Forced Oscillation Technique (FOT) is a noninvasive method of measuring respiratory mechanical properties that utilizes pressure waves applied to the mouth during tidal breathing across a range of frequencies [1]. While FOT has been studied extensively over several decades, questions remain on how to best interpret these measurements across a variety of conditions. One such condition is when FOT is measured following deep breathing maneuvers given the known effects of deep breaths on lung mechanics [2, 3]. For example, a deep inspiration to maximum inflation in healthy individuals appears to be bronchoprotective [4], while expiration to maximum deflation can result in airway closure [5]. Current technical standards for FOT use recommend avoiding deep breaths or forced exhalation maneuvers prior to oscillometric testing [6], but whether these maneuvers influence standard oscillometry measurements performed during tidal breathing remains unclear.
A single-center cohort of healthy subjects was recruited to participate in this observational study. An Institutional Research Subject Review Board approved this study and written informed consent was obtained from all participants. Demographic and basic medical information was collected for each subject including: age, biological sex, height, weight, and history of lung disease. FOT measurements were made before and after a deep breathing maneuver. Before the initial FOT measurement, subjects were asked to avoid any deep breathing, coughing, sighing, or yawning for five to ten minutes. FOT measurements were then taken using a THORASYS® tremoFlo® C-100 Airwave Oscillometry System™. Measurements were made at least three times to ensure repeatability for a R5 coefficient of variance of <10%. The subject was then asked to perform an “inflation-deflation” deep breathing maneuver consisting of 5 sequential breaths to maximal inflation (TLC) followed by maximal lung deflation (RV). Within seconds of completing this inflation-deflation maneuver, FOT measurements were repeated. Pre- and post-inflation-deflation oscillometry variables were measured including common parameters of interest; mean low frequency resistance (R5), mean frequency dependence of resistance (R5-R20), and mean area of reactance (Ax). Differences in pre- and post-inflation-deflation values were determined using a paired t-test with statistical significance defined as p < 0.05.
A total of 20 subjects (10 female, 10 male) with a median age of 36.1 years (23-59) were enrolled. The median height was 171 cm (158-185), median weight 76 kg (57-104), and median BMI was 26.2 kg/m2 (18.8-42.0). One subject reported a history of mild-intermittent asthma, but was not on regular therapy. Pre- and post-inflation-deflation oscillometry values are shown in Table 1. The pre- and post-inflation-deflation measurements of commonly reported outcome parameters for all subjects were within normal limits according to normative data referenced by the tremoFlo® software.
Table 1. Oscillometry Data.
Pre- and post-inflation-deflation maneuver oscillometry variables of interest and the calculated mean differences including confidence intervals and p-values. Common parameters of interest including R5, R5-R20, and Ax are reported. Exploratory parameters of interest; Inspiratory R5, Expiratory R5, and End-Expiratory R5 are reported. The comparison of mean R5 pre-inflation-deflation maneuver to the first R5 measurement post-inflation-deflation maneuver is also included.
| Oscillometry Variable | Pre-Inflation- Deflation |
Post-Inflation- Deflation |
Mean Difference |
|---|---|---|---|
| R5, mean | 2.73 ± 1.07 | 2.80 ± 1.20 | 0.0687 (95% CI −0.0965 to 0.233, p=0.396) |
| R5-R20, mean | −0.056 ± 0.20 | −0.031 ± 0.25 | −0.0250 (95% CI −0.0652 to 0.115, p=0.569) |
| Ax, mean | 3.80 ± 2.37 | 3.89 ± 2.58 | 0.0887 (95% CI −0.602 to 0.779, p=0.791) |
| Inspiratory R5, mean | 2.61 ± 0.99 | 2.55 ± 0.91 | −0.0587 (95% CI −0.214 to 0.0969, p=0.439) |
| Expiratory R5, mean | 2.82 ± 1.14 | 2.94 ± 1.36 | 0.114 (95% CI −0.0869 to 0.314, p=0.250) |
| End-Expiratory R5, mean | 2.48 ± 1.08 | 2.45 ± 1.21 | −0.0315 (95% CI −0.222 to 0.159, p=0.733) |
| Mean R5 Pre-Inflation-Deflation vs | 2.73 ± 1.07 | 3.00 ± 1.24 | 0.273 (95% CI 0.0104 to 0.535, p=0.042) * |
| First Measurement Post-Inflation-Deflation R5 |
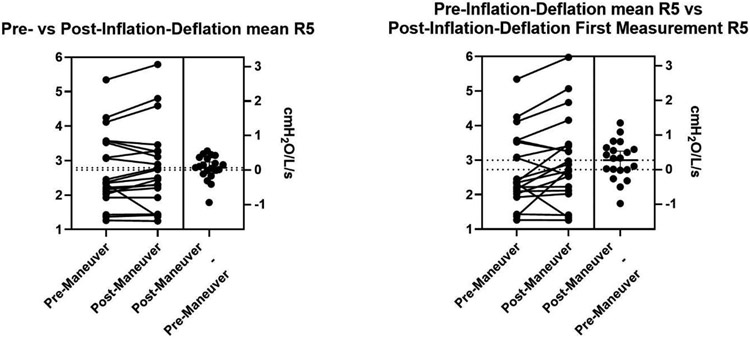
Post-inflation-deflation maneuver oscillometry variables were similar to pre-inflation-deflation values for the majority of parameters of interest (Table 1). The R5 measured over the first breaths following the inflation-deflation maneuver was significantly increased to 3.00 cmH2O/L/s ± 1.24 compared to the pre-inflation-deflation mean R5 of 2.73 cmH2O/L/s ± 1.07 (95% CI 0.0104 to 0.535, p = 0.042). This difference in R5 post-inflation-deflation was not maintained when the mean R5 over three measurements post-inflation-deflation maneuver was compared to the mean R5 pre-inflation-deflation. Figure 1 depicts the comparisons of pre- and post-inflation-deflation mean R5 as well as post-inflation-deflation R5 over the first post-inflation-deflation measurement.
Figure 1.
Pre- and post-Inflation-Deflation mean R5 for individual subjects as well as mean of differences (LEFT). Pre-Inflation-Deflation mean R5 vs post-Inflation-Deflation R5 over first breath for the individual subjects as well as mean of differences (RIGHT).
In this single-center observational study of healthy subjects, we evaluated whether a deep breathing maneuver, five deep breaths from TLC to RV, would affect commonly measured oscillometry variables. The majority of oscillometry variables evaluated were not significantly different suggesting that a significant deep breathing maneuver from TLC to RV does not affect standard oscillometry measurements in healthy subjects. Although our study may not have had sufficient power to detect smaller differences in oscillometry variables, we believe that even a small statistical difference in pre- and post-inflation-deflation oscillometry variables in a larger cohort is unlikely to have clinical significance.
While we did not observe a significant difference between mean R5 pre- and post-inflation-deflation maneuver, the R5 over the first post-inflation-deflation measurement was slightly elevated when compared to the pre-inflation-deflation mean R5. This slight increase in R5 may represent transient airway narrowing from the last inflation-deflation maneuver, which involved forceful exhalation to RV. This increase in R5 was not maintained when the remaining post-inflation-deflation measurements were averaged, suggesting that any airway narrowing present quickly resolves once regular tidal breathing is resumed. In other studies where oscillometry is measured in real-time over a deep breathing maneuver, any airway narrowing or re-narrowing seems to occur within one minute once tidal breathing is resumed [5, 7]. Our limited observational data in this study suggests that slight changes in airway resistance following inflation-deflation maneuvers are transient and do not impact oscillometry variables when measured in the standardized fashion using three separate measurements to achieve a R5 coefficient of variance of <10%.
In conclusion, this observational study of healthy subjects adds to the growing body of data informing whether volume history affects standard oscillometry measurements. More study using vital capacity maneuvers and spirometry are needed to determine if these tests affect measurements of lung function obtained by oscillometry in healthy subjects, or those with lung diseases.
Funding Information
The project described was supported by Award Number T32 HL066988, Multidisciplinary Training in Pulmonary Research and the Parkes Family Foundation.
Abbreviations:
- FOT
Forced Oscillation Technique
- TLC
Total Lung Capacity
- RV
Residual Volume
- R5
Low-frequency resistance at 5 Hz
- R5-R20
Frequency dependence of resistance
- Ax
Area under the reactance curve
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interest
Patrick Donohue, MD, Nicholas C Love MD, Margaret Connolly MD, Sandhya Khurana MD, and Steve N Georas MD declare that they have no known competing financial interests or disclosures that may have influenced the work reported in this paper.
Informed Consent
The Research Subjects Review Board approved this study and written informed consent was obtained for all human subjects. This study was registered at clinicaltrials.gov (NCT05085795).
REFERENCES
- 1.Pride NB. Forced oscillation techniques for measuring mechanical properties of the respiratory system. Thorax. 1992. Apr;47(4):317–20. 10.1136/thx.47.4.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nadel JA, Tierney DF. Effect of a previous deep inspiration on airway resistance in man. J Appl Physiol. 1961. Jul;16:717–9. 10.1152/jappl.1961.16.4.717. [DOI] [PubMed] [Google Scholar]
- 3.Oostveen E, Peslin R, Gallina C, Zwart A. Flow and volume dependence of respiratory mechanical properties studied by forced oscillation. J Appl Physiol (1985). 1989. Dec;67(6):2212–8. 10.1152/jappl.1989.67.6.2212. [DOI] [PubMed] [Google Scholar]
- 4.Scichilone N, Kapsali T, Permutt S, Togias A. Deep inspiration-induced bronchoprotection is stronger than bronchodilation. Am J Respir Crit Care Med. 2000. Sep;162(3 Pt 1):910–6. 10.1164/ajrccm.162.3.9907048. [DOI] [PubMed] [Google Scholar]
- 5.Kelly VJ, Brown NJ, Sands SA, Borg BM, King GG, Thompson BR. Effect of airway smooth muscle tone on airway distensibility measured by the forced oscillation technique in adults with asthma. J Appl Physiol (1985). 2012. May;112(9):1494–503. 10.1152/japplphysiol.01259.2011. [DOI] [PubMed] [Google Scholar]
- 6.King GG, Bates J, Berger KI, Calverley P, de Melo PL, Dellacà RL, Farré R, Hall GL, Ioan I, Irvin CG, Kaczka DW, Kaminsky DA, Kurosawa H, Lombardi E, Maksym GN, Marchal F, Oppenheimer BW, Simpson SJ, Thamrin C, van den Berge M, Oostveen E. Technical standards for respiratory oscillometry. Eur Respir J. 2020. Feb 27;55(2):1900753. 10.1183/13993003.00753-2019. [DOI] [PubMed] [Google Scholar]
- 7.Gazzola M, Lortie K, Henry C, Mailhot-Larouche S, Chapman DG, Couture C, Seow CY, Paré PD, King GG, Boulet LP, Bossé Y. Airway smooth muscle tone increases airway responsiveness in healthy young adults. Am J Physiol Lung Cell Mol Physiol. 2017. Mar 1;312(3):L348–L357. 10.1152/ajplung.00205.2019. [DOI] [PubMed] [Google Scholar]