Abstract
Objectives:
Previous studies on a potential association between endodontic infection (EI) and cardiovascular disease (CVD) produced mixed results. Endodontic treatment (ET) may also be linked to cardiovascular risk, as a marker for prior chronic dental infection and subclinical EI in other teeth. We tested the hypothesis that ET is associated with elevated risk of coronary heart disease (CHD), ischemic stroke (IS), heart failure (HF), or venous thromboembolism (VTE).
Methods:
ARIC participants who completed the dental ancillary study exam 4 (1996–1998; n = 6,638) were included in the analyses. Participants were followed through 2013 for CHD, stroke, and HF and 2011 for VTE. Cox-proportional hazards regression models were used to estimate hazard ratios (HR) and 95% confidence intervals (CI) for CHD, IS, HF, and VTE across ET classifications adjusting for age, sex, race/center, education, income, smoking, alcohol consumption, BMI, statin use, family history of CHD, physical activity, diet quality, insurance status, last dental visit, dental visit frequency, having a current dentist, and tooth loss due to gum disease.
Results:
Among participants, 21.0% reported a single ET, while 28.5% reported multiple ETs. Over a median of 15.8 years of follow-up, there were 506 incident CHD events, 311 IS events, 739 HF events, and 219 VTE events. There were no significant associations between self-reported history of ET and any of our outcomes (HR (95%CI): CHD = 1.16 (0.87,1.44), IS = 0.77 (0.55,1.09), HF = 1.00 (0.81,1.24), VTE = 0.98 (0.67,1.43)) after adjustment.
Conclusions:
Our results do not support an independent association between ET and development of CHD, IS, HF, or VTE.
Keywords: endodontic, endodontic treatment, infection, cardiovascular diseases, coronary disease, stroke, heart failure, venous thromboembolism
Introduction
Endodontic infection (EI) is a chronic inflammatory disease caused by infection of the dental root canal system in the pulp of the tooth and the major etiologic agent of apical periodontitis (AP) or infection of the apex of the tooth root.1 Previous studies on the association between EI/AP and cardiovascular disease (CVD) have been mixed with some studies not supporting an association2,3 while other studies demonstrated an association.4–7 The primary mechanisms linking EI/AP and CVD includes systemic inflammation8 that leads to atherosclerotic development, platelet aggregation, and hypercoagulability.6
EI/AP is relatively common; estimates of the prevalence among adults in western countries have varied between 14% and 70%.9 EI/AP is treated through root canal, or endodontic treatment (ET). In the absence of radiographic information about EI/AP, one way to estimate history of EI/AP is through self-reported previous ET.
In 2006, Joshipura et al. evaluated the association between ET and CHD among males from the Health Professionals Follow-Up Study. They found compared to men without ET, those with ET had higher CHD risk but the association was limited to dentists and no association was observed among nondentists.10 In 2009, using data from the Atherosclerosis Risk in Communities study (ARIC) dental ancillary study (D-ARIC), Caplan et al. reported a cross-sectional association between self-reported history of ET and prevalent CHD among study participants with 25 or more teeth but failed to find an association among those with 24 or fewer teeth.5 At present, few previous studies have prospectively evaluated the association between ET and the longitudinal development of ischemic stroke (IS), heart failure (HF), or venous thromboemsoblism (VTE), and evidence for CHD requires additional inquiry due to the mixed results of previous studies including Joshipura et al and Caplan et al.5,10 Therefore, we used longitudinal data from the ARIC study to test the hypothesis ET is independently associated with risk of incident CHD, incident IS, incident HF, and incident VTE since it may be a marker of subclinical EI and future EI. We further hypothesized the association would be graded with those with multiple ETs at highest risk of incident cardiovascular events.
Methods
The ARIC study is a multicenter population-based prospective cohort study designed to investigate the etiology and natural history of atherosclerosis in middle-aged Americans.11 At baseline in 1987–1989 (visit 1), 15,792 mostly white and black men and women ages 45–64 were enrolled from 4 U.-S. communities: Forsyth County, North Carolina; Jackson, Mississippi; suburbs of Minneapolis, Minnesota; and Washington County, Maryland.11 Subsequent clinic exams took place during 1990 to 1992 (visit 2), 1993 to 1995 (visit 3), 1996 to 1998 (visit 4), 2011 to 2013 (visit 5), and 2016-2017(visit 6) with continuous surveillance for CVD events. A dental ancillary study (D-ARIC) took place among ARIC participants at all 4 study sites during visit 4 (1996–1998) to determine the prevalence, extent, and severity of periodontal conditions in the dentate ARIC population.12 All ARIC participants who had natural teeth, no contraindications, and did not require antibiotic prophylaxis for periodontal probing were eligible to participate in D-ARIC. Details of the D-ARIC study objectives and methodology have been described in a previous publication.13 Institutional review board approval for ARIC and D-ARIC was obtained at each participating site, and informed consent was obtained from each participant.
We used a prospective cohort study design in which visit 4 (1996–1998) served as the baseline for these analyses. All ARIC participants who completed the dental history questionnaire and D-ARIC exam (n = 6,638) were included in the analysis. Those of races other than black and white (n = 25), African-Americans from the Minnesota or Maryland field centers (n = 24) where small numbers were recruited, and those taking anticoagulants at baseline (visit 4) (n = 61) who may be less susceptible to infection-induced hypercoagulability were excluded from the analysis. Only prevalent cases of each outcome as determined by self-report at study entry or incident CVD events occurring prior to the dental exam were excluded. Our final sample sizes after exclusions were n = 6,274 for CHD, n = 6,397 for IS, n = 6,196 for HF, and n = 6,400 for VTE.
Endodontic therapy ascertainment
The exposure of interest was self-reported history of root canal treatment, which was assessed as part of the D-ARIC study during visit 4 (1996–1998). Exposure was classified according to responses to the questions, “Have you ever had root canal therapy?” and “(If you have had root canal therapy), Have you had more than one?” Exposure was trichotomized as multiple root canals, one root canal, and no root canals. Participants whose ET status was unknown were excluded.
Covariate ascertainment
Covariate information from the time of the dental exam (visit 4) was used, unless otherwise noted. Demographic factors included age, race, education (visit 1; some high school or less, high school diploma, college degree or higher), and income (<$25,000/year, $25,000 – <$50,000/year, $50,000 – <$75,000/year, >$75,000/year). Traditional CVD risk factors included smoking (current, former, never), diabetes (yes/no), hypertension (yes/no), LDL (mg/dL), HDL (mg/dL), triglycerides (mg/dL), statin use (yes/no), BMI (Kg/M2), and alcohol consumption (yes/no and grams/week). Family history of premature CHD (yes/no) was defined at visit 1 by participant self-report of a heart attack occurring in a father before age 55 or in a mother before age 60.14 Physical activity and diet quality (ideal, intermediate, and poor) were categorized according to the American Heart Association (AHA) definitions for cardiovascular health, as has been done previously in ARIC.15 Finally, access to care and dental care use data were collected during the D-ARIC dental history questionnaire. These included medical insurance status (private insurance, medicare/medicaid only, none), last dental visit (<6 months ago, 6 months – <2 years ago, 2 – <5 years ago, >5 years ago), dental visit frequency (regularly, only for discomfort or repair, do not regularly visit the dentist), and having a current dentist (yes/no). Periodontal disease was assessed using self-reported history of tooth loss due to gum disease (yes/no).
Outcome ascertainment
The outcomes of interest were incident CHD, incident IS, incident HF, and incident VTE. Each outcome was analyzed separately. The methods used for outcome ascertainment included: (1) participants were contacted annually by phone and interviewed about interim hospitalizations; (2) local hospitals provided lists of hospital discharges with cardiovascular diagnoses, and these were reviewed to identify cohort hospitalizations; and (3) participant names were linked to state and national death registries. CVD events were classified by a combination of computer algorithm and adjudicated physician review; disagreements were adjudicated by the ARIC Mortality and Morbidity Classification Committee using standardized ARIC criteria.16
Incident CHD was defined as confirmed CHD death, and fatal and nonfatal myocardial infarction (MI).17 Incident IS was identified and classified as thrombotic or cardioembolic stroke based on discharge codes, signs, symptoms, neuroimaging (computerized tomography/magnetic resonance imaging), and other diagnostic reports.18 Both CHD and stroke events were validated by study physician review.
Incident HF was defined as the first occurrence of either (1) a hospitalization, which included an international classification of diseases, 9th revision, discharge code of 428 (428.0 to 428.9) in any position, or (2) a death certificate with a 428 (HF) or ICD-10 code I50 (HF) in any position and was only adjudicated by physician review after 2005.19
Incident VTE was defined as pulmonary embolisms (PE) or deep vein thromboses (DVT) occurring in the leg and was identified using diagnosis codes, hospital records, physician and consultant reports, and discharge summaries and was validated by LITE study physician review according to LITE study protocol.20
Statistical analysis
Participant characteristics at the time of the D-ARIC ancillary study (visit 4) were calculated stratified by ET status. Each CVD outcome of interest was analyzed separately using cox-proportional hazards regression models to estimate hazard ratios and 95% confidence intervals between ET categories. No prior root canal treatment was the referent group. The proportional hazards assumption was assessed by visual inspection of the Kaplan–Meier (KM) survival curves and by testing the interaction between root canal treatment status and follow-up time.
Crude (unadjusted) models and those adjusting for potential confounding variables were conducted. Confounders were selected based on being independent predictors of CVD and ET and not on the potential causal pathway between ET and CVD. Further, covariates considered in the analyses were sociodemographic, dental, and medical variables that were identified as confounders in previous ARIC dental studies addressing associations between oral infections and CVD5,13,21 and variables reflective of dental care use or caries history based on the approach used by Caplan et al.5 Adjusted models were constructed with increasing level of confounder adjustment based on confounding categories outlined below. Model 1 included adjustment for demographic and SES variables including age, sex, race/center, education, and income. Model 2 added adjustment for relevant CVD risk factors that may also be association with oral infection risk including smoking, alcohol consumption, BMI, statin use, diabetes, hypertension, LDL, HDL, and triglycerides. Hypertension, diabetes, LDL, HDL, and triglycerides were not included as covariates in the VTE analysis due to the lack of an independent association between these factors and VTE.22 Finally, model 3 additionally included adjustment for family history of premature CHD, physical activity, diet quality, and variables related to access to care and dental care use including medical insurance status, last dentist visit, dental visit frequency, having a current dentist, and reported tooth loss due to gum disease.
We conducted analyses stratified by the median number of teeth23 similar to the approach used by Caplan et al.5 This allowed us to evaluate the potential impact of ET among those with 25 or more teeth who may have had access to care and received root canal treatment when needed. We further conducted stratified analyses by gender and median age at event to see if the ET-CVD relationship differed between genders or different age groups. For all analyses, follow-up time began at entry into the study (visit 4) when ET status was assessed and outcomes accrued continually from baseline until the first incident event, loss to follow-up, death, or else, December 31, 2013 for CHD, IS, and HF and December 31, 2011 for VTE.
Results
Baseline (ARIC visit 4) characteristics of the 6,528 participants in the study sample are provided in Table 1, stratified by self-reported ET status. Of the sample, 50.5% reported no ET, 21.0% 1 ET, and 28.5% ≥2 treatments. In general, ET was more common among whites compared to blacks and among those of high SES status compared to those of low SES. Those with past ET were less likely to be smokers and have diabetes compared to those without a history of ET. Finally, those with past ET were more likely to have medical insurance, a current dentist, and visit the dentist regularly.
Table 1.
Visit 4 (1996–1998) Characteristics of ARIC Participants by Endodontic Treatment Status
| Endodontic treatment |
|||
|---|---|---|---|
| None | 1 Treatment | ≥ 2 Treatments | |
| Total, count (%) | 3,299 (50.5) | 1,371 (21.0) | 1,858 (28.5) |
| Age (years), mean ± SD | 62.3 (5.7) | 62.7 (5.7) | 62.3 (5.4) |
| Male sex, count (%) | 1,507 (45.7) | 590 (43.0) | 869 (46.8) |
| White race, count (%) | 2,385 (72.3) | 1,208 (88.1) | 1,701 (91.6) |
| Education, count (%) | |||
| Some high school | 639 (19.4) | 119 (8.7) | 119 (6.4) |
| High school diploma | 1,425 (43.3) | 597 (43.5) | 790 (42.6) |
| Bachelor’s or graduate degree | 1,229 (37.3) | 656 (47.8) | 946 (51.0) |
| Income >$35,000 | 1,588 (50.5) | 844 (63.5) | 1,210 (66.7) |
| Smoker, count (%) | |||
| Current | 442 (13.5) | 151 (11.0) | 226 (12.2) |
| Former | 1,327 (40.4) | 597 (43.5) | 911 (49.1) |
| Never | 1,513 (46.1) | 655 (47.8) | 717 (38.7) |
| Diabetes mellitus, count (%) | 522 (15.9) | 155 (11.4) | 217 (11.7) |
| Hypertension, count (%) | 1,231 (37.5) | 448 (32.8) | 576 (31.1) |
| LDL (mg/dL), mean ± SD | 3.2 (0.9) | 3.2 (0.8) | 3.1 (0.8) |
| HDL (mg/dL), mean ± SD | 1.3 (0.4) | 1.3 (0.5) | 1.3 (0.4) |
| Triglycerides (mg/dL), mean ± SD | 1.6 (0.9) | 1.6 (0.9) | 1.7 (1.0) |
| Statin use, count (%) | 321 (9.8) | 142 (10.4) | 214 (11.5) |
| BMI (Kg/M2), mean ± SD | 28.9 (5.7) | 28.1 (4.9) | 28.5 (5.1) |
| Physical activity | |||
| Ideal | 1,096 (34.5) | 348 (26.0) | 526 (28.8) |
| Intermediate | 755 (23.7) | 702 (53.5) | 451 (24.7) |
| Poor | 1,329 (41.8) | 673 (50.2) | 849 (46.5) |
| Diet | |||
| Ideal | 1,326 (42.9) | 584 (44.5) | 741 (41.2) |
| Intermediate | 1,712 (55.4) | 702 (53.5) | 1,000 (55.7) |
| Poor | 52 (1.7) | 27 (2.1) | 56 (3.1) |
| Family history of premature CHD | 253 (9.1) | 122 (10.1) | 164 (10.1) |
| Alcohol consumers, count (%) | 1,614 (49.2) | 782 (57.2) | 1,131 (60.9) |
| Alcohol (g/week), mean ± SD | 31.5 (74.8) | 38.0 (77.4) | 38.7 (83.4) |
| Care payment, count (%) | |||
| Health plan | 2,793 (85.0) | 1,285 (93.9) | 1,747 (94.1) |
| Medicare/medicaid only | 262 (7.9) | 50 (3.7) | 57 (3.1) |
| None | 230 (7.0) | 33 (2.4) | 52 (2.8) |
| Have current dentist, count (%) | 2,746 (83.3) | 1,304 (95.3) | 1,776 (95.7) |
| Last dental visit, count (%) | |||
| Within last 6 months | 1,770 (53.8) | 946 (69.1) | 1,353 (72.9) |
| 6 months to 2 years ago | 803 (24.4) | 326 (23.8) | 402 (21.7) |
| 2 to 5 years ago | 389 (11.8) | 68 (5.0) | 77 (4.2) |
| More than 5 years ago | 330 (10.0) | 30 (2.2) | 25 (1.4) |
| Dental visit, count (%) | |||
| Regular basis | 2,079 (63.0) | 1,138 (83.0) | 1,560 (84.5) |
| Discomfort/something fixed | 1,102 (33.4) | 225 (16.4) | 280 (15.2) |
| Do not go to dentist | 73 (2.2) | 1 (0.1) | 6 (0.3) |
| Periodontal tooth loss, count (%) | 318 (9.8) | 126 (9.3) | 156 (8.6) |
Over a median of 15.8 years of follow-up, 506 incident CHD events, 311 IS events, and 739 HF events were identified in the ARIC cohort at risk. A median of 14.0 years of follow-up yielded 219 VTE events. Overall incidence rates for CHD, IS, HF, and VTE were 5.6, 3.3, 8.3, and 2.6 per 1,000 person-years of follow-up, respectively. Incidence rates by ET status are found for each outcome of interest in Figure 1.
Figure 1.
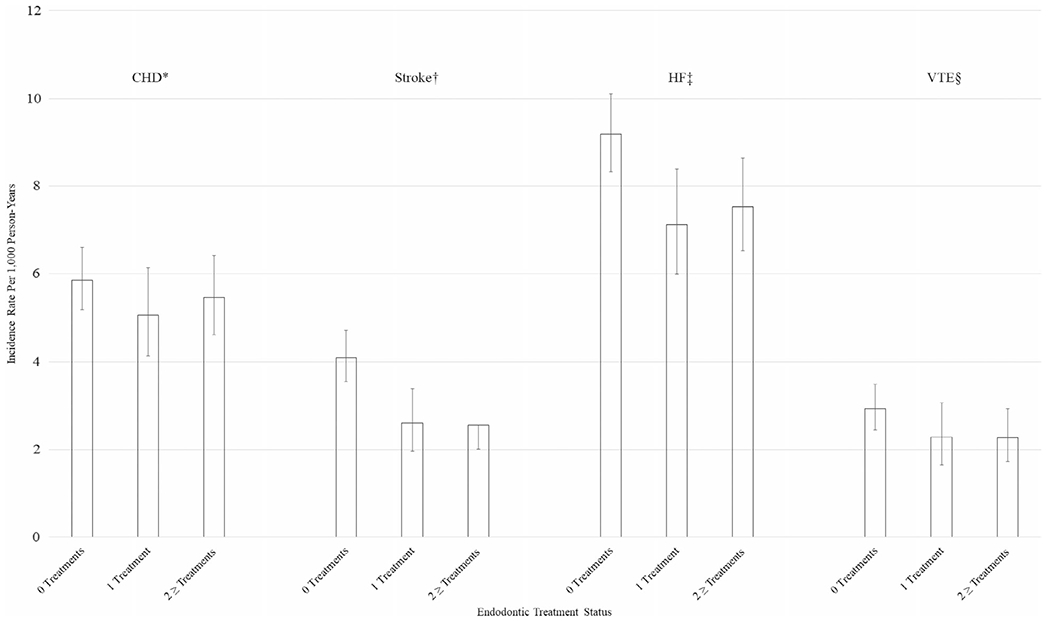
Incidence rates of cardiovascular outcomes per 1,000 person-years of follow-up by endodontic treatment status: the ARIC study, 1996–98 to 2013. *Coronary Heart Disease. †Ischemic Stroke. ‡Heart Failure. §Venous Thromboembolism.
The proportional hazards assumption was assessed by visual inspection of the Kaplan–Meier (KM) plots and by testing the interaction between ET status and follow-up time. The KM curves revealed no significant departures from proportionality. Further, no significant interactions between ET status and follow-up time were observed (all p-values >0.05).
Table 2 contains the results of the cox proportional hazards regression models for ET and CHD. Both crude and adjusted models with all study participants showed no statistically significant associations between ET and CHD risk. Similarly, among those with more than 24 teeth, no statistically significant associations were observed between those with a single ET (HR = 1.15 (0.77, 1.74)) or multiple ETs (HR = 0.95 (0.64, 1.42)) and CHD risk after adjustment for confounding (Model 3).
Table 2.
Association (Hazard Ratio and 95% Confidence Interval) Between Self-Reported Endodontic Treatment and Incident Coronary Heart Disease, Overall and Stratified by the Median Number of Teeth: The ARIC Study, 1996–1998 to 2013
| Variable | Events | N | Crude model | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|---|---|
| Endodontic treatment | ||||||
| No ET | 265 | 3,160 | Ref | Ref | Ref | Ref |
| 1 ET | 99 | 1,333 | 0.86 (0.68, 1.09) | 0.96 (0.76, 1.22) | 1.06 (0.83, 1.35) | 1.14 (0.87, 1.50) |
| ≥ 2 ET | 142 | 1,781 | 0.93 (0.76, 1.14) | 1.03 (0.83, 1.28) | 1.09 (0.87, 1.37) | 1.16 (0.87, 1.44) |
| No ET and ≥ 25 Teeth | 90 | 1,455 | Ref | Ref | Ref | Ref |
| 1 ET and ≥ 25 Teeth | 43 | 723 | 0.96 (0.67, 1.38) | 1.02 (0.71, 1.48) | 1.12 (0.77, 1.64) | 1.15 (0.77, 1.74) |
| ≥ 2 ET and ≥ 25 Teeth | 57 | 890 | 1.02 (0.73, 1.42) | 1.08 (0.77, 1.53) | 1.09 (0.76, 1.56) | 0.95 (0.64, 1.42) |
| No ET and ≤ 24 Teeth | 175 | 1,705 | Ref | Ref | Ref | Ref |
| 1 ET and ≤ 24 Teeth | 56 | 610 | 0.85 (0.63, 1.15) | 0.87 (0.63, 1.19) | 0.95 (0.69, 1.32) | 1.07 (0.74, 1.56) |
| ≥ 2 ET and ≤ 24 Teeth | 85 | 891 | 0.91 (0.70, 1.18) | 0.90 (0.67, 1.20) | 1.01 (0.75, 1.36) | 1.18 (0.84, 1.67) |
| No ET and Age ≥ 77 | Ref | |||||
| 1 ET and Age ≥ 77 | 1.09 (0.70, 1.71) | |||||
| ≥ 2 ET and Age ≥ 77 | 0.84 (0.53, 1.33) | |||||
| No ET and Age < 77 | Ref | |||||
| 1 ET and Age < 77 | 1.25 (0.89, 1.77) | |||||
| ≥ 2 ET and Age < 77 | 1.30 (0.86, 1.78) | |||||
| Age (in Years) | - | - | - | 1.08 (1.06, 1.09) | 1.08 (1.06, 1.10) | 1.08 (1.06, 1.10) |
| Sex (Males) | - | - | - | 2.14 (1.77, 2.57) | 2.04 (1.62, 2.57) | 2.07 (1.59, 2.70) |
| Race/study center | ||||||
| Whites, Minnesota | - | - | - | Ref | Ref | Ref |
| Whites, Maryland | - | - | - | 1.14 (0.89, 1.46) | 1.11 (0.86, 1.44) | 1.07 (0.81, 1.42) |
| Whites, North Carolina | - | - | - | 1.25 (0.98, 1.60) | 1.29 (1.00, 1.91) | 1.22 (0.92, 1.62) |
| Blacks, North Carolina | - | - | - | 1.13 (0.57, 2.23) | 1.04 (0.52, 2.08) | 1.13 (0.48, 2.66) |
| Blacks, Mississippi | - | - | - | 1.49 (1.11, 2.00) | 1.38 (1.00, 1.91) | 1.28 (0.83, 1.96) |
| Education | ||||||
| Some high school | - | - | - | Ref | Ref | Ref |
| High school diploma | - | - | - | 0.84 (0.65, 1.10) | 0.86 (0.66, 1.13) | 1.00 (0.72, 1.37) |
| Bachelor’s or graduate degree | - | - | - | 0.71 (0.54, 0.94) | 0.74 (0.56, 0.99) | 0.85 (0.61, 1.21) |
| Income (>$35,000) | - | - | - | 0.91 (0.74, 1.12) | 0.98 (0.79, 1.21) | 1.02 (0.80, 1.30) |
| Smoking | ||||||
| Never | - | - | - | - | Ref | Ref |
| Former | - | - | - | - | 2.11 (1.56, 2.46) | 1.24 (0.98, 1.58) |
| Current | - | - | - | - | 1.28 (1.03, 1.59) | 1.79 (1.29, 2.49) |
| Diabetes | - | - | - | - | 1.96 (1.56, 2.46) | 1.77 (1.36, 2.31) |
| Alcohol consumers | - | - | - | - | 0.98 (0.79, 1.22) | 0.98 (0.77, 1.25) |
| Alcohol (g/week) | - | - | - | - | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) |
| BMI (Kg/M2) | - | - | - | - | 1.00 (0.98, 1.02) | 1.01 (0.98, 1.03) |
| Hypertension | 1.45 (1.19, 1.77) | 1.41 (1.13, 1.76) | ||||
| LDL (mg/dL) | - | - | - | - | 1.34 (1.21, 1.50) | 1.31 (1.16, 1.49) |
| HDL (mg/dL) | - | - | - | - | 0.88 (0.64, 1.21) | 0.93 (0.65, 1.34) |
| Triglycerides (mg/dL) | - | - | - | - | 1.18 (1.04, 1.35) | 1.22 (1.05, 1.41) |
| Statin use | - | - | - | - | 1.20 (0.89, 1.61) | 1.11 (0.79, 1.55) |
| Physical activity | ||||||
| Poor | - | - | - | - | - | Ref |
| Intermediate | - | - | - | - | - | 1.13 (0.87, 1.48) |
| Ideal | - | - | - | - | - | 1.09 (0.85, 1.41) |
| Diet | ||||||
| Poor | - | - | - | - | - | Ref |
| Intermediate | - | - | - | - | - | 0.99 (0.46, 2.12) |
| Ideal | - | - | - | - | - | 1.30 (0.61, 2.77) |
| Family history of CHD versus not | 1.20 (0.86, 1.67) | |||||
| Medical care | ||||||
| Health plan | - | - | - | - | - | Ref |
| Medicare/medicaid only | - | - | - | - | - | 0.95 (0.60, 1.49) |
| None | - | - | - | - | - | 1.63 (1.01, 2.66) |
| Last dental visit | ||||||
| Within last 6 months | - | - | - | - | - | Ref |
| 6 months to 2 years ago | - | - | - | - | - | 0.97 (0.74, 1.27) |
| 2 to 5 years ago | - | - | - | - | - | 1.08 (0.67, 1.73) |
| More than 5 years ago | - | - | - | - | - | 1.39 (0.78, 2.47) |
| Dental visit | ||||||
| Regular basis | - | - | - | - | - | Ref |
| Discomfort/something fixed | - | - | - | - | - | 0.99 (0.71, 1.39) |
| Do not go to dentist | - | - | - | - | - | 1.06 (0.35, 3.25) |
| Have current dentist | - | - | - | - | - | 1.19 (0.76, 1.87) |
| Periodontal tooth loss | - | - | - | - | - | 1.19 (0.85, 1.65) |
Model 1 included age, sex, race/center, education, and income. Model 2 added smoking, diabetes, alcohol consumption, BMI, hypertension, LDL, HDL, triglycerides, statin use. Model 3 added family history of premature CHD, physical activity, diet quality, usual medical care payment mechanism, last dental visit, dental visit frequency, having a current dentist, and periodontal tooth loss.
IS results are found in Table 3. Crude models from the combined analysis showed lower stroke risk among both those with a single ET and those with multiple ETs that was attenuated with adjustment for confounders and was no longer significant. In the stratified analysis, among those with 25 teeth or more, no significant associations between single ET (HR = 1.12 (0.64, 1.98)) and multiple ETs (HR = 0.92 (0.53, 1.60)) and IS were observed in the fully adjusted model (Model 3).
Table 3.
Association (Hazard Ratio and 95% Confidence Interval) Between Self-Reported Endodontic Treatment and Incident Ischemic Stroke, Overall, and Stratified by the Median Number of Teeth: The ARIC Study, 1996–1998 to 2013
| Variable | Events | N | Crude model | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|---|---|
| Endodontic treatment | ||||||
| No ET | 190 | 3,224 | Ref | Ref | Ref | Ref |
| 1 ET | 52 | 1,347 | 0.63 (0.47, 0.86) | 0.77 (0.56, 1.06) | 0.79 (0.57, 1.10) | 0.72 (0.49, 1.05) |
| ≥ 2 ET | 69 | 1,826 | 0.62 (0.47, 0.82) | 0.79 (0.59, 1.06) | 0.83 (0.62, 1.12) | 0.77 (0.55, 1.09) |
| No ET and ≥ 25 Teeth | 59 | 1,465 | Ref | Ref | Ref | Ref |
| 1 ET and ≥ 25 Teeth | 23 | 728 | 0.78 (0.48, 1.26) | 0.88 (0.54, 1.44) | 0.96 (0.58, 1.60) | 1.12 (0.64, 1.98) |
| ≥ 2 ET and ≥ 25 Teeth | 28 | 912 | 0.75 (0.48, 1.17) | 0.84 (0.53, 1.34) | 0.86 (0.53, 1.39) | 0.92 (0.53, 1.60) |
| No ET and ≤ 24 Teeth | 131 | 1,759 | Ref | Ref | Ref | Ref |
| 1 ET and ≤ 24 Teeth | 29 | 619 | 0.60 (0.40, 0.89) | 0.68 (0.45, 1.05) | 0.69 (0.44, 1.06) | 0.53 (0.31, 0.89) |
| ≥2 ET and ≤ 24 Teeth | 41 | 914 | 0.58 (0.41, 0.83) | 0.70 (0.48, 1.04) | 0.76 (0.51, 1.13) | 0.66 (0.42, 1.04) |
| No ET and Age ≥ 77 | Ref | |||||
| 1 ET and Age ≥ 77 | 0.65 (0.35, 1.21) | |||||
| ≥2 ET and Age ≥ 77 | 0.76(0.44, 1.32) | |||||
| No ET and Age < 77 | Ref | |||||
| 1 ET and Age < 77 | 0.71 (0.44, 1.16) | |||||
| ≥2 ET and Age < 77 | 0.77 (0.49, 1.21) | |||||
| Age (in Years) | - | - | - | 1.10 (1.07, 1.12) | 1.09 (1.07, 1.12) | 1.10 (1.07, 1.13) |
| Sex (Males) | - | - | - | 1.48 (1.17, 1.87) | 1.49 (1.12, 1.99) | 1.52 (1.08, 2.14) |
| Race/study center | ||||||
| Whites, Minnesota | - | - | - | Ref | Ref | Ref |
| Whites, Maryland | - | - | - | 0.79 (0.57, 1.09) | 0.74 (0.53, 1.04) | 0.67 (0.46, 0.98) |
| Whites, North Carolina | - | - | - | 0.84 (0.60, 1.16) | 0.83 (0.59, 1.17) | 0.76 (0.51, 1.12) |
| Blacks, North Carolina | - | - | - | 0.47 (0.15, 1.51) | 0.28 (0.07, 1.17) | 0.22 (0.03, 1.58) |
| Blacks, Mississippi | - | - | - | 1.50 (1.06, 2.13) | 1.36 (0.92, 1.99) | 1.42 (0.85, 2.35) |
| Education | ||||||
| Some high school | - | - | - | Ref | Ref | Ref |
| High school diploma | - | - | - | 0.72 (0.52, 0.99) | 0.73 (0.53, 1.01) | 0.57 (0.39, 0.82) |
| Bachelor’s or graduate degree | - | - | - | 0.71 (0.51, 1.00) | 0.73 (0.52, 1.04) | 0.54 (0.36, 0.81) |
| Income (>$35,000) | - | - | - | 0.69 (0.53, 0.90) | 0.75 (0.57, 0.99) | 0.84 (0.61, 1.16) |
| Smoking | ||||||
| Never | - | - | - | - | Ref | Ref |
| Former | - | - | - | - | 0.88 (0.67, 1.15) | 0.91 (0.67, 1.23) |
| Current | - | - | - | - | 1.25 (0.86, 1.83) | 1.29 (0.83, 2.02) |
| Diabetes | - | - | - | - | 2.09 (1.58, 2.78) | 2.24 (1.61, 3.10) |
| Alcohol consumers | - | - | - | - | 0.86 (0.64, 1.14) | 0.79 (0.57, 1.09) |
| Alcohol (g/week) | - | - | - | - | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) |
| BMI (Kg/M2) | - | - | - | - | 1.00 (0.98, 1.03) | 1.00 (0.97, 1.03) |
| Hypertension | 1.48 (1.15, 1.90) | 1.42 (1.06, 1.90) | ||||
| LDL (mg/dL) | - | - | - | - | 1.10 (0.96, 1.27) | 1.12 (0.93, 1.32) |
| HDL (mg/dL) | - | - | - | - | 0.88 (0.60, 1.30) | 0.83 (0.53, 1.31) |
| Triglycerides (mg/dL) | - | - | - | - | 1.18 (1.01, 1.39) | 1.22 (1.02, 1.47) |
| Statin Use | - | - | - | - | 1.22 (0.86, 1.73) | 1.12 (0.75, 1.67) |
| Physical activity | ||||||
| Poor | - | - | - | - | - | Ref |
| Intermediate | - | - | - | - | - | 1.08 (0.77, 1.52) |
| Ideal | - | - | - | - | - | 1.08 (0.77, 1.51) |
| Diet | ||||||
| Poor | - | - | - | - | - | Ref |
| Intermediate | - | - | - | - | - | 0.94 (0.41, 2.14) |
| Ideal | - | - | - | - | - | 0.78 (0.34, 1.80) |
| Family history of CHD versus not | - | - | - | - | - | 0.71 (0.42, 1.20) |
| Medical care | ||||||
| Health plan | - | - | - | - | - | Ref |
| Medicare/medicaid only | - | - | - | - | - | 0.77 (0.45, 1.33) |
| None | - | - | - | - | - | 0.83 (0.41, 1.70) |
| Last dental visit | ||||||
| Within last 6 months | - | - | - | - | - | Ref |
| 6 months to 2 years ago | - | - | - | - | - | 1.11 (0.79, 1.54) |
| 2 to 5 years ago | - | - | - | - | - | 0.98 (0.54, 1.75) |
| More than 5 years ago | - | - | - | - | - | 0.91 (0.43, 1.91) |
| Dental visit | ||||||
| Regular basis | - | - | - | - | - | Ref |
| Discomfort/something fixed | - | - | - | - | - | 1.34 (0.89, 2.00) |
| Do not go to dentist | - | - | - | - | - | 3.42 (1.02, 11.43) |
| Have current dentist | - | - | - | - | - | 1.83 (1.03, 3.23) |
| Periodontal tooth loss | - | - | - | - | - | 0.87 (0.55, 1.38) |
Model 1 included age, sex, race/center, education, and income. Model 2 added smoking, diabetes, alcohol consumption, BMI, hypertension, LDL, HDL, triglycerides, statin use. Model 3 added family history of premature CHD, physical activity, diet quality, usual medical care payment mechanism, last dental visit, dental visit frequency, having a current dentist, and periodontal tooth loss.
Table 4 contains the results of the Cox proportional hazards regression models for ET and HF. The crude models from the unstratified analysis showed ET was associated with lower HF risk that was attenuated with adjustment for confounders and was no longer statistically significant. Among those with 25 teeth or more, Model 3 showed no significant associations between ET and HF for both single ET (HR = 0.87 (0.61, 1.24)) and multiple ETs (HR = 0.75 (0.53, 1.07)).
Table 4.
Association (Hazard Ratio and 95% Confidence Interval) Between Self-Reported Endodontic Treatment and Incident Heart Failure, Overall and Stratified by the Median Number of Teeth: The ARIC Study, 1996–1998 to 2013
| Variable | Events | N | Crude model | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|---|---|
| Endodontic treatment | ||||||
| No ET | 408 | 3,116 | Ref | Ref | Ref | Ref |
| 1 ET | 136 | 1,309 | 0.77 (0.63, 0.93) | 0.88 (0.72, 1.08) | 0.92 (0.75, 1.14) | 1.00 (0.80, 1.26) |
| ≥ 2 ET | 195 | 1,771 | 0.81 (0.69, 0.96) | 0.97 (0.81, 1.17) | 0.95 (0.79, 1.15) | 1.00 (0.81, 1.24) |
| No ET and ≥ 25 Teeth | 145 | 1,441 | Ref | Ref | Ref | Ref |
| 1 ET and ≥ 25 Teeth | 54 | 712 | 0.75 (0.55, 1.03) | 0.82 (0.59, 1.13) | 0.83 (0.60, 1.15) | 0.87 (0.61, 1.24) |
| ≥ 2 ET and ≥ 25 Teeth | 67 | 884 | 0.73 (0.55, 0.97) | 0.80 (0.59, 1.09) | 0.77 (0.57, 1.06) | 0.75 (0.53, 1.07) |
| No ET and ≤ 24 Teeth | 263 | 1,675 | Ref | Ref | Ref | Ref |
| 1 ET and ≤ 24 Teeth | 82 | 597 | 0.83 (0.65, 1.06) | 0.92 (0.71, 1.19) | 0.96 (0.73, 1.26) | 1.08 (0.79, 1.47) |
| ≥ 2 ET and ≤ 24 Teeth | 128 | 887 | 0.89 (0.72, 1.10) | 1.04 (0.82, 1.31) | 1.06 (0.83, 1.36) | 1.19 (0.90, 1.57) |
| No ET and Age ≥ 77 | Ref | |||||
| 1 ET and Age ≥ 77 | 1.02 (0.73, 1.44) | |||||
| ≥2 ET and Age ≥ 77 | 0.96 (0.69, 1.34) | |||||
| No ET and Age < 77 | Ref | |||||
| 1 ET and Age < 77 | 1.10 (0.80, 1.52) | |||||
| ≥2 ET and Age < 77 | 1.13 (0.84, 1.50) | |||||
| Age (in Years) | 1.09 (1.08, 1.11) | 1.10 (1.09, 1.12) | 1.12 (1.10, 1.14) | |||
| Sex (Males) | - | - | - | 1.44 (1.24, 1.67) | 1.32 (1.09, 1.60) | 1.33 (1.07, 1.66) |
| Race/study center | ||||||
| Whites, Minnesota | - | - | - | Ref | Ref | Ref |
| Whites, Maryland | - | - | - | 1.24 (1.00, 1.52) | 1.14 (0.92, 1.42) | 1.15 (0.90, 1.45) |
| Whites, North Carolina | - | - | - | 1.15 (0.93, 1.42) | 1.17 (0.93, 1.46) | 1.18 (0.92, 1.50) |
| Blacks, North Carolina | - | - | - | 1.41 (0.84, 2.37) | 1.11 (0.64, 1.91) | 1.00 (0.51, 1.96) |
| Blacks, Mississippi | - | - | - | 1.71 (1.35, 2.17) | 1.42 (1.09, 1.84) | 1.38 (0.98, 1.94) |
| Education | ||||||
| Some high school | - | - | - | Ref | Ref | Ref |
| High school diploma | - | - | - | 0.80 (0.65, 0.99) | 0.86 (0.69, 1.07) | 0.93 (0.72, 1.20) |
| Bachelor’s or graduate degree | - | - | - | 0.75 (0.60, 0.94) | 0.81 (0.64, 1.03) | 0.89 (0.67, 1.17) |
| Income (>$35,000) | - | - | - | 0.75 (0.63, 0.89) | 0.82 (0.68, 0.98) | 0.86 (0.71, 1.05) |
| Smoking | ||||||
| Never | - | - | - | - | Ref | Ref |
| Former | - | - | - | - | 1.44 (1.20, 1.72) | 1.56 (1.27, 1.91) |
| Current | - | - | - | - | 2.43 (1.92, 3.07) | 2.44 (1.85, 3.21) |
| Diabetes | - | - | - | - | 1.99 (1.65, 2.39) | 1.75 (1.41, 2.17) |
| Alcohol consumers | - | - | - | - | 0.99 (0.82, 1.19) | 0.95 (0.77, 1.16) |
| Alcohol (g/week) | - | - | - | - | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) |
| BMI (Kg/M2) | - | - | - | - | 1.04 (1.03, 1.06) | 1.04 (1.02, 1.06) |
| Hypertension | - | - | - | - | 1.52 (1.29, 1.79) | 1.63 (1.36, 1.96) |
| LDL (mg/dL) | - | - | - | - | 0.93 (0.85, 1.02) | 0.95 (0.85, 1.06) |
| HDL (mg/dL) | - | - | - | - | 0.99 (0.77, 1.28) | 0.99 (0.75, 1.32) |
| Triglycerides (mg/dL) | - | - | - | - | 1.07 (0.96, 1.19) | 1.06 (0.93, 1.20) |
| Statin use | - | - | - | - | 1.37 (1.10, 1.70) | 1.27 (0.99, 1.63) |
| Physical activity | ||||||
| Poor | Ref | |||||
| Intermediate | 0.87 (0.69, 1.09) | |||||
| Ideal | 1.01 (0.82, 1.25) | |||||
| Diet | ||||||
| Poor | Ref | |||||
| Intermediate | 1.19 (0.65, 2.19) | |||||
| Ideal | 1.17 (0.63, 2.15) | |||||
| Family history of CHD versus not | 0.94 (0.69, 1.27) | |||||
| Medical care | ||||||
| Health plan | - | - | - | - | - | Ref |
| Medicare/medicaid only | - | - | - | - | - | 0.83 (0.57, 1.20) |
| None | - | - | - | - | - | 1.57 (1.04, 2.36) |
| Last dental visit | ||||||
| Within last 6 months | - | - | - | - | - | Ref |
| 6 months to 2 years ago | - | - | - | - | - | 1.01 (0.81, 1.25) |
| 2 to 5 years ago | - | - | - | - | - | 1.27 (0.88, 1.82) |
| More than 5 years ago | - | - | - | - | - | 0.92 (0.57, 1.50) |
| Dental visit | ||||||
| Regular basis | - | - | - | - | - | Ref |
| Discomfort/something fixed | - | - | - | - | - | 1.18 (0.90, 1.55) |
| Do not go to dentist | - | - | - | - | - | 1.07 (0.40, 2.85) |
| Have current dentist | - | - | - | - | - | 1.10 (0.77, 1.57) |
| Periodontal tooth loss | - | - | - | - | - | 1.03 (0.78, 1.36) |
Model 1 included age, sex, race/center, education, and income. Model 2 added smoking, diabetes, alcohol consumption, BMI, hypertension, LDL, HDL, triglycerides, statin use. Model 3 added family history of premature CHD, physical activity, diet quality, usual medical care payment mechanism, last dental visit, dental visit frequency, having a current dentist, and periodontal tooth loss.
Table 5 contains the Cox proportional hazards regression model results for ET and VTE. Both crude and adjusted models with all study participants showed no statistically significant associations between ET and risk. The stratified analysis showed no significant increase in VTE risk among those with >25 teeth for both single ET (HR = 0.87 (0.48, 1.58)) or multiple ETs (HR = 1.09 (0.64, 1.85)) after adjustment for confounding (Model 3).
Table 5.
Association (Hazard Ratio and 95% Confidence Interval) Between Self-Reported Endodontic Treatment and Incident Venous Thromboembolism, Overall and Stratified by the Median Number of Teeth: The ARIC Study, 1996–1998 to 2011
| Variable | Events | N | Crude model | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|---|---|
| Endodontic treatment | ||||||
| No ET | 123 | 3,229 | Ref | Ref | Ref | Ref |
| 1 ET | 41 | 1,347 | 0.77 (0.54, 1.10) | 0.85 (0.59, 1.24) | 0.87 (0.60, 1.25) | 0.86 (0.57, 1.31) |
| ≥ 2 ET | 55 | 1,824 | 0.77 (0.56, 1.06) | 0.90 (0.64, 1.26) | 0.90 (0.64, 1.27) | 0.98 (0.67, 1.43) |
| No ET and ≥ 25 Teeth | 47 | 1,471 | Ref | Ref | Ref | Ref |
| 1 ET and ≥ 25 Teeth | 19 | 726 | 0.81 (0.48, 1.38) | 0.88 (0.51, 1.51) | 0.89 (0.52, 1.53) | 0.87 (0.48, 1.58) |
| ≥ 2 ET and ≥ 25 Teeth | 31 | 914 | 1.04 (0.66, 1.64) | 1.08 (0.67, 1.74) | 1.12 (0.67, 1.81) | 1.09 (0.64, 1.85) |
| No ET and ≤ 24 Teeth | 76 | 1,758 | Ref | Ref | Ref | Ref |
| 1 ET and ≤ 24 Teeth | 22 | 621 | 0.77 (0.48, 1.24) | 0.86 (0.51, 1.44) | 0.88 (0.53, 1.48) | 0.92 (0.51, 1.66) |
| ≥2 ET and ≤ 24 Teeth | 24 | 910 | 0.59 (0.37, 0.93) | 0.77 (0.47, 1.27) | 0.77 (0.46, 1.27) | 0.94 (0.54, 1.64) |
| No ET and Age ≥ 77 | Ref | |||||
| 1 ET and Age ≥ 77 | 0.82 (0.39, 1.73) | |||||
| ≥2 ET and Age ≥ 77 | 0.54 (0.23, 1.28) | |||||
| No ET and Age < 77 | Ref | |||||
| 1 ET and Age < 77 | 0.95 (0.57, 1.58) | |||||
| ≥2 ET and Age < 77 | 1.18 (0.77, 1.82) | |||||
| Age (in years) | - | - | - | 1.06 (1.03, 1.08) | 1.07 (1.04, 1.10) | 1.07 (1.04, 1.10) |
| Sex (male versus female) | - | - | - | 1.19 (0.90, 1.58) | 1.28 (0.95, 1.72) | 0.98 (0.70, 1.38) |
| Race/study center | ||||||
| Whites, Minnesota | - | - | - | Ref | Ref | Ref |
| Whites, Maryland | - | - | - | 1.63 (1.09, 2.44) | 1.62 (1.08, 2.44) | 1.83 (1.17, 2.87) |
| Whites, North Carolina | - | - | - | 1.61 (1.07, 2.42) | 1.73 (1.14, 2.63) | 1.68 (1.06, 2.67) |
| Blacks, North Carolina | - | - | - | 2.21 (0.93, 5.25) | 2.09 (0.87, 5.01) | 2.43 (0.91, 6.48) |
| Blacks, Mississippi | - | - | - | 2.20 (1.41, 3.45) | 1.92 (1.20, 3.06) | 1.77 (0.98, 3.21) |
| Education | ||||||
| Some high school | - | - | - | Ref | Ref | Ref |
| High school diploma | - | - | - | 0.75 (0.51, 1.11) | 0.78 (0.53, 1.16) | 0.71 (0.45, 1.13) |
| Bachelor’s or graduate degree | - | - | - | 0.89 (0.59, 1.34) | 0.95 (0.63, 1.43) | 0.91 (0.56, 1.49) |
| Income (>$35,000) | - | - | - | 0.79 (0.57, 1.08) | 0.83 (0.61, 1.15) | 0.83 (0.58, 1.19) |
| Smoking | 1.01 (0.75, 1.37) | |||||
| Never | - | - | - | - | Ref | Ref |
| Former | - | - | - | - | 1.01 (0.75, 1.37) | 1.10 (0.78, 1.56) |
| Current | - | - | - | - | 1.09 (0.68, 1.74) | 1.23 (0.73, 2.06) |
| Alcohol consumers versus not | - | - | - | - | 1.01 (0.73, 1.40) | 0.88 (0.61, 1.27) |
| Alcohol (g/week), mean ± SD | - | - | - | - | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) |
| BMI (Kg/M2), mean ± SD | - | - | - | - | 1.06 (1.04, 1.09) | 1.06 (1.03, 1.09) |
| Statin use versus not | - | - | - | - | 0.59 (0.34, 1.01) | 0.56 (0.30, 1.03) |
| Physical activity | ||||||
| Poor | - | - | - | - | - | Ref |
| Intermediate | - | - | - | - | - | 0.61 (0.40, 0.95) |
| Ideal | - | - | - | - | - | 0.82 (0.57, 1.181) |
| Diet | ||||||
| Poor | - | - | - | - | - | Ref |
| Intermediate | - | - | - | - | - | 1.75 (0.43, 7.14) |
| Ideal | - | - | - | - | - | 2.17 (0.53, 8.87) |
| Family history of CHD versus not | 0.89 (0.51, 1.54) | |||||
| Medical care | ||||||
| Health plan | - | - | - | - | - | Ref |
| Medicare/medicaid only | - | - | - | - | - | 0.73 (0.36 1.50) |
| None | - | - | - | - | - | 0.77 (0.33 1.80) |
| Last dental visit | ||||||
| Within last 6 months | - | - | - | - | - | Ref |
| 6 months to 2 years ago | - | - | - | - | - | 1.70 (1.19 2.44) |
| 2 to 5 years ago | - | - | - | - | - | 1.60 (0.84, 3.06 |
| More than 5 years ago | - | - | - | - | - | 0.84 (0.33, 2.15) |
| Dental visit | ||||||
| Regular basis | - | - | - | - | - | Ref |
| Discomfort/something fixed | - | - | - | - | - | 0.93 (0.58, 1.49) |
| Do not go to dentist | - | - | - | - | - | 0.49 (0.06, 3.90) |
| Have current dentist versus not | - | - | - | - | - | 0.84 (0.46, 1.51) |
| Periodontal tooth loss versus not | - | - | - | - | - | 1.17 (0.71, 1.93) |
Model 1 included age, sex, race/center, education, income. Model 2 added smoking, alcohol consumption, BMI, statin use. Model 3 added family history of premature CHD, physical activity, diet quality, medical care payment mechanism, last dental visit, dental visit frequency, having a current dentist, and periodontal tooth loss.
No significant interactions between ET status and gender were observed for any of the outcomes of interest (data not shown). Results stratified by median age at event (77) are presented in Tables 2–5 for each outcome of interest. No age interactions reached statistical significance (all p-values >0.05).
Discussion
In this prospective cohort study on ET and incidence of CHD, IS, HF, and VTE, there was no evidence that self-reported history of ET was associated with any of our outcomes of interest, after adjustment for confounding. This was true in the overall analyses and in analyses restricted to those with 25 or more teeth.
Previous studies of a potential association between EI/ET and CVD have found mixed results. In 2006, Joshipura et al. evaluated the association between ET and CHD among males from the health professionals follow-up study.10 Among dentists, those with ET had higher CHD risk compared to those without ET. However, they found no association among nondentists. Other previous studies have found EI/ET to be associated with greater CVD risk.6,7 Our results were similar to previous studies that failed to find an association between EI/ET and CHD.2,3
In 2009, Caplan et al. conducted a cross-sectional study using ARIC data and found that among participants with 25 or more teeth, those reporting having had ET two or more times had 1.62 times higher odds of prevalent CHD compared with those reporting never having had ET.5 There are a number of differences between their study and ours that may explain the discrepancy in the results. Our study examined the association between ET with incident CVD events longitudinally while the study by Caplan et al examined the association between ET and prevalent CVD at a single point in time. This cross-sectional study may be more prone to bias including temporal bias since it is unable to establish that ET preceded CHD. The difference in study design also required slight variation in confounding control, which may also explain the differences between the studies. It is however possible that the relationship between infection and CVD could vary based on age and background CVD risk. Caplan et al’s cross-sectional study identified ARIC participants who developed CHD at a younger age compared to our longitudinal study in which visit 4 served as baseline at which point participants had a mean age of 63 years and did not have a history of CVD. An earlier study by Caplan et al. in a different study population found that among those ≤40 years old, endodontic lesions were significantly associated with incident CHD (p < 0.05) but found no association among those >40 years old.6 Other research on infection and CVD has found that infection is a stronger CVD risk factor among those with low background CVD risk compared to those with elevated background CVD risk.24 It is possible EI was a risk factor for CVD among ARIC participants when they were young with an otherwise low background CVD risk when they were studied by Caplan et al., but not among ARIC participants when they are older with an elevated background CVD risk profile, as in the present study. However, our analyses stratified by median age at CVD event (i.e., 77 years) failed to reach statistical significance. Further research among diverse populations is needed to explain how the EI-CVD relationship varies across ages and CVD risk levels.
Our study has a number of other strengths including a large sample size from a community-based cohort with assessment of many potential confounding factors, a large number of CVD events, and rigorous methodology to adjudicate CVD events. Our study also has a number of potential limitations that could result in failing to detect a potential association between ET and CVD. Our study could be susceptible to measurement error since self-reported ET at a single point in time (visit 4) was used as a proxy for EI/AP. Successful ET may resolve the EI and resulting inflammation related to CVD risk and may explain the absence of significant findings. ET may resolve the chronic inflammatory burden associated with active EI/AP and therefore potentially mitigate elevations in CVD risk that may occur during active EI/AP. Further, ET could be performed for restorative reasons, or secondary to dental trauma, rather than for reasons related to EI/AP. Also, a lack of ET does not necessarily imply the absence of EI/AP since teeth could be extracted or remain asymptomatic. Since exposure was only assessed at a single point in time, ET that occurred during follow-up was not accounted for and could create misclassification of our exposure groups. A potential time lag between exposure and our outcomes of interest may result in non-differential misclassification, which would likely bias our results towards to null. Recall bias could also take place since historical ET may be forgotten or mistaken for other procedures.
Two studies have evaluated the validity of self-reported history of ET compared to radiographic verified ET. Pitiphat et al. found that self-reported history of root canal treatment had 90% sensitivity, 94% specificity, a positive predictive value of 86%, and a negative predictive value of 95% compared to clinical and radiograph examinations.23 A more recent study conducted by Gomes et al. found that self-reported history of ET had 92% sensitivity, 89% specificity, 82% positive predictive value, and 95% negative predictive value compared to panoramic radiographs.25 Both studies concluded that self-reported ET is a highly accurate method to predict historic ET.23,25
Those who reported never having had ET consist of two highly disparate subgroups: those who had good oral health and never needed a root canal and those who had poor oral health and needed root canals but never received them. Individuals who do not have access to dental care may not have received ET when it would be otherwise warranted. We attempted to isolate those with access to dental care by stratifying by the median number of teeth since number of teeth may serve as proxy for historical access to dental care.5 We also included predictors of dental care in our adjusted models but measurement error could persist. Residual confounding may also be present, for instance related to medication use. Likewise, factors such as sugar consumption, which is associated with both dental infections and cardiovascular disease, were not considered in the present analysis.
Conclusion
ET was not independently associated with risk of CHD, IS, HF, or VTE in this community-based study.
Acknowledgments
We thank the staff and participants of the ARIC study for their important contributions. The ARIC study was supported by National Heart, Lung, and Blood Institute (NHLBI) contracts HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C. The LITE study was funded by National Heart, Lung, and Blood Institute (NHLBI) grant R01 HL59367. The collection and analysis of dental data were supported by the National Institute of Dental and Craniofacial Research (grants DE 13807-01A1 and DE1 1551) L.T.C. was supported by an NHLBI training grant T32 HL007779.
Footnotes
CONFLICTS OF INTEREST
We have no conflicts of interest to disclose.
References
- 1.Narayanan LL, Vaishnavi C. Endodontic microbiology. J Conserv Dent. 2010;13(4):233–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frisk F, Hakeberg M, Ahlqwist M, Bengtsson C. Endodontic variables and coronary heart disease. Acta Odontol Scand. 2003;61(5):257–62. [DOI] [PubMed] [Google Scholar]
- 3.Frisk F Epidemiological aspects on apical periodontitis. Studies based on the prospective population study of women in Goteborg and the population study on Oral health in Jonkoping, Sweden. Swed Dent J Suppl. 2007;(189):11–78. [PubMed] [Google Scholar]
- 4.Liljestrand JM, Mantyla P, Paju S, Buhlin K, Kopra KA, Persson GR et al. Association of endodontic lesions with coronary artery disease. J Dent Res. 2016;95:1358–65. [DOI] [PubMed] [Google Scholar]
- 5.Caplan DJ, Pankow JS, Cai J, Offenbacher S, Beck JD. The relationship between self-reported history of endodontic therapy and coronary heart disease in the atherosclerosis risk in communities study. J Am Dent Assoc. 2009;140(8):1004–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caplan DJ, Chasen JB, Krall EA, Cai J, Kang S, Garcia RI, Offenbacher S, Beck JD. Lesions of endodontic origin and risk of coronary heart disease. J Dent Res. 2006;85(11):996–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costa TH, de Figueiredo Neto JA, de Oliveira AE, Lopes e MMF, de Almeida AL. Association between chronic apical periodontitis and coronary artery disease. J Endod. 2014;40(2):164–7. [DOI] [PubMed] [Google Scholar]
- 8.Gomes MS, Blattner TC, Sant’Ana Filho M, Grecca FS, Hugo FN, Fouad AF, Reynolds MA. Can apical periodontitis modify systemic levels of inflammatory markers? A systematic review and meta-analysis. J Endod. 2013;39(10):1205–17. [DOI] [PubMed] [Google Scholar]
- 9.Caplan DJ Epidemiologic issues in studies of association between apical periodontitis and systemic health. Endodontic Topics. 2004;8(1):15–35. [Google Scholar]
- 10.Joshipura KJ, Pitiphat W, Hung HC, Willett WC, Colditz GA, Douglass CW. Pulpal inflammation and incidence of coronary heart disease. J Endod. 2006;32(2):99–103. [DOI] [PubMed] [Google Scholar]
- 11.The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989;129(4):687–702. [PubMed] [Google Scholar]
- 12.Elter JR, Champagne CM, Offenbacher S, Beck JD. Relationship of periodontal disease and tooth loss to prevalence of coronary heart disease. J Periodontol. 2004;75(6):782–90. [DOI] [PubMed] [Google Scholar]
- 13.Beck JD, Elter JR, Heiss G, Couper D, Mauriello SM, Offenbacher S. Relationship of periodontal disease to carotid artery intima-media wall thickness: the atherosclerosis risk in communities (ARIC) study. Arterioscler Thromb Vasc Biol. 2001;21(11):1816–22. [DOI] [PubMed] [Google Scholar]
- 14.Florido R, Zhao D, Ndumele CE, Lutsey PL, McEvoy JW, Windham BG et al. Physical activity, parental history of premature coronary heart disease, and incident atherosclerotic cardiovascular disease in the atherosclerosis risk in communities (ARIC) study. J Am Heart Assoc. 2016;5(9):e003505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD et al. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57(16):1690–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.White AD, Folsom AR, Chambless LE, Sharret AR, Yang K, Conwill D, Higgins M, Williams OD, Tyroler HA, The ARIC Investigators. Community surveillance of coronary heart disease in the atherosclerosis risk in communities (ARIC) study: methods and initial two years’ experience. J Clin Epidemiol. 1996;49(2):223–33. [DOI] [PubMed] [Google Scholar]
- 17.Hardy DS, Hoelscher DM, Aragaki C, Stevens J, Steffen LM, Pankow JS, Boerwinkle E. Association of glycemic index and glycemic load with risk of incident coronary heart disease among whites and African Americans with and without type 2 diabetes: the atherosclerosis risk in communities study. Ann Epidemiol. 2010;20(8):610–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the atherosclerosis risk in communities (ARIC) cohort. Stroke. 1999;30(4):736–43. [DOI] [PubMed] [Google Scholar]
- 19.Loehr LR, Rosamond WD, Chang PP, Folsom AR, Chambless LE. Heart failure incidence and survival (from the atherosclerosis risk in communities study). Am J Cardiol. 2008;101(7):1016–22. [DOI] [PubMed] [Google Scholar]
- 20.Cushman M, Tsai AW, White RH, Heckbert SR, Rosamond WD, Enright P, Folsom AR. Deep vein thrombosis and pulmonary embolism in two cohorts: the longitudinal investigation of thromboembolism etiology. Am J Med. 2004;117(1):19–25. [DOI] [PubMed] [Google Scholar]
- 21.Elter JR, Offenbacher S, Toole JF, Beck JD. Relationship of periodontal disease and edentulism to stroke/TIA. J Dent Res. 2003;82(12):998–1001. [DOI] [PubMed] [Google Scholar]
- 22.Mahmoodi BK, Cushman M, Anne Naess I, Allison MA, Jan Bos W, Braekkan SK et al. Association of traditional cardiovascular risk factors with venous thromboembolism: an individual participant data meta-analysis of prospective studies. Circulation. 2017;135(1):7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pitiphat W, Garcia RI, Douglass CW, Joshipura KJ. Validation of self-reported oral health measures. J Public Health Dent. 2002;62(2):122–8. [DOI] [PubMed] [Google Scholar]
- 24.Cowan LT, Alonso A, Pankow JS, Folsom AR, Rosamond WD, Gottesman RF, Lakshminarayan K. Hospitalized infection as a trigger for acute ischemic stroke: the atherosclerosis risk in communities study. Stroke. 2016;47(6):1612–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gomes MS, Hugo FN, Hilgert JB, Padilha DM, Simonsick EM, Ferrucci L et al. Validity of self-reported history of endodontic treatment in the Baltimore longitudinal study of aging. J Endod. 2012;38(5):589–93. [DOI] [PMC free article] [PubMed] [Google Scholar]


