to thoroughly assess available data on mHealth availability and use, guiding future research in the field.
Results
SSA is on the verge of stages 2 and 3 in the demographic transition with a youthful population and high birth rate. Communicable, maternal, neonatal, and nutritional diseases contribute to high mortality and disease burden, including child mortality. Europe is on the verge of stages 4 and 5 in the demographic transition with low birth and death rates. Europe's population is old, and non-communicable diseases (NCDs) pose major health challenges. The mHealth literature adequately covers cardiovascular disease/heart failure, and cancer. However, it lacks approaches for respiratory/enteric infections, malaria, and NCDs.
Conclusions
mHealth systems in SSA are underutilized than in Europe, despite alignment with the region's demographics and major health issues. Most initiatives in SSA lack implementation depth, with only pilot tests or small-scale implementations. Europe's reported cases highlight actual implementation and acceptability, indicating a strong implementation depth of mHealth systems.
Keywords: Demography, Europe, healthcare, mHealth, Sub-Saharan Africa
Introduction
Three of the eight Millennium Development Goals (MDGs) are specifically related to health 1 as follows: MDG 4: reduce child mortality, MDG 5: improve maternal health, and MDG 6: combat HIV/AIDS and malaria. Unsurprisingly, the three goals are aimed at the main health issues of developing countries. 2 Like in the MDGs, health plays an important role in the 2030 agenda on Sustainable Development Goals (SDGs); especially in SDG 3: “Ensure healthy lives and promoting well-being for all at all ages”. 3 The important detail to note is the addition of “at all ages” in the title, considering all ages including aging that could be the future problem in developing countries. The most straightforward indicator for the health status of a population is mortality-based estimates. 4 However, mortality alone does not fully encompass the health status, often referred to as the “burden of disease”, of a population5,6 The overall burden of disease is assessed using the disability-adjusted life year (DALY).7,8 Similarly, the top two indicators for measuring healthcare are the health worker density and distribution and the coverage of essential health services. 9 One available metric to track progress on this is the universal health coverage (UHC) index. The UHC index is the geometric mean of 14 indicators measuring the coverage of essential services including reproductive, maternal, newborn and child health, infectious diseases, non-communicable diseases (NCDs), and service capacity and access, among the general population and the most disadvantaged population. It is also one of the indicators used to track SDG target.10,11 As of 15 November 2022, the world population is projected to reach 8 billion as a result of the great acceleration.12,13 The consumption of energy, resources, land, food, etc. also increased quickly in tandem with this explosive population growth. 14
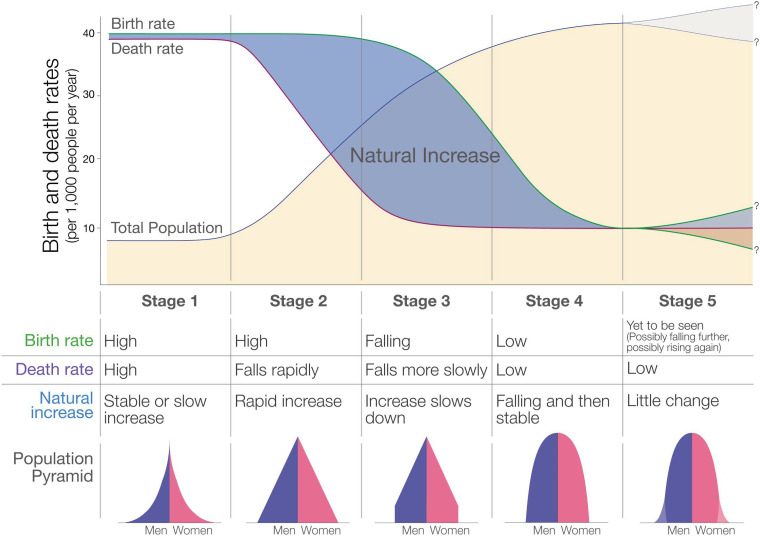
Demographic transition model
Natural growth of the world population is only determined by the number of births; and the number of deaths (mortality). 15 However, birth rate and mortality alone do not tell the whole story. If both decline at the same time, the world population would not increase. The clue here is the timing at which those changes in birth rate and mortality happen. This rapid growth of the world population can be explained by the demographic transition model that contains five stages. 16 It is an elegant, empirically determined model that describes the observed pattern of demographic transition in countries around the world. Each stage is characterized by a specific birth rate and mortality, which is reflected in the associated age structure of that population. Each stage in this demographic transition comes with its typical health issues. Generally, in the early stages of the demographic transition model, which is characterized by young generation, crude death rates are high due to diseases, epidemics, famine, lacking hygiene, lack of food, poor education, and insufficient healthcare. As medical care, hygiene and access to food improve, life expectancy increases in the middle stages. However, child mortality still remains high in these young populations due to inadequate healthcare. At the later stages, as the population grows older, ageing becomes a problem. From empirical evidence, it is clear that the demographic transition model can be applied to any country or region but not all countries go through the different stages at the same time or at the same rate. Future population growth 17 mainly depends on how fertility—the number of children per woman—will evolve. 18 To have a stable, sustainable population in the future when mortality is decreasing, fertility also needs to decrease. 19 Empirical evidence and theoretical explanation indicate that a reduction in child mortality is the key to a sustainable, developed future population. While this might not be very obvious at first glance, indeed, there is a causal relationship between child mortality and fertility—the number of children born per woman during reproductive years, regardless of pregnancy outcome. Countries with a low child morality typically have one to four children per woman. Countries with higher child mortalities have four to six children per woman. 17 The two theories that can support these are the child replacement theory in which parents that have lost a child might deliberately decide to have additional child shortly after, and the other is the insurance or hoarding effect in which when mortality is high, prudent couples will try to overshoot their actual target family size to ensure a minimum number of surviving children that eventually reach adulthood. As a result, It is argued that population growth can be halted by ensuring the survival of children.20,21 Mortality changes have a large impact on fertility reductions and can account for a major part of the fertility change characterizing demographic transitions.
mHealth: a solution to our health problems?
The introduction of digital systems and mass availability and use of mobile phones globally opens a new opportunity for provision of improved access and equity to healthcare service. At the end of 2018, 5.1 billion people across the world owned a mobile device subscription, and it is estimated that by 2025, this number will grow to 5.8 billion. 22 Hence, mHealth applications provide a significant potential of technologies to be integrated into clinical services to support quality medical care worldwide. The World Health Organization (WHO) defines mobile health (mHealth) as the use of mobile wireless technologies for public health. 23 The added value of mHealth is that it can support new models of care by surpassing geographical and temporal barriers and can contribute to the sustainability of healthcare systems. 24 By offering creative and affordable alternatives for healthcare delivery, removing financial and geographic constraints, and enhancing health literacy and awareness, digital health has the potential to promote equity and access to healthcare services.25,26,27 It is clear that, now more than ever, mHealth can be a solution to many of the healthcare challenges present today. 28
The problem with the world ever growing population is that there is a physical limit to the number of people that can inhabit our planet. Already, some urban regions on our planet are becoming overcrowded. This overcrowding puts general health and well-being of the people who live there at risk. To make matters worse, social distancing required as a result of recent COVID-19 made face-to-face consultation and care-taking impossible in many instances.29,30 In addition to the problems stated above, the COVID-19 pandemic further impacted health worker density. Additionally, COVID-19 claimed the lives of 115,000 front-line healthcare workers. 31
Even though we are on the era of enhancement of digitalizing the global healthcare system, there is a huge gap between the availability and use of mHealth systems in the developed world and the developing world. The main aim of this study is to describe these differences in the availability and use of mHealth systems between Europe and Sub-Saharan Africa (SSA) in the context of current health, healthcare status, and demographic structure.
Methods
Health status
To assess the health status of SSA as a representative of a developing region and Europe as a representative of a developed region, we look at the current data on three different indicators. The most straightforward indicator for health status of a population is mortality. For both SSA and Europe, we look at what the share of deaths is by each cause, to identify the major causes of mortality. For both SSA and Europe, we have a look at the major causes of DALYs. We investigate whether the target for child mortality is reached in the different countries of SSA and Europe. We also investigate the major causes of child mortality in both regions.
Healthcare
To assess the healthcare status of SSA and Europe, we look at the current data on two different indicators. The first indicator is the health worker density, typically given per 1000 or 10,000 people. We look at the density of four different categories of health workers: medical doctors; nurses and midwifes; dentists; and pharmacists. The second indicator we look at is the UHC index which is a composite indicator comprising 14 measures of essential service coverage, including reproductive, maternal, newborn and child health, infectious and NCDs, service capacity, and access. It is calculated as a geometric mean and is used to track progress towards achieving the SDG target, particularly among the general and most vulnerable populations.10,11 The UHC index of the different countries in both SSA and Europe was investigated as well as the mean number of the UHC index for both regions.
Demographic analysis of SSA and Europe
Demographic analysis
In the demographic analysis, the most recent numbers or estimates for several demographic parameters were presented and discussed. The data was retrieved from the databases of the United Nations, the World Bank, and Our World in Data. The first parameter investigated was the total population of SSA and Europe. We look at how the total population has changed since 1950. We look at the most recent estimation of total population. Finally, we take a look at the projections for the total population in the years to come, up until 2100. The second and third parameters investigated were the crude birth rate and the crude death rate. Again, we look at how both, birth and death rates, have changed since 1950; what the current birth and death rates are; and the projections of the change of these rates up until 2100. When looking at these two parameters, we indirectly also look at another parameter, which is natural growth. Natural growth is the difference between birth rate and death rate. The fourth parameter we investigated was the current demographic age structure of both regions. This is done by looking at the so called ‘population pyramids’ of both regions. The final parameter that is investigated is the fertility rate, or the number of children per woman. Again, we look at how the fertility rate has changed since 1950; the current fertility rates; and how these rates are projected up until 2100. Since there is a relationship between fertility and child mortality, we take the opportunity to look at the current fertility and child mortality rates for the different countries in both regions.
Placement within the demographic transition model
With the information retrieved in the demographic analysis of SSA and Europe, it was pinpointed in which stage both regions are located within the demographic transition model and which stage they will go through in the years to come.
Availability and use of mHealth systems
A narrative review using a systematic approach is carried out to give a thorough assessment of the available data and to assist in directing future research in mHealth. The literature search used four databases: Scopus, Web of Science, IEEE Xplore, and PubMed. The search query was (“Mobile health” OR mHealth OR telehealth OR telemedicine OR “Wearable devices”) AND (“Sub Saharan Africa”) AND (Use* OR Practice OR Implementation* OR Enactment OR Application OR Operation OR Employment OR Execution OR Development OR Growth OR Expansion OR Advance OR Progress OR Change). Identical search is used for Europe, except replacing ''Europe'' instead of “Sub Saharan Africa”.”. Only articles published in 2000 and later were presented as results for both search searches. Each database was last searched on 20 December 2021. The title and abstract were successively screened by two reviewers. Table 1 lists the inclusion criteria that were applied during the screening procedure. All overarching studies and systematic reviews that discussed mHealth systems in SSA and Europe (or parts of those regions) were used for retrieving the data with respect to the availability and use of mHealth system and to compare them with the current health, health status, and demographic structure of SSA and Europe.
Table 1.
Inclusion criteria for paper selection.
| Inclusion criteria |
|---|
| 1. The paper is a systematic review and/or overarching study in SSA and Europe. |
| 2. mHealth is addressed as a primary issue. |
| 3. mHealth implementation and feedback are discussed in the paper. |
| 4. The mHealth approach is towards human domain. |
| 5. The mHealth approach is directly for patients (not for educating nurses, doctors, etc.). |
As the study is a review employing secondary data from published articles and databases, obtaining patient consent was deemed unnecessary. It was ensured that no identifiable patient information was included in the utilized data.
Results
Health status
Mortality
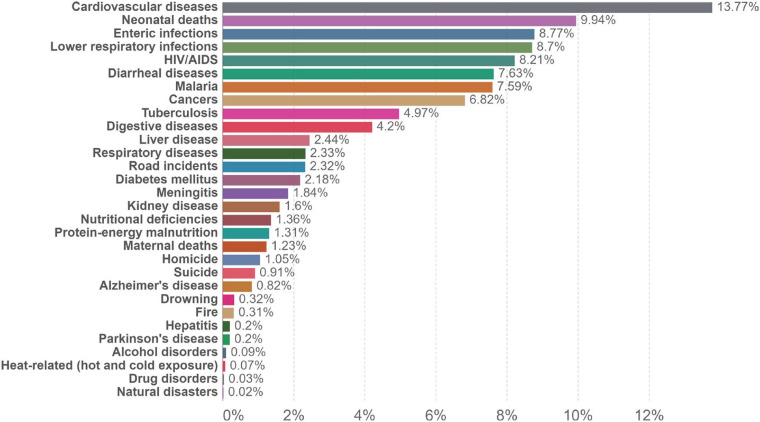
The share of deaths by each cause for SSA and Europe in the year 2019 can be seen in Figures 1 and 2, respectively. In SSA, the leading cause of death are cardiovascular diseases (CVDs), accounting for 13,77% of total deaths. If we have a look at the rest of the top 10 causes of death, we see that their shares are relatively close together, ranging from 9,94% to 4,20% of total deaths. The causes are, in descending order of their share, neonatal diseases, enteric infections, lower respiratory infections, human immunodeficiency viruses (HIVs)/acquired immunodeficiency syndrome (AIDS), diarrheal diseases, malaria, cancers, tuberculosis, and digestive diseases.
Figure 1.
Share of deaths by cause, SSA, 2019. 32 (CC BY 4.0). https://creativecommons.org/licenses/by/4.0/deed.en_US.
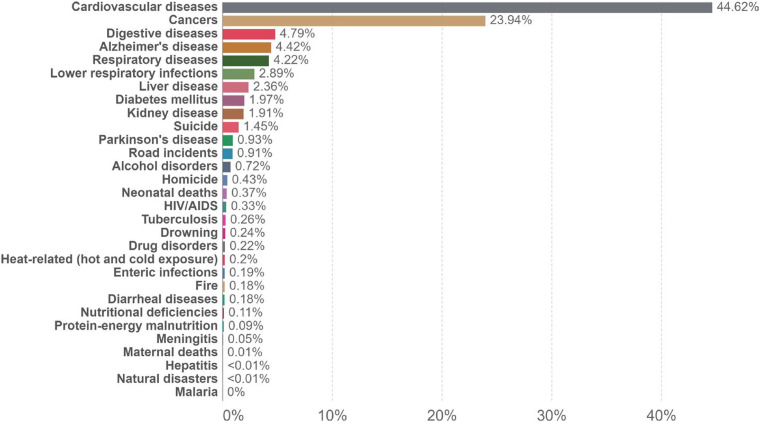
Figure 2.
Share of deaths by cause, Europe, 2019. 32 (CC BY 4.0). https://creativecommons.org/licenses/by/4.0/deed.en_US.
In Europe, CVDs are the major cause of death, accounted for an astonishing 44,62% of total death. Cancers are the second major cause with 23,94%; following these are digestive diseases, Alzheimer's disease, and respiratory diseases, each accounting for almost 5% of total deaths. Except for lower respiratory infections and suicides, all causes of death in the top 10 are NCDs.
Burden of disease
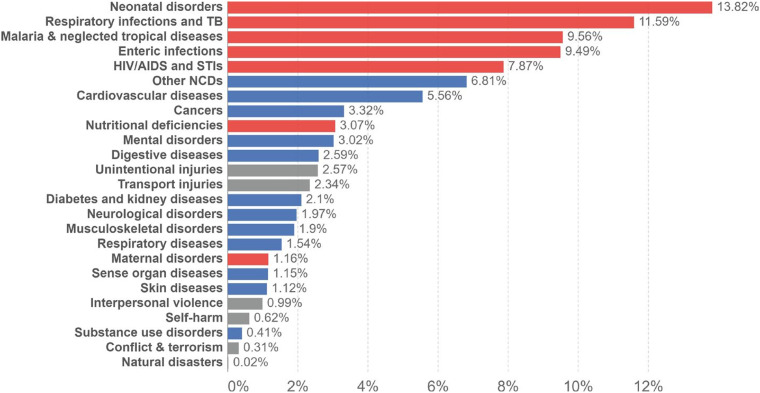
The share of DALYs by cause in 2019 for both SSA and Europe can be found in Figures 3 and 4, respectively. In both figures, the disease burden is divided into three categories: NCDs); communicable, maternal, neonatal, and nutritional diseases; and injuries. The number one cause of disease burden in SSA is neonatal disorders (13,82%), followed by respiratory infections and tuberculosis (TB) (11,59%); malaria and neglected tropical diseases (9,49%); and enteric infections and HIV/AIDS and sexually transmitted infections (STIs) (7,87%).
Figure 3.
Share of total disease burden (measured in DALYs) by cause, SSA, 2019. 32 (CC BY 4.0). (https://creativecommons.org/licenses/by/4.0/).
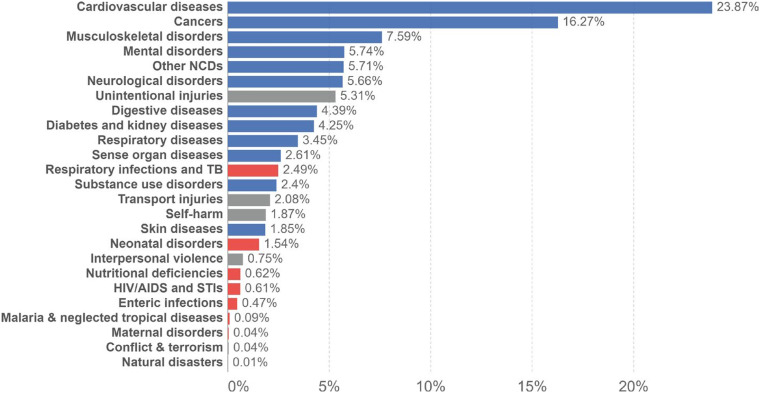
Figure 4.
Share of total disease burden (measured in DALYs) by cause, Europe, 2019. 32 (CC BY 4.0). (https://creativecommons.org/licenses/by/4.0/).
Child mortality
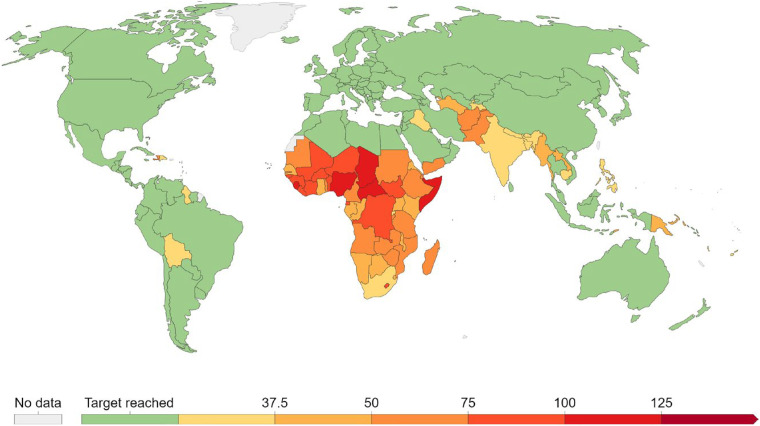
The countries where the SDG target of under-5 mortality being as low as 25 per 1000 live births is reached are identified separately. The remaining countries are catagorized based on their child mortality rates, using varying level of gradation as shown in the Figure 5.
Figure 5.
Under-5 mortality (per 1000), 2020. 32 (CC BY 4.0). https://creativecommons.org/licenses/by/4.0/deed.en_US.
Based on color alone, one can easily identify SSA on the world map. The average under-5 mortality in SSA is 73 per 1000. 33 When looking at Europe, we see that all countries have reached the SDG target of under-5 mortality being as low as 25 per 1000 live birth. The average under-5 mortality in Europe is 4 per 1000. 33 Child mortality is still so high in SSA.
Healthcare
Health worker density
The most recent numbers of each subdivision of health worker density are given in Table 2.
Table 2.
Health worker density (per 10,000), 2020. 34
| SSA | Europe | |
|---|---|---|
| Nursing and midwifery personnel | 12,89 | 83,41 |
| Medical doctors | 2,92 | 36,61 |
| Pharmacists | 0,80 | 6,47 |
| Dentists | 0,33 | 6,20 |
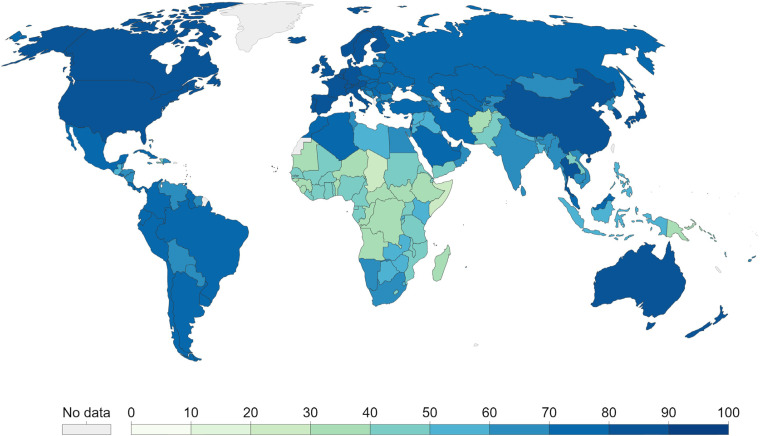
UHC
An overview of the UHC index—ranging from 0–100, where 0 is the worst case and 100 is the best case per country, can be seen in Figure 6.
Figure 6.
UHC index per country, 2019. 11 (CC BY 4.0). (https://creativecommons.org/licenses/by/4.0/).
From the colored world map, it is immediately clear that there is a big difference in health coverage between SSA and Europe. The mean UHC index is 44,56 for SSA and 79,22 for Europe. 35 Within Europe, we also see some differences between different regions. Western and Central European countries have the best UHC indices, all scoring above 80. Eastern European countries all have UHC indices between 70 and 80.
Demographic analysis of SSA and Europe
Demographic analysis
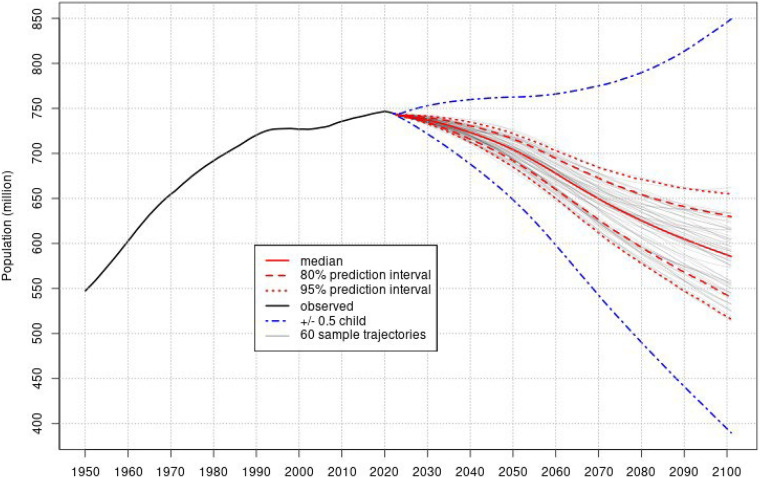
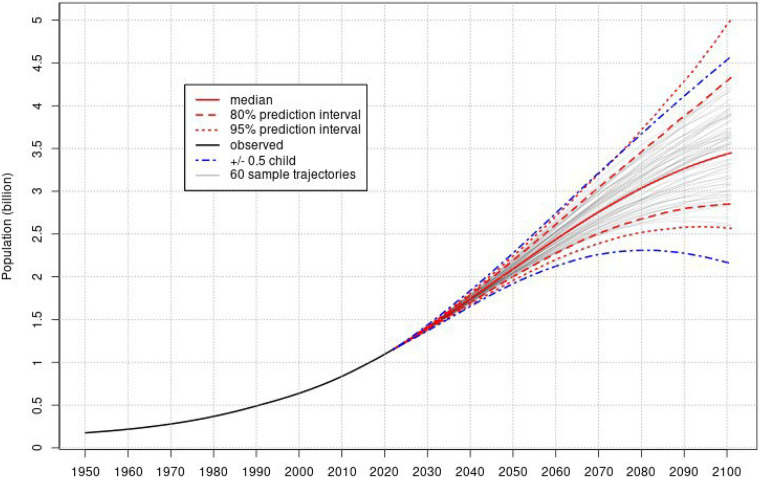
Total population
The UN currently estimates the total population in SSA at 1,166,871,764. 17 Figure 7 displays how the population has changed since 1950 and what the projected population change is up until 2100. We can see that the population of SSA has doubled since 1995. The population is projected to double again by 2050. Likewise, the UN currently estimates the total population in Europe at 743,147,538. 17 Figure 8 displays how the population has changed since 1950 and what the projected population change is up until 2100.
Figure 7.
Total population, SSA, 1950–2100. 17 (CC BY 3.0 IGO). https://creativecommons.org/licenses/by/3.0/igo/.
Figure 8.
Total population, Europe, 1950–2100. 17 (CC BY 3.0 IGO). https://creativecommons.org/licenses/by/3.0/igo/.
Birth rate and death rate
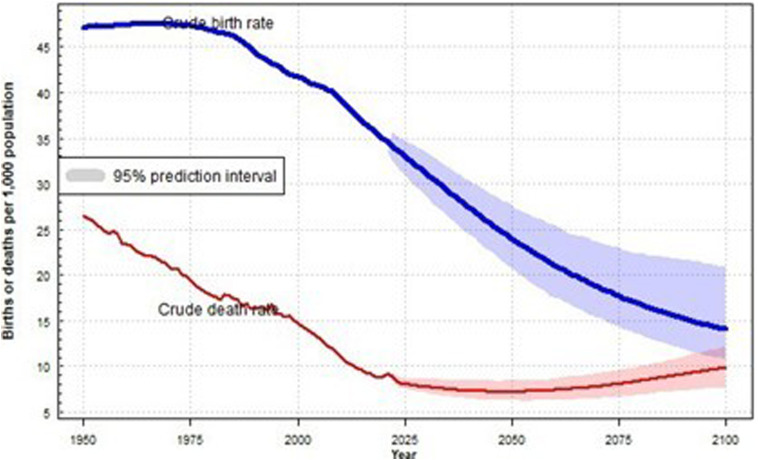
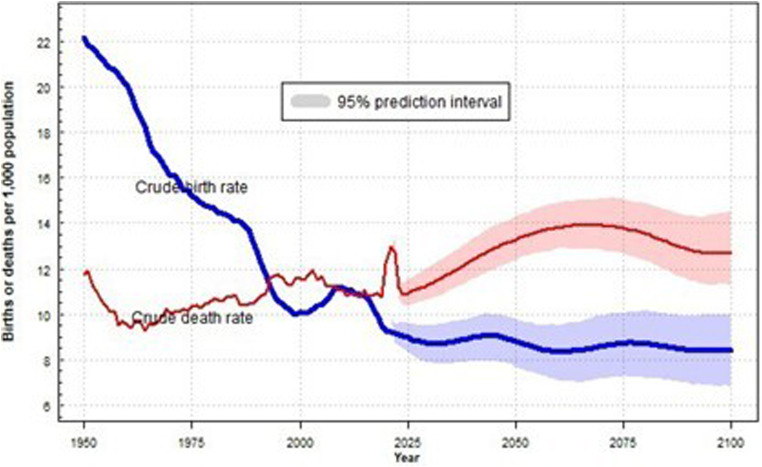
Figure 9 displays how crude birth rate and death rate in SSA have evolved since 1950 and the future projection of these rates up until 2100. We see that the death rate has been in decline since a long time. Death rate has currently reached a very low level of about 0,9%. The projection predicts the death rate reaching a plateau in the years to come. Notably, we see a small bump in death rate in the last 2 years, which can be attributed to the COVID-19 pandemic. Figure 10 displays how crude birth rate and death rate in Europe have evolved since 1950 and the future projection of these rates up until 2100. We see that death rate declined to about to the low level of 1,0% in 1960. Since then, the death rate stayed at roughly the same low level, hovering between 1,0% and 1,2% up until now. Similar to what we saw in the death rate of SSA, we also see the bump in death rate in Europe, which can be attributed to the COVID-19 pandemic. Future projections predict a slight increase in death rate.
Figure 9.
Crude birth rate and crude death rate, SSA, 1950–2100. 17 (CC BY 3.0 IGO). https://creativecommons.org/licenses/by/3.0/igo/.
Figure 10.
Crude birth rate and crude death rate, Europe, 1950–2100. 17 (CC BY 3.0 IGO). https://creativecommons.org/licenses/by/3.0/igo/.
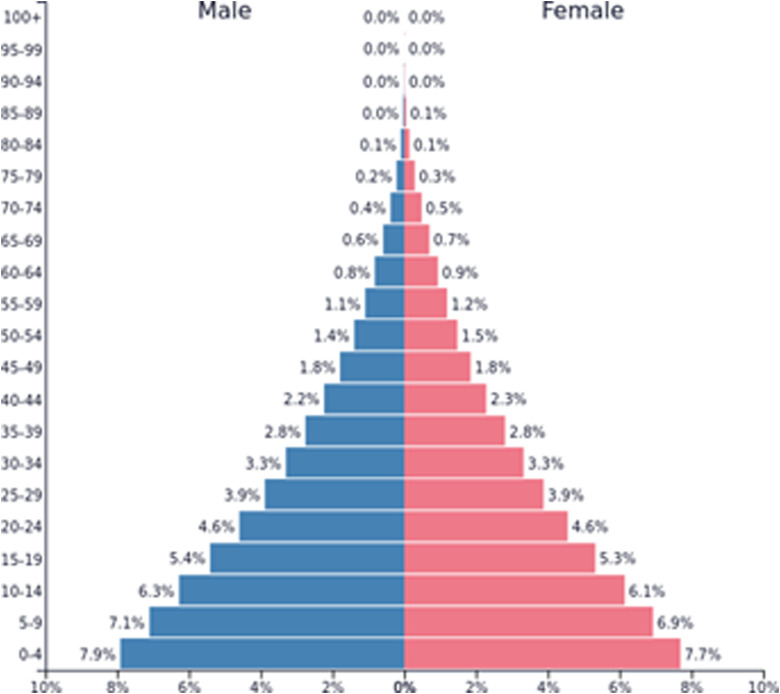
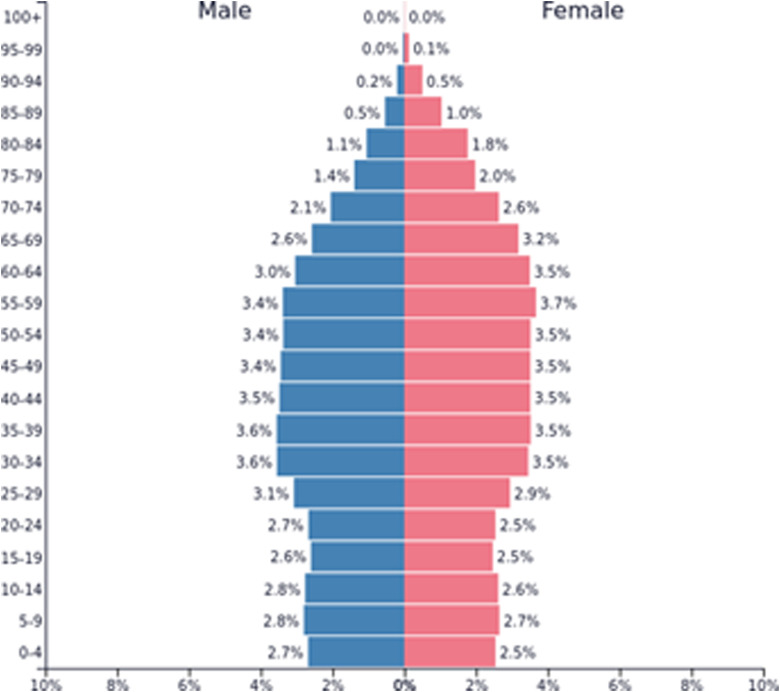
Age structure
The demographic age structure of a population is typically visualized by a population pyramid. On the horizontal axis, the amount or share of males and females is placed, on the vertical axis, the different age groups. The population pyramid of SSA can be seen in Figure 11. The population pyramid of Europe can also be seen in Figure 12.
Figure 11.
Population pyramid, SSA, 2020. 36 (CC BY 3.0 IGO). (https://creativecommons.org/licenses/by/3.0/igo/).
Figure 12.
Population pyramid, Europe, 2020. 36 (CC BY 3.0 IGO). (https://creativecommons.org/licenses/by/3.0/igo/).
Fertility
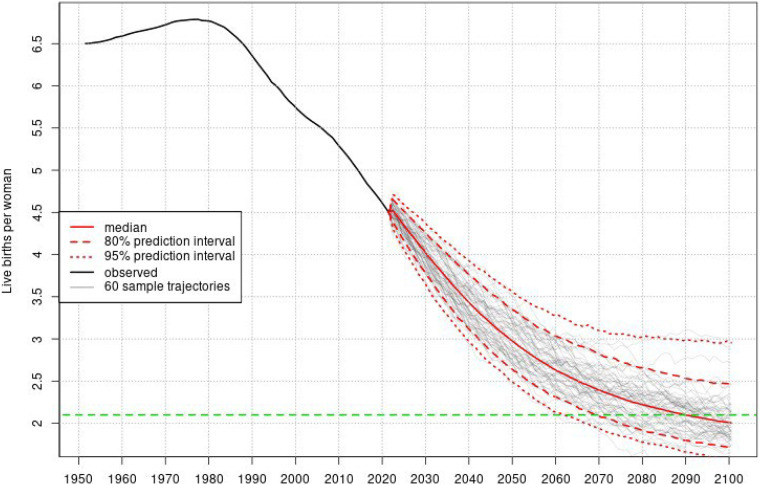
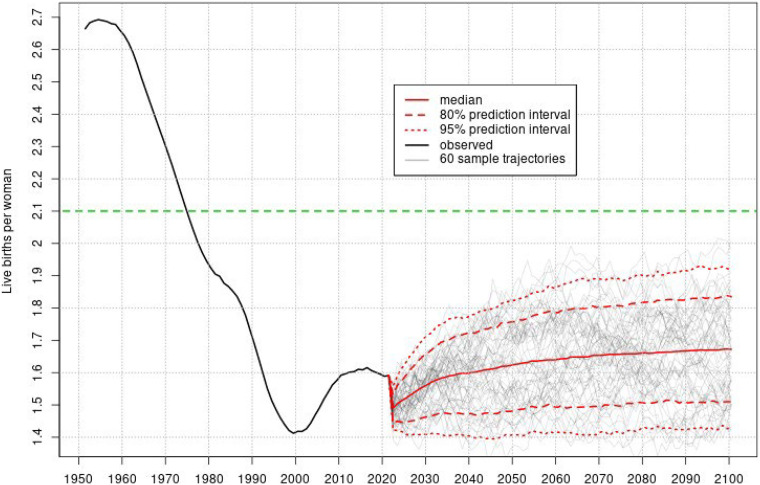
The final demographic parameter we look at in this demographic analysis is fertility, or the number of children per women. The fertility rate since 1950 and further projection up until 2100 for SSA and Europe is seen in Figures 13 and 14, respectively. In both figures, the important replacement fertility rate of 2,1 children per woman—i.e., the fertility rate at which a population replaces itself from one generation to the next—is indicated.
Figure 13.
Fertility, SSA, 1950–2100. 17 (CC BY 3.0 IGO). https://creativecommons.org/licenses/by/3.0/igo/.
Figure 14.
Fertility, Europe, 1950–2100. 17 (CC BY 3.0 IGO). https://creativecommons.org/licenses/by/3.0/igo/.
Placement within the demographic transition model
The population pyramid in SSA has the typical pyramid shape, with a broad base, gradually narrowing towards the top, indicating a very young population. With this information, we can place the region of SSA somewhere on the verge of stages 2 and 3 within the demographic transition model referring to the five stages of demographic transition model 16 in Figure 15. The population pyramid in Europe has a very narrow base and a broad center, only narrowing at the very top, indication of a very old population. With this information, we can place the region of Europe somewhere on the verge of stages 4 and 5 within the demographic transition model referring to the five stages of demographic transition model 16 in Figure 15.
Figure 15.
The five stages of the demographic transition model. 16 (CC BY-SA 4.0). https://creativecommons.org/licenses/by-sa/4.0/.
Demography and health
SSA still has a lot of major health issues that need to be addressed in the years to come. However, when looking at crude death rate, we saw that death rate is already very low in SSA. So, from a health perspective, one could conclude that the situation is not as bad as it seems in SSA. This conclusion however, is—not correct. The crucial thing to realize here is that the population of SSA is very young. With better healthcare, the death rate of this young population should be even lower. However, with current health issues still existing in SSA, the death rate of the very young population is about the same as the death rate in the much older European population.
This shows the importance of also looking at the demographic structure when assessing the health status of a population. This is indirectly done by looking at indicator such as child mortality instead of mortality alone. Indeed, the difference in health status becomes very clear if we compare the child mortality in SSA and Europe.
Use and availability of mHealth systems of SSA and Europe
The SSA article search revealed a total of 1020 articles, of which 831 remained after duplicates were removed. The search query for Europe articles produced a total of 2477 articles, of which 1605 remained after duplicates were removed. After title and abstract screening, 593 SSA articles were eliminated, leaving 238 for further screening; and 1201 publication for Europe were excluded, leaving 404 for further review. The remaining articles were then evaluated for their suitability for further investigation. Following screening for eligibility, 14 articles for SSA and 20 articles for Europe were chosen.
mHealth solutions—SSA
The youth predominates in SSA as a result of population changes. There is a great need for technological solutions to be included into the healthcare system due to the region's double burden of communicable disease and NCDs, as well as the fact that there is insufficient healthcare service delivery and staff. There has been little research on the availability and use of mHealth by health workers for disease diagnosis. 37 However, a substantial amount of evidence has been reported on the use of mobile technology as a clinical decision support system in SSA, indicating an increase in the domain and its potential for improving health service delivery in low-resource settings. 38 Pregnant women, young moms, HIV and AIDS patients, children, adolescents, and adults in general in SSA were the major targets of mHealth interventions. 39 These interventions have been shown to improve adherence to treatment and medication procedures, promote clinical appointment compliance, and improve drug collection on time. 40
Telemedicine has been successfully deployed in SSA in many fields: dermatology, ophthalmology, HIV prevention and care, clinical psychology and psychiatry, neurosurgery, radiology, and NCDs, including hypertension. 41 There are also attempts for adoption and integration of telemonitoring to support HIV and tuberculosis uptake, retention, adherence, prevention, and treatment in all settings. 42 mHealth and telemonitoring systems hold great promise for improving healthcare, particularly for those on long-term treatment, such as HIV and TB. The most recent technological advancements in SSA offer tremendous opportunity to integrate telehealth strategies into the various stages of the hypertension control cascade. 43
The majority of the health issues addressed by mHealth projects were associated with the most frequent causes of mortality and disease burden in SSA, which fall into the categories of communicable, maternal, neonatal, and nutritional diseases, despite not being well established or having widespread implementation.
In terms of area of mHealth Interventions, mHealth technologies are mostly distributed within the rural and semirural areas of SSA. Initiatives are targeting at locations which are understaffed in terms of health personnel and lack of specialist health personnel. 39 Most mHealth interventions are telemedicine applications to transmit diagnostic information and SMS based approaches for informing and reminding the patient.39,44
A lack of existing mHealth research is reported regarding childhood and adolescent obesity in SSA. 45
It is also reported that the scale-up of mHealth in antenatal care programs in SSA is hampered by a number of organizational and financial issues. Scale-up has also been slowed down by the lack of experience with mHealth technologies in landlocked and developing nations like South Sudan, Rwanda, and Somalia. There is a need for research into the long-term effects of mHealth interventions on antenatal care outcomes as well as on the cost-effectiveness of such interventions to help with the transition beyond the pilot phase. 46 Such information could aid in the development of appropriate policies and procedures for use in healthcare facilities, enabling the expansion of mHealth interventions. 46
In SSA, mHealth for maternal health, NCDs care, and telehealth interventions for hypertension are still limited, are inadequate, and are in its early stages. However, everyone agrees that the prospects are promising.47,48,43 Moreover, mHealth innovation used by palliative care services and research on the use of mHealth interventions to manage chronic disease conditions such as HIV, tuberculosis, cancer, and hypertension is limited.40, 49 However, it has been demonstrated that mHealth interventions can be used to effectively treat and manage both communicable and non-communicable diseases. 37 Additionally, there is a lack of studies reporting on acceptability and efficacy of telemedicine for neurology. 41 Several evidence gaps must be addressed, including specific mechanisms underlying the use, sustainability, and effects of mobile technology for clinical decision-making on quality of care, as well as their ability to be fully integrated into routine practice. 38 The lack of scientific evidence could be explained in part by a systematic failure to consider success factors in the implementation and use of mHealth during project design. SSA does have a lack of documentation on mHealth success factors; 47 and there is insufficient evidence to support its effectiveness. 48
It is critical to invest in simple, cost-effective, and dependable telemonitoring approaches to increase acceptability, uptake, and retention in health systems. 42 When developing mHealth, it is important to take into account the evidence already available from other conditions. This may provide guidance for developing interventions that are in line with the evolving patient population needs, who are likely to have rising chronic care needs, in the years to come. 49
mHealth solutions—Europe
As a result of demographic changes, Europe's population is getting older. People's reliance on digital technologies is growing, and health ministries are investing more money in digitization. Older people are impacted by societal digital demands, and learning to use new telehealth systems and digital devices is seen as a way to meet their needs. 50 The majority of the health conditions that the implemented mHealth systems in Europe dealt with were related to aging. The focus of mHealth research has also been on chronic medical conditions. Heart and CVD-related conditions (24.5%), mental disorders (17.8%), obesity, weight management, and healthy diet (13.3%), diabetes (11.1%), and neurological diseases (8.9%) were the health issues most frequently addressed by mHealth systems. 51 This coincides very well with the disease burden the region is experiencing. Cardiovascular Disease/Heart Failure (CVD/HF) is the most common health issue in Europe (23,2%), followed by chronic diseases (8,7%).
Many telemedicine trials and projects have been focused on chronic heart failure since the early 2000s. The first telemedicine initiatives relied on telemonitoring, or telephone follow-up for elderly patients. Over the past 10 years, a number of second-generation telemedicine projects for heart failure have emerged in Europe or are still being developed. 52 Remote monitoring of cardiac implantable electronic devices (CIEDs) is reported to be safe and cost-effective. Most patients readily accept it, and it allows for the early identification of significant clinical issues. 53
The management of CIEDs will be significantly impacted by remote monitoring, and most centers would like to have remote device programming capabilities in the future. 53 Chronic disease home telemonitoring appears to be a promising patient management strategy that generates accurate and trustworthy data, empowers patients, affects their attitudes and behaviors, and may even improve their health conditions. 54 Methods for assessing dietary intake that make use of modern technology, like mHealth, may be more appealing and entertaining than those that rely on paper, especially for children and young adults. When compared to more objective measures, gaps between many of the new technology tools and traditional methods of measuring dietary intake are larger. 55 It has been demonstrated that Internet- and mobile-based psychological interventions (IMIs) are adaptable, technically diverse methods that lend themselves to a variety of application areas and indications of varying severity. They are viewed as a helpful addition to the treatment options rather than a replacement for traditional psychotherapeutic interventions. 56 Compelling evidence is provided by a number of studies demonstrating the viability and acceptability of web- and mobile-based interventions for people with schizophrenia and/or other psychotic disorders for both patients and caregivers. There is some evidence that certain aspects of mental healthcare processes, such as shared decision-making, symptom monitoring, disease management, information provision, and empowerment, may be improved by e-mental health interventions. They may also enhance outcomes by encouraging symptom reduction and treatment adherence, according to early research. 57
Positive results are reported from telehealth interventions for chronic obstructive pulmonary disease (COPD). 58 It has been reported that eHealth and telephone support for overweight or obese children are available in Europe. 59 In studies examining the monitoring of workload in team sports, Europe is cited as a pioneer. Typically, Global Positioning System (GPS) data is used to monitor workload and determine the risk of injury. 60
Websites are the most popular source, while apps are the least popular. The majority of the sources emphasized a healthy lifestyle, nutrition, and physical activity rather than obesity specifically. To initiate behavior change, eHealth and telephone guidance mediums target risk factors. 59 In general, the research regarding childhood and adolescent obesity is currently lacking in Europe. 45
Apps have reportedly been found to be useful for promoting healthy lifestyles among students and adolescents in Europe, serving as tools for tracking both dietary intake and physical activity. The apps allow users to set goals and monitor their own progress, offer customized feedback, and ultimately increase awareness and motivation. 61
Many nations in Central and Eastern Europe are still working to lower the rate of maternal mortality. These nations would profit from mHealth initiatives that raise awareness of the ways to improve their quality of life and assist with childcare; particularly given that medical professionals are migrating to Europe's wealthier nations, while the number of professionals in Central and Eastern European nations is already quite low. 62 This is consistent with the fact that UHC is lower in Eastern Europe. Many European nations struggle to keep up with vaccination rates and combat vaccine hesitancy. This emphasizes the requirement for creative digital approaches in immunization programs. The current use of digital-based interventions to support vaccine delivery is dispersed, and there is insufficient oversight and evaluation of their effects on population health. 63
It is shown that telemedicine uptake among genetics professionals in Europe is currently low. 64 In some European nations, like the Netherlands, Sweden, Norway, or England, IMIs are currently established as a component of standard medical care. But in most other European nations, their integration into mental healthcare is less pervasive. 56
In Europe, telemedicine for diabetics has increased and intensified as a result of COVID-19 and the need for social isolation. For adults and children with type 1 diabetes, glucose-sensing technologies have made it possible for effective glycemic control that is comparable to pre-COVID-19 standard care and has, for many people, led to better glucose control. There is evidence that both adults and children with diabetes are capable and willing to communicate with their doctor via phone, text, and videoconference systems, and that they believe these methods have a significant positive impact on their health-related quality of life. 65
Because of the COVID-19 pandemic, 66 there is a decreased capacity to see patients in the outpatient clinic, and mHealth has become an important component of many atrial fibrillation outpatient clinics. Many validated mHealth solutions for remote heart rate and rhythm monitoring and risk factor assessment are reported to be available. 67 A 2021 study on pandemic pediatric telemedicine use found that pediatric providers used telemedicine more during the COVID-19 pandemic, as well as a partially sustained effect that will promote telemedicine use as part of a hybrid care provision in the post-pandemic era. 68
Discussion
In SSA, notably only three of the top 10 causes of death are NCDs; CVD (13.77%), cancers (6.82%), and digestive diseases (4.2%). The other seven all fall under the category of communicable (enteric infections (8.77%), tuberculosis (4.97%), diarrheal diseases (7.63), HIV/AIDS (8.21%), malaria (7.59%)), neonatal (neonatal deaths (9.94%)), and nutritional diseases. In Europe, we see a quite different story. Almost 70% of deaths are caused by only two diseases, namely CVDs (44.62%) and cancer (23.94%). While looking at disease burden in SSA (Figure 10), we immediately see some differences with the causes of mortality, underlining the importance of looking at burden of disease when assessing the health status of a population. Contrary to the causes of mortality, the top five disease burdens in SSA are: neonatal disorders (13.82%), respiratory infections and TB (11.59%), malaria and neglected tropical illnesses (9.56%), enteric infections (9.49%), HIV/AIDS, and STIs (7.87%). NCDs also contribute significantly to the disease burden, with CVDs (5.56%) and cancers (3.32%) ranking seventh and eighth, respectively. Upon comparison of the regions of SSA and Europe, it becomes evident that CVDs and cancer represent significant contributors to mortality in both regions. This observation aligns with existing literature that substantiates the epidemiological landscape of said regions. Furthermore, the available evidence suggests that there has been a discernible shift in disease epidemiology. 69 The most salient divergence is observed in the context of SSA, wherein a comprehensive spectrum of communicable, maternal, neonatal, and nutritional ailments persists as primary contributors to mortality. This is congruent with the prevailing circumstance that the SSA region is confronted with the onerous task of tackling a dual burden of communicable and non-communicable diseases.70,71
When looking at the causes of disease burden in Europe at first glance, we see a more similar result to the causes of mortality, with CVDs (23.87%) and cancer (16.27%) again at the top by a great margin. However, the respective percentages of are much lower for disease burden than for mortality. We also see some other diseases which have a large share in cause of disease burden as opposed to the cause of mortality, including musculoskeletal disorders (7.59%), mental disorders (5.74%), and neurological diseases (5.66%). This is consistent with recent estimations that have confirmed that non-fatal diseases including low back pain, headaches, and depressive disorders are among the top causes of DALYs. 72 When looking at the kind of disease, we see that in Europe, nine of the top 10 causes of disease burden are NCDs. The difference in causes of disease burden between SSA and Europe is even bigger than the causes of mortality, with the top five causes of disease burden being completely different between the two regions. In SSA, the top five still consist of communicable, maternal, neonatal, and nutritional diseases while in Europe, the top five are all NCDs.
In 2020, none of the individual countries in SSA had reached the SDG target child mortality of 25 per 1000. 33 We see that health worker density is extremely low in SSA. The difference with Europe is enormous. Most notably, European countries have more than six times the number of nurses/midwifes and even more than 12 times the number of medical doctors available for the same number of people. This is coherent with literature indicating the major global imbalances between the demand for and supply of health personnel, resulting in inequitable allocation and provisioning of health workers. 73 The significant difference in health worker density between SSA (UHC index = 44.56) and Europe (UHC index = 79.22) contributes significantly to the low health coverage observed in SSA, emphasizing the urgent need for additional investment and resources to address the disparity. It is estimated that by 2030, there will be a shortage of approximately 10 million healthcare workers worldwide, with the greatest impact felt in low- and middle-income countries, exacerbating the situation further. 74 More than half of global population growth between now and 2050 is expected to occur in the continent of Africa. 75 The population of Europe is projected to decrease further in the years to come. We see that the population pyramid of SSA has a very broad base and rather a narrow center and top. This shows that the population of SSA is very young. This of course is the result of the still very high birth rate. We see that the population pyramid of Europe has a narrow base and broad center and top to finally get narrower only at the higher ages. This shows that the population of Europe is very old. This of course is the result of the still very low birth rate.
All countries of SSA have a fertility rate which is higher than the replacement fertility rate of 2,1 and are thus increasing in population. 16 The opposite is true for Europe. When comparing fertility with child mortality, we see that indeed countries with lower child mortality tend to have fewer children per women. The demographic age structures of SSA and Europe also bring some perspective to the current differences in health issues. In SSA, child mortality is still a very big issue, while in Europe, a lot of the health issues can be related to ageing.
As the majority of the population in Africa still lives in rural areas and there are issues with Internet network availability and smartphone cost, the future of telemedicine across the continent may depend on how far we the continent has advanced.76,77 Yet collecting those who are obedient and receptive to telemedicine would undoubtedly ease the burden on patients and doctors. Also, it would encourage the physical distance required for COVID-19 pandemic containment and lessen congestion at the medical institutions. Rather than relying on traditional infrastructure and a traditional healthcare system, African populations need real problem-solving technologies that are affordable, accessible, and readily available. 78 Due to population changes, youth predominate in SSA. Although SSA has a slower rate of Internet use by individuals (Internet is accessible to 29% of the population) in comparison to Europe (Internet is accessible to 87% of the population), the region is growing and demonstrating a strong desire to embrace rapid technological change, taking advantage of its versatility, and closing the world's digital divide.79,80,81 As a result, both general literacy and digital literacy are rising. 82 Also, there is a rising need for mHealth solutions. The digitalization of the mHealth system is also being considered by the health ministries.
Various mHealth systems have been successfully integrated into the healthcare system in Europe. It has been stated that healthcare services in many specialties are being given using a telemedicine platform, particularly during the pandemic. Moreover, sophisticated mHealth-based technology solutions are being used, including cardiac implanted electronic implants. This is not the situation with SSA. The healthcare system has only modest integration and implementation of mHealth systems. To reduce the digital gap, experiences and lessons from the industrialized world, such as Europe, should be drawn.
Most articles on mHealth systems in SSA do not report on the acceptability and viability of such systems among users, largely due to the minimal initiatives and implementation of mHealth systems in the region. Furthermore, the insufficiency of matured systems that are ready for acceptability and user feedback evaluation can be attributed to the inadequate mHealth platform available.
A similar scenario can be observed in both Europe and SSA with respect to research on mHealth and childhood and adolescent obesity, indicating a lack of focus on this area. While both regions have made promising strides in incorporating telemedicine platforms, the extent of implementation and coverage of specialties is not comparable. For instance, while telemedicine is widely used among genetic professionals in Europe, this issue has not been addressed in SSA.
Although there are reports of successful incorporation of telemedicine services for diabetics and glucose-sensing mHealth technologies that have resulted in improved glucose control in Europe, the opposite is observed in SSA, where coverage of conventional healthcare services for diabetics lags behind the needs of people living with diabetes, leading to poor glycemic control.
The pandemic has presented significant challenges to the conventional provision of healthcare systems in both regions. While Europe swiftly incorporated the use of mHealth systems for healthcare service delivery to facilitate access for patients, SSA was not as quick to adapt to the changes brought on by the pandemic and faced greater difficulty in managing healthcare services during this time. This is evident from the reported cases.
Recommendations for future research, development, and implementation of mHealth
Prioritize mHealth approaches targeting towards child survival and communicable disease fight as well as NCDs
This work showed that child survival is one of key goals for healthcare at this moment in SSA. Currently, a few research reported mHealth approaches targeting towards pregnancy, birth, and childcare, and none of the other mHealth approaches were specifically targeting towards pneumonia, diarrheal diseases, or malaria in SSA.
Identify and address gaps in current mHealth research and development
Numerous studies found gaps in or sparse or fragmented research on mHealth approaches in SSA for a number of aspects of healthcare such as maternal health, pneumonia, antenatal care, malaria, neurology, hypertension, and obesity.83,38,41,47,48,45,43 In Europe, findings also reported gaps or limited and fragmented research on several mHealth approaches such as COPDs, obesity, maternal and child health, vaccination programs, and genetics.58,45,62,63,64 Research should be carried out to address these and other existing gaps.
Anticipate future stages in demographic transition and adapt mHealth research and development accordingly
While both SSA and Europe have to deal with current challenges in health and healthcare, demography is constantly evolving, bringing new challenges to the table. Therefore, it is crucial to be aware of what changes are projected in the near future. As SSA moves on through the third stage by improving healthcare and reducing child mortality, among others, family planning and birth control will become very important. mHealth can definitely help a lot in these areas, e.g., by informing future parents on family planning and birth control. Also, the population will grow older, and health issues regarding ageing, like CVD and cancer, will be more prevalent. A lot of mHealth approaches towards CVD and cancer are already available, mainly in more developed regions of the world, so lessons should be learned from them. As Europe moves on through stage 5, a further ageing of the population is predicted. This will increase the occurrence of already widely present age-related issues, like CVD and cancer. Elderly care will become increasingly important. Therefore, further research and development mHealth systems for home-monitoring of elderly and chronic disease self-management should be promoted.
Conclusion
SSA is situated between the transitional stages of stage 2 and stage 3 within the demographic transition model. Meanwhile, Europe is positioned between the transitional stages of stage 4 and stage 5 within the demographic transition model. SSA bears the burden of both communicable and non-communicable diseases, leading to a high death rate despite its young population. Moreover, there is a high fertility rate in the region, exacerbating the burden on the already scarce healthcare workforce. The low healthcare worker density, coupled with the poor health coverage observed in the UHC data, further limits access to quality healthcare services for the population. However, there is some hope, as Internet and mobile subscription rates are gradually improving, and initiatives to implement mobile health systems are being observed. While the implementation depth of such initiatives is not yet significant, mHealth could potentially improve the provision of healthcare services in the region, given the shortage of healthcare workers and inadequate healthcare service provision. NCDs represent the leading causes of mortality and morbidity in Europe. The continent's aging population has resulted in an increased reliance on digital devices and technology for healthcare services, particularly for the management and treatment of chronic illnesses. Europe's fertility and mortality rates are low, and its health worker density is satisfactory, albeit suboptimal. In contrast to SSA, Europe boasts superior health coverage. Advanced mobile health (mHealth) solutions designed to manage chronic diseases and other medical specializations have been implemented widely in Europe. In response to the pandemic, numerous telemedicine systems have been established and continue to be utilized in the post-pandemic era. Given the existing scarcity of healthcare workers and the prevalence of disease burden in SSA countries, implementing mHealth platforms, such as telemedicine, to provide healthcare services, including remote consultations in underserved areas, may be beneficial. It is important to prioritize mHealth approaches targeting child survival, communicable diseases, and NCDs. Additionally, identifying and addressing current gaps in mHealth systems are crucial. A context-based design procedure should be followed to increase the uptake of such systems. Anticipating future stages in the demographic transition model and adopting mHealth technology research and development accordingly can further ensure that mHealth systems are effective and accessible tools for improving health outcomes in both regions.
Limitations of the study
One of the study's limitations is that it relied only on secondary data from published studies and databases including the WHO, Our World in Data, and the United Nations. As a result, the quality and availability of the data sources restrict the conclusions given in this study. Moreover, because this was a narrative literature review, the results may have been influenced by publication bias, as only studies that were published and accessible for review were included. While efforts were taken to alleviate these limitations by using a diverse set of sources and rigorously analyzing the literature, the study's findings should be viewed with caution. To further investigate the topics discussed in this paper, future studies may benefit from employing a broader range of data sources, including primary data collecting.
Acknowledgements
The authors would like to thank all individuals who directly or indirectly contributed to this research.
Footnotes
Contributorship: GTA co-conceived the study with J-MA and GLS. GTA and MVW designed and implemented the search strategy. The title and abstract screenings were performed by GTA and MVW. GTA and MVW both contributed to the data synthesis and extraction processes. GTA and MVW drafted the manuscript, which was revised by all authors. J-MA and GLS supervised the review process and critically revised the manuscript for significant intellectual content. At all stages of the manuscript's development, all authors discussed the findings and read and approved the final version.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: Genet Tadese Aboye.
ORCID iD: Genet Tadese Aboye https://orcid.org/0000-0002-3156-8809
References
- 1.UN. List of MDGs English—UN. 2015;2015. Available from: www.un.org/millenniumgoals
- 2.Ritchie H, Roser M. Now it is possible to take stock – did the world achieve the Millennium Development Goals? Our World Data, 2018.
- 3.DESA. Sustainable development. history. New York, USA: United Nations Dep Econ Soc Aff, 2022. [Google Scholar]
- 4.National Academy of Sciences. Defining and measuring population health. Washington (DC): National Academies Press (US), 2010. Available from: https://www.ncbi.nlm.nih.gov/books/NBK53336/#!po=98.8636 [Google Scholar]
- 5.Mathers CD. History of global burden of disease assessment at the World Health Organization. Arch Public Heal 2020; 78: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sciensano. Burden of Disease. Heal Top, 2022.
- 7.WHO. THE GLOBAL HEALTH OBSERVATORY Explore a world of health data [Internet]. 2022 [cited 2022 Aug 31]. Available from: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/4643
- 8.WHO. Disability-adjusted life years (DALYs). Geneva, Switherland:World Heal Organ, 2022. [Google Scholar]
- 9.Liu J, Eggleston K. The association between health workforce and health outcomes: a cross-country econometric study. Soc Indic Res [Internet] 2022; 163: 609–632. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO. Universal health coverage. Geneva, Switherland: World Heal Organ, 2022. [Google Scholar]
- 11.Ritchie H Roser MMispy. et al. et al. Measuring progress towards the Sustainable Development Goals. SDG-Tracker. 2019.
- 12.USCB. Historical estimates of world population. USA: United States Census Bur, 2021. [Google Scholar]
- 13.Herrmann M. The global population will soon reach 8 billion—then what? New York, USA: United Nations, 2022. [Google Scholar]
- 14.Ritchie H, Roser M, Rosado P. Energy [Internet]. Our World in Data. 2022. Available from: https://ourworldindata.org/energy-production-consumption#citation
- 15.Rodés-Guirao L, Roser M. Future Population Growth [Internet]. Our World in Data. 2013. Available from: https://ourworldindata.org/future-population-growth#citation
- 16.Roser M, Ritchie H, Ortiz-Ospina E. World Population Growth. Our World Data, 2020.
- 17.DESA. World population prospects 2022. New York, USA: United Nations Dep Econ Soc Aff, 2022. [Google Scholar]
- 18.Reher DS, Sandström G, Sanz-Gimeno Aet al. et al. Agency in fertility decisions in Western Europe during the demographic transition: a comparative perspective. Demography [Internet] 2017; 54: 3–22. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roser M. Future Population Growth. Our World Data, 2019.
- 20.TED. Global population growth, box by box—Hans Rosling. TED@Cannes, 2010.
- 21.Angeles L. Demographic transitions: analyzing the effects of mortality on fertility. J Popul Econ 2009; 23: 99–120. [Google Scholar]
- 22.Geopol. Global Mobile Penetration Growth [Internet]. 2022 [cited 2022 Aug 31]. Available from: https://www.geopoll.com/blog/global-mobile-penetration-growth/
- 23.WHO. mHealth—Use of appropriate digital technologies for public health. Seventy-First World Heal Assem Provisional agenda item 124. 2018.
- 24.Emmanouilidou M. The status of mHealth in Europe and a review of regulative challenges. In: L. R, M. M, editors. 2016 International Conference on E-Health, EH 2016 [Internet]. Kent Business School, University of Kent, Canterbury, Kent, CT2 7NZ, United Kingdom: IADIS; 2016. p. 203–6. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85040195146&partnerID=40&md5=f9f80b4d6996c02bafb120b8f9d4a114
- 25.Qureshi S, Xiong J, Deitenbeck B. The effect of mobile health and social inequalities on human development and health outcomes: mHealth for health equity. Proc Annu Hawaii Int Conf Syst Sci 2019; 2019-Janua: 3943–3952. [Google Scholar]
- 26.Bradway M, Carrion C, Vallespin B, et al. mHealth assessment: conceptualization of a global framework. JMIR mHealth uHealth 2017; 5:1–8. 10.2196/mhealth.7291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ryu S. Book review: mHealth: new horizons for health through mobile technologies: based on the findings of the second global survey on eHealth (global observatory for eHealth series, volume 3). Healthc Inform Res 2012; 18: 231. [Google Scholar]
- 28.Messner EM, Probst T, O’Rourke T, et al. mHealth applications: potentials, limitations, current quality and future directions. In: Baumeister H, Montag C. (eds) Digital phenotyping and mobile sensing: new developments in psychoinformatics. Ulm, Germany: Ulm Univ, Clin Psychol & Psychotherapy, 2019, pp.235–248. [Google Scholar]
- 29.The impact of COVID-19 on health and care workers: a closer look at deaths. 2021;(September).
- 30.Kenny P. WHO estimates at least 115,000 healthcare workers died in pandemic [Internet]. WORLD HEALTH. [cited 2022 Aug 31]. Available from: https://www.aa.com.tr/en/health/who-estimates-at-least-115-000-healthcare-workers-died-in-pandemic/2252384# [Google Scholar]
- 31.UN. The sustainable development goals report 2022. New York, USA: United Nations, 2022. [Google Scholar]
- 32.Roser M, Ritchie H, Dadonaite B. Child and Infant Mortality. Our World Data, 2019.
- 33.Bank W. Mortality rate, under-5 (per 1000). Databank—World Dev Indic. 2020.
- 34.WHO. Health topics. health workforce. Geneva, Switherland: World Heal Organ, 2022. [Google Scholar]
- 35.Bank W. UHC service coverage index. Data—Indic. 2019.
- 36.PopulationPyramid. Population Pyramids of the World from 1950 to 2100. PopulationPyrarmid.net. 2022.
- 37.Osei E, Agyei K, Tlou B, et al. Availability and use of mobile health technology for disease diagnosis and treatment support by health workers in the Ashanti Region of Ghana: a cross-sectional survey. Diagnostics (Basel, Switzerland). 2021 Jul; 11. 10.3390/diagnostics11071233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Adepoju I-OO, Albersen BJA, De Brouwere V, et al. mHealth for clinical decision-making in Sub-Saharan Africa: a scoping review. JMIR mHealth UHealth 2017 Mar; 5: e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bervell B, Al-Samarraie H. A comparative review of mobile health and electronic health utilization in Sub-Saharan African countries. Soc Sci Med 2019 Jul; 232: 1–16. [DOI] [PubMed] [Google Scholar]
- 40.Osei E, Kuupiel D, Vezi PNet al. et al. Mapping evidence of mobile health technologies for disease diagnosis and treatment support by health workers in Sub-Saharan Africa: a scoping review. BMC Med Inform Decis Mak 2021 Jan; 21: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sarfo FS, Adamu S, Awuah Det al. et al. Tele-neurology in Sub-Saharan Africa: a systematic review of the literature. J Neurol Sci 2017 Sep; 380: 196–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yah CS, Tambo E, Khayeka-Wandabwa Cet al. et al. Impact of telemonitoring approaches on integrated HIV and TB diagnosis and treatment interventions in Sub-Saharan Africa: a scoping review. Heal Promot Perspect 2017; 7: 60–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Muiruri C, Manavalan P, Jazowski SA, et al. Opportunities to leverage telehealth approaches along the hypertension control cascade in Sub-Saharan Africa. Curr Hypertens Rep 2019 Aug; 21: 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tapera R, Singh Y. A bibliometric analysis of medical informatics and telemedicine in Sub-Saharan Africa and BRICS nations. J Public health Res 2021 Jun; 10. 10.4081/jphr.2021.1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reddy P, Dukhi N, Sewpaul R, et al. Mobile health interventions addressing childhood and adolescent obesity in Sub-Saharan Africa and Europe. Current landscape and potential for future research. Front Public Heal 2021; 9: 604439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Manyati TK, Mutsau M. A systematic review of the factors that hinder the scale up of mobile health technologies in antenatal care programmes in Sub-Saharan Africa. African J Sci Technol Innov Dev [Internet] 2021; 13: 125–131. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85086929965&doi=10.1080%2F20421338.2020.1765479&partnerID=40&md5=f938b77afd26ab297a9e648df68eff31. [Google Scholar]
- 47.Ag Ahmed MA, Gagnon M-P, Hamelin-Brabant L, et al. A mixed methods systematic review of success factors of mHealth and telehealth for maternal health in Sub-Saharan Africa. mHealth 2017; 3: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bloomfield GS, Vedanthan R, Vasudevan L, et al. Mobile health for non-communicable diseases in Sub-Saharan Africa: a systematic review of the literature and strategic framework for research. Global Health 2014 Jun; 10: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Allsop MJ, Powell RA, Namisango E. The state of mHealth development and use by palliative care services in Sub-Saharan Africa: a systematic review of the literature. BMJ Support Palliat Care 2018 Jun; 8: 155–163. [DOI] [PubMed] [Google Scholar]
- 50.Raja M, Bjerkan J, Kymre IG, et al. Telehealth and digital developments in society that persons 75 years and older in European countries have been part of: a scoping review. BMC Health Serv Res 2021 Oct; 21: 1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Koumpouros Y, Georgoulas A. A systematic review of mHealth funded R&D activities in EU: trends, technologies and obstacles. Inform Health Soc Care 2020; 45: 168–187. [DOI] [PubMed] [Google Scholar]
- 52.Andrès E, Talha S, Zulfiqar A-A, et al. Current research and new perspectives of telemedicine in chronic heart failure. Narrative review and points of interest for the clinician. J Clin Med 2018 Dec; 7.DOI: 10.3390%2Fjcm7120544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hernández-Madrid A, Lewalter T, Proclemer A, et al. Remote monitoring of cardiac implantable electronic devices in Europe: results of the European Heart Rhythm Association survey. Eur Eur Pacing, Arrhythmias, Card Electrophysiol J Work Groups Card Pacing, Arrhythmias, Card Cell Electrophysiol Eur Soc Cardiol 2014 Jan; 16: 129–132. [DOI] [PubMed] [Google Scholar]
- 54.Pare G, Jaana M, Sicotte C. Systematic review of home telemonitoring for chronic diseases: the evidence base. J Am Med INFORMATICS Assoc 2007; 14: 269–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Eldridge AL, Piernas C, Illner A-K, et al. Evaluation of new technology-based tools for dietary intake assessment—an ILSI Europe dietary intake and exposure task force evaluation. Nutrients 2018 Dec; 11. 10.3390/nu11010055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ebert DD, Van Daele T, Nordgreen T, et al. Internet- and mobile-based psychological interventions: applications, efficacy, and potential for improving mental health: a report of the EFPA e-health taskforce. Eur Psychol [Internet] 2018; 23: 167–187. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85047119411&doi=10.1027%2F1016-9040%2Fa000318&partnerID=40&md5=615415f08c3287c6386369e07aa9063a. [Google Scholar]
- 57.Gaebel W, Großimlinghaus I, Kerst A, et al. European Psychiatric Association (EPA) guidance on the quality of eMental health interventions in the treatment of psychotic disorders. Eur Arch Psychiatry Clin Neurosci 2016 Mar; 266: 125–137. [DOI] [PubMed] [Google Scholar]
- 58.Gaveikaite V, Grundstrom C, Winter S, et al. A systematic map and in-depth review of European telehealth interventions efficacy for chronic obstructive pulmonary disease. Respir Med 2019; 158: 78–88. [DOI] [PubMed] [Google Scholar]
- 59.Deshpande S, Rigby MJ, Blair M. The presence of eHealth support for childhood obesity guidance. Stud Health Technol Inform 2018; 247: 945–949. [PubMed] [Google Scholar]
- 60.Benson LC, Räisänen AM, Volkova VG, et al. Workload a-wear-ness: monitoring workload in team sports with wearable technology. A scoping review. J Orthop Sports Phys Ther [Internet] 2020; 50: 549–563. https://www.scopus.com/inward/record.uri?eid=2-s2.0-85092354268&doi=10.2519%2Fjospt.2020.9753&partnerID=40&md5=7872d69a305db05eecbaa0324e12132f. Available from. [DOI] [PubMed] [Google Scholar]
- 61.Dute DJ, Bemelmans WJE, Breda J. Using mobile apps to promote a healthy lifestyle among adolescents and students: a review of the theoretical basis and lessons learned. JMIR mHealth UHealth 2016 May; 4: e39–e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mambou S, Krejcar O, Maresova P, et al. The Need for Mobile Apps for Maternal and Child Health Care in Center and East Europe [Internet]. I. A, M. Y, P. U, M. A, editors. Vol. 11673 LNCS, 16th International Conference on Mobile Web and Intelligent Information Systems, MobiWIS 2019. Faculty of Informatics and Management, Center for Basic and Applied Research, University of Hradec Kralove, Rokitanskeho 62, Hradec Kralove, 500 03, Czech Republic: Springer; 2019. p. 95–108. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85077134778&doi=10.1007%2F978-3-030-27192-3_8&partnerID=40&md5=cdb6ae55a16daf0702312bdd39b5abad
- 63.Odone A, Gianfredi V, Sorbello S, et al. The use of digital technologies to support vaccination programmes in Europe: state of the art and best practices from experts’ interviews. Vaccines [Internet] 2021; 9. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85116775250&doi=10.3390%2Fvaccines9101126&partnerID=40&md5=ea406707919635415cb61b20efd6bf27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Otten E, Birnie E, Lucassen AM, et al. Telemedicine uptake among genetics professionals in Europe: room for expansion. Eur J Hum Genet 2016 Feb; 24: 157–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Choudhary P, Bellido V, Graner M, et al. The challenge of sustainable access to telemonitoring tools for people with diabetes in Europe: lessons from COVID-19 and beyond. Diabetes Ther Res Treat Educ Diabetes Relat Disord 2021 Sep; 12: 2311–2327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.El Sherif DM, Abouzid M. Analysis of mHealth research : mapping the relationship between mobile apps technology and healthcare during COVID—19 outbreak. Global Health [Internet] 2022; 18: 1–11. 10.1186/s12992-022-00856-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hermans ANL, van der Velden RMJ, Gawalko M, et al. On-demand mobile health infrastructures to allow comprehensive remote atrial fibrillation and risk factor management through teleconsultation. Clin Cardiol 2020 Nov; 43: 1232–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Reingold SM, Hadjipanayis A, van Esso D, et al. COVID-19 era effect on pandemic and post-pandemic pediatric telemedicine use: a survey of the European Academy of Pediatrics research in ambulatory settings network. Front Pediatr 2021; 9: 713930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yuyun MF, Sliwa K, Kengne AP, et al. Cardiovascular diseases in Sub-Saharan Africa compared to high-income countries : an epidemiological perspective. World Heart Federation. Global Heart. 2020; 15: 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mapesi H, Paris DH. Non-communicable diseases on the rise in Sub-Saharan Africa, the underappreciated threat of a dual disease burden. Praxis (Bern 1994). 2019 Nov; 108: 997–1005. [DOI] [PubMed] [Google Scholar]
- 71.Mudie K Jin MMTan, et al. Non-communicable diseases in Sub-Saharan Africa: a scoping review of large cohort studies. J Glob Health 2019 Dec; 9: 20409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wyper GMA, Assuncao R, Fletcher E, et al. The increasing significance of disease severity in a burden of disease framework. Scand J Public Health 2023; 51: 296–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Global strategy on human resources for health : Workforce 2030. [DOI] [PMC free article] [PubMed]
- 74.Lumley AR. T. Why is there a global medical recruitment and retention crisis [Internet]. World Economic Forum. 2023 [cited 2023 Mar 30]. Available from: https://www.weforum.org/agenda/2023/01/medical-recruitment-crisis-davos23/#:∼:text=Therewillbeanestimated,oftheglobalhealthcareworkforce.
- 75.UN. Global issues. population. New York, USA: United Nations, 2019. [Google Scholar]
- 76.Mbunge E, Muchemwa B, Batani J. Are we there yet? Unbundling the potential adoption and integration of telemedicine to improve virtual healthcare services in African health systems. ScienceDirect. 2022;3. [DOI] [PMC free article] [PubMed]
- 77.Ftouni R, Aljardali B, Hamdanieh M, et al. Challenges of telemedicine during the COVID—19 pandemic : a systematic review. BMC Medical Informatics and Decision Making 2022; 0: 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mesko DB. Africa Is A Hotspot For Digital Health. The Medical Futurist [Internet]. 2018; Available from: https://medicalfuturist.com/africa-hotspot-digital-health/
- 79.Individuals using the Internet (% of Population)—European Union [Internet]. The World Bank. 2023 [cited 2023 Mar 30]. Available from: https://data.worldbank.org/indicator/IT.NET.USER.ZS?locations=EU&name_desc=true
- 80.Individuals using the Internet (% of Population)—Su-Saharan Africa [Internet] . The World Bank 2023. Available from: https://data.worldbank.org/indicator/IT.NET.USER.ZS?locations=ZG&name_desc=true. [cited 2023 Mar 30].
- 81.Digital Literacy in Africa [Internet]. [cited 2023 Mar 28]. Available from: https://www.do4africa.org/en/digital-literacy-in-africa/
- 82.The Future of Digital Literacy in Africa [Internet]. Americal Library association. [cited 2023 Mar 28]. Available from: https://www.ala.org/news/member-news/2022/09/future-digital-literacy-africa
- 83.Osei E, Nkambule SJ, Vezi PNet al. et al. Systematic review and meta-analysis of the diagnostic accuracy of mobile-linked point-of-care diagnostics in Sub-Saharan Africa. Diagnostics (Basel, Switzerland) 2021 Jun; 11. DOI: 10.3390%2Fdiagnostics11061081. [DOI] [PMC free article] [PubMed] [Google Scholar]