Abstract
Purpose:
This study aimed to determine the functional and radiographic outcomes following corrective distal humeral osteotomies for the treatment of supracondylar fracture malunions in children. We hypothesized that such secondary reconstructive procedures could restore a reasonable and near-normal amount of functionality in a large patient cohort at a tertiary referral center.
Methods:
We retrospectively reviewed the clinical and radiological records of 38 children who underwent corrective osteotomy for posttraumatic supracondylar humeral malunion using K-wire fixation. All clinical data were extracted after chart review, including age, sex, dominant side whenever available, follow-up duration, and elbow range of motion preoperatively and at the final visit. Radiographic parameters, including Baumann’s angle, humeroulnar angle, humerocondylar angle, and elbow range of motion were evaluated preoperatively, postoperatively, and at the final visit to identify the surgical correction outcomes.
Results:
The mean age of the patients at fracture was 5.6 (±2.7) years, and the mean age at surgical intervention was 8.6 (±2.6) years. The mean follow-up period of the current series was 28.2 (±31.1) months. Baumann’s angle, humeroulnar angle, and humerocondylar angle were successfully restored to physiological ranges (72.6°, 5.4°, and 36.1°, respectively). Postoperatively, elbow extension improved from -22° (±5.7) to -2.7° (±7.2) versus flexion from 115° (±13.2) to 128.2° (±11.1). Three revision surgeries (8%) were encountered.
Conclusions:
Corrective osteotomy of the distal humerus with K-wire fixation is a reliable method to efficiently correct malunion of the distal humerus in different planes, thereby improving elbow range of motion and appearance.
Level of evidence:
level IV: Retrospective therapeutic study.
Keywords: Supracondylar fracture, malunion, cubitus varus, cubitus valgus, flexion osteotomy
Introduction
Fractures around the elbow are common in the pediatric age group. 1 However, elbow fracture cases may be missed and/or present late due to the presence of cartilaginous ossification centers.2,3 Supracondylar humeral (SCH) fractures are the most frequent fractures around the elbow, accounting for 5% of all pediatric fractures and 50%–70% of elbow fractures with a peak incidence between 4 and 7 years.4,5 Moreover, child abuse should be suspected in cases of fractures in nonambulatory children and with certain fractures patterns such as transphyseal distal humerus fracture. 6 Recommendations regarding the treatment of SCH fracture have been made. Nevertheless, the results and level of evidence have been inconsistent to date. 7
Complications of SCH fractures are fairly prevalent and include neurovascular injuries, compartment syndrome, restricted range of motion, and posttraumatic deformities. 8 Numerous anatomic components of SCH malunions have been documented, including elbow varus deformity, elbow hyperextension, and internal malrotation.
Elbow varus deformity, also called cubitus varus, is the most common problem after pediatric supracondylar fracture, which includes lateral prominence of the elbow area. Cubitus varus is a blend of varus, hyperextension, and internal rotation in most patients. 8 The frequency of cubitus varus deformity secondary to SCH fractures ranges from 3% to 57%. 7 It not only results in an unfavorable aesthetic deformity of the elbow, but may also increase the incidence of lateral condyle fractures, internal rotational malalignment, elbow discomfort and dysfunction, and other secondary fractures. 8 In contrast, isolated extension deformity is associated with a high remodeling rate in younger children. 9 However, flexion osteotomy may nevertheless be needed in cases of limited flexion of the elbow joint and in patients 6–8 years and older.10,11
Correcting SCH malunion using various surgical approaches, osteotomies, and fixation methods has been explored, and the results show satisfactory function with relatively few complications. French, for example, was an orthopedic physician who invented the lateral closing-wedge osteotomy surgery to treat malunited supracondylar humerus in 1959. 6 He described a method that resulted in adequate exposure, facilitated osteotomy, permitted early elbow motion, and had a satisfactory functional outcome. Other techniques include step-cut osteotomies, dome-shaped osteotomies, and gradual correction with an external fixator.12–14
This retrospective study aimed to determine functional and radiographic outcomes following corrective osteotomies in one of the largest patient populations to date. We hypothesized that such secondary reconstructive procedures could restore reasonable and near-normal functionality.
Materials and methods
This retrospective study reviewed the clinical and radiological records of all pediatric patients who underwent corrective osteotomy for posttraumatic supracondylar cubitus varus or valgus deformity and extension or flexion deformity at the Pediatric Orthopedic Department of the Orthopedic Hospital Speising during the period 2007–2021. The study included all patients who were (1) younger than 18 years old, (2) underwent either a distal humerus closing-wedge corrective osteotomy to correct cubitus varus or valgus malunion, or (3) distal humeral flexion or extension osteotomy to correct an extension or flexion deformity, and (4) had standardized pre- and postoperative radiographs (elbow anteroposterior and lateral) obtained at our institution. All cases with insufficient documentation and improper radiographs were excluded. Contralateral radiographs were obtained whenever possible for anatomical comparisons between the two sides. The appropriate institutional review board waived ethical approval due to the retrospective (radiographic) nature of the research, which did not include active patient involvement (MA15-EK/22-186-VK_KANN).
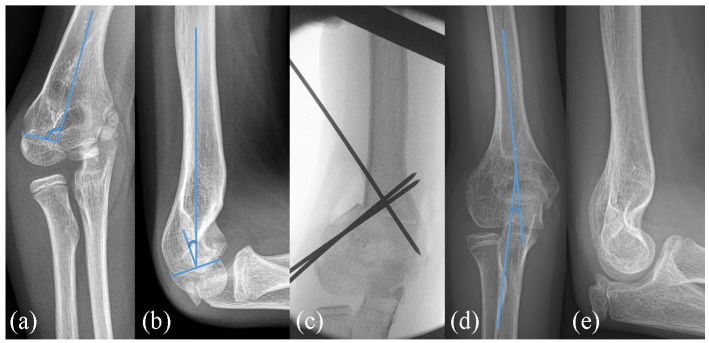
The following three radiographic measurements were taken preoperatively, postoperatively and at the final visit: Baumann’s angle (BA; Figure 1(a)), formed by the humeral axis and a straight line through the epiphyseal plate of the capitulum; humeroulnar angle (“carrying angle,” HUA; Figure 1(c)) in the anteroposterior plane, determined by the intersection of the humeral and ulnar shaft axes; and humerocondylar angle (HCA; Figure 1(d)) in the lateral plane, formed by a line drawn along the anterior humerus shaft and a second line perpendicular to the physeal line. Given that our hospital is not the main institution for trauma treatment, all patients were previously treated at various healthcare facilities around the nation. Furthermore, all clinical data were extracted after chart review, including age, sex, dominant side whenever available, follow-up duration, and elbow range of motion preoperatively and at the final visit as secondary outcome parameters.
Figure 1.
An illustrative case of a severe posttraumatic varus deformity is shown (a). In the sagittal plane, a pseudoextension deformity is present. The patient had full flexion without any impairment due to the specific fracture pattern (b). Following a 30° K-wire correction (c), and the final images (d, e) revealed a physiologic position with a well-remodeled distal humerus shape.
Surgical technique
Surgery was performed under general anesthesia with the patient in the supine position and the arm resting on the arm table. A sterile upper arm tourniquet was applied. All deformities except valgus deformity underwent osteotomy through the described lateral approach, while valgus osteotomies were performed using a medial approach (the ulnar nerve was decompressed and held aside to allow osteotomy).
A 5-cm S-shaped incision was created proximal to the lateral humeral epicondyle, and the subcutaneous tissue was dissected to expose the lateral crista humeri. The ulnar nerve is regularly decompressed proximal to the cubital tunnel to protect it during osteotomy. This was performed through a separate medial approach.
To mark the osteotomy, a 1.2 mm smooth pin was inserted 1–2 cm above the olecranon fossa perpendicular to the humeral longitudinal axis under fluoroscopy supervision, a second pin was inserted proximally in the same way, and the appropriate amount of correction was determined.
Generally, a lateral closing-wedge osteotomy is preferred between the two guidewires to achieve the necessary correction, as indicated radiographically (Figures 1 and 2). Malalignment is then corrected by closing the osteotomy sides and, whenever necessary, by completing a three-dimensional osteotomy. Prior to excision of the bone wedge, two 1.8 or 2.0 smooth pins are introduced through the lateral epicondyle, with a third pin placed under direct supervision from the lateral cortex (“Dorgan`s pin”) 15 proximal to the osteotomy site and directed medially and caudally. Wires are advanced just proximal to the osteotomy site, and the osteotomy is completed by the oscillating saw under continuous irrigation.
Figure 2.
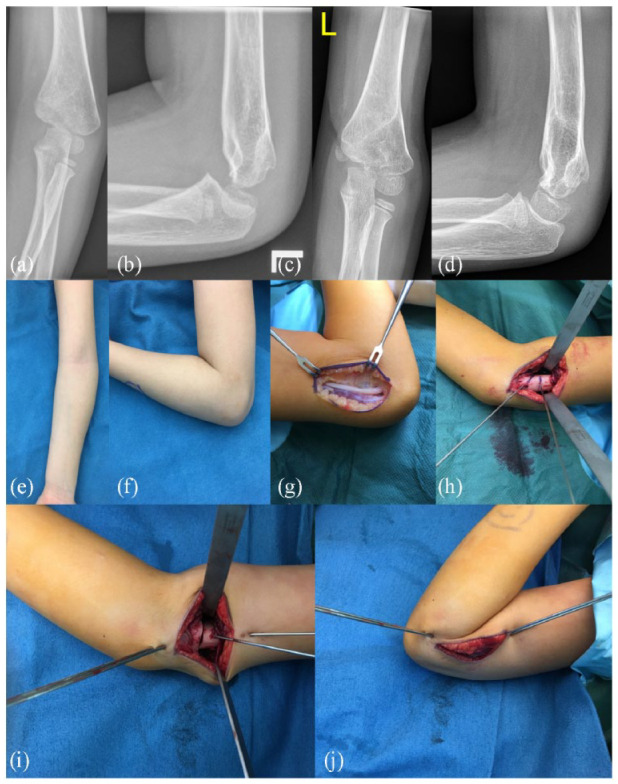
An illustrative case of a three-dimensional corrective osteotomy is shown. Both a varus and distal humeral extension deformity are present (a and b), which have been corrected through a ventral-lateral closing-wedge osteotomy (c and d). The clinical picture with varus and lack of flexion is shown (e and f). Following prophylactic ulnar nerve release (g), the wedge was marked with pencil and wires (h), the osteotomy completed and secured (i). Note the improved full elbow flexion (j).
The medial cortex hinge and periosteum were maintained intact whenever possible. The wedge fragment was then excised, the osteotomy side was closed with correction in two or three planes, and the pins were advanced through the contralateral cortex. Additional pins may be added from either the lateral or medial cortex to increase stability. A tourniquet was deflated, hemostasis was ensured, the wound was closed in layers, and pin ends were cut and bent. A dressing and a long-arm cast were applied for 4–8 weeks. Thereafter, healing was confirmed by elbow radiography, pins were removed in the office, and a removable long-arm brace was applied. Gentle physical therapy was initiated after the cast was removed.
Statistical analysis
The pre- and postoperative elbow range of motion and outcome parameters (BA, HUA, and HCA) were tabulated. Descriptive analysis using means, standard deviation (SD), and ranges was performed using MS Excel (2016). Statistical tests (paired t-tests) were performed to compare the outcome parameters of the subgroups with a sufficient sample size (varus, extension, and varus + extension deformity). A p-value of <0.05 was considered statistically significant.
Results
A total of 38 patients (22 boys and 16 girls) were included in the study (Table 1). The mean age of patients at fracture was 5.6 (±2.7) years and the mean age at surgical intervention was 8.6 (±2.6) years, with an average of 3-year intervals from fracture to correction (3.0 ± 2.5). The mean follow-up period was 28.2 (±31.1) months (range: 1–96 months). The left side was affected in two-thirds of patients.
Table 1.
Sociodemographic characteristics and deformity frequency.
| N (%) | |
|---|---|
| Gender | |
| Male | 22 (58) |
| Female | 16 (42) |
| Extremity | |
| Right | 12 (32) |
| Left | 26 (68) |
| Deformity | |
| Coronal plane deformity | |
| Cubitus varus | 10 (26) |
| Cubitus valgus | 3 (8) |
| Sagittal plane deformity | |
| Extension | 15 (39) |
| Flexion | 1 (3) |
| Multiplane deformity | |
| Cubitus varus and extension | 9 (24) |
| Complication | |
| Infection | 2 (5.3) |
| Nerve lesions | 2 (5.3) |
| Loss of correction | 3 (7.9) |
The deformities in the coronal plane comprised 10 cubitus varus and three cubitus valgus. In the sagittal plane, there were 15 extension deformities and one flexion deformity (Figure 3). Combined varus and extension deformities were observed in nine elbows. However, isolated extension deformities were observed in 15 of the elbows.
Figure 3.
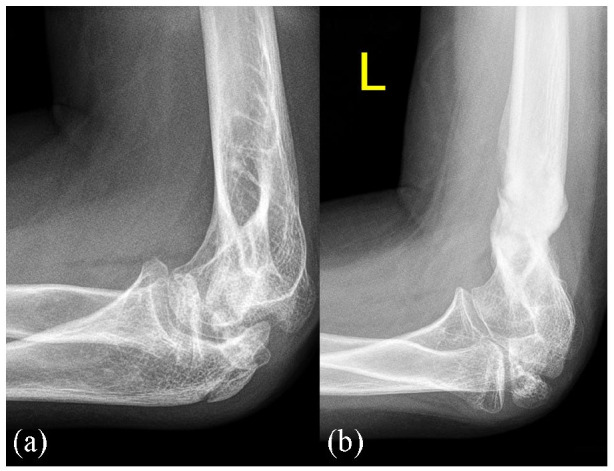
A case with a flexion deformity (clinically marked lack of extension) after meningococcal sepsis before (a) and after (b) extension osteotomy is shown.
The ROM improved from 0-45-150 before surgery to 0-25-120 after surgery.
To avoid any traction injury during manipulation, prophylactic neurolysis was performed in 32 of 38 procedures (13 in extension correction, 10 in varus correction (Figure 1), 3 in valgus, 1 in flexion, and 5 neurolyses in combined extension and varus deformities). However, therapeutic median nerve neurolysis was performed in two patients with extension deformities. Six patients who underwent surgery at the beginning of this series did not undergo prophylactic neurolysis during corrective surgery.
Table 2 shows elbow parameters preoperatively, immediately postoperatively, and at the final follow-up for all elbows and each deformity individually. The preoperative elbow parameters for the entire cohort were as follows: BA 76.2°(±12.2, 47.4 to 95), HUA 1.2°(±16.6, -27.5 to 41.9), and HCA 22.3°(±18.2, -8.3 to 63). The measured parameters at the follow-up postoperatively were as follows: BA 74.3°(±9.6, 58 to 91.7), HUA 7.1°(±9.7, -19 to 27.1), and HCA 35.3°(±11.1, 11.3 to 54.5). At the final follow-up, the parameters were as follows: BA 72.6° (±7.9, 58.1 to 85), HUA 5.4°(±9.9, -22.1 to 22), and HCA 36.1°(±11.6, 12.4 to 61.1). Elbow extension improved from -22°(±5.7, -30 to -15) to -2.7°(±7.2, -20 to 15) and the flexion from 115°(±13.2, 100 to 140) to 128.2°(±11.1, 90 to 145). As expected, in cubitus varus and valgus deformities, deformity improvement was mainly reflected in the BA and HUA with smaller changes in the HCA. In contrast, extension and flexion deformities are reflected mainly in the HCA, with limited changes in the BA and HUA. Table 3 summarizes the individual case data for the 38 patients.
Table 2.
Parameters for all patients with supracondylar mal-united fracture and individual deformity patterns.
| Total | Cubitus varus | Cubitus valgus | Extension | Flexion | Cubitus varus + extension | |
|---|---|---|---|---|---|---|
| Total | 38 | 10 | 3 | 15 | 1 | 9 |
| Mean age at fracture | 5.6 (2.7) | 5.9 (3.4) | 6.6 (2.5) | 5.6 (2.6) | 4 | 5.5 (2.4) |
| Mean age at surgery | 8.6 (2.6) | 10.4 (3.2) | 9.3 (4.04) | 7.8 (1.6) | 4 | 8.2 (1.8) |
| Follow-up (month) | 28.2 (31.1) | 44.3 (32.4) | 3.6 (2.08) | 13.2 (17.3) | na | 43 (38.8) |
| Baumann angle | ||||||
| Pre. Op | 76.2 (12.2) | 76.9 (14.6) | 57.5 (7.6) | 72.9 (8.9) | 77.1 | 87.1 (5.2) |
| Post. Op | 74.3 (9.6) | 75.2 (9.7) | 66.3 (1.5) | 74.4 (8.5) | 75.3 (12.4) | |
| Last follow up | 72.6 ( 7.9) | 65.9 (5.9) | 75.4 | 75.3 (6.2) | na | 71.8 (11) |
| p-value | 0.013 | 0.059 | 0.042 | |||
| Humeroulnar angle | ||||||
| Pre. Op | 1.2 (16.6) | −14.1 (8.1) | 35.8 (10.5) | 11 (7.8) | 1.9 | −9.6 (4.6) |
| Post. Op | 7.1 (9.7) | 8.1 (3.8) | 5.9 (4.3) | 9.6 (11.5) | 21.2 | 1.1 (9.6) |
| Last follow up | 5.4 (9.9) | 3.8 (8.6) | 10.5 (3) | 9.1 (8.4) | na | −0.3 (12.5) |
| p-value | 0.004 | 0.140 | 0.044 | |||
| Humerocondylar angle | ||||||
| Pre. Op | 22.3 (18.2) | 33.6 (16.6) | 43.6 (8.6) | 10.5 (12.3) | 63 | 17.7 (10.9) |
| Post. Op | 35.3 (11.1) | 37.7 (13) | 36.3 (4.1) | 33.2 (11.5) | 35 | 35.9 (11.3) |
| Last follow up | 36.1 (11.6) | 40.7 (10.1) | 39.2 (13.1) | 30.9 (9.9) | na | 38.6 (13.5) |
| p-value | 0.001 | <0.001 | 0.010 | |||
| Extension ROM | ||||||
| Pre. Op | −3.9 (16.4) | 1.7 (6.1) | −7.5 (10.6) | −5.7 (22.2) | na | −6.4 (12.5) |
| Post. Correction | 1.9 (6.9) | 5 (9.1) | 6.7 (5.8) | 0.3 (7.4) | na | 0 |
| Flexion ROM | ||||||
| Pre. Op | 111.5 (17.2) | 125.6 (15.1) | 135 (7.1) | 101.3 (13.6) | na | 108.6 (9.4) |
| Post. Correction | 128.2 (10.7) | 131.4 (8.5) | 130 (10) | 129.2 (7.9) | na | 123.1 (15.6) |
Na: not available (missing data); Post. Op, postoperative measurement; Pre. Op, preoperative measurement; ROM. range-of-motion.
Statistically significant values are shown in bold.
Table 3.
Preoperative and postoperative data of the study patients.
| Case | Sex | Side | Deformity | Age at Fracture | Age at OR | FU | Pre BA |
Post BA |
Last BA |
Pre HUA | Post HUA | Last HUA | Pre HCA | Post HCA | Last HCA |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | L | Ext, Var | 3 | 6 | 2 | 77.6 | 58 | na | −8.7 | 7.5 | na | 32.3 | 53.9 | 41.5 |
| 2 | M | R | Ext, Var | 9 | 10 | 85 | 91.3 | 70 | na | −11.3 | 7.8 | −7 | 8.4 | 36.2 | 41 |
| 3 | F | L | Ext | 4 | 7 | 13 | 69.2 | 79 | 70.8 | 19.5 | 19 | 16.8 | 5.8 | 21.2 | 31.3 |
| 4 | F | L | Ext | 2 | 7 | 3 | 72.3 | 74.6 | 78 | −5.3 | 2.5 | 10.4 | 4.3 | 53.5 | 56.5 |
| 5 | F | R | Ext, Var | 5 | 8 | 97 | 93.3 | 83.1 | na | −13.7 | −10.1 | 12 | 26 | 32.9 | 42 |
| 6 | M | L | Ext | 5 | 6 | na | 72.5 | 66.2 | na | 11.8 | 14 | na | 15.7 | 35.5 | na |
| 7 | M | L | Var | 11 | 15 | 92 | 95 | 76.5 | na | −27.5 | 2.3 | −6 | 8.3 | 13.8 | 23.2 |
| 8 | M | L | Ext | 7 | 8 | 16 | 73.8 | 77.7 | na | 12.7 | 10.2 | 6.9 | 5.8 | 53.9 | 36.6 |
| 9 | F | L | Var | 8 | 12 | 16 | 70.2 | 62.8 | 58.8 | −12.6 | 11.7 | 0.5 | 42 | 37.2 | 27.9 |
| 10 | M | R | Ext, Var | 9 | 10 | 85 | 85 | 62.3 | na | −9.3 | 9.8 | −7.3 | 2.8 | 37.1 | 30.7 |
| 11 | F | L | Ext | 4 | 7 | 13 | 70.9 | 71.3 | 77.4 | 18.9 | 19.3 | 15.5 | −8.3 | 24.5 | 31.9 |
| 12 | M | L | Var | 6 | 11 | 45 | 82.5 | 83.6 | 64.9 | −13.3 | na | 3.8 | 34.3 | 47.3 | 43.2 |
| 13 | M | R | Ext | 7 | 8 | 9 | 73.9 | 74.6 | na | 8.5 | 7.2 | na | 4.6 | 30.6 | 18.5 |
| 14 | M | L | Ext, Var | 5 | 11 | 23 | 85 | 83 | 85 | −19.4 | −19 | −22.1 | 7.8 | 36.8 | 39.6 |
| 15 | F | L | Var | 2 | 6 | 78 | 80.6 | 69.8 | na | −16.1 | 8.4 | 15 | 40.6 | 41.3 | 53 |
| 16 | F | R | Ext, Var | 5 | 7 | 46 | 84.1 | 71.5 | 58.1 | −5.7 | 2.7 | 1.6 | 12.2 | 15.4 | 61.1 |
| 17 | F | L | Valgus | 9 | 13 | 3 | 65.1 | 65.2 | na | 23.6 | 10.7 | 12 | 46.2 | 38.4 | 52.4 |
| 18 | F | L | Ext, Var | 5 | 9 | 2 | 86.6 | 91.6 | 65.8 | −6.9 | 3.2 | 18.8 | 14.9 | na | 30.1 |
| 19 | M | L | Ext | 10 | 11 | 1 | 73.6 | 74.4 | 75.2 | 11.1 | 4.5 | 5.7 | 2.9 | 11.3 | 29.5 |
| 20 | M | L | Ext, Var | 2 | 6 | 2 | 86.6 | 66.7 | 80.6 | −4.4 | 6.9 | 0.1 | 24.7 | 45.6 | 49.2 |
| 21 | M | L | Ext | 6 | 10 | 8 | 57.7 | 60.1 | 61 | 21.7 | 27.1 | 21.1 | 38.3 | 34.5 | 41.4 |
| 22 | F | L | Ext | 7 | 7 | 5 | 82.2 | 84.6 | 81.5 | 8.4 | 10.1 | 8.8 | 16.7 | 33.7 | 24.5 |
| 23 | M | L | Ext | 4 | 5 | 68 | 82 | 79.9 | 82.8 | 1.6 | 7.6 | −2.4 | 24.6 | 33.3 | 21.8 |
| 24 | M | L | Var | 3 | 6 | 63 | 89.5 | 91.1 | 73 | −15.9 | 5.7 | −12 | 39.6 | 51 | 40 |
| 25 | M | R | Var | 6 | 7 | 72 | 79.6 | 75 | 674 | −3.4 | 12.5 | na | 6.4 | 33.8 | 42 |
| 26 | M | L | Ext | 9 | 9 | 29 | 74.2 | 87.6 | 76.4 | 7.4 | −4 | 2.4 | 19.4 | 45.9 | 18.6 |
| 27 | F | L | Ext, Var | 7 | 7 | 48 | 94.2 | 91.7 | 69.5 | −7.3 | 0.8 | 1.3 | 30.6 | 29.4 | 12.4 |
| 28 | F | L | Valgus | 3 | 5 | 1 | 50 | 67.3 | 75.4 | 41.9 | 2.3 | 12.5 | 34 | 31.6 | 26.2 |
| 29 | F | L | Valgus | 7 | 10 | 6 | 57.4 | na | na | 41.8 | 4.7 | 7 | 50.6 | 38.9 | 39 |
| 30 | M | R | Flex | 3 | 4 | na | 77.1 | na | na | 1.9 | 21.2 | na | 63 | 35 | na |
| 31 | M | R | Ext | 0 | 10 | 19 | 68.2 | na | na | 8.3 | 14.3 | 6 | 22 | 35.6 | 35 |
| 32 | F | R | Ext | 5 | 6 | 3 | 58 | 60 | 78 | 24.9 | 24.1 | 22 | −6 | 31.9 | 30 |
| 33 | F | R | Var | 4 | 13 | 11 | na | na | na | −3 | 5.7 | 8.2 | 28.7 | 25.2 | 37.2 |
| 34 | F | R | Var | 3 | 9 | 14 | 70 | 67.5 | na | −13 | 11.9 | 9 | 62.6 | 54.5 | 51.4 |
| 35 | M | L | Ext | 8 | 9 | 2 | 71 | 68.7 | 72.2 | 7.6 | 6.6 | −3.9 | 3.6 | 22 | 25.7 |
| 36 | M | R | Var | 4 | 12 | 11 | 47.4 | na | na | −26 | 3.8 | 4 | 42 | 47 | 48 |
| 37 | M | L | Ext | 6 | 7 | 1 | 94 | 82.8 | na | 7.2 | −19 | na | 7.8 | 31.3 | 31.3 |
| 38 | M | L | Var | 12 | 14 | na | na | na | na | −10.4 | 10.5 | na | 31.8 | 26.3 | na |
BA, Baumann’s angle; Ext, extension; F, female; Flex, flexion; FU, follow-up period; HCA, humerocondylar angle; HUA, humeroulanar angle; L, left; M, male; na, not available (missed data); OR, odds ratio; R, right; Var, varus.
In our study, two cases were complicated by deep infection, another two by partial nerve laceration by K-wire injury (ulnar nerve and ulnar/median nerve, respectively), and three elbows showed loss of correction in the subsequent follow-up. Three cases (8%; one septic loss of correction, two nerve injuries) necessitated revision surgery with neurolysis (median/ulnar nerve) and repeat corrective osteotomy. All patients recovered well, and sensory and motor deficits resolved several weeks after the intervention. Other cases of infection were successfully managed using oral antibiotics.
Discussion
The results of this study showed that corrective osteotomies following distal humeral malunion can reliably restore anatomy and function, even in cases of complicated three-dimensional deformities, such as varus-extension deformities. Moreover, the correction can be achieved using K-wires without the need for plate fixation, with subsequent hardware removal. The current study is unique as it presents one of the largest cohorts to date on this topic, with a plethora of possible deformities and variations around the pediatric distal humerus.
Malunion after closed reduction and percutaneous fixation of SCH occurs in approximately 5% of cases. Or et al. 16 defined malalignment as 10° loss in any plane or loss of a correct anterior humeral line. Liu et al. 17 compared the outcome of SCH repair by pediatric fellows and attending specialists and found that both groups had a similar rate of loss of reduction. However, the combined loss of reduction and nonideal reduction was much lower for attending specialists. Nevertheless, there were no significant differences in complications between groups.
Loss of reduction in Gartland type III SCH fracture is more frequent with fractures treated with two lateral pins, but no failures were reported in three-pin-fixed fractures. 18 Malreduction is a three-dimensional deformity that manifests mainly by hyperextension in the sagittal plane and cubitus varus in the coronal plane. Remodeling in younger children can correct the deformity and improve flexion deficits. However, older children may experience a loss of elbow flexion which affects their activities of daily living. Simanovsky et al. 19 followed 30 patients with SCH fracture with a mean follow-up of 8.2 years and found that 77% had 5° difference in humerocondylar angle compared with the contralateral limb. However, 50% of them manifested clinically, but only 10% of patients felt minor subjective functional disability at the last follow-up.
Guven et al. 20 evaluated the long-term functional and cosmetic results according to the Flynn criteria and the sagittal and coronal plane remodeling of displaced SCH fractures treated with open reduction and internal fixation in 49 patients after a mean of 22.4 years of follow-up. The cosmetic and functional outcomes were satisfactory in 93.9% and 83.7% of the patients, respectively. The average flexion deficit was 5 ± 8°, while the average extension deficit was 4 ± 5°. At the final follow-up, the mean difference in the Baumann’s and humeral condylar angles between the injured and uninjured sides were -4 ± 7° and 0 ± 3°. 20
The current study reported the results of 38 children who underwent corrective osteotomies for malunited SCH fractures. The senior authors` current preferred indications are side differences of > 20° of deformity, lateral elbow pain (which is very rare), and sometimes cosmetic difficulties for frontal plane deformities, and flexion deficit ≥ 20° or extension deficit >25 to 30° for sagittal plane deformities. The preferred technique in this series was a lateral closing-wedge osteotomy technique with K-wire fixation to correct the deformity (medial closing-wedge technique for the valgus case). Some authors have described new techniques to improve the planning and surgery of such complex deformities through custom-made surgical templates.21–23 However, these computer-assisted procedures require radiation-intensive computed tomography images to create the templates and are expensive. 22 They may, however, be a reasonable alternative method to address three-dimensional deformities more precisely. The method described in this paper is workable and reliable. Other authors have recently described alternative methods for sagittal plane correction with external fixators. 23 In our institution, external devices are avoided whenever possible owing to their relative inconvenience, complication rates, and rather long duration of use.
Our results showed that correction of the humerus in the sagittal plane most significantly improved the overall range of motion of the elbow, particularly elbow flexion. Postoperatively, however, the entire range of motion increased owing to the normalized and improved sliding movement of the olecranon in the olecranon fossa after anterior reorientation of the condyle. Postoperative formal physiotherapy helped regain motion after cast fixation. Although the radiological parameters were corrected for all deformity patterns, cases with concomitant cubitus varus correction did not improve as much in elbow flexion as in cases with sagittal plane correction alone, which can be explained by the concomitant distal fragment malrotation in some cases and probably the more technically demanding intervention. Moreover, our frontal plane deformities (varus and/or valgus) showed markedly improved radiological parameters. These cases were normalized to carrying angles of approximately 8° (BA 66°).
Two patients developed transient nerve palsy regardless of ulnar nerve decompression; this corresponded to 5.3% of the study sample. However, this compares favorably with our previously published article on a smaller cohort with distal humeral flexion osteotomies alone, which included these nerve injuries; in that study, the rate was higher at 12% of patients. 24
The drawbacks of this study are its retrospective nature and the loss of postoperative outcome measures in some patients. However, this is one of the largest series to date on this topic, including frontal, sagittal, and complex 3D-corrections of humerus malunions in a consecutive and thoroughly collected dataset.
In conclusion, corrective osteotomy of the distal humerus is a reliable method to efficiently correct malunion of the distal humerus in different planes, thereby improving elbow range of motion and cosmetic appearance. Overall, the results of this study show relevant clinical and radiological improvements that are of vital importance for activities of daily living.
Footnotes
Author contributions: SF conceived the study, edited the manuscript and approved the final version; MT collected the data, performed statistical analysis and wrote the first draft; AA reviewed and edited the manuscript and approved the article; RG reviewed and approved the article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The appropriate institutional review board waived ethical approval due to the retrospective (radiographic) character of the research, which did not include active patient involvement (MA15-EK/22-186-VK_KANN).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by “Exzellenzfeld Orthopädie der Vinzenz Gruppe”.
ORCID iD: Mohammed M Tarabishi  https://orcid.org/0000-0003-2903-7723
https://orcid.org/0000-0003-2903-7723
References
- 1.Hussain S, Dar T, Beigh AQ, et al. Pattern and epidemiology of pediatric musculoskeletal injuries in Kashmir valley, a retrospective single-center study of 1467 patients. J Pediatr Orthop B 2015; 24(3): 230–237. [DOI] [PubMed] [Google Scholar]
- 2.Zapala MA, Livingston K, Phelps AS, et al. Digital tomosynthesis of the pediatric elbow. Pediatr Radiol 2019; 49(12): 1643–1651. [DOI] [PubMed] [Google Scholar]
- 3.Underschultz JG, Stagg A, MacGougan CK. Applying CRITOE in pediatric elbow trauma: is that a fracture or an ossification center? CJEM 2021; 23(3): 398–400. [DOI] [PubMed] [Google Scholar]
- 4.Lahoti O, Akilapa O. Not kidding! Sequelae of elbow trauma in children. J Clin Orthop Trauma 2021; 20: 101471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abzug JM, Kozin SH. Pediatric upper extremity trauma. Curr Orthopaed Pract 2008; 19(5): 485–490. [Google Scholar]
- 6.Pandya NK, Baldwin K, Wolfgruber H, et al. Child abuse and orthopaedic injury patterns: analysis at a level I pediatric trauma center. J Pediatr Orthop 2009; 29(6): 618–625. [DOI] [PubMed] [Google Scholar]
- 7.Solichin I, Sandjaya G, Prabowo I, et al. The lateral curved osteotomy for cubitus varus deformity in children: a case report and literature review. Ann Med Surg 2021; 65: 102315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hell AK, Gadomski C, Braunschweig L. Spontaneous humeral torsion deformity correction after displaced supracondylar fractures in children. BMC Musculoskel Disord 2021; 22(1): 1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gamble JG, Vorhies JS. Remodeling of sagittal plane malunion after pediatric supracondylar humerus fractures. J Pediatr Orthop 2020; 40(10): e903–e909. [DOI] [PubMed] [Google Scholar]
- 10.Oura K, Shigi A, Oka K, et al. Corrective osteotomy for hyperextended elbow with limited flexion due to supracondylar fracture malunion. J Shoulder Elbow Surg 2018; 27(8): 1357–1365. [DOI] [PubMed] [Google Scholar]
- 11.Farr S, Scheider P. The molding hands of time: remodeling of sagittal plane malunion after pediatric supracondylar humerus fractures. J Pediatr Orthop 2021; 41(8): e700. [DOI] [PubMed] [Google Scholar]
- 12.Moradi A, Vahedi E, Ebrahimzadeh MH. Surgical technique: spike translation: a new modification in step-cut osteotomy for cubitus varus deformity. Clin Orthop Relat Res 2013; 471(5): 1564–1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tien YC, Chih HW, Lin GT, et al. Dome corrective osteotomy for cubitus varus deformity. Clin Orthop Relat Res 2000(380): 158–166. [DOI] [PubMed] [Google Scholar]
- 14.Belthur MV, Iobst CA, Bor N, et al. Correction of cubitus varus after pediatric supracondylar elbow fracture: alternative method using the Taylor spatial frame. J Pediatr Orthop 2016; 36(6): 608–617. [DOI] [PubMed] [Google Scholar]
- 15.Queally JM, Paramanathan N, Walsh JC, et al. Dorgan’s lateral cross-wiring of supracondylar fractures of the humerus in children: a retrospective review. Injury 2010; 41(6): 568–571. [DOI] [PubMed] [Google Scholar]
- 16.Or O, Weil Y, Simanovsky N, et al. The outcome of early revision of malaligned pediatric supracondylar humerus fractures. Injury 2015; 46(8): 1585–1590. [DOI] [PubMed] [Google Scholar]
- 17.Liu RW, Roocroft J, Bastrom T, et al. Surgeon learning curve for pediatric supracondylar humerus fractures. J Pediatr Orthop 2011; 31(8): 818–824. [DOI] [PubMed] [Google Scholar]
- 18.Sankar WN, Hebela NM, Skaggs DL, et al. Loss of pin fixation in displaced supracondylar humeral fractures in children: causes and prevention. J Bone Joint Surg Am 2007; 89(4): 713–717. [DOI] [PubMed] [Google Scholar]
- 19.Simanovsky N, Lamdan R, Mosheiff R, et al. Underreduced supracondylar fracture of the humerus in children: clinical significance at skeletal maturity. J Pediatr Orthop 2007; 27(7): 733–738. [DOI] [PubMed] [Google Scholar]
- 20.Guven MF, Kaynak G, Inan M, et al. Results of displaced supracondylar humerus fractures treated with open reduction and internal fixation after a mean 22.4 years of follow-up. J Shoulder Elbow Surg 2015; 24(4): 640–646. [DOI] [PubMed] [Google Scholar]
- 21.Takeyasu Y, Oka K, Miyake J, et al. Preoperative, computer simulation-based, three-dimensional corrective osteotomy for cubitus varus deformity with use of a custom-designed surgical device. J Bone Joint Surg Am 2013; 95: e173. [DOI] [PubMed] [Google Scholar]
- 22.Murase T, Oka K, Moritomo H, et al. Three-dimensional corrective osteotomy of malunited fractures of the upper extremity with use of a computer simulation system. J Bone Joint Surg Am 2008; 90(11): 2375–2389. [DOI] [PubMed] [Google Scholar]
- 23.Tricot M, Duy KT, Docquier PL. 3D-corrective osteotomy using surgical guides for post-traumatic distal humeral deformity. Acta Orthop Belg 2012; 78: 538–542. [PubMed] [Google Scholar]
- 24.Farr S, Ganger R, Girsch W. Distal humeral flexion osteotomy for the treatment of supracondylar extension-type malunions in children. J Pediatr Orthop B 2018; 27(2): 115–120. [DOI] [PubMed] [Google Scholar]