Abstract
Purpose:
Prior studies have identified a significant relationship between internalized transphobia and poor mental health among transgender and gender-diverse (TGD) adults; however, this relationship has not been extensively examined among youth. Further, little research has sought to explore protective factors, such as identity pride, and their influence on this relationship. We examined the association between internalized transphobia and depression and anxiety symptoms among TGD youth and explored the moderating role of gender identity pride on these associations.
Methods:
Participants were 315 TGD youth ages 12–20 years (M = 16; SD = 1.89) seeking gender-affirming hormone treatment at one of four major pediatric hospitals across the U.S. At the time of enrollment, participants were naïve to gender-affirming hormone treatment. Participants self-reported mental health, internalized transphobia, and identity pride. Multiple regression models were used with depression and anxiety symptoms as outcomes, and age, designated sex at birth, and perceived parental support included as covariates.
Results:
Greater internalized transphobia was associated with greater depressive symptoms, and gender identity pride moderated this relationship, such that greater gender identity pride was associated with fewer depressive symptoms. Greater internalized transphobia was significantly associated with greater anxiety symptoms; no moderation effect was observed for this relationship.
Conclusions:
Gender identity pride influenced mental health symptoms for youth experiencing internalized transphobia and represents a potential key protective factor. These results support efforts to further develop, test, and implement clinical inventions to bolster identity pride for TGD youth.
Keywords: transgender, non-binary, adolescents and young adults, internalized transphobia, gender identity pride, mental health
Transgender and gender-diverse (TGD) individuals are those whose gender identity is not congruent with their designated sex at birth and may include those who identify as non-binary, agender, and other identities outside of a male-female gender binary1. A growing literature has observed that TGD individuals experience higher rates of mental health problems (e.g., depression, anxiety) compared to their cisgender peers (i.e., those whose gender identity is congruent with their designated sex at birth)1,2 and their cisgender sexual minority peers (i.e., cisgender lesbian, gay, bisexual individuals)3. These mental health disparities are present by adolescence and highlight the importance of identifying factors that impact healthy development in TGD youth2, including mental health symptoms and protective factors.
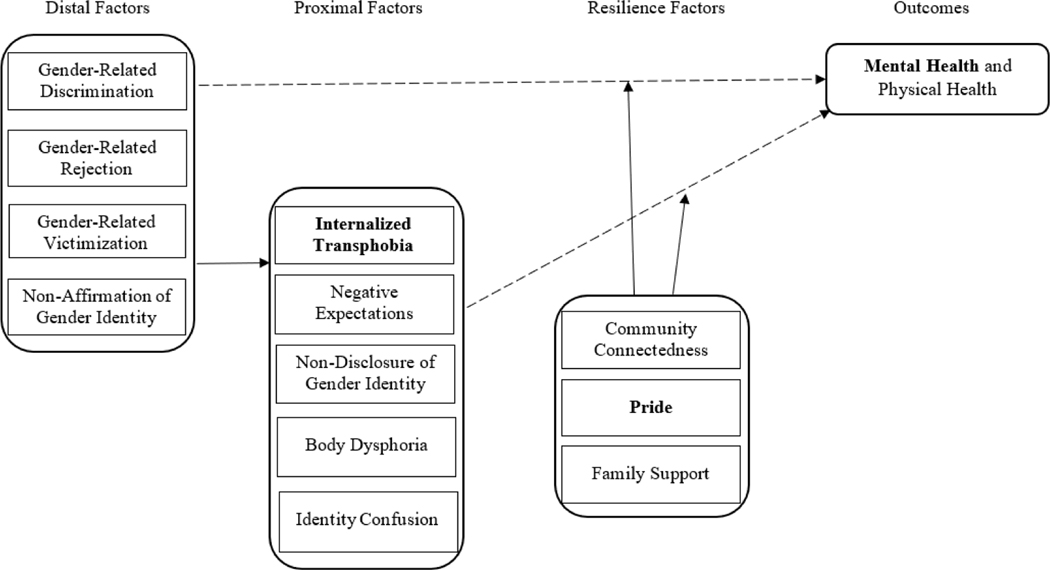
Disparities in mental health outcomes among TGD youth compared to their cisgender peers are speculated to stem from chronic, pervasive stress associated with their minoritized identity (i.e., gender minority stress)4–7. The Gender Minority Stress (GMS) Model, based on the Minority Stress framework8, posits that the cumulative effects of proximal (e.g., internalized stigma and shame)9 and distal stressors (e.g., policies that promote discrimination, lack of community resources)1,4 contribute to negative mental health outcomes among TGD individuals. The GMS model also includes factors that may ameliorate the substantial toll of minority stress on mental health outcomes in youth (e.g., identity pride, community connectedness)5. Moreover, this framework has continued to be expanded upon to include more expansive models of transgender resilience, such as the Transgender Resilience Intervention Model (TRIM), with implications and guidelines for intervention and policy efforts to address minority stress and strengthen sources of resilience10. More recently, in their model, Coyne and colleagues (2020)11 presented an adapted Gender Minority Stress framework that accounts for additional resilience factors that may buffer the effects of stressors (see figure 1).
Figure 1.
Adapted gender minority stress and resilience factors model from Coyne et al. (2020). Bolded factors are the focus of the present analysis.
Internalized transphobia is a stress process in which an individual experiences discomfort with their own transgender identity as a result of internalizing society’s negative attitudes toward TGD people (e.g., anti-transgender legislation and policies, family/peer rejection)12,13. Research has linked experiencing distal stressors, such as non-affirmation and anti-transgender bias, to the development of greater internalized transphobia; moreover, researchers found that such minority stressors were both directly and indirectly (via internalized transphobia) linked to greater severity of post-traumatic stress14. Internalized transphobia has also been found to increase the risk of having a diagnosis of Major Depressive Disorder (MDD) and Generalized Anxiety Disorder (GAD) among TGD youth15.
Gender identity pride, a source of internal resilience for TGD youth, has begun to be explored as a potential buffer against the impact of chronic minority stress10,16. Gender identity pride within a Western socio-cultural context has been conceptualized as feelings of positive regard related to one’s identity as part of the gender minority community16. Findings from burgeoning research suggest that gender identity pride may buffer against internalized stigma and shame related to belonging to a gender minority group16,17. More recently, outpatient, camp-based, and telehealth interventions focused on improving self-esteem and identity pride for TGD youth have been developed and evaluated18–21. These efforts have identified important facets for treatment, including positive identity development, use of narrative methods, positive social support and community building, and reducing internalized transnegativity19–22. However, to date, few studies have quantitatively investigated the relationship between internalized transphobia and gender identity pride among TGD youth and whether identity pride serves as a protective factor in mitigating or buffering against negative outcomes16,23. The current study aims to contribute to the literature supporting these ongoing efforts.
The present study explored two potential mechanisms of mental health risk and resilience among TGD youth. First, we examined whether internalized transphobia is associated with depression and anxiety symptoms in a sample of TGD youth. We then examined how gender identity pride may moderate associations between internalized transphobia and symptoms of depression and anxiety. We hypothesized that internalized transphobia would be associated with greater depression and anxiety (Hypothesis 1) and that gender identity pride would moderate these associations such that the internalized transphobia—depression/anxiety association would be strongest at low levels of gender identity pride (Hypothesis 2).
Methods
Participants and recruitment
The Trans Youth Care Study is an ongoing, multisite, observational study of TGD initiating medical treatment with gender-affirming hormones (i.e., testosterone or estrogen) 24,25. The study’s aims include the longitudinal tracking of gender-affirming treatment outcomes, mental health, and overall well-being of TGD youth. Participants were recruited from four pediatric gender clinics located in major metropolitan areas of the U.S., reflecting demographics from the western, midwestern, and northeastern areas of the country (i.e., Los Angeles, San Francisco, Chicago, and Boston). Eligibility criteria include: (1) presence of gender dysphoria as determined by a clinician; (2) appropriateness and readiness to initiate gender-affirming hormones (GAH) (i.e., estrogen or testosterone) as determined by the clinical team; (3) age 20 years or younger; (4) English proficiency; and (5) psychiatrically and cognitively able to give informed consent/assent for participation. Data were collected by a computer-assisted survey instrument from youth only. While the Trans Youth Care study recruited two cohorts (i.e., GAH cohort and gonadotropin-releasing hormone agonist [GnRHa] cohort), the present study used only the GAH cohort baseline survey data, which were collected prior to participants initiating GAH. Exploring the mental health of these youth prior to treatment was indicated so as not to have effects of treatment confound our findings, given that youth generally report improved mental health after accessing hormone treatment26. The GnRHa cohort is comprised of younger youth accessing puberty-blocking hormones for which key variables in the current analysis were not available (i.e., gender minority stress and resilience scale); thus, they were not included in the present study. A detailed description of the Trans Youth Care Study methods and data on the full cohort are published elsewhere24. Researchers received institutional review board approval from all study sites. Consent and assent were obtained for all participants; parental permission was obtained for minors.
Initial findings on the baseline characteristics of the study have been previously published25. Participants were 315 youth ages 12–20 (M = 16.01; SD = 1.87). The baseline survey initially included 316 individuals; however, one participant was ultimately excluded for not meeting inclusion criteria.
Demographics.
Participants self-reported age in years, race/ethnicity, and designated sex at birth. The sample identified as White non-Hispanic/Latinx (58.7%), White Hispanic/Latinx (7.9%), non-White Hispanic/Latinx (15.9%), Multiracial (10.2%), Black/African American (3.5%), Asian/Pacific Islander (3.2%) and Other (0.6%); see Table 1. Participants were transmasculine/male (60.3%), transfeminine/female (33.7%), non-binary (3.8%), genderqueer/gender fluid (1.3%) and other (1%). These responses were recoded into three categories: transmasculine/male (60.3%), transfeminine/female (33.7%), and non-binary (6.0%).
Table 1.
Participant characteristics (N = 315).
| Variable | Frequency - Number (%) |
|---|---|
|
| |
| Age (Mean = 16.01; SD = 1.87) | |
| 12 | 6 (1.9) |
| 13 | 23 (7.3) |
| 14 | 38 (12.1) |
| 15 | 67 (21.3) |
| 16 | 55 (17.5) |
| 17 | 51 (16.2) |
| 18 | 48 (15.2) |
| 19 | 15 (4.8) |
| 20 | 12 (3.8) |
| Gender Identity * | |
| Transmasculine/male | 190 (60.3) |
| Transfeminine/female | 106 (33.6) |
| Non-Binary | 12 (3.8) |
| Genderqueer/gender fluid | 4 (1.3) |
| Other | 3 (1.0) |
| Sex Assigned at Birth | |
| Male | 111 (35.2) |
| Female | 204 (64.8) |
| Race/Ethnicity | |
| White | 185 (58.7) |
| Non-white Hispanic/Latinx | 50 (15.9) |
| White Hispanic/Latinx | 25 (7.9) |
| Black/African American | 11 (3.5) |
| Multiracial | 32 (10.2) |
| Asian/Pacific Islander | 10 (3.2) |
| Other/Unknown | 2 (0.6) |
| Beck Depression Inventory (BDI) | |
| Minimal | 129 (48.1) |
| Mild | 48 (17.9) |
| Moderate | 50 (18.7) |
| Severe | 41 (15.3) |
| M (SD) | |
| Revised-Children’s Manifest Anxiety Scale (RCMAS-2) | 60.03 (11.48) |
| Total T-score (range = 29–81) | |
| Gender Minority Stress and Resilience - select scales | |
| Internalized Transphobia (range = 0–32) | 13.27 (8.48) |
| Gender Identity Pride (range = 0–32) | 8.06) |
One participant indicated that their designated sex at birth and gender identity were aligned at baseline and met eligibility criteria for the study.
Perceived parental support.
General parental support was assessed using four items adapted from the Family subscale of the Multidimensional Scale of Perceived Social Support (MSPSS)27,28 (i.e., statements changed “family” to “parent”). Examples of items include: “My parent or parents really try to help me” and “I get the emotional help and support I need from my parent or parents”. The items are rated on a 5-point Likert scale (1=strongly disagree to 5=strongly agree) with higher scores indicating greater perceived parental support.
Mental health.
The Revised-Children’s Manifest Anxiety Scale (RCMAS-2)29 assessed anxiety with a 49-item “yes”/ “no” response scale. “Yes” responses were summed and converted into T-scores (>60 = clinically significant) reflecting a Total Anxiety score.
The 21-item Beck Depression Inventory-II (BDI-II)30 is a self-report measure of depressive symptoms (e.g., sadness, loss of interest, worthlessness) over the previous two weeks scored on a 0–3 scale. For example, for “Sadness”, respondents choose from 0 = “I do not feel sad” to 3 = “I am so sad or unhappy that I can’t stand it.” Scores were summed and compared to standardized cutoffs reflecting minimal (0–13), mild (14–19), moderate (20–28), and severe depression (29–63).
Gender Minority Stress and Resilience.
The Gender Minority Stress and Resilience Measure for Adolescents (GMSR-A) is a self-report measure assessing social stigma and psychosocial resilience associated with gender minority identity7 adapted for adolescents31. The GMSR-A is comprised of nine subscales (i.e., internalized transphobia, non-affirmation, non-disclosure, negative expectations, gender identity pride, community connectedness). Two subscales were used in the current study: internalized transphobia (e.g., “ When I think about my gender identity or expression, I feel unhappy”, “I feel that my gender identity or expression is embarrassing”) and gender identity pride (“I am proud to be a person whose gender identity is different from my sex assigned at birth”, “I have no problem talking about my gender identity and gender history to almost anyone”). All subscales were rated on a 5-point Likert scale (1=strongly disagree to 5=strongly agree). Subscale items were summed with higher scores indicating greater minority stress or resilience, respectively.
Data Analyses
Data analyses were conducted using SPSS 28.032. Correlation analyses were performed to examine relationships between predictor and outcome variables for the total sample. Age, designated sex at birth, and perceived parental support were included as covariates based on prior analytic findings indicating significant associations with the outcomes of interest25. In addition, after accounting for significant outliers (n = 2), ANOVAs did not identify any significant mean differences on predictor or outcome variables based on racial/ethnic groups or clinic location. Additional key covariates were included in the initial models, including race/ethnicity and location, but were statistically non-significant and not included in the final models to retain statistical power. Two initial univariate regression models examined the role of internalized transphobia as a predictor of anxiety and depression with age, designated sex at birth (dummy coded 0 for designated male at birth and 1 for designated female at birth), and perceived parental support entered as covariates in step 1 and internalized transphobia added in step 2. Two univariate regression models were performed using the PROCESS macro.33 Model 1 (simple moderation) examined the moderating role of gender identity pride on the relationship between internalized transphobia and each mental health outcome (i.e., anxiety, depression) independently, with age, designated sex at birth, and perceived parental support included as covariates in Step 1, internalized transphobia and gender identity pride added as covariates in step 2, and an interaction term for internalized transphobia x gender identity pride added in step 3. The PROCESS macro utilizes bootstrapping that non-parametrically re-samples the dataset 5,000 times. Bootstrapping is considered robust for managing skewness and missing data, stringent in avoiding Type 1 error, and statistically more powerful than traditional analytical approaches34. The significant interactions were further interpreted using a simple slopes analysis in which we observed the effect of internalized transphobia for high levels of identity pride (one SD above the mean), the main effect of internalized transphobia (for mean-centered levels of identity pride), and low levels of identity pride (one SD below the mean)35. Missing data were addressed using individual mean imputation, which can reduce bias introduced by excluding cases with missing data, when a case contains a majority of responses and calculating missing responses is needed to create composite scales36. Models included participants who had complete data (n = 304 for depression and n = 303 for anxiety outcomes).
Results
Bivariate correlations found that age was positively associated with anxiety (ρ = .117, p < .05) and gender identity pride (ρ = .130, p < .05; i.e., older age was associated with higher levels of anxiety and higher gender identity pride) while being designated female at birth was associated with lower levels of gender identity pride (ρ = −.178, p <.01). Greater perceived parental support was significantly associated with younger age (ρ = −.252, p <.01), lower internalized transphobia (ρ = −.135, p <.05), lower anxiety (ρ = −.209, p <.01), and lower depression (ρ = −.259, p <.01). Higher levels of depression and anxiety were associated with greater internalized transphobia (ρ = .436 and ρ = .427, p < .01, respectively) and lower levels of gender identity pride (ρ = −.186 and ρ = −.172, p < .01, respectively). Finally, greater internalized transphobia was associated with lower levels of gender identity pride (ρ = −.367, p < .01). See Table 2.
Table 2.
Correlation table.
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| 1. Age | --- | ||||||
| 2. Designated Sex at Birth | −.101 | --- | |||||
| 3. MSPSS-Family Scale | −.252** | .047 | --- | ||||
| 4. BDI-II | .087 | −.039 | −.259** | --- | |||
| 5. RCMAS Total Score | .117 * | .037 | −.209** | .706 ** | --- | ||
| 6. IT | .082 | .056 | −.135* | .436 ** | .417 ** | --- | |
| 7. GIP | .130 * | −.178** | .067 | −.186** | −.172** | −.367** | --- |
p < .05
p < .01
Note: MSPSS – Multidimensional Scale of Perceived Social Support. BDI-II – Beck Depression Inventory, Second Edition. RCMAS – Revised Children’s Manifest Anxiety Scale. IT – Internalized Transphobia subscale. GIP – Gender Identity Pride subscale.
Hypothesis 1.
We hypothesized that internalized transphobia would be associated with greater depression and anxiety. Consistent with this hypothesis, internalized transphobia was significantly associated with greater depression, b = .53 [95% CI .37–.69], p <.01, and anxiety, b = .47 [95% CI .15–.79], p<.01. Further, internalized transphobia was significantly associated with greater anxiety when gender identity pride was added as a moderator to the model, b = .52 [95% CI .37–.67], p < .01. Based on bivariate analysis and consistent with prior literature, age, designated sex at birth, and perceived parental support were retained as covariates in all models. Only lower perceived parental support was associated with greater depression and anxiety across all steps of the regression models (p < .05). See Table 3.
Table 3.
Regression analysis main and interaction effects.
| Variable | B | SE | p | LLCI-ULCI | Adjusted R2 | R2 Change (Interaction) |
|---|---|---|---|---|---|---|
|
| ||||||
| BDI-II Total Score (n=302) | ||||||
|
| ||||||
| Step 1 | .04 | |||||
|
| ||||||
| - Age | .02 | .38 | .95 | |||
| - Designated Sex at Birth | −1.31 | 1.42 | .36 | |||
| - Perceived Parental Support | −.66 | .19 | <.01 | |||
|
| ||||||
| Step 2 | .20 | |||||
|
| ||||||
| - Age | −.04 | .35 | .91 | |||
| - Designated Sex at Birth | −2.05 | 1.32 | .12 | |||
| - Perceived Parental Support | −.49 | .18 | <.01 | |||
| - Internalized Transphobia (IT) | .53 | .08 | <.01 | |||
| - Gender Identity Pride (GIP) | −.12 | .09 | .18 | |||
|
| ||||||
| Step 3 | .22 | .0 1 | ||||
|
| ||||||
| - Age | −.06 | .35 | .87 | −.75–.63 | ||
| - Designated Sex at Birth | −1.79 | 1.31 | .17 | −4.38–.80 | ||
| - Perceived Parental Support | −.50 | .17 | <.01 | −.84–.−.15 | ||
| - IT | .52 | .08 | <.01 | .36–.67 | ||
| - GIP | −.09 | .09 | .30 | −.26–.08 | ||
| - IT x GIP | −.02 | .01 | .03 | −.04– −.00 | ||
|
| ||||||
| RCMAS Total T-Score (n=301) | ||||||
|
| ||||||
| Step 1 | .04 | |||||
|
| ||||||
| - Age | .42 | .36 | .25 | |||
| - Designated Sex at Birth | 1.80 | 1.36 | .19 | |||
| - Perceived Parental Support | −.54 | .18 | <.01 | |||
|
| ||||||
| Step 2 | .18 | |||||
|
| ||||||
| - Age | .29 | .34 | .40 | |||
| - Designated Sex at Birth | 1.41 | 1.28 | .27 | |||
| - Perceived Parental Support | −.38 | .17 | .03 | |||
| - Internalized Transphobia (IT) | .50 | .08 | <.01 | |||
| - Gender Identity Pride (GIP) | −.01 | .08 | .89 | |||
|
| ||||||
| Step 3 | .19 | .00 | ||||
|
| ||||||
| - Age | .29 | .34 | .39 | −.38–.96 | ||
| - Designated Sex at Birth | 1.38 | 1.28 | .28 | −1.15–3.90 | ||
| - Perceived Parental Support | −.38 | .17 | .03 | −.71– −.04 | ||
| - IT | .50 | .08 | <.01 | .35–.66 | ||
| - GIP | −.02 | .08 | .86 | −.18–.15 | ||
| - IT x GIP | .00 | .01 | .75 | −.01–.02 | ||
Bolded p values indicate significance.
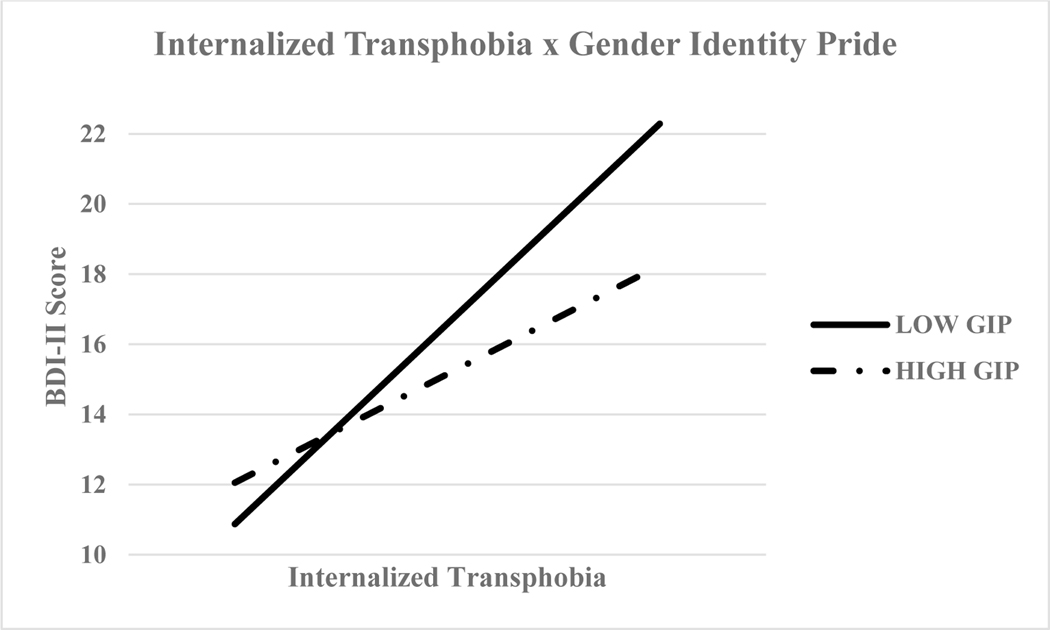
Hypothesis 2.
We hypothesized that gender identity pride would moderate associations between internalized transphobia and mental health outcomes. The second hypothesis was partially supported with a significant interaction observed for the model with depression as the outcome but not for the model with anxiety as the outcome. As noted above, simple slopes for the associations between internalized transphobia and mental health outcomes were examined at low (−1.0 standard deviation [SD]), mean or average, and high (+1.0 standard deviation [SD]) levels of gender identity pride. Gender identity pride significantly moderated the association between internalized transphobia and depression at all levels; specifically, at low levels (b = .68, p < .01), average levels (b = .53, p < .01), and at high levels (b = .38, p < .01). The strongest moderation effects were observed at the lowest levels of identity pride, ΔR2 = .01, ΔF(1, 298) = 4.72, p = .03 suggesting that youth with the highest levels of internalized transphobia and lowest levels of gender identity pride reported the highest levels of depressive symptoms. Figure 2 displays the simple slopes. Moderation was not observed in the model examining anxiety as the outcome. See Table 3 for significant main and interaction effects.
Figure 2.
Moderating effect of gender-identity pride on the association between internalized transphobia and depressive symptoms (p = .03).
Note: GIP = Gender Identity Pride
Discussion
Internalized transphobia contributes significantly to poorer mental health among TGD individuals5,16. Prior research has identified internalized transphobia as a significant, intervenable factor in addressing high rates of negative mental health among TGD individuals37. The present study found that greater internalized transphobia was significantly associated with greater anxiety and depressive symptoms16,38, extending prior findings to a larger sample of TGD youth23 and highlighting internalized transphobia as an important target for mental health intervention. In partial support of our hypothesis, we found that gender identity pride moderated the relationship between internalized transphobia and depressive symptoms. This association was present for all levels of gender identity pride; however, the strongest effects were observed at the lowest level of identity pride. More specifically, youth with high internalized transphobia and low identity pride endorsed greater depressive symptoms. These results provide additional evidence to support interventions aimed at improving gender identity pride as a factor in reducing depressive symptoms among TGD youth with internalized transphobia. Contrary to our hypothesis, we did not observe a similar moderating effect of gender identity pride on the relationship between internalized transphobia and anxiety for TGD youth.
As noted, previous studies have explored the moderating role of gender identity pride on the relationship between internalized transphobia and mental health among TGD adults7,16,39. However, this study is among the first to examine these relationships in TGD youth. According to prior research with other minoritized communities, pride in one’s identity supports positive mental health and promotes healthy behaviors40. Burgeoning clinical research indicates that such minority stressors, like internalized transphobia, can be addressed through gender-affirmative therapy with youth and families41; specifically, as a component of interventions to address internalized stigma and transphobia10,42. For instance, a brief online cognitive-behavioral therapy intervention for LGBTQ+ youth that focused on addressing multiple minority stressors, including stigma and discrimination, and promoting resilience (i.e., reflective coping, adaptive stress appraisal) was found to significantly reduce depression and increase use of positive coping strategies10,42.
Our findings suggest that among TGD youth with internalized transphobia, low gender identity pride is associated with greater depressive symptoms. When assessing mental health among TGD youth, screening for any or all of these domains may be useful when assessing the need for or specificity of a mental health referral. If youth have high levels of internalized transphobia, a helpful referral would be to a gender-affirming psychotherapist who may employ established interventions that aim to reduce depressive symptomology by targeting underlying internalized transphobia through cognitive restructuring43. In addition, evidence has found that increasing a sense of identity pride in peer support groups may also improve mental health outcomes, particularly for ethnically/racially minoritized TGD youth19–21. While these constructs are considered distinct yet associated experiences, one may assess these potential targets for intervention independently, using tools like the GMSR-A measure31. While the GMSR-A has been validated for youth ages 12 and older, it would be beneficial to validate with younger youth, and potentially examine factors, such as internalized transphobia and gender identity pride, with youth prior to pubertal development44. Our findings provide further support for the importance of targeting identity-related constructs to increase TGD youths’ resilience and to ameliorate depressive symptoms10 above and beyond the influence of perceived parental support, a covariate in our analyses. We observed that perceived parental support in our sample continued to be a significant predictor for mental health outcomes. Parental support may reflect a potential protective factor as well for these youth, which is supported by prior findings in the literature45. For instance, parental involvement in building positive identity development has been associated with positive youth development, including psychological adjustment and better mental health46. Future research is warranted to further explore the influence of parental support on the development of identity pride, which will likely have significant implications for the ongoing development and evaluation of family-based interventions47.
As noted, gender identity pride did not moderate the positive relationship between internalized transphobia and anxiety symptoms. Future research should explore other potential influences on the relationship between internalized transphobia and anxiety. For instance, anxiety may be uniquely associated with specific elements of gender minority stress not tested here (e.g., non-disclosure, perception of anti-transgender policies and legislation, and negative expectations for the future)15,48. Though anxiety and depression often co-occur, anxiety may also be associated with positive experiences, including the “coming out” process, and may not necessarily be associated with greater internalized transphobia.
Limitations and Future Directions
The data for the current analyses were cross-sectional in nature, which limited our efforts to infer directionality of results; however, with ongoing data collection, future Trans Youth Care Study research should examine these relationships longitudinally. Further, subgroup differences by gender identity, while pertinent for future analyses, were outside of the current scope of this study and limited by small subgroup sizes. Future investigations are needed to examine subgroups within the community of TGD youth, specifically racially diverse and transfeminine communities, to see if our findings are consistent or differ, as well as to identify predictors of risk or resilience to best tailor treatment approaches. Given the sample size, we were unable to observe any differences by racial/ethnic group or by geographic location. Thus, our current analysis was unable to examine differences across multiple marginalized identities in considering other demographic characteristics that may also influence identity pride (e.g., sexual orientation; race/ethnicity). Therefore, this remains an important area for future research. These efforts can further the development of appropriate interventions that can lessen the impact of internalized transphobia and augment identity pride, particularly among youth who hold multiple marginalized identities19.
Finally, the youth in our sample live in major metropolitan areas within parts of the U.S. that are considered more liberal, inclusive, and supportive for TGD individuals. It should be noted that living in more supportive geographic locations does not completely protect youth from the impact of discrimination and harmful policies occurring on a national level against TGD youth and their families. These findings may not be generalizable to other areas of the country where there is greater stress and discrimination present for TGD youth49,50 highlighting the need to understand and address the mental health needs of youth in these areas.
These results contribute to a dearth of literature specifically examining the role of potential protective factors, like gender identity pride, on the relationship between internalized transphobia and negative mental health. Our findings contribute to this literature and provide further support for behavioral interventions designed to bolster identity pride, a correlate of depressive symptoms in our study17,41. While important, gender identity pride represents only one aspect of strength and resilience for TGD youth. Thus, future research is encouraged to examine whether specific kinds of protective factors, including gender identity pride, community connectedness, and/or positive coping skills, uniquely contribute to well-being and improved mental health. Future research should also consider longitudinal analyses that examine processes and mechanisms by which forms of minority stress and resilience influence pathways of mental health within a population that continue to experience significant marginalization and stigmatization.
Implications and Contributions:
Gender identity pride moderated the relationship between internalized transphobia and depressive symptoms. These findings support the ongoing development and evaluation of interventions to mitigate the impact of internalized transphobia by bolstering gender identity pride.
Funding Source/Acknowledgements
This work was supported by funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD; R01HD082554).
Footnotes
Disclosure
The authors confirm that all listed authors have contributed to this manuscript and have reviewed the final draft.
Conflicts of Interest
The authors have no conflicts of interests or financial disclosures to report relevant to the present analysis/manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Price-Feeney M, Green AE, Dorison S. Understanding the mental health of transgender and nonbinary youth. J Adolesc Health. 2020;66(6):684–690. doi: 10.1016/j.jadohealth.2019.11.314 [DOI] [PubMed] [Google Scholar]
- 2.Newcomb ME, Hill R, Buehler K, Ryan DT, Whitton SW, Mustanski B. High burden of mental health problems, substance use, violence, and related psychosocial factors in transgender, non-binary, and gender diverse youth and young adults. Arch Sex Behav. 2020;49(2):645–659. doi: 10.1007/s10508-019-01533-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Srivastava A, Rusow JA, Goldbach JT. Differential risks for suicidality and mental health symptoms among transgender, nonbinary, and cisgender sexual minority youth accessing crisis services. Transgend Health. 2021;6(1):51–56. doi: 10.1089/trgh.2020.0034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lefevor GT, Boyd-Rogers CC, Sprague BM, Janis RA. Health disparities between genderqueer, transgender, and cisgender individuals: An extension of minority stress theory. J Couns Psychol. 2019;66(4):385–395. doi: 10.1037/cou0000339 [DOI] [PubMed] [Google Scholar]
- 5.Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the Minority Stress Model. Prof Psychol Res Pr. 2012;43(5):460–467. doi: 10.1037/a0029597 [DOI] [Google Scholar]
- 6.Valentine SE, Shipherd JC. A systematic review of social stress and mental health among transgender and gender non-conforming people in the United States. Clin Psychol Rev. 2018;66:24–38. doi: 10.1016/j.cpr.2018.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Testa RJ, Habarth J, Peta J, Balsam K, Bockting W. Development of the Gender Minority Stress and Resilience Measure. Psychol Sex Orientat Gend Divers. 2015;2(1):65–77. doi: 10.1037/sgd0000081 [DOI] [Google Scholar]
- 8.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/00332909.129.5.674i [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trujillo MA, Perrin PB, Sutter M, Tabaac A, Benotsch EG. The buffering role of social support on the associations among discrimination, mental health, and suicidality in a transgender sample. Int J Transgend. 2017;18(1):39–52. doi: 10.1080/15532739.2016.1247405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matsuno E, Israel T. Psychological nterventions promoting resilience among transgender individuals: Transgender Resilience Intervention Model (TRIM). Couns Psychol. 2018;46(5):632–655. doi: 10.1177/0011000018787261 [DOI] [Google Scholar]
- 11.Coyne CA, Poquiz JL, Janssen A, Chen D. Evidence-based psychological practice for transgender and non-binary youth: Defining the need, framework for treatment adaptation, and future directions. Evid Based Prac Child Adol Ment Health. 2020;5(3):340–353. doi: 10.1080/23794925.2020.1765433 [DOI] [Google Scholar]
- 12.Pellicane MJ, Ciesla JA. Associations between minority stress, depression, and suicidal ideation and attempts in transgender and gender diverse (TGD) individuals: Systematic review and meta-analysis. Clin Psychol Rev. 2022;91:102113. doi: 10.1016/j.cpr.2021.102113 [DOI] [PubMed] [Google Scholar]
- 13.Bockting WO, Miner MH, Swinburne Romine RE, et al. The Transgender Identity Survey: A measure of internalized transphobia. LGBT Health. 2019;7(1):15–27. doi: 10.1089/lgbt.2018.0265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barr SM, Snyder KE, Adelson JL, Budge SL. Posttraumatic stress in the trans community: The roles of anti-transgender bias, non-affirmation, and internalized transphobia. Psychol Sex Orientat Gend Divers. 2022;9(4): 410–421. doi: 10.1037/sgd0000500 [DOI] [Google Scholar]
- 15.Chodzen G, Hidalgo MA, Chen D, Garofalo R. Minority stress actors associated with depression and anxiety among transgender and gender-nonconforming youth. J Adolesc Health. 2019;64(4):467–471. doi: 10.1016/j.jadohealth.2018.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bockting W, Miner MH, Swinburne Romine RE, Hamilton A, Coleman E. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. 2013;103(5):943–951. doi: 10.2105/AJPH.2013.301241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bockting W. The impact of stigma on transgender identity development and mental health. In: Kreukels BPC, Steensma TD, de Vries ALC, eds. Gender Dysphoria and Disorders of Sex Development: Progress in Care and Knowledge. Springer US; 2014:319–330. [Google Scholar]
- 18.Clements ZA, Rostosky SS, McCurry S, Riggle EDB. Piloting a brief intervention to increase positive identity and well-being in transgender and nonbinary individuals. Prof Psychol Res Pr. 2021;52:328–332. doi: 10.1037/pro0000390 [DOI] [Google Scholar]
- 19.Poquiz JL, Shrodes A, Garofalo R, Chen D, Coyne CA. Supporting pride, activism, resiliency, and community: A telemedicine-based group for youth with intersecting gender and racial minority identities. Transgender health. 2021;doi: 10.1089/trgh.2020.0152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Developing Martin S. and evaluating QueerViBE: an online intervention to empower trans and non-binary youth. Anglia Ruskin University; 2019. [Google Scholar]
- 21.Weinhardt LS, Wesp LM, Xie H, et al. Pride Camp: Pilot study of an intervention to develop resilience and self-esteem among LGBTQ youth. Int. J. Equity Health 2021;20(1):150. doi: 10.1186/s12939-021-01488-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Israel T, Matsuno E, Choi AY, et al. Reducing internalized transnegativity: Randomized controlled trial of an online intervention. Psychol Sex Orientat Gend Divers. 2021;8(4):429–439. doi: 10.1037/sgd0000447 [DOI] [Google Scholar]
- 23.Bochicchio L, Reeder K, Aronson L, McTavish C, Stefancic A. Understanding factors associated with suicidality among transgender and gender-diverse identified youth. LGBT Health. 2021;8(4):245–253. doi: 10.1089/lgbt.2019.0338 [DOI] [PubMed] [Google Scholar]
- 24.Olson-Kennedy J, Chan Y-M, Garofalo R, et al. Impact of early medical treatment for transgender youth: Protocol for the longitudinal, observationalTrans Youth Care Study. JMIR Res Protoc. 2019;8(7):e14434. doi: 10.2196/14434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen D, Abrams M, Clark L, et al. Psychosocial characteristics of transgender youth seeking gender-affirming medical treatment: Baseline findings from the Trans Youth Care Study. J Adolesc Health. 2021;68(6):1104–1111. doi: 10.1016/j.jadohealth.2020.07.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuper LE, Mathews S, Lau M. Baseline mental mealth and psychosocial functioning of transgender adolescents seeking gender-affirming hormone therapy. J Dev Behav Pediatr. 2019;40(8):589–596. doi: 10.1097/dbp.0000000000000697 [DOI] [PubMed] [Google Scholar]
- 27.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52(1):30–41. doi: 10.1207/s15327752jpa5201_2 [DOI] [PubMed] [Google Scholar]
- 28.Canty-Mitchell J, Zimet GD. Psychometric properties of the Multidimensional Scale of Perceived Social Support in urban adolescents. Am J Community Psychol. 2000;28(3):391–400. doi: 10.1023/a:1005109522457 [DOI] [PubMed] [Google Scholar]
- 29.Guyer AE, Lau JY, McClure-Tone EB, et al. Amygdala and ventrolateral prefrontal cortex function during anticipated peer evaluation in pediatric social anxiety. Arch Gen Psychiatry. 2008;65(11):1303–12. doi: 10.1001/archpsyc.65.11.1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beck AT, Steer RA, Brown GK. Manual for Beck Depression Inventory-II. Psychological Corporation; 1996. [Google Scholar]
- 31.Hidalgo MA, Petras H, Chen D, Chodzen G. The Gender Minority Stress and Resilience Measure: Psychometric validity of an adolescent extension. Clin Pract Pediatr Psychol. 2019;7(3):278–290. doi: 10.1037/cpp0000297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.IBM SPSS Statistics for Windows. Version 28.0. IBM Corp.; 2021. [Google Scholar]
- 33.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. The Guilford Press; 2013. [Google Scholar]
- 34.Russell CJ, Dean MA. To Log or Not to Log: Bootstrap as an alternative to the parametric estimation of moderation effects in the presence of skewed dependent variables. Organ. Res. Methods 2000;3(2):166–185. doi: 10.1177/109442810032002 [DOI] [Google Scholar]
- 35.Aiken LS, West SG, Reno RR. Multiple regression: Testing and interpreting interactions. Sage; 1991. [Google Scholar]
- 36.Patrician PA. Multiple imputation for missing data. Res Nurs Health. 2002;25(1):76–84. [DOI] [PubMed] [Google Scholar]
- 37.Bauer GR, Scheim AI, Pyne J, Travers R, Hammond R. Intervenable factors associated with suicide risk in transgender persons: a respondent driven sampling study in Ontario, Canada. BMC public health. 2015;15:525. doi: 10.1186/s12889-015-1867-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rood BA, Reisner SL, Puckett JA, Surace FI, Berman AK, Pantalone DW. Internalized transphobia: Exploring perceptions of social messages in transgender and gender-nonconforming adults. Int J Transgend. 2017;18(4):411–426. doi: 10.1080/15532739.2017.1329048 [DOI] [Google Scholar]
- 39.Meyer IH. Resilience in the study of minority stress and health of sexual and gender minorities. Psychol Sex Orientat Gend Divers. 2015;2(3):209–213. doi: 10.1037/sgd0000132 [DOI] [Google Scholar]
- 40.Goffnett J, Routon J, Flores A. The construction of shame and pride: A grounded theory model of identity, emotions, and wellbeing among sexual minority adolescents. Youth Soc. 2021:44118. doi: 10.1177/0044118X211019783 [DOI] [Google Scholar]
- 41.Chavanduka TMD, Gamarel KE, Todd KP, Stephenson R. Responses to the gender minority stress and resilience scales among transgender and nonbinary youth. J LGBT Youth. 2021;18(2):135–154. doi: 10.1080/19361653.2020.1719257 [DOI] [Google Scholar]
- 42.Craig S, Austin A. The AFFIRM open pilot feasibility study: A brief affirmative cognitive behavioral coping skills group intervention for sexual and gender minority youth. Child Youth Serv Rev. 2016;64. doi: 10.1016/j.childyouth.2016.02.022 [DOI] [Google Scholar]
- 43.Austin A, Craig SL, Alessi EJ. Affirmative Cognitive Behavior Therapy with transgender and gender nonconforming adults. Psychiatr. Clin. North Am 2017;40(1):141–156. doi: 10.1016/j.psc.2016.10.003 [DOI] [PubMed] [Google Scholar]
- 44.Toomey RB. Advancing research on minority stress and resilience in trans children and adolescents in the 21st century. Child Dev. Perspect 2021;15(2):96–102. [Google Scholar]
- 45.Hale AE, Chertow SY, Weng Y, Tabuenca A, Aye T. Perceptions of support among transgender and gender-expansive adolescents and their parents. J Adolesc Health. 2021;68(6):1075–1081. doi: 10.1016/j.jadohealth.2020.11.021 [DOI] [PubMed] [Google Scholar]
- 46.Nelson SC, Syed M, Tran A, Hu AW, Lee RM. Pathways to ethnic-racial identity development and psychological adjustment: The differential associations of cultural socialization by parents and peers. Dev Psychol. 2018;54(11):2166–2180. doi: 10.1037/dev0000597 [DOI] [PubMed] [Google Scholar]
- 47.Parker CM, Hirsch JS, Philbin MM, Parker RG. The urgent need for research and interventions to address family-based stigma and discrimination against lesbian, gay, bisexual, transgender, and queer youth. J Adolesc Health. 2018;63(4):383–393. doi: 10.1016/j.jadohealth.2018.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tüzün Z, Başar K, Akgül S. Social connectedness matters: Depression and anxiety in transgender youth during the COVID-19 pandemic. J Sex Med. 2022;19(4):650–660. doi: 10.1016/j.jsxm.2022.01.522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Price-Feeney M, Green AE, Dorison SH. Impact of bathroom discrimination on mental health among transgender and nonbinary youth. J Adolesc Health. 2021;68(6):1142–1147. doi: 10.1016/j.jadohealth.2020.11.001 [DOI] [PubMed] [Google Scholar]
- 50.Barrera E, Millington K, Kremen J. The medical implications of banning transgender youth from sport participation. JAMA Pediatr. 2021;doi: 10.1001/jamapediatrics.2021.4597 [DOI] [PubMed] [Google Scholar]