ABSTRACT
Primary chylopericardium (PC) is a rare entity in the pediatric population with very few reported cases. Most cases of chylopericardium manifest after trauma or following cardiac surgery. The other etiologies which may lead to chylopericardium are malignancy, tuberculosis, or congenital lymphangiomatosis. We report two cases of PC in the pediatric population with contrasting outcomes. Both failed conservative management with dietary modification and octreotide. Surgery with pleuropericardial and pleuroperitoneal windows was performed in both. The first case had a thoracic duct ligation. The first patient died, and the second survived.
Keywords: Chylopericardium, octreotide, pericardial effusion, pericardiocentesis
INTRODUCTION
Primary chylopericardium (PC) is a rare entity in the pediatric population with very few reported cases.[1] Most cases of chylopericardium manifest after trauma or following cardiac surgery. The other etiologies which may lead to chylopericardium are malignancy, tuberculosis, or congenital lymphangiomatosis.[2] We report two such cases and the challenges encountered during the management.
CLINICAL SUMMARY
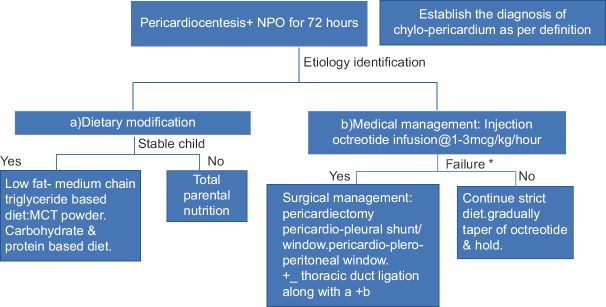
A 2.5-year-old male baby weighing 9.8 kg presented with gradual onset shortness of breath and intermittent cough for 2 weeks. On examination, he was tachypneic and tachycardic and had muffled heart sounds, no murmurs, and decreased breath sounds bilaterally. He had normal inflammatory markers with normal liver, renal, and thyroid profile. Chest X-ray (CXR) showed cardiomegaly [Figure 1a]. Electrocardiogram showed low-voltage QRS complexes. A massive pericardial effusion (PE) with early features of cardiac tamponade was evident on echocardiography [Figure 1b]. Pericardiocentesis aspirated 300 ml of milky white pericardial fluid which was confirmed to be chyle on biochemical and cytological examinations (sugar –134 mg/dl, protein –6.6 g/dl, cholesterol –36 mg/dl, triglyceride –2748 mg/dl, cell count –2300 cells/cumm, and 86% lymphocytes). No microorganisms were isolated from blood or chyle. After 72 h of nil per mouth, the child was initiated with a medium-chain triglyceride (MCT) diet at roughly 80% of total fluid requirement. Octreotide infusion was started from day 7 initially at 3 mcg/kg/h and then gradually increased by 0.5 mcg/kg/h every 24 h to 5 mcg/kg/h, as he kept draining 80–100 ml of chyle per day. Total parenteral nutrition was provided. Albumin infusion was also administered. With no response to conservative management, the child underwent thoracic duct ligation and pericardiopleural window creation by median sternotomy on day 14. Octreotide was tapered off once chyle changed to a serous discharge between day 18 and day 24. There was a further recurrence of drainage of chyle from day 28. On day 35, he underwent total pericardiectomy with creation of pleuroperitoneal window. A histopathologic study of pericardium showed nonspecific pericarditis. The child was difficult to wean off invasive ventilation. Bronchoscopy and lung biopsy were inconclusive. There was failure of response to medical and surgical management, and the child succumbed on day 58 to multiorgan failure secondary to sepsis.
Figure 1.
(a) Chest X-ray suggestive of pericardial effusion in case 1. (b) Echocardiography suggestive of pericardial effusion in case 1. (c) HRCT thorax suggestive of pericardial effusion in case 2. (d) Normal chest X-ray for case 2 in follow-up. HRCT: High resolution computerised tomography
A 13-month-old female child presented with a history of excessive cry and irritability for 7 days. On examination, she was afebrile, tachypneic, and tachycardic with intermittent nasal flaring, intercostal retractions, and muffled heart sounds. CXR showed cardiomegaly. Echocardiography revealed a structurally normal heart with a massive PE with features of early cardiac tamponade. There was no history of trauma, surgery, or family history of a similar condition.
She underwent pericardiocentesis, and 210 ml of milky white fluid was drained. Pericardial fluid analysis revealed glucose –145 mg/dl (blood glucose −160 mg/dl), protein –6 g/dl, cholesterol –11 mg/dl, triglyceride –2303 mg/dl, and cell count –3500 cells/mm3 with 90% lymphocytes and was suggestive of chylopericardium. Gram stain and acid-fast bacillus stain were negative. GeneXpert from the fluid was negative for tuberculosis. Fluid culture did not detect any organism. Sepsis markers were negative. Serum cholesterol was 237 mg/dl (normal <200 mg/dl), LDL –153 mg/dl, and triglyceride –140 mg/dl. Her liver and renal function was normal. High resolution computerised tomography (HRCT) thorax revealed PE [Figure 1c].
The child was initially managed conservatively with fluids and parenteral nutrition. Enteral nutrition with MCT and low-fat diet was commenced after 72 h. She remained hemodynamically stable. Octreotide was commenced at 1 mcg/kg/h from day 3. Over the course of the next 10 days, she had 100–120 ml of chylous fluid aspirated per day despite being on octreotide infusion. As MR lymphangiogram was not feasible in a small child in our setup, we could not rule out lymphangiomatosis.
Pericardiectomy with creation of adequate pericardioperitoneal window was done. Thoracic duct ligation was not done in this second child. Pleural and pericardial chest drains were removed on the 4th postoperative day as the drain output was almost negligible. The child was discharged on the 6th postoperative day with MCT, fat-soluble vitamins, and subcutaneous octreotide injection.
She was followed up regularly with monthly echocardiography and chest X-ray [Figure 1d]. Octreotide was gradually weaned off over the next 3 months. At 12-month follow-up, she is growing well (25th centile for height and weight) and achieving milestones as per age.
DISCUSSION
Chylopericardium is a rare presentation of PE in children. Symptoms vary depending on the extent of involvement, and children may be asymptomatic or present with cough, dyspnea on exertion, chest pain, fatiguability, palpitation, and syncope.[3,4] Chylopericardium can occur due to abnormalities in the lymphatics between the thoracic duct and the pericardium; It can occur due to a. obstruction leading to increased pressure within the thoracic ducts, b. increased permeability of lymphatics, c. ruptured lymphatics or d. vavular incompetence after trauma.[5,6] Diagnosis is on the basis of elevated triglycerides in the fluid 110–2000 mg/dl and cholesterol triglyceride ratio <1 as we saw in our patients.[3]
Treatment is initially conservative. Dietary restriction with a low-fat diet and MCT is provided.[7] We had a similar approach for our patients. The aim is to decrease the formation of lymph and absorption of these nutrients by the portal system bypassing the lymphatics. Medical management involves the use of sympathomimetic drugs such as octreotide which increases smooth muscle contraction and thereby increases lymph drainage. The dose and duration of treatment with octreotide have varied in different case reports. We started with 1 mcg/kg/h and switched over to subcutaneous injection once the second child stabilized after surgery. Medication was stopped 3 months after the surgery for the second case. Surgical approach was planned once dietary modification and octreotide failed to bring any improvement for our patients.
Surgical management involves thoracic duct ligation, pericardiectomy, pericardial windows, and pericardial peritoneal shunt.[1,8] In our first patient, thoracic duct ligation along with pleura-pericardial window did not help; hence, after 2 weeks, pericardiectomy with peritoneal window was created, but the patient succumbed. Our second patient responded well following the creation of pericardioperitoneal window. Surgery was performed as there was no improvement in her clinical condition despite 2 weeks of medical management.[9] She had also lost 500 g of weight before the surgery. Chylous pericardium if left untreated can lead to cardiac tamponade or constrictive pericarditis. Our patients had impending cardiac tamponade. It can also compromise the nutritional and immunological status. Adequate and appropriate nutrition needs to be provided.
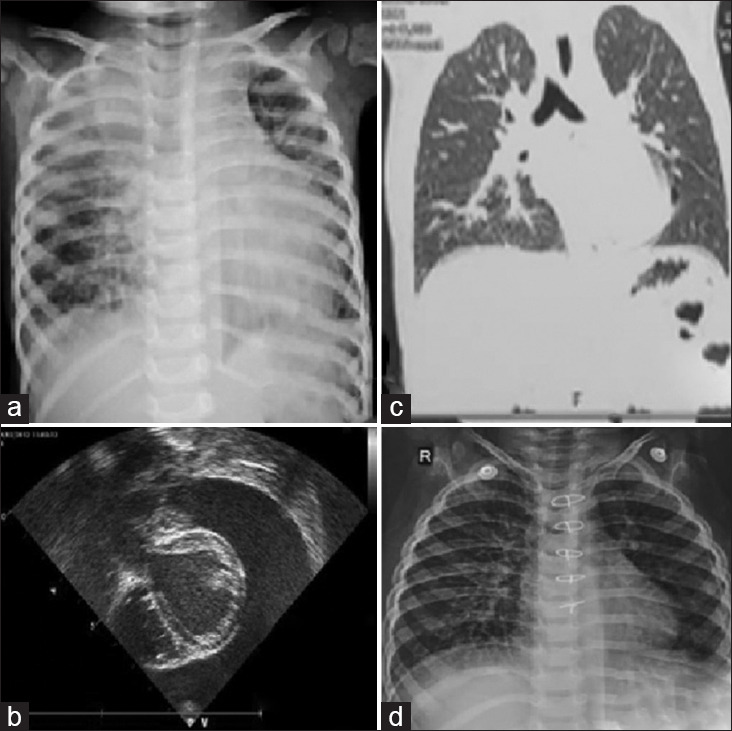
PC is difficult to manage conservatively. Nonsurgical interventions should not be continued beyond 2–3 weeks.[10] Early surgical interventions along with pharmacological therapy and dietary replacement of MCT may be a better option for effective treatment. Prolonged octreotide therapy may be beneficial in high-risk cases to prevent the relapse [Figure 2]. Follow-up is mandatory at serial intervals with echocardiographic assessment.
Figure 2.
Flowchart for approach to a child with primary chylopericardium
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Dr. Saurabhi Das and Dr. Sudipto Bhattacharjya – Department of Pediatric Cardiology, The Mission Hospital, Durgapur; Dr. Mohammad Ali – Department of Pediatric Cardiac Intensive Care, The Mission Hospital; Dr. Uttam Mandal and Dr. Emon Das – Pediatric Cardiac Anesthesia, The Mission Hospital, Durgapur; and Dr. Anil Singhi, pediatric cardiologist, Medica Hospital, Kolkata.
REFERENCES
- 1.Ossiani MH, McCauley RG, Patel HT. Primary idiopathic chylopericardium. Pediatr Radiol. 2003;33:357–9. doi: 10.1007/s00247-003-0885-x. [DOI] [PubMed] [Google Scholar]
- 2.Courtney M, Ayyagari RR. Idiopathic chylopericardium treated by percutaneous thoracic duct embolization after failed surgical thoracic duct ligation. Pediatr Radiol. 2015;45:927–30. doi: 10.1007/s00247-014-3182-y. [DOI] [PubMed] [Google Scholar]
- 3.Mandarry MT, Ru XH, Wei ZQ, Ge MJ. Primary idiopathic chylopericardium: A rare case with a synopsis of the literature. Singapore Med J. 2012;53:e156–8. [PubMed] [Google Scholar]
- 4.Sleilaty G, Rassi I, Alawi A, Jebara VA. Primary isolated chronic chylopericardium. Interact Cardiovasc Thorac Surg. 2002;1:86–7. doi: 10.1016/s1569-9293(02)00061-0. [DOI] [PubMed] [Google Scholar]
- 5.Yüksel M, Yildizeli B, Zonüzi F, Batirel HF. Isolated primary chylopericardium. Eur J Cardiothorac Surg. 1997;12:319–21. doi: 10.1016/s1010-7940(97)00126-7. [DOI] [PubMed] [Google Scholar]
- 6.Gallant TE, Hunziker RJ, Gibson TC. Primary chylopericardium: The role of lymphangiography. AJR Am J Roentgenol. 1977;129:1043–5. doi: 10.2214/ajr.129.6.1043. [DOI] [PubMed] [Google Scholar]
- 7.Machado JD, Suen VM, Marchini JS. Is oral nutritional therapy effective for the treatment of chylothorax?A case report. Nutrition. 2008;24:607–9. doi: 10.1016/j.nut.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Dib C, Tajik AJ, Park S, Kheir ME, Khandieria B, Mookadam F. Chylopericardium in adults: A literature review over the past decade (1996-2006) J Thorac Cardiovasc Surg. 2008;136:650–6. doi: 10.1016/j.jtcvs.2008.03.033. [DOI] [PubMed] [Google Scholar]
- 9.Densupsoontorn NS, Jirapinyo P, Wongarn R, Thamonsiri N, Nana A, Laohaprasitiporn D, et al. Management of chylothorax and chylopericardium in pediatric patients: Experiences at Siriraj hospital, Bangkok. Asia Pac J Clin Nutr. 2005;14:182–7. [PubMed] [Google Scholar]
- 10.Han Z, Li S, Jing H, Liu H. Primary idiopathic chylopericardium: A retrospective case series. BMC Surg. 2015;15:61. doi: 10.1186/s12893-015-0047-8. [DOI] [PMC free article] [PubMed] [Google Scholar]