Abstract
This study comprehensively examined trends in alcohol-induced overdose mortality in the USA between 1999 and 2020 by age, sex, race/ethnicity, census region, and type of injury. Using the CDC WONDER database, 605,948 alcohol-induced deaths were recorded. Mortality increased by 14.1% per year (95% CI 8.2, 20.3) from 2018 to 2020, with the highest rates among males, non-Hispanic Whites, individuals aged 55–64, and the Western census region. Rising trends were observed across racial/ethnic subgroups, except for American Indians/Alaska Natives, with annual increases of 17% among non-Hispanic Blacks, 14.3% among non-Hispanic Whites, 9.5% among Asian/Pacific Islanders, and 12.6% among Hispanics. Males, females, all age groups, and census regions also experienced increasing trends. In conclusion, this study underscores worsening alcohol-induced mortality in the recent two decades and the need for research to identify its determinants. Such research can guide evidence-based public health interventions to reduce excessive alcohol use consequences.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11469-023-01083-1.
Keywords: Alcohol-induced mortality, Alcohol-related mortality, Trends, USA
Alcohol use, as the seventh leading risk factor for both death and disability globally in 2016, poses an undeniable threat to public health (GBD 2016 Alcohol Collaborators, 2018). In the USA, it ranks as one of the most prevalent preventable causes of death, trailing behind cigarette smoking, poor diet, and physical inactivity (Mokdad et al., 2004). Chronic alcohol abuse has been linked to a myriad of life-threatening diseases and conditions that amplify mortality risks, such as various malignancies, liver cirrhosis, gastrointestinal complications, and severe cardiovascular and neurological consequences, including stroke (Shield et al., 2013). Furthermore, the role of alcohol as a cause of death remains underreported, as alcohol-induced impairments in processing speed, motor coordination, impulse control, and judgment often lead to violence, crime, or accidents that are not reflected in mortality records (Brumback et al., 2007; Miller & Fillmore, 2014), In 2021, alcohol constituted a staggering 39.33% of all drug-related emergency visits, emerging as the most common cause (Drug Abuse Warning Network, 2021).
Despite the well-documented health risks and potential for substance dependency, alcohol consumption remains widespread in the USA. Over the past two decades, drinking patterns have evolved dramatically, with significant increases observed in women, older adults, and the socioeconomically disadvantaged populations (Grant et al., 2017; White, 2020). The COVID-19 pandemic has further intensified alcohol consumption since its declaration as a national emergency in March 2020 (National Institute on Alcohol Abuse and Alcoholism, 2020; National Institute on Drug Abuse, 2022). However, a comprehensive examination of trends in alcohol-induced mortality spanning two decades (1999–2020) had not been conducted prior to our study. Spillane et al. reported an accelerated increase in alcohol-induced death rates between 2012 and 2016, but trends across sex, age, race/ethnicity, census region, and type of injury subgroups in the US population post-2016 remained unexplored (Spillane et al., 2020).
In this study, we aimed to assess the trends in alcohol-induced mortality by age, sex, race/ethnicity, census region, and type of injury in the USA from 1999 to 2020, while accounting for other determinants of higher risk of mortality. We chose to focus on data from 1999 to 2020 because it provides a robust, two-decade-long baseline to identify trends, while 2021 and 2022 data have not yet been fully validated and may still be subject to ongoing revisions. Moreover, the lag in data collection, processing, and availability is common for nationwide mortality statistics. As alcohol use is a leading cause of premature mortality globally, our findings hold significant implications for public health in the USA and other countries experiencing similar shifts in alcohol consumption (GBD 2016 Alcohol Collaborators, 2018; Stelander et al., 2021). By shedding light on these trends, we hope to inform targeted intervention strategies aimed at reducing the devastating impact of alcohol-induced mortality.
Methods
Study Design and Data Source
We conducted a cross-sectional study using the Underlying Cause of Death files from the Centers for Disease Control and Prevention’s (Wide-ranging Online Data for Epidemiologic Research (WONDER) database, 2021) which covers the years 1999–2020. The national mortality data in WONDER is provided by the National Center for Health Statistics and is based on death certificate records for US residents.
To identify alcohol-induced deaths, we focused on instances where alcohol was listed as an underlying cause. This was determined using the following International Classification of Diseases, 10th revision (ICD-10) codes: E24.4 (alcohol-induced pseudo-Cushing syndrome), F10 (alcohol related disorders), G31.2 (degeneration of the nervous system due to alcohol), G62.1 (alcoholic polyneuropathy), G72.1 (alcoholic myopathy), I42.6 (alcoholic cardiomyopathy), K29.2 (alcoholic gastritis), K70 (alcoholic liver disease), K85.2 (alcohol-induced acute pancreatitis), K86.0 (alcohol-induced chronic pancreatitis), R78.0 (finding of alcohol in the blood), X45 (accidental poisoning by and exposure to alcohol), X65 (intentional self-poisoning by and exposure to alcohol), and Y15 (poisoning by and exposure to alcohol, undetermined intent).
We then abstracted crude and age-adjusted mortality rates (AAMR) based on factors such as type of injury (alcohol poisoning (overdose) and all other alcohol-induced causes), age groups (15–24; 25–34; 35–44; 45–54; 55–64; 65–74; 75–84; ≥ 85), sex (male; female), race/ethnicity (non-Hispanic White; non-Hispanic Black; Asian/Pacific Islander; American Indian/Alaska Native; Hispanic), and census region (Northeast; Midwest; South; West).
Since the WONDER database is de-identified and publicly available, our study was exempt from Institutional Review Board review.
Statistical Analysis
We examined the distribution of alcohol-induced mortality by type of injury and regional and sociodemographic characteristics using counts, percentages, and age-adjusted mortality rates. To assess temporal trends, we initially estimated a 5-year simple moving average (SMA) for AAMR. While SMA smooths inter-year variations in rates, it does not provide annual or average annual percentages for trends over time.
To address this limitation, we employed a joinpoint regression model. This model begins by assuming a linear trend in AAMR without joinpoints. It then includes a joinpoint, representing a change in trend, and performs a statistical test to assess the significance of the model with one joinpoint compared to the null model with no joinpoints. Additional joinpoints are incorporated using Monte Carlo permutation, and statistical tests are repeated until the optimal number of joinpoints is identified.
In the joinpoint model, we fitted the log-transformed AAMR as the dependent variable and the year of death as the independent variable. We selected “annual” for the interval type and used an uncorrelated error model suitable for constant standard error variance in the data. Default settings were applied for the grid search method, number of joinpoints (0–4), model selection method (permutation test), AAPC segment ranges (entire range), and APC confidence interval (parametric method).
Our results were reported as average annual percentage changes (AAPC) in AAMR and annual percentage changes (APC), along with their corresponding 95% confidence intervals (CIs). All statistical analyses were conducted using Stata 17.0 (College Station, Texas).
Results
A total of 605,948 alcohol-induced deaths were recorded from 1999 through 2020 (AAMR = 8.3 per 100,000; 95% CI 8.3–8.3). The largest mortality was observed among males (AAMR = 12.7; 95% CI 12.7–12.7), American Indian/Alaska Native Non-Hispanic Whites (AAMR = 38.7; 95% CI 38.1–39.2), persons aged 55 to 64 years (AAMR = 24.7; 95% CI 24.6–24.8), and decedents from the Western census region (AAMR = 12.4; 95% CI 12.3–12.4) (Table 1). A description of the characteristics of decedents in the joinpoint with a remarkable impact on mortality rates is presented in eTable 1 in the Supplement.
Table 1.
Descriptive statistics of select variables on alcohol-induced mortality, USA, 1999–2020
| Variable | n (%) | Age-adjusted mortality rate per 100,000 (95% CI) |
|---|---|---|
| Total | 605,948 (100.0) | 8.3 (8.3–8.3) |
| Sex | ||
| Male | 445,791 (73.6) | 12.7 (12.7–12.7) |
| Female | 160,157 (26.4) | 4.3 (4.3–4.3) |
| Age group (years) | ||
| 15–24 | 3241 (0.5) | 0.3 (0.3–0.4) |
| 25–34 | 23,244 (3.8) | 2.6 (2.5–2.6) |
| 35–44 | 80,124 (13.2) | 8.6 (8.5–8.6) |
| 45–54 | 180,457 (29.8) | 19.3 (19.2–19.4) |
| 55–64 | 189,178 (31.2) | 24.7 (24.6–24.8) |
| 65–74 | 91,578 (15.1) | 17.7 (17.6–17.9) |
| 75–84 | 31,399 (5.2) | 10.6 (10.5–10.7) |
| ≥ 85 | 6511 (1.1) | 5.4 (5.3–5.5) |
| aRace | ||
| Non-Hispanic White | 438,968 (72.4) | 8.4 (8.4–8.4) |
| Non-Hispanic Black | 58,428 (9.6) | 7.1 (7.1–7.2) |
| Asian/Pacific Islander | 6946 (1.1) | 2.0 (1.9–2.0) |
| American Indian/Alaska Native | 20,308 (3.4) | 38.7 (38.1–39.2) |
| Hispanic | 77,998 (12.9) | 9.7 (9.6–9.8) |
| US census region | ||
| Northeast | 83,925 (13.9) | 6.2 (6.1–6.2) |
| Midwest | 119,391 (19.7) | 7.5 (7.5–7.5) |
| South | 199,951 (33.0) | 7.4 (7.3–7.4) |
| West | 202,681 (33.4) | 12.4 (12.3–12.4) |
| Type of injury | ||
| Alcohol poisoning (overdose) | 35,182 (5.8) | 0.5 (0.5–0.5) |
| All other alcohol-induced causes | 570,766 (94.2) | 7.8 (7.8–7.8) |
aHispanics could be of any race; all other categories are non-Hispanic
Overall Mortality Trends
Between 1999 and 2020, alcohol-induced mortality overall increased by 50%, from 7.0 to 10.5 deaths per 100,000. Joinpoint analysis revealed an average annual increase of 2.9% (95% CI 2.3, 3.4) during the entire two decades of the study (Table 2). However, upon detailed examination, three distinct trends were noted: AAMR was stable from 1999 to 2007 (APC = 0.0; 95% CI − 0.6, 0.6) but increased at an annual rate of 3% (95% CI 2.6, 3.5) from 2007 to 2018. Between 2018 and 2020, the AAMR increased at an annual of 14.1% (95% CI 8.2, 20.3).
Table 2.
Annual percentage changes and average annual percentage changes in alcohol-induced mortality rates, USA, 1999–2020
| Variable | Trend segment | Segment endpoints | APC (95% CI) | Five-year simple moving average | AAPC | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Overall | 1 | 1999 | 2007 | 0.0 (− 0.6, 0.6) | 7.00, 10.50 | *2.9 (2.3, 3.4) |
| 2 | 2007 | 2018 | *3.0 (2.6, 3.5) | |||
| 3 | 2018 | 2020 | *14.1 (8.2, 20.3) | |||
| Race/ethnicity | ||||||
| Non-Hispanic White | 1 | 1999 | 2007 | *1.3 (0.8, 1.8) | 6.52, 11.30 | *3.7 (3.2, 4.2) |
| 2 | 2007 | 2018 | *3.7 (3.3, 4.1) | |||
| 3 | 2018 | 2020 | *14.3 (9.1, 19.9) | |||
| Non-Hispanic Black | 1 | 1999 | 2007 | * − 6.2 (− 7.0, − 5.3) | 8.74, 7.58 | − 0.3 (− 1.2, 0.6) |
| 2 | 2007 | 2018 | *1.2 (0.5, 1.9) | |||
| 3 | 2018 | 2020 | *17.0 (7.3, 27.5) | |||
| Asian/Pacific Islander | 1 | 1999 | 2015 | *1.1 (0.1, 2.0) | 1.60, 2.48 | *3.0 (1.6, 4.4) |
| 2 | 2015 | 2020 | *9.5 (3.6, 15.6) | |||
| American Indian/Alaska Native | 1 | 1999 | 2018 | *3.2 (2.7, 3.7) | 28.78, 52.58 | *4.5 (2.9, 6.1) |
| 2 | 2018 | 2020 | 17.9 (− 0.3, 39.3) | |||
| Hispanic | 1 | 1999 | 2004 | * − 3.8 (− 6.0, − 1.5) | 9.96, 10.62 | 0.7 (− 0.4, 1.8) |
| 2 | 2004 | 2018 | *0.7 (0.2, 1.3) | |||
| 3 | 2018 | 2020 | *12.6 (1.3, 25.1) | |||
| Sex | ||||||
| Male | 1 | 1999 | 2009 | − 0.0 (− 0.5, 0.4) | 11.22, 15.50 | *2.4 (1.8, 3.0) |
| 2 | 2009 | 2018 | *3.0 (2.4, 3.6) | |||
| 3 | 2018 | 2020 | *12.5 (6.4, 19.1) | |||
| Female | 1 | 1999 | 2007 | *1.0 (0.4, 1.5) | 3.26, 5.90 | *4.0 (3.5, 4.5) |
| 2 | 2007 | 2018 | *4.3 (3.9, 4.8) | |||
| 3 | 2018 | 2020 | *14.7 (9.1, 20.5) | |||
| Type of injury | ||||||
| Alcohol poisoning (overdose) | 1 | 1999 | 2005 | * − 2.7 (− 4.2, − 1.2) | 0.10, 0.72 | *9.6 (8.2, 11.0) |
| 2 | 2005 | 2008 | *98.9 (81.7, 117.9) | |||
| 3 | 2008 | 2020 | 0.3 (− 0.3, 0.8) | |||
| All other alcohol-induced causes | 1 | 1999 | 2009 | * − 0.4 (− 0.8, − 0.1) | 6.88, 9.76 | *2.6 (2.1, 3.0) |
| 2 | 2009 | 2018 | *3.5 (3.0, 4.0) | |||
| 3 | 2018 | 2020 | *14.4 (9.7, 19.2) | |||
| Age (years) | ||||||
| 15–24 | 1 | 1999 | 2008 | *8.3 (5.1, 11.6) | 0.24, 0.34 | 3.0 (− 0.3, 6.5) |
| 2 | 2008 | 2012 | − 9.1 (− 22.8, 7.1) | |||
| 3 | 2012 | 2020 | *3.7 (0.0, 7.5) | |||
| 25–34 | 1 | 1999 | 2005 | − 0.6 (− 3.2, 2.2) | 1.56, 4.24 | *6.4 (4.6, 8.2) |
| 2 | 2005 | 2018 | *7.2 (6.2, 8.2) | |||
| 3 | 2018 | 2020 | *24.2 (5.9, 45.8) | |||
| 35–44 | 1 | 1999 | 2011 | * − 1.4 (− 1.8, − 0.9) | 8.28, 11.20 | *2.9 (2.1, 3.8) |
| 2 | 2011 | 2018 | *4.7 (3.3, 6.1) | |||
| 3 | 2018 | 2020 | *24.9 (15.5, 35.0) | |||
| 45–54 | 1 | 1999 | 2020 | *1.8 (1.4, 2.1) | 16.8, 22.52 | *1.8 (1.4, 2.1) |
| 55–64 | 1 | 1999 | 2006 | 0.4 (− 0.3, 1.1) | 18.48, 32.7 | *3.5 (3.0, 4.1) |
| 2 | 2006 | 2018 | *4.3 (4.0, 4.7) | |||
| 3 | 2018 | 2020 | *10.3 (4.7, 16.2) | |||
| 65–74 | 1 | 1999 | 2011 | − 0.5 (− 1.0, 0.0) | 15.5, 22.32 | *2.3 (1.8, 2.7) |
| 2 | 2011 | 2020 | *6.0 (5.1, 6.9) | |||
| 75–84 | 1 | 1999 | 2002 | − 3.7 (− 7.7, 0.6) | 9.74, 12.56 | *1.3 (0.5, 2.0) |
| 2 | 2002 | 2011 | 0.5 (− 0.5, 1.4) | |||
| 3 | 2011 | 2020 | *3.8 (2.9, 4.6) | |||
| ≥ 85 | 1 | 1999 | 2002 | − 6.2 (− 12.8, 0.8) | 4.98, 6.34 | 0.8 (− 0.4, 2.1) |
| 2 | 2002 | 2013 | *1.2 (0.1, 2.4) | |||
| 3 | 2013 | 2020 | *3.5 (1.5, 5.5) | |||
| Census region | ||||||
| Northeast | 1 | 1999 | 2005 | * − 1.8 (− 2.6, − 1.1) | 5.30, 7.90 | *2.6 (2.1, 3.1) |
| 2 | 2005 | 2018 | *3.2 (2.9, 3.5) | |||
| 3 | 2018 | 2020 | *13.4 (8.2, 18.8) | |||
| Midwest | 1 | 1999 | 2007 | 0.4 (− 0.5, 1.3) | 5.78, 10.48 | *4.0 (3.1, 4.9) |
| 2 | 2007 | 2018 | *4.4 (3.7, 5.1) | |||
| 3 | 2018 | 2020 | *17.3 (8.0, 27.4) | |||
| South | 1 | 1999 | 2009 | * − 0.9 (− 1.3, − 0.4) | 6.60, 9.30 | *2.5 (1.8, 3.1) |
| 2 | 2009 | 2018 | *3.9 (3.2, 4.6) | |||
| 3 | 2018 | 2020 | *13.4 (6.8, 20.3) | |||
| West | 1 | 1999 | 2018 | *1.6 (1.4, 1.8) | 10.62, 14.56 | *2.5 (1.8, 3.2) |
| 2 | 2018 | 2020 | *11.8 (4.0, 20.2) | |||
*Significant at p < 0.05; confidence interval does not include zero
aTrends were not assessed for persons less than 15 years of age due to unstable rates from low death counts
APC annual percentage changes, AAPC average annual percentage changes
Trends by Race/Ethnicity
The 5-year SMA for non-Hispanic Whites increased by 73.3%, from 6.52 to 11.30, corresponding to an average annual increase in AAMR of 3.7% (95% CI 3.2, 4.2) from 1999 to 2020. Joinpoint analysis revealed three segments: AAMR increased by 1.3% per year (95% CI 0.8, 1.8) from 1999 to 2007; 3.7% per year (95% CI 3.3, 4.1) from 2007 to 2018; and 14.3% (95% CI 9.1, 19.9) from 2018 to 2020.
Among non-Hispanic Blacks, the SMA decreased by 13.27%, from 8.74 to 7.58 deaths per 100,000. Based on a more detailed analysis, the trend declined at an annual rate of 6.2% (95% CI − 7.0, − 5.3) from 1999 to 2007 but increased at an annual rate of 1.2% (95% CI 0.5, 1.9) from 2007 to 2018 and further increased at a yearly rate of 17.0% (95% CI 7.3, 27.5) from 2018 to 2020.
Trends among Asian/Pacific Islanders increased by 55%, from 1.60 to 2.48. There was an initial annual rate increase of 1.1% (95% CI: 0.1, 2.0) from 1999 to 2015 and a larger yearly rate increase of 9.5% (95% CI 3.6, 15.6) from 2015 to 2020. Among American Indians/Alaska Natives, mortality trends increased by 3.2% per year (95% CI 2.7, 3.7) from 1999 to 2018 and stabilized from 2018 to 2020 (APC = 17.9; 95% CI − 0.3, 39.3). SMA increased by 6.6% among Hispanics, from 9.96 to 10.62 deaths per 100,000. In a more detailed analysis, AAMR decreased by 3.8% per year (95% CI − 6.0, − 1.5) from 1999 to 2004; increased by 0.7% per year (95% CI 0.2, 1.3) from 2004 to 2018; and increased by 12.6% per year (95% CI 1.3, 25.1) from 2018 to 2020.
Trends by Sex
The SMA increased by 38.1% among males, from 11.22 to 15.50 deaths per 100,000, and by 80.9% among females, from 3.26 to 5.90 deaths per 100,000. Based on the latest joinpoint segment, recent death trends in males increased at an annual rate of 12.5% (95% CI 6.4, 19.1) from 2018 to 2020. Similarly, the latest trend in females increased at an annual rate of 14.7% (95% CI 9.1, 20.5) from 2018 to 2020 (Fig. 1).
Fig. 1.
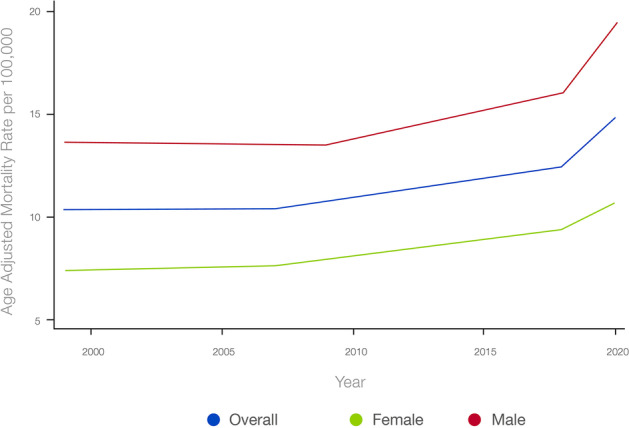
Trends by sex
Trends by Age
Recent mortality trends increased across all age groups. AAMR increased by 3.7% per year (95% CI 0.0, 7.5) among persons aged 15 to 24 years, by 24.2% per year (95% CI 5.9, 45.8) among persons aged 25 to 34 years, by 24.9% per year (95% CI 15.5, 35.0) among persons aged 35 to 44 years, by 1.8% per year (95% CI 1.4, 2.1) among persons aged 45 to 54 years, by 10.3% per year (95% CI 4.7, 16.2) among persons aged 55 to 64 years, by 6.0% per year (95% CI 5.1, 6.9) among persons aged 65 to 74 years, by 3.8% per year (2.9, 4.6) among persons aged 75 to 84 years, and by 3.5% per year (95% CI 1.5, 5.5) among persons aged at least 85 years (Table 2).
Trends by Type of Injury
Trends in alcohol-overdose deaths declined by 2.7% per year (95% CI − 4.2, − 1.2) from 1999 to 2005, increased by 98.9% per year (95% CI 81.7, 117.9) from 2005 to 2008, and stabilized from 2008 to 2020 (APC = 0.3; 95% CI − 0.3, 0.8). Trends in other alcohol-induced deaths—e.g., alcoholic gastritis—declined at an annual rate of 0.4% (95% CI − 0.8, − 0.1) from 1999 to 2009 but then increased by 3.5% per year (95% CI 3.0, 4.0) from 2009 to 2018 and by 14.4% per year (95% CI 9.7, 19.2) from 2018 to 2020.
Trends by Census Region
Recent death trends from alcohol-induced causes increased across all census regions of the USA. The latest trends increased in the Northeast at an annual rate of 13.4% (95% CI 8.2, 18.8) from 2018 to 2020. A similar finding was recorded in the Midwest, where the trends increased at an annual rate of 17.3% (95% CI 8.0, 27.4) from 2018 to 2020; the south, where the rate increased by 13.4% per year (95% CI 6.8, 20.3) from 2018 to 2020, and the West, where the rate increased by 11.8% per year (95% CI 4.0, 20.2) from 2018 to 2020 (Fig. 2).
Fig. 2.
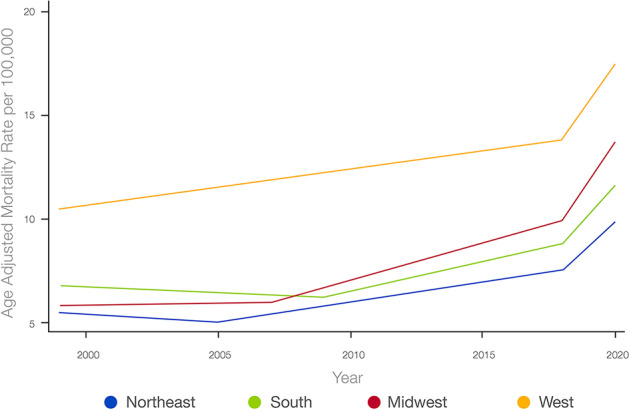
Trends by census region
Discussion
This study observed a substantial increase in alcohol-induced deaths from 1999 to 2020, with the average mortality rate rising notably among women. Consistent with earlier findings, this increase aligns with the significant growth in women’s alcohol consumption (White, 2020; White et al., 2015). The highest mortality rates occurred among males, non-Hispanic Whites, individuals aged 55–64, and residents of the US Census Bureau West Region.
From 2018 to 2020, alcohol-induced overall mortality rates sharply increased, corroborating other studies using multiple causes of death data that demonstrated a significant rise in alcohol-related deaths during this period (White et al., 2022; Yeo et al., 2022). This trend was consistent across races (highest among American Indian/Alaska Native), both genders (slightly higher in women), and all census regions (highest in the Midwest). Intriguingly, the increase was most prominent among those aged 25–34 and 35–44, with a 25% surge in annual mortality. This period coincided with a sharp rise in synthetic opioid-related deaths, primarily involving illicitly manufactured fentanyl (Centers for Disease Control and Prevention, 2022) Although the link between increased mortality rates and these opioids remains unclear, polysubstance abuse is common, making it highly probable for someone with opioid abuse problems to also use or abuse alcohol. Both alcohol and opioids are central nervous system depressants, amplifying the risk of overdose when used simultaneously.
In the context of the rapid narrowing of the alcohol consumption gap between women and men in the USA and worldwide (White, 2020), the World Health Organization (WHO) reported that women’s total alcohol per capita consumption in the USA was about a little less than one-third of men’s in 2019 (World Health Organization, 2022). Our results suggest that changes in women’s drinking behavior have led to disproportionate increases in mortality rates. Although men consistently have higher age-adjusted mortality rates in the USA, the average mortality rate increased by 80.9% among women compared to a 38.1% increase among men between 1990 and 2020 (Erol & Karpyak, 2015). This supports evidence suggesting women are more vulnerable to the harmful effects of alcohol consumption due to biological differences in alcohol metabolism.
Over the past three decades, several factors have directly impacted the chronicity and severity of alcohol consumption in the USA. Increased life expectancy and reduced fertility rates have led to an aging population, with the percentage of adults over 65 growing from 12% in 1990 to 16% in 2020 (United States Census Bureau, 2020). Alcohol’s effects on the body and central nervous system change with age, which may be due to metabolic efficiency changes and a decline in metabolic rate in older adults (Eckardt et al., 1998; Squeglia et al., 2014; Meier & Seitz, 2008; Pontzer et al., 2021). Indeed, the harmful effects of heavy drinking could increase even if the amount of drinking itself does not change, with older individuals presenting with higher blood ethanol concentrations compared to younger individuals (Jones & Neri, 1985; Lucey et al., 1999).
Additionally, exposure to alcohol advertisements has become more prevalent in the 2010s compared to the 1990s, mainly due to technological advances leading to the development of social media platforms and advancements in traditional media platforms. Although exposure to alcohol advertising among US adults shows a weak positive association with alcohol drinking behavior and total consumption (Niederdeppe et al., 2021; Wilcox et al., 2015), among youth, longitudinal studies have shown that advertising increases the likelihood of alcohol use onset and augments more drinking among those already using alcohol, particularly on social media (Anderson et al., 2009; Berey et al., 2017).
This study has limitations, including its focus on alcohol as the underlying cause of death, excluding other contributing factors. As a result, the overall death burden may be underestimated. Future studies should consider multiple causes of death involving alcohol use (Polednak, 2016). Potential misclassification bias in death certificate data cannot be ruled out, but underrecognition of alcohol use disorders would likely result in lower recorded death rates (Castle et al., 2014).
Conclusions
Trends in alcohol-induced mortality have consistently increased in recent decades, emphasizing the urgent need for further research to identify the determinants of these trends. A deeper understanding of these determinants will enable the development of evidence-based public health interventions, tailored strategies for the prevention of alcohol-induced deaths, and targeted intervention programs catering to diverse populations and risk groups. Taking into account the unique sociodemographic and regional characteristics of affected communities will ensure more effective and responsive interventions. Collaborative efforts from policymakers, healthcare providers, and community organizations are essential in implementing and promoting these strategies, ultimately contributing to a comprehensive approach to combat this pressing public health issue, reducing the burden of alcohol-induced mortality, and improving the overall well-being of society.
Supplementary Information
Below is the link to the electronic supplementary material.
Author Contribution
NM contributed to the literature review, hypothesis formulation, and the structure and sequence of theoretical arguments and theoretical consolidation of the current work and revised and edited the final manuscript.
IY contributed to the literature review, hypothesis formulation, and the structure and sequence of theoretical arguments and theoretical consolidation of the current work and revised and edited the final manuscript.
IMK contributed to the literature review, hypothesis formulation, data collection and analyses, and the structure and sequence of theoretical arguments and theoretical consolidation of the current work and revised and edited the final manuscript.
Data Availability
The data utilized in this study manuscript were obtained from the CDC WONDER (Wide-ranging Online Data for Epidemiologic Research) database. Access to the CDC WONDER database is publicly available and can be obtained from the official CDC WONDER website (https://wonder.cdc.gov/). Detailed information regarding the specific dataset used and the corresponding data parameters can be provided upon request to the authors.
Declarations
Ethical Standards—Animal Rights
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent
The study used publicly available de-identified data; hence, informed consent was not required.
Conflict of Interest
The authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors confirm that this paper has not been either previously published or submitted simultaneously for publication elsewhere.
Contributor Information
Nasim Maleki, Email: NMALEKI@mgh.harvard.edu.
Ismaeel Yunusa, Email: iyunusa@mailbox.sc.edu.
Ibraheem M. Karaye, Email: Ibraheem.m.karaye@hofstra.edu
References
- Anderson P, de Bruijn A, Angus K, Gordon R, Hastings G. Impact of alcohol advertising and media exposure on adolescent alcohol use: A systematic review of longitudinal studies. Alcohol and Alcoholism. 2009;44(3):229–243. doi: 10.1093/alcalc/agn115. [DOI] [PubMed] [Google Scholar]
- Berey BL, Loparco C, Leeman RF, Grube JW. The myriad influences of alcohol advertising on adolescent drinking. Current Addiction Reports. 2017;4(2):172–183. doi: 10.1007/s40429-017-0146-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brumback T, Cao D, King A. Effects of alcohol on psychomotor performance and perceived impairment in heavy binge social drinkers. Drug and Alcohol Dependence. 2007;91(1):10–17. doi: 10.1016/j.drugalcdep.2007.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castle IJP, Yi H-Y, Hingson RW, White AM. State variation in underreporting of alcohol involvement on death certificates: Motor vehicle traffic crash fatalities as an example. Journal of Studies on Alcohol and Drugs. 2014;75(2):299–312. doi: 10.15288/jsad.2014.75.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Understanding the opioid overdose epidemic. https://www.cdc.gov/opioids/basics/epidemic.html#:~:text=The%20first%20wave%20began%20with,overdose%20deaths%20involving%20heroin4. Accessed 21 Nov 2022.
- Drug Abuse Warning Network (DAWN) (2021). Preliminary findings from drug-related emergency department visits. https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP22-07-03-001.pdf. Accessed 5 Nov 2022.
- Eckardt MJ, File SE, Gessa GL, et al. Effects of moderate alcohol consumption on the central nervous system. Alcoholism, Clinical and Experimental Research. 1998;22(5):998–1040. doi: 10.1111/j.1530-0277.1998.tb03695.x. [DOI] [PubMed] [Google Scholar]
- Erol A, Karpyak VM. Sex and gender-related differences in alcohol use and its consequences: Contemporary knowledge and future research considerations. Drug and Alcohol Dependence. 2015;156:1–13. doi: 10.1016/j.drugalcdep.2015.08.023. [DOI] [PubMed] [Google Scholar]
- GBD Alcohol Collaborators Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet (london, England). 2018;392(10152):1015–1035. doi: 10.1016/S0140-6736(18)31310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911–923. doi: 10.1001/jamapsychiatry.2017.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones AW, Neri A. Age-related differences in blood ethanol parameters and subjective feelings of intoxication in healthy men. Alcohol and Alcoholism. 1985;20(1):45–52. [PubMed] [Google Scholar]
- Lucey MR, Hill EM, Young JP, Demo-Dananberg L, Beresford TP. The influences of age and gender on blood ethanol concentrations in healthy humans. Journal of Studies on Alcohol. 1999;60(1):103–110. doi: 10.15288/jsa.1999.60.103. [DOI] [PubMed] [Google Scholar]
- Meier P, Seitz HK. Age, alcohol metabolism and liver disease. Current Opinion in Clinical Nutrition and Metabolic Care. 2008;11(1):21–26. doi: 10.1097/MCO.0b013e3282f30564. [DOI] [PubMed] [Google Scholar]
- Miller MA, Fillmore MT. Protracted impairment of impulse control under an acute dose of alcohol: A time-course analysis. Addictive Behaviors. 2014;39(11):1589–1596. doi: 10.1016/j.addbeh.2013.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse (2022). COVID-19 & substance use. https://nida.nih.gov/research-topics/comorbidity/covid-19-substance-use. Accessed 5 Nov 2022.
- National Institute on Alcohol Abuse and Alcoholism (2020). Alcohol sales during the COVID-19 pandemic (surveillance report COVID-19). Bethesda, Md, National Institute on Alcohol Abuse and Alcoholism. https://pubs.niaaa.nih.gov/publications/surveillance-covid-19/COVSALES.htm. Accessed 5 Nov 2022.
- Niederdeppe J, Avery RJ, Tabor E, Lee NW, Welch B, Skurka C. Estimated televised alcohol advertising exposure in the past year and associations with past 30-day drinking behavior among American adults: Results from a secondary analysis of large-scale advertising and survey data. Addiction. 2021;116(2):280–289. doi: 10.1111/add.15088. [DOI] [PubMed] [Google Scholar]
- Polednak AP. Surveillance of US death rates from chronic diseases related to excessive alcohol use. Alcohol and Alcoholism. 2016;51(1):54–62. doi: 10.1093/alcalc/agv056. [DOI] [PubMed] [Google Scholar]
- Pontzer H, Yamada Y, Sagayama H, et al. Daily energy expenditure through the human life course. Science. 2021;373(6556):808–812. doi: 10.1126/science.abe5017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shield KD, Parry C, Rehm J. Chronic diseases and conditions related to alcohol use. Alcohol Research. 2013;35(2):155–173. [PMC free article] [PubMed] [Google Scholar]
- Stelander LT, Høye A, Bramness JG, et al. The changing alcohol drinking patterns among older adults show that women are closing the gender gap in more frequent drinking: The Tromsø study, 1994–2016. Substance Abuse Treatment, Prevention, and Policy. 2021;16(1):45–45. doi: 10.1186/s13011-021-00376-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spillane S, Shiels MS, Best AF, et al. Trends in alcohol-induced deaths in the United States, 2000–2016. JAMA Network Open. 2020;3(2):e1921451–e1921451. doi: 10.1001/jamanetworkopen.2019.21451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squeglia LM, Boissoneault J, Van Skike CE, Nixon SJ, Matthews DB. Age-related effects of alcohol from adolescent, adult, and aged populations using human and animal models. Alcoholism, Clinical and Experimental Research. 2014;38(10):2509–2516. doi: 10.1111/acer.12531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. (2020). Census. https://data.census.gov/. Accessed 30 Oct 2022.
- Wide-Ranging Online Data for Epidemiologic Research Database (2021). https://wonder.cdc.gov/. Accessed 5 Nov 2022.
- Wilcox GB, Kang E, Chilek L. Beer, wine, or spirits? Advertising’s impact on four decades of category sales. International Journal of Advertising. 2015;34:641–657. doi: 10.1080/02650487.2015.1019961. [DOI] [Google Scholar]
- White AM. Gender differences in the epidemiology of alcohol use and related harms in the United States. Alcohol Research. 2020;40(2):01–01. doi: 10.35946/arcr.v40.2.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A, Castle IJ, Chen CM, Shirley M, Roach D, Hingson R. Converging patterns of alcohol use and related outcomes among females and males in the United States, 2002 to 2012. Alcoholism, Clinical and Experimental Research. 2015;39(9):1712–1726. doi: 10.1111/acer.12815. [DOI] [PubMed] [Google Scholar]
- White AM, Castle IJP, Powell PA, Hingson RW, Koob GF. Alcohol-related deaths during the COVID-19 pandemic. JAMA. 2022;327(17):1704–1706. doi: 10.1001/jama.2022.4308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Alcohol, total per capita (15+) consumption (in litres of pure alcohol) (SDG Indicator 3.5.2). https://www.who.int/data/gho/data/indicators/indicator-details/GHO/total-(recorded-unrecorded)-alcohol-per-capita-(15-)-consumption. Accessed 30 Oct 2022.
- Yeo YH, He X, Ting P-S, et al. Evaluation of trends in alcohol use disorder-related mortality in the US before and during the COVID-19 pandemic. JAMA Network Open. 2022;5(5):e2210259–e2210259. doi: 10.1001/jamanetworkopen.2022.10259. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data utilized in this study manuscript were obtained from the CDC WONDER (Wide-ranging Online Data for Epidemiologic Research) database. Access to the CDC WONDER database is publicly available and can be obtained from the official CDC WONDER website (https://wonder.cdc.gov/). Detailed information regarding the specific dataset used and the corresponding data parameters can be provided upon request to the authors.


