Abstract
The human body has a unique way of saying when something is wrong with it. The molecules in the body fluids can be helpful in the early detection of diseases by enabling health and preventing disease progression. These biomarkers enabling better healthcare are becoming an extensive area of research interest. Biosensors that detect these biomarkers are becoming the future, especially Point Of Care (POC) biosensors that remove the need to be physically present in the hospital. Detection of complex and systemic diseases using biosensors has a long way to go. Saliva-based biosensors are gaining attention among body fluids due to their non-invasive collection and ability to detect periodontal disease and identify systemic diseases. The possibility of saliva-based diagnostic biosensors has gained much publicity, with companies sending home kits for ancestry prediction. Saliva-based testing for covid 19 has revealed effective clinical use and relevance of the economic collection. Based on universal biomarkers, the detection of systemic diseases is a booming research arena. Lots of research on saliva-based biosensors is available, but it still poses challenges and limitations as POC devices. This review paper talks about the relevance of saliva and its usefulness as a biosensor. Also, it has recommendations that need to be considered to enable it as a possible diagnostic tool.
Graphical Abstract
Keywords: Salivary biomarkers, Systemic diseases, Serum, Salivary components, Biosensors
Introduction
Any disease deviates from healthy well-being, and early disease detection is critical for proper treatment and eradication. Saliva-based diagnosis has drawn significant attention due to its ease of collection, cost-effectiveness, accessible storage, and non-invasiveness. Other body fluids like blood and urine routinely used for disease diagnosis have associated collection issues. Saliva has biocomponents that could be used as potential biomarkers. Hence, saliva as a diagnostic tool will add to the diagnostic arsenal, providing critical information about oral and systemic health. The Salivary biomarkers range in different omic realms, from proteomics to metabolomics to transcriptomics. Considering its various possibilities, this review explores several studies in saliva-related diagnostics and its correlation with systemic diseases, highlighting its potential as a diagnostic specimen.
Saliva is a crucial human body fluid that protects the oral cavity from infections [1]. It acts as a lubricant that protects teeth and regulates the enzymatic activity in the mouth. Research shows a salivary flow reduction can indicate dental caries risk [2]. The salivary biofilm covers the tooth surface [3], naturally protecting the tooth against decay and erosion.
The major and minor salivary glands secrete saliva, which flows through the ducts and reaches the mouth [4]. The significant glands include the parotid gland, submandibular gland, and sublingual gland (Fig. 1), and are the combination of mucous and serous cells that aid in the secretion of saliva. Mucous cells are columnar; they secrete thick and viscous saliva, while serous cells are triangular and secrete thin, watery saliva [5] (Fig. 2). Serous cells are found to be smaller, with an oval-shaped nucleus; mucous cells are much larger and have a paler color. Humans produce nearly 600 mL of saliva daily, essentially composed of 99% water and containing sodium, potassium, and chloride electrolytes. The salivary composition depends on the diet or nutrient intake. The presence of genetic material in the saliva of the person aids in many genomic applications, including forensic evidence [6]. Saliva contains proteins such as amylases and immunoglobulin, which break down starch and other substances that aid digestion [7]. Additionally, it contains antimicrobial factors that retain the health of oral microbiota and substances like urea and ammonia [8]. Collectively, these components in saliva make it a powerful and valuable diagnostic tool.
Fig. 1.
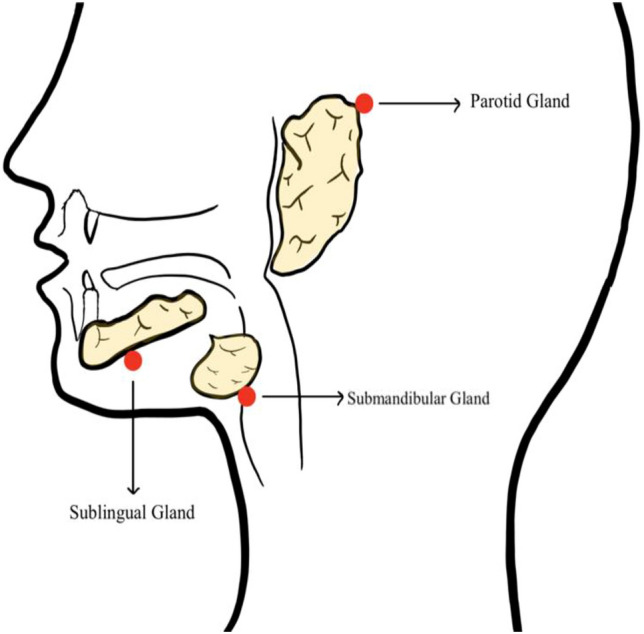
Diagram shows the three salivary glands and their locations
Fig. 2.
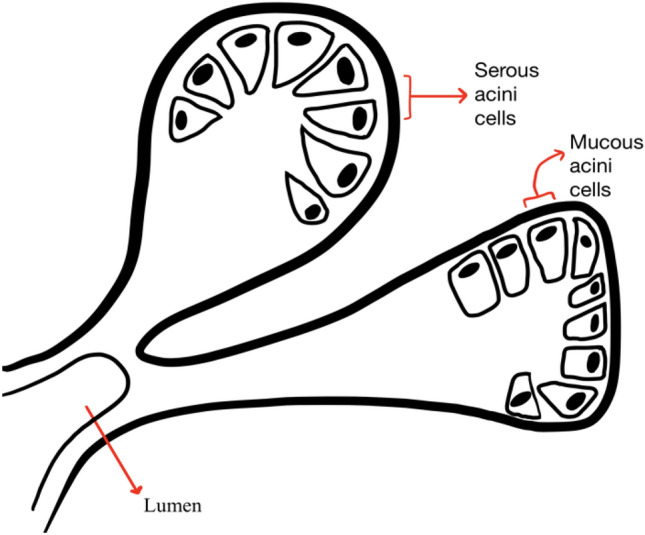
Diagram shows the types of acinar cells in salivary glands
The main focus of this review is to summarize the existing studies that use salivary biomarkers and identify salivary biomarkers for various systemic diseases. This review has three specific objectives (a) to summarize the literature in terms of different kinds of salivary biomarkers, especially those associated with systemic diseases; (b) to examine the relationship with periodontitis and also the advantage of oral/salivary biosensors; (c) to look at the change in the field after the covid pandemic.
Method of Review
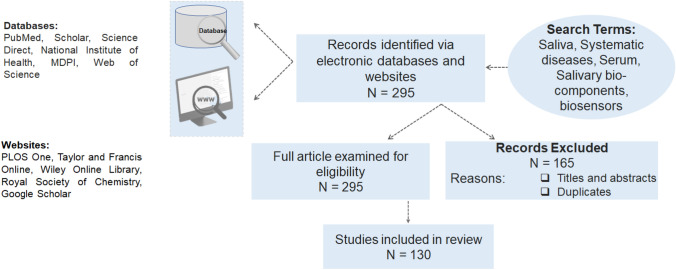
This review was based on salivary biocomponent presence, which could be used as biomarkers for early detection and diagnosis of oral health and the potential association with oral and systemic diseases. The principle question, which is the focus of this review, is, “Is there any change in salivary biocomponents which could be used in diagnostic/biosensor development”. Electronic databases such as PubMed, Scholar, Science Direct, NIH, MDPI, Web of Science, and other websites such as Wiley online library, RSC Publishing, and Google Scholar were considered for this review focusing only on the available literature. Figure 3 illustrates the article selection method adopted to conduct this review. No limits on dates were placed on the database search. The search query included saliva, systemic diseases, salivary bio components, and serum.
Fig. 3.
Flowchart representing the article selection method
Saliva as a Potential Biofluid for Biosensing
Saliva: The Primary Function
Saliva can act as a buffer in the oral cavity to prevent pathogens from infecting the cavity, and it neutralizes the acids produced by highly acidic food consumed [9]. This prevents enamel from degradation and protects the teeth. For example, consuming fermented carbohydrates in cookies, soda, and candy can lead to decreased oral pH, and salivary peptides are released to increase the pH of the saliva to maintain the normal oral pH [10]. Ammonia and urea in saliva also increase pH, allowing the buffer system to function effectively. The ability to analyze normal vs. abnormal levels of urea and other substances in saliva opens the door for various biosensor development, where specific biosensors can test for various salivary biomarkers and categorize them as normal versus abnormal. As a result of this analysis, abnormal signs or increased/decreased levels of crucial enzymes or biomarkers can be used to diagnose possible disease or infection detection.
Other functions of saliva include rinsing, solubilizing food substances, bacterial clearance, lubricating soft tissues, bolus formation, swallowing, speech, and facilitation of mastication; all related to its fluid characteristics and specific components. In addition, saliva components contribute to mucosal coating, digestion, and antibacterial defense [11].
Properties of Saliva
Saliva is a hypotonic solution that contains water, electrolytes, mucus, and enzymes. Approximately 90% of saliva is secreted from major salivary glands such as parotid, submandibular, and sublingual. Elements of non-salivary origin include gingival crevicular fluid (GCF), expectorated bronchial and nasal secretions, serum and blood derivatives from oral wounds, bacteria and bacterial products, viruses, and fungi desquamated epithelial cells, other cellular components, and food debris [12].
Human saliva mirrors the body's health and well-being. More than 20% of proteins in the blood are also found in saliva, making saliva an invasive option for detecting biomarkers that correlate with the disease state. Saliva has numerous advantages over blood as a diagnostic fluid, allowing for a non-invasive, simple, and safe sample collection. Its composition reflects the state of health and illness in a body, and it can potentially be a diagnostic medium for systemic diseases. Saliva can be considered as gland-specific saliva or whole saliva. Evaluations of the secretions from the individual salivary glands help detect gland-specific pathology, i.e., infection and obstruction. However, the whole saliva is most frequently studied with analysis for systemic disorders.
Salivary Constituents
An average person can produce 600 mL of saliva per day. Saliva contains 99% water and one percent organic molecules such as salivary amylase, mucopolysaccharide, mucin, and lysozymes, and some inorganic matter such as sodium, potassium, calcium chloride, and thiocyanate ions. Various bio-components are also found in saliva, including protein and related molecules, nucleic acid components, and endogenous and exogenous metabolites[13]. Examples of biocomponents detectable in saliva [14–16] are summarized in Table 1.
Table 1.
Examples of biocomponents detectable in saliva
| Biocomponents in saliva | Examples |
|---|---|
| Steroid Hormones | Cortisol, Insulin, Testosterone, Oestrogen |
| Cytokines | Interleukins (IL-1beta, IL-6, IL-8), Tumor necrosis factors |
| Antibodies | IgG, IgA, IgM |
| Proteins/Enzymes | Carbonic anhydrase, Lysozyme, Peroxidase, Amylase, Pepsin, matrix metalloproteinases-8 (MMP-8), Creactive protein, mucin, lactoferrins, Leptin |
| Growth factors | Epidermal growth factor, vascular endothelial growth factor, insulin-like growth factor |
| Nucleic acid | Human and microbial DNA, mRNA |
| Bacteria |
P. gingivalis, S. mutans, s, Lactobacillus spp, T forsythia, E. coli, H. pylori, M. tuberculosis |
| Viruses | HIV, HSV-1, HSV-2, EBV, HPV, VZV, CMV, HCV |
| Metabolites/Electrolytes | Phosphate, calcium, sodium, potassium, glucose, chloride, nitrate, uric acid, amino acids, lipids, carbohydrates |
| Small signaling molecules | Adenosine-triphosphate |
| Cells | Epithelial cells, Neutrophils |
Advantages of Salivary Test
The main advantage of this non-invasive technique is that patients with needle usage restrictions, such as children, aged, and hemophiliac patients, can do the sample collection and test for biomarkers. Also, unlike blood, saliva can be self-collected, and unlike urine, saliva can be collected at any time. These are the necessary conditions that point-of-care testing (POCT) must meet to make on-site testing possible anywhere at home or the workplace. Furthermore, it can be beneficial for mass screening tests and continuous monitoring. Table 2 shows various approaches to diagnosing systemic diseases and body conditions using salivary biomarkers with the possibility of being used as diagnostic methodologies even in a clinical setting.
Table 2.
Summary of various approaches to diagnosing systemic diseases and body conditions using salivary biomarkers
| Systemic diseases | Salivary biomarker | References | Comments |
|---|---|---|---|
| Atherosclerosis |
IL-1beta, IL-6, TNF- alpha & prostaglandin E2 increases significantly |
Kosaka [81] | |
| Acute Myocardial Infarction | C-reactive protein (CRP), Cardiac troponin T (hs-cTnT) | Pay et al. [82], Mirzaii-Dizgah et al. [37] | Salivary CRP and cardiac troponin T can be used to monitor and diagnosis of myocardial infarction |
| Cardiovascular diseases | Alpha-2-HS glycoprotein in saliva decreases, NT-proBNP levels increases in saliva |
Zheng |
Salivary Alpha-2-HS glycoprotein and NT-proBNP can be used as early diagnosis of heart failure |
| Type-2 Diabetes Mellitus | Alpha-2 macroglobulin increases in the saliva | Aitken et al.[84] | Salivary glucose level can be used as potential indicator in screening, diagnosis and monitoring of diabetes mellitus |
| Chronic Liver diseases | Hepatitis C virus increases in the saliva | Parisi et al. [61] |
Sample Collection
Saliva can be collected in two methods: unstimulated and stimulated saliva. Unstimulated saliva is produced consistently within the oral cavity and is present in the mouth. The second type is stimulated saliva, collected using chewing gum or a flavor drop into the oral cavity. The activated taste buds respond to the brain and increase the secretion of saliva in larger quantities [8]. Previous research exposes that stimulated saliva expressed more than three times the number of biomolecules than unstimulated saliva [17]. Stimulated saliva contributes to most daily secretions, whereas unstimulated saliva covers the oral tissue and acts as a lubricant [18].
A Lashley cup can be used to collect oral fluids via suction from a specific gland. Cotton swabs can also be used but may cause unwanted bias. Various saliva-collecting devices are manufactured by companies like Salimetrics®v (State College, PA, USA), DNAGenotek (Kanata, ON, Canada), and Oasis Diagnostics® Corporation (Vancouver, WA, USA). These devices revolutionized collecting saliva and its transportation methods without contamination [16]. However, draining, spitting, and suctioning are standard approaches [19]. Regardless of the method used, the subject should clean the oral cavity with water to avoid contamination before collection.
Biosensor Selections
Biosensors are an exciting addition to the world of nanomedicine and technology. They allow patients and healthcare providers to monitor disease progressions and treatment efficiency [20]. Biosensors can detect various indicators of diseases in fluids, such as blood, saliva, and urine. Additionally, biosensors allow patients to understand their illnesses and their betterment over time. The development of biosensors allows patients to have an affordable alternative to doctors' appointments and reduce the need for stressful medical bills and inefficient circumstances. Such devices are considered to be “point-of-care”. This means they play a vital role in detecting diseases early on and surveilling any crucial data to provide patients with early treatments and prevent disease progression (Tables 3 and 4).
Table 3.
Summary of literature reviews on oral biosensors
| Biosensors | Main principle | Advantages | Disadvantages | References |
|---|---|---|---|---|
| Titanium Biosensor |
- Utilizing titanium coated biosensors to gain insight on periodontal health and detecting harmful levels of streptococcus Gordonii. This will allow for further testing on autoimmune diseases and biomarkers present pre and post surgeries |
- Noninvasive - Utilizes the understanding of a bacteria that has been the subject of extensive research—Allows CHX, which is used widely in hospital/surgical settings, to be further utilized as a protective oral health tool -Titanium is durable, does not corrode, high quality |
- Using CHX as a coating may introduce other factors not accounted for - May be costly to obtain all the materials necessary for this biosensor |
[85] |
|
AlphaAmylase Biosensor (Fig. 4) |
- Detecting levels of alphaamylase in saliva |
- Readily available - Noninvasive - Provides insight on the diet of an individual—Concrete substance to test and manipulate that is constantly present in saliva - Provides inside on levels of acidity in the oral cavity due to digestion of complex carbohydrates |
- Diet of an individual may cause skews in data - Pre-existing health conditions may influence patient’s results |
[86] |
|
Urea Smartphone Biosensor (Fig. 4) |
- Detecting levels of salivary urea and connecting a transducer with a smartphone application that evaluates the range of urea levels (Fig. 3) | - Concrete substance to test and manipulate—Previous research articles on levels of urea show that higher levels of urea were associated with kidney disease or periodontal disease | - Requires the presence of a smartphone and most likely a WIFI connection to transfer data to clinics and medical professionals—Color detection may be skewed based on lighting and other environmental factors -May cause anxiety for patients who may panic if numbers are not within the same range | [87] |
|
Non-invasive Impedimetric Biosensor for Oral Cancer Detection (Fig. 4) |
- Efficient biomarker focused on detecting the cancer biomarker CYFRA-21–1 in saliva |
- Noninvasive - Allows for early detection of cancer without any surgical procedures or costly treatments—Utilizes ELISA, a method that has been used vastly and can be manipulated by scientists - Introduces an extremely sensitive biosensor that detects precise values - IR spectroscopy bands utilized to detect specific functional groups |
-May provide insight on lung cancer and or other cancers that may not be applicable to oral cancer - Requires clear understanding of CYFRA21-1 biomarker and its functionalization |
[35] |
Table 4.
Clinical Need for Biosensors
| Advantages | Disadvantages | What is currently being used? | References | |
|---|---|---|---|---|
| Biosensors that monitor astronaut’s health | High exposure to cosmic rays can cause harmful side effects in astronauts health such as carcinogenic influences- These biosensors are crucial to detect harmful levels of biomarkers or cancer cells | Extremely expensive and require extensive research | A team in Bologna, Italy is utilizing biosensors that offer a full health screening for astronauts in space. This can save them before they even enter a dangerous zone or progression of the disease | [88] |
| Biosensors supporting food safety | Biosensors were developed to detect food fraud or harmful contents in foods. Ensuring safe food and sustainability is crucial for consumers | Increased panic in individuals and spread of misinformation | Currently used worldwide to analyze levels of fermentation or acidity and safety for consumers | [89] |
| Biosensor for Salmonella detection |
An impedimetric biosensor was developed for salmonella detection in food such as milk and is based on the ‘Nisin’ antimicrobial peptide that destroys bacterial cells. Detection levels can be as small as 1.5*10^1 CFU/mL |
Minimal disadvantages | Biosensors used to detect foodborne salmonella, aiding both consumers as well as food distributors as well as detecting serotypes | [90] |
|
Biosensor for COVID-19 detection |
Extremely efficient and noninvasive for the patient. A safe method for obtaining the sample for both the patient and healthcare professional | Waiting period | SARS-CoV-2 detection through IgA measured in Saliva. The nasopharyngeal swab allows for a sample to be obtained | [91] |
A fully developed biosensor will generally consist of a bioreceptor, which recognizes the substance of interest [20] (Fig. 4). It will also contain a substance transducer to convert the biomarker into a viable number or readable graph. For example, viruses, such as COVID-19, can also be detected through saliva. This allows highly contagious diseases to be detected quickly [21]. This allows easy and quick data processing and communication between patients, clinics, and doctors from their homes. Figure 4a) is a representation of a potential app that can be developed to connect with a transducer and used to send important data to healthcare professionals; Fig. 4b) shows a sample disposable transducer test strip that can be used with the collected saliva in a test tube which offers a non-invasive testing possibility.
Fig. 4.
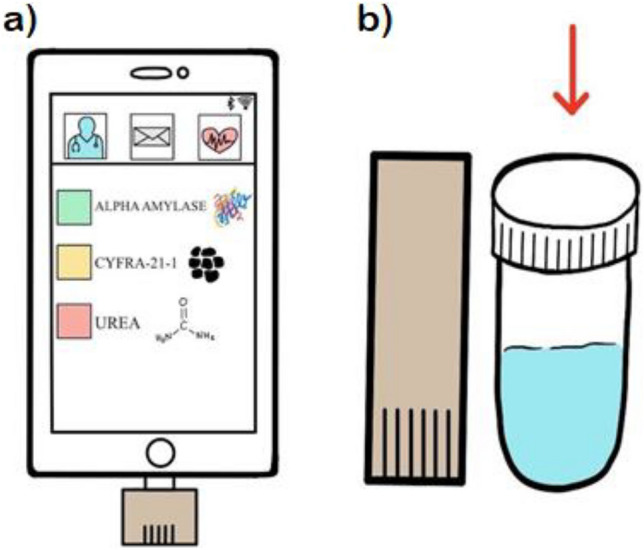
a Diagram shows a potential app that can be developed to connect with a transducer and send important data to healthcare professionals, b Diagram shows a sample test tube that will include the easily obtained saliva sample and the disposable transducer strip
Cobalt metal diagnostic devices are currently used for glucose quantification [22]. This diagnostic device, the cobalt metal framework, monitors glucose levels in patients. It is paper-based, which makes it cheap and effective, and disposable. However, this device requires blood as a sample medium instead of saliva, which could risk infection if mishandled and make it less accessible. Figure 5 is a schematic of the commonly used three biomarkers in the collected saliva with a transducer used for it.
Fig. 5.
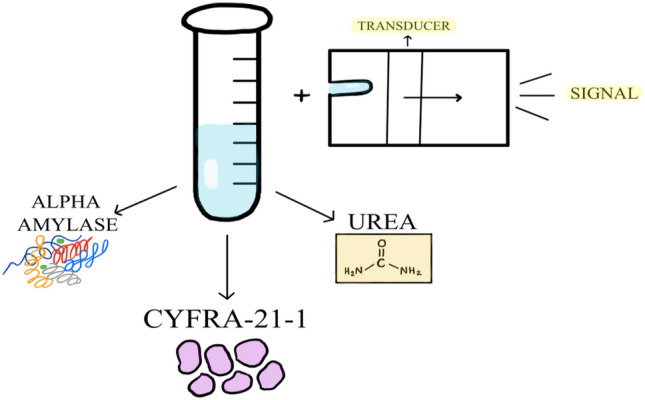
Diagram shows an example of a transducer and the three main biomarkers to be tested
Salivary Biomarkers
Various biomarkers are present in saliva, and some are identified through infrared spectroscopy. Cells proliferate much faster, and therefore, cancers can metastasize quickly. Apart from monitoring periodontal diseases [23, 24], saliva has been used to identify systemic inflammations and screening purposes in epidemiological studies [25], revealing its possibility as a diagnostic tool. The presence of cancer-detection biomolecules leads researchers to believe that biomarkers in saliva can indicate cancers and provide options for early detection[26].
Gingival Crevicular Fluid (GCF) GCF
Gingival crevicular fluid (GCF) is a fluid secreted by the gums, specifically at the line where the gums and the teeth meet. GCF is unique because it is considerably low in quantity in a healthy oral cavity and spikes higher when a patient has gum disease or infection. GCF is also non-invasive, and its concentration can indicate disease [27]. The composition of GCF is unique due to its electrolytes, albumins, globulins, lipoproteins, and other components. GCF has shown its ability to detect anti-HIV antibodies [28], which enables its use as a diagnostic marker in HIV-positive patients.
Microbiome as a Biomarker
A typical example of bacteria in the saliva is Streptococcus Gordonii, which is found in periodontal environments and causes bone loss and inflammation [29]. Additionally, S. Gordonii can enter the blood circulatory system and cause life-threatening diseases such as endocarditis. It can affect the formation of healthy biofilm protective layers, thereby increasing the risk of dental caries [30]. With the overwhelming use of Ti-based dental implants, the Ti-based biosensors are crucial as they can provide information about peri-implantitis and bacterial disintegration upon antibacterial or antimicrobial agents.
Alpha-Amylase as Biomarker
Alpha-amylase plays a significant role in odor, flavor, and oral texture [31], it also monitors stress levels [32]. Although alpha-amylase is only found in small amounts in saliva, it still significantly influences the oral cavity.
Urea as Biomarker
Levels of urea in saliva can provide insight into chronic kidney disease [33] and renal failure. Salivary urea and bicarbonate act as a buffer, and their levels can vary based on salivary gland stimulation [34]. Providing patients with a biosensor will allow them to better understand their condition through a simple smartphone app. Additionally, they can seek medical help if normal urea levels are shifted and remain aware of their bodily functions, further preventing emergencies. The presence of urea in saliva makes saliva a test sample facilitating easy, point-of-care feasibility using optical or electrochemical biosensors.
Cancer Biomarkers
With oral cancer being one of the top cancers in the world, controlling its cell cycle and early detection is a crucial step to prevent it from spreading [35]. Generally, detecting oral cancer can take a long period, is expensive, and is invasive for the patient. Collecting a sample and analyzing it directly through a biosensor allows painless detection, is time efficient, and does not require the presence of a trained expert. Serum and plasma are often used to detect biomarkers, specifically for monitoring diseases and their progression.
Diagnosis of Systemic Diseases Using Saliva
Some systemic diseases may affect the composition of salivary biomarkers presence. These characteristic changes may contribute to the diagnosis and early detection of these diseases.
Metabolic Diseases—Heart Diseases, Diabetes, and Liver Diseases
Cardiovascular Diseases
Cardiovascular diseases are reported as one of the leading causes of death annually by the World Health Organization (WHO). Human saliva plays a significant diagnostic role in the detection of cardiovascular diseases by examining the salivary biomarkers, e.g., C-reactive proteins (CRP) [36], Cardiac troponin (cTn) [37], and Creatine phosphokinase [38] and NT-ProBNP [39]. Table 5 summarizes various Salivary Biomarkers in Cardiovascular diseases. Activation of MMP-8 plays a vital role in the pathogenesis of coronary artery diseases. It causes infarction growth, tissue repair, and cardiac remodeling [40]. MMP-8 and its tissue inhibitor TIMP-1(tissue inhibitor of matrix metalloproteinase-1) concentration are associated with ischemia and infarction [41]. The ratio of MMP-8/TIMP-1 reflects the progression of cardiovascular diseases in serum [42]. The additional enzyme involved is Lysozyme, which is present in saliva and other secretions such as mucus and tears [43].
Table 5.
Summary of various salivary biomarkers in cardiovascular diseases
| Disease | Biomarkers | Sample type | Result | References |
|---|---|---|---|---|
| Myocardial Necrosis |
C-reactive protein, Troponin 1, Myeloperoxidase, MMP-9 |
Serum and Saliva |
Elevated in both, Significant correlation between serum and saliva observed | Foley et al. [62] |
| Acute Myocardial Infarction |
C-reactive Protein, Creatine kinase, BNP |
Serum and saliva | CRP detected significantly in serum and saliva |
Miller et al [44] |
| Inflammation tissue injury and remodeling |
C-reactive protein, Myeloperoxidase, MMP-9 |
Serum and Saliva |
Elevated in both | Foley et al. [62] |
| Heart Failure Patients | NT-proBNP | Serum and saliva | No correlation found between saliva and serum, though elevated in both | Foo et al. [39] |
Literature reports the compatibility between a biomarker of saliva and blood for the diagnosis of Acute Myocardial Infarction (AMI). Serum biomarkers for Acute Myocardial Infarction were Troponin 1, B-type natriuretic peptide, and creatine kinase. In saliva, C-reactive protein (CRP) was found as a biomarker that is the most predictive biomarker of AMI. AMI was diagnosed with 80.0% sensitivity and 100% specificity. This finding shows the potential of salivary biomarkers combined with ECG as an additional diagnostic method for AMI patients [44].
Diabetes Mellitus
Diabetes is another common systemic disease in the world and developing rapidly due to dietary habits, genetics, and other systemic disease-related complications. In addition, patients with diabetes have higher glucose and alpha-hydroxybutyrate levels and significant changes in carbohydrate, lipid, and oxidative stress levels. The relation between HbA1c and Salivary glucose concentrations in patients with diabetes is reported, indicating blood glucose levels could be easily monitored by the saliva in patients with diabetes mellitus [45]. MMP-8 levels are also elevated in patients who have diabetes [43]. It can be used as a salivary biomarker; however, further studies are needed to diagnose diabetes. Table 6 shows various Salivary Biomarkers found for diabetes in different research experiments.
Table 6.
Summary of various salivary biomarkers found for diabetes
| Disease | Biomarkers | Sample type | Result | References |
|---|---|---|---|---|
| Diabetes | Glucose | Serum and saliva | A significant correlation between serum and saliva found | Gupta et al.[63] |
| Diabetes mellitus | Glucose | Serum and saliva | Significant correlation between fasting blood and salivary glucose levels and postprandial blood and salivary glucose levels |
Gupta et al [92] |
| Type-2 diabetes mellitus |
Glucose and HbA1c |
Serum and saliva | Significant correlation between salivary glucose concentration and associated glycemia/HbA1c values | Mascarenhas et al. [93] |
| Diabetes Mellitus | Glucose | Serum and saliva | Significant correlation between salivary and serum blood glucose levels in both diabetic and nondiabetic patients | Bhattacharyya et al. [94] |
| Diabetes mellitus | Salivary amylase | Saliva | Salivary amylase concentration increased in diabetic patients which can be used as a potential biomarker to evaluate and clinical management of diabetic patients |
Pérez-Ros et al [95] |
| Diabetes Mellitus | Glucose |
Serum and Saliva |
Significant correlation is found between serum and salivary glucose levels which suggest that salivary glucose can be used to monitor blood glucose concentration |
Amer et al [96] |
| Diabetes Mellitus |
Glucose and HbA1C |
Serum and Saliva |
Significant correlation is found between serum and salivary glucose and between serum and salivary glucose and serum glycated hemoglobin |
Naseri et al [97] |
| Type-2 Diabetes Mellitus | Glucose, amylase and proteins |
Serum and Saliva |
Significantly higher salivary glucose, lower amylase and total protein observed which suggest that diabetes influence the composition of saliva |
Indira et al [98] |
| However, further is needed to use saliva as a diagnostic tool for diabetes mellitus | ||||
| Diabetes Mellitus |
Salivary glucose, Salivary amylase and immunoglob ulins |
Serum and saliva | Increase in levels of post prandial blood glucose, HBA1A, salivary glucose, salivary amylase and salivary immunoglobulin A in diabetic patients. Significant correlation is found between post prandial blood glucose and salivary glucose in diabetic patients | Abd-Elraheem et al. [99] |
| Type 2 diabetes | Salivary glucose and urea | Saliva and plasma | Significant correlation is found between salivary and plasma glucose levels as well as in salivary and blood urea |
Mrag et al [100] |
| Diabetes mellitus |
Salivary glucose and HbA1C |
Serum and Saliva |
Significant Correlation found between fasting salivary glucose and blood glucose and fasting salivary glucose and HbA1C in diabetic patients |
Satish et al [45] |
Liver Diseases
Hepatocellular Carcinoma (HCC) is one of the deadliest types of cancer that causes a large number of deaths around the world. Early detection of HCC is complicated. Salivary long non-coding RNA-PCDH9-13:1(salivary lnc-PCDH9-13:1) is a specific biomarker for the diagnosis of early HCC [46]. HCC tissue, by necrosis and apoptosis, secretes lncRna in blood, and then through the salivary gland blood supply, it goes to saliva. Alpha-fetoprotein-L3 is also a promising salivary biomarker of HCC [47]. Hepatitis B and C virus infections commonly cause chronic liver diseases and liver cirrhosis. The natural history of hepatitis B and C virus infection can remain latent without manifesting symptoms. Most patients are asymptomatic, unaware of existing illnesses, and prone to disease progression and transmission. Additionally, some infected people remain undiagnosed due to their unwillingness to provide a blood sample. HBV and HCV infections are monitored mainly by blood and serological test. Interestingly, reports have indicated that HBV and HCV DNAS, viral antigens, and antibodies also exist in infected person’s saliva and correlate significantly with blood samples [48]. These findings show the potential role of saliva as a non-invasive diagnostic method for HBV and HCV infection. A commercially available test that can rapidly identify HCV antibodies in saliva using an Enzyme Immunoassay (EIA) was also developed [49]. The result obtained by this test is almost similar to that of serum immunoassay. It is widely available in Europe; however, waiting for approval by the FDA in the United States. Once approved, this could impact the early detection and management of HCV infections [50]. Table 7 summarizes salivary biomarkers found in the literature for liver diseases.
Table 7.
Summary of various salivary biomarkers found for liver diseases
| Disease | Biomarkers | Sample type | Result | References |
|---|---|---|---|---|
| Hepatocellular Carcinoma |
Alpha Feta Protein (AFP) |
Serum and Saliva |
Elevated AFP level in saliva and serum | You et al. [47] |
|
Early Hepatocellular Carcinoma |
salivary long noncoding RNA-PCDH9- 13:1 |
Serum and Saliva |
A significant correlation between serum and saliva found | Xie et al. [46] |
| Hepatitis C viral (HCV) infection | HCV |
Serum and Saliva |
The clinical performance of the OraQuick HCV Test is comparable to that of laboratorybased tests with both serum and oral fluid | Cha et al. [101] |
| Hepatitis A viral (HAV) infection | HAV | Saliva | IgG antibodies detected in saliva for HAV infection |
Augustine. et al [102] |
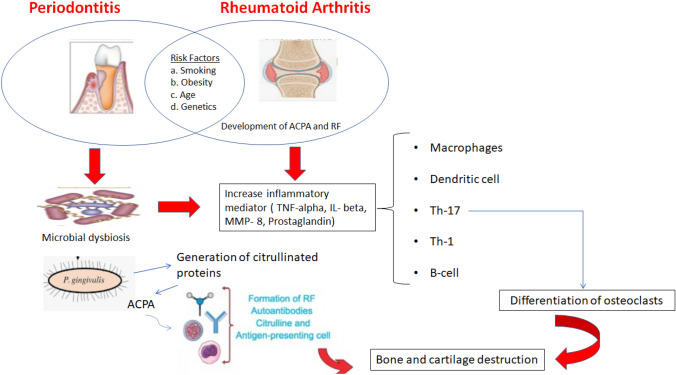
Inflammatory Disease—Rheumatoid Arthritis
Rheumatoid arthritis causes joint pain and damage throughout the body, as it is a chronic inflammatory disease. In rheumatoid arthritis, the body attacks its tissue; in severe cases, it may destroy internal organs. Because of pain and swelling IL-1beta, MMP-8, and TNF-alpha increase in inflamed joints and serum. It is anticipated that rheumatoid arthritis increases the risk of periodontal diseases. MMP-8 is elevated in saliva in patients with rheumatoid arthritis, and its increased level causes periodontal inflammation [51]. Several studies have suggested a strong association between rheumatoid arthritis and periodontal diseases. IL-1beta level in the saliva is high in rheumatoid arthritis compared to patients with periodontal disease [52]. Rheumatoid arthritis patients receiving anti-TNF-alpha antibody therapy have lower IL-1beta and TNF-alpha levels in saliva. Table 8 summarizes salivary biomarkers found for Rheumatoid arthritis during the current review.
Table 8.
Summary of salivary biomarkers found for Rheumatoid arthritis
| Disease | Biomarkers | Sample type | Result | References |
|---|---|---|---|---|
|
Rheumatoid arthritis |
MMP-8 |
Serum and Saliva |
MMP-8 is elevated in saliva at early stage of Rheumatoid arthritis |
Äyräväinen et al. [51] |
|
Rheumatoid arthritis |
IL-1, TNF-alpha |
Serum and Saliva |
Anti-TNF alpha antibody therapy reduces levels of IL-1 and TNFalpha in Saliva | Mirrielees et al. [52] |
|
Rheumatoid arthritis |
IL-1 beta | Serum and GCF |
Periodontal therapy significantly decreases DAS28 and IL-1 beta levels in Rheumatoid arthritis patient |
Bıyıkoğlu et al. [103] |
|
Rheumatoid arthritis |
ACPA (Anti- citrullinated protein antibodies). Antiporphyromonas gingivalis |
Serum and Saliva |
Anti-porphyromonas gingivalis antibodies are associated with ACPA |
Hitchon et al. [104, 105] |
Malignant Tumors—Breast Cancer and Cystic Fibrosis
Breast Cancer
Breast cancer, besides skin cancer, is the most common type of cancer in females. Mammography, the most generic method used to detect breast cancer, has a few limitations, such as overdiagnosis and false positives. It fails for small, early-stage tumors, dense breast tissue, and women under 40. The most crucial aspect of saving a patient is the early detection of breast cancer. There are several challenges and concerns in the early detection of breast cancer, including the risk of disease transfer through serum-based breast cancer screening. To address these challenges, a handy and self-screening saliva-based biosensor was developed by Sania Arif et al. [53] by using salivary autoantibodies ATP6AP1 [76]. Lately, detecting Human Epidermal Receptor-2 (HER2) levels in saliva has also been suggested to diagnose breast cancer [54]. Cancer antigen 15-3 (CA 15-3) is a protein that is produced by normal breast cells. In many people with cancerous breast tumors, there is an increased production of CA 15-3.
The salivary level of CA 15-3 is 50% higher in an infected person than in a healthy person or those with benign tumor cases. Therefore, it has been suggested to use CA 15-3 for the early detection of breast cancer [55]. Tumor protein p53 regulates cell division by keeping cells from growing and proliferating too fast or uncontrolled. Salivary levels of p53 are reported less in breast cancer patients than in healthy individuals [56]. Salivary autoantibodies against both HER2 and MUC-1 have been reported for the early detection of breast cancer [57]. Milk-derived peptides proline and valine are suggested as potential salivary biomarkers for detecting early and advanced stages of breast cancer [58]. Table 9 indicates various salivary biomarkers found for breast cancer.
Table 9.
Summary of various salivary biomarkers found for breast cancer
| Salivary biomarkers | |
|---|---|
| Breast cancer | Cystic fibrosis |
| Increase Cancer antigen 15-3 | Increase protein and calcium levels |
| Decrease Tumor protein 53 | Increase turbidity of saliva |
| Anti-MUC1, Anti-HER2 | Increase phosphate level |
| Proline and Valine | Increase lipid and fatty acid levels |
Cystic Fibrosis
Cystic Fibrosis (CF) is a genetically transmitted disease among children and young adults. It occurs due to defective electrolyte transport in epithelial cells and viscous mucus secretions from glands and epithelia [59]. The organs most affected in CF are (a) sweat glands, which produce a secretion with elevated concentrations of sodium and chloride; (b) the lungs, which develop the chronic obstructive pulmonary disease; (c) the pancreas, resulting in pancreatic insufficiency [60]. DNA analysis is not considered for CF diagnosis due to mutations in the CF gene. At the same time, the diagnosis is derived from the characteristic clinical signs and symptoms and elevated sweat chloride values analysis.
CF patients contain increased calcium levels [61–63]. Elevated levels of calcium and proteins in submandibular saliva resulted in a calcium-protein aggregation which caused turbidity of saliva [64]. The elevated calcium and phosphate levels in the saliva of children diagnosed with CF may explain why these children demonstrate a higher occurrence or formation of calculus than healthy controls [65]. The effect of alteration in the salivary compositions is also seen in the lipid profile of cystic fibrotic patients, which is markedly changed compared to healthy subjects [66]. The submandibular gland saliva of cystic fibrosis patients contains 66% more lipid per 100 ml saliva than that of a healthy subject. The salivary fatty acid profile can be a good indicator of the early detection of tumorigenesis processes and cardiovascular diseases, which are influenced by dietary intake [67]. Table 9 shows the summary of salivary biomarkers found for cystic fibrosis. Saliva-based CF disease diagnosis might take a long way to reach the bedside from the bench.
Infectious Diseases
Human Immunodeficiency Virus (HIV) causes AIDS and weakens the body's ability to fight infection. This virus can be transmitted through contact with infected blood, semen, and vaginal fluids. Today, strict antiretroviral therapy can slow down the disease progression and complications. Both HIV and anti-HIV antibodies can be detected in saliva [68], which provides an alternative method to detect HIV antibodies apart from blood. In 1980, oral fluid was collected with the particular collecting device "OraSure" for the saliva HIV antibody test [69]. OraSure is commercially available in the United States and can be used to diagnose HIV. Additionally, rapidly screening HIV-1 and HIV-2 via saliva-based enzyme-linked immunosorbent assay (ELISA) in 20 min also eliminates the necessity for blood tests [70]. Since it is widely accessible after the approval of the FDA, the over-the-counterpoint of care ELISA kit makes HIV tests not only easy but also private [71]. Currently, 25% of HIV-positive individuals are unaware of their infection and responsible for most new cases annually. The point-of-care testing kit provided a means to assess their HIV status and possibly reduce HIV infections. Furthermore, it may enhance long-term survival rates by facilitating retroviral therapy's early initiation. Secretory Leukocyte Protease Inhibitor enzyme (SLPI) present in saliva shows antiretroviral therapy and prevents HIV-1 infection for 3 weeks after infection; however, human plasma and synovial fluid cannot inhibit HIV-1 infectivity [64].
Diagnosis of HIV with saliva is safe over blood, as saliva collection is painless, non-invasive with minimal or no risk of infection, inexpensive, simple, and rapid. Furthermore, viral transmission via saliva is unlikely as the infectious virus is rarely isolated from saliva [72]. Saliva collection also simplifies the diagnostic process in special populations for whom blood drawing is challenging. This population can be individuals with compromised venous access (e.g., injecting drug users), patients with hemophilia, and children. Studies have demonstrated that HIV infection diagnosis based on a specific salivary antibody is equivalent to a serum-based diagnosis. And, therefore, applicable for both clinical use and epidemiological surveillance [73]. In conclusion, the collection and analysis of saliva offer a simple, safe, well-tolerated, and accurate method for diagnosing HIV infection.
Additionally, saliva-based diagnoses are not only limited to HIV infection. It also plays a significant role in diagnosing infectious diseases such as Malaria, dengue, Ebola, Mycobacterium tuberculosis, and Herpes Simplex virus. The malaria level of IgG antibodies Plasmodium falciparum antigen is present in saliva and strongly correlates with the plasma level [74]. Using saliva as a medium for point-of-care screening will improve early disease state management by identifying the source of infection at an early stage.
Relationship Between Peridontitis and Systemic Diseases
A positive correlation is found between alpha-2 macroglobulin and HbA1c, demonstrating that alpha-2-macroglobulin in saliva could reflect the glycemic control in patients with Type-2 diabetes mellitus [64], whereas the concentration of salivary melatonin decreases in Type-2 diabetes and periodontitis patients. This indicates that salivary melatonin is essential in the pathogenesis of diabetes and periodontal diseases and can be used as a biomarker in diagnosing and treating these two diseases [65].
Periodontal therapy can collaborate with systemic rheumatoid therapy to improve rheumatoid arthritis conditions [74]. After periodontal therapy in rheumatoid arthritis patients, Disease activity score 28 (DAS28) decreases significantly, showing that periodontal therapy can be used in association with RA systemic therapy. Structural damage resulting from chronic inflammation is the primary cause of loss of function and pain seen in the progression of rheumatoid arthritis and periodontal diseases. Also, the porphyromonas gingivalis periodontal pathogen is associated with the production of Anti-citrullinated proteins antibodies (ACPA) in Rheumatoid arthritis patients (Fig. 6) [75]. However, further studies should be established to verify this link between rheumatoid arthritis and periodontal diseases [75]. Several studies reported severe periodontal symptoms in rheumatoid arthritis patients. Therefore, paying attention to the oral cavity of rheumatoid arthritis patients and referring them for regular dental checkups might positively impact the management and treatment of rheumatoid arthritis.
Fig. 6.
Common risk factors and pathogen in the pathogenesis of rheumatoid arthritis and periodontitis
Advantages of Oral Biosensors
Oral biosensor research reported so far confirms its feasibility to assess health and reports disease states as viable numbers or signals based on biomarkers present in the specimen used, such as the whole saliva. An essential aspect of this approach is its non-invasive needleless nature, easy collection, and availability.
A biosensor capable of detecting oral cancer from saliva samples facilitates one of the historical goals of cancer research. With the help of salivary biomarkers, a non-invasive oral cancer diagnostic strategy is established, with minimum expense, ease to use, and a home-based routine testing possibility [76, 77]. Existing biosensor studies are grouped under tables representing their general (Table 3) and clinical (Table 4) perspectives.
Current Status and Future Direction
The biosensor as a diagnostic tool has been used for decades to diagnose, treat, and prevent countless diseases. When observing the usage of biosensors during a pandemic, their meaning takes on a new level. After the COVID-19 pandemic began in late 2019, salivary biosensors have become the primary tool to detect the virus and begin the process of spread prevention and treatment [78].
Comparing these tests shows that these biosensors can efficiently analyze a common denominator, saliva. Saliva is being used as an easy communication path between both clinics and marketing companies to provide a wide range of services. Due to its easy accessibility and inexpensive extraction, it is increasingly becoming a popular medium for scientists to use for viruses, ancestry, and other disease biomarkers that indicate severe or fatal diseases.
In an experiment with the saliva and serum sample of 250 individuals with a prior history of cardiovascular diseases, salivary levels of CRP, prostaglandin E2 (PGE2), leukotriene B4 (LTB4), matrix metalloproteinase 9 (MMP9), creatinine, and lysozyme were measured. A significant correlation identified between salivary and serum CRP levels among patients with ischemic heart disease (IHD) confirms that saliva can be used as an alternative means for the evaluation of cardiovascular risk [79]
Saliva contains several biomarkers that play an important role in determining systemic diseases. Salivary biomarkers such as C-reactive protein, Myeloperoxidase, MMP-9, salivary glucose, IL-1, salivary proteins, TNF-alpha, can be used to diagnose various systemic diseases; however, further studies are required to confirm the significance of these biomarkers. A panel of biomarkers can be used to screen and assess systemic disease risk. As our knowledge of salivary biomarkers expands, the potential applications, interconnection, and common biomarkers for oral and systemic disease diagnosis will also grow. Table 10 summarizes various salivary biosensors used for various systemic diseases. In the future, there are rich possibilities that salivary diagnostics can be used as an effective tool for saving lives and preserving those already saved.
Table 10.
Summary of various salivary biosensors for systemic disease detection
| Systemic diseases | Salivary biomarkers | Salivary biosensors | References |
|---|---|---|---|
| Diabetes mellitus | Glucose | Salivary nanobiosensor | Zhang et al. [106] |
| HIV | Immunoglobulin | Electrochemical peptide-based biosensors | McQuistan et al. [107] |
| Cardiovascular diseases | CRP, Lactate |
Electro chemiluminescence biosensor Microchip assay biosensor |
Claver et al [108] Christodoulides et al [109] |
| Breast cancer |
ATP6AP1, CA15-3, CEA, CA125, HER- 2/neu |
Quartz crystal biosensor Surface plasma resonance biosensor Multiplexed microfluidic biosensor |
Arif et al. [53] Liang et al. [110] Jokerst et al. [111] |
| Hyperphosphatemia | Phosphate | Amperometric biosensor | Kwan et al. [112] |
Saliva-based diagnostics seems to be an important tool for regularly screening larger populations. However, further technology development and identification of robust and discriminatory sets of salivary biomarkers are required to apply saliva as a diagnostic tool in day-to-day practice. Saliva is non-invasive, easy to handle, and with the possibility of self-collection fluid—these characteristics are critical in a pandemic scenario, enabling less exposure to healthcare professionals.
Conclusions
This review paper highlights the need for saliva-based biosensors that can benefit patients and healthcare providers. It also reveals the importance of developing a system that can function based on salivary biomarkers for each systemic disease detection. From a healthcare professional's perspective, using a biosensor will allow faster results that do not always require a medical appointment. The data transferred from patient to doctor can be discussed and sent to multiple healthcare professionals, allowing for various opinions on the data analyzed by that biosensor. They would also allow cost-effective strategies to track patients and their disease progression and real-time monitoring. The development of whole saliva-based biosensors will be challenging due to the variation in the dietary habits of individuals. However, it will provide an efficient resource that can lower the risks of the progression of oral diseases and early prediction of other systemic diseases. Advances in machine learning and ultra-sensitive detector modalities will overcome big data issues and lower concentrations. AI and machine learning can help find relationships, nullifying variabilities like age, race, and food habits [80]. This knowledge will contribute to a better understanding and correlation between systemic and oral health. The main findings of this review are:
Saliva can be an alternative biological diagnostic fluid.
Non-invasive saliva collection facilitates a home-based diagnosis approach; however, more studies should be in place to incorporate saliva-based diagnostics into daily use.
While several questions remain open, the potential advantages of salivary analysis for diagnosing systemic disease suggest that further studies are warranted.
Saliva-based diagnosis is gaining attention after the covid pandemic, with oral health as an indicator of overall health, and dentists will have greater involvement in identifying non-oral or systemic diseases apart from their routine responsibilities.
Acknowledgements
The authors would like to acknowledge the financial support of NIH Funding 1 R01 DE031832-01, and Blazer foundation, Rockford, IL, USA.
Author Contributions
SS and MS-literature review, RAR-Manuscript editing. SG-Organize the tables and editing, HG- Editing, RW-Editing and review, RPP-Editing and supervising, MM-Editing supervising.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
There is no competing interest between authors on this submitted work.
References
- 1.Fábián TK, Hermann P, Beck A, Fejérdy P, Fábián G. Salivary defense proteins: their network and role in innate and acquired oral immunity. Int. J. Mol. Sci. 2012;13(4):4295–4320. doi: 10.3390/ijms13044295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.King RB, Bakos J, Hoff CD, Marko L. Poly(tertiary phosphines and arsines). 17. Poly(tertiary phosphines) containing terminal neomenthyl groups as ligands in asymmetric homogeneous hydrogenation catalysts. J. Org. Chem. 1979;44(18):3095–3100. doi: 10.1021/jo01332a001. [DOI] [Google Scholar]
- 3.Baumann T, Kozik J, Lussi A, Carvalho TS. Erosion protection conferred by whole human saliva, dialysed saliva, and artificial saliva. Sci. Rep. 2016;6(June):6–13. doi: 10.1038/srep34760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.A. Punj, Secretions of Human Salivary Gland, vol. i (IntechOpen, 2018), pp. 3–11. 10.5772/57353
- 5.Basbaum C, Tsuda T, Takeuchi K, Royce F, Jany B. Lysozyme and mucin cDNAs as tools for the study of serous and mucous cell differentiation. Chest. 1992;101(3 SUPPL.):45S–47S. doi: 10.1378/chest.101.3_Supplement.45S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Madalli VB. Saliva—a diagnostic tool. IOSR J. Dent. Med. Sci. 2013;11(6):96–99. doi: 10.9790/0853-1169699. [DOI] [Google Scholar]
- 7.Tiwari S, et al. Amylases: an overview with special reference to alpha amylase. J. Global Biosci. 2015;4(1):1886–1901. [Google Scholar]
- 8.de Almeida PDV. Saliva composition and functions: a comprehensive review. J. Contemp. Dent. Pract. 2008;9(3):2–80. [PubMed] [Google Scholar]
- 9.Roblegg E, Coughran A, Sirjani D. The composition, function and role of saliva in maintaining oral health: a review. Int. J. Contemp. Dent. Med. Rev. 2019;2017:133–141. doi: 10.15713/ins.ijcdmr.121. [DOI] [Google Scholar]
- 10.Proctor GB, Carpenter GH. Salivary secretion: mechanism and neural regulation. Monogr. Oral Sci. 2014;24:14–29. doi: 10.1159/000358781. [DOI] [PubMed] [Google Scholar]
- 11.Lee Y-H, Wong DT. Saliva: an emerging biofluid for early detection of diseases. Am. J. Dent. 2009;22(4):241–248. [PMC free article] [PubMed] [Google Scholar]
- 12.Kaufman E, Lamster IB. The diagnostic applications of saliva—a review. Crit. Rev. Oral Biol. Med. 2002;13(2):197–212. doi: 10.1177/154411130201300209. [DOI] [PubMed] [Google Scholar]
- 13.Wong DT. Salivary diagnostics powered by nanotechnologies, proteomics and genomics. J. Am. Dent. Assoc. 2006;137(3):313–321. doi: 10.14219/jada.archive.2006.0180. [DOI] [PubMed] [Google Scholar]
- 14.Malamud D. Saliva as a diagnostic fluid. Dent. Clin. N. Am. 2011;55(1):159–178. doi: 10.1016/j.cden.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoshizawa JM, Schafer CA, Schafer JJ, Farrell JJ, Paster BJ, Wong DTW. Salivary biomarkers: toward future clinical and diagnostic utilities. Clin. Microbiol. Rev. 2013;26(4):781–791. doi: 10.1128/CMR.00021-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abdul Rehman S, et al. Role of salivary biomarkers in detection of cardiovascular diseases (CVD) Proteomes. 2017 doi: 10.3390/proteomes5030021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gomar-Vercher S, Simón-Soro A, Montiel-Company JM, Almerich-Silla JM, Mira A. Stimulated and unstimulated saliva samples have significantly different bacterial profiles. PLoS ONE. 2018;13(6):1–12. doi: 10.1371/journal.pone.0198021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weber F, Barrantes A. Real-time formation of salivary films onto polymeric materials for dental applications: differences between unstimulated and stimulated saliva. Colloids Surf. B. 2017;154:203–209. doi: 10.1016/j.colsurfb.2017.03.022. [DOI] [PubMed] [Google Scholar]
- 19.Navazesh M. Methods for collecting saliva. Ann. N. Y. Acad. Sci. 1993;694:72–77. doi: 10.1111/j.1749-6632.1993.tb18343.x. [DOI] [PubMed] [Google Scholar]
- 20.Bhalla N, Jolly P, Formisano N, Estrela P. Introduction to biosensors. Essays Biochem. 2016;60(1):1–8. doi: 10.1042/EBC20150001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aita A, et al. SARS-CoV-2 identification and IgA antibodies in saliva: one sample two tests approach for diagnosis. Clin. Chim. Acta. 2020;510(September):717–722. doi: 10.1016/j.cca.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al Lawati HAJ, Hassanzadeh J. Dual-function 2D cobalt metal-organic framework embedded on paper as a point-of-care diagnostic device: application for the quantification of glucose. Anal. Chim. Acta. 2020;1139:15–26. doi: 10.1016/j.aca.2020.09.026. [DOI] [PubMed] [Google Scholar]
- 23.AlMoharib HS, AlMubarak A, AlRowis R, Geevarghese A, Preethanath RS, Anil S. Oral fluid based biomarkers in periodontal disease: Part 1. Saliva. J. Int. Oral Health JIOH. 2014;6(4):95–103. [PMC free article] [PubMed] [Google Scholar]
- 24.AlRowis R, AlMoharib HS, AlMubarak A, Bhaskardoss J, Preethanath RS, Anil S. Oral fluid-based biomarkers in periodontal disease—Part 2. Gingival crevicular fluid. J. Int. Oral Health JIOH. 2014;6(5):126–135. [PMC free article] [PubMed] [Google Scholar]
- 25.Rathnayake N, et al. Salivary biomarkers for detection of systemic diseases. PLoS ONE. 2013;8(4):e61356. doi: 10.1371/journal.pone.0061356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paluszkiewicz C, et al. Saliva as a first-line diagnostic tool: a spectral challenge for identification of cancer biomarkers. J. Mol. Liq. 2020 doi: 10.1016/j.molliq.2020.112961. [DOI] [Google Scholar]
- 27.Rahnama M, Czupkałło Ł, Kozicka-Czupkałło M, Łobacz M. Gingival crevicular fluid—composition and clinical importance in gingivitis and periodontitis. Pol. J. Public Health. 2014;2:8. doi: 10.2478/pjph-2014-0022. [DOI] [Google Scholar]
- 28.Atram P, Patil P, Saify F, Rathod V, Gotmare S. Gingival crevicular fluid: as a diagnostic marker in HIV positive patients. J. Int. Soc. Prev. Community Dent. 2015;5(1):24–30. doi: 10.4103/2231-0762.151969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park O-J, Kim J, Kim HY, Kwon Y, Yun C-H, Han SH. Streptococcus gordonii induces bone resorption by increasing osteoclast differentiation and reducing osteoblast differentiation. Microb. Pathog. 2019;126:218–223. doi: 10.1016/J.MICPATH.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 30.Kim AR, et al. Streptococcus gordonii lipoproteins induce IL-8 in human periodontal ligament cells. Mol. Immunol. 2017;91(September):218–224. doi: 10.1016/j.molimm.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 31.De Wijk RA, Prinz JF, Engelen L, Weenen H. The role of α-amylase in the perception of oral texture and flavour in custards. Physiol. Behav. 2004;83(1):81–91. doi: 10.1016/j.physbeh.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 32.Della Ventura B, Sakač N, Funari R, Velotta R. Flexible immunosensor for the detection of salivary α-amylase in body fluids. Talanta. 2017;174:52–58. doi: 10.1016/J.TALANTA.2017.05.075. [DOI] [PubMed] [Google Scholar]
- 33.Peng CH, Xia YC, Wu Y, Zhou ZF, Cheng P, Xiao P. Influencing factors for saliva urea and its application in chronic kidney disease. Clin. Biochem. 2013;46(3):275–277. doi: 10.1016/j.clinbiochem.2012.10.029. [DOI] [PubMed] [Google Scholar]
- 34.Evans R, et al. Diagnostic performance of a saliva urea nitrogen dipstick to detect kidney disease in Malawi. Kidney Int. Rep. 2017;2(2):219–227. doi: 10.1016/j.ekir.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kumar S, Panwar S, Kumar S, Augustine S, Malhotra BD. Biofunctionalized non-invasive impedometric biosensor for efficient detection of oral cancer. Nanomater. - MDPI. 2019;9(9):14. doi: 10.3390/nano9091190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Out D, Hall RJ, Granger DA, Page GG, Woods SJ. Assessing salivary C-reactive protein: longitudinal associations with systemic inflammation and cardiovascular disease risk in women exposed to intimate partner violence. Brain. Behav. Immun. 2012;26(4):543–551. doi: 10.1016/j.bbi.2012.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mirzaii-Dizgah I, Riahi E. Salivary high-sensitivity cardiac troponin T levels in patients with acute myocardial infarction. Oral Dis. 2013;19(2):180–184. doi: 10.1111/j.1601-0825.2012.01968.x. [DOI] [PubMed] [Google Scholar]
- 38.Mirzaii-Dizgah I, Jafari-Sabet M. Unstimulated whole saliva creatine phosphokinase in acute myocardial infarction. Oral Dis. 2011;17(6):597–600. doi: 10.1111/j.1601-0825.2011.01817.x. [DOI] [PubMed] [Google Scholar]
- 39.Foo JYY, et al. NT-ProBNP levels in saliva and its clinical relevance to heart failure. PLoS ONE. 2012;7(10):e48452. doi: 10.1371/journal.pone.0048452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hojo Y, Ikeda U, Ueno S, Arakawa H, Shimada K. Expression of matrix metalloproteinases in patients with acute myocardial infarction. Jpn. Circ. J. 2001;65(2):71–75. doi: 10.1253/jcj.65.71. [DOI] [PubMed] [Google Scholar]
- 41.Ayisi NK, Gupta SV, Qualtiere LF. Modified tetrazolium-based colorimetric method for determining the activities of anti-HIV compounds. J. Virol. Methods. 1991;33(3):335–344. doi: 10.1016/0166-0934(91)90033-v. [DOI] [PubMed] [Google Scholar]
- 42.Tuomainen AM, et al. Serum matrix metalloproteinase-8 concentrations are associated with cardiovascular outcome in men. Arterioscler. Thromb. Vasc. Biol. 2007;27(12):2722–2728. doi: 10.1161/ATVBAHA.107.154831. [DOI] [PubMed] [Google Scholar]
- 43.Salivary Biomarkers for Detection of Systemic Diseases. 10.1371/journal.pone.0061356 [DOI] [PMC free article] [PubMed]
- 44.Miller CS, et al. Utility of salivary biomarkers for demonstrating acute myocardial infarction. J. Dent. Res. 2014;93(7 Suppl):72S–79S. doi: 10.1177/0022034514537522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Satish BNVS, Srikala P, Maharudrappa B, Awanti SM, Kumar P, Hugar D. Saliva: a tool in assessing glucose levels in Diabetes Mellitus. J. Int. Oral Health. 2014;6(2):114–117. [PMC free article] [PubMed] [Google Scholar]
- 46.Xie Z, et al. Lnc-PCDH9-13:1 is a hypersensitive and specific biomarker for early hepatocellular carcinoma. EBioMedicine. 2018;33:57–67. doi: 10.1016/j.ebiom.2018.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.You XY, Jiang J, Yin FZ. Preliminary observation on human saliva alpha-fetoprotein in patients with hepatocellular carcinoma. Chin. Med. J. (Engl.) 1993;106(3):179–182. [PubMed] [Google Scholar]
- 48.González V, et al. Detection of hepatitis C virus antibodies in oral fluid specimens for prevalence studies. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2008;27(2):121–126. doi: 10.1007/s10096-007-0408-z. [DOI] [PubMed] [Google Scholar]
- 49.OraSure Technologies, Inc. Home. https://www.orasure.com/. Accessed 20 July 2021.
- 50.Drobnik A, Judd C, Banach D, Egger J, Konty K, Rude E. Public health implications of rapid hepatitis C screening with an oral swab for community-based organizations serving high-risk populations. Am. J. Public Health. 2011;101(11):2151–2155. doi: 10.2105/AJPH.2011.300251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Äyräväinen L, et al. Inflammatory biomarkers in saliva and serum of patients with rheumatoid arthritis with respect to periodontal status. Ann. Med. 2018;50(4):333–344. doi: 10.1080/07853890.2018.1468922. [DOI] [PubMed] [Google Scholar]
- 52.Mirrielees J, et al. Rheumatoid arthritis and salivary biomarkers of periodontal disease. J. Clin. Periodontol. 2010;37(12):1068–1074. doi: 10.1111/j.1600-051X.2010.01625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Arif S, Qudsia S, Urooj S, Chaudry N, Arshad A, Andleeb S. Blueprint of quartz crystal microbalance biosensor for early detection of breast cancer through salivary autoantibodies against ATP6AP1. Biosens. Bioelectron. 2015;65:62–70. doi: 10.1016/j.bios.2014.09.088. [DOI] [PubMed] [Google Scholar]
- 54.Streckfus CF, Arreola D, Edwards C, Bigler L. Salivary protein profiles among HER2/neu-receptor-positive and -negative breast cancer patients: support for using salivary protein profiles for modeling breast cancer progression. J. Oncol. 2012;2012:e413256. doi: 10.1155/2012/413256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Streckfus C, Bigler L, Tucci M, Thigpen JT. A preliminary study of CA15-3, c-erbB-2, epidermal growth factor receptor, cathepsin-D, and p53 in saliva among women with breast carcinoma. Cancer Investig. 2000;18(2):101–109. doi: 10.3109/07357900009038240. [DOI] [PubMed] [Google Scholar]
- 56.Streckfus C, Bigler L, Tucci M, Thigpen JT. A preliminary study of CA15-3, c-erbB-2, epidermal growth factor receptor, cathepsin-D, and p53 in saliva among women with breast carcinoma. Cancer Invest. 2000;18(2):101–109. doi: 10.3109/07357900009038240. [DOI] [PubMed] [Google Scholar]
- 57.Laidi F, Bouziane A, Errachid A, Zaoui F. Usefulness of salivary and serum auto-antibodies against tumor biomarkers HER2 and MUC1 in breast cancer screening. Asian Pac. J. Cancer Prev. 2016;17(1):335–339. doi: 10.7314/APJCP.2016.17.1.335. [DOI] [PubMed] [Google Scholar]
- 58.Porto-Mascarenhas EC, et al. Salivary biomarkers in the diagnosis of breast cancer: a review. Crit. Rev. Oncol. Hematol. 2017;110:62–73. doi: 10.1016/j.critrevonc.2016.12.009. [DOI] [PubMed] [Google Scholar]
- 59.Grody WW. Cystic fibrosis: molecular diagnosis, population screening, and public policy. Arch. Pathol. Lab. Med. 1999;123(11):1041–1046. doi: 10.5858/1999-123-1041-CF. [DOI] [PubMed] [Google Scholar]
- 60.Davis PB. Pathophysiology of cystic fibrosis with emphasis on salivary gland involvement. J. Dent. Res. 1987;66:667–671. doi: 10.1177/00220345870660S210. [DOI] [PubMed] [Google Scholar]
- 61.Parisi MR, et al. Point-of-care testing for HCV infection: recent advances and implications for alternative screening. New Microbiol. 2014;37(4):449–457. [PubMed] [Google Scholar]
- 62.Foley JD, et al. Salivary biomarkers associated with myocardial necrosis: results from an alcohol septal ablation model. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012;114(5):616–623. doi: 10.1016/j.oooo.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gupta S, Nayak MT, Sunitha J, Dawar G, Sinha N, Rallan NS. Correlation of salivary glucose level with blood glucose level in diabetes mellitus. J. Oral Maxillofac. Pathol. 2017;21(3):334–339. doi: 10.4103/jomfp.JOMFP_222_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.McNeely TB, Dealy M, Dripps DJ, Orenstein JM, Eisenberg SP, Wahl SM. Secretory leukocyte protease inhibitor: a human saliva protein exhibiting anti-human immunodeficiency virus 1 activity in vitro. J. Clin. Invest. 1995;96(1):456–464. doi: 10.1172/JCI118056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wotman S, Baer L, Mandel ID, Laragh JH. Salivary electrolytes, renin, and aldosterone during sodium loading and depletion. J. Appl. Physiol. 1973;35(3):322–324. doi: 10.1152/jappl.1973.35.3.322. [DOI] [PubMed] [Google Scholar]
- 66.Slomiany BL, Murty VL, Slomiany A. Salivary lipids in health and disease. Prog. Lipid Res. 1985;24(4):311–324. doi: 10.1016/0163-7827(85)90009-8. [DOI] [PubMed] [Google Scholar]
- 67.Actis AB, Perovic NR, Defagó D, Beccacece C, Eynard AR. Fatty acid profile of human saliva: a possible indicator of dietary fat intake. Arch. Oral Biol. 2005;50(1):1–6. doi: 10.1016/j.archoralbio.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 68.Freel SA, et al. Characterization of human immunodeficiency virus type 1 in saliva and blood plasma by V3-specific heteroduplex tracking assay and genotype analyses. J. Virol. 2001;75(10):4936–4940. doi: 10.1128/JVI.75.10.4936-4940.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Granade TC, et al. Detection of antibodies to human immunodeficiency virus type 1 in oral fluids: a large-scale evaluation of immunoassay performance. Clin. Diagn. Lab. Immunol. 1998;5(2):171–175. doi: 10.1128/CDLI.5.2.171-175.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Delaney KP, et al. Performance of an oral fluid rapid HIV-1/2 test: experience from four CDC studies. AIDS Lond. Engl. 2006;20(12):1655–1660. doi: 10.1097/01.aids.0000238412.75324.82. [DOI] [PubMed] [Google Scholar]
- 71.O. of the Commissioner. Facts About In-Home HIV Testing. FDA, Sep. 2020, Accessed 20 July 2021. [Online]. https://www.fda.gov/consumers/consumer-updates/facts-about-home-hiv-testing
- 72.Ratner L, et al. Complete nucleotide sequence of the AIDS virus, HTLV-III. Nature. 1985;313(6000):6000. doi: 10.1038/313277a0. [DOI] [PubMed] [Google Scholar]
- 73.Hodinka RL, Nagashunmugam T, Malamud D. Detection of human immunodeficiency virus antibodies in oral fluids. Clin. Diagn. Lab. Immunol. 1998;5:419–426. doi: 10.1128/CDLI.5.4.419-426.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Estévez PT, Satoguina J, Nwakanma DC, West S, Conway DJ, Drakeley CJ. Human saliva as a source of anti-malarial antibodies to examine population exposure to Plasmodium falciparum. Malar. J. 2011;10(1):104. doi: 10.1186/1475-2875-10-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.de Molon RS, Rossa C, Thurlings RM, Cirelli JA, Koenders MI. Linkage of periodontitis and rheumatoid arthritis: current evidence and potential biological interactions. Int. J. Mol. Sci. 2019 doi: 10.3390/ijms20184541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Eftekhari A, Hasanzadeh M, Sharifi S, Dizaj SM, Khalilov R, Ahmadian E. Bioassay of saliva proteins: the best alternative for conventional methods in non-invasive diagnosis of cancer. Int. J. Biol. Macromol. 2019;124:1246–1255. doi: 10.1016/j.ijbiomac.2018.11.277. [DOI] [PubMed] [Google Scholar]
- 77."PCR Test for COVID-19: What it Is, How its Done, What the Results Mean. Cleveland Clinic. https://my.clevelandclinic.org/health/diagnostics/21462-covid-19-and-pcr-testing. Accessed 17 July 2021
- 78.J. Bardill, N.A. Garrison, Genetic Ancestry Testing. (2015).
- 79.Labat C, et al. Inflammatory mediators in saliva associated with arterial stiffness and subclinical atherosclerosis. J. Hypertens. 2013;31(11):2251–2258. doi: 10.1097/HJH.0b013e328363dccc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Patil S, Albogami S, Hosmani J, Mujoo S, Kamil MA, Mansour MA, Abdul HN, Bhandi S, Ahmed SSSJ. Artificial intelligence in the diagnosis of oral diseases: applications and pitfalls. Diagnostics (Basel). 2022;12(5):1029. doi: 10.3390/diagnostics12051029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kosaka T, et al. Salivary inflammatory cytokines may be novel markers of carotid atherosclerosis in a Japanese general population: the Suita study. Atherosclerosis. 2014;237(1):123–128. doi: 10.1016/j.atherosclerosis.2014.08.046. [DOI] [PubMed] [Google Scholar]
- 82.Pay JB, Shaw AM. Towards salivary C-reactive protein as a viable biomarker of systemic inflammation. Clin. Biochem. 2019;68:1–8. doi: 10.1016/j.clinbiochem.2019.04.006. [DOI] [PubMed] [Google Scholar]
- 83.Zheng H, et al. Salivary biomarkers indicate obstructive sleep apnea patients with cardiovascular diseases. Sci. Rep. 2014;4:7046. doi: 10.1038/srep07046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Aitken JP, et al. α-2-macroglobulin in saliva is associated with glycemic control in patients with type 2 diabetes mellitus. Dis. Markers. 2015;2015:128653. doi: 10.1155/2015/128653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Xu Z, et al. Saliva-coated titanium biosensor detects specific bacterial adhesion and bactericide caused mass loading upon cell death. Biosens. Bioelectron. 2019;129:198–207. doi: 10.1016/J.BIOS.2019.01.035. [DOI] [PubMed] [Google Scholar]
- 86.Zou C-S, et al. Preparation of disposable saliva α-amylase biosensor. Chin. J. Anal. Chem. 2008;36(9):1217–1220. doi: 10.1016/S1872-2040(08)60068-7. [DOI] [Google Scholar]
- 87.Soni A, Surana RK, Jha SK. Smartphone based optical biosensor for the detection of urea in saliva. Sens. Actuators B Chem. 2018;269:346–353. doi: 10.1016/J.SNB.2018.04.108. [DOI] [Google Scholar]
- 88.Zangheri M, et al. Chemiluminescence-based biosensor for monitoring astronauts' health status during space missions: results from the International Space Station. Biosens. Bioelectron. 2019;129(July):260–268. doi: 10.1016/j.bios.2018.09.059. [DOI] [PubMed] [Google Scholar]
- 89.Griesche C, Baeumner AJ. Biosensors to support sustainable agriculture and food safety. TrAC. 2020;128:115906. doi: 10.1016/j.trac.2020.115906. [DOI] [Google Scholar]
- 90.Malvano F, Pilloton R, Albanese D. A novel impedimetric biosensor based on the antimicrobial activity of the peptide nisin for the detection of Salmonella spp. Food Chem. 2020;325(April):126868. doi: 10.1016/j.foodchem.2020.126868. [DOI] [PubMed] [Google Scholar]
- 91.Abid SA, et al. Biosensors as a future diagnostic approach for COVID-19. Life Sci. 2021;273(October):119117. doi: 10.1016/j.lfs.2021.119117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gupta V, Kaur A. Salivary glucose levels in diabetes mellitus patients: a case-control study. J. Oral Maxillofac. Pathol. 2020;24(1):187. doi: 10.4103/jomfp.JOMFP_15_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mascarenhas P, Fatela B, Barahona I. Effect of diabetes mellitus type 2 on salivary glucose—a systematic review and meta-analysis of observational studies. PLoS ONE. 2014;9(7):e101706. doi: 10.1371/journal.pone.0101706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bhattacharyya A, Chandra S, Singh A, Raj V, Gupta B. Salivary glucose levels and oral candidal carriage in Type 2 diabetics. J. Oral Biol. Craniofacial Res. 2018;8(3):158–164. doi: 10.1016/j.jobcr.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pérez-Ros P, Navarro-Flores E, Julián-Rochina I, Martínez-Arnau FM, Cauli O. Changes in salivary amylase and glucose in diabetes: a scoping review. Diagn. Basel Switz. 2021;11(3):453. doi: 10.3390/diagnostics11030453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Amer S, Yousuf M, Siddqiui PQ, Alam J. Salivary glucose concentrations in patients with diabetes mellitus—a minimally invasive technique for monitoring blood glucose levels. Pak. J. Pharm. Sci. 2001;14(1):33–37. [PubMed] [Google Scholar]
- 97.Naseri R, Mozaffari HR, Ramezani M, Sadeghi M. Effect of diabetes mellitus type 2 on salivary glucose, immunoglobulin A, total protein, and amylase levels in adults: a systematic review and meta-analysis of case-control studies. J. Res. Med. Sci. 2018;23:89. doi: 10.4103/jrms.JRMS_135_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Indira M, Chandrashekar P, Kattappagari KK, Chandra LPK, Chitturi RT, Bv RR. Evaluation of salivary glucose, amylase, and total protein in Type 2 diabetes mellitus patients. Indian J. Dent. Res. 2015;26(3):271–275. doi: 10.4103/0970-9290.162883. [DOI] [PubMed] [Google Scholar]
- 99.Abd-Elraheem SE, El Saeed AM, Mansour HH. Salivary changes in type 2 diabetic patients. Diabetes Metab. Syndr. 2017;11(Suppl 2):S637–S641. doi: 10.1016/j.dsx.2017.04.018. [DOI] [PubMed] [Google Scholar]
- 100.Mrag M, et al. Saliva diagnostic utility in patients with type 2 diabetes: future standard method. J. Med. Biochem. 2020;39(2):140–148. doi: 10.2478/jomb-2019-0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Cha YJ, et al. Performance evaluation of the OraQuick hepatitis C virus rapid antibody test. Ann. Lab. Med. 2013;33(3):184–189. doi: 10.3343/alm.2013.33.3.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Augustine SAJ, et al. Rapid salivary IgG antibody screening for hepatitis A. J. Clin. Microbiol. 2020 doi: 10.1128/JCM.00358-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Bıyıkoğlu B, et al. Periodontal therapy in chronic periodontitis lowers gingival crevicular fluid interleukin-1beta and DAS28 in rheumatoid arthritis patients. Rheumatol. Int. 2013;33(10):2607–2616. doi: 10.1007/s00296-013-2781-5. [DOI] [PubMed] [Google Scholar]
- 104.Hitchon CA, et al. Antibodies to porphyromonas gingivalis are associated with anticitrullinated protein antibodies in patients with rheumatoid arthritis and their relatives. J. Rheumatol. 2010;37(6):1105–1112. doi: 10.3899/jrheum.091323. [DOI] [PubMed] [Google Scholar]
- 105.Okada M, Kobayashi T, Ito S, Yokoyama T, Abe A, Murasawa A, Yoshie H. Periodontal treatment decreases levels of antibodies to porphyromonas gingivalis and citrulline in patients with rheumatoid arthritis and periodontitis. J. Periodontol. 2013;84(12):e74–e84. doi: 10.1902/jop.2013.130079. [DOI] [PubMed] [Google Scholar]
- 106.Zhang W, Du Y, Wang ML. Non-invasive glucose monitoring using saliva nano-biosensor. Sens. Bio-Sens. Res. 2015;4:23–29. doi: 10.1016/j.sbsr.2015.02.002. [DOI] [Google Scholar]
- 107.Use of thiolated oligonucleotides as anti-fouling diluents in electrochemical peptide-based sensors - Chemical Communications (RSC Publishing). https://pubs.rsc.org/en/content/articlelanding/2014/cc/c4cc01290a#!divAbstract. Accessed 7 June 2021. [DOI] [PubMed]
- 108.Claver JB, Mirón MCV, Capitán-Vallvey LF. Disposable electrochemiluminescent biosensor for lactate determination in saliva. Analyst. 2009;134(7):1423–1432. doi: 10.1039/B821922B. [DOI] [PubMed] [Google Scholar]
- 109.Christodoulides N, et al. Application of microchip assay system for the measurement of C-reactive protein in human saliva. Lab. Chip. 2005;5(3):261–269. doi: 10.1039/b414194f. [DOI] [PubMed] [Google Scholar]
- 110.Liang Y-H, Chang C-C, Chen C-C, Chu-Su Y, Lin C-W. Development of an Au/ZnO thin film surface plasmon resonance-based biosensor immunoassay for the detection of carbohydrate antigen 15–3 in human saliva. Clin. Biochem. 2012;45(18):1689–1693. doi: 10.1016/j.clinbiochem.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 111.Jokerst JV, et al. Nano-bio-chips for high performance multiplexed protein detection: determinations of cancer biomarkers in serum and saliva using quantum dot bioconjugate labels. Biosens. Bioelectron. 2009;24(12):3622–3629. doi: 10.1016/j.bios.2009.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kwan RCH, Leung HF, Hon PYT, Cheung HCF, Hirota K, Renneberg R. Amperometric biosensor for determining human salivary phosphate. Anal. Biochem. 2005;343(2):263–267. doi: 10.1016/j.ab.2005.05.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.