Abstract
Background
Potentially avoidable hospitalisations (PAHs) are proxy measures of effective primary care at a population level. PAHs are higher in rural and disadvantaged areas. This qualitative study sought a deeper understanding of PAHs for chronic health conditions in a rural context from the perspectives of patients and health professionals, and aimed to develop a logic model for rural health services to identify intervention targets.
Methods
Patients with chronic obstructive pulmonary disease, congestive cardiac failure or type 2 diabetes, admitted to a rural hospital in Australia and local health professionals were invited to participate in interviews in late 2019. Semistructured interviews were recorded, transcribed verbatim and thematically analysed. Themes were mapped against a programme logic model developed in a similar study.
Results
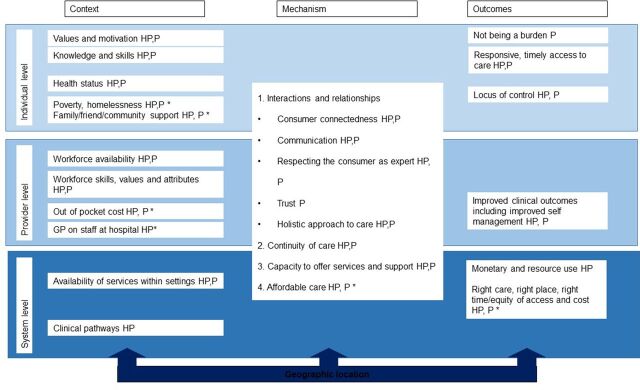
patients and 16 health professionals participated. The logic model encompassed patient level (knowledge, skills, health status), provider level (workforce availability, attributes) and system level (clinical pathways) contexts. These contexts influenced key mechanisms of relationships, continuity of care and capacity to offer services. Outcomes included responsive and timely access to care, improved clinical outcomes and resource use. Themes that did not readily map to the logic model included socioeconomic disadvantage and healthcare costs, which influenced affordability and equity of access.
Conclusion
Patients’ complex health and social circumstance, health service access and unclear care pathways were strong themes associated with PAH in this rural context. Patient, provider and system contexts influencing key mechanisms and outcomes need to be understood when designing solutions to address PAHs in rural settings. Ideally, interventions should address the cost of healthcare alongside interventions to enhance relationships, continuity of care and capacity to offer services.
Keywords: Chronic disease management, Ambulatory care, Qualitative research
What is already known about this subject?
Potentially avoidable hospitalisations (PAHs) are typically higher in rural areas and socioeconomically disadvantaged areas.
PAHs pose a high financial burden to the health system and poorer quality of life for patients.
Avoidable hospitalisation is reportedly associated with a multitude of factors, for example, poverty, poor health literacy, health service availability and socioeconomic factors, but less is known about the impact of the rural context, or factors identified from the patient’s perspective.
What does this study add?
Patients and health professionals identified that PAH were influenced by the patients’ complex health and social circumstances, health service access and unclear care pathways.
Cost of healthcare was a barrier to optimal chronic disease management, likely placing patients at risk of avoidable hospitalisation.
The programme logic model developed points to a number of targets for intervention to ultimately reduce avoidable hospitalisations.
How might this impact on clinical practice or future developments?
Interventions that aim to reduce PAHs in this rural context will require an integrated approach involving the hospital, primary care and social services.
Background
Potentially avoidable hospitalisations (PAHs) are hospitalisations that may be avoided with appropriate, preventative health interventions and chronic disease management in primary care settings.1 An estimated 7% of all hospitalisations are potentially avoidable in Australia,1 although the rate is not evenly distributed, with PAH increasing with distance from major cities.2 In Australia, there are 22 conditions for which hospitalisations are defined as potentially avoidable1 which are divided into vaccine preventable and acute and chronic admissions. Congestive cardiac failure, chronic obstructive pulmonary disease (COPD) and diabetes complications account for over half of the chronic PAH admissions.1 PAH is a proxy measure for effective primary care at a population level3 and is used as a key performance indicator for health services and is linked to hospital funding in Australia.4 PAH pose a substantial financial burden to the health system and impact patient quality of life. PAH are therefore a target to reduce costs, improve health systems and alleviate patient suffering.5 It must be acknowledged that a proportion of hospital admissions for key chronic health conditions are planned, and are therefore unavoidable.6
Factors associated with preventable hospitalisation have been identified as person priorities (symptom management and supportive relationships), programme priorities (self-management and service delivery) and place priorities (local infrastructure and socioeconomic factors)7. The contribution of patient characteristics, such as disease severity, complexity and current health status to PAH have also been examined in detail.7
Deep understanding of PAH however also requires input from community-based health professionals and patients8 9 and an appreciation of the impact of context is crucial. Geographical variation in PAH is thought to be driven primarily by socioeconomic disadvantage, which in turn is influenced by population health and health behaviours10. An Australian study identified that community or multipurpose health services and smaller, district hospitals, that is, the predominant health services in rural areas, exhibited higher PAH than major or principal referral hospitals, due to differences in propensity to admit, even after adjusting for patient and geographical variation.10 A qualitative study of patients in regional New South Wales demonstrated factors associated with potentially preventable hospitalisation included a lack of support, lack of medication adherence, poor mental health and poor understanding of their disease.9 The same team investigated the perspectives of community-based service providers and found that complexity of service provision, lack of awareness of services and how to access them, a lack of services, poverty, rurality and transport issues were associated with avoidable hospital admissions.8
Understanding PAH in rural areas and other areas of high PAH may assist in redesigning chronic disease models of care, increasing access to primary care, optimising integration of care and identifying patients at risk of PAH who may require additional support. Programme logic can be used to organise key findings in a way that identifies targets for intervention and describe complex systems effectively.11 The primary aim of this study was to better understand PAHs for key chronic health conditions (COPD, heart failure and type 2 diabetes complications) in a rural context from the perspectives of patients and health professionals. The secondary aim was to map findings to a rural-specific programme logic model in order to identify targets for intervention by individual rural health services. Specifically, our research question was ‘Which factors are perceived as contributing to PAH in a rural context and could therefore be targets for intervention?’.
Methods
Design
A qualitative study using semistructured interviews and inductive thematic analysis was undertaken. Thematic analysis was chosen as it allowed for synthesis focused on a phenomenon of interest,12 this being factors associated with PAHs for congestive cardiac failure, COPD or type 2 diabetes in a rural Australian setting. Thematic analysis is also a transparent method that actively seeks to remain close to the primary data and avoids over analysis.13 Reporting followed the consolidated criteria for reporting qualitative research guidelines.14
Setting
This research was conducted in a medium-sized rural town (Modified Monash Model 415), located approximately 200 km from the Victorian state capital city of Melbourne. The local government area (LGA) is more socioeconomically disadvantaged than the state average (Index of Relative Socioeconomic Disadvantage (IRSD) of 957 compared with Victorian average IRSD of 1010 (16) and has a high percentage of people aged 65+ years (23% compared with 15% in Victoria)16. The number of general practitioners (GPs) per 1000 population (1.2) is equivalent to the state average,16 although access to bulk-billed services (no out-of-pocket cost is incurred by patient) is lower than state average.17
The rural LGA experienced higher than state average PAHs during the financial years 2015/2016, 2016/2017 and 2017/2018 for COPD (3/3 of these financial years), congestive cardiac failure (2/3 of these financial years) and type 2 diabetes mellitus (1/3 of these financial years)18. The local health service is a multisector health service provider employing 330 staff across acute, community and residential aged care services including a public hospital with 24 acute beds servicing a catchment of 13 800 people.18 The hospital medical service is delivered by local GPs. The urgent care centre is staffed by nurses, and patients typically incur a fee if a doctor is required to attend. There is one pharmacist on staff and no dedicated discharge coordinator. At times, patients from the rural town receive healthcare from the hospital in a neighbouring larger town which is located approximately 50 km away.
Participants
The study included a convenience sample of patients admitted to a rural health service with a primary diagnosis of COPD, congestive cardiac failure or diabetes in the preceding 12 months (International Classification of Disease codes beginning E10 (type 1 diabetes mellitus), E11 (type 2 diabetes mellitus with or without complications), E13 (other specified diabetes mellitus), E14 (unspecified diabetes mellitus), I50 (congestive cardiac failure, congestive heart failure), I11 (hypertensive heart disease with (congestive) heart failure), J81 (pulmonary odema) or J20 (acute bronchitis, but only in conjunction with J41, J42, J43 or J44), J41 (simple or mucopurulent chronic bronchitis), J42 (unspecified chronic bronchitis), J43 (emphysema) or J44 (other chronic obstructive pulmonary disease) were used). A letter was sent to all eligible patients inviting them to participate in an interview. An email was sent to all organisations within the surrounding LGA employing health professionals involved in the care of patients with COPD, diabetes or congestive cardiac failure for distribution to their staff inviting them to participate in an interview.
Patient and public involvement
Patients were involved in the conduct of this research. During the study, a patient representative was a member of the project reference group and assisted with interpretation of findings. When the findings have been published and the health service is ready to trial an intervention, patient representatives will again be included on the project reference group. Patient participants will be informed of the results via a newsletter suitable for a non-specialist audience and via the hospital website.
Data collection
Semistructured interview questions were developed in consultation with experts in the field of chronic illness and community healthcare. A previous project in the same region (KG, TA, RD) had identified that integration of care was an important issue in PAH (unpublished data), which has also been reported in the literature.19 The questions sought to explore PAHs in the rural context, from the perspectives of patients and health professionals (see online supplemental appendix 1). The questions did not undergo pilot testing. In-person interviews were conducted at a location chosen by the participant which included private homes, workplaces and community health facilities. The female interviewers (KG, PhD, Research Fellow and TA, BPhty, MPH, Project Officer) had training in interviewing techniques, experience in chronic disease management (TA) and healthcare delivery research. The interviewers had no prior or ongoing relationship with the participants. Member checking did not occur. One interviewer was present at each interview. Interviews were audio recorded and transcribed verbatim. There were no non-participants or non-researchers present during the interviews. No repeat interviews were conducted. One participant did not consent to audio recording and notes were taken by the interviewer. Names of people, towns, clinics and unusual health conditions have been changed in the reporting of this study to ensure anonymity of participants. Illustrative quotes are denoted by ‘P’ for patient participants and ‘HP’ for health professional participants. All people who expressed an interest in participating were interviewed.
ihj-2021-000124supp001.pdf (163.7KB, pdf)
Analysis
A framework analysis approach was used,20 in which two authors familiarised themselves with the data and free codes were identified while coding the same transcript. These codes were then collaboratively charted and organised into descriptive themes. Identified themes were then mapped to an existing programme logic model which had been developed in a study of COPD outcomes and avoidable hospitalisation in a comparable rural context.21 This process enabled verification of identified themes and identification of new themes that had not been reported in the existing programme logic model. Research team analysis meetings were held at key intervals to verify data analysis and interpretation. By the final interview, new information was no longer impacting on the codebook, thus reaching data saturation as defined by Guest et al.22 Data management software was not used.
Results
Participants
There were 32 unique patients admitted to the rural health service in the financial year 2018–2019 with a primary diagnosis of COPD, 35 with congestive cardiac failure and 13 with complications of type 2 diabetes, as summarised in table 1.
Table 1.
Characteristics of patients admitted to rural hospital with primary diagnosis of congestive cardiac failure, COPD or complications of type 2 diabetes in the financial year 2018–2019
| COPD admissions | Congestive cardiac failure admissions | Type 2 diabetes admissions | |
| Number of admissions | 48 | 45 | 16 |
| Number of unique patients | 32 | 35 | 13 |
| Sex (unique patients) | 38% male | 51% male | 62% male |
| Age (unique patients) mean±SD | 75±10 | 85±8 | 71±13 |
| Length of stay (days, mean±SD (range)) | 4.15±2.32 (1–12) | 3.73±2.03 (1–13) | 4.00±1.71 (1–7) |
| Patients eligible for interview | 29 | 28 | 12 |
COPD, chronic obstructive pulmonary disease.
Approximately half of the admissions for these conditions were repeat admissions during the 12-month period (51 of 109 admissions). After exclusion of patients who had since passed away, 69 patients were eligible to participate. In total, 9 patients consented to participate (13% response rate), along with 16 health professionals, as summarised in tables 2 and 3. No participants dropped out of the study. Interviews were undertaken between September and October 2019, with a duration of 13–33 min for health professional interviews (average 21 min) and 8–48 min for patient interviews (average 30 min). The response rate for health professionals was unable to be calculated as recruitment was via an email invitation to the organisation rather than to individuals.
Table 2.
Characteristics of health professional participants
| Health professional participant number | Discipline | Sex |
| 1 | Pharmacist | Female |
| 2 | Pharmacist | Female |
| 3 | GP practice nurse | Female |
| 4 | Nurse | Male |
| 5 | Physiotherapist | Female |
| 6 | Nurse | Female |
| 7 | Nurse | Male |
| 8 | Nurse | Female |
| 9 | Nurse | Female |
| 10 | Nurse | Female |
| 11 | Nurse | Male |
| 12 | Nurse | Female |
| 13 | GP | Male |
| 14 | GP practice nurse | Female |
| 15 | GP practice nurse | Female |
| 16 | Nurse | Female |
Table 3.
Characteristics of patient participants
| Patient participant number | Health condition (self-described) | Sex | Living alone? |
| 1 | Diabetes and heart condition | Male | Yes |
| 2 | COPD | Male | Yes |
| 3 | COPD | Female | Yes |
| 4 | COPD | Male | No |
| 5 | COPD | Female | Yes |
| 6 | Heart condition | Female | No |
| 7 | Diabetes, respiratory condition | Female | No |
| 8 | Heart condition | Female | Yes |
| 9 | Diabetes | Male | Yes |
COPD, chronic obstructive pulmonary disease.
Qualitative results
Themes and subthemes were mapped onto the existing logic model and new subthemes were added, see figure 1. The new subthemes are described in detail below. Illustrative quotes for each theme/subtheme are outlined in (online supplemental table 1).
Figure 1.
Logic model, themes as identified by patients (P) or health professionals (HP). New themes are denoted with an asterisk.
ihj-2021-000124supp002.pdf (257.3KB, pdf)
Theme 1: contexts of care
In the comparison logic model, contexts of care refer to the various system-level, provider-level and individual-level contexts that influence outcomes of care (such as hospitalisation). At the individual level, individual patient circumstances and context significantly influence their chronic disease management. Patient (individual) contexts include their health status, pre-existing values, self-motivation to learn more about their condition and having the knowledge and skills to act. At the provider level, the context of service provision encompassed health professionals’ skills, values, attributes and workforce availability. At the system level, experience of chronic disease management is dependent on availability of services, within all settings (acute and community), as well as the presence, or absence, of optimal clinical pathways. These themes were also identified in this research (see online supplemental table 1). Many patients could not easily identify the reason for their admission or readily list their health conditions.
New subthemes: socioeconomic disadvantage and isolation
New themes from this research that mapped to the individual-level context included issues relating to socioeconomic disadvantage, poverty, isolation or a lack of support. Socioeconomic disadvantage and isolation/lack of support were found to impact patients’ capacity and confidence to manage their health. A physiotherapist discussed how isolation or a lack of support could influence a patient’s confidence to self-manage and ability to respond to an exacerbation and avoid hospitalisation.
We have a very high incidence of people living alone in [this town] and I think that contributes to just not being confident in managing your chronic illness… and when you start to go down, there is no one there to tell you to go to the doctor or whatever, and so maybe you missed that opportunity where it can be fixed quickly or then, it’s panic stations and I have to go to the hospital because there’s no one around to certainly look after me. (HP 5)
One patient described the reality of their socioeconomic disadvantage and the frustration of this situation not being fully appreciated by their treating doctor.
I couldn’t believe my own doctor who has known me for 30 years or something could say I could just go home, I have been saying to him for 10 years, I’m broke. I can’t get a job, I’m living off New Start (unemployment benefits). It’s not enough. I have not enough food, I’m getting food vouchers to survive. I have to count potatoes. They don’t get it. They don’t get it. They don’t live like that. They don’t see it. They have no f**ing idea that it’s real and I’m not the only one. Right? (P5)
New subthemes: out-of-pocket costs and nuanced context of hospital staffed by GPs
New themes mapping to the provider-level context related to out-of-pocket costs for health services were identified, as was the nuanced context arising from having the hospital staffed by GPs.
A nurse discussed local socioeconomic disadvantage combined with out-of-pocket costs for both GP services and urgent care potentially restricting access to healthcare.
So, considering we have quite a, we do have a very high low socioeconomic group in [this town] Financially to pay for GP services I’d be concerned that they would be limiting their access to medical care. Also having paid Urgent Care (Centre) here as well. (HP16)
One nurse mentioned that occasionally patients were admitted to hospital in order to connect them with beneficial services due to restrictive eligibility criteria.
…it does happen that we do have people admitted for discharge planning. (HP9)
Another nurse discussed a potentially low, and possibly conflicted, threshold for admission.
The hospital admissions are obviously GP driven as well because they have to (emphasis added) admit them (GPs are the admitting doctors). (HP11)
Theme 2: mechanisms for receiving and providing care
In the comparison logic model, mechanisms refer to patient experienced facilitators and barriers to receiving care. Subthemes from the comparator logic model included mechanisms in which consumers describe that their experiences with the management of their chronic disease are highly dependent on developing and maintaining effective interactions and relationships between themselves, health and medical practitioners, family and carers and via continuity of care. In this research, participants also identified that effective relationships are maximised if there is continuity in relationships with health providers, communication is timely and delivered appropriately; trust has developed and there is capacity to receive holistic services and support, particularly in the rural and regional settings in which consumers live (see online supplemental table 1).
New subtheme: affordable care
A strong theme from this research that was not identified in the existing programme logic model related to the affordability of healthcare and potential for cost to be a barrier to access.
They (patients with chronic health conditions) might be looking at $80 for a 15 minute (GP) appointment and they only get $35 back, so if you’re expected to see your GP every week or fortnight, well you can see how people slip through the cracks. (HP8)
A further theme that was not included in the existing logic model related to ability to pay as being a barrier to equitable access to care. A nurse spoke of issues of out-of-pocket costs and access to healthcare and contrasted the local situation to the usual situation in cities.
I think a town like [this town] that’s got so many struggling people, like there’s a large amount of low socioeconomic status people in [this town], it’s a shame that we can’t provide a decent free healthcare service. Like if they were living in the city, there’d be bulk-billing clinics everywhere. (HP8)
Theme 3: outcomes of care
In the comparison logic model, outcomes of care refer to both patient valued outcomes and outcomes of importance to healthcare providers. Subthemes that were identified at the individual patient level included not being a burden, receiving responsive and timely access to care. At the provider level, improved clinical outcomes were discussed, while monetary and resource use was discussed at the health system level. These themes were also identified in this research (see online supplemental table 1).
New subthemes: timely access to care
Receiving responsive and timely access to care was a strong theme that was also identified in this research. However, when mapping this theme onto the existing logic model, a new relationship between the mechanism and outcome data was identified. Similar to the comparator logic model, patient participants typically did not consider their hospitalisations to have been avoidable. As this participant identifies, effective relationships involving communication and trust (mechanism) had a direct impact on a client valued outcome of being able to access responsive and timely access to care, with subsequent impact on resource use.
If he (the GP) listened to me, I might not have been in the situation or as bad as I was. I actually had to get the MICA (Mobile Intensive Care Ambulance) paramedic down to me because that’s how bad I was. I was really sick, and, you know, it might have been a two day stay instead of nine days, if the doctor listened. (P2)
Discussion
This study aimed to better understand PAHs in a rural context in Victoria, Australia, from the perspectives of both patients and health professionals. There was value in exploring both the health professional and patient perspective in this study such that a deeper, more complete picture of PAH could be realised. While the importance of giving patients a voice in this issue has been recognised,8 few studies have included the patient perspective,9 which is important as patients receive care from multiple providers and services.
Mapping of themes to an existing programme logic model21 enabled ongoing development of a PAH framework to identify targets for intervention. The existing programme logic model21 is further strengthened by the addition of a number of new themes from this qualitative research. These included the nuanced context arising from having GPs on staff at the hospital and the inter-related issues of socioeconomic disadvantage and prohibitive out-of-pocket medical expenses. An individual’s income, insurance status,23 socioeconomic status and the cost of care19 have been shown to influence access to healthcare, patient outcomes and hospitalisation in other studies.
Individual contexts identified in this research and the comparative programme logic model have been reinforced in two similar studies in rural Australia which identified factors associated with PAH from the perspectives of patients (lack of support, medication issues, poor mental health, poor understanding of disease)9 and service providers (lack of services, lack of awareness of local services, poverty and transport issues).8 Reiterated in this research and the comparative logic model was also that a patient’s locus of control was linked to their capacity to self-manage.
Key mechanisms around continuity of care that were identified in this research and the comparative logic model have been shown to be associated with PAH24, as have managed care plans25. The value of connecting patients to beneficial services, particularly on discharge, is a core mechanism for continuity of care. Research from rural Canada and Australia demonstrates that a significant proportion of readmissions are preventable if best practice discharge preparation and enactment were followed.25 26
Similar to the comparator logic model, patient participants typically did not consider their hospitalisations to have been avoidable. Many patients could not easily identify the reason for their admission or readily list their health conditions. This appeared particularly so for patients with heart conditions, and although the researchers did not have access to their primary presenting diagnosis, no participants identified ‘heart failure’ as one of their health conditions. Patient lack of awareness of heart failure has been identified previously27 and it is thought that the term may be being avoided by health professionals as it can been seen as anxiety provoking.28 Alternatively, heart failure has been recognised to be difficult to diagnose and differentiate from comorbid conditions.29
Identified in this study were a mixture of issues that could be considered ‘impactable’ and other issues that are far less so. For example, the socioeconomic status of a town is complex and unable to be readily influenced from within the health system. However, embedding individualised, meaningful exercise and rehabilitation programmes, action plans and GP management plans may be far more readily influenced, within the health system. This point has been raised previously, in that short-term improvements to healthcare access are more feasible via changes to health service resourcing than addressing population needs.30 The influence of socioeconomic disadvantage and psychosocial factors on PAHs was recognised by health professional and patient participants alike. However, there was a level of frustration associated with the inflexibility of services to respond to these needs. Participants appreciated the value of the long term, local health professional workforce and proactive local council in provision of services. The role of ‘place’ in health and well-being has been well recognised.31
The themes identified at individual, professional and system level are highly inter-related. This inter-relationship between contexts, mechanisms and outcomes at each of these levels was demonstrated by mapping themes to the existing logic model. For example, socioeconomic disadvantage (individual-level context) combined with out-of-pocket healthcare costs (individual and system level mechanisms) influenced the degree to which healthcare was accessible (individual outcome). Levesque’s conceptual framework of healthcare access reinforces this finding, in which realised access is a function of the costs (both direct and indirect) of receiving health services and the patient’s economic ability to pay.32
In our study, knowledgeable, skilled and proactive health professionals enabled connection of patients with beneficial services. Information sharing, continuity of care and trust impacted relationships between patients and their healthcare team. Family, friends or community groups provided care for patients, allayed fears, increased confidence in self-management and supported connectedness and independence. Some patients felt that others were more deserving or in greater need of the support. When a patient did not have these support networks they were more vulnerable when they became unwell. On two occasions, patient participants identified that not being able to see their usual GP, who listened to them and took their concerns seriously, may have contributed to their hospitalisation.
The relationships between contexts, mechanisms and outcomes at the individual patient and system level are core to the reference logic model which identifies the ‘appropriateness’ of the interaction between the healthcare provider (coordination of care, continuity of care, interpersonal skills) and influences the patient’s ability to engage with healthcare services (empowerment, support from caregivers)32 and as such has an impact on the outcomes of care.
Limitations
These findings have limited generalisability, as this study was limited to a single health service. However, the study benefitted from the perspectives of both health professionals and patients in a region that has experienced high rates of PAH for several chronic health conditions over a number of years. Comparison of findings to a relevant programme logic model was also valuable. Findings may be of value to other rural areas facing similar issues.
Conclusion
Issues related to PAH in this rural context were complex and inter-related. These issues encompassed access to, and disease management within, health services and cost as a barrier to healthcare access. These results suggest that improved access to primary care and support services may ultimately reduce unnecessary hospitalisations.
Acknowledgments
The authors wish to thank the participants of this study and staff at the recruiting sites. The authors sincerely thank the team involved in the potentially avoidable hospitalisations project, in particular the Reference Group, the Governance Group, Heather Betts, Bronwyn Phillips and Tammie Long.
Footnotes
Twitter: @kristenglenist1
Contributors: KG and TA designed the study and collected, analysed and interpreted data. RD acted as the independent third person during analysis. KG, TA, RD and AM drafted the article and revised it critically for important intellectual content. SW and DK contributed to subsequent drafts. All authors read and approved the final draft. KG is the Guarantor.
Funding: This research received funding from the Murray Primary Health Network. KG and RD’s work was supported by the Australian Government Department of Health through the Rural Health Multidisciplinary Training Programme.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Data are not publicly available due to risk of participant identifiability.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Northeast Health Wangaratta Human Research and Ethics Committee (Project ID: 175, August 2016). Participants gave signed, informed consent to participate in the study before taking part.
References
- 1. Australian Institute of Health and Welfare . Potentially preventable hospitalisations in Australia by age groups and small geographic areas, 2017–18, 2019. Available: https://www.aihw.gov.au/reports/primary-health-care/potentially-preventable-hospitalisations/contents/overview
- 2. Australian Institute of Health and Welfare . Rural & remote health, 2019. Available: https://www.aihw.gov.au/reports/phe/193/rural-remote-health/contents/access-to-health-care [Accessed 27 Feb 2020].
- 3. Australian Institute of Health and Welfare . Disparities in potentially preventable hospitalisations across Australia, 2012-13 to 2017-18. Canberra: AIHW, 2020. [Google Scholar]
- 4. Passey ME, Longman JM, Johnston JJ, et al. Diagnosing potentially preventable hospitalisations (DaPPHne): protocol for a mixed-methods data-linkage study. BMJ Open 2015;5:e009879. 10.1136/bmjopen-2015-009879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Eggli Y, Desquins B, Seker E, et al. Comparing potentially avoidable hospitalization rates related to ambulatory care sensitive conditions in Switzerland: the need to refine the definition of health conditions and to adjust for population health status. BMC Health Serv Res 2014;14:25. 10.1186/1472-6963-14-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hodgson K, Deeny SR, Steventon A. Ambulatory care-sensitive conditions: their potential uses and limitations. BMJ Qual Saf 2019;28:429–33. 10.1136/bmjqs-2018-008820 [DOI] [PubMed] [Google Scholar]
- 7. Muenchberger H, Kendall E. Predictors of preventable hospitalization in chronic disease: priorities for change. J Public Health Policy 2010;31:150–63. 10.1057/jphp.2010.3 [DOI] [PubMed] [Google Scholar]
- 8. Longman JM, Singer JB, Gao Y, et al. Community based service providers' perspectives on frequent and/or avoidable admission of older people with chronic disease in rural NSW: a qualitative study. BMC Health Serv Res 2011;11:265. 10.1186/1472-6963-11-265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Longman JM, Rix E, Johnston JJ, et al. Ambulatory care sensitive chronic conditions: what can we learn from patients about the role of primary health care in preventing admissions? Aust J Prim Health 2018. 10.1071/PY17191. [Epub ahead of print: 06 08 2018]. [DOI] [PubMed] [Google Scholar]
- 10. Falster MO, Leyland AH, Jorm LR. Do hospitals influence geographic variation in admission for preventable hospitalisation? A data linkage study in New South Wales, Australia. BMJ Open 2019;9:e027639. 10.1136/bmjopen-2018-027639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Baxter SK, Blank L, Woods HB, et al. Using logic model methods in systematic review synthesis: describing complex pathways in referral management interventions. BMC Med Res Methodol 2014;14:62. 10.1186/1471-2288-14-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 13. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8:45 http://www.biomedcentral.com/content/pdf/1471-2288-8-45.pdf 10.1186/1471-2288-8-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 15. Australian Government Department of Health . Modified Monash model, 2015. Available: http://www.doctorconnect.gov.au/internet/otd/publishing.nsf/Content/MMM_locator [Accessed 31 Jun 2015].
- 16. State government of Victoria department of health. Benalla, 2014. Available: http://docs.health.vic.gov.au/docs/doc/Benalla- [Accessed 19 Jul 2021].
- 17. Glenister K, Disler R, Hulme A, et al. The mosaic of general practice bulk billing in regional Victoria. Aust J Gen Pract 2019;48:77–8. 10.31128/AJGP-07-18-4659 [DOI] [PubMed] [Google Scholar]
- 18. Benalla Health . Benalla health strategic plan 2016-2020, 2016. Available: https://www.benallahealth.org.au/userfiles/files/Benalla%20Health%20Strategic%20Plan%202016-2020%20-%20full%20version.pdf
- 19. Erny-Albrecht K, Oliver-Baxter J, Bywood P. Primary health care-based programmes targeting potentially avoidable hospitalisations in vulnerable groups with chronic disease. PHCRIS Policy Issue Review. Adelaide: Primary Health Care Research & Information Service, 2016. [Google Scholar]
- 20. Srivastava A, Thomson SBJC, eJournal GAL. Framework analysis: a qualitative methodology for applied policy research. J Admin Gove 2009;4:72–9. [Google Scholar]
- 21. Moran A, Chapman G, Picard R, et al. Consumer experiences of chronic obstructive pulmonary disease in regional Australia: a mixed methods study and logic model to identify consumer-experience mechanisms to avoid hospital and enhance outcomes. Patient Exp J 2020;7:98–108. 10.35680/2372-0247.1421 [DOI] [Google Scholar]
- 22. Guest G, Bunce A, Johnson L. How many interviews are enough?: an experiment with data saturation and variability. Field Metho 2006;18:59–82. [Google Scholar]
- 23. Minteer S, Long T, Harrigan S, et al. A logic model for understanding and reducing preventable hospitalizations. R I Med J 2015;98:57–9. [PubMed] [Google Scholar]
- 24. Falster MO, Jorm LR, Douglas KA, et al. Sociodemographic and health characteristics, rather than primary care supply, are major drivers of geographic variation in preventable hospitalizations in Australia. Med Care 2015;53:436–45. 10.1097/MLR.0000000000000342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ross Baker G, et al. Enhancing the continuum of care. Report of the avoidable hospitalization Advisory panel 2011.
- 26. Provencher V, Clemson L, Wales K, et al. Supporting at-risk older adults transitioning from hospital to home: who benefits from an evidence-based patient-centered discharge planning intervention? Post-hoc analysis from a randomized trial. BMC Geriatr 2020;20:84. 10.1186/s12877-020-1494-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Selan S, Siennicki-Lantz A, Berglund J, et al. Self-awareness of heart failure in the oldest old-an observational study of participants, ≥ 80 years old, with an objectively verified heart failure. BMC Geriatr 2016;16:23. 10.1186/s12877-016-0195-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Barnes S, Gott M, Payne S, et al. Communication in heart failure: perspectives from older people and primary care professionals. Health Soc Care Community 2006;14:482–90. 10.1111/j.1365-2524.2006.00636.x [DOI] [PubMed] [Google Scholar]
- 29. Fry M, McLachlan S, Purdy S, et al. The implications of living with heart failure; the impact on everyday life, family support, co-morbidities and access to healthcare: a secondary qualitative analysis. BMC Fam Pract 2016;17:139. 10.1186/s12875-016-0537-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Frenk J. Concept and measurement of accessibility. Salud pública de México 1992;27:438–53. [PubMed] [Google Scholar]
- 31. Eyles J, Williams A. Sense of place, health, and quality of life. Aldershot: Geographies of health, 2008. [Google Scholar]
- 32. Levesque J-F, Harris MF, Russell G. Patient-Centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health 2013;12:18. 10.1186/1475-9276-12-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ihj-2021-000124supp001.pdf (163.7KB, pdf)
ihj-2021-000124supp002.pdf (257.3KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Data are not publicly available due to risk of participant identifiability.