Abstract
Day-to-day clinical management of patients with inborn errors of immunity, including chronic granulomatous disease (CGD), has been affected by the coronavirus disease-2019 (COVID-19) pandemic. There is a dearth of information on impact of this pandemic on clinical care of children with CGD and psychological profile of the caretakers. Among the 101 patients with CGD followed up in our center, 5 children developed infection/complications associated with COVID-19. Four of these children had a mild clinical course, while 1 child developed features of multisystem inflammatory syndrome in children (MISC) requiring intravenous glucocorticoids. Parents and caretakers of CGD patients (n = 21) and 21 healthy adults with similar ages and genders were also evaluated on the following scales and questionnaires: COVID-19 Fear Scale (FCV 19S), Impact of Event Scale (IES-R), Depression, Anxiety, and Stress Scale (DASS 21), Preventive COVID-19 Behavior Scale (PCV 19BS), and a “COVID-19 Psychological wellbeing questionnaire.” Median age of the parents/caregivers was 41.76 years (range: 28–60 years). Male:female ratio was 2:1. In the study group, 71.4% had higher IES scores compared to 14.3% in controls. The caregivers had a high prevalence of stress, anxiety, avoidance behavior, and depression compared to controls (p < 0.001). Children with CGD have had predominantly mild infection with COVID-19; however, caregivers/parents of these children were at risk of developing psychological distress. The COVID-19 pandemic has brought to light the importance of patients’ and caretakers’ mental health which needs periodic assessment and appropriate interventions.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10875-023-01524-5.
Keywords: COVID-19, Chronic granulomatous disease, Psychosocial profile, Caregiver, India
Introduction
Since its emergence in December 2019, the coronavirus disease-2019 (COVID-19) has rapidly spread over the entire world and has led to unprecedented repercussions on physical and mental health across ethnicities [1–3]. Nearly 760 million people have been affected until date with cumulative deaths of approximately 6.8 million, and a case fatality rate of 2.5 [4]. The high transmission risk and mortality rates have led many countries to impose nation-wide lockdowns and shutdown of state borders, closure of schools and various institutions, restriction of social gatherings, and solitary confinement of both healthy and affected individuals to contain the spread of the disease [5]. The Government of India, in particular, imposed a nation-wide lockdown on 25th March 2020 affecting the movement of nearly 1.4 billion people [5]. Such measures, although necessary, have made a significant detrimental impact on the psychosocial milieu of every individual across the globe [1–3, 5]. Various authors have reported a surge in intensity of anxiety, depression, and stress among every stratum of the population during this pandemic with the frequency of abnormal psychological impact ranging from 15 to 75% [2, 3, 6–8]. In particular, the lower and middle socio-economic classes have had a harrowing time because of lack of earning opportunities and inability to access healthcare facilities. These factors have compounded features of emotional lability, anxiety, stress, depression, and even post-traumatic stress symptoms, especially in caregivers who are looking after children with chronic diseases such as inborn errors of immunity (IEI) [9–11].
Among the IEIs, chronic granulomatous disease (CGD) belongs to the group of phagocytic disorders that is associated with defective respiratory burst of phagocytes [12, 13]. These children frequently receive hematopoietic stem cell transplantation (HSCT) in Western hospitals, but due to financial limitations, the majority of them in India only receive prophylactic antimicrobials [14–16]. Accessing appropriate care for these children has been made more difficult due to the pandemic. Parents were filled with uncertainty, anxiety, and fear, especially in light of their child’s potential exposure to the coronavirus, and their situation was made more difficult by the shift to telemedicine and online care [17].
In general, only a few studies have explored psychological comorbidities in caregivers of children with IEIs (Table 1) [9, 11, 13, 18–22]. Most of these studies, however, have reported higher incidence of psychological comorbidities in both patients and their caregivers in IEIs as a whole (Table 1). To the best of our knowledge, no study has explored the impact of COVID-19 on clinical care and psychological profile in parents/caregivers of CGD.
Table 1.
Previous studies describing psychological profile of patients/caregivers with CGD
| Author, country, year (reference) | Total number of CGD patients/families [total patients with PID] | Median age of participants with CGD (years) [range] | Psychosocial scales/outcome measures used | Determination of impact of COVID-19 pandemic | Remarks |
|---|---|---|---|---|---|
| Cole et al., UK, 2013 [18] | 73/47 § | §§ |
PedsQL SDQ |
Not applicable | Patients and caregivers/parents of children with CGD have lower quality of life and poor emotional health; however, those who undergo HSCT have comparable emotional health to healthy controls |
| Battersby et al., UK, 2019 [19] | 75/62* [75] | 43 [3–77] |
SF-36 V2 HADS |
Not applicable |
All XL-CGD carriers had reduced quality of life Among XL-CGD carriers, 26/61 and 5/61 reported moderate-to-severe anxiety and depression respectively Higher anxiety scores were directly proportional to depression scores, low self-esteem, presence of arthritis or bowel disease, and increased fatigue |
| Pulvirenti et al., Italy, 2019 [13] | 47/47 [47] |
7.3 ± 4.4** 27.6 ± 8.0*** |
PedsQL SDQ SF-12 |
Not applicable |
Children with CGD reported more problems in social/school areas, peer relationship, and conduct/emotional problems as compared to controls Adults with CGD also reported higher difficulties both in mental and physical domains as compared to controls No significant difference was noted between patients who underwent HSCT versus those who did not |
| Deshpande et al., USA, 2020 [20] | NA [565] # | NA | PROMIS | Yes |
Of the 565 patients with PIDs, 543 (96%) had primary antibody defects Nearly 63% (359/565) patients with PIDs had issues with accessing healthcare during COVID-19 pandemic Mean PROMIS global physical (39.6) and mental health scores (43.5) were reduced as compared to the national population Patients who had healthcare access problems more commonly reported a moderate-to-severe negative impact on their physical and mental health vs those without access issues |
| Sowers et al., USA, 2021 [11] | 1/1 [511] | NA | Questionnaire (Qualtrics survey platform) | Yes |
< 2% of patients with PID reported positivity for COVID-19 infection About 30.9% (n = 158) were “extremely concerned” with the possibility that their ward or family member would contract COVID-19 infection and 16.8% (n = 86) reported disruption of daily activity due to COVID-19 Nearly half (n = 292) reported that they were “mostly isolated” during the pandemic About 56.6% (n = 289) utilized telemedicine to contact primary physician managing their ward with PID |
| Manusama et al., Netherlands, 2022 [21] | 1/1 [176] | NA | 4-DSQ | No | Patients with PIDs had more numbers of “moderate” and “high” scores in all 4 domains, i.e., distress (33.9% vs 16.3%), depression (18.6% vs 5.7%), anxiety (22.4% vs 8%), and somatization (36.2% vs 11.2%) as compared to controls |
| Meelad et al., Malaysia, 2022 [22] | 1/1 [10] | 19 | Semi-structured interview | No | Parents/caregivers had concerns on 5 thematic aspects: (1) living with fear and anxiety; (2) struggles of PID healthcare system; (3) knowledge about disease; (4) social constraint; and (5) coping |
| Akdag ˘ et al., Turkey, 2022 [9] | 0/0 [65] | NA |
GAD-7 PTSD checklist civilian version |
Yes |
Parents/caregivers of patients with PID reported higher rates of moderate-to-severe anxiety in comparison to parents with healthy children (67.7% vs 32.1%) PTSD checklist civilian scores were also higher in parents/caregivers of patients with PID (p < 0.05) |
CGD, chronic granulomatous disease; COVID-19, coronavirus disease-2019; PedsQL, Pediatric Quality of Life Inventory; SDQ, Strengths and Difficulties questionnaire; HSCT, hematopoietic stem cell transplantation; SF-36 V2, Medical Outcomes Study Short Form 36 version 2; HADS, Hospital Anxiety and Depression Scale; SF-12, 12-item Short Form health survey; PROMIS, Patient-reported Outcomes Measurement Information System; PID, primary immunodeficiency disorder; 4-DSQ, 4-Dimensional Symptom Questionnaire; GAD-7, generalized anxiety disorder 7-item; PTSD, post-traumatic stress disorder; NA, not available
§Forty-seven and 42 parents completed PedsQL and SDQ questionnaires, respectively, and 35 children completed self-report PedsQL questionnaires
§§In the group where parents completed PedsQL, median age was 9 years ((range 3–15) for non-HSCT) and 10 years ((range 4–14 years) for post-HSCT). In the group where children completed PedsQL, median age was 10 years (range 5–15) for both non-HSCT and post-HSCT. In the group where parents completed SDQ, median age was 9 years for non-HSCT and 10 years for post-HSCT
*X-linked carriers of CGD: 75
**Mean age of pediatric patients
***Mean age of adult patients
#Total no. of patients with primary immunodeficiencies: 565
The present study aimed at elucidating the difficulties and psychological status of caregivers of children with CGD during the COVID-19 pandemic, from the perspective of a developing country. We also report the clinical manifestations of COVID-19 infection and its resultant complications in our cohort of CGD from North India.
Methodology
We retrieved the medical records of children with CGD who were followed up at Pediatric Immunodeficiency Clinic of the Advanced Pediatrics Center, Post Graduate Institute of Medical Education and Research, Chandigarh, India, and had COVID-19 infections or its complications. The diagnosis of CGD was based on diagnosis according to the revised European Society of Immunodeficiencies (ESID) registry [23].
We designed a “COVID-19 Psychological wellbeing questionnaire” based on the Impact of Event Scale (IES-R); Depression, Anxiety, and Stress Scale (DASS 21); Fear of COVID-19 Scale (FCV 19S); and Preventive COVID-19 Behavior Scale (PCV 19BS). Written and verbal consent were sought prior to assessment. Only those parents/caregivers who gave informed consent and understood/answered all sections of the questionnaire were recruited in the present study. After initial screening, the responses of 21 parents/caregivers of patients with CGD and 21 age- and gender-matched adults who fulfilled the abovementioned criteria were assessed at the end of the study.
Parents/caregivers were assessed personally or telephonically by a trained psychologist or senior resident (post-doctoral fellow) on study measures. The study was approved by our Institute’s Ethics Committee (No:INT/IEC/2022/SPL-51). Parents/caregivers of patients with CGD were assessed on the following measures.
The Impact of Event Scale (IES-R)
The original scale was a 15-item self-reported measure developed in 1979 to assess subjective distress caused by traumatic events [24]. Revision of this scale was done by Weiss and Marmar in 2007 [25], and distress was assessed on 3 dimensions: intrusion, avoidance, and hyperarousal. To explore the level of distress, participants were asked to remember stressful life event (COVID-19 pandemic) and report their level of distress. Total score of IES-R ranges between 0 and 88 (0–23: no impact; 24–32: clinical concern for post-traumatic stress disorder (PTSD); 33–37: probable diagnosis of PTSD; and 37–88: high enough to suppress immune system’s functioning, even 10 years after an impact event) [26]. Cut-off score for the scale was 24 and higher scores were indicative of higher distress. The scale had good psychometric properties (Cronbach’s alpha 0.79 to 0.91) with test–retest reliability of 0.89 to 0.94.
Depression, Anxiety, and Stress Scale (DASS 21)
This scale was used to measure distress along three axes of stress, anxiety, and depression [27]. It had 21 items (7 items for each component of stress, anxiety, depression) and all items of the scale were rated on a 4-point Likert scale (0 = did not apply to me at all, 1 = applied to me sometimes, 3 = applied to me most of the times). For the present study, total scores of DASS21 were multiplied by two to get scores equivalent to original DASS 42 scale [28]. There were cut-off scores for each domain to assess the severity of stress, anxiety, and depression. Cronbach’s alpha coefficient, for the entire scale, was 0.83, and for depression, anxiety, and stress were 0.83, 0.85, and 0.80, respectively.
Fear of COVID-19 Scale (FCV 19S)
This was a 7-item scale to measure affective and physiological aspects of fear [29]. Items were rated on a 5-point Likert scale. Minimum score was 1 and maximum score was 5 for each item, and total score ranged from 7 to 35 with higher scores reflecting higher fear. The present scale had good psychometric properties with internal consistency of 0.82 and test–retest reliability of 0.72, and good concurrent validity. Cronbach’s alphas were 0.82 for affective response, and 0.86 for physiological response [30].
Preventive COVID-19 Behavior Scale (PCV19BS)
Preventive behavior during the COVID-19 pandemic was assessed by using PCV as per World Health Organization (WHO) guidelines, i.e., washing hands, respiratory hygiene, staying at home and maintaining social distancing, etc. [31]. The present scale consisted of 9 domains and items of the scale were rated on a 5-point Likert scale. Overall score was derived from summed up scores of all the items. Higher the score, greater is the adherence towards preventive behavior.
Statistical Analysis
The data obtained was transferred to a Google Excel sheet and analyzed by using Statistical Package for Social Science (SPSS) version 28 (IBM SPSS Statistics, New York, USA). Descriptive data was analyzed by using frequency distribution, percentage, and median. IQR and comparison between different categories were done with the chi-square test/Ficher’s exact test and Kruskal–Wallis test with post hoc analysis. Spearman’s co-relation coefficient was used to explore the association between clinical measures and socio-demographic variables.
Psychological Wellbeing COVID Questionnaire
As the pandemic had a great impact on mental health of caregivers of children with chronic diseases, thus, a specially designed questionnaire was formulated to assess subjective experiences of parents of children with CGD during the COVID-19 pandemic. The questionnaire was administered on 21 caregivers’ children with CGD, and content and face validity of the scale was assessed by 2 pediatric immunologists, 2 senior residents in pediatric clinical immunology and rheumatology, and 1 child psychologist. Subjective experiences were recorded on a Likert scale (not at all = 0; a little bit = 1; moderately = 2; quite a bit = 3; extremely = 4) (Suppl. table 1).
Results
Among the 101 patients with CGD, 5 children developed infection/complications associated with COVID-19. A 15-year-old child with NCF1 mutation had mild fever and influenza-like illness. On investigation, he was noted to be COVID-19 positive; however, he became well after 5 days with routine supportive care. Another 2 siblings [18-year-old girl and 15-year-old boy] with NCF1 mutation had features of cough, nasal discharge, and anosmia. All of their family members had similar features, and were found to be COVID-19 positive. Children of both these families had a mild phenotype and were managed conservatively.
A 4-year-old boy with CYBB mutation presented with fever, mild cough, and cervical lymphadenitis (Staphylococcus aureus). During routine evaluation, he was found to be COVID-19 positive. He was treated with intravenous antibiotics for 2 weeks, following which his symptoms resolved.
Another 10-year-old boy with NCF2 mutation had a difficult course with COVID-19. He had initially presented with an acute febrile illness with a gastrointestinal focus of infection. Within 48 h, he developed myocardial dysfunction, coagulopathy, and laboratory features suggestive of hemophagocytic lymphohistiocytosis. On reviewing his history, it was noted that 4 weeks back, he had come in contact with one of his neighbors who was COVID-19 positive. Further investigation revealed elevated titers of antibodies against spike protein of COVID-19. A diagnosis of multisystem inflammatory syndrome in children (MIS-C) was made and methylprednisolone (30 mg/kg/day) was initiated, and given for 3 days. He responded within 24 h and was subsequently discharged on tapering doses of oral steroid. He remains well on follow-up.
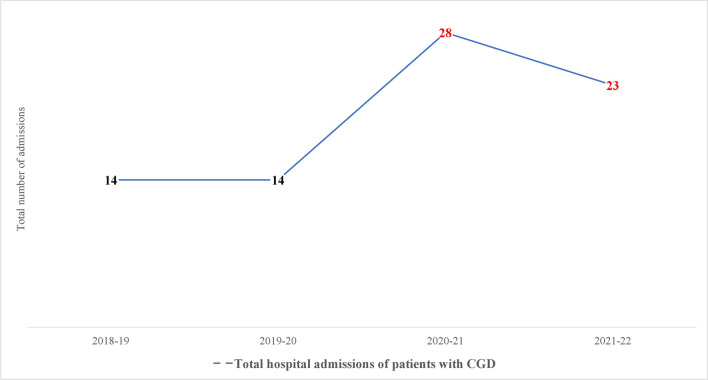
We also observed that the rate of hospital-admission of patients with CGD increased during the COVID-19 pandemic as compared to pre-COVID-19 era (Fig. 1). The likely cause of this increase in hospital admissions was that parents of children with CGD had heightened experiences of uncertainty and worry as well as fears, in the context of their child’s rare chronic illness. In addition, most caregivers felt that they were more comfortable with the primary doctor (at Chandigarh) managing and treating their children, irrespective of whether their children were afflicted with COVID-19 or otherwise.
Fig. 1.
Total number of hospital admissions of patients with CGD before and during COVID-19 pandemic
The COVID-19 psychological wellbeing questionnaire was assessed in parents/caregivers of 21 children diagnosed with CGD and compared with 21 age- and gender-matched adults from general population (control group). Except for the child who developed MIS-C, all other children had contracted COVID-19 infection after their parents/caregivers had answered the COVID-19 psychological wellbeing questionnaire. None of the children had received COVID-19 vaccines before the commencement of the present study. The median age of the parents/caregivers was 41.76 years (range: 28–60 years). Male:female ratio was 2:1. Among the study group, majority of caregivers had attained intermediate-level education (61.9%), 52.4% were earning ≤ 238 US dollars per month, 42.9% belonged to lower-middle socio-economic status (SES), and approximately half (52.4%) were living in joint families in urban locality. Among the control group, about half of the participants (52.4%) were graduates, 47.6% were earning ≥ 475 US dollars, 57.1% were from upper-middle SES, and 76.2% were living in urban locality (and 57.1% living in nuclear families) (Table 2).
Table 2.
Demographic description of the participants
| Demographic parameters | Group 1 (N = 21) Caregivers of children with CGD |
Group 2 (N = 21) Healthy adults |
|
|---|---|---|---|
|
Age (in years) Range |
41.76 ± 7.90 (28–60 years) |
41.76 ± 7.90 (28–60 years) |
|
| Age range |
≤ 40 years ≥ 40 years |
9 (42.9) 12 (57.1) |
9 (42.9) 12 (57.1) |
| Gender |
Male Female |
28 (66.7%) 14 (33.3%) |
28 (66.7%) 14 (33.3%) |
| Education | |||
|
Intermediate Graduate/postgraduate/doctorate |
13 (61.9%) 8 (38.1%) |
10 (47.6%) 11 (52.4%) |
|
| Occupation | |||
| Elementary occupation/house makers |
9 (42.9%) 9 (42.9%) |
5 (23.8%) 4 (19.0%) |
|
|
Skilled/semiskilled/agriculture/shop Clerical/ministerial staff Associate professional/professional |
2 (9.4%) 1 (4.8%) |
5 (23.8%) 7 (33.4%) |
|
| Family income (in rupees) | |||
|
≤ 238 US dollars 239–474 US dollars ≥ 475 US dollars |
11 (52.4%) 7 (33.3%) 3 (14.3%) |
3 (14.3%) 8 (38.1%) 10 (47.6%) |
|
| Socio-economic status (SES) | |||
|
Upper lower Lower middle Upper middle Upper |
6 (28.6%) 9 (42.9%) 6 (28.6%) 0 (0%) |
4 (19.0%) 1 (4.8%) 12 (57.1%) 4 (19.0%) |
|
| Family type |
Nuclear Joint |
10 (47.6%) 11 (52.4%) |
12 (57.1%) 9 (42.9%) |
| Locality |
Urban Rural |
11 (52.4%) 10 (47.6%) |
16 (76.2%) 5 (23.8%) |
Perception of Caregivers
Among the caregivers, 38.1% reported that their children were admitted during study period. About 66% were in favor of their wards ( 18 years of age) getting COVID-19 vaccination. Caregivers of 28.6% children were concerned that their children were more vulnerable of getting infection during pandemic lockdown because of underlying CGD. However, only 4.8% reported lapse in compliance to therapy (prophylactic antimicrobials-cotrimoxazole/itraconazole) because of inability to procure drugs due to lockdown. Majority of them (71.4%) tried to contact their treating doctor at the time of crisis/disease flare, and 47.6% were on regular follow-up for treatment of their children. About one-fourth of caregivers (23.8%) were worried that their children may not be able to get adequate medical assistance for worsening disease parameters because of lockdown.
Impact of COVID-19 on Mental Health of Participants
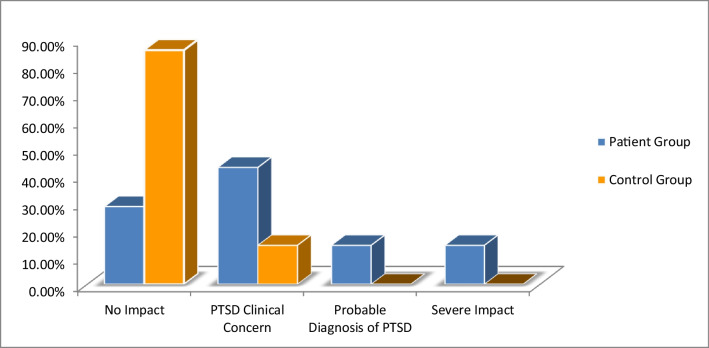
Negative experiences of the participants were assessed by using IES-R and we found that avoidance behavior was the most prevalent behavior exhibited by the parents/caregivers of children with CGD, followed by dissociative and “similar to flashbacks experiences” (avoidance) than the control group (p < 0.001) (Table 3). Majority of participants in the study group (71.40%) also had higher scores (IES Score ≥ 23) signifying notable distress. In addition, 42.9% of participants showed some symptoms of PTSD, and 14.3% of them may probably fit into a diagnosis of PTSD (Fig. 2 and Suppl. Figure 1).
Table 3.
Comparative scores of participants on various clinical measures
| Variables | Group 1 (n = 21) Caregivers of children with CGD Median (IQR) |
Group 2 (n = 21) Healthy adults Median (IQR) |
K Wallis | P value |
|---|---|---|---|---|
| The Impact of Event Scale (IES-R) | ||||
| Intrusion | 9.00 (6.00) | 3.00 (6.00) | 15.129 | < 0.001 |
| Avoidance | 12.00 (3.00) | 4.00 (9.00) | 17.007 | < 0.001 |
| Hyper arousal | 7.00 (6.00) | 1.00 (4.50) | 15.606 | < 0.001 |
| Total IES | 26.00 (9.50) | 10.00 (17.00) | 18.878 | < 0.001 |
| Depression, Anxiety, and Stress Scale (DASS 21) | ||||
| Stress | 12.00 (10.50) | 8.00 (5.00) | 1.674 | 0.196 |
| Anxiety | 8.00 (5.00) | 4.00 (6.00) | 5.565 | 0.018 |
| Depression | 8.00 (6.00) | 6.00 (4.00) | 5.009 | 0.025 |
| Fear of COVID-19 Scale (FCV 19S) | ||||
| Emotional fear reaction | 11.00 (9.00) | 7.00 (3.50) | 2.157 | 0.142 |
| Expressional fear | 7.00 (3.00) | 4.00 (2.50) | 1.911 | < 0.001 |
| Total FCV | 17.00 (7.50) | 12 (3.50) | 11.203 | 0.001 |
| Preventive COVID-19 Behavior Scale (PCV19BS) | ||||
| Preventive behavior | 41.00 (6.00) | 39.00 (3.50) | 5.356 | 0.021 |
Fig. 2.
Severity of impact of COVID-19 event among the caregivers group and control group participants
Stress, Anxiety, and Depression
Parents/caregivers of children with CGD experienced significant higher distress related to the COVID-19 pandemic. In comparison to the control group, the study group showed significantly more distress in terms of anxiety (p-0.018) and depression (p-0.025) (Table 3). About half (47.6%) of them experienced mild stress, about one-fourth (23.8%) experienced moderate anxiety, and 14.3% showed mild to moderate symptoms of depression. Among the control group, 9.5% experienced mild stress, 14.3% exhibited anxiety symptoms, and only 4.8% had depressive symptoms (Suppl. Figure 2).
Fear of COVID-19 and Preventive Behaviors During Pandemic
Fear of the COVID-19 pandemic had great impact on mental health and wellbeing of everyone, especially on patients with chronic illness and on their caregivers as well. Groupwise comparison revealed that parents/caregivers of children with CGD exhibited significantly higher COVID-19-related fears during the pandemic (p < 0.001). On expressional fear reaction dimensions of FCV 19S, study group participants scored significantly higher than their counterparts (p < 0.001) and no significant difference was observed on affective dimension. They were also following more preventive behaviors than controls (p-0.021) (Table 3).
Correlation Analysis Between Psychosocial Variables
Results of correlation analysis revealed that overall distress had significant positive association with stress (p-0.010), depression (p-0.026), overall fear of COVID-19 (p-0.018), and preventive behaviors (p-0.001). Similar associations were observed in all dimensions of IES, intrusion, avoidance, and hyper arousal behaviors. Stress also had significant association with emotional expression of fear (p-0.004) and overall fear of COVID-19 (p-0.014), anxiety with emotional fear reaction (p-0.031), and overall FCV (p-0.017). Preventive behaviors also had significant positive associations with emotional expression of fear (p-0.001) and overall FCV (p-0.045) (Table 4).
Table 4.
Association between distress (IES) and stress, anxiety, depression (DASS 21), and Fear of COVID scale (FCS) and Preventive Behavior Scale (PCS) among the caregivers of children with chronic granulomatous disease
| ST | ANX | DEP | FCV I | FCV II | FCV total | PCV | |
|---|---|---|---|---|---|---|---|
| Intrusion (IES I) | .395** | – | .343* | – | .663** | .363* | .486** |
| Avoidance (IES II) | .418** | .407** | – | – | .516** | .450** | .317* |
| Hyper arousal (IES III) | .451** | – | .312* | – | .580** | .259 | .409** |
| Total IES | .469** | – | .358* | – | .624** | .393* | .443** |
| STR | .306* | – | – | .434** | .371 | – | |
| ANX | – | .334* | – | .367* | – | ||
| FCV I | – | .811** | – | ||||
| FCV II | .603** | .502** | |||||
| FCV total | .311* |
*Significant at 0.005. **Significant at 0.001
IES Impact of Event Scale, IES I: intrusion, IES II: avoidance, IES III: hyper arousal; DASS Depression, Anxiety, Stress Scale, STR stress, ANX anxiety, FCV Fear of COVID, FCV I: emotional fear reaction, FCV II: expressional fear, PCV Preventive Behavior Scale
Association Between Socio-demographic and Psycho-social Variables
Association between socio-demographic profile and clinical variables was also explored. Significant negative association was observed among gender, education, occupation, income and SES and distress, fear of COVID-19, and preventive behaviors. Parents’ occupation was significantly associated with intrusion, hyper arousal and overall distress, depression, fear of COVID-19, and preventive behaviors. Males were more stressed than female caregivers (male mean rank: 24.14; female mean rank: 16.21; p-0.046), and participants having intermediate-level education were more stressed than graduate/post graduates (intermediate: mean rank 25.20; graduate/post-graduate: mean rank 17.03; p-0.030).
Parents/caregivers with elementary occupation were significantly more distressed in terms of dissociative experiences (p-0.011), hyper-arousal (p-0.019), and fear of COVID-19 (p-0.028), and followed more preventive behaviors (p-0.046) than those with skilled profession. Income had a negative association with distress with participants earning less (≤ 238 US dollars per/month) being significantly more distressed than parents earning more (p-0.002). Similarly, participants belonging to lower-middle income group were more distressed than upper-middle/upper income group participants (p-0.015) and fear of COVID-19 (p-0.016) (Table 5 and Suppl. table 2).
Table 5.
Association between psychological and socio-demographic variables
| IES I | IES II | IES III | IES total | STR | DEP | FCV II | PCV | |
|---|---|---|---|---|---|---|---|---|
| – | – | – | – | -.326* | – | – | – | |
| Education | – | -.350* | -.437** | -.360* | -.357* | – | – | – |
| Occupation | -.436** | – | -.481** | -.406** | – | -.409** | -.314* | -.215 |
| Income | -.537** | -.463** | -.611** | -.568** | -.537** | -.505** | -.401** | -.322* |
| SES | -.502** | -.370* | -.584** | -.514** | -.434** | -.418** | -.351* | -.295 |
*Significant at 0.005. **Significant at 0.001
IES Impact of Event Scale, IES I: intrusion, IES II: avoidance, IES III: hyper arousal; DASS Depression, Anxiety, Stress Scale (DASS), STR stress, DEP depression, FCV Fear of COVID, FCV II: expressional fear, PCV Preventive Behavior Scale, SES Socio-economic scale
Predictors of Distress
To explore the impact of COVID-19 impact (distress), we used linear regression analysis, where demographic and clinical variables were considered as independent variables. Results of regression analysis revealed that income, fear of COVID-19, and preventive behaviors jointly contributed 47% in accounting the variance among participants (R = 0.47, F = 19.157, p < 0.001) (Suppl. table 3).
Discussion
At the emergence of the COVID-19 pandemic, it was predicted that presence of an IEI could be an added risk factor in contracting moderate to severe COVID-19 (312). However, with increasing knowledge about the immunopathogenesis of COVID-19, it has been observed that most patients with IEIs have had a mild clinical course [33, 34] (Suppl. table 4). Only certain subsets of IEIs such as combined immunodeficiencies, especially those involving the T-cell compartment, type-Ι interferon pathway dysregulation defects, and primary antibody defects such as common variable immunodeficiency, were more predisposed towards developing severe infection [35–38] (Suppl. table 4). A similar mild clinical course of COVID-19 infection has also been reported in CGD [33–38]. It has been hypothesized that defective respiratory burst and impaired neutrophil extracellular trap formation in CGD may prevent exaggerated lung tissue damage seen in severe COVID-19 infection, and probably has led to better outcomes in this subset of IEIs [39]. Nevertheless, complications including mortalities have also been reported in certain studies [40–42]. Castano‐Jaramillo et al. reported a fatal MIS-C-like illness in a 16-year-old boy with CYBB mutation [41]. A similar report of MIS-C in CGD (with CYBB mutation) was published by Chou et al. who described a 16-year-old boy with acute febrile illness with a gastrointestinal focus of infection [42]. In the present study, our child with NCF2 mutation had similar clinical features, and he showed a rapid clinical response after methylprednisolone therapy. Whether the underlying genetic defect in CGD plays a part in development, pathogenesis and consequent treatment of MIS-C remain speculative. With a few exceptions, most children with CGD, overall, have had essentially a mild clinical course with COVID-19 and have responded well to conventional supportive care.
Although the clinical manifestations of COVID-19 in children with CGD were mild, parents/caregivers underwent significant psychological distress, especially during the nation-wide lockdown and subsequent “waves” that ravaged the country. About one-fourth of caregivers were concerned that their children may be more vulnerable to COVID-19 due to their underlying disease and/or may not get necessary assistance during disease flare in the lockdown period. However, nearly three-fourth (71.4%) of caregivers were able to contact their treating doctor during times of crisis/disease flare, and about one-half (47.6%) were on regular follow-up with their primary physician through telemedicine and social media platforms such as “WhatsApp.” It was also noted that all parents/caregivers were more inclined towards admitting their children at their primary Hospital (at Chandigarh) for any observed flare or disease worsening. Mustafa et al. reported that in their Allergy/Immunology Clinic, patient satisfaction was comparable in both the in-person and video/telephonic consultation groups during the pandemic [43]. Most studies concur that by discussion and dissemination of appropriate information by primary care physicians may go a long way in quelling “emotional burden” of patients with chronic diseases, and ensure compliance to therapy [1–3]. This is also highlighted in the present study where > 95% caregivers reported compliance to therapy (that included prophylactic antimicrobials-cotrimoxazole/itraconazole) despite major logistical issues during the lockdown.
There were also psychological concerns related to COVID-19 vaccination. Population-based studies from China observed that “fake news” and “false information” regarding efficacy and side-effects related to vaccines were responsible for adverse psychological stress in the general public [44, 45]. Authors reported that other family members’ experiences with vaccination played a positive role in ameliorating an individual’s psychosocial stress [45]. The Indian Government published recommendations to vaccinate children from 1st January, 2022 onwards [46]. None of the children in our cohort had received any COVID-19 vaccines before the commencement of the present study. Once the recommendations and the vaccines were made available, about one-third of parents/caregivers were hesitant in advocating vaccination for their eligible children. However, with presentation of accurate information about the pros and cons of COVID-19 vaccines through telemedicine by the treating doctor, the anxiety concerns regarding vaccination were mitigated.
The current study used the following scales/outcome measures to determine the psychological impact of COVID-19 on caregivers/parents of CGD: IES-R, DASS 21, FCV 19S, and PCV 19 BS. It appeared that negative experiences, especially “avoidance behavior,” of participants were significantly increased in parents/caregivers of children with CGD, and 60% of them had certain features of PTSD. This also translated into significantly increased stress (61.8% vs 9.5%), moderate-to severe anxiety (33.3% vs 14.3%), and depression (14.3% vs 4.8%) in comparison to controls. Although there is no available literature on psychosocial and behavioral profile of caregivers/parents of children with CGD vis-à-vis COVID-19, these findings are comparable to other IEIs such as primary antibody defects [9–11, 20]. One of the first studies to describe the quality of life in CGD was, however, reported from the UK in 2013 [18]. Authors observed that patients with CGD who were managed with conservative therapy (prophylactic antimicrobials) were likely to have a disturbed psychological milieu as compared to those who underwent HSCT. Another study from Italy did not find such an association between patients who underwent HSCT versus those who did not [13]. However, both these studies were conducted before the emergence of COVID-19 and as such, these associations need further investigation. In the present study, 1 patient underwent HSCT prior to the onset of the pandemic, and his parents’ psychological profile was similar to the parents whose children were being managed with antimicrobial prophylaxis.
The FCV 19S and PCV 19 BS scores were 7 for “expressional fear reaction” and 41, respectively, and these scores were significantly increased in the study group as compared to controls. The high score of FCV 19S likely translated into parents/caregivers resorting to COVID-19 preventive measures such as frequent handwashing, maintaining social distance, avoiding large gatherings, and wearing masks. We also investigated any association between socio-demographic profile and clinical variables. It was noted that there was significant negative association among gender, education, occupation, income and SES with overall distress, fear of COVID-19, and preventive behaviors. Males were more stressed than female caregivers (male: mean rank: 24.14; female mean rank: 16.21; p 0.046). This is in contrast to Western literature where mothers with children who had IEIs were noted to have more psychological distress [9, 11]. This may partially be explained by the fact that in Asian (including Indian subcontinent) culture, fathers are the primary breadwinners and contribute to decisions that determine the health and other socio-economic parameters of a family [47–49]. In addition, the COVID-19 pandemic heralded unanticipated “lockdowns” and subsequent restriction of earning opportunities, and further compounded the psychological distress of caregivers, especially fathers [7]. It is also interesting to note that participants having intermediate-level education, elementary occupation, and low-income were more stressed than those who were graduate/post graduates or those who were skilled professionals and had a higher income. This again underscores the need for case-based psychosocial interventions through psychoeducation, cognitive behavioral therapy, counselling, and family therapy. Further exploration of these parameters in larger cohorts and other IEIs is needed from the point of view of a developing nation such as India.
The present study underlines that psychological distress, especially in the context of COVID-19, may hinder caregivers/parents’ care towards their wards, and as such, counselling and psychological interventions may be needed to ensure good quality of life. Appropriate use of telemedicine and dissemination of correct information may reduce distress in patients as well as their caregivers/parents.
The strength of this study was that this was the largest cohort of caregivers/parents with CGD from India, wherein the psychosocial profile was explored with respect to the COVID-19 pandemic. However, some limitations include the cross-sectional nature of the study and absence of psychological data of caregivers/parents before the onset of the pandemic, and the recall methods wherein caregivers/parents were asked about their mental status during the lockdown and subsequent waves of the pandemic.
Conclusion
Children with CGD have had predominantly mild infection with COVID-19 and have responded favorably to conventional supportive care and treatment. However, caregivers/parents of these children are at risk of developing psychological distress. Scores for stress, anxiety, and distress were significantly elevated in this group as compared to controls. The COVID-19 pandemic has unmasked the lacunae in taking into consideration the mental health of caregivers/parents with CGD. This pandemic has also underscored the utility of telemedicine and social media during the “lockdown” to address the non-urgent medical needs of patients. Timely recognition of the psychosocial concerns is essential for identifying personalized psychological support to the affected families. Future studies should evaluate psychological interventions such as psychoeducation, cognitive behavioral therapy, counselling, and family therapy with a larger sample size in patients with CGD and their caregivers/parents.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We acknowledge the support from patients and caregivers of affected families with chronic granulomatous disease who are followed up at our center.
Author Contribution
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Rajni Sharma, Prabal Barman, and Sanjib Mondal. The first draft of the manuscript was written by Rajni Sharma and Prabal Barman, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics
This study was performed in line with the principles of the Declaration of Helsinki. The intramural Ethics Committee of the Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India, approved the study protocol (No:INT/IEC/2022/SPL-51). The Departmental Review Board of the Advanced Pediatrics Centre, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India, approved this manuscript (No. 17–23, dt. 14.03.2023).
Consent to Participate
Informed consent was obtained from the parents of the child included in this report.
Consent for Publication
All authors have given final consent for publication. Parents consented for publication of the clinical details of their child in an academic journal.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Pandiarajan Vignesh, Rajni Sharma, and Prabal Barman contributed equally.
Contributor Information
Pandiarajan Vignesh, Email: vigimmc@gmail.com.
Amit Rawat, Email: rawatamit@yahoo.com.
References
- 1.Wang C, Tee M, Roy AE, Fardin MA, Srichokchatchawan W, Habib HA, et al. The impact of COVID-19 pandemic on physical and mental health of Asians: a study of seven middle-income countries in Asia. PLoS ONE. 2021;16(2):e0246824. doi: 10.1371/journal.pone.0246824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Budu MO, Rugel EJ, Nocos R, Teo K, Rangarajan S, Lear SA. Psychological impact of COVID-19 on people with pre-existing chronic disease. Int J Environ Res Public Health. 2021;18(11):5972. doi: 10.3390/ijerph18115972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO COVID-19 Dashboard. Geneva: World Health Organization, 2020. Available online: https://covid19.who.int/ (last cited: [March 16, 2023]).
- 5.Grover S, Sahoo S, Mehra A, Avasthi A, Tripathi A, Subramanyan A, et al. Psychological impact of COVID-19 lockdown: an online survey from India. Indian J Psychiatry. 2020;62(4):354–362. doi: 10.4103/psychiatry.IndianJPsychiatry_427_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Addis SG, Nega AD, Miretu DG. Psychological impact of COVID-19 pandemic on chronic disease patients in Dessie town government and private hospitals. Northeast Ethiopia Diabetes MetabSyndr. 2021;15(1):129–135. doi: 10.1016/j.dsx.2020.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varshney M, Parel JT, Raizada N, Sarin SK. Initial psychological impact of COVID-19 and its correlates in Indian Community: an online (FEEL-COVID) survey. PLoS ONE. 2020;15(5):e0233874. doi: 10.1371/journal.pone.0233874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chawla N, Tom A, Sen MS, Sagar R. Psychological impact of COVID-19 on children and adolescents: a systematic review. Indian J Psychol Med. 2021;43(4):294–299. doi: 10.1177/02537176211021789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akdağ B, Önder A, GizliÇoban Ö, KocacıkUygun DF, SürerAdanır A, Erdem A, et al. Psychological state of parents of children with primary immunodeficiencies during the COVID-19 pandemic. Pediatr Allergy Immunol Pulmonol. 2022;35(1):12–18. doi: 10.1089/ped.2021.0081. [DOI] [PubMed] [Google Scholar]
- 10.Kılıç AO, Uzun N, Akın F, Akıncı MA, Yazar A, Bozkurt Alan H, et al. The effects of COVID-19 pandemic on mental health in children with primary immunodeficiency. Pediatric Practice Res. 2022;10(2):83–88. doi: 10.21765/pprjournal.1133096. [DOI] [Google Scholar]
- 11.Sowers KL, Galantino ML. Living with primary immunodeficiency disease during the Covid-19 pandemic. Z GesundhWiss. 2022;30(12):2753–2760. doi: 10.1007/s10389-021-01545-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anjani G, Vignesh P, Joshi V, Shandilya JK, Bhattarai D, Sharma J, et al. Recent advances in chronic granulomatous disease. Genes Dis. 2019;7(1):84–92. doi: 10.1016/j.gendis.2019.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pulvirenti F, Sangerardi M, Plebani A, Soresina A, Finocchi A, Pignata C, et al. Health-related quality of life and emotional difficulties in chronic granulomatous disease: data on adult and pediatric patients from Italian Network for Primary Immunodeficiency (IPINet) J Clin Immunol. 2020;40(2):289–298. doi: 10.1007/s10875-019-00725-1. [DOI] [PubMed] [Google Scholar]
- 14.Yonkof JR, Gupta A, Fu P, Garabedian E, the United States Immunodeficiency Network Consortium Dalal J 2019 Role of allogeneic hematopoietic stem cell transplant for chronic granulomatous disease (CGD) a report of the United States Immunodeficiency Network. J Clin Immunol. 2019;39(4):448–458. doi: 10.1007/s10875-019-00635-2. [DOI] [PubMed] [Google Scholar]
- 15.Chiesa R, Wang J, Blok HJ, Hazelaar S, Neven B, Moshous D, et al. Hematopoietic cell transplantation in chronic granulomatous disease: a study of 712 children and adults. Blood. 2020;136(10):1201–1211. doi: 10.1182/blood.2020005590. [DOI] [PubMed] [Google Scholar]
- 16.Rawat A, Vignesh P, Sudhakar M, Sharma M, Suri D, Jindal A, et al. Clinical, immunological, and molecular profile of chronic granulomatous disease: a multi-centric study of 236 patients from India. Front Immunol. 2021;12:625320. doi: 10.3389/fimmu.2021.625320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garfan S, Alamoodi AH, Zaidan BB, Al-Zobbi M, Hamid RA, Alwan JK, et al. Telehealth utilization during the Covid-19 pandemic: a systematic review. Comput Biol Med. 2021;138:104878. doi: 10.1016/j.compbiomed.2021.104878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cole T, McKendrick F, Titman P, Cant AJ, Pearce MS, Cale CM, et al. Health related quality of life and emotional health in children with chronic granulomatous disease: a comparison of those managed conservatively with those that have undergone haematopoietic stem cell transplant. J Clin Immunol. 2013;33(1):8–13. doi: 10.1007/s10875-012-9758-0. [DOI] [PubMed] [Google Scholar]
- 19.Battersby AC, Braggins H, Pearce MS, McKendrick F, Campbell M, Burns S, et al. Health-related quality of life and emotional health in X-linked carriers of chronic granulomatous disease in the United Kingdom. J Clin Immunol. 2019;39(2):195–199. doi: 10.1007/s10875-019-00607-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deshpande D, Scalchunes C, Orange J, Milner J. Impact of the COVID-19 pandemic on physical and mental health among individuals with primary immunodeficiency: results of a nationwide survey. J Allergy Clin Immunol. 2021;147(2):AB153. doi: 10.1016/j.jaci.2020.12.549. [DOI] [Google Scholar]
- 21.Manusama OR, van Beveren NJM, van Hagen PM, Drexhage HA, Dalm VASH. Psychological symptoms in primary immunodeficiencies: a common comorbidity? J Clin Immunol. 2022;42(3):695–698. doi: 10.1007/s10875-022-01207-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahmed Meelad R, Abd Hamid IJ, Hashim IF, Zainudeen ZT, Abu Bakar FF, Taib F, et al. Impact of primary immunodeficiency diseases on the life experiences of patients in Malaysia from the caregivers’ perspective: a qualitative study. Front Pediatr. 2022;10:846393. doi: 10.3389/fped.2022.846393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seidel MG, Kindle G, Gathmann B, Quinti I, Buckland M, van Montfrans J, et al. The European Society for Immunodeficiencies (ESID) registry working definitions for the clinical diagnosis of inborn errors of immunity. J Allergy Clin Immunol Pract. 2019;7(6):1763–1770. doi: 10.1016/j.jaip.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 24.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Weiss DS. The Impact of Event Scale: revised. In: Wilson, J.P., Tang, C.Sk. (eds) Cross-cultural assessment of psychological trauma and PTSD. International and Cultural Psychology Series. Springer, Boston, MA. (2007) 10.1007/978-0-387-70990-1_10.
- 26.Kawamura N, Kim Y, Asukai N. Suppression of cellular immunity in men with a past history of posttraumatic stress disorder. Am J Psychiatry. 2001;158(3):484–486. doi: 10.1176/appi.ajp.158.3.484. [DOI] [PubMed] [Google Scholar]
- 27.Lovibond SH, Lovibond Peter F, Psychology Foundation of Australia. Manual for the depression anxiety stress scales. 2nd ed. Sydney, N.S.W.: Psychology Foundation of Australia; 1995.
- 28.Kumar K, Kumar S, Mehrotra D, Tiwari SC, Kumar V, Dwivedi RC. Reliability and psychometric validity of Hindi version of Depression, Anxiety and Stress Scale-21 (DASS-21) for Hindi speaking head neck cancer and oral potentially malignant disorders patients. J Cancer Res Ther. 2019;15(3):653–658. doi: 10.4103/jcrt.JCRT_281_17. [DOI] [PubMed] [Google Scholar]
- 29.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID-19 Scale: development and initial validation. Int J Ment Health Addict. 2022;20(3):1537–1545. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lathabhavan RA. Psychometric analysis of Fear of COVID-19 Scale in India. Int J Ment Health Addict. 2021:1–8. [DOI] [PMC free article] [PubMed]
- 31.World Health Organization. (2020). Q&A on coronaviruses (COVID-19). Retrieved March 30, 2020, from https://www.who.int/news-room/q-a-detail/q-a-coronaviruses.
- 32.Babaha F, Rezaei N. Primary immunodeficiency diseases in COVID-19 pandemic: a predisposing or protective factor? Am J Med Sci. 2020;360(6):740–741. doi: 10.1016/j.amjms.2020.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meyts I, Bucciol G, Quinti I, Neven B, Fischer A, Seoane E, et al. Coronavirus disease 2019 in patients with inborn errors of immunity: an international study. J Allergy Clin Immunol. 2021;147(2):520–531. doi: 10.1016/j.jaci.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goudouris ES, Pinto-Mariz F, Mendonça LO, Aranda CS, Guimarães RR, Kokron C, et al. Outcome of SARS-CoV-2 infection in 121 patients with inborn errors of immunity: a cross-sectional study. J Clin Immunol. 2021;41(7):1479–1489. doi: 10.1007/s10875-021-01066-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carter-Timofte ME, Jørgensen SE, Freytag MR, Thomsen MM, Brinck Andersen NS, Al-Mousawi A, et al. Deciphering the role of host genetics in susceptibility to severe COVID-19. Front Immunol. 2020;11:1606. doi: 10.3389/fimmu.2020.01606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Al Yazidi LS, Al Rawahi H, Al Busaidi I, Al TS. COVID-19 and primary immunodeficiency: one-year experience. J Paediatr Child Health. 2021;57(4):594. doi: 10.1111/jpc.15433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marcus N, Frizinsky S, Hagin D, Ovadia A, Hanna S, Farkash M, et al. Minor clinical impact of COVID-19 pandemic on patients with primary immunodeficiency in Israel. Front Immunol. 2021;11:614086. doi: 10.3389/fimmu.2020.614086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Delavari S, Abolhassani H, Abolnezhadian F, Babaha F, Iranparast S, Ahanchian H, et al. Impact of SARS-CoV-2 pandemic on patients with primary immunodeficiency. J Clin Immunol. 2021;41(2):345–355. doi: 10.1007/s10875-020-00928-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mantravadi V, Nguyen ST, Morley SC, Bednarski JJ, Kitcharoensakkul M, Cooper MA. Recovery from COVID-19 in a child with chronic granulomatous disease and T cell lymphopenia. J Clin Immunol. 2021;41(1):23–25. doi: 10.1007/s10875-020-00896-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Esmaeilzadeh H, Dehghani SS, Shahhoseini B, Alyasin S, Nabavizadeh SH, Askari A. COVID-19 in chronic granulomatosis disease: a case report. Iran J Allergy Asthma Immunol. 2022;21(4):478–483. doi: 10.18502/ijaai.v21i4.10295. [DOI] [PubMed] [Google Scholar]
- 41.Castano-Jaramillo LM, Yamazaki-Nakashimada MA, O'Farrill-Romanillos PM, MuzquizZermeño D, Scheffler Mendoza SC, Venegas Montoya E, et al. COVID-19 in the context of inborn errors of immunity: a case series of 31 patients from Mexico. J Clin Immunol. 2021;41(7):1463–1478. doi: 10.1007/s10875-021-01077-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chou J, Platt CD, Habiballah S, Nguyen AA, Elkins M, Weeks S, et al. Mechanisms underlying genetic susceptibility to multisystem inflammatory syndrome in children (MIS-C) J Allergy Clin Immunol. 2021;148(3):732–738.e1. doi: 10.1016/j.jaci.2021.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mustafa SS, Vadamalai K, Ramsey A. Patient satisfaction with in-person, video, and telephone allergy/immunology evaluations during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2021;9(5):1858–1863. doi: 10.1016/j.jaip.2021.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang C, Han B, Zhao T, Liu H, Liu B, Chen L, et al. Vaccination willingness, vaccine hesitancy, and estimated coverage at the first round of COVID-19 vaccination in China: a national cross-sectional study. Vaccine. 2021;39(21):2833–2842. doi: 10.1016/j.vaccine.2021.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kasi SG, Dhir SK, Shah A, Shivananda S, Verma S, Marathe S, et al. Coronavirus disease 2019 (COVID-19) vaccination for children: position statement of Indian Academy of Pediatrics Advisory Committee on Vaccination and Immunization Practices. Indian Pediatr. 2022;59(1):51–57. doi: 10.1007/s13312-022-2421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stark L, Seff I, Weber A, Darmstadt GL. Applying a gender lens to global health and well-being: framing a Journal of Global Health special collection. J Glob Health. 2020;10:010103. doi: 10.7189/jogh.10.010103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dhar D, Jain T, Jayachandran S. Intergenerational transmission of gender attitudes: evidence from India. J Dev Stud. 2019;55:2572–2592. doi: 10.1080/00220388.2018.1520214. [DOI] [Google Scholar]
- 49.Gupta GR, Oomman N, Grown C, Conn K, Hawkes S, Shawar YR, et al. Gender equality and gender norms: framing the opportunities for health. Lancet. 2019;393:2550–2562. doi: 10.1016/S0140-6736(19)30651-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.