Abstract
Objective and Background:
Little is known about pediatric psychotropic medication use in the emergency department (ED), despite a rise in mental and behavioral health visits. This study describes psychotropic medication use in a nationally representative sample of pediatric mental and behavioral health ED visits over a 14-year period.
Methods:
We conducted a cross-sectional analysis of pediatric (6–17 years) mental and behavioral health ED visits using the National Hospital Ambulatory Medical Care Survey, 2006–2019. We describe administration of psychotropic medications by medication type, diagnosis, and over time. Using multivariable survey weighted logistic regression, we examine associations between medication administration and sociodemographics.
Results:
A psychotropic medication was administered in 11.4% of the estimated 11,792,860 pediatric mental and behavioral health ED visits in our sample. Benzodiazepines were administered most frequently (4.9% of visits). Visits with anxiety disorders had the highest frequency of psychotropic medication use (26.7%). Visits by Black non-Hispanic patients had a 60% decreased odds of medication administration compared to visits for White non-Hispanic patients. Visits with public compared to private insurance had a 3.5 times increased odds of psychotropic polypharmacy. The proportion of visits in which a psychotropic medication was administered did not change statistically over time.
Conclusions:
A psychotropic medication was administered in one in ten pediatric mental and behavioral health ED visits. Use differed by sociodemographics but did not change over time. As more youth seek mental and behavioral healthcare in the ED, we must better understand appropriate medication use to ensure quality and equitable care.
Keywords: Mental and behavioral health, emergency medicine, emergency service, health equity
Introduction
An increasing number of United States (US) youth receive care in emergency departments (EDs) for mental and behavioral health needs.1,2 The COVID-19 pandemic has only exacerbated this trend.3–5 Psychotropic medications are often a necessary component of ED management, for example, to address acute symptoms (e.g. anxiety), to sedate in the setting of agitation when safety is at risk, or to administer home medications.6–8 However, psychotropic medications can cause adverse effects in children, including oversedation, antidepressant related suicidal symptoms, benzodiazepine related substance use, and antipsychotic related extrapyramidal symptoms and metabolic dysregulation.9 Despite risks, minimal data guide psychopharmacological management of pediatric patients in the ED.6,7 In response to U.S. Food and Drug Administration recommendations, prescriptions of psychotropic medications in the office-based setting decreased throughout the 2000s.10–12 Corresponding ED trends are unknown.
Given the paucity of evidence-based guidance,6,13 psychotropic medication use in the ED is likely variable and subject to discretion and disparities in care.14,15 Existing evidence demonstrates racial, ethnic, gender, and insurance-based disparities in the prescription of antipsychotics and polypharmacy in office-based care,10 as well as in the administration of psychotropic medications for the purpose of restraint in children’s hospitals EDs.16 Variation in care is potentially more pronounced in low pediatric volume EDs, where over 90% of pediatric patients receive emergency care,17 but only one-third of which have pediatric mental and behavioral health policies to guide management.18 Beyond prejudice at the point of care, structural factors impacting healthcare access, may influence the severity of clinical presentation and likelihood of medication use.19
Understanding the national scope of psychotropic medication use in EDs and variation by sociodemographic group can help inform efforts to standardize guidelines, train providers, and provide adequate resources to ensure EDs deliver safe and equitable care for children with mental and behavioral health needs. This study describes the administration of psychotropic medications in a nationally representative sample of youth ED visits for mental and behavioral health needs over a 14-year period, focusing on sociodemographic differences and temporal trends.
Methods
Design and Data
We conducted a cross-sectional analysis of pediatric ED visits between 2006–2019 using the National Hospital Ambulatory Medical Care Survey (NHAMCS). NHAMCS is an annual survey of ED visits to US hospitals administered by the National Center for Health Statistics (NCHS). NHAMCS uses three-stage probability sampling to provide weighted national estimates.20 NHAMCS data are deidentified and publicly available. This study was deemed exempt from the Yale University School of Medicine institutional review board review.
Sample
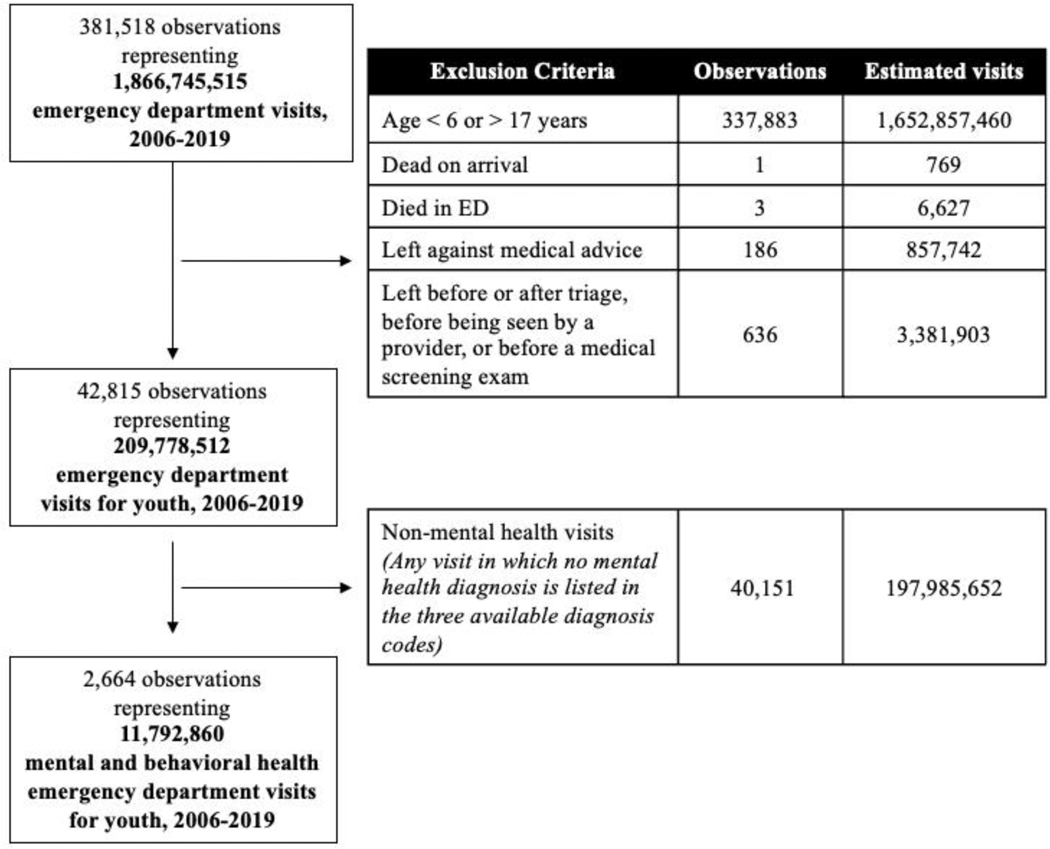
Our study included mental and behavioral health ED visits, as defined below, for patients ages 6–17 years.1,21,22 We excluded visits of patients who died in the ED or left against medical advice, before triage, or before being seen by a provider (Figure 1).21
Figure 1:
Flow chart – study sample and inclusion criteria.
Mental and behavioral health ED visits
Consistent with prior work,21 we defined ED visits as mental and behavioral health visits if any of the first three discharge International Classification of Diseases (ICD)-9 or 10 diagnosis codes were included in the Child and Adolescent Mental Health Disorder Classification System (CAMHD-CS) (Figure 1).23
We further categorized mental and behavioral health visits into diagnostic groups: suicide (ideation/attempt) or self-harm; anxiety disorders; substance use disorders; depressive disorders; disruptive, impulse control or conduct disorders; bipolar and related disorders; autism spectrum or neurodevelopmental disorders; trauma or stressor-related disorders; and other mental and behavioral health diagnoses. We determined diagnosis groups based on established CAMHD-CS categories,23 and by collapsing several categories based on clinical alignment, and sample frequency (Supplemental Table A).
Variables
Psychotropic medications
Each NHAMCS visit documents at least nine medications. We identified medications as psychotropic based on Multum’s classification system,20 and prior pediatric literature.10,16 We included all medications categorized by Multum’s as psychotherapeutic (antidepressants and antipsychotics), stimulants and benzodiazepines. Based on prior literature,10,16 we also included select medications from the following Multum’s categories: barbiturates; miscellaneous anxiolytics, sedatives, and hypnotics; anticonvulsants; general anesthetics; and antiadrenergic agents. The aggregate medication list was divided into seven groups: antipsychotics, benzodiazepines, antihistamines, antidepressants, anticonvulsants, stimulants, and other psychotropic agents. We excluded antihistamines (eg. diphenhydramine), anticonvulsants (eg. valproic acid), and antiadrenergic medications (eg. clonidine) for diagnoses related to allergy, seizure, or cardiac presentations respectively (full list of medications available upon request).
Outcome variables
Our primary outcome was the proportion of visits in which any psychotropic medication was administered, by any route, in the ED. Our secondary outcomes were the proportion of visits in which (a) >1 psychotropic medication (polypharmacy) was administered in the ED, and (b) any psychotropic medication was prescribed upon ED discharge. Our dataset did not include route of administration, the medication’s indication (by diagnosis, acute vs. chronic, new vs. home), or whether a prescription was filled upon discharge.
Additional variables
Sociodemographic variables included race and ethnicity (four-level variable created by the NCHS), insurance type, patient age, and sex. Visit variables included arrival time, region, disposition, and year.
Analysis
Primary Analysis
We reported by medication type, the proportion of mental and behavioral health visits in which a psychotropic medication was (a) administered in the ED and (b) prescribed upon ED discharge. We additionally reported by diagnostic category, the proportion of visits in which a psychotropic medication was administered in the ED. We reported both the number of visit observations and survey-weighted national estimates. Following NCHS recommendations, we did not report population estimates for fewer than 30 observations or relative standard errors > 30%.20
In the most recent era (2012–2019), we used multivariable survey weighted logistic regression to examine associations between two outcomes – the proportion of visits in which any and >1 psychotropic medication was administered - and sociodemographic characteristics. In both models, we adjusted for race and ethnicity, insurance type, age, sex, arrival time, geographic region, and disposition. For race and ethnicity, we used visits for White non-Hispanic patients as the reference category because these visits had the highest psychotropic medication use. To avoid inappropriately attenuating racial and ethnic disparities in care, we did not adjust for diagnosis in our models given evidence of bias in mental and behavioral health diagnoses.24,25
Secondary Analysis
We examined trends in psychotropic medication use over time by comparing four periods: 2006–2008, 2009–2011, 2012–2015, and 2016–2019. We reported average yearly survey weighted national estimates and the proportion of mental and behavioral health ED visits for youth with (a) any psychotropic medication administered in the ED, specifically (b) an antipsychotic and (c) benzodiazepine administered in the ED, and lastly (d) any psychotropic medication prescribed upon ED discharge. To test statistical significance, we conducted pairwise comparisons using logistic regression between each of the consecutive time groups.
For medications administered in the ED, we also examined trends over time by sociodemographic subgroups. Due to sample size constraints, we compared two time periods (2012–2019 to 2006–2011). All models were examined at the visit level, using survey weighted estimates. All tests of statistical significance utilized an alpha level of 0.05. All analyses were conducted using Stata v. 16.1.
Results
Primary Analysis
We studied 2,664 records, which, after survey weighting, represented approximately 11,792,000 pediatric mental and behavioral health ED visits between 2006–2019 (Figure 1). 59.5% of estimated visits were for White non-Hispanic patients, 19.8% for Black non-Hispanic, 17.2% for Hispanic, and 3.5% for patients with an “other” race/ethnicity. 45.2% of visits were for patients with public insurance (37.7% private and 18.1% “other”). 74.4% of visits were for youth 13–17 years old. 53.0% of visits were by female patients.
A psychotropic medication was administered during 11.4% (95%CI 9.6–13.1%) of all mental and behavioral health visits and more than one psychotropic during 3.6% (95%CI 2.6–4.6%) of visits. A psychotropic medication was given as a prescription upon discharge for 8.8% (95%CI 7.0–10.6%) of visits. (Table 1).
Table 1:
Frequency of psychotropic medications administered in the emergency department and prescribed upon discharge from youth mental and behavioral health emergency department visits, by medication type (2006–2019).
| Administered in the Emergency Department* | Prescribed upon Discharge* | ||||||
|---|---|---|---|---|---|---|---|
| Type of Medication | Most Common Medication in Class (Generic) | N a | Estimate b | % Visitsc (95% CI) | N a | Estimate b | % Visits (95% CI) |
| Any psychotropic | Lorazepam | 352 | 1,341,452 | 11.4 (9.6–13.1) | 234 | 1,040,449 | 8.8 (7.0–10.6) |
| >1 Psychotropic | Haloperidol/Lorazepam | 128 | 426,080 | 3.6 (2.6–4.6) | 89 | 338,009 | 2.9 (2.8–3.9) |
| Benzodiazepines | Lorazepam | 135 | 582,751 | 4.9 (3.8–6.1) | 51 | 295,295 | 2.5 (1.5–3.5) |
| Antipsychotics | Haloperidol | 145 | 419,469 | 3.6 (2.6–4.5) | 92 | 329,921 | 2.7 (2.8–3.6) |
| Antihistamines | Diphenhydramine | 86 | 394,850 | 3.4 (2.2–4.5) | 42 | 268,338 | 2.3 (2.0–3.5) |
| Antidepressants | Sertraline | 69 | 216,424 | 1.8 (2.2–2.6) | 65 | 245,448 | 2.1 (1.3–2.9) |
| CNS stimulants | Methylphenidate | 35 | 119,846 | 1.0 (0.4–1.6) | 52 | 168,803 | 1.4 (0.8–2.0) |
| Anticonvulsants | Divalproex sodium | 39 | 116,878 | 1.0 (0.5–1.5) | 32 | 95,269 | 0.8 (0.4–1.2) |
| Other psychotropics | Clonidine | 30 | 133,301 | 1.1 (0.6–1.7) | 31 | 132,028 | 1.1 (0.5–1.8) |
N indicates the number of observations in the sample.
Estimate indicates survey weighted national estimates.
A single visit may list up to 9 medications. Individual visits may fall under multiple medication categories. Therefore, the percentage of visits for each individual medication do not add to 100%, nor the percentage of visits in which any psychotropic medication was administered.
Dataset is unable to identify route of administration, indication, or whether a medication is new to the patient or part of a patient’s home medication regimen.
Benzodiazepines were the most frequent medication type administered during the visit (4.9% of visits; 95%CI 3.8–6.1%), followed by antipsychotics (3.6%; 95%CI 2.6–4.5%) antihistamines (3.4%; 95%CI 2.2–4.5%), antidepressants (1.2%; 95%CI 2.2–2.6%), stimulants (1.0%; 95%CI 0.4–1.6%), anticonvulsants (1.0%; 95%CI 0.5–1.5%), and other psychotropic medications (1.1%; 95%CI 0.6–1.7%) (Table 1). Visit duration was on average eight hours longer for visits in which an antidepressant or stimulant was given compared to visits in which other psychotropic medications were given (8.3 hours; 95%CI 3.2–13.3 hours). The distribution of psychotropic medication types differed if medications were prescribed upon discharge; antipsychotics (2.7%) were prescribed most frequently followed closely by benzodiazepines (2.5%), antihistamines (2.3%), antidepressants (2.1%) and stimulants (1.4%) (Table 1).
Of all pediatric mental and behavioral health visits, the most common diagnosis was anxiety (13.3%; 95%CI 11.6–15.8%), followed by depressive (10.7%; 95%CI 8.6–12.8%) and substance use (10.1%; 95%CI 8.3–11.8%) disorders (Table 2). Visits with an anxiety diagnosis most frequently had a psychotropic medication administered (26.7%; 95%CI 18.7–33.6). A psychotropic medication was administered during 22.1% (95%CI 12.0–32.2%) of visits with bipolar and related disorders, 10.0% (95%CI 3.6–12.3%) of visits with depressive disorders, and in 12.6% (95%CI 7.9–17.3%) of visits with diagnoses categorized as “other mental and behavioral health diagnoses.”
Table 2:
Frequency of psychotropic medications administered during youth mental and behavioral health emergency department visits, by diagnosis (2006–2019).
| Mental and Behavioral Health Emergency Department Visits by Diagnosis | Psychotropic Medication Administered During Mental and Behavioral Health Emergency Department Visit | |||||
|---|---|---|---|---|---|---|
| Type of Diagnosisa | Na | Estimateb | % of Visitsc (95% CI) | Na | Estimateb | % of Visits (95% CI ) |
| Anxiety | 318 | 1,616,322 | 13.7 (11.6–15.8) | 79 | 431,330 | 26.7 (19.7–33.6) |
| Depressive | 232 | 1,261,804 | 10.7 (8.6–12.8) | 30 | 125,640 | 10.0 (3.6–16.3) |
| Substance Use | 277 | 1,187,610 | 10.1 (8.3–11.8) | N/R | N/R | N/R |
| Suicide or Self-Harm | 194 | 908,760 | 7.7 (6.1–9.4) | N/Rd | N/R | N/R |
| Disruptive/Impulse Control | 152 | 551,522 | 4.7 (3.1–6.3) | N/R | N/R | N/R |
| Bipolar and Related | 139 | 510,776 | 4.3 (3.2–5.5) | 31 | 112,874 | 22.1 (12.0–32.2) |
| ASD/Neurodevelopmental | 89 | 437,136 | 3.7 (2.6–4.9) | N/R | N/R | N/R |
| Trauma or Stressor-Related | 34 | 99,378 | 0.8 (0.4–1.3) | N/R | N/R | N/R |
| Other Mental and Behavioral Health Diagnosese | 318 | 1,196,269 | 10.1 (8.2–12.1) | 64 | 150,791 | 12.6 (7.9–17.3) |
N indicates the number of observations in the sample.
Estimate indicates survey weighted national estimates.
A single visit can list up to 3 diagnoses. Individual visits may fall under multiple diagnosis categories. Therefore, the percentage of visits for each individual diagnosis do not add to 100%, nor the percentage of visits in which any psychotropic medication was administered.
N/R, not reportable because of unreliable survey-weighted estimates (<30 unweighted observations or relative SEs >30%).
The most common diagnosis in the “Other Mental and Behavioral Health Diagnoses” category was “Unspecified episodic mood disorder,” followed by other diagnoses under the CAMHD-CS categories of “mental health symptoms” and “miscellaneous” mental and behavioral health disorders.
Among visits in the most recent period (2012–2019), the odds of psychotropic medication administration differed by race and ethnicity after adjustment for other visit characteristics. For visits by Black non-Hispanic patients, there was a 62% decreased odds of psychotropic medication administration compared to visits for White non-Hispanic patients (OR 0.38; 95%CI 0.18–0.77). For visits resulting in discharge, there was a 52% decreased odds of psychotropic medication administration in the ED compared to visits resulting in admission (OR 0.48, 95%CI 0.30–0.75). Administration of psychotropic medications in the ED did not differ statistically by insurance, age, or sex (Table 3).
Table 3:
Adjusted odds of psychotropic medication administration during youth mental and behavioral health emergency department visits (2012–2019).
| Adjusted Odds of Any Psychotropic Medication Administration during Emergency Department Visit | Adjusted Odds of > 1 Psychotropic Medication Administered (of visits with any psychotropic medication administration) | |||
|---|---|---|---|---|
| aORa | 95% CI | aOR | 95% CI | |
| Race and Ethnicity | ||||
| White non-Hispanic | Ref | Ref | Ref | Ref |
| Black non-Hispanic | 0.38 | (0.18–0.77) | 0.73 | (0.12–4.07) |
| Hispanic | 0.67 | (0.36–1.22) | 0.32 | (0.08–1.21) |
| Other | 2.56 | (0.92–7.11) | 0.82 | (0.15–4.37) |
| Insurance | ||||
| Private | Ref | Ref | Ref | Ref |
| Public | 0.92 | (0.54–1.54) | 3.49 | (1.01–11.9) |
| Other | 0.77 | (0.34–1.72) | 1.95 | (0.34–11.0) |
| Age | ||||
| 6–12years | Ref | Ref | Ref | Ref |
| 13–17years | 0.81 | (0.50–1.31) | 0.92 | (0.32–2.56) |
| Sex (Female) | ||||
| Female | 1.02 | (0.65–1.58) | 0.74 | (0.29–1.85) |
| Weekday (Weekend) | ||||
| Yes | 1.47 | (0.86–2.49) | 0.93 | (0.26–3.29) |
| Arrival Time | ||||
| 7A-3P | Ref | Ref | Ref | Ref |
| 3P-11P | 0.78 | (0.42–1.42) | 3.35 | (1.01–11.0) |
| 11P-7A | 0.96 | (0.44–2.05) | 0.33 | (0.08–1.30) |
| Region | ||||
| Midwest | Ref | Ref | Ref | Ref |
| Northeast | 1.17 | (0.52–2.60) | 1.67 | (0.34–8.17) |
| South | 1.01 | (0.52–1.95) | 4.07 | (0.98–16.7) |
| West | 1.01 | (0.51–1.99) | 1.01 | (0.29–3.41) |
| Disposition | ||||
| Admit/Transfer | Ref | Ref | Ref | Ref |
| Discharge | 0.48 | (0.30–0.75) | 0.12 | (0.04–0.35) |
| Other | 0.69 | (0.17–2.65) | 1.30 | (0.25–6.71) |
aOR, Adjusted Odds Ratio
Among mental and behavioral health visits in which a psychotropic medication was administered, visits with public insurance had a 3.5 times increased odds of polypharmacy (>1 psychotropic medication administered) compared to visits with private insurance (OR 3.50; 95%CI 1.01–11.90). For visits resulting in discharge, there was an 88% decreased odds of psychotropic medication administration in the ED compared to visits resulting in admission (OR 0.12, 95%CI 0.04–0.35). There was no difference in polypharmacy use by race and ethnicity, age, or sex (Table 3).
Secondary Analysis
Between 2006–2008 and 2016–2019 the average number of yearly mental and behavioral health ED visits almost doubled from 620,000 visits/year (12.4 visits/1000 population) to 1,115,000 visits/year (22.5 visits/1000 population); the proportion of total youth ED visits increased from 4.5% to 6.8% (Supplemental Figure A), (OR 1.49; 95%CI 1.20–1.86).
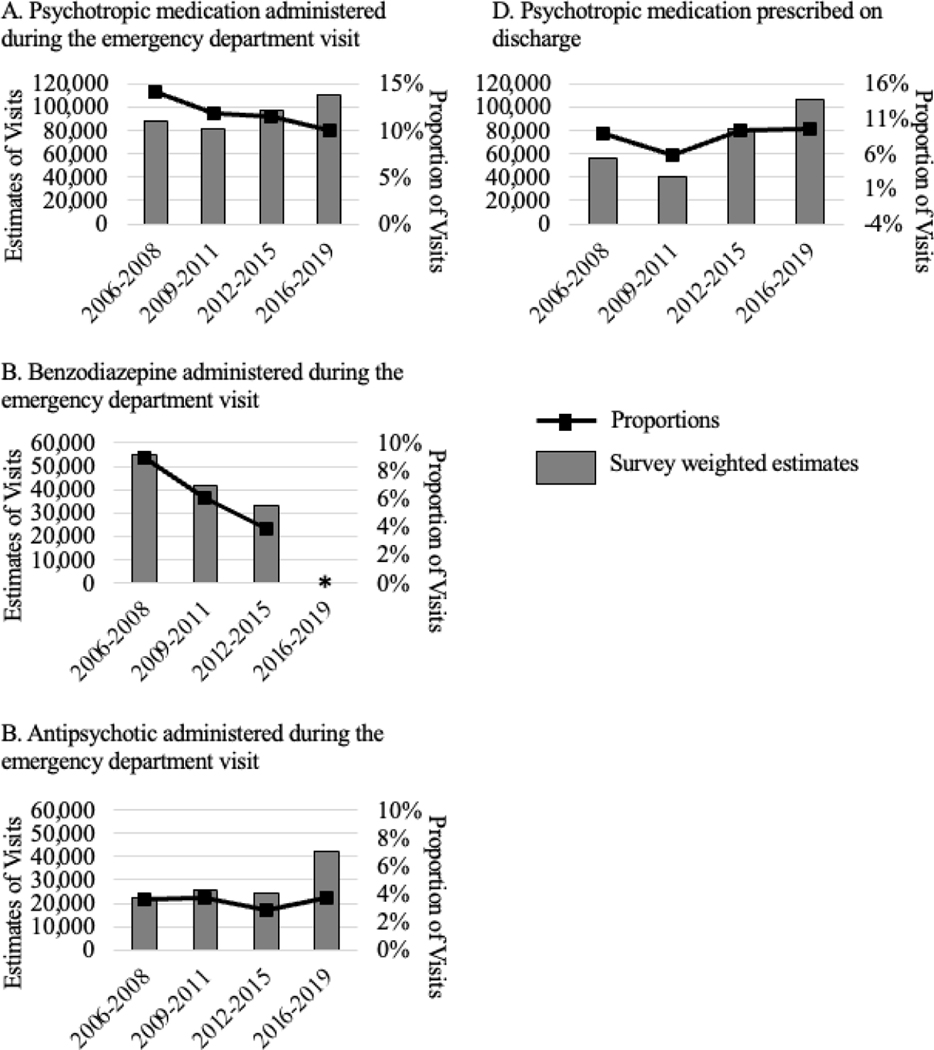
The proportion of youth mental and behavioral health ED visits in which a psychotropic medication was administered was 14.2% in 2006–2008 and 9.9% in 2016–2019. The proportion in which a psychotropic medication was given as a prescription upon discharge was 9.0% in 2006–2008 and 9.6% in 2016–2019 (Figure 2, Supplemental Table B). The proportion of visits in which an antipsychotic was administered in the ED was 3.6% in 2006–2008 and 3.8% in 2016–2019. The proportion of visits in which a benzodiazepine was given was 8.9% in 2006–2008 and 3.8% of visits in 2012–2015 (2016–2019 unreportable) (Figure 2, Supplemental Table B). These trends were also not statistically significant (Supplemental Table C).
Figure 2: Trends over time in the proportion of mental and behavioral health emergency department visits for youth with any psychotropic medication administered during the visit, 2006–2019.
Figure A, B, and C depict trends over time in the average annual estimates (survey weighted) and proportion of visits in which a psychotropic medication was administered: specifically, any psychotropic medication (A), benzodiazepines (B), and antipsychotics (C). Figure D depicts trends in the number and proportion of visits in which any psychotropic medication was prescribed upon discharge. There were no statistically significant differences between time periods.
*Unable to report stable survey weighted estimates for benzodiazepine use in 2016–2019.
Stratified by sociodemographic subgroup, there were no statistically significant differences in psychotropic medication use between 2006–2011 and 2012–2019 (Supplemental Table D).
Discussion
Over the 14-year study period, any psychotropic medication was administered during 11.4% of mental and behavioral health ED visits for US youth, and more than one psychotropic medication was administered during 3.6% of visits. Benzodiazepines were the most common medication type and visits with anxiety disorders had the highest proportion of psychotropic medication use. Use of psychotropic medications differed by sociodemographic characteristics. Black non-Hispanic youth were less likely to receive a psychotropic medication in the ED compared to White Non-Hispanic youth, and polypharmacy was more frequent in visits paid by public insurance. Although proportionate use did not change statistically over time, as the number of mental and behavioral health ED visits continues to increase, so will the absolute number of US youth who receive psychotropic medications in the ED setting and the urgency to understand clinical management of this population.
Even before the COVID-19 pandemic, ED use for youth mental and behavioral health crises was increasing.1,2,26 In light of the pandemic’s impact on mental health,3 in October 2021 the American Academy of Pediatrics, American Academy of Child and Adolescent Psychiatry, and Children’s Hospital Association declared a National State of Emergency in Children’s Mental Health,27 followed by the US Surgeon General three months later.28 While improved access to preventative services is paramount, in the meantime we must address care for the large number of youth presenting to acute settings.
Our study expands on limited research examining pharmacologic management of youth seeking mental and behavioral healthcare in the ED. Prior work has been restricted to children’s hospitals or single centers, or focused on specific medication types or indications (e.g restraint).29,30 Therefore, it is challenging to directly compare our study to prior research. We examined psychotropic medication use for any indication, in a nationally representative sample, which includes general and community EDs, where the majority of children receive care.2,17 In contrast, children’s hospitals’ EDs see a higher volume and acuity of pediatric patients, but are also more likely to have resources to support behavioral symptom management, potentially decreasing the need for psychotropic medications. These resources include care pathways, 24-hour access to psychiatric consultation, and onsite personnel trained in de-escalation.31
Understanding the distribution of medication types is an important first step towards characterizing appropriate use, quality of care, and gaps in guidelines and supports for ED clinicians. Consistent with prior research, benzodiazepines were the most frequently used medication type.16,29 While not statistically significant, our data suggest that benzodiazepine use may be decreasing over time. In the outpatient setting, benzodiazepine prescriptions for commercially insured pediatric beneficiaries increased in the 2000s but decreased more recently (2015–2019),32 potentially reflective of concerns for misuse and abuse. Although we cannot infer etiology, changes in ED benzodiazepine use may reflect increased application of non-pharmacologic interventions, or substituting other medications (e.g. antihistamines) for sedation and anxiolysis.
Although an acute care setting, our study suggests that ED management of youth with mental and behavioral health needs includes psychotropic medications typically indicated for chronic conditions, such as antidepressants and stimulants. In our sample, these medications were more frequently administered during longer visits and were prescribed in higher proportions upon discharge. All to suggest that these medications may represent a continuation of a patient’s home medication regimen. While practice guidelines reference using home medications to prevent or manage agitation, there is little reference to administering home psychotropic medications for other presentations.13 As length of stay for youth mental and behavioral health visits increases,21 so will the need to provide in the ED or upon discharge, patients’ chronic psychotropic medications.
Consistent with overall patterns of racial disparities in mental healthcare utilization, we found that psychotropic medication administration was less frequent in visits for Black non-Hispanic compared to White non-Hispanic youth. In the office-based setting, even with an indication for use and access to care, Black youth are less likely to receive psychotropic medications. The etiology of these disparities are multifactorial and include (but are not limited to) inadequate access (due to insurance barriers or challenges accessing minimally adequate treatment), stigma, differences in perceptions of mental and behavioral healthcare, and provider bias.12,26,33–35 From our study data, we cannot assess appropriateness of medication use, and therefore cannot infer whether these findings represent disparities or inequities.14 Nonetheless, when faced with racial differences in the care delivery, we must interpret our findings in the context of the pervasive impact of structural racism on health and healthcare. For example, decreased psychotropic medication use may reflect differences in clinical management by EDs serving a higher number of Black youths, or lower acuity visits by Black patients due to poor access in the outpatient setting. Decreased use may also represent racial bias in diagnosis,24,25 (psychotropic medications administration seemed to differ by diagnosis). Future work should define appropriate use and aim to better characterize and understand these differences.
Among visits administering any psychotropic medication, visits for publicly insured patients were more likely to use polypharmacy, consistent with patterns in office-based settings.10 Consensus guidelines recommend avoiding psychotropic polypharmacy when possible in managing agitation.6,7 Although we cannot assess the clinical severity of presentation, differences in polypharmacy likely represent inequities, potentially due to inequities in access to outpatient care and the disproportionate impact of adverse childhood experiences and toxic stress on publicly insured patients,19,36 both of which may influence disease severity on presentation.
NHAMCS is a large, nationally representative dataset, with inherent limitations. First, the number of visits in which a psychotropic medication was administered was relatively small, limiting our ability to produce stable estimates for some sub-analyses. Second, we could not distinguish between medications administered to address acute symptoms and as a continuation of home regimens – which may bias results. Third, almost 10% of visits listed diagnoses categorized as “other mental and behavioral health diagnoses”- a category with minimal clinical interpretability. We hypothesize that these non-specific diagnoses are used for patients who present with symptoms, but without established psychiatric diagnoses, or by ED providers uncertain of labeling presenting symptoms with specific diagnoses. Fourth, NHAMCS does not provide information beyond geographic region on hospital type (such as children’s vs. general hospital). Lastly, NHAMCS data are at the visit (not patient) level - we cannot assess the impact of repeat visits.
Conclusion
A psychotropic medication was administered in approximately one of every ten US ED visits for youth receiving care in the ED for mental and behavioral health needs over the 14-year study period, amounting to an annual average of approximately 110,000 visits in the most recent years (2016–2019). Use of psychotropic medications differed by race and ethnicity and insurance type, potentially reflective of discretionary care within the ED as well as inequities in access to preventative care. Although proportionate use of psychotropic medications did not change significantly over time, as more youths seek mental and behavioral healthcare in the ED, so will the number that receives psychotropic medications in this setting. Especially in the context of COVID-19’s impact on mental health, we must prioritize understanding appropriate use of psychotropic medications in the ED and ensure that EDs nationally have the necessary resources and support to provide high quality, equitable care.
Supplementary Material
What’s New:
11% of ED visits for youth with mental and behavioral health needs received psychotropic medications. Use differed by sociodemographic groups but did not change over time. As mental and behavioral visits increase so will psychotropic medication use in the ED.
Funding/Support
This publication was made possible by National Clinician Scholars Program and the CTSA Grant Number TL1 TR001864 from the National Center for Advancing Translational Science (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NIH. This publication was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1TR001873. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Dr. Venkatesh reports support of the American Board of Emergency Medicine – National Academy of Medicine Anniversary Fellowship and prior support of Award KL2 TR001862 from the National Center for Advancing Translational Science (NCATS), a component of the National Institutes of Health
Funders/Sponsors did not participate in the work.
Abbreviations
- ASD
Autism Spectrum Disorder
- CI
Confidence Interval
- CAMHD- CS
Child and Adolescent Mental Health Disorder Classification System
- CDC
Center for Disease Control and Prevention
- DD
Developmental Delay
- ED
Emergency Department
- ICD
International Classification of Disease
- NHAMCS
National Hospital Ambulatory Medical Care Survey
- NCHS
National Center for Health Statistics
- aOR
Adjusted Odds Ratio
- OR
Odds Ratio
- SUD
Substance Use Disorder
- US
United States
Footnotes
Contributors Statement Page:
Dr. Nash conceptualized and designed the study, conducted data analysis, drafted the initial manuscript, and revised the manuscript.
Mr. Rothenberg provided critical support for data analysis and methodology and reviewed and revised the manuscript.
Drs. Olfson, Anderson, and Pincus, contributed to the conceptualization and design of the study, critically reviewed, and revised the manuscript.
Dr. Venkatesh conceptualized and designed the study, critically reviewed the manuscript for important intellectual content, reviewed and revised the manuscript.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Declaration of Competing Interest
none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kalb LG, Stapp EK, Ballard ED, Holingue C, Keefer A, Riley A. Trends in Psychiatric Emergency Department Visits Among Youth and Young Adults in the US. Pediatrics. 2019:e20182192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lo CB, Bridge JA, Shi J, Ludwig L, Stanley RM. Children’s Mental Health Emergency Department Visits: 2007–2016. Pediatrics. 2020;145(6):e20191536. [DOI] [PubMed] [Google Scholar]
- 3.Samji H, Wu J, Ladak A, et al. Review: Mental health impacts of the COVID-19 pandemic on children and youth - a systematic review. Child Adolesc Ment Health. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leeb RT BR, Radhakrishnan L, Martinez P, Njai R, Holland KM. Mental Health–Related Emergency Department Visits Among Children Aged <18 Years During the COVID-19 Pandemic — United States, January 1–October 17, 2020. MMWR Morb Mortal Wkly Rep 2020.69:1675–1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shankar LG, Habich M, Rosenman M, Arzu J, Lales G, Hoffmann JA. Mental Health Emergency Department Visits by Children Before and During the COVID-19 Pandemic. Academic Pediatrics. 2022;22(7):1127–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoffmann JA, Pergjika A, Konicek CE, Reynolds SL. Pharmacologic Management of Acute Agitation in Youth in the Emergency Department. Pediatr Emerg Care. 2021;37(8):417–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gerson R, Malas N, Feuer V, et al. Best Practices for Evaluation and Treatment of Agitated Children and Adolescents (BETA) in the Emergency Department: Consensus Statement of the American Association for Emergency Psychiatry. Western Journal of Emergency Medicine. 2019;20(2):409–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kendrick JG, Goldman RD, Carr RR. Pharmacologic Management of Agitation and Aggression in a Pediatric Emergency Department - A Retrospective Cohort Study. J Pediatr Pharmacol Ther. 2018;23(6):455–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vitiello B, Davico C. Twenty years of progress in paediatric psychopharmacology: accomplishments and unmet needs. Evid Based Ment Health. 2018;21(4):e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chirdkiatgumchai V, Xiao H, Fredstrom BK, et al. National Trends in Psychotropic Medication Use in Young Children: 1994–2009. Pediatrics. 2013;132(4):615–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Comer JS, Olfson M, Mojtabai R. National Trends in Child and Adolescent Psychotropic Polypharmacy in Office-Based Practice, 1996–2007. J Am Acad Child Adolesc Psychiatry. 2010;49(10):1001–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Olfson M, Blanco C, Liu L, Moreno C, Laje G. National Trends in the Outpatient Treatment of Children and Adolescents With Antipsychotic Drugs. Archives of General Psychiatry. 2006;63(6):679. [DOI] [PubMed] [Google Scholar]
- 13.Gerson R, Malas N, Feuer V, Silver GH, Prasad R, Mroczkowski MM. Best Practices for Evaluation and Treatment of Agitated Children and Adolescents (BETA) in the Emergency Department: Consensus Statement of the American Association for Emergency Psychiatry. West J Emerg Med. 2019;20(2):409–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Institute of Medicine Committee on U, Eliminating R, Ethnic Disparities in Health C. In: Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington (DC): National Academies Press (US) Copyright 2002 by the National Academy of Sciences. All rights reserved.; 2003. [PubMed] [Google Scholar]
- 15.Healthcare Disparities and Cultural Competency Consensus Standards: Disparities-Sensitive Measure Assessment Technical Report. National Quality Forum; November 2012. 2012. [Google Scholar]
- 16.Foster AA, Porter JJ, Monuteaux MC, Hoffmann JA, Hudgins JD. Pharmacologic Restraint Use During Mental Health Visits in Pediatric Emergency Departments. J Pediatr. 2021;236:276–283.e272. [DOI] [PubMed] [Google Scholar]
- 17.Whitfill T, Auerbach M, Scherzer DJ, Shi J, Xiang H, Stanley RM. Emergency Care for Children in the United States: Epidemiology and Trends Over Time. J Emerg Med. 2018;55(3):423–434. [DOI] [PubMed] [Google Scholar]
- 18.Remick K, Gausche-Hill M, Joseph MM, Brown K, Snow SK, Wright JL. Pediatric Readiness in the Emergency Department. Pediatrics. 2018;142(5):e20182459. [DOI] [PubMed] [Google Scholar]
- 19.Marrast L, Himmelstein DU, Woolhandler S. Racial and Ethnic Disparities in Mental Healthcare for Children and Young Adults: A National Study. International Journal of Health Services. 2016;46(4):810–824. [DOI] [PubMed] [Google Scholar]
- 20.About the Ambulatory Healthcare Surveys. The Center for Disease Control and Prevention. https://www.cdc.gov/nchs/ahcd/about_ahcd.htm. Updated December 30th, 2021. Accessed June 30, 2022, 2022. [Google Scholar]
- 21.Nash KA, Zima BT, Rothenberg C, et al. Prolonged Emergency Department Length of Stay for US Pediatric Mental Health Visits (2005–2015). Pediatrics. 2021;147(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holder SM, Rogers K, Peterson E, Shoenleben R, Blackhurst D. The Impact of Mental Health Services in a Pediatric Emergency Department: The Implications of Having Trained Psychiatric Professionals. Pediatric Emergency Care. 2017;33(5):311–314. [DOI] [PubMed] [Google Scholar]
- 23.Zima BT, Rodean J. Mental Health Disorder Codes, Child and Adolescent Mental Health Disorders Classification System (CAMHD-CS). https://www.childrenshospitals.org/Research-and-Data/Pediatric-Data-and-Trends/2019/Mental-Health-Disorder-Codes. Published 2019. Updated 9/10/19. Accessed 1/20/20. [Google Scholar]
- 24.Coker TR, Elliott MN, Toomey SL, et al. Racial and Ethnic Disparities in ADHD Diagnosis and Treatment. Pediatrics. 2016;138(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fadus MC, Ginsburg KR, Sobowale K, et al. Unconscious Bias and the Diagnosis of Disruptive Behavior Disorders and ADHD in African American and Hispanic Youth. Acad Psychiatry. 2020;44(1):95–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prevention CfDCa. Youth Risk Behavior Survey (YRBS) Data Summary and Trends 2009–2019. Center for Disease Control and Prevention;2019. [Google Scholar]
- 27.AAP-AACAP-CHA Delcaration of a National Emergency in Child and Adolescent Mental Health [press release]. aap.org: American Academy of Pediatrics 10/19/21 2021. [Google Scholar]
- 28.U.S. Surgeon General Issues Advisory on Youth Mental Health Crisis Further Exposed by COVID-19 Pandemic [press release]. HHS.gov: U.S. Department of Health and Human Services; 12/7/21 2021. [Google Scholar]
- 29.Kendrick JG, Goldman RD, Carr RR. Pharmacologic Management of Agitation and Aggression in a Pediatric Emergency Department – A Retrospective Cohort Study. The Journal of Pediatric Pharmacology and Therapeutics. 2018;23(6):455–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Foster AA, Porter JJ, Monuteaux MC, Hoffmann JA, Hudgins JD. Pharmacologic Restraint Use During Mental Health Visits in Pediatric Emergency Departments. J Pediatr. 2021. [DOI] [PubMed] [Google Scholar]
- 31.Gausche-Hill M, Ely M, Schmuhl P, et al. A National Assessment of Pediatric Readiness of Emergency Departments. JAMA Pediatrics. 2015;169(6):527–534. [DOI] [PubMed] [Google Scholar]
- 32.Toce MS, Michelson KA, Hudgins JD, Olson KL, Bourgeois FT. Trends in Benzodiazepine Prescribing for US Adolescents and Young Adults From 2008 to 2019. JAMA Pediatrics. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang S, Cain DS, Liao M. Racial/ethnic disparities in the decision points of mental health service use and psychotropic medication receipt among depressed youth. Youth & Society. 2021;53(4):610–635. [Google Scholar]
- 34.Rodgers CRR, Flores MW, Bassey O, Augenblick JM, Cook BL. Racial/Ethnic Disparity Trends in Children’s Mental Healthcare Access and Expenditures From 2010 to 2017: Disparities Remain Despite Sweeping Policy Reform. J Am Acad Child Adolesc Psychiatry. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cummings JR, Ji X, Lally C, Druss BG. Racial and Ethnic Differences in Minimally Adequate Depression Care Among Medicaid-Enrolled Youth. J Am Acad Child Adolesc Psychiatry. 2019;58(1):128–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Trent M, Dooley DG, Dougé J. The Impact of Racism on Child and Adolescent Health. Pediatrics. 2019;144(2):e20191765. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.