Abstract
In this descriptive, qualitative study, we conducted eight focus groups with diverse informal and formal caregivers to explore their experiences/challenges with nursing home (NH) to emergency department (ED) transfers and whether telehealth might be able to mitigate some of those concerns. Interviews were transcribed and analyzed using a grounded theory approach. Transfers were commonly viewed as being influenced by a perceived lack of trust in NH care/capabilities and driven by four main factors: questioning the quality of NH nurses’ assessments, perceptions that physicians were absent from the NH, misunderstandings of the capabilities of NHs and EDs, and perceptions that responses to medical needs were inadequate. Participants believed technology could provide “the power of the visual” permitting virtual assessment for the off-site physician, validation of nursing assessment, “real time” assurance to residents and families, better goals of care discussions with multiple parties in different locations, and family ability to say goodbye.
Keywords: nursing home, emergency department, telehealth, care transitions, focus group
Introduction
Nursing home (NH) residents commonly experience potentially avoidable emergency department (ED) visits and hospitalizations (Ouslander et al., 2010). Such unnecessary care transitions are not only disruptive and disorienting for an already frail population, but they increase the risk of complications and account for more than US$2.6 billion in Medicare expenditures (Walsh et al., 2012). Since October 2012, the Centers for Medicare and Medicaid Services has monitored and subsequently imposed financial penalties to hospitals for excessive 30-day readmission rates. Until recently, however, NHs were not part of this monitoring and financial penalty process. As of 2018, under the Skilled Nursing Facility Value-Based Purchasing (SNF VBP) Program, NHs are now required to measure their potentially preventable 30-day postdischarge readmissions and will be subject to incentivized payments based on performance beginning January 2019. Thus, decreasing inappropriate ED or hospital transfers may improve outcomes and decrease costs, making this a high priority for patients, families, NHs, and health systems.
Concerns about the quality of NH care, particularly symptom management (Ersek & Jablonski, 2014), are long standing and often contribute to unnecessary ED transfers (Stephens, Sackett, Govindarajan, & Lee, 2014). Such care quality concerns are fueled by the lack of relevant diagnostic resources within NHs (especially laboratory results and electrocardiograms), the unavailability of on-site medical expertise, the quality of assessment of resident changes in condition (Gruneir et al., 2010; Oneill, Parkinson, Dwyer, & Reid-Searl, 2015; Unroe et al., 2018), and lack of available palliative care services and supports in the NH setting (Chang, Chen, & Chang, 2009; Tsai & Tsai, 2010; Unroe et al., 2018; Woods & Snow, 2013). Underlying chronic, suboptimal staffing levels further compound these issues (Gozalo et al., 2011; Gruneir et al., 2010; Miller, Lima, Looze, & Mitchell, 2012).
Studies further suggest that families play a significant role in ED transfer decisions (Boockvar & Burack, 2007; Houttekier et al., 2014; Lamb, Tappen, Diaz, Herndon, & Ouslander, 2011; Robinson et al., 2012; Simmons, Durkin, Rahman, Schnelle, & Beuscher, 2014; Stephens et al., 2015). For example, when they are faced with a change in their loved one’s condition, they often perceive the most reasonable alternative is to opt for an ED evaluation (Tappen et al., 2014). Such family transfer decisions are driven by perceptions of inadequate NH care and lack of understanding of their loved one’s prognosis and what treatment options are available in the NH (Cusack et al., 2008; Stephens et al., 2015). As a result, NH residents commonly undergo burdensome and potentially preventable care transitions for symptoms or conditions, such as pneumonia, urinary tract infections, and dehydration, that can be safely and effectively treated in the NH setting (Casarett et al., 2005; Loeb et al., 2006; Unroe et al., 2018; Walsh et al., 2012).
Emerging health technologies (EHTs), such as telehealth or telemedicine, are increasingly being used as a care transitions solution across several domains in health care, including NH care (Edirippulige, Martin-Khan, Beattie, Smith, & Gray, 2013; Sävenstedt, Zingmark, & Sandman, 2004). The ability to provide remote delivery of health care services and clinical information using telecommunications technology can include, but is not limited to, the use of wireless tools, email, two-way video, smartphones, remote physical assessment, electronic transmission of digital images, monitoring of vital signs remotely, and other methods of telecommunications technology to improve patient health status. Recent studies suggest EHTs have the potential to improve access to care and care coordination and provide more timely assessments through virtual consultations and provider visits (Chang et al., 2009; Cusack et al., 2008; Rahman, Foster, Grabowski, Zinn, & Mor, 2013; Sävenstedt et al., 2004; Tsai & Tsai, 2010; Woods & Snow, 2013). No studies to date, however, have specifically triangulated diverse stakeholder concerns about factors driving ED transfers and how EHTs might address those concerns. Evidence suggests that including the perspectives of end users of technology-based interventions (e.g., patients, families, providers) enhances the relevance of the research to the actual health decisions they face, and improves uptake of the approach and the likelihood that patients will achieve the health outcomes they desire (Frank, Basch, & Selby, 2014).
To address these gaps in knowledge, we conducted eight 2-hr focus group interviews to explore diverse formal and informal caregiver perspectives on (a) the experiences and challenges they faced with NH resident transfers to the ED and (b) the potential role of EHTs to help address those concerns.
Research Design and Method
Study Design
We utilized an exploratory qualitative approach using focus group interviews (n = 8 groups, average five participants) to better understand stake-holders’ perspectives on NH to ED transfers, and whether telehealth interventions might be able to mitigate against potentially avoidable transfers. The institutional review board for the University of California, San Francisco, approved this study.
Sample and Setting
Eligible study participants included English-speaking formal and informal caregivers involved in the care of an NH resident transferred to the hospital in the prior 3 to 6 months. Such caregivers included NH resident family members; NH administrators, providers, and nursing staff; as well as ED and hospital providers. We used an array of methods to recruit participants, including displaying recruitment posters, meeting in person, emailing individuals, and via select local and statewide NH listservs. We also promoted snowball sampling.
We chose focus groups as the most pragmatic approach for collecting data from this diverse group of individuals that included busy health professionals from different NHs and health systems (Creswell, 2014; Sandelowski, 2000). Focus groups took place in the San Francisco Bay Area, most in private rooms in a public library. Initially, purposeful sampling was used to construct focus groups of like individuals (e.g., NH nurses). This strategy was used to minimize potential real and perceived power differentials, ensuring that groups felt comfortable talking to one another. As recurrent themes became apparent, groups of mixed stakeholders (e.g., providers and families) were convened. The meeting of different perspectives further optimized the richness, depth, diversity, and complexity of group dynamics by eliciting stories and experiences (Jayasekara, 2012; Speziale & Carpenter, 2003). Individuals were only allowed to participate in one focus group.
Procedures
After obtaining informed consent, the principal investigator (C.S.) facilitated the focus group using a semistructured interview guide, whereas the study coordinator (E.H.) recorded field notes and observations. Each participant was then asked to describe recent experience(s) where they were involved with an NH resident who transferred to the ED. The second part of the focus group began with a video demonstration of a telehealth consult between an off-site physician, NH resident, family member, and NH nurse. Participants were asked how they might have used this technology in the recent ED transfer they had described earlier, and how that technology might have changed that experience. Interviews were recorded, transcribed verbatim, and then checked for accuracy.
Analysis
Analysis was undertaken using a grounded theory approach in which inductive reasoning allows findings to emerge from the data (Charmaz, 2004; Strauss, 1987). Constant comparative analysis initially involved line-by-line coding and continued with emergent analytical strategies that included memo writing and integrative diagramming techniques to examine relationships and conceptualize themes within the data (Charmaz, 2014). Research team members met regularly to reach consensus on codes and identify concepts, categories, and themes from patterns in the data. The interview guide was refined to reflect these emerging concepts (see the appendix). Data saturation was reached when no new concepts or perspectives were introduced during the focus groups (Charmaz, 2004; Strauss, 1987). Several strategies were employed to ensure the trustworthiness of this study: the considered use of reflexivity by the research team to examine their preconceptions and biases, methodological transparency, and the collection of rich and sufficient data from a wide range of informants.
Results
Participant Characteristics
Characteristics of the 41 focus group participants are shown in Table 1. The sample included six family members, 16 NH nurses (six licensed vocational nurses and 10 registered nurses), 11 primary care providers (including six NH physicians, four nurse practitioners, one physician assistant [PA]), two ED physicians, two ED nurses, three NH administrators, and one hospitalist. Participants were from facilities in three different counties spanning urban, suburban, and semirural areas. There was no relationship between the NH and ED settings. Fifty-one percent of the participants were above the age of 46 years, 63% were female, and 50% were White. Approximately half of all the health care providers had more than 15 years of clinical practice or experience as NH administrator.
Table 1.
Demographics and Characteristics of Formal and Informal Caregivers (N = 41).
| n (%) | |
|---|---|
| Age (years) | |
| 18–35 | 6 (15) |
| 36–40 | 8 (20) |
| 41–45 | 7 (18) |
| 46–50 | 5 (13) |
| Above 50 | 15 (38) |
| Gender | |
| Male | 16 (40) |
| Female | 25 (63) |
| Race | |
| American Indian/Alaska Native | 1 (3) |
| Asian | 11 (28) |
| Native Hawaiian/Other Pacific Islander | 1 (3) |
| Black or African American | 2 (5) |
| White | 20 (50) |
| More than one race | 1 (3) |
| Unknown/not reported | 5 (13) |
| Participant role | |
| Family member/responsible party | 6 (15) |
| NH nursea | 16 (46) |
| NH physician | 6 (17) |
| Nurse practitioner/physician assistant | 5 (14) |
| ED nurse | 2 (6) |
| ED physician | 2 (6) |
| NH administrator | 3 (9) |
| Hospitalist | 1 (3) |
| Years of experience in clinical practice/NHs for health care providers | |
| 1–5 | 8 (23) |
| 6–10 | 7 (20) |
| 10–15 | 3 (9) |
| More than 15 | 17 (49) |
NH nurses included six licensed vocational nurses and 10 RNs. RNs served in leadership roles, as is typically found in nursing homes, such as directors of nursing, MDS coordinators, and directors of staff development.
NH = nursing home; ED = emergency department; RN = registered nurse; MDS = minimum data set.
“They Don’t Trust Us”
Resident transfers to the ED were commonly seen by all stakeholders as being influenced by a perceived lack of trust in NH care and capabilities. This lack of trust was described as being driven by four main factors: questioning the quality of NH nurses’ assessments; perceptions that physicians were absent from the NH; misunderstandings of the capabilities of NHs and EDs; and perceptions that responses to medical needs were inadequate (see Figure 1).
Figure 1.
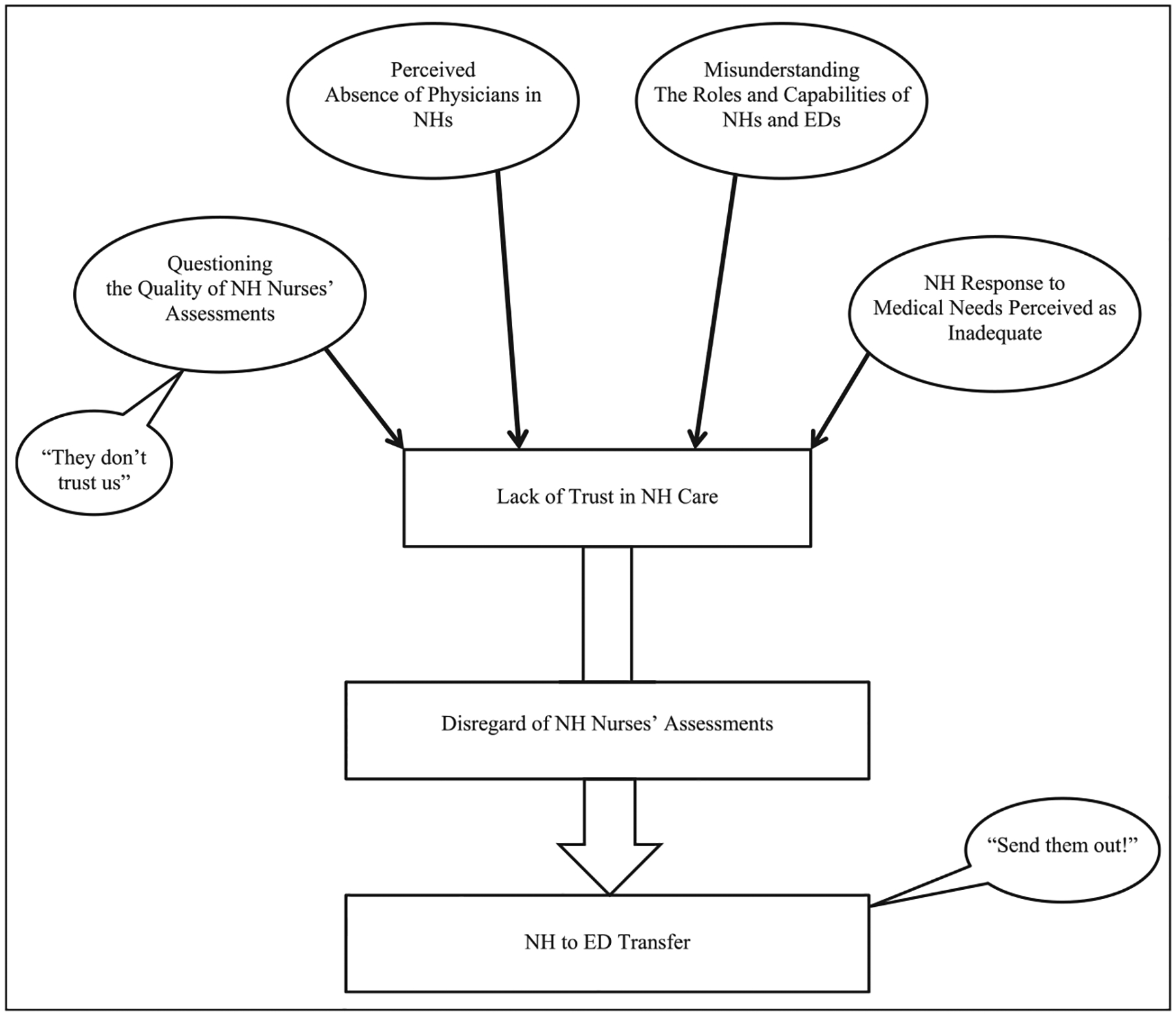
“They don’t trust us” driving NH to emergency room transfers.
Note. NH = nursing home; ED = emergency department.
Questioning the quality of NH nurses’ assessments.
Questioning the quality of NH nurses’ assessments was described as driving ED transfers. NH providers described their trust of assessments as dependent on knowing the individual nurse, and cited inconsistencies in quality and detail. ED providers described NH nurses’ assessments as minimal, incomplete, illegible, or absent, and expressed their frustrations in trying to get further information by phone. Even the nurses themselves described their nursing colleagues’ lack of confidence as a contributing factor to care transitions:
Some of the nurses might not be as comfortable, you know, making that decision [to treat at the NH]. They might think … “I’d rather send the patient out than take that risk” … [they’re] not confident enough …
(nurse)
NH nurses described a lack of trust in having their assessments disregarded, ignored, or overruled with resulting transfers to ED they regarded as unnecessary. At times, they described feeling unheard:
[The physician] said, “no, you call 911.” Well, based on my assessment, the patient that’s stable doesn’t need a 911 … [the physician] said, “so all you have to do is you have to follow doctor’s orders.” Okay, I call 911, they [emergency medical technicians (EMTs)] arrive, they look, and they said “so why did you call us?” Because [the physician] said so. I mean, they even question my assessment, they don’t trust us …
(nurse)
In addition to having her assessment ignored by the physician and being told to blindly follow orders, this nurse also had to deal with the criticism of the EMTs when they arrived. Similar situations involving dehydration and high blood glucose levels were described, where NH nurses would have been able to do what the ED staff did—start an I.V. or give insulin. Frustration at not being able to influence the decision to transfer was compounded by the ED staff assuming the transfer was the NH nurse’s responsibility.
The absence of physicians in the NH.
Family members and NH nurses described the lack of physician presence in the NH as influencing transfer to the ED. Physicians were often not available to give reassurance to families, regarding goals of care or to undertake clinical assessments, and this led to a lack of trust in NH competence.
NH nurses described the need families had to speak to the physician in person, especially when it came to setting expectations and determining goals of care. In the physician’s absence, these nurses described feeling like the unwelcome messenger, distrusted to relay information accurately:
I think … [the physician interaction is] key, because a lot of our patients are like, well, “I want to see my doctor,” and it’s like, “well, you can’t … ” … the physician is very important for the patients, the families, to feel reassured, because we’re just telling them what the doctor said … And sometimes it’s like “well, I really kind of don’t believe you.”
(nurse)
Family members described rarely seeing a doctor in the NH, and expressed disappointment and lost opportunities for conversations about important issues:
I only saw the doctor once … she was on vacation … they had someone at the end of the phone … but no one coming to the NH itself apparently … the level of care that the physicians were providing to support the NH was really much more limited than I would like to have seen … there was never any discussion about whether the DNR was appropriate …
(family member)
NH nurses are required to inform the NH physician of a resident’s change in condition. In describing this, nurses told of their frustration when an NH physician, often unfamiliar with the resident, reacted to news of a change of condition by sending the resident out to the ED. This decision was often counter to their own clinical assessment, and was often perceived as the NH physician covering himself or herself against all eventualities. In this example, the NH nurse’s frustration was palpable:
Oh, it frustrates me, because I just want them to take more time to thoroughly assess … I can … give them my report, but … it’s just, “all right, send them out … ” … Do I feel that the doctor … could have assessed more [before sending them out]? Oh, yes, he could have been doing a lot more.
(nurse)
ED providers also attributed limited initial assessment by NH physicians as resulting in unnecessary transfers and medical interventions:
… there’s a lot of “let me just cover myself.” It’s not uncommon to see someone coming for chest pain. When was chest pain? It was four hours ago, … sometimes [the transfer is a result of] the doctor on call saying “I don’t know the patient, so send them to the ER.”
(physician)
The absence of physicians in the NH was described as eroding the overall trust in NH care. Physicians’ inability to directly assess situations led them to default to transfer, a decision compounded by physician mistrust of assessments of nurses physically present with residents.
Misunderstanding the roles of NHs and EDs.
The focus group conversations elicited data that characterized the lack of trust in NH care as a simple misunderstanding of what NHs could provide, and what constituted an appropriate referral to the ED. Both families and NH physicians were reported as seeking transfers to ED for hydration, infection, and hypo/hyperglycemic episodes that NH nurses and ED staff perceived could have been managed in the facility. This view was supported by the daughter of a resident, where she perceived not only that the NH’s regular care was not adequate but also that this care is best provided in the ED:
… when she [mother] has a UTI, I prefer her to go out [to the ED] then to just do the regular thing here and give her antibiotics. They need to run some tests on her blood and urine and see what’s going on.
(daughter)
This misunderstanding of the ED as a place not for emergency care, but rather as a source of supplementary care, was reinforced by descriptions from NH nurses:
… whenever she [resident] was sick, she would say she needs to go [to ED] … and … [doctor] would just say, “yup, send her out … ” … And so that’s why she ended up going multiple times.
(nurse)
Questioning the need for transfer to the ED for nonemergency issues was a frequent theme illustrated here by an ED physician who queried why residents who have abnormal laboratory results are transferred:
… so we get a lot of transports just for abnormal labs … And I find that very frustrating, because if somebody has always been anemic, and they’re anemic today, why are you sending them to the ER?
(physician)
The use of emergency services for residents who were actively dying was another cause for concern among providers and families. One director of nursing estimated half of the Medicare patients they sent to the hospital had died there.
Reflected in these accounts was the perception that families had not adjusted to the reality of death being close at hand. A lack of trust in NH care, misunderstandings about what EDs are capable of, and failure to set residents’ and families’ expectations, all contributed to situations such as these where families insisted on transfer to the ED against provider advice:
… [the family] felt the patient should go to the hospital … [the nurse said] the patient was fine, but that the family was just super anxious and upset. I said, okay, I’ll see them … Within a half hour, the family had called 9-1-1 themselves … sometimes they just go right past the nursing home.
(PA)
These data reflect that motivations for a transfer to the ED and expectations from such a visit were often not associated with emergency care needs, but driven by challenges with prognostication, capabilities for more intensive care in the NH setting, and an underlying lack of trust. Because decisions were made using these criteria, the ED was seen as a place where NH residents all too often arrived to die.
Perceptions that NH responses to medical needs were inadequate.
Perceptions were expressed that NHs were often unable to respond to residents’ medical needs (e.g., symptom management, diagnostic evaluation, and provision of medical nutrition and hydration), and that responses were slow. Providers and families were perceived as driven to demand ED transfer because they perceived that their loved one’s medical needs would not be met in the NH:
… the family is saying, “well, they’re [NH] not taking care of your pain,” or “I’m not getting whatever I need,” or conditions are … they’re below their expectations I guess.
(physician)
Specifically, the inability to get timely laboratory tests, analgesics, and feeding tubes reinserted in the NH were themes in the data, and were perceived as contributing factors to ED transfer:
… if you just had a few more tests done, which can’t be done there [in NH], you could avoid an emergency department … such as maybe a hemogram, IV or urinalysis in a timely manner … but they’re not really practicable in a present situation.
(physician)
Untreated pain was often described as occurring shortly after admission to the NH, resulting from issues of access to medication due to confused communication, poor documentation, and incomplete protocols relating to narcotic prescriptions:
… she wanted pain pills, you know, we were trying to rush the pharmacy, couldn’t get the pain pills, and her LOC [level of consciousness] just decreased hour by hour, [she was] just getting more and more confused, more and more agitated … And so, we sent her out [to the ED].
(nurse)
Perceptions of inadequate responses to medical needs and unmet expectations contributed to the lack of trust in NH care, and promoted transition to ED as solution.
“The Power of the Visual”
When asked which potential features of EHTs would have been beneficial in their experiences with NH resident transfers, participants repeatedly spoke about perceiving the use of remote visual connections between residents, families, and providers in and outside the NH as an asset. This concept was characterized by stakeholders as the power of the visual. This technology was potentially seen as able to influence decisions related to ED transfer in ways that included permitting virtual assessment for the off-site physician, validation of nursing assessment, “real time” assurance to residents and families, better goals of care discussions with multiple parties in different locations, and family ability to say goodbye.
The ability for off-site physicians to conduct virtual assessments using technology was described as reducing the likelihood of transfers and improving on what one NH physician described as his usual “frustrating telephone experience” in undertaking assessments. Other NH physicians agreed, one concluding that video conference with screen sharing of a prior electrocardiography (EKG) could
most definitely … save you from sending somebody off to the emergency department … the physician could be more comfortable in having a person treated in the facility with this added technology.
(NH physician)
The power of the visual for remote physician assessments was exemplified in this description:
… there are times, if you could just put your eyes on the patient, you would know right away whether or not they were sick, or not sick.
(NH physician)
It was seen as a better use of physicians’ time too:
… if they [physicians] could be doing it from their office, even if it’s at the end of the day after they’ve [physicians] seen their patients, they scope out an hour or half-an-hour where they’re going to be doing this, I think that would be a plus for them not to have to hop in their car.
(nurse)
Nurses identified the power of the visual as a feature that would allow “ … everybody to be on the same page.” For the NH physician to be present with the nurse and resident through technology was seen by nurses as a way of gaining validation for their assessments:
… there would be more credibility of the clinical decision and clinical assessment of the nurses in the eyes of the physician, he’d have more confidence, and I think we, as nurses, would like the support. I love the idea.
(nurse)
Because a lot of the times, we describe, we assess, and we say what we see. But sometimes with the physicians [remotely], hearing, seeing, what we’re seeing, you know, it’s a lot better.
(nurse)
Being on the same page through visual connection was perceived as especially useful where family members were not in agreement, lived at a distance, or were not at the NH when residents experienced a change of condition and transfer was being considered:
… [visual technology] would have been helpful in several ways. First, if it was just the family, like perhaps if they could see what their mom looked like, on the bed, and perhaps maybe feel what we felt …
(nurse)
In the case where residents feel a lack of connection with their NH physician, and anxious about lack of access to them, participants described how video connections might help. For example, in talking about whether he sees himself using EHT in his practice, this physician said,
Most definitely … I just think the more information we have, both paper information, but also the visual information [the better]. And I think, in the video, I think it’s hugely important for patients and family to see, you know, see the face of the clinician.
(NH physician)
Nurses also appreciate this aspect of EHT potential:
So that’s the biggest complaint that they have is … “I never even see my doctor, he doesn’t even come by … ” … they would just be more reassured [connecting through technology].
(nurse)
Nurses further described the remote presence of the NH physician as increasing resident’s trust in their care and confidence in their physician:
… I think that these methods of video feed could certainly enhance the care given to the resident, and their … confidence in their doctor.
(nurse)
A final benefit attributed to the power of the visual was illustrated with this key example. Unable to be at her husband’s side in the last hours of his life, this woman made the decision to transfer him to the ED. He died in transit, and she lives with her regret:
… if you had this kind of technology [a visual], you’d be aware sooner [that your loved one was dying], people would be able to notify you within a reasonable amount of time, so you might be able to see your family member before they pass. But even if you aren’t, you can at least say good-bye. And that was very hard—not being able to say good-bye.
(wife)
These data relating to the power of the visual describe the potential of using existing and accessible technology to help mitigate issues of trust in NH care.
Discussion
In this descriptive, qualitative study we conducted eight focus groups with diverse informal and formal caregivers to explore their experiences and challenges with NH resident ED transfers and whether EHT interventions might be able to mitigate some of those concerns. Consistent with prior research (Charmaz, 2004; Ersek & Jablonski, 2014; Gruneir et al., 2010; Oneill et al., 2015; Stephens, Newcomer, Blegen, Miller, & Harrington, 2012; Stephens et al., 2014; Wang, Shah, Allman, & Kilgore, 2011), we found that ED transfers are often driven by the lack of on-site medical expertise, communication challenges, and questioning the quality of assessment of, and response to, resident changes in condition. This is the first study, however, to characterize this overarching phenomenon of “They Don’t Trust Us” driving ED transfers and connect stakeholder concerns regarding such transfers with potential technology-based solutions. Our diverse informal and formal caregivers felt that the challenges to decision making in an untrusting and uncertain environment may be mitigated by the use of technology to improve communication, trust, and assessment prior to making a decision to send a resident to the ED. Specifically, these stakeholders felt telehealth could permit virtual assessments by the off-site physician, validation of nursing assessment, “real time” assurance to residents and families, better goals of care discussions with multiple parties in different locations, and family ability to say goodbye.
Preventable ED transfer from NHs has been identified as a key quality measure in health care (Neuman, Wirtalla, & Werner, 2014; Ouslander et al., 2016). Medicare has adopted financial incentives to minimize preventable rehospitalizations for patients discharged to NHs from hospitals. Until recently, NHs received no penalty for hospital readmissions. As of 2018, however, skilled nursing facilities are required to measure potentially preventable 30-day postdischarge readmissions in the Skilled Nursing Facility Quality Reporting Program (Centers for Medicare & Medicaid Services [CMS] & U.S. Department of Health and Human Services [HHS], 2016). In January 2019, NHs will be subject to incentivized payments as outlined by the SNF VBP Program, which includes performance on this quality measure (CMS & U.S. HHS, 2016). Consequently, this study identifies modifiable factors that may limit avoidable NH rehospitalizations, potentially reducing costs of care.
Several NH factors have historically contributed to potentially avoidable hospitalizations of NH residents. These include underresourced skilled nurse staffing; communication barriers and challenges between staff, residents, family, and providers; flawed care processes; and suboptimal advance care planning and palliative care discussions (Dellefield, Castle, Mcgilton, & Spilsbury, 2015; Gillespie, Gleason, Karuza, & Shah, 2010; Harrington, Olney, Carrillo, & Kang, 2012; Harrington, Schnelle, Mcgregor, & Simmons, 2016; Ouslander et al., 2016; Unroe et al., 2018; Walsh et al., 2012). Studies suggest that NH residents residing in facilities with higher staffing levels, more highly skilled professionals (e.g., nurse practitioners), and work environments that support nurses’ professional development have a lower risk of potentially preventable hospitalizations (Dubois et al., 2013; Konetzka, Spector, & Limcangco, 2008).
Some progress has been made through the implementation of evidence-based quality initiative programs such as the Interventions to Reduce Acute Care Transfers (INTERACT), which has been associated with a 24% reduction in hospitalizations of NH residents (Ouslander, Bonner, Herndon, & Shutes, 2014). Use of structured communication tools, such as the Situation–Background–Assessment–Recommendation form from INTERACT (Pathway Health, 2018), can enhance communication with doctors and bedside mentoring to improve clinical assessment skills of nursing staff (Unroe et al., 2018). Improving the strength of nursing assessments and clarity of communication of findings to NH resident primary care providers and families may further increase the confidence of all stakeholders to initiate treatment of acutely ill residents in the facility rather than sending them to the hospital (Unroe et al., 2018).
According to CMS, 45% of NH resident hospital admissions could be avoided if telehealth were available. NH providers express an openness to using telehealth for consultation to prevent avoidable rehospitalization; yet, few have identified ways to harness these interventions (Driessen et al., 2018). Telehealth has been a useful intervention to optimize health care in a number of SNF environments. Surveillance of dangerous lab values and automated clinical decision support for NH residents have used telehealth to trigger automated alerts in electronic health records (Culley, Perera, Marcum, Kane-Gill, & Handler, 2015; Kane-Gill, Achanta, Kellum, & Handler, 2016; Kane-Gill et al., 2017). Others have successfully used off-hour telemedicine consultation as opposed to on-call NH providers to reduce preventable NH to ED transfers (Grabowski & O’Malley, 2014). Telehealth has been successfully employed as a means to bring clinical consulting to the NH environment to assess diabetic foot ulcer care (Kolltveit et al., 2018), motor symptoms in Parkinson’s disease (Biglan et al., 2009), psychiatric health (Rabinowitz et al., 2010), and geriatric conditions (Georgeton et al., 2015). The extension for community healthcare outcomes (ECHO) projects telehealth study joined frontline NH staff with clinical experts at an academic medical center for video case discussion and didactic training on dementia and psychology management, and reduced physical restraint use by 75% and antipsychotic use by 17% compared with control facilities (Gordon et al., 2016). Each of these studies introduces telehealth in NHs as a means to bring virtual support to resource-limited NH environments.
The growth of telehealth in health care has been exponential and introduces new challenges and opportunities in virtually every aspect of care for patients (Nochomovitz & Sharma, 2018). Although limited interventions have been used in the NH setting, the field is primed for adoption of novel technological solutions to address persistent systemic problems. Understanding the perspectives of the end users of technology-based interventions (e.g., patients, families, providers) enhances the relevance of the research to the actual health decisions they face, and improves uptake of the approach and the likelihood that patients will achieve the health outcomes they desire (Frank et al., 2014).
This study supports the use of telehealth in the NH and suggests a novel application: incorporating telehealth technology with visual and audio real-time capabilities to overcome family mistrust of clinical decision making in NH environment. In these circumstances, telehealth has the added potential for meaningful palliative care discussions about goals and values of care to make more informed decisions with respect to hospital transfers. Citing the key theme, “the power of the visual,” providers and family members expressed the desire of “being on the same page” to overcome mistrust of the NH staff and communication misconceptions about goals of care.
This study has some important limitations to consider. First, the study sample was relatively small and only included perspectives of resident families and providers across three counties in northern California. Individuals in other parts of the state and country might have different experiences and perspectives. Second, the inability to engage NH residents in the focus groups (due to complex medical conditions, potential fatigue, and transportation logistics) leaves a big gap in understanding this phenomenon from the resident perspective. Future studies should aim to integrate this important perspective. Third, the positive outlook on the use of telehealth technology may be attributed to participants self-selecting to participate in this study based on their technology interests. Those not interested in technological solutions in the NH setting may have opted not to participate in the study. Nevertheless, rich qualitative data were obtained from a wide range of stakeholders with different roles and working in diverse settings, including for-profit/not-for-profit and large chain/small chain facilities located in both urban and suburban settings primarily serving ethnically and racially diverse communities.
In conclusion, this study highlights key themes identified by families, NH nurses, and NH and ED providers that contribute to unnecessary ED transfers. Each stakeholder group supports the use of telehealth to improve the quality of assessments and communication, reduce mistrust, and potentially reduce avoidable transfers. Although telehealth has been used to provide consultation and management in NHs, this study also supports its use for improved communication between family members and staff to avert avoidable ED transfers when care could be provided in the NH environment. Future research is needed to better understand how this technology could also improve access to palliative care expertise and support in the NH setting. Such an application of telehealth may further improve communication regarding goals of care, anticipatory guidance, and overall symptom management, thereby reducing expensive, and often burdensome, care transitions at the end of life.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported by the National Institutes of Health (K76AG054862); University of California, San Francisco (UCSF) Clinical and Translational Sciences Institute (8 KL2 TR0001870-01); UCSF Claude D. Pepper Older Americans Independence Center; and by Tideswell at UCSF, which promotes promising new research aimed at better understanding and addressing late-life disability in vulnerable populations (all to CS).
Biographies
Caroline E. Stephens is an associate professor in the UCSF School of Nursing’s Department of Community Health Systems and associate Director of UCSF’s Hartford Center of Gerontological Nursing Excellence.
Elizabeth Halifax is an assistant clinical professor in UCSF School of Nursing’s Department of Physiological Nursing and Senior Clinical Research Coordinator for this project.
Daniel David is an assistant professor in UCSF School of Nursing’s Department of Community Health Systems and was a VA Quality Scholar postdoctoral fellow at the San Francisco VA during this project.
Nhat Bui is an adult gerontological nurse practitioner at Asian Health Services in Oakland, CA and served as a research assistant on this project.
Sei J. Lee is an associate professor in the UCSF Division of Geriatrics and Senior Scholar of the San Francisco VA Quality Scholars fellowship.
Janet Shim is a professor of Sociology in UCSF School of Nursing’s Department of Social and Behavioral Sciences.
Christine S. Ritchie is the Harris Fishbon Distinguished Professor in Clinical Translational Research and Aging in the UCSF Division of Geriatrics.
Appendix
Excerpts From the Focus Group Guide.
|
Introductions First, I would like to ask each of you to introduce yourself, state your role in caring for NH residents, and briefly tell us why you were interested in participating in this focus group study. Experience caring for residents requiring further ED evaluation Think back to a recent experience you had with an NH resident who became ill and required a transfer to the ED. Take a few moments to silently reflect on what that experience was like and how it unfolded. Now, I’d like to go around and ask each of you to describe what happened in that recent experience. I think we should have enough time for each of you to talk for about 3–5 min or so. Probes
Now, I would like to show you a short video demonstration of a telehealth consultation. Telehealth is the use of digital technologies to deliver care and health education by connecting users in different locations. This video shows a visit between an NH resident, daughter, nurse, and primary care provider. It is from 4 years ago. Now, we have many more health technologies at our disposal. But the video will hopefully give you an idea of how telehealth could potentially be used in the NH context. Now that you have watched the video, let me tell you about the new potential features and capabilities that could be used (hand out list). Perceptions of telehealth technology in practice Based on the video and list of potential features, I would like you to tell us how you might have used the technology in the situation you described earlier and how the technology might have changed that experience. Probes
Now, please take a moment to put your initials at the top of the paper and then circle those features and capabilities that would most enhance your care of NH residents requiring a possible ED evaluation. Feel free to write any notes for us on the paper. Perceived barriers and incentives to implementing telehealth technology Now I would like to ask you, could you see yourselves using this kind of technology in the future? Probes
|
Note. NH = nursing home; ED = emergency department.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Biglan KM, Voss TS, Deuel LM, Miller D, Eason S, Fagnano M, … Dorsey ER (2009). Telemedicine for the care of nursing home residents with Parkinson’s disease. Movement Disorders, 24, 1073–1076. doi: 10.1002/mds.22498 [DOI] [PubMed] [Google Scholar]
- Boockvar KS, & Burack OR (2007). Organizational relationships between nursing homes and hospitals and quality of care during hospital-nursing home patient transfers. Journal of the American Geriatrics Society, 55, 1078–1084. doi: 10.1111/j.1532-5415.2007.01235.x [DOI] [PubMed] [Google Scholar]
- Casarett D, Karlawish J, Morales K, Crowley R, Mirsch T, & Asch DA (2005). Improving the use of hospice services in nursing homes. Journal of the American Medical Association, 294, 211–217. doi: 10.1001/jama.294.2.211 [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services & U.S. Department of Health and Human Services. (2016). Medicare program; Prospective payment system and consolidated billing for skilled nursing facilities for FY 2017, SNF value-based purchasing program, SNF quality reporting program, and SNF payment models research. Final rule. Federal Register, 81, 51969–52053. [PubMed] [Google Scholar]
- Chang J, Chen L, & Chang C (2009). Perspectives and expectations for telemedicine opportunities from families of nursing home residents and caregivers in nursing homes. International Journal of Medical Informatics, 78, 494–502. doi: 10.1016/j.ijmedinf.2009.02.009 [DOI] [PubMed] [Google Scholar]
- Charmaz K (2004). Premises, principles, and practices in qualitative research: Revisiting the foundations. Qualitative Health Research, 14, 976–993. doi: 10.1177/1049732304266795 [DOI] [PubMed] [Google Scholar]
- Charmaz K (2014). Constructing grounded theory. London, England: Sage. [Google Scholar]
- Creswell JW (2014). Research design: Qualitative, quantitative, and mixed methods approaches (4th ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Culley CM, Perera S, Marcum ZA, Kane-Gill SL, & Handler SM (2015). Using a clinical surveillance system to detect drug-associated hypoglycemia in nursing home residents. Journal of the American Geriatrics Society, 63, 2125–2129. doi: 10.1111/jgs.13648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cusack CM, Pan E, Hook JM, Vincent A, Kaelber DC, & Middleton B (2008). The value proposition in the widespread use of telehealth. Journal of Telemedicine and Telecare, 14, 167–168. doi: 10.1258/jtt.2007.007043 [DOI] [PubMed] [Google Scholar]
- Dellefield ME, Castle NG, Mcgilton KS, & Spilsbury K (2015). The relationship between registered nurses and nursing home quality: An integrative review (2008–2014). Nursing Economics, 33, 95–108, 116. [PubMed] [Google Scholar]
- Driessen J, Chang W, Patel P, Wright RM, Ernst K, & Handler SM (2018). Nursing home provider perceptions of telemedicine for providing specialty consults. Telemedicine and e-Health, 24, 510–516. doi: 10.1089/tmj.2017.0076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubois CA, D’amour D, Tchouaket E, Clarke S, Rivard M & Blais R (2013). Associations of patient safety outcomes with models of nursing care organization at unit level in hospitals. International Journal for Quality in Health Care, 25(2), 110. doi: 10.1093/intqhc/mzt019 [DOI] [PubMed] [Google Scholar]
- Edirippulige S, Martin-Khan M, Beattie E, Smith AC, & Gray LC (2013). A systematic review of telemedicine services for residents in long term care facilities. Journal of Telemedicine and Telecare, 19, 127–132. [DOI] [PubMed] [Google Scholar]
- Ersek M, & Jablonski A (2014). A mixed-methods approach to investigating the adoption of evidence-based pain practices in nursing homes. Journal of Gerontological Nursing, 40, 52–60. doi: 10.3928/00989134-20140311-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank L, Basch E, & Selby JV (2014). The PCORI perspective on patient-centered outcomes research. Journal of the American Medical Association, 312, 1513–1514. doi: 10.1001/jama.2014.11100 [DOI] [PubMed] [Google Scholar]
- Georgeton E, Aubert L, Pierrard N, Gaborieau G, Berrut G, & Decker LD (2015). General practitioners adherence to recommendations from geriatric assessments made during teleconsultations for the elderly living in nursing homes. Maturitas, 82, 1842–189. doi: 10.1016/j.maturitas.2015.06.038 [DOI] [PubMed] [Google Scholar]
- Gillespie SM, Gleason LJ, Karuza J, & Shah MN (2010). Healthcare providers’ opinions on communication between nursing homes and emergency departments. Journal of the American Medical Directors Association, 11, 204–210. doi: 10.1016/j.jamda.2009.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon SE, Dufour AB, Monti SM, Mattison ML, Catic AG, Thomas CP, & Lipsitz LA (2016). Impact of a videoconference educational intervention on physical restraint and antipsychotic use in nursing homes: Results from the ECHO-AGE pilot study. Journal of the American Medical Directors Association, 17, 553–556. doi: 10.1016/j.jamda.2016.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gozalo P, Teno JM, Mitchell SL, Skinner J, Bynum J, Tyler D, & Mor V (2011). End-of-life transitions among nursing home residents with cognitive issues. The New England Journal of Medicine, 365, 1212–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC, & O’Malley AJ (2014). Use of telemedicine can reduce hospitalizations of nursing home residents and generate savings for Medicare. Health Affairs, 33, 244–250. doi: 10.1377/hlthaff.2013.0922 [DOI] [PubMed] [Google Scholar]
- Gruneir A, Bell CM, Bronskill SE, Schull M, Anderson GM, & Rochon PA (2010). Frequency and pattern of emergency department visits by long-term care residents—A population-based study. Journal of the American Geriatrics Society, 58, 510–517. doi: 10.1111/j.1532-5415.2010.02736.x [DOI] [PubMed] [Google Scholar]
- Harrington C, Olney B, Carrillo H, & Kang T (2012). Nurse staffing and deficiencies in the largest for-profit nursing home chains and chains owned by private equity companies. Health Services Research, 47, 106–128. doi: 10.1111/j.1475-6773.2011.01311.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington C, Schnelle JF, Mcgregor M, & Simmons SF (2016). Article commentary: The need for higher minimum staffing standards in U.S. nursing homes. Health Services Insights, 9. doi: 10.4137/hsi.s38994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houttekier D, Vandervoort A, Van de Block L, van der Steen JT, Stichele RV, & Deliens L (2014). Hospitalizations of nursing home residents with dementia in the last month of life: Results from a nationwide survey. Palliative Medicine, 28, 1110–1117. doi: 10.1177/0269216314535962 [DOI] [PubMed] [Google Scholar]
- Jayasekara RS (2012). Focus groups in nursing research: Methodological perspectives. Nursing Outlook, 60, 411–416. doi: 10.1016/j.outlook.2012.02.001 [DOI] [PubMed] [Google Scholar]
- Kane-Gill SL, Achanta A, Kellum JA, & Handler SM (2016). Clinical decision support for drug related events: Moving towards better prevention. World Journal of Critical Care Medicine, 5, 204–211. doi: 10.5492/wjccm.v5.i4.204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane-Gill SL, Niznik J, Kellum J, Culley C, Boyce R, Marcum Z, …Handler S (2017). Use of telemedicine to enhance pharmacist services in the nursing facility. The Consultant Pharmacist, 32, 93–98. doi: 10.4140/tcp.n.2017.93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolltveit BH, Thorne S, Graue M, Gjengedal E, Iversen MM, & Kirkevold M (2018). Telemedicine follow-up facilitates more comprehensive diabetes foot ulcer care: A qualitative study in home-based and specialist health care. Journal of Clinical Nursing, 27, e1134–e1145. doi: 10.1111/jocn.14193 [DOI] [PubMed] [Google Scholar]
- Konetzka RT, Spector W, & Limcango MR (2008). Reducing hospitalizations from long-term care settings. Medical Care Research and Review, 65(1), 40. [DOI] [PubMed] [Google Scholar]
- Lamb G, Tappen R, Diaz S, Herndon L, & Ouslander JG (2011). Avoidability of hospital transfers of nursing home residents: Perspectives of frontline staff. Journal of the American Geriatrics Society, 59, 1665–1672. doi: 10.1111/j.1532-5415.2011.03556.x [DOI] [PubMed] [Google Scholar]
- Loeb M, Carusone SC, Goeree R, Walter SD, Brazil K, Krueger P, … Marrie T (2006). Effect of a clinical pathway to reduce hospitalizations in nursing home residents with pneumonia. Journal of the American Medical Association, 295, 2503–2510. doi: 10.1001/jama.295.21.2503 [DOI] [PubMed] [Google Scholar]
- Miller SC, Lima JC, Looze J, & Mitchell SL (2012). Dying in U.S. nursing homes with advanced dementia: How does health care use differ for residents with, versus without, end-of-life Medicare skilled nursing facility care? Journal of Palliative Medicine, 15, 43–50. doi: 10.1089/jpm.2011.0210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuman MD, Wirtalla C, & Werner RM (2014). Association between skilled nursing facility quality indicators and hospital readmissions. Journal of the American Medical Association, 312, 154–1551. doi: 10.1001/jama.2014.13513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nochomovitz M, & Sharma R (2018). Is it time for a new medical specialty? Journal of the American Medical Association, 319, 437–438. doi: 10.1001/jama.2017.17094 [DOI] [PubMed] [Google Scholar]
- Oneill B, Parkinson L, Dwyer T, & Reid-Searl K (2015). Nursing home nurses’ perceptions of emergency transfers from nursing homes to hospital: A review of qualitative studies using systematic methods. Geriatric Nursing, 36, 423–430. doi: 10.1016/j.gerinurse.2015.06.001 [DOI] [PubMed] [Google Scholar]
- Ouslander JG, Bonner A, Herndon L, & Shutes J (2014). The INTERACT quality improvement program: An overview for medical directors and primary care clinicians in long-term care. Journal of the American Medical Directors Association, 15, 162–170. doi: 10.1016/j.jamda.2013.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouslander JG, Lamb G, Perloe M, Givens JH, Kluge L, Rutland T, … Saliba D (2010). Potentially avoidable hospitalizations of nursing home residents: Frequency, causes, and costs. Journal of the American Geriatrics Society, 58, 627–635. doi: 10.1111/j.1532-5415.2010.02768.x [DOI] [PubMed] [Google Scholar]
- Ouslander JG, Naharci I, Engstrom G, Shutes J, Wolf DG, Alpert G, … Newman D (2016). Root cause analyses of transfers of skilled nursing facility patients to acute hospitals: Lessons learned for reducing unnecessary hospitalizations. Journal of the American Medical Directors Association, 17, 256–262. doi: 10.1016/j.jamda.2015.11.018 [DOI] [PubMed] [Google Scholar]
- Pathway Health INTERACT. (2019). Retrieved from: http://www.pathway-interact.com
- Rabinowitz T, Murphy KM, Amour JL, Ricci MA, Caputo MP, & Newhouse PA (2010). Benefits of a telepsychiatry consultation service for rural nursing home residents. Telemedicine and e-Health, 16, 34–40. doi: 10.1089/tmj.2009.0088 [DOI] [PubMed] [Google Scholar]
- Rahman M, Foster AD, Grabowski DC, Zinn JS, & Mor V (2013). Effect of hospital–SNF referral linkages on rehospitalization. Health Services Research, 48, 1898–1919. doi: 10.1111/1475-6773.12112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson C, Bottorff J, Lilly M, Reid C, Abel S, Lo M, & Cummings G (2012). Stakeholder perspectives on transitions of nursing home residents to hospital emergency departments and back in two Canadian provinces. Journal of Aging Studies, 26, 419–427. doi: 10.1016/j.jaging.2012.06.001 [DOI] [PubMed] [Google Scholar]
- Sandelowski M (2000). Combining qualitative and quantitative sampling, data collection, and analysis techniques in mixed-method studies. Research in Nursing & Health, 23, 246–255. [DOI] [PubMed] [Google Scholar]
- Sävenstedt S, Zingmark K, & Sandman P (2004). Being present in a distant room: Aspects of teleconsultations with older people in a nursing home. Qualitative Health Research, 14, 1046–1057. doi: 10.1177/1049732304267754 [DOI] [PubMed] [Google Scholar]
- Simmons SF, Durkin DW, Rahman AN, Schnelle JF, & Beuscher L (2014). The value of resident choice during daily care: Do staff and families differ? Journal of Applied Gerontology: The Official Journal of the Southern Gerontological Society, 33, 655–671. doi: 10.1177/0733464812454010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speziale HJ, & Carpenter DR (2003). Qualitative research in nursing: Advancing the humanistic imperative (3rd ed.). Philadelphia, PA: Lippincott Williams & Wilkins. [Google Scholar]
- Stephens CE, Halifax E, Bui N, Lee SJ, Harrington C, Shim J, & Ritchie C (2015). Provider perspectives on the influence of family on nursing home resident transfers to the emergency department: Crises at the end of life. Current Gerontology and Geriatrics Research, 2015, 893062. doi: 10.1155/2015/893062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens CE, Newcomer R, Blegen M, Miller B, & Harrington C (2012). Emergency department use by nursing home residents: Effect of severity of cognitive impairment. The Gerontologist, 52, 383–393. doi: 10.1093/geront/gnr109 [DOI] [PubMed] [Google Scholar]
- Stephens CE, Sackett N, Govindarajan P, & Lee SJ (2014). Emergency department visits and hospitalizations by tube-fed nursing home residents with varying degrees of cognitive impairment: A national study. BMC Geriatrics, 14, Article 35. doi: 10.1186/1471-2318-14-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss AL (1987). Qualitative analysis for social scientists. Cambridge, UK: Cambridge University Press. [Google Scholar]
- Tappen RM, Worch SM, Elkins D, Hain DJ, Moffa CM, & Sullivan G (2014). Remaining in the nursing home versus transfer to acute care: Resident, family, and staff preferences. Journal of Gerontological Nursing, 40, 48–57. doi: 10.3928/00989134-20140807-01 [DOI] [PubMed] [Google Scholar]
- Tsai H, & Tsai Y (2010). Older nursing home residents’ experiences with video-conferencing to communicate with family members. Journal of Clinical Nursing, 19, 1538–1543. doi: 10.1111/j.1365-2702.2010.03198.x [DOI] [PubMed] [Google Scholar]
- Unroe KT, Hickman SE, Carnahan JL, Hass Z, Sachs G, & Arling G (2018). Investigating the avoidability of hospitalizations of long stay nursing home residents: Opportunities for improvement. Innovation in Aging, 2(2), 1–9. doi: 10.1093/geroni/igy017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh EG, Wiener JM, Haber S, Bragg A, Freiman M, & Ouslander JG (2012). Potentially avoidable hospitalizations of dually eligible Medicare and Medicaid beneficiaries from nursing facility and home- and community-based services waiver programs. Journal of the American Geriatrics Society, 60, 821–829. doi: 10.1111/j.1532-5415.2012.03920.x [DOI] [PubMed] [Google Scholar]
- Wang HE, Shah MN, Allman RM, & Kilgore M (2011). Emergency department visits by nursing home residents in the United States. Journal of the American Geriatrics Society, 59, 1864–1872. doi: 10.1111/j.1532-5415.2011.03587.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods LW, & Snow SW (2013). The impact of telehealth monitoring on acute care hospitalization rates and emergency department visit rates for patients using home health skilled nursing care. Home Healthcare Nurse, 31, 39–45. doi: 10.1097/nhh.0b013e3182778dd3 [DOI] [PubMed] [Google Scholar]


