Abstract
Objective
This study aimed to assess the reliability and validity of the translated Chinese version of the Service User Technology Acceptability Questionnaire (C-SUTAQ).
Methods
Patients with cancer (n = 554) from a tertiary hospital in China completed the C-SUTAQ. Item analysis, content and construct validity test, internal consistency test, and test-retest reliability analysis were conducted on the instrument to test its applicability.
Results
The critical ratio of each item of the C-SUTAQ ranged from 11.869 to 29.656; the correlation of each item and subscale ranged from 0.736 to 0.929. The Cronbach's α value for each subscale ranged from 0.659 to 0.941, and the test-retest reliability ranged from 0.859 to 0.966. The content validity index of the scale level and the item level content validity index of the instrument were both 1. Exploratory factor analysis indicated it was reasonable that the C-SUTAQ consists of six subscales after rotation. Confirmatory factor analysis demonstrated good construct validity (χ2/df = 2.459, comparative fit index = 0.922, incremental fit index = 0.907, standardized root mean square residual = 0.060, root-mean-square error of approximation = 0.073, goodness of fit index = 0.875, normed fit index = 0.876.
Conclusions
The C-SUTAQ had good reliability and validity and may be useful to assess Chinese patients’ acceptability of telecare. However, the small sample size limited generalization and there is a need to expand the sample to include persons with other diseases. Further studies are required using the translated questionnaire.
Keywords: Telecare, Technology acceptability, Cross-cultural adaptation, Reliability, Validity
Introduction
Telehealth is important to China to reduce the gap between rural and urban medical services, manage the high cost of access to medical services, and improve public health. However, few studies exist to understand the willingness of patients with cancer to use telehealth to improve or enhance their health outcomes.
In 2018, the National Health Commission of China launched the Action Plan for Further Improvement of Medical Services (2018–2020). This plan proposed the development of “Internet plus” as a means to provide patients with appropriate interventions for telehealth monitoring, education, administration, and research to promote the progressive development of telecare.1 Telecare or telehealth involves the use of mobile phones, video conferencing, and mobile applications (APP) to provide healthcare services between healthcare providers and patients in their homes or different geographic locations.2
Telecare has been gradually assimilated with long-term traditional care service models to manage chronic diseases, long-term care, and symptoms,3 which is especially suitable for patients with cancer.4 During the COVID-19 pandemic, strong recommendations were made to use telecare for patients with cancer as they were considered at high-risk for contracting the disease.5,6 Telecare could provide continuous care,4 help nurses manage symptoms and side effects post-chemotherapy, and improve efficiency.7,8 Telecare was particularly attractive for patients in remote locations to access health care 24/7 and reduce outpatient visits.
To serve patients better, our hospital provides telecare services mainly through WeChat mini-programs. Patients with cancer and those with chronic diseases, no longer queue to access the services of a doctor, examination results, or prescription medication. Patients also have the option to purchase prescription medication online and use express delivery. Telecare facilitates convenient reciprocal communication with healthcare professionals via text, images, or audio. In this way, healthcare professionals positively interacted with patients in consultations and guide postoperative patients and/or chemotherapy patients on exercise, diet, and schedule follow-up checks.
The rapid development of telecare in recent years has resulted in several evaluation tools to evaluate user satisfaction and assess the usability of telemedicine systems.9 The current aspects of telecare assessment tools include service subscales such as perception of risks and benefits,10 satisfaction,11 and usefulness12 from the patient's perspective, and acceptance13 and readiness assessment14 from the perspective of healthcare professionals. Patient perception is an important role in the evaluation of telecare services, as patient acceptability and satisfaction are relevant to any potential roll out of these services and commonly used indicators for measuring quality in health care.15,16 Patients with cancer who are willing to accept telecare will affect China's ability to successfully mainstream these services in the future.17 Our research focused on patients with cancer and their willingness to accept telehealth services.
The acceptability of telecare is often used synonymously with satisfaction.18 Hirani et al. investigated the concept of technology acceptance in more detail.19 In 2016, Hirani et al. developed the Service User Technology Acceptability Questionnaire (SUTAQ) to measure the acceptability of telehealth services among 478 older people in the UK. The tool was instructive as it could predict individual differences in beliefs and behavior and discriminate between groups to identify those more likely to reject telecare services.19 The 22-item SUTAQ instrument consists of 6 subscales: enhanced care, satisfaction, increased accessibility, kit as substitution, privacy and discomfort, and care personnel concerns. Based on a 6-point Likert-type scale, scores for each subscale were calculated using the mean of the items which were ranked from a higher to a lower score (6 “strongly agree” to 1 “strongly disagree”). The subscales privacy and discomfort and care-personnel concerns were inverted subscales, in which a high value reflected a negative attitude, while higher scores on the other four subscales indicated a more positive perception of telecare services. All subscales had a 3.5 median score.16 The instrument showed satisfactory results for reliability and validity and had been translated and applied in telemedicine services in countries such as Italy and Norway.16,18,20 The SUTAQ was considered an appropriate method for testing the acceptance of telecare technology.
Therefore, the objective of this study was to translate the English version of SUTAQ into Chinese and assess its validity as a tool for patient acceptability of telecare in China.
Methods
Study design
This cross-sectional study consisted of two phases: (1) translation and cross-cultural adaptation of the SUTAQ into Chinese to better reflect the Chinese healthcare and cultural environment and (2) testing of the reliability and validity of the C-SUTAQ in adult patients with cancer.
Description of the questionnaire
Phase 1: translation and cross-cultural adaptation procedures
The SUTAQ was translated from English to Chinese using the forward backward translation method based on recommendations from the World Health Organization.21 The WHODAS 2.0 Translation package Version 1.0 provided a protocol for translation and linguistic evaluation to enable uniform and standard application of health and disability-related classifications and linked assessment instruments worldwide. The guidelines provided specific recommendations for the procedure for translation and back-translation, including linguistic evaluation. Permission was first obtained from the designers of the questionnaire.
Forward translation and synthesis
Two native Chinese translators with nursing degrees and proficiency in English independently translated the SUTAQ into Chinese. One translator had a doctorate and the other had a master's degree (T1 and T2 versions). The two translators and a medical expert who had studied in the UK for at least one year analyzed and compared the two translated versions with the original instrument, discussed, and made modifications to obtain the forward translation (Version 1).
Back translation
Two translators (BT1 and BT2) were asked to back-translate the forward translation (Version 1). Both were nurses who had studied abroad but had no initial association with the SUTAQ. After discussions, a prefinal version was obtained.
Expert panel discussion and cross-cultural adaptation
Three professors, each in the area of linguistics, medicine, and nursing, and the four translators were invited to discuss and analyze the forward translation (Version 1) and back translation (Version 1) of the SUTAQ on an item-by-item basis. Checks were made for cross-cultural comparability and the conceptual equivalence between the C-SUTAQ and the SUTAQ to ensure semantic and conceptual consistency between both versions.
After a draft of the C-SUTAQ was obtained, Hirani et al. were contacted after which further modifications were made based on their suggestions. A few statements were changed to adhere better to the Chinese culture, they thought those are appropriate. They replied item 10 was not similar to item 22 and explained further that item 10 was about the process of care, ie, the service generally, while item 22 was about the outcome (health). We accepted their suggestions and changed a few statements for cultural adaptability. The questionnaire underwent two more revisions.
Pilot study
A pilot study was conducted among 30 eligible patients focused on evaluating the fluency of items. Cognitive interviews were conducted to identify any difficulties patients experienced in reading and understanding the items by asking the participants to rate the questionnaire. There is an open-ended question that allows participants to express their opinions about the questionnaire. Participants rated their scores for each item based on a 5-point Likert-type agreement scale. Scores for each item were ranked from a higher to a lower score (5 = strong fluency to 1 = weak fluency and 5 = strong comprehensibility to 1 = weak comprehensibility). No further modifications were required after the pilot study.
Phase 2: a validation field study
Participants and sample size
Patients hospitalized with cancer in the gynecology and oncology wards of a tertiary hospital in Shenyang were recruited using convenience sampling from the beginning of July 2022 to the end of November 2022.
The C-SUTAQ had 22 items. The sample size used for exploratory factor analysis (EFA) was 5–10 times of the items.22,23 The sample size was increased by 20% to allow for a drop out rate,24 and final sample size was 264. The sample size of confirmatory factor analysis (CFA) required ≥ 200 cases.22 A total of 564 instruments were distributed and 554 were returned representing an effective response rate of 98.23%. The data were inputted into the computer which randomly divided the data in half. One half (n = 277) was used for EFA and the other for CFA. A random selection of 41 participants answered the C-SUTAQ again at an interval of 14 days with the first complement required to assess the test-retest reliability.
The inclusion criteria were patients who: (1) were aged ≥ 18 years; (2) were diagnosed with malignant tumors by pathological or cytological examination, and were aware of their diagnosis; (3) used telecare service ≥ 3 times; (4) were willing to participate in this study. The exclusion criteria were patients who: (1) had a cognitive or mental impairment and were unable to communicate; (2) had a severe hearing impairment and were unable to communicate.
Data analysis
Data were analyzed using IBM SPSS v25.0 (IBM Corp., Armonk, NY, USA) and IBM AMOS v24.0 (IBM, Armonk, NY, USA). Descriptive statistics illustrated the demographic characteristics and mean ± SD or n (%).
Item analysis
(1) Critical ratio (CR) method: the total score of C-SUTAQ was sorted from high to low, then the data were divided into 2 subgroups by their scores (bounded by 27% and 73% quantiles). Independent samples for the t-test were chosen to calculate the CR for every item, where a value < 3 was considered for deletion25; (2) Correlative coefficient method: the correlation coefficient was used to indicate the correlation between each item and the total questionnaire scores, with a value > 0.4 considered to represent a good correlation between the two.25
Content validity
The content validity index (CVI) was applied to evaluate the content relevance, including the scale level (S-CVI) and the item level (I-CVI). Additionally, the panel of experts was instrumental in scoring the entire questionnaire and each item for relevancy, clarity, and cultural adaptability using a 4-point Likert scale (1 = strongly disagree, 2 = must be modified or disagree, 3 = agree after minor modification, 4 = strongly agree). I-CVI values were above > 0.78 and S-CVI values were above > 0.9.25
Construct validity
EFA was performed by principal components analysis with varimax rotation to obtain the factor structure. Kaiser–Meyer–Olkin's (KMO) measure and Bartlett's sphericity were verified before the EFA; a KMO value > 0.5 and significant Bartlett's test P < 0.05 were considered qualified. The factor loadings of each item were > 0.40.25
CFA verified the internal structure of the scale and whether the structural model fit the actual data. The parameters of the model were estimated using the maximum likelihood estimation method. A model with good fitness should meet the following criteria: χ2/df < 3; comparative fit index, incremental fit index, and Tucker–Lewis index > 0.9; standardized root mean square residual and root-mean-square error of approximation < 0.08.25 The goodness of fit index (GFI) and normed fit index (NFI) values should be greater than 0.90, which are relatively good.26 Many researchers interpret GFI and NFI values in the range of 0.8–0.9 are acceptable and represent a good fit as they are quite affected by the sample size.26,27
Reliability
Reliability was evaluated by internal consistency reliability and test-retest reliability. The internal consistency of the C-SUTAQ was tested by Cronbach's α coefficient. Cronbach's α coefficient ≥ 0.60 for each subscale indicated acceptable internal consistency.28 Text-retest reliability was tested by Pearson's correlation coefficient (r), where a value of > 0.70 was considered acceptable.29
Ethical considerations
The study was approved by the Ethics Committee of the First Affiliated Hospital of China Medical University (IRB No. AF-SOP-07-1.1-01). Participants provided written informed consent after the research objective and procedures regarding anonymity, withdrawal from the study, and permissions were explained. The data were aggregated from the self-reported paper and electronic questionnaires completed on the WeChat platform.
Results
Phase 1: translation and cross-cultural adaptation
The pilot study produced a fluency score of (4.70 ± 0.46) and a comprehensibility score of (4.73 ± 0.44). The readability and comprehensibility statistics were determined as satisfactory. All the items in the original SUTAQ were retained in the C-SUTAQ except that the kit referring to the Telehealth equipment was replaced with Telecare. All modifications were based on the Chinese culture and healthcare environment. For instance, (1) China has no social care as in the UK healthcare system. The phrase social care was replaced with care; (2) the phrase visit my General Practitioner (GP) clinic or other health/social care professional as often in the item The kit I received has saved me time in that I did not have to visit my GP clinic or other health/social care professional as often was translated as go to the hospital outpatient clinic to see my doctor or go to other health facilities (eg, health centers, community health centers, etc.); (3) the item The kit has been explained to me sufficiently was translated as Health care professionals have explained telecare to me sufficiently for patients’ better understanding; (4) the phrase my health in item The kit has made me more actively involved in my health was interpreted as my health management for clarity; (5) the phrase people looking after me in items 13,18 was changed to health care professionals as it was consistent with the healthcare situation.
Phase 2: validity and reliability of C-SUTAQ
Demographic characteristics
Of the sample of 554 patients with cancer, 250 (45.1%) were males and 304 (54.9%) were females. The age range was 34–79 years, with an average age of (60.92 ± 7.23) years. More details are shown in Table 1.
Table 1.
Demographic characteristics of the patients (n = 554).
| Characteristics | n (%) | Characteristics | n (%) | ||
|---|---|---|---|---|---|
| Gender | Male | 250 (45.1) | Disease | Lung cancer | 190 (34.3) |
| Female | 304 (54.9) | Colorectal cancer | 59 (10.6) | ||
| Education level | Breast cancer | 30 (5.4) | |||
| Primary school and below | 36 (6.5) | Stomach cancer | 38 (6.9) | ||
| Junior high school | 124 (22.4) | Cervical cancer | 80 (14.4) | ||
| High school | 335 (60.5) | Endometrial cancer | 60 (10.8) | ||
| College or above | 59 (10.6) | Ovarian cancer | 88 (15.9) | ||
| Tumor stage | I | 25 (4.5) | Others | 9 (1.6) | |
| II | 177 (31.9) | With other chronic diseases | |||
| III | 252 (45.5) | Yes | 293 (52.9) | ||
| IV | 100 (18.1) | No | 261 (47.1) | ||
Item analysis
A total of 554 questionnaires were submitted for item analysis. The results showed the CR value of each item was > 3 (P < 0.01), indicating a favorable differentiation (Table 2).
Table 2.
Item analysis for the C-SUTAQ (n = 554).
| Item | CR value | r value |
| 1. Telecare has saved me time because I do not have to often go to the hospital outpatient clinic to see my doctor or go to other health facilities (eg, health centres, community health centres, etc.). | 20.568 | 0.831∗∗ |
| 2. Telecare has interfered with my everyday life daily routine. | 23.804 | 0.853∗∗ |
| 3.Telecare has increased my access to care (from health care professionals). | 16.895 | 0.852∗∗ |
| 4. Telecare has helped me to improve my health. | 21.796 | 0.895∗∗ |
| 5. Telecare has invaded my privacy. | 18.970 | 0.778∗∗ |
| 6.Health care professionals have explained telecare to me sufficiently. | 29.656 | 0.916∗∗ |
| 7. Telecare can be trusted to work appropriately. | 26.940 | 0.911∗∗ |
| 8. Telecare has made me feel uncomfortable (eg, physically or emotionally). | 17.751 | 0.820∗∗ |
| 9. I am concerned about the level of expertise of those who monitor my status through telecare. | 20.836 | 0.845∗∗ |
| 10. Telecare has allowed me to be less concerned about my health and/or care. | 24.277 | 0.924∗∗ |
| 11. Telecare has made me more actively involved in my health management. | 19.561 | 0.898∗∗ |
| 12. Telecare makes me worry about my private information being leaked. | 24.546 | 0.852∗∗ |
| 13. Telecare allows health care professionals to better monitor me and my condition. | 22.001 | 0.929∗∗ |
| 14. I am satisfied with telecare. | 19.742 | 0.866∗∗ |
| 15. Telecare can/should be recommended to people in a similar condition to mine. | 19.840 | 0.855∗∗ |
| 16. Telecare can be a replacement for my regular health care. | 20.274 | 0.765∗∗ |
| 17. Telecare can be a good complement to my regular health. | 19.332 | 0.893∗∗ |
| 18. Telecare is not as suitable as regular face-to-face consultations with health care professionals. | 19.452 | 0.782∗∗ |
| 19. Telecare makes easier for me to get in touch with my health care professionals. | 17.697 | 0.865∗∗ |
| 20. Telecare interferes with the continuity of my care (ie, I cannot contact the same health care professional each time). | 22.122 | 0.850∗∗ |
| 21. I am concerned that the people who monitors my status via telecare does not know my health history. | 25.522 | 0.880∗∗ |
| 22. Telecare makes me reduce my concerns about my health condition. | 11.869 | 0.736∗∗ |
∗∗P<0.01.
Validity
Content validity: Seven experts with more than five years'experience and held senior titles of deputy or above were invited to assess the I-CVI and S-CVI. One expert was located in the discipline of English, one in medicine, two in medical informatics, and three in nursing. As a result of a Delphi expert consultation, the expert response rate was 100%, I-CVI ranged from 0.857 to 1.000, and S-CVI/Ave was 0.948.
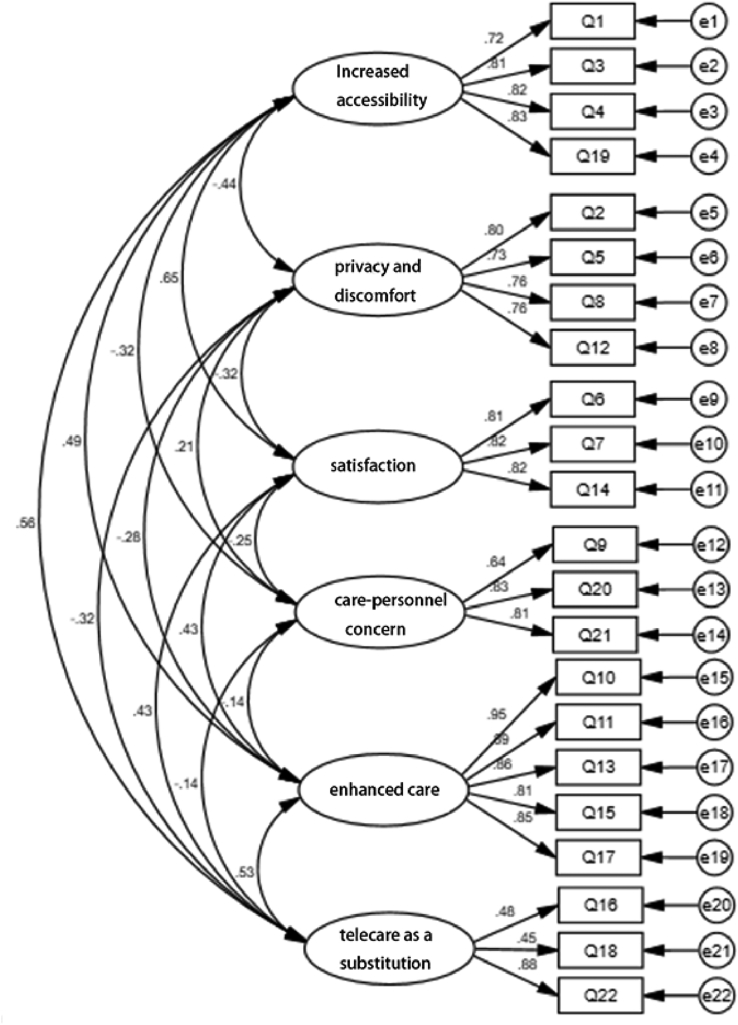
Construct validity EFA results showed that the KMO value of the C-SUTAQ was 0.872 and Bartlett's test was χ2 = 3806.392, P < 0.001, indicating the fitness for EFA. The principal components analysis with varimax rotation extracted six common factors, which were the same as the original SUTAQ. These were enhanced care, satisfaction, increased accessibility, telecare as a substitution, privacy and discomfort, and care-personnel concerns. All factor loadings were > 0.6, and the cumulative variance contribution rate was 75.46%, which met the requirement that the cumulative variance contribution rate should be at least 40%.25 The details are shown in Table 3. CFA results were good: χ2/df = 2.459, comparative fit index = 0.922, Tucker–Lewis index = 0.907, incremental fit index = 0.923, standardized root mean square residual = 0.060, root-mean-square error of approximation = 0.073, GFI = 0.875, and NFI = 0.876, which indicated that the six-factor model was fit (Fig. 1).26,27
Table 3.
Factor loadings of the C-SUTAQ (n = 277).
| Item | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Factor 6 |
|---|---|---|---|---|---|---|
| 1. Telecare has saved me time because I do not have to often go to the hospital outpatient clinic to see my doctor or go to other health facilities (eg, health centres, community health centres, etc.). | 0.772 | −0.227 | 0.137 | −0.095 | 0.131 | 0.180 |
| 3. Telecare has increased my access to care (from health care professionals). | 0.751 | −0.155 | 0.234 | −0.082 | 0.266 | 0.052 |
| 4. Telecare has helped me to improve my health. | 0.823 | −0.111 | 0.201 | 0.048 | 0.251 | 0.088 |
| 19. Telecare makes easier for me to get in touch with my health care professionals. | 0.794 | −0.180 | 0.168 | −0.150 | 0.213 | 0.031 |
| 2. Telecare has interfered with my everyday life daily routine. | −0.154 | 0.828 | −0.114 | 0.034 | −0.065 | 0.006 |
| 5. Telecare has invaded my privacy. | −0.165 | 0.736 | −0.011 | 0.148 | −0.144 | 0.087 |
| 8. Telecare has made me feel uncomfortable (eg, physically or emotionally). | −0.213 | 0.762 | −0.143 | 0.084 | −0.016 | −0.008 |
| 12. Telecare makes me worry about my private information being leaked. | −0.054 | 0.846 | −0.017 | 0.118 | −0.097 | 0.003 |
| 6. Health care professionals have explained telecare to me sufficiently. | 0.196 | −0.072 | 0.875 | −0.087 | 0.096 | 0.152 |
| 7. Telecare can be trusted to work appropriately. | 0.175 | −0.142 | 0.874 | 0.066 | 0.169 | 0.024 |
| 14. I am satisfied with telecare. | 0.277 | −0.060 | 0.777 | 0.035 | 0.265 | 0.024 |
| 9. I am concerned about the level of expertise of those who monitor my status through telecare. | −0.138 | 0.234 | −0.081 | 0.810 | −0.063 | 0.029 |
| 20. Telecare interferes with the continuity of my care (ie, I cannot contact the same health care professional each time). | −0.070 | 0.029 | 0.026 | 0.850 | 0.029 | 0.044 |
| 21. I am concerned that the people who monitors my status via telecare does not know my health history. | 0.000 | 0.099 | 0.055 | 0.875 | 0.057 | −0.037 |
| 10. Telecare has allowed me to be less concerned about my health and/or care. | 0.128 | −0.003 | 0.064 | 0.044 | 0.911 | 0.178 |
| 11. telecare has made me more actively involved in my health management. | 0.159 | −0.179 | 0.091 | 0.023 | 0.866 | 0.057 |
| 13. Telecare allows health care professionals to better monitor me and my condition. | 0.185 | −0.061 | 0.156 | 0.022 | 0.891 | 0.071 |
| 15. Telecare can/should be recommended to people in a similar condition to mine. | 0.214 | −0.023 | 0.317 | −0.006 | 0.764 | 0.182 |
| 17. Telecare can be a good complement to my regular health. | 0.231 | −0.108 | 0.068 | −0.066 | 0.856 | 0.035 |
| 16. Telecare can be a replacement for my regular health care. | 0.140 | 0.354 | 0.056 | −0.017 | 0.210 | 0.641 |
| 18. Telecare is not as suitable as regular face-to-face consultations with health care professionals. | 0.112 | −0.069 | 0.006 | −0.005 | 0.029 | 0.856 |
| 22. Telecare makes me reduce my concerns about my health condition. | 0.040 | −0.056 | 0.259 | 0.101 | 0.432 | 0.614 |
| Characteristic values | 3.238 | 1.934 | 1.833 | 1.304 | 7.089 | 1.205 |
| Cumulative variance contribution rate (%) | 13.387 | 26.657 | 38.165 | 48.442 | 67.851 | 75.461 |
Factor 1: increased accessibility; Factor 2: privacy and discomfort; Factor 3: satisfaction; Factor 4: care personnel concerns; Factor 5: enhanced care; Factor 6: telecare as a substitution.
Fig. 1.
Causal path diagram.
Reliability
The Cronbach's α of each subscale was > 0.8, except for telecare as a substitution, which was 0.659, indicating good internal consistency. A total of 41 patients completed and returned the retest survey. Pearson's correlation coefficient ranged from 0.859 to 0.966, showing an acceptable test-retest reliability (Table 4).
Table 4.
The reliability of the C-SUTAQ.
| Subscale | Cronbach's α (n = 554) | Test–retest reliability (n = 41) |
|---|---|---|
| Increased accessibility | 0.871 | 0.896∗∗ |
| Privacy and discomfort | 0.848 | 0.966∗∗ |
| Satisfaction | 0.854 | 0.859∗∗ |
| Care personnel concerns | 0.805 | 0.897∗∗ |
| Enhanced care | 0.941 | 0.934∗∗ |
| Telecare as a substitution | 0.659 | 0.896∗∗ |
∗∗ P<0.01
Discussion
This study translated the SUTAQ into Chinese and tested its validity and reliability among Chinese patients with cancer in a tertiary hospital and who had experience using telecare services. The results demonstrated that the C-SUTAQ (shown in Appendix A) was effective in capturing patients' perceptions of their acceptability of telecare. The translation and cross-cultural adaptation steps rigorously followed the WHO translation guidelines. A competent team of content experts and professional translators performed the forward and back translation and facilitated discussions for cross-cultural adaptation. In addition, the authors communicated with the original designers of SUTAQ to ensure conceptual and linguistic equivalence. We also conducted cognitive interviews to ensure the readability and comprehensibility of the instrument same as the Norwegian study.
The practicality of the scale
Similar to the Italian and Norwegian models, the C-SUTAQ was also adjusted for language and cultural modifications. To this end, the C-SUTAQ with a six-factor structure was developed, which was the same as the original version and the Italy version, All items in the original SUTAQ were retained in the C-SUTAQ, only some modifications were based on the Chinese culture and healthcare environment. For example, we replaced the kit (referring to the Telehealth equipment) with Telecare. Since Mainland China does not provide “social care” as interpreted in the UK,30 as patients are admitted to hospital when ill where they are cared for by doctors and nurses, rather than social care professionals, we replaced “social care” with “care”. This precise treatment also removed any ambiguities as identified in the Italian and original SUTAQ where reference to “social care” may have included relatives or other caregivers.16,19 For the same reason, the phrase people looking after me in items 13, 18 was changed to health care professionals as it was consistent with the healthcare situation and more clearer.
The scientificity of the scale
Content validity reflected the consistency of patients' understanding of the items and the designer's expectations about inquiry related to the relevant content. I-CVI and S-CVI were superior to the standard value, indicating agreement among the experts and their satisfaction with the scale. For structural validity, EFA was conducted using the principal component method. The results showed that the C-SUTAQ produced six common factors, which were consistent with the original questionnaire. The factor loadings of each item were > 0.4, showing that the questionnaire had good validity.31 The CFA results showed that each index met the requirement, indicating that the constructed model better reflected the original data and provided satisfactory fitness.
Internal consistency reliability of the C-SUTAQ was acceptable. The Cronbach's α of each subscale ranged from 0.659 to 0.941, the value for enhanced care subscale was highest at 0.941, indicating a high degree of acceptability of service in all clusters. This high degree of acceptability was also perceived in the C-SUTAQ as patients saw the service as an adjunct, which synced with Hirani et al.’s study (value of 0.831).19 The value for telecare as a substitution was lowest at 0.659, which was similar to the original SUTAQ (Hirani et al. reported a value of 0.642). The subscale for all clusters was between 3 and 4 indicating that patients moderately agreed that telecare service could act as a substitute for usual care. This response differed from Dario et al., who reported a range between 2 and 3 which suggested patients only mildly disagreed that telemedicine should act as a substitute, yet had a positive attitude toward telemonitoring.16 For this factor, the patients were divided since they were satisfied but because older persons formed the greater majority (69.31%) in the research, they may have had technical anxiety.30,32 We thought the lower value may because that most patients were satisfied with telecare and concurred it can reduce their concerns and was a good complement for regular health; however, they did not agree that telecare can replace the traditional face-to-face treatment mode.33 Accordingly, we inferred that older people might not be willing to use telecare, as most may need treatment due to their unique physical conditions or find it difficult to operate intelligent devices.32,34,35
The test-retest reliability of each subscale ranged from 0.859 to 0.966, which was good. The test-retest survey was completed by 41 patients with an interval of 14 days, indicating good temporal stability of the questionnaire.36 The Italian study conducted neither formal validation by performing for test-retest reliability16 nor did the Norwegian study as they had not attained sufficient numbers due to financial and logistic difficulties;18 therefore, statistical power could not be performed as was done in this study.
The final version of the C-SUTAQ contained 22 items, the original six subscales were confirmed which is the same as the original19 and Italian version.20 However, in the Norwegian version, the original subscales were not confirmed, although it revealed good internal consistency, with a Cronbach alpha of 0.851.18 The Norwegian results indicated that a one-factor solution, or at most a three-factor solution, was sufficient, as the explained variance increased by < 6% when adding more factors.18
The C-SUTAQ comprises short, easily understood, and convenient questions for patients to complete within 10 min. This confirmed the convenience of the instrument for investigating clinical situations in a time-bound situation. The SUTAQ can assess the acceptability of telecare services and explore the reasons for accepting/refusing telecare services. It can also function as a predictive tool for people who are more likely to refuse telecare services.19 Based on this small sample, the C-SUTAQ is proved to be an effective evaluation tool for telecare services in China and acts as a reference for the targeted implementation of personalized telecare services.
Limitations
However, there are some limitations to this study. First, the subjects of this research were all cancer patients. In the future, it might be instructive to investigate patients with other diseases, such as chronic obstructive pulmonary disease, diabetes, kidney, and heart disease. Second, criterion-related validity was not tested so it was impossible to compare the C-SUTAQ with the other validated measures. This should be considered in future studies to further confirm the instrument's applicability to China.
Conclusions
This study translated the SUTAQ to Chinese and established its good reliability and validity through testing on 554 Chinese patients with cancer. The study confirmed the C-SUTAQ suitability for assessing patients' acceptance of telecare services. The contents and items of the C-SUTAQ were easily understandable and convenient to complete. However, future investigations could include a pre-test and post-test design to explore patients’ willingness to accept and/or refuse telecare services. This may be conducive to designing more appropriate telecare services for wider groups of patients with one or more comorbidities.
Acknowledgments
A special thanks to Shashivadan P. Hirani and the team who established the SUTAQ and for their support and patience in responding to our questions throughout the study. We are also extremely appreciative of all translators and experts for their time, assistance, and interest in the study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.apjon.2023.100239.
Credit author statement
Nuo Cheng: Conceptualization, Methodology, Formal analysis, Writing - Original and Revised draft preparation. Yue Zhao: Investigation, Formal analysis. Xia Li: Investigation, Formal analysis. Xiuying He: Investigation, Validation. Aiping Wang: Methodology, Data curation, Writing - Revised draft preparation. All authors had full access to all the data in the study, and the corresponding author had final responsibility for the decision to submit for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Declaration of competing interest
All authors have none to declare.
Funding
This study received no external funding.
Ethics approval statement
This study was conducted after obtaining approval from the Research Ethics Review Committee of the First Affiliated Hospital of China Medical University (IRB No. AF-SOP-07-1.1-01). All participants provided written informed consent.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.National Health Commission . 2017. The Action Plan for Further Improvement of Medical Services (2018-2020) (Chinese)http://www.gov.cn/gongbao/content/2018/content_5299607.htm [Google Scholar]
- 2.Dennett A.M., Harding K.E., Peiris C.L., et al. Efficacy of group exercise-based cancer rehabilitation delivered via telehealth (TeleCaRe): protocol for a randomized controlled trial. JMIR Res Protoc. 2022;11(7) doi: 10.2196/38553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwok J., Olayiwola J.N., Knox M., et al. Electronic consultation system demonstrates educational benefit for primary care providers. J Telemed Telecare. 2018;24(7):465–472. doi: 10.1177/1357633X17711822. [DOI] [PubMed] [Google Scholar]
- 4.Rasche P., Wille M., Bröhl C., et al. Prevalence of health app use among older adults in Germany: national survey. JMIR Mhealth Uhealth. 2018;6(1):e26. doi: 10.2196/mhealth.8619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ohannessian R., Duong T.A., Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill. 2020;6(2) doi: 10.2196/18810. Published 2020 Apr 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin M., Guerrero-Zotano A., Montero Á., et al. GEICAM guidelines for the management of patients with breast cancer during the COVID-19 pandemic in Spain. Oncol. 2020;25(9):e1339–e1345. doi: 10.1634/theoncologist.2020-0363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Komariah M., Maulana S., Platini H., et al. A scoping review of telenursing's potential as a nursing care delivery model in lung cancer during the COVID-19 pandemic. J Multidiscip Healthc. 2021;14:3083–3092. doi: 10.2147/JMDH.S337732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kruse C., Fohn J., Wilson N., et al. Utilization barriers and medical outcomes commensurate with the use of telehealth among older adults: systematic review. JMIR Med Inform. 2020;8(8) doi: 10.2196/20359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hajesmaeel-Gohari S., Bahaadinbeigy K. The most used questionnaires for evaluating telemedicine services. BMC Med Inf Decis Making. 2021;21(1):36. doi: 10.1186/s12911-021-01407-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Demiris G., Speedie S., Finkelstein S. A questionnaire for the assessment of patients' impressions of the risks and benefits of home telecare. J Telemed Telecare. 2000;6(5):278–284. doi: 10.1258/1357633001935914. [DOI] [PubMed] [Google Scholar]
- 11.Yip M.P., Chang A.M., Chan J., et al. Development of the Telemedicine Satisfaction Questionnaire to evaluate patient satisfaction with telemedicine: a preliminary study. J Telemed Telecare. 2003;9(1):46–50. doi: 10.1258/135763303321159693. [DOI] [PubMed] [Google Scholar]
- 12.Bakken S., Grullon-Figueroa L., Izquierdo R., et al. Development, validation, and use of English and Spanish versions of the telemedicine satisfaction and usefulness questionnaire. J Am Med Inf Assoc. 2006;13(6):660–667. doi: 10.1197/jamia.M2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhen L., Yan Z., Zijuan Y., et al. Research progress of telecare assessment tools and evaluation indicators(Chinese) Nurs Res. 2019;33(19):3371–3374. doi: 10.12102/j.issn.1009-6493.2019.19.015. [DOI] [Google Scholar]
- 14.Liu Z., Zhang Y., Dong S., et al. The psychometric properties of the Chinese version of the telehealth readiness assessment tool (Chinese) Chinese Nursing Management. 2020;20(8):1154–1158. doi: 10.3969/j.issn.1672-1756.2020.08.008. [DOI] [Google Scholar]
- 15.Allemann Iseli M., Kunz R., Blozik E. Instruments to assess patient satisfaction after teleconsultation and triage: a systematic review. Patient Prefer Adherence. 2014;8:893–907. doi: 10.2147/PPA.S56160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dario C., Luisotto E., Dal Pozzo E., et al. Assessment of patients' perception of telemedicine services using the service user technology acceptability questionnaire. Int J Integrated Care. 2016;16(2):13. doi: 10.5334/ijic.2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rossen S., Kayser L., Vibe-Petersen J., et al. Technology in exercise-based cancer rehabilitation: a cross-sectional study of receptiveness and readiness for e-Health utilization in Danish cancer rehabilitation. Acta Oncol. 2019;58(5):610–618. doi: 10.1080/0284186X.2018.1562213. [DOI] [PubMed] [Google Scholar]
- 18.Torbjørnsen A., Småstuen M.C., Jenum A.K., et al. The service user technology acceptability questionnaire: psychometric evaluation of the Norwegian version. JMIR Hum Factors. 2018;5(4) doi: 10.2196/10255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hirani S.P., Rixon L., Beynon M., et al. Quantifying beliefs regarding telehealth: development of the whole systems demonstrator service user technology acceptability questionnaire. J Telemed Telecare. 2017;23(4):460–469. doi: 10.1177/1357633X16649531. [DOI] [PubMed] [Google Scholar]
- 20.Picardo E., Baù M.G., Anatrone C., et al. Oncophone20 study: patients' perception of telemedicine in the COVID-19 pandemic during follow-up visits for gynecological and breast cancers. Int J Gynaecol Obstet. 2021;155(3):398–403. doi: 10.1002/ijgo.13825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization . 2018. Process of Translation and Adaptation of Instruments.http://www.who.int/substance_abuse/research_tools/translation/en/ accessed December 2022. [Google Scholar]
- 22.Minglong W. Chongqing University Press; Chongqing Province: 2010. Structural Equation Modeling - Operation and Application of AMOS(Chinese) [Google Scholar]
- 23.Lai J., Zhang R., Hong M., Li N. Development and validation of the nurse's workplace mental health questionnaire. Int J Nurs Sci. 2022;9(4):521–528. doi: 10.1016/j.ijnss.2022.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Allman-Farinelli M., Partridge S.R., McGeechan K., et al. A mobile health lifestyle program for prevention of weight gain in young adults (TXT2BFiT): nine-month outcomes of a randomized controlled trial. JMIR Mhealth Uhealth. 2016;4(2):e78. doi: 10.2196/mhealth.5768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tang P., Lu Q., Wu Y., et al. The Chinese version of the quality of life in childhood epilepsy questionnaire-16-C (QOLCE-16-C): translation, validity, and reliability. Health Qual Life Outcome. 2022;20(1):52. doi: 10.1186/s12955-022-01960-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li C.H., Chan O.L.K., Chow Y.T., et al. Evaluating the effectiveness of digital content marketing under mixed reality training platform on the online purchase intention. Front Psychol. 2022;13 doi: 10.3389/fpsyg.2022.881019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abedi G., Rostami F., Nadi A. Analyzing the dimensions of the quality of life in hepatitis B patientsusing confirmatory factor analysis. Global J Health Sci. 2015;7(7 Spec No):22–31. doi: 10.5539/gjhs.v7n7p22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chowdhury S.R., Kabir H., Chowdhury M.R., et al. Workplace bullying and violence on burnout among Bangladeshi registered nurses: a survey following a year of the COVID-19 pandemic. Int J Publ Health. 2022;67 doi: 10.3389/ijph.2022.1604769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.La Touche R., Pardo-Montero J., Cuenca-Martínez F., et al. Cross-cultural adaptation and psychometric properties of the Spanish version of the tampa scale for kinesiophobia for temporomandibular disorders. J Clin Med. 2020;9(9):2831. doi: 10.3390/jcm9092831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Simpson G., Mutindi Kaluvu L., Stokes J., et al. Understanding social care need through primary care big data: a rapid scoping review. BJGP Open. 2022;6(4) doi: 10.3399/BJGPO.2022.0016. BJGPO.2022.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang C., Yang Z., Zhang H. Psychometric evaluation of the Chinese version of occupational LowBack pain prevention behaviors questionnaire among clinical nurses: a validation study. Front Public Health. 2022;10 doi: 10.3389/fpubh.2022.827604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu L., Wu F., Tong H., et al. The digital divide and active aging in China. Int J Environ Res Publ Health. 2021;18(23) doi: 10.3390/ijerph182312675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rodler S., Apfelbeck M., Schulz G.B., et al. Telehealth in uro-oncology beyond the pandemic: toll or lifesaver? Eur Urol Focus. 2020;6(5):1097–1103. doi: 10.1016/j.euf.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chunxiao N., Yiqin S., Hui L. Research status and development strategy of tele-home care (Chinese) Chin J Nurs. 2016;51(11):1344–1348. doi: 10.3761/j.issn.0254-1769.2016.11.013. [DOI] [Google Scholar]
- 35.Stavropoulos T.G., Lazarou I., Diaz A., et al. Wearable devices for assessing function in alzheimer's disease: a European public involvement activity about the features and preferences of patients and caregivers. Front Aging Neurosci. 2021;13 doi: 10.3389/fnagi.2021.643135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yi H., Chen H., Wang X., Xia H. Cross-cultural adaptation and validation of the Chinese version of the brace questionnaire. Front Pediatr. 2022;9 doi: 10.3389/fped.2021.763811. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.