Abstract
BACKGROUND:
Stress experienced by medical students is a well-documented and widespread phenomenon that may have physical and psychological effects on their well-being. One solution is to provide students with the tools to recognize and cope with stress. The aim of this study was to incorporate restorative yoga training—a well-recognized tool for stress reduction—in the third-year medical student pediatrics clerkship and assess the intervention's impact on students’ well-being.
MATERIALS AND METHOD:
Restorative yoga, as a prospective intervention, was offered to third-year medical students at Texas Tech University Health Sciences Center during their pediatrics rotation. The study was between March and August 2020. Each yoga session lasted 45-minutes, once a week for six weeks. Participants completed anonymous questionnaires before and after the intervention via the Warwick-Edinburgh Mental Well-being Scale (WEMWBS).
RESULT:
Over the six-month study period, 25 (71%) of 35 medical students, having been given the option, chose to participate. The WEMWBS contains 14 statements on well-being, and all but one from the list showed a positive increase in average rating from pre intervention to post intervention. The statements “I’ve been feeling more relaxed” and “I’ve been thinking clearly” showed the greatest average increase. Following Chi-squared testing, two statements were found to be significantly different (P < 0.05) before intervention and after intervention: “I’ve been feeling more relaxed” and “I’ve been feeling good about myself.”
CONCLUSION:
Students’ well-being is paramount to medical schools. Restorative yoga offers hopeful outcomes for effective mitigation of the stresses of medical education and may be recommended for wider use.
Keywords: Medical students, stress, wellness, yoga
Introduction
Medical education is academically rigorous and time-intensive, leading to emotional and physical strain of students throughout their training.[1] Many medical students report experiencing anxiety, depression, and other changes in mood in response to sustained stress.[2,3,4] These negative effects on psychological well-being may even precipitate burnout[5] — major issue among medical providers[6] —as students enter the workforce. During the third year of medical school, students traditionally transition to a more clinical role and begin choosing a field of medicine while continuing to study for examinations. This period is likely pivotal for establishing long-term coping strategies that can be useful throughout their career.[7]
Previous literature shows a high prevalence rate of anxiety among medical students: 33.8% according to a global meta-analysis,[1,8] relative to 7.3% prevalence globally.[8] In the meta-analysis, the pooled odds ratio comparing anxiety in medical versus non-medical students was also statistically significant.[1,8] A systematic review of studies examining North American medical students found higher rates of anxiety in medical versus non-medical students and the age-matched general population.[9] Studies also revealed that reported stress increased as medical students progressed through their studies.[10] Over time, stress and anxiety can contribute to burnout, which is associated with reductions in physician competency, timely and quality patient care, and empathy.[9,10,11]
One possible solution to medical students’ stress is implementing yoga as a coping mechanism. Previous studies have recognized that mindfulness, meditation, and yoga positively impact the resolution of depression and anxiety.[11,13,14] In this respect, yoga functions like other self-soothing techniques, such as meditation, relaxation, exercise, or even socializing with friends. Yoga modulates stress response systems by reducing perceived stress and anxiety. This, in turn, decreases physiological arousal: for example, reducing the heart rate, lowering blood pressure, and easing respiration. There is also evidence that yoga helps increase heart rate variability, an indicator of the body's ability to respond to stress more flexibly.[13,14] Previous works have even examined yoga as an intervention at institutions of higher education. University faculty, staff, and graduate students attended weekly yoga sessions for ten weeks, resulting in decreased perceived stress and decreased psychological, behavioral, and physical manifestations of stress.[12,13,14]
The goal of this study was to design, evaluate, and optimize a restorative yoga program that trained students to cope with stress and anxiety, thus benefiting their well-being. This study is one of its kind, evaluating impacts of restorative yoga on the well-being of stressed medical students.
Materials and Methods
The hypothesis of our study was that restorative yoga therapy would help students cope with stress, anxiety, and depression and benefit their well-being. Restorative yoga was offered as an option to third-year medical students on the pediatric rotation at the Texas Tech University Health Sciences Center (TTUHSC) Amarillo campus. The study period was from March 2020 to August 2020. The study protocol was approved by the School of Medicine (SOM) Family Educational Rights and Privacy Act (FERPA) and TTUHSC IRB # 0000097. Students received information on the known beneficial effects of yoga on well-being. They were led in a 45-minute restorative yoga practice by a certified instructor once a week for six weeks.
Student participants underwent anonymous screening by the Warwick-Edinburgh Mental Well-being Scale (WEMWBS) questionnaire, before and after six weeks of yoga training, to evaluate the program's impact on their mental health and well-being. The WEMWBS is a 14-question survey with answers rated on a scale of 1–5, with 1 denoting “none” and five denoting “all the time”.[15,16]
Students anonymously and voluntarily completed a questionnaire specifying sessions they attended and their satisfaction with the program. In addition to this, there was a section for optional comments and feedback. Yoga classes were held in person from March 2020, then moved online to Zoom in July 2020 due to COVID-19. The same certified instructor taught the classes. Zoom sessions were less popular than in-person participation.
Data analysis was done using Microsoft Excel (Microsoft 2020) to determine the differences in the well-being of participants before and after a trial of restorative yoga and to process the satisfaction questionnaire. Participant responses were reported as averages for continuous variables and as numbers and percentages for categorical variables.
Study data was analyzed by the paired sample Chi-squared test for questions that showed a positive percentile increase in rating, with a significance value of P < 0.05. Chi-squared analysis was divided into two categories: (1) less than or equal to 3, and (2) greater than 3.
Results
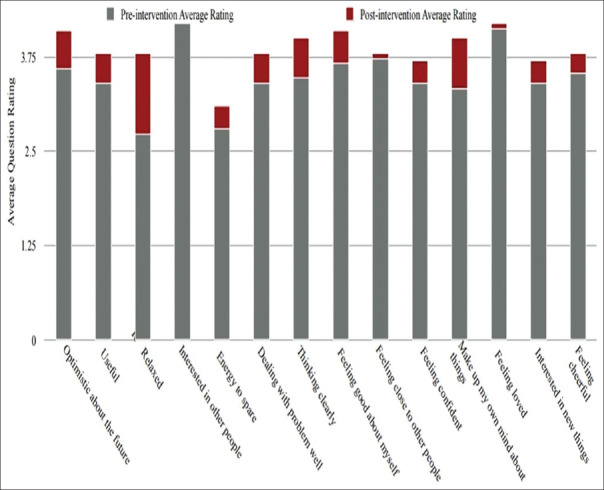
All 25 students participated and completed the six weeks of yoga training, and pre-training and post-training WEMWBS questionnaires. Every statement except one from the WEMWBS showed a positive increase in the average rating [Table 1]. There was no difference between in-person and online session outcomes. The statements “I’ve been feeling more relaxed” and “I’ve been thinking clearly” showed the greatest average increase. Five statements showed the most improvement: “I’ve been feeling relaxed” increased by 43.94%, “I’ve been thinking clearly” by 25.00%, “I’ve been feeling good about myself” by 20.59%, “I’ve been able to make up my own mind about things” by 20.48%, and “I’ve been interested in new things” by 20.13% [Figures 1 and 2].
Table 1.
WEMWBS statement showing change in question scores from average pre-intervention rating to average post-intervention rating
| WEMWBS Statement | Average Pre-intervention Rating | Average Post-intervention Rating |
|---|---|---|
| I‘ve been feeling optimistic about the future | 3.6 | 4.1 |
| I’ve been feeling useful | 3.4 | 3.8 |
| I’ve been feeling relaxed | 2.7 | 3.8 |
| I’ve been feeling interested in other people | 4.2 | 4.2 |
| I’ve had energy to spare | 2.8 | 3.1 |
| I’ve been dealing with problems well | 3.4 | 3.8 |
| I’ve been thinking clearly | 3.5 | 4.0 |
| I’ve been feeling good about myself | 3.7 | 4.1 |
| I’ve been feeling close to other people | 3.7 | 3.8 |
| I’ve been feeling confident | 3.4 | 3.7 |
| I’ve been able to make up my own mind about things | 3.3 | 4.0 |
| I’ve been feeling loved | 4.1 | 4.2 |
| I’ve been interested in new things | 3.4 | 3.7 |
| I’ve been feeling cheerful | 3.5 | 3.8 |
Figure 1.
Change in WEMWBS statement question scores from average pre-intervention rating to average post-intervention rating
Figure 2.
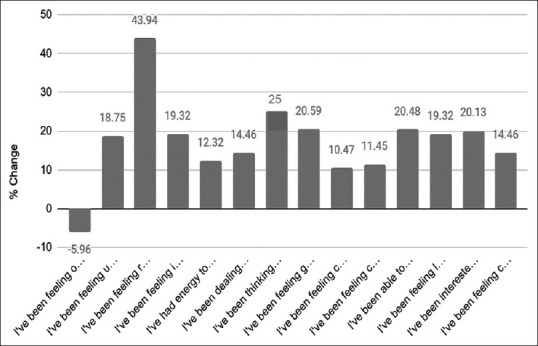
Percentage change in average score from pre to post intervention
Seventy percent of the participants endorsed recommending participation in a program like this to a friend, and 60% felt the program benefited their overall well-being and would participate again.
The Chi-squared analysis showed that two statements were found to be significantly different (P < 0.05) pre and post intervention: “I’ve been feeling more relaxed” and “I’ve been feeling good about myself” [Table 2].
Table 2.
Chi-Squared Analysis of Pre- and Post- Analysis Change in Average Question Scores
| Question | Chi squared result (3 or less/greater than 3) | P |
|---|---|---|
| I’ve been feeling optimistic about the future | 1.268 | 0.260 |
| I’ve been feeling useful | 1.449 | 0.229 |
| I’ve been feeling relaxed | 9.989 | *0.002 |
| I’ve been feeling interest other people | 2.158 | 0.142 |
| I’ve had energy to spare | 1.377 | 0.241 |
| I’ve been dealing with problems | 1.933 | 0.164 |
| I’ve been thinking clearly | 2.260 | 0.133 |
| I’ve been feeling good about myself | 3.969 | *0.046 |
| I’ve been feeling close to other people | 1.145 | 0.285 |
| I’ve been feeling confident | 0.104 | 0.748 |
| I’ve been able to make up my own mind about things | 1.451 | 0.228 |
| I’ve been feeling loved | 0.013 | 0.911 |
| I’ve been interested in new things | 0.002 | 0.961 |
| I’ve been feeling cheerful | 0.567 | 0.452 |
*Significant value with P<0.05
Discussion
Stress and anxiety in higher education are well reported.[16,17] In 2018, 63% of college students in the United States reported overwhelming anxiety in the past year, with 23% being diagnosed or treated by a mental health professional for anxiety.[16,17,18,19] This trend shows no signs of decline, with anxiety levels in the general population increasing in recent years, especially among young adults internationally.[18,19] This research was reproduced in the US and showed a decrease in psychological well-being among adolescents and young adults over the past several years.[17,18,19]
Considering the stress and anxiety seen in higher education and young adults, the demands of medical education and working as a physician generate stress that can negatively affect psychological well-being. One systematic review found that 45%–56% of medical students had symptoms suggestive of burnout, with the prevalence of burnout increasing over time.[18,19] As medical students become residents, the prevalence of burnout increases to 60%.[18,19]
Burnout continues into the physicians’ careers, with rate estimates ranging from 45% to 65%.[17,18,19]. Particularly in the context of COVID-19, it is important that medical students learn techniques to decrease stress and increase relaxation, as burnout has likely started and will only continue as their career advances.
Yoga, a collection of mixed techniques that combine mental and physical well-being,[20] is one possible burnout mitigator. Yoga is a series of postures, breathing techniques, and meditation that promote relaxation.[11,12,13,14,20] In the last decade, yoga has become a more researched topic with regards to its psychophysiological benefits. Reviews of a wide range of yoga practices suggest that they can reduce the impact of exaggerated stress responses and may be helpful for both anxiety and depression.[11,12,13,14,20,21] One randomized control trial on yoga's effect on cancer patients’ anxiety showed that yoga sessions for eight weeks significantly reduced perceived depression and anxiety.[21]
This study suggests that restorative yoga could improve the well-being of medical students, specifically by increasing relaxation and reducing stress related to decision-making. Literature on burnout frequently suggests that exercise and other activities that help physicians relax and be available for themselves could mitigate burnout.[12,13,14,18,19,20,21] However, physicians and students alike often feel time pressures and that they must choose studying or patient care over self-care. However, students in this study experienced positive changes in well-being based on just six 45-minute weekly sessions, demonstrating the possible time efficiency of a restorative yoga practice. Future research examining the effects of multiple shorter practices each week or longer practices every few weeks could help students and physicians pick a schedule that works best for them.
Three statements had the highest percent increase in rating: “I’ve been feeling relaxed,” “I’ve been thinking clearly,” “I’ve been feeling good about myself,” “I’ve been interested in new things,” and “I’ve been able to make up my own mind about things.” Medicine is a career in which important decisions about an individual's career path are made early, such as choosing a specialty or a residency program. Many participants reported stress, decreased decision-making self-efficacy, and indecisiveness because of the potentially immense consequences of their decisions during the second half of medical school. However, the increased rating of those statements suggests that restorative yoga can help take the weight off the decision-making process. As students make many decisions regarding residency and their future lives during their third and fourth years, restorative yoga may provide an avenue for improved well-being.
The statements that had the lowest positive change in rating were statements about social interaction and interpersonal relationships, such as “I’ve been feeling interested in other people,” “I’ve been feeling loved,” and “I’ve been feeling close with other people.” This trend indicates that, while restorative yoga may have been effective at decreasing stress and increasing mindfulness on an intrapersonal level, it did not help create a sense of community. This result was counterintuitive, as many reports have stated that attending a group with shared interests, such as a running or reading, increased feelings such as interpersonal connection and others showing care. This effect may have been less due to the virtual setting of the subsequent yoga classes. Perhaps if the sessions were provided to the same cohort of students in person and over a longer period, a stronger sense of community and support would form. Future research could also offer other relaxation activities to reduce stress and anxiety, such as music therapy where students could pick an area they are genuinely interested in and form bonds with fellow group attendees.
Another limiting factor in implementing social-distancing measures brought on by COVID-19 was the decrease in participation.
Although virtual sessions provide the benefits of increased flexibility in participant location and thus potentially easier access, participants likely felt their experiences were not as good when following an instructor through a screen without other people next to them. Although participants still experienced well-being benefits from attending Zoom sessions, it limited the ability of the yoga teacher to interact with students and help them achieve the full benefits of restorative yoga. Virtual participation also limited the ability of participants to socialize and connect with peers outside of an academic setting. However, the COVID-19 pandemic has changed our world in possibly permanent ways. In the future, it will be important to explore participants’ views on in-person versus virtual sessions and attempt to measure how this affects the possible benefits of restorative yoga. We hope to move the sessions back to in person as COVID-19 precautions allow and continue to offer a virtual option.
Overall, our data suggest the recommendation of a weekly restorative yoga practice as part of burnout and stress reduction initiatives for medical students. This practice would likely also benefit medical residents and practicing physicians, targeting high rates of anxiety, depression, and other mental health issues seen in medical professionals. Yoga is correlated with a positive change in relaxation, mental clarity, and self-esteem. Increasing these qualities during a pivotal time in medical education when students make important and potentially anxiety-inducing career choices could hopefully have enduring benefits for their well-being.
Working to help students reduce their stress levels will hopefully help them form favorable long-term coping techniques that will benefit them as they progress through their medical career with potentially enduring effects on well-being. It seems that restorative yoga could bring clarity around decision-making.
Some of the study limitations include small sample size of students who received the yoga intervention, no control data (students’ response to questionnaire and received no intervention), and single institution. The strength of the study includes same yoga instructor for all participants, either in-person or virtually. Our study hypothesis could be reevaluated further with a larger group of students and a control group with no yoga intervention.
Conclusion
The results indicate that restorative yoga could improve the well-being of medical students during the demanding time of medical school, specifically by increasing relaxation and reducing stress around decision-making. Overall, long-term yoga usefulness was demonstrated, as most participants endorsed that they would recommend the program to a friend and participate again. It would be useful to continue to explore the application of restorative yoga for well-being when participation is not limited by restriction of in-person classes.
Ethics statement
No individual patient-level data were utilized for this study, and the data were fully anonymized. The study was approved by Texas Tech University Health Sciences Center (TTUHSC), School of Medicine (SOM), Family Educational Rights and Privacy Act (FERPA) and TTUHSC Institutional review board (IRB) # 0000097.
Financial support and sponsorship
The study was supported by a grant from Dean's office at Texas Tech University Health Sciences Center, School of Medicine.
Conflict of interest
There are no conflicts of interest.
Acknowledgement
The authors appreciate Ellen Brown MS4, Mrs. Howard, and Dr. Hefley for their valuable input and study management.
References
- 1.Quek T, Tam W, Tran B, Tran B, Zhang M, Zhang Z, et al. The global prevalence of anxiety among medical students: A meta-analysis. Int J Environ Res Public Health. 2019;16:2735. doi: 10.3390/ijerph16152735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aktekin M, Karaman T, Senol YY, Erdem S, Erengin H, Akaydin M. Anxiety, depression, and stressful life events among medical students: A prospective study in Antalya, Turkey. Med Educ. 2001;35:12–7. doi: 10.1046/j.1365-2923.2001.00726.x. [DOI] [PubMed] [Google Scholar]
- 3.Bond AR, Mason HF, Lemaster CM, Shaw SE, Mullin CS, Holick EA, et al. Embodied health: The effects of a mind body course for medical students. Med Educ Online. 2013;18:1–8. doi: 10.3402/meo.v18i0.20699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shoaib M, Afzal A, Aadil M. “Medical students” burnout—need of student mentor and support groups and emotional resilience skills training to be a part of medical school curriculum. Adv Med Educ Pract. 2017;8:179–80. doi: 10.2147/AMEP.S132809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yilmaz A. Burnout, job satisfaction, and anxiety-depression among family physicians: A cross-sectional study. J Family Med Prim Care. 2018;7:952–6. doi: 10.4103/jfmpc.jfmpc_59_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of burnout among physicians: A systematic review. JAMA. 2018;11:1131–50. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schiller J, Stansfield R, Belmonte D, Purkiss JA, Reddy RM, House JB, et al. Medical students’ use of different coping strategies and relationship with academic performance in preclinical and clinical years. Teach Learn Med. 2017;30:15–21. doi: 10.1080/10401334.2017.1347046. [DOI] [PubMed] [Google Scholar]
- 8.Baxter AJ, Scott KM, Vos T, Whiteford HA. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychol Med. 2013;43:897–910. doi: 10.1017/S003329171200147X. [DOI] [PubMed] [Google Scholar]
- 9.Dyrbye L, Thomas M, Shanafelt T. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81:354–73. doi: 10.1097/00001888-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50:132–49. doi: 10.1111/medu.12927. [DOI] [PubMed] [Google Scholar]
- 11.Breedvelt JJF, Amanvermez Y, Harrer M, Karyotaki E, Gilbody S, Bockting CLH, et al. The effects of meditation, yoga, and mindfulness on depression, anxiety, and stress in tertiary education students: A meta-analysis. Front Psychiatry. 2019;10:193. doi: 10.3389/fpsyt.2019.00193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brems C. A yoga stress-reduction intervention for university staff, faculty, and graduate students. Int J Yoga Therap. 2015;5:61–7. doi: 10.17761/1531-2054-25.1.61. [DOI] [PubMed] [Google Scholar]
- 13.Cocchiara RA, Peruzzo M, Mannocci A, Ottolenghi L, Villari P, Polimeni A, et al. The use of yoga to manage stress and burnout in healthcare workers: A systematic review. J Clin Med. 2019;8:284. doi: 10.3390/jcm8030284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prasad L, Varrey A, Sisti G. Medical students’ stress levels and sense of well-being after six weeks of yoga and meditation. Evid Based Complement Alternat Med 2016. 2016 doi: 10.1155/2016/9251849. 9251849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh mental well-being scale (WEMWBS): Development and UK validation. Health Qual Life Outcomes. 2007;5:63. doi: 10.1186/1477-7525-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Calling S, Midlöv P, Johansson S, Sundquist K, Sundquist J. Longitudinal trends in self-reported anxiety. Effects of age and birth cohort during 25 years. BMC Psychiatry. 2017;17:119. doi: 10.1186/s12888-017-1277-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.West C, Dyrbye L, Shanafelt T. Physician burnout: Contributors, consequences and solutions. J Int Med. 2018;283:51629. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- 18.Shanafelt T, Hasan O, Dyrbye L, Sinsky C, Satele D, Sloan J, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proc. 2015;90:1600–13. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 19.Shanafelt T, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Int Med. 2012;172:1377–85. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 20.Mohammad A, Thakur P, Kumar R, Kaur S, Saini RV, Saini AK. Biological markers for the effects of yoga as a complementary and alternative medicine. J Complement Integr Med. 2019;16 doi: 10.1515/jcim-2018-0094. doi: 10.1515/jcim-2018-0094. [DOI] [PubMed] [Google Scholar]
- 21.Mirandola M, Rueda S, Andreis F, Meriggi F, Codignola C, Gadaldi E, et al. Yoga Protocol for cancer patients: A systematic exploration of psychophysiological benefits. Rev Recent Clin Trials. 2019;14:261–8. doi: 10.2174/1574887114666190729143742. [DOI] [PubMed] [Google Scholar]