Abstract
T cells are important in preventing severe disease from SARS-CoV-2, but scalable and field-adaptable alternatives to expert T-cell assays are needed. The interferon-gamma release assay QuantiFERON platform was developed to detect T-cell responses to SARS-CoV-2 from whole blood with relatively basic equipment and flexibility of processing timelines. Forty-eight participants with different infection and vaccination backgrounds were recruited. Whole blood samples were analysed using the QuantiFERON SARS-CoV-2 assay in parallel with the well-established ‘Protective Immunity from T Cells in Healthcare workers’ (PITCH) ELISpot, which can evaluate spike-specific T-cell responses. The primary aims of this cross-sectional observational cohort study were to establish if the QuantiFERON SARS-Co-V-2 assay could discern differences between specified groups and to assess the sensitivity of the assay compared with the PITCH ELISpot. The QuantiFERON SARS-CoV-2 distinguished acutely infected individuals (12–21 days post positive PCR) from naïve individuals (P < 0.0001) with 100% sensitivity and specificity for SARS-CoV-2 T cells, whilst the PITCH ELISpot had reduced sensitivity (62.5%) for the acute infection group. Sensitivity with QuantiFERON for previous infection was 12.5% (172–444 days post positive test) and was inferior to the PITCH ELISpot (75%). Although the QuantiFERON assay could discern differences between unvaccinated and vaccinated individuals (55–166 days since second vaccination), the latter also had reduced sensitivity (44.4%) compared to the PITCH ELISpot (66.6%). The QuantiFERON SARS-CoV-2 assay showed potential as a T- cell evaluation tool soon after SARS-CoV-2 infection but has lower sensitivity for use in reliable evaluation of vaccination or more distant infection.
Keywords: QuantiFERON, SARS-CoV-2, T cells, ELISpot, COVID-19
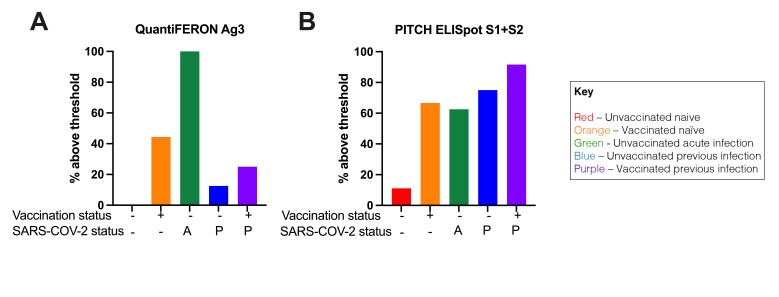
With the exception of acute infection group, the PITCH ELISpot S1 + S2 had greater sensitivity for SARS-CoV-2 specific T-cell responses compared with the QuantiFERON SARS-CoV-2 assay tube Ag3.
Graphical Abstract
Graphical Abstract.
Introduction
COVID-19 is a respiratory infection caused by SARS-CoV-2 with a recorded global burden of more than 500 million confirmed cases and over 6 million deaths [1]. We and others have sought to characterize the immunological response to SARS-CoV-2 both following natural infection and vaccination [2–11]. T cells are an important component of the immune response to SARS-CoV-2 infection and vaccination, persisting for several months post infection [4, 8–10, 12–16]. T cells have also been extensively studied following vaccination alone [4, 5, 17–20] as well as in participants with combined past SARS-CoV-2 infection [5, 17].
Multiple assay platforms, including the ex vivo interferon-gamma enzyme-linked absorbent spot (IFN-γ ELISpot), activation-induced cell marker (AIM), intracellular staining (ICS), T-cell proliferation assays, and whole blood IFN-γELISA assays, can be employed to evaluate T-cell responses. Although these assays provide characterization of T-cell function, they can be time-consuming and require extensive laboratory reagents, equipment as well as expertise within hours of blood draw for reliable results.
The QuantiFERON SARS-CoV-2 assay is based on the well-characterized QuantiFERON TB interferon-gamma release assay (IGRA) [21]. The basis for this platform is a whole blood cell-stimulation assay with plasma harvest for IFN-γ ELISA evaluation. The advantage of this platform is the workflow is straight forward to follow with tolerance for pause between steps which could accommodate various levels of expertise and diverse clinical/research settings including in low- and middle-income countries. A handful of studies have utilized the QuantiFERON SARS-CoV-2 assay with PITCH [21–29]. A small internal feasibility study carried out by Qiagen found quantifiable responses to vaccination over the course of 4 weeks after second vaccination [21]. When analyzing T-cell responses after SARS-CoV-2 infection, the study showed detectable responses in three out of four participants with the assay. However, an important limitation of this small study was the lack of reference to a well-established cell-based assay to evaluate the potential of the QuantiFERON SARS-CoV-2 assay to accurately assess T-cell responses.
Therefore, the present study sought to evaluate T-cell responses using the QuantiFERON SARS-CoV-2 assay with parallel analysis using the well-established protective immunity from T cells to Covid-19 in Health workers (PITCH) ELISpot [4–6, 17, 30] following SARS-CoV-2 infection and vaccination. The study also explored the sensitivity and specificity of the QuantiFERON SARS-CoV-2 assay in detecting SARS-CoV-2-specific T-cell responses. Herein we present data to demonstrate a potential role for QuantiFERON SARS-CoV-2 as a reliable T-cell evaluation tool soon after SARS-CoV-2 infection, but with low sensitivity compared to the conventional ELISpot assay for studying T cells following vaccination.
Materials and Methods
Study design and participant recruitment
Participants were sampled in the community or OPTIC (Oxford Protective T cell Immunity against COVID-19) study clinic in Oxford, UK once each between 9 and 18 June 2021.
Forty-eight participants were invited to participate by word of mouth and email communication of local healthcare workers, research scientists, and students and informed consent was obtained under one of two studies: The GI Biobank Study 16/YH/0247, approved by the research ethics committee (REC) at Yorkshire & The Humber—Sheffield Research Ethics Committee on 29 July 2016, which had been amended for this purpose on 8 June 2020 or the Family Study R71346/RE001, approved by Oxford University’s Medical Sciences Inter-Divisional REC (MS-IDREC-R71346/RE00). Our target was 10 participants per group as a feasible number allowing meaningful statistical comparison, although no formal power calculation was performed.
Participants were sampled in the community or at the OPTIC study clinic in Oxford, UK once each during the month of June 2021. Following blood draw, samples for the QuantiFERON SARS-CoV-2 assay were kept at 4–8 °C degrees for up to 48 h before processing. The rest of the sample was used for isolation of peripheral blood mononuclear cells (PBMC) that were cryopreserved on the sample day and frozen for future use in the PITCH ELISpot assay. Participants were designated as naïve or previously infected for SARS-CoV-2 based on a positive PCR and/or serology at any time. Acute SARS-CoV-2 infection group was classified as blood sampling 12–21 days since a positive PCR test. For vaccination status, participants were designated as unvaccinated or vaccinated according to self-reported status. Serological status was determined using the Mesoscale Discovery (MSD) assay as described below, with a positive result for anti-S and/or anti-N supporting previous infection in an unvaccinated participant, and a positive result for anti-N supporting previous infection in a vaccinated participant (Supplementary Figure 1) meriting their exclusion from analysis.
QuantiFERON SARS-CoV-2 assay
SARS-CoV-2-specific T cells were analyzed using the QuantiFERON SARS-CoV-2 Research Use Only platform. The QuantiFERON SARS-CoV-2 Starter Pack (Qiagen, cat. no. 626115), Extended Pack (Qiagen, cat. no. 626215), and Control Set (Qiagen, cat. no. 626015) were employed, consisting of assay tubes coated with one of three sets of selected SARS-CoV-2 T cell antigens: Ag1-CD4+ T-cell epitopes from the S1 subunit (receptor binding domain) of the SARS-CoV-2 spike protein, Ag2-CD4+ and CD8+ epitopes from the S1 and S2 subunits of the SARS-CoV-2 spike protein and Ag3 (Extended Pack)-CD4+ and CD8+ epitopes from S1 and S2, as in Ag2, but also immunodominant CD8+ epitopes of the whole proteome. The Control pack contains a ‘Nil tube’ which serves as the negative control and a ‘Mitogen tube’ which serves as a positive control.
The QuantiFERON SARS-CoV-2 kits were used in accordance with the manufacturer’s instructions. Whole blood samples, 0.8–1.2 ml, were collected directly into the assay collection tubes or into lithium heparin blood tubes for later transfer to the assay tubes. Assay tubes containing the whole blood were shaken and incubated for 16–24 hours at 37°C before centrifugation at 2500 × g for 15 minutes. Plasma was harvested from the top layer of the tube by gentle pipetting before being subjected to IFN-γELISA (Qiagen, cat. no. 626410). Following ELISA, quantitative results (IFN-γ concentration in IU/ml) were generated by subtracting the ‘Nil’ values from samples and interpolating values using an 8-parameter logistic model standard curve. The threshold to designate responses as positive was 0.2, as recommended by the manufacturer [21]. A total of 6–7 ml whole blood per participant time point was required for the three antigen tubes and controls. Samples were collected and processed in random order with the technician blinded to study group status to mitigate performance and verification bias.
Isolation of peripheral blood mononuclear cells (PBMC), plasma, and serum
PBMCs and plasma were isolated by density gradient centrifugation from 10 ml blood collected in EDTA tubes, and serum was collected in a serum-separating tube (SST, Becton Dickinson) as previously described [4]. Briefly, PBMCs were isolated by density gradient centrifugation using LymphoprepTM (P = 1.077 g/ml, Stem Cell Technologies), washed twice with R0 (RPMI 1640 (Sigma, St. Louis, MO, USA) containing 10 mM Pen/Strep (100 U/mL) and 2 mM L-glutamine (100 μg/mL) (Sigma)) and resuspended in R10 (R0 supplemented with 10% FBS) or AutoMACs Rinse Buffer and counted using the Guava® ViaCountTM assay on the Muse Cell Analyzer (Luminex Cooperation). PBMCs were resuspended in freezing mix (FBS with 10% DMSO) and frozen down to −80 °C before storage in liquid nitrogen. To obtain plasma, the uppermost fraction following the initial Lymphoprep centrifugation above was collected and centrifuged at 2000 × g for 10 minutes to remove platelets before storage at −80°C. Donor blood was also collected in a serum-separating tube (SST, Becton Dickinson) which was centrifuged at 2000 × g for 10 minutes. Serum was removed and stored at −80°C. As for the QuantiFERON testing, samples were randomized for processing with the technician blinded to study group status in order to mitigate performance and verification bias.
In-house PITCH ELISpot assay
The PITCH ELISpot Standard Operating Procedure (SOP) is available as published previously [17]. Ex vivo IFN-γ ELISpot assays were set up from cryopreserved peripheral blood mononuclear cells (PBMCs) using the Human IFN-γ ELISpot Basic kit (Mabtech 3420-2A). MultiScreen-IP filter plates (Millipore, MAIPS4510) were coated with 50 μl/well using the ELISpot Basic Kit Capture antibody (clone 1-D1K) at 10 μg/ml diluted in sterile phosphate buffered saline (PBS; Fisher Scientific) or sterile carbonate bicarbonate (Sigma Aldrich) for 8 to 48 h at 4°C. PBMCs were thawed and resuspended in Rab10 (filtered R0 media (Sigma) supplemented with 10% Human serum) with DNase and allowed to rest for 2–3 h in an incubator at 37°C, 5% CO2, 95% humidity prior to stimulation with peptides. The capture antibody coated plates were washed twice with R0, then blocked with 100 μL/well of Rab10 for 1/2-8 h at RT or 8–48 h at 4°C. Rested cells were centrifuged and resuspended in 1 ml Rab10 for counting on MuseTM Cell Analyser or Bio-Rad TC10TM Automated Cell Counter. After blocking, overlapping peptide pools (18-mers with 10 amino acid overlap Mimotopes) representing the spike (S1 + S2), Membrane (M), or nucleocapsid (NP) SARS-CoV-2 proteins were added to 200,000 PBMCs/well at a final concentration of 2 μg/ml for 16–18 h. S1 and S2 were added in separate test wells, M and NP were combined in a singular test well. Pools consisting of CMV, EBV and influenza peptides at a final concentration of 2 μg/ml (CEF; Proimmune) and concanavalin A (ConA) at a final concentration of 5 μg/ml were used as positive controls. DMSO was used as the negative control at the equivalent concentration to the peptides. After cell stimulation overnight, wells were washed 7 times 100–200 μl/well with PBS with 0.05% (v/v) Tween 20 (Sigma-Aldrich) and incubated with 50 μl/well of the ELISpot Basic kit biotinylated detection antibody (clone 7-B6-1) diluted in PBS at 1 μg/ml, for 2–4 h at room temperature (RT). Wells were then washed 7 times with 100–200 μL/well PBS-0.05% (v/v) Tween20, and then incubated with 50 μL/well of the ELISpot Basic kit streptavidin-ALP, diluted in PBS at 1 μg/ml for 1–2 h at RT. Wells were then washed 7 times with 100–200 μL/well PBS-0.05% Tween 20 and colour development was carried out using the 1-step NBT/BCIP Substrate Solution. Fifty microlitres of filtered NBT/BCIP were added to each well for 5–7 minutes in the dark at RT. Colour development was stopped by washing the wells with cold tap water. Air dried plates were scanned and analyzed with the CTL Cellular Technologies Series 6 ALFA. Antigen-specific responses were quantified by subtracting the mean spots of the control wells from the test wells and the results were expressed as spot-forming units (SFU)/106 PBMCs. Responses were defined as positive if values were greater than the mean of the DMSO control + 2 SD with a minimum of 20 SFCs per 1 million PBMCs [4].
MSD binding assay
IgG responses to SARS-CoV-2 were measured using a multiplexed MSD immunoassay: The V-PLEX COVID-19 Coronavirus Panel 3 (IgG) Kit from Meso Scale Diagnostics, Rockville, MD USA. A MULTI-SPOT® 96-well, 10 spot plate was coated with three SARS CoV-2 antigens (S, RBD, N) and bovine serum albumin. Antigens were spotted at 200 − 400 μg/mL (MSD® Coronavirus Plate 3). Multiplex MSD assays were performed as per the instructions of the manufacturer. To measure IgG antibodies, 96-well plates were blocked with MSD Blocker A for 30 minutes. Following washing with washing buffer, samples diluted 1:1000–10,000 in diluent buffer, or MSD standard or undiluted internal MSD controls, were added to the wells. After 2 h incubation and a washing step, detection antibody (MSD SULFO-TAG Anti-Human IgG Antibody, 1/200) was added. Following washing, MSD GOLD Read Buffer B was added and plates were read using a MESO® SECTOR S 600 Reader. The standard curve was established by fitting the signals from the standard using a 4-parameter logistic model. Concentrations of samples were determined from the electrochemiluminescence signals by back-fitting to the standard curve and multiplied by the dilution factor. Concentrations are expressed in arbitrary units per millilitre. Cut-offs were determined for each SARS-CoV-2 antigen (S, RBD, and N) based on the concentrations measured in 103 pre-pandemic sera + 3 SD as previously published [5]. Cut-off for S: 1160 AU/ml; cut-off for RBD: 1169 AU/ml; cut-off for N: 3874 AU/ml. Samples were processed blindly to mitigate performance and verification bias.
Statistical analyses
Data were analysed by non-parametric tests: Mann–Whitney for non-paired comparisons between two groups and Kruskal–Wallis with Dunn’s correction for comparisons between multiple groups. QuantiFERON SARS-CoV-2 assay data were transformed log10 with zero values y = (log x + 1). Correlation studies to compare values from different assays was calculated using Spearman correlation coefficient using linear values. To calculate sensitivity, specificity, positive predictive value and negative predictive value, the gold standard was designated as the ‘clinical phenotype’(CP)—self-reported vaccination or infection, with input from the MSD antibody binding assay. The threshold above which a sample was designated as ‘positive’ was designated as 0.2 IU/ml (as per manufacturer [21]) for QuantiFERON and as mean of the negative + 2 SD [4] for PITCH ELISpot. Five tests were assessed: QuantiFERON SARS-CoV-2 Ag1, Ag2 and Ag3 and PITCH ELISpot S1 + S2 and M + NP. For any of the given tests, a true positive (TP) was designated as being above threshold in CP+. A true negative (TN) was below threshold in CP−. A false positive (FP) was above threshold in CP−. A false negative was below threshold in CP+. To calculate sensitivity, specificity, positive predictive values (PPV) and negative predictive values, a 2 × 2 table was designed for each test and the following formulae applied: sensitivity = TP/TP + FN; specificity = TN/TN + FP; PPV = TP/TP + FP and NPV = TN/TN + FN.
GraphPad Prism v9.1.0 was used for statistical analysis and graphical representation.
Results
Participants of the study
Participants were recruited in June 2021 when the delta variant of SARS-CoV-2 was the dominant variant [31]. Participants were assigned into 5 groups based on previous SARS-CoV-2 infection and vaccination status: Unvaccinated Naïve, Vaccinated Naïve, Unvaccinated Acute Infection, Unvaccinated Previous Infection, and Vaccinated Previous Infection. Prior to data analysis, anti-S and anti-N antibodies were measured by Meso Scale discovery (MSD) assay to exclude asymptomatic previous infection status (Supplementary Figure 1) resulting in two participants being excluded from further analysis. One was excluded from the ‘unvaccinated naïve’ as they had positive Spike IgG, suggesting previous infection/vaccination. The other was excluded from the ‘vaccinated naïve’ group as they had positive N IgG suggesting previous infection. None of the participants who had previous infection required hospitalisation. Demographic information about the 46 participants included in the analysis is shown in Table 1. The age of the participants ranged from 18 to 56 with a median age of 24. Unvaccinated individuals were younger than vaccinated individuals (median 23 v median 28, respectively, P = 0.002) due to the progress of the national vaccination programme at the time of sampling (Table 1). There was no statistically significant difference between the median age of naïve and previously infected (27 v. 24, respectively, P = 0.18). In general, gender balance was achieved—except for the unvaccinated, acute infection group who were all participants from an outbreak in a local women’s rugby team. The participants in all groups predominantly identified as being of ‘white’ ethnicity. Most recipients received the Pfizer/BioNTech BNT162b2 vaccine reflecting the national vaccination roll out in the UK for this age group, with the remainder receiving the Oxford/AstraZeneca AZD1222 vaccine.
Table 1.
Characteristics of participants in this study
| Unvaccinated naive | Vaccinated naive |
Unvaccinated acute infection |
Unvaccinated previous infection |
Vaccinated previous infection |
|
|---|---|---|---|---|---|
| Number of subjects | 9 | 9 | 8 | 8 | 12 |
| Age, median (range) | 23 (22, 37) | 30.1 (27, 46) | 26 (19, 33) | 23 (18, 24) | 25.2 (21, 56) |
| Gender | |||||
| Male | 5 (55.5%) | 3 (33.3%) | 0 (0%) | 4 (50%) | 6 (50%) |
| Female | 4 (44.4%) | 6 (66.6%) | 8 (100%) | 4 (50%) | 6 (50%) |
| Other | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Ethnicity | |||||
| White | 5 (55.5%) | 7 (77.7%) | 7 (87.5%) | 7 (87.5%) | 9 (75%) |
| Black | 1 (11.1%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (8.33%) |
| Asian | 2 (22.2%) | 1 (11.1%) | 0 (0%) | 1 (12.5%) | 1 (8.33%) |
| Mixed | 1 (11.1%) | 0 (0%) | 1 (12.5%) | 0 (0%) | 1 (8.33%) |
| Other | 0 (0%) | 1 (11.1%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Vaccine | |||||
| Pfizer BNT162b2 | N/A | 8 (88.8%) | N/A | N/A | 8 (75%) |
| Oxford/AstraZeneca AZD1222 | N/A | 1 (11.1%) | N/A | N/A | 4 (25%) |
| Days since V2, median (range) | N/A | 102 (55, 166) | N/A | N/A | 65 (54, 160) |
| Days since SARS-COV-2, median (range) | N/A | N/A | 16 (12, 21) | 256 (172, 444) | 221 (145, 433) |
QuantiFERON SARS-CoV-2 in SARS-CoV-2-infected individuals
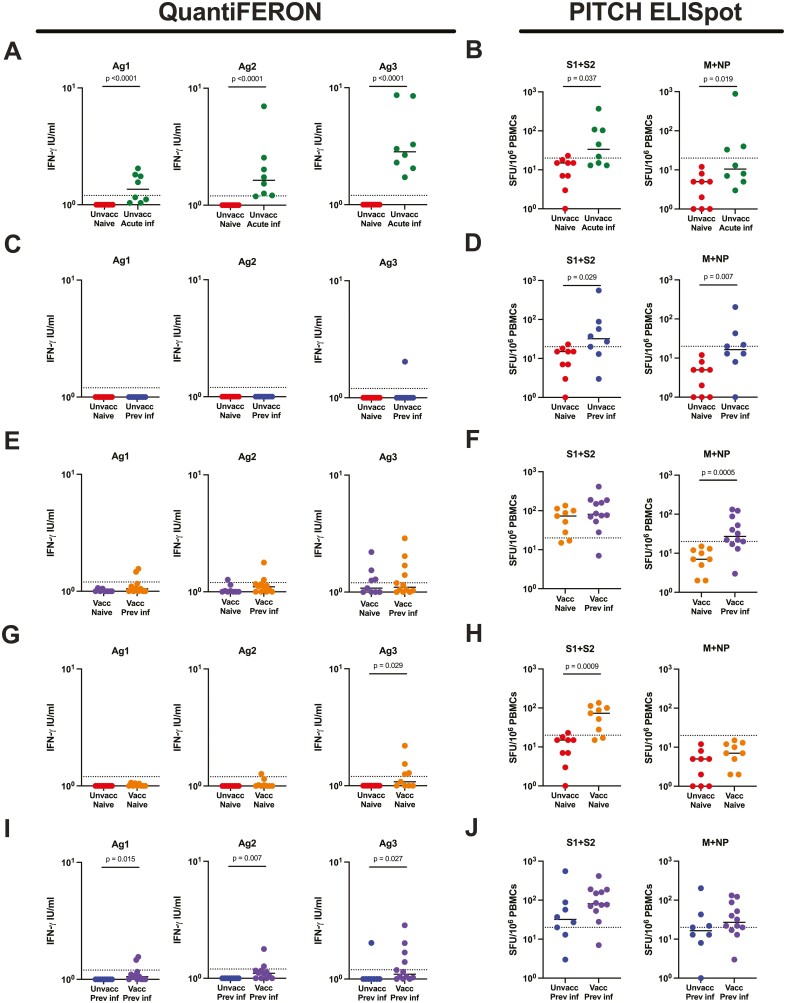
To examine the QuantiFERON SARS-CoV-2 assay in SARS-CoV-2-infected individuals, samples from the unvaccinated naïve group were compared with unvaccinated, acute infection samples (median of 16 days, range 12–21 days since positive SARS-CoV-2 PCR). The same unvaccinated naïve samples were also compared to unvaccinated, previous infection samples (median of 256, range 172–444 days since positive test). For all three QuantiFERON assay tubes, Ag1, Ag2, and Ag3, there was significantly greater IFN-γ detected for acute infection individuals compared to naïve controls (Figure 1A; P < 0.0001 for all). Samples were also compared using two PITCH ELISpot assays—one against the spike protein (S1 + S2) and one against structural proteins M protein and nucleocapsid protein (M + NP). A significant difference was also seen in the PITCH ELISpot comparison for S1 + S2 and M + NP between naïve and acute infection groups (Figure 1B; P = 0.037 and P = 0.019, respectively). For the naïve vs previous infection group comparison, there was no statistically significant difference in the amount of IFN-γ produced in any of the three QuantiFERON tubes (Figure 1C), although the PITCH ELISpot was able to detect differences in S1 + S2 (P = 0.029) and M + NP (P = 0.007) when comparing the two groups (Figure 1D). When looking at vaccinated individuals and aiming to differentiate SARS-CoV-2 infection naïve and previous infection (median of 222 days, range 175–433 days since positive test), there were no statistically significant differences between the groups using QuantiFERON Ag1, Ag2, or Ag3 (Figure 1E). The PITCH ELISpot found a difference between the vaccinated naïve and vaccinated previous infection groups with M + NP (P = 0.0005) but not for S1 + S2 (P = 0.254) (Figure 1F).
Figure 1.
Comparison of T-cell responses between indicated groups measured by QuantiFERON and PITCH ELISpot. (A) T-cell responses to SARS-CoV-2 in unvaccinated naïve and unvaccinated acute infection using QuantiFERON Ag1, Ag2, and Ag3, and (B) ELISpot S1 + S2 and M + NP. (C) T-cell responses to SARS-CoV-2 in unvaccinated naïve and unvaccinated previous infection using QuantiFERON Ag1, Ag2, and Ag3, and (D) ELISpot S1 + S2 and M + NP. (E) T-cell responses to SARS-CoV-2 in vaccinated naïve and vaccinated previous infection using QuantiFERON Ag1, Ag2, and Ag3, and (F) ELISpot S1 + S2 and M + NP. (G) T-cell responses to SARS-CoV-2 in unvaccinated naïve and vaccinated naive using QuantiFERON Ag1, Ag2, and Ag3, and (H) ELISpot S1 + S2 and M + NP. (I) T-cell responses to SARS-CoV-2 in unvaccinated previous infection and vaccinated previous infection using QuantiFERON Ag1, Ag2, and Ag3, and (J) ELISpot S1 + S2 and M + NP. QuantiFERON assay data were log10 transformed with zero values y = log(x + 1). naïve—unvaccinated naïve, n = 9; unvacc acute inf—unvaccinated acute infection, n = 8; unvacc prev inf—unvaccinated previous infection, n = 8; vacc naïve—vaccinated naïve, n = 10; vacc prev inf—vaccinated previous infection, n = 12. Unpaired comparisons between groups were performed using Mann–Whitney test, with statistical significance as P < 0.05. Horizontal-dotted lines represent the threshold of each assay based on negative assay controls (see Methods).
QuantiFERON SARS-CoV-2 in individuals vaccinated against SARS-CoV-2
To examine the QuantiFERON SARS-CoV-2 assay in vaccinated individuals, we compared samples from unvaccinated naïve versus vaccinated naïve individuals (median of 102, range 55–166 days since second vaccination). Here, there was no difference between the two groups for Ag1 (P = 0.206) or Ag2 (P = 0.082) but there was a statistically significant difference for Ag3 (P = 0.029) (Figure 1G). The PITCH ELISpot demonstrated differences between the groups for S1 + S2 (p = 0.0005) but not M + NP (P = 0.072) (Figure 1H).
We also compared SARS-CoV-2 previously infected individuals with and without vaccination, (median of 65, range 54–160 days since second vaccination). The QuantiFERON assay was able to detect statistically significant differences between the two groups for all three assay tubes; Ag1 (P = 0.015), Ag2 (P = 0.007), and Ag3 (P = 0.027) (Figure 1I)—largely due to a lack of responses in the previously infected unvaccinated cohort. The PITCH ELISpot did not present differences between the groups for either S1 + S2 (P = 0.115) or M + NP (P = 0.245) (Figure 1J).
Sensitivity of the QuantiFERON SARS-CoV-2 assay
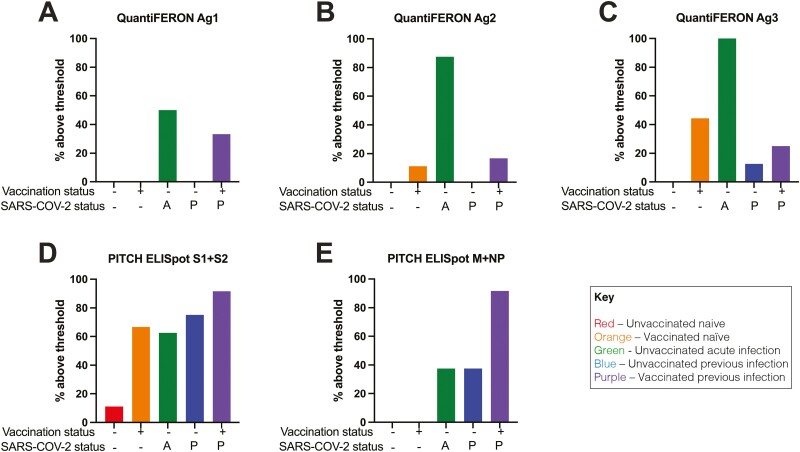
The QuantiFERON SARS-CoV-2 assay utilizes the QuantiFERON IGRA technology, known for its use in detecting tuberculosis with QuantiFERON TB Gold. This assay has a standardized threshold for designating samples as being ‘positive’. As such, we sought to present the current data as qualitative positive or negative results, as per the threshold utilized by the manufacturer [21]. Samples above threshold were used to determine the sensitivity of a given test for SARS-CoV-2 T-cell responses.
Using this threshold, for Ag1, none of the unvaccinated or vaccinated naïve samples were above threshold (Figure 2A), with 50% of unvaccinated acute infection, none of unvaccinated previous infection, and 33.3% of vaccinated previous infection above threshold. For Ag2, none of the unvaccinated naïve samples were above threshold, with 12.1% of vaccinated naïve, 87.5% of unvaccinated acute infection, none of unvaccinated previous infection and 16.7% of vaccinated previous infection above threshold (Figure 2B). For Ag3, none of the unvaccinated naïve samples were above threshold. 44.4% of vaccinated naïve samples were above threshold, 100% unvaccinated acute infection, 12.5% of unvaccinated previous infection and 25% of vaccinated previous infection were above threshold (Figure 2C). The S1 + S2 PITCH ELISpot showed greater sensitivity for SARS-CoV-2 T cell responses in general (Figure 2D). 11.11% of unvaccinated naïve samples were above threshold, with 66.6% of vaccinated naïve, 62.5% of unvaccinated acute infection, 75% of unvaccinated previous infection and 91.7% of vaccinated previous infection above threshold. For M + NP, there was less sensitivity compared to S1 + S2 with 0% of naive unvaccinated and naive vaccinated above threshold (Figure 2E), 37.5% of unvaccinated acute infection and unvaccinated previous infection, and 91.7% of vaccinated previous infection above threshold.
Figure 2.
Percentage of samples above threshold for indicated groups using QuantiFERON and PITCH ELISpot. The threshold to designate responses as positive for QuantiFERON was as per manufacturer’s recommendation and for ELISpot was values greater than the mean of the Nil controls + 2 standard deviations, with a minimum of 20 SFCs per million PBMCs for ELISpot. Percentage of samples above threshold for all five groups using (A) QuantiFERON Ag1, (B) QuantiFERON Ag2, (C) QuantiFERON Ag3, (D) PITCH ELISpot S1 + S2, (E) PITCH ELISpot M + NP. Unvaccinated naïve, n = 9; unvaccinated acute infection, n = 8; unvaccinated previous infection, n = 8; vaccinated naïve, n = 10; vaccinated previous infection, n = 12. A—acute infection; P—previous infection.
Sensitivity and specificity for SARS-CoV-2-specific T cells as well as positive and negative predictive values and negative predictive values of all groups for each of the five tests are detailed in Table 2. The clinical positive (CP) phenotypes were determined on the basis of historic infection and/or vaccination, with the MSD antibody assay removing those reported naïve which had positive antibody responses. For unvaccinated naïve samples, all three QuantiFERON SARS-CoV-2 assay tubes had 100% specificity and 100% negative predictive value (NPV) for SARS-CoV-2 T cells, as did the PITCH ELISpot M + NP but PITCH ELISpot S1 + S2 had only 88.9% specificity. For vaccinated naïve samples, PITCH ELISpot S1 + S2 had greater sensitivity (55.5%) than any of the QuantiFERON tubes Ag1, Ag2 or Ag3 (0%, 12.1% and 44.4% respectively). For this group, all tests had 100% positive predictive value for SARS-CoV-2 T cells. For the unvaccinated acute infection group, all five tests exhibited 100% PPV, and as stated before, the QuantiFERON SARS-CoV-2 assays exhibited 50%, 87.5% and 100% sensitivity for Ag1, Ag2 and Ag3 respectively with PITCH ELISpot S1 + S2 having 62.5% sensitivity and M + NP with 37.5%. For the unvaccinated previous infection group, as before the PITCH ELISpot had superior sensitivity with S1 + S2 at 75% and M + NP at 37.5% whilst the QuantiFERON SARS-CoV-2 achieved 0%, 0% and 12.5% for Ag1, Ag2, and Ag3, respectively. Finally, for the vaccinated previously infected group, there was greater sensitivity using the PITCH ELISpot (91.7% for both S1 + S2 and M + NP) than QuantiFERON SARS-CoV-2 which only achieved 33.33% sensitivity with Ag1, 16.7% with Ag2 and only 25% for Ag3. All tests for this group had 100% PPV.
Table 2.
Sensitivity, specificity, positive predictive values, and negative predictive vales for QuantiFERON and ELISpot assays. TP, true positive; FP, false positive; TN, true negative; FN, false negative
| QuantiFERON Ag1 | QuantiFERON Ag2 | QuantiFERON Ag3 | PITCH ELISpot S1 + S2 | PITCH ELISpot M + NP | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SARS-COV-2 unvaccinated naive | CP+ | CP− | CP+ | CP− | CP+ | CP− | CP+ | CP− | CP+ | CP− | ||||||||||
| Test+ | 0 | 0 | NA | Test+ | 0 | 0 | NA | Test+ | 0 | 0 | NA | Test+ | 0 | 1 | 0 | Test+ | 0 | 0 | NA | |
| Test− | 0 | 9 | 100 | Test− | 0 | 9 | 100 | Test− | 0 | 9 | 100 | Test− | 0 | 8 | 100 | Test− | 0 | 9 | 100 | |
| NA | 100 | NA | 100 | NA | 100 | NA | 88.8 | NA | 100 | |||||||||||
| SARS-COV-2 vaccinated naïve |
CP+ | CP− | CP+ | CP− | CP+ | CP− | CP+ | CP− | CP+ | CP− | ||||||||||
| Test+ | 0 | 0 | 100 | Test+ | 1 | 0 | 100 | Test+ | 4 | 0 | 100 | Test+ | 5 | 0 | 100 | Test+ | 0 | 0 | NA | |
| Test− | 9 | 0 | 0 | Test− | 8 | 0 | 0 | Test− | 5 | 0 | 0 | Test− | 2 | 0 | 0 | Test− | 0 | 9 | 100 | |
| 0 | NA | 12.1 | NA | 44.4 | NA | 55.5 | NA | NA | 100 | |||||||||||
| SARS-COV-2 unvaccinated acute |
CP+ | CP− | CP+ | CP− | CP+ | CP− | CP+ | CP− | CP+ | CP− | ||||||||||
| Test+ | 4 | 0 | 100 | Test+ | 6 | 0 | 100 | Test+ | 8 | 0 | 100 | Test+ | 5 | 0 | 100 | Test+ | 3 | 0 | 100 | |
| Test− | 4 | 0 | 0 | Test− | 2 | 0 | NA | Test− | 0 | 0 | NA | Test− | 3 | 0 | 0 | Test− | 5 | 0 | 0 | |
| 50 | NA | 75 | NA | 100 | NA | 62.5 | NA | 37.5 | NA | |||||||||||
| SARS-COV-2 unvaccinated previously infected |
CP+ | CP− | CP+ | CP− | CP+ | CP− | CP+ | CP− | CP+ | CP− | ||||||||||
| Test+ | 0 | 0 | NA | Test+ | 0 | 0 | NA | Test+ | 1 | 0 | 100 | Test+ | 6 | 0 | 100 | Test+ | 3 | 0 | 100 | |
| Test− | 8 | 0 | 0 | Test− | 8 | 0 | 0 | Test− | 7 | 0 | 0 | Test− | 2 | 0 | 0 | Test− | 5 | 0 | 0 | |
| 0 | NA | 0 | NA | 12.5 | NA | 75 | NA | 37.5 | NA | |||||||||||
| SARS-COV-2 vaccinated previously infected |
CP+ | CP− | CP+ | CP− | CP+ | CP− | CP+ | CP− | CP+ | CP− | ||||||||||
| Test+ | 4 | 0 | 100 | Test+ | 2 | 0 | 100 | Test+ | 3 | 0 | 100 | Test+ | 11 | 100 | Test+ | 11 | 0 | 100 | ||
| Test− | 8 | 0 | 0 | Test− | 10 | 0 | 0 | Test− | 9 | 0 | 0 | Test− | 1 | 0 | 0 | Test− | 1 | 0 | 0 | |
| 33.3 | NA | 16.7 | NA | 25 | NA | 91.7 | NA | 91.7 | NA | |||||||||||
| Key | ||||||||||||||||||||
| CP+ | CP− | |||||||||||||||||||
| Test+ | TP | FP | PPV% | |||||||||||||||||
| Test− | FN | TN | NPV% | |||||||||||||||||
| Sn% | Sp% | |||||||||||||||||||
CP, clinical phenotype; Sn, sensitivity, [TP/(TP + FN)] × 100; Sp, specificity, [TN/(TN + FP)] × 100; PPV, positive predictive value, [TP/(TP + FP)] × 100; NPV, negative predictive value, [FN/(FN + TN)] × 100.
Correlation of QuantiFERON SARS-CoV-2 assay tubes
Correlation analysis was performed between the three assay tubes for the QuantiFERON SARS-CoV-2 (Supplementary Figure 2). For all three comparisons (Ag1 v Ag2, Ag1 v Ag3 and Ag2 v Ag3) there was significant correlation (R2 0.7132 – 0.889, P < 0.0001).
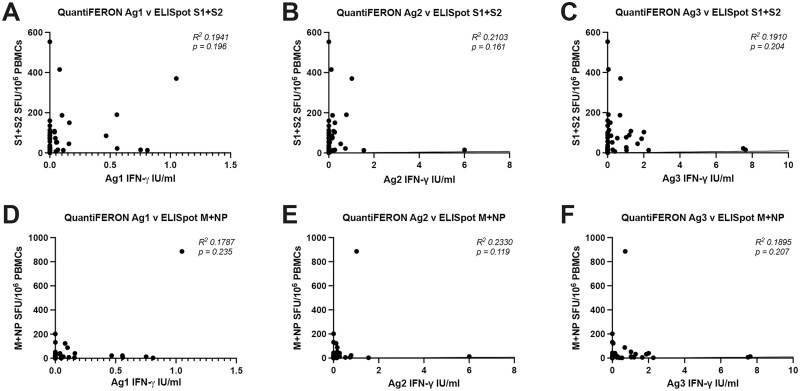
Correlation of the QuantiFERON SARS-CoV-2 assay with PITCH ELISpot and MSD antibody platform
Correlation analysis was performed between the three QuantiFERON SARS-CoV-2 assay tubes and the PITCH ELISpot assay. For all three assay tubes there was no significant correlation with PITCH ELISpot S1 + S2 (Figure 3A–C) or with PITCH M + NP (Figure 3D–F).
Figure 3.
Correlation between T-cell responses measured by QuantiFERON and PITCH ELISpot. (A–C) Correlation between QuantiFERON Ag1, Ag2, and Ag3 with ELISpot S1 + S2. (D–F) Correlation between QuantiFERON Ag1, Ag2 and Ag3 with ELISpot M + NP. N = 47 for each analysis. Correlation analysis was carried out with Spearman’s r correlation and 2-tailed P values reported, with α = 0.05.
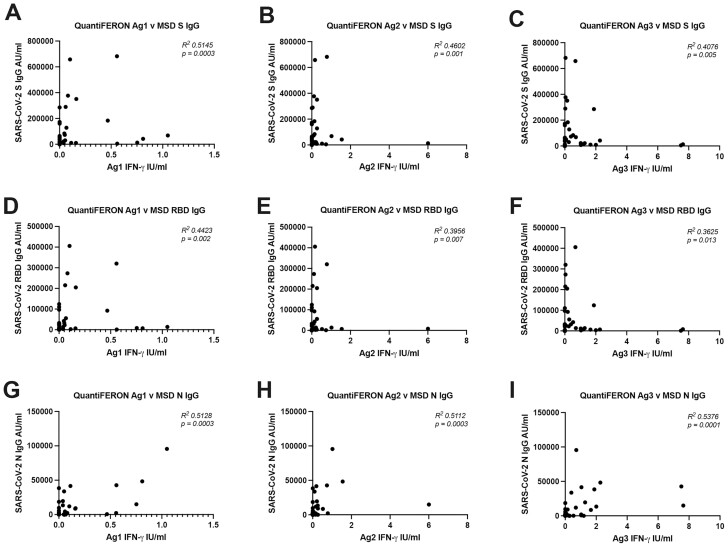
The QuantiFERON SARS-CoV-2 Ag1, Ag2 and Ag3 showed statistically significant correlation with S IgG (Figure 4A–C) RBD IgG (Figure 4D–F) and N IgG (Figure 4G–I). The data from the PITCH ELISpot was correlated to that of the MSD antibody data (Supplementary Figure 3). There were low R squared values for all correlations and statistical significance was achieved for all but one comparisons, (ELISpot S1+S2 vs MSD N IgG (p = 0.062)).
Figure 4.
Correlation between T cell responses measured by QuantiFERON and antibodies measured by MSD binding assay. (A–C) Correlation between QuantiFERON Ag1, Ag2, and Ag3 with MSD S IgG. (D–F) Correlation between QuantiFERON Ag1, Ag2, and Ag3 with MSD RBD IgG. (G–I) Correlation between QuantiFERON Ag1, Ag2, and Ag3 with MSD N IgG. N = 47 for each analysis. Correlation analysis was carried out with Spearman’s r correlation and 2-tailed P-values reported, with α = 0.05.
Discussion
T cells are increasingly recognised for their role in SARS-CoV-2 infection and vaccination [32–35]. However, cell-based assays which evaluate T cells are typically labour- and expertise-intensive, require specialist equipment, and need specialist processing of fresh blood within 3–4 hours of blood draw. Therefore, validating simple, commercially available kits could expand the repertoire of tools for evaluating T cells in the context of SARS-CoV-2, particularly in research laboratories which do not have means to overcome the above barriers. The present study sought to do this with the commercially available QuantiFERON SARS-CoV-2 assay, which is based on the same technology of the QuantiFERON TB Gold used worldwide (reviewed in [36]). This assay has a straight-forward work-flow, basic equipment requirements compared to other cell-based assays and tolerance of delays in processing. Moreover, the read-out can be seen at times with the naked eye, which may merit further investigation (Supplementary Figure 4).
To our knowledge this is the first QuantiFERON study to analyse a sample set include five different spike exposures. The data presented in this study demonstrates a robust read-out for all three QuantiFERON assay tubes (Ag1, Ag2, Ag3) for acute infection samples In keeping with other studies [21, 27], with superior sensitivity for SARS-CoV-2 T cell responses than both the S1 + S2 and M + NP ELISpot for these samples. Furthermore, none of the naïve samples generated a positive result, making the QuantiFERON SARS-CoV-2 highly specific. These results support a utility for the QuantiFERON SARS-CoV-2 in evaluating T cell responses during or soon after acute infection. However, our study has failed to show significant differences following more distant infection or past vaccination compared to other studies [23–25, 27], with many of the samples exhibiting values below the level of detection. This study also exhibited lower sensitivity values compared to other studies [23, 24]. It has been demonstrated with longitudinal evaluation that signal from the assays decreases over time from antigen exposure [21]. As our samples were gathered at a more distant time point from exposure (vaccination and distant infection) compared to other studies, this likely explains the lower values generated for these groups. Effector T-cell responses to SARS-CoV-2 infection decrease over time [8, 13] which may explain why T cell responses were not detected in more distant infection, but are typically still detectable by research assays more than 6 months later [20, 37, 38]. Further work to increase the sensitivity of the QuantiFERON SARS-CoV-2 assay to detect SARS-CoV-2 T-cell responses in this group would be useful for evaluating T cell responses in distant antigen exposure.
The highly sensitive and specific results in the acute infection samples show potential for the assay to be used as a diagnostic test, as is the case for the QuantiFERON TB IGRA in settings where PCR testing may not be feasible. T cells can be detected as soon as 3–5 post symptom onset, with a similar kinetic profile to antibody detection [39, 40], which supports the use of T-cell-based diagnostic SARS-CoV-2 tests. However, the utility of such a diagnostic test would be at the time of symptom onset, which was not possible to assess in the current study due to national isolation guidelines at the time of sampling. Further studies closer to symptom onset are required to investigate further.
The low responses to Ag1, Ag2, or Ag3 seen in naïve participants post vaccination limit the utility of the QuantiFERON assay for scaled up study of response to vaccination. This is disappointing when there is a huge need for large scale prospective longitudinal studies in a range of populations and settings, to establish immune correlates of protection and differences in vaccine response between vulnerable patient groups. A larger dynamic range of IFN-γ responses post vaccination or infection has been observed in another whole blood ELISA-based assay [9, 10], although some of these samplings were taken closer to the time of vaccination which may explain their greater sensitivity for SARS-CoV-2 T-cell responses than in the present study. Further work to raise the sensitivity of the QuantiFERON assay, such as increasing the detection of IFN-γ by ELISA, would be hugely valuable and would have high potential for transfer to other emerging outbreak pathogens in regions of the world with limited laboratory capacity. Nevertheless, the presence or absence of a T-cell response detectable by the QuantiFERON assay could prove to be a useful parameter to include in longitudinal studies of vaccine immunogenicity and correlates of protection.
With the exception of the acutely infected group, the PITCH ELISpot S1 + S2 exhibited superior sensitivity for SARS-CoV-2 T-cell responses compared with the QuantiFERON SARS-CoV-2 assay in keeping with other studies which have demonstrated the value of ELISpot compared to other T-cell evaluation tools [41, 42]. Likely factors contributing to the relatively inferior performance of the QuantiFERON platform could include the T-cell concentration in whole blood samples, processing timelines and concentrations/selection of epitopes for T-cell stimulation. However, much of the information required to draw strong conclusions is proprietary information, thus limiting our understanding for the performance differences between the platforms.
According to the manufacturer, the epitopes lining the Ag1 assay tube activate CD4+ T cells specific to RBD, Ag2 activates CD4+ and CD8+ T cells specific to S1 and S2, and Ag3 activates CD4+ and CD8+ T cells against numerous SARS-CoV-2 peptides including spike. In the five sets of two-group comparisons illustrated in Figure 1, Ag1 was able to discern statistically significant differences in two of the five group comparisons, Ag2 in three of five and Ag3 in three of five. In terms of sensitivity, Ag3 had the highest sensitivity for SARS-CoV-2-specific T cells in four of the five individual groups. Overall, there was correlation between the QuantiFERON SARS-CoV-2 assay tubes. Taken together, the present data suggests the Ag3 tube may be the most useful of the three for evaluating SARS-CoV-2-specific T cells in infection and vaccination. Unfortunately, none of the combination of antigens provided by the manufacturer enable identification of previous infection in vaccinated individuals, because all three antigen sets contain spike peptides.
There was little evidence to support a strong correlation between the QuantiFERON SARS-CoV-2 assay tubes and the ELISpot assay. Interestingly, there was statistically significant correlations between QuantiFERON SARS-CoV-2 and the MSD antibody data; however, R2 values were relatively low, therefore strong conclusions about a true relationship between the sample sets cannot be drawn but may merit further investigation with a larger sample set. Unfortunately, the zero values of the QuantiFERON assay would greatly impede the ability of comparative analysis to yield meaningful data.
The primary aim of this study was to determine the utility of the commercially available QuantiFERON SARS-CoV-2 assay in evaluating T cells following SARS-CoV-2 infection and vaccination. The data demonstrates this assay, particularly the Ag3 assay tube, to be highly sensitive and specific in detecting SARS-CoV-2 T cells in acute but not past infection, and capable of discerning differences in T-cell responses in unvaccinated and vaccinated individuals albeit with reduced sensitivity compared to the PITCH ELISpot. The assay was also relatively easy to perform, using equipment commonly available in a hospital laboratory. Therefore, the assay may be beneficial in laboratories which do not have access to established T-cell assays, and as a dichotomous measure for monitoring of vaccine immunogenicity. Further research is required to define a suitable timeline following infection or vaccination during which the QuantiFERON SARS-CoV-2 assay may be applied to detect SARS-CoV-2-specific T cells as well as further development of the platform to increase the sensitivity for SARS-CoV-2 T-cell responses in more distant infection and vaccination.
Limitations
This study has a number of limitations. Firstly, genotype data for past infections were unavailable, although we know that the previously infected participants were chiefly infected by early pandemic strain virus in wave 1, and the acute infection group were infected when the delta variant was predominant [31]. Further testing in populations with documented different variants is required, although T-cell responses have been shown to be only marginally impacted by alpha, beta, gamma, and delta variants [5, 6] and 75-85% preserved in Omicron [43–49]. This study involved only a single time point, without samples between the acute and previous infection timepoints. Furthermore, for naïve samples, we cannot rule out the possibility that asymptomatic infection may have occurred previously as antibodies reduce significantly over time [8]. This study enrolled young (ages 18–56) and healthy individuals, whilst T-cell response to vaccination is known to be affected by aging [50] and immunosuppression [51, 52]. This study was biased toward female participants, although larger studies have not found sex to be a determinant of SARS-CoV-2-specifiic T-cell responses [5]. There was also limited ethnic diversity in this cohort. Finally, the number of participants recruited may have rendered some of the statistical analysis sub-optimal, particularly in regard to correlation analysis with a significant proportion of zero values in the QuantiFERON assays. A formal power calculation was not performed for this study but we were limited by the availability of clinical samples. The limitations suggest further larger studies with genetically sequenced strains with a population to include a range of SARS-CoV-2 variants, ages, co-morbidities, sexes and ethnicities are warranted.
Supplementary Material
Acknowledgements
We are grateful to all our healthcare worker colleagues who participated in the study, and to Lisa Fielding for administrative support.
Abbreviations
- AIM
activation-induced cell marker
- ELISA
enzyme-linked immunoassay
- ELISpot
interferon-gamma enzyme-linked absorbent spot
- FN
false negative
- FP
false positive
- ICS
intracellular staining
- IFN-γ
interferon-gamma
- IGRA
interferon-gamma release assay
- M
membrane
- MSD
mesoscale discovery
- NP
nucleocapsid
- OPTIC
Oxford protective T-cell immunity against COVID-19
- PBMC
peripheral blood mononuclear cells
- PITCH
protective immunity from T cells to Covid-19 in health workers
- S
spike
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
- SOP
standard operating procedure
- TB
tuberculosis
- TN
true negative
- TP
true positive
Contributor Information
Síle A Johnson, Peter Medawar Building for Pathogen Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; University of Oxford Medical School, University of Oxford, Oxford, UK; University Hospitals of Derby and Burton NHS Foundation Trust, Derby, UK.
Eloise Phillips, Peter Medawar Building for Pathogen Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK.
Sandra Adele, Peter Medawar Building for Pathogen Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; Oxford Centre For Global Health Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; Mahidol-Oxford Tropical Medicine Research Unit, Mahidol University, Bangkok, Thailand.
Stephanie Longet, Wellcome Centre for Human Genetics, Nuffield Department of Medicine, University of Oxford, Oxford, UK; Pandemic Sciences Institute, Nuffield Department of Medicine, University of Oxford, Oxford, UK.
Tom Malone, Peter Medawar Building for Pathogen Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK.
Chris Mason, University of Oxford Medical School, University of Oxford, Oxford, UK.
Lizzie Stafford, Oxford University Hospitals NHS Foundation Trust, Oxford, UK; Department of Experimental Medicine, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK.
Anni Jamsen, Oxford University Hospitals NHS Foundation Trust, Oxford, UK; Department of Experimental Medicine, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK.
Siobhan Gardiner, Oxford University Hospitals NHS Foundation Trust, Oxford, UK; Department of Experimental Medicine, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK.
Alexandra Deeks, Peter Medawar Building for Pathogen Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; Department of Experimental Medicine, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK.
Janice Neo, University Hospitals of Derby and Burton NHS Foundation Trust, Derby, UK.
Emily J Blurton, University Hospitals of Derby and Burton NHS Foundation Trust, Derby, UK.
Jemima White, University of Oxford Medical School, University of Oxford, Oxford, UK.
Muhammed Ali, Peter Medawar Building for Pathogen Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; Oxford Centre For Global Health Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; Mahidol-Oxford Tropical Medicine Research Unit, Mahidol University, Bangkok, Thailand.
Barbara Kronsteiner, Peter Medawar Building for Pathogen Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; Oxford Centre For Global Health Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK.
Joseph D Wilson, Peter Medawar Building for Pathogen Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; King’s College Hospital NHS Foundation Trust, London, UK.
Dónal T Skelly, Peter Medawar Building for Pathogen Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; Oxford University Hospitals NHS Foundation Trust, Oxford, UK; Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, UK.
Katie Jeffery, Oxford University Hospitals NHS Foundation Trust, Oxford, UK; Radcliffe Department of Medicine, University of Oxford, Oxford, UK.
Christopher P Conlon, Oxford Centre For Global Health Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; Oxford University Hospitals NHS Foundation Trust, Oxford, UK.
Philip Goulder, Peter Medawar Building for Pathogen Research, Department of Paediatrics, University of Oxford, Oxford, UK.
PITCH Consortium, Peter Medawar Building for Pathogen Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK.
Miles Carroll, Wellcome Centre for Human Genetics, Nuffield Department of Medicine, University of Oxford, Oxford, UK; Pandemic Sciences Institute, Nuffield Department of Medicine, University of Oxford, Oxford, UK.
Eleanor Barnes, Peter Medawar Building for Pathogen Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; Oxford University Hospitals NHS Foundation Trust, Oxford, UK; NIHR Oxford Biomedical Research Centre, University of Oxford, Oxford, UK; Translational Gastroenterology Unit, University of Oxford, Oxford, UK.
Paul Klenerman, Peter Medawar Building for Pathogen Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; Oxford University Hospitals NHS Foundation Trust, Oxford, UK; NIHR Oxford Biomedical Research Centre, University of Oxford, Oxford, UK; Translational Gastroenterology Unit, University of Oxford, Oxford, UK.
Susanna J Dunachie, Peter Medawar Building for Pathogen Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; Oxford Centre For Global Health Research, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK; Mahidol-Oxford Tropical Medicine Research Unit, Mahidol University, Bangkok, Thailand; Oxford University Hospitals NHS Foundation Trust, Oxford, UK.
Ethics approval
Participants were enrolled in the OPTIC study (GI Biobank Study 16/YH/0247, approved by the research ethics committee (REC) at Yorkshire & The Humber—Sheffield Research Ethics Committee on 29 July 2016, and amended for the OPTIC study on 8 June 2020 or the Family Study R71346/RE001, approved by Oxford University’s Medical Sciences Inter-Divisional REC (MS-IDREC-R71346/RE00).
Conflict of interests
S.J.D. declares fees as a Scientific Advisor to the Scottish Parliament on COVID-19. No other competing interests declared. QuantiFERON assays were purchased as part of a commercial contract and the company played no role in this report.
Funding
This work was funded by the UK Department of Health and Social Care as part of the PITCH (Protective Immunity from T cells to Covid-19 in Health workers) Consortium, with contributions from the National Core Study: Immunity (NCSi4P programme) ‘Optimal cellular assays for SARS-CoV-2 T cell, B cell and innate immunity’, UKRI through the UK Coronavirus Immunology Consortium (UK-CIC), the Huo Family Foundation, The National Institute for Health Research (UKRIDHSC COVID-19 Rapid Response Rolling Call, Grant Reference Number COV19-RECPLAS), and U.S. Food and Drug Administration Medical Countermeasures Initiative contract 75F40120C00085. E.B. and P.K. are NIHR Senior Investigators and P.K. is funded by WT109965MA. S.J.D. is funded by an NIHR Global Research Professorship (NIHR300791). D.S. is supported by the NIHR Academic Clinical Lecturer programme in Oxford. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, the Department of Health and Social Care or UKHSA or the US Food and Drug Administration.
Data availability
The data underlying this article are available in the article and Supplementary material.
Author contributions
S.A.J., S.J.D., E.B., and P.K. conceptualized the study. S.A.J., S.J.D., E.B., M.C., K.J., C.P.C., and P.K. designed and oversaw the clinical study. S.A.J., C.M., L.S., A.J., J.W., and S.J.D. recruited participants and collected samples. S.A.J., E.P., S.A., S.L., T.M., M.A., D.T.S. implemented laboratory testing. S.A.J., J.N., and J.D.W. undertook data analysis. A.D. undertook project administration. S.J.D., P.K., and E.B. acquired the funding. S.A.J., J.N., E.J.B., P.K., and S.D. prepared the manuscript, which was reviewed by all contributing authors.
Patient consent statement
All participants in the study gave written, informed consent.
Permission to reproduce
Not applicable.
Clinical trial registration
Not applicable.
References
- 1. WHO Coronavirus (COVID-19) Dashboard [Internet]. https://covid19.who.int (19 April 2022, date last accessed).
- 2. Amirthalingam G, Bernal JL, Andrews NJ, Whitaker H, Gower C, Stowe J, et al. Serological responses and vaccine effectiveness for extended COVID-19 vaccine schedules in England. Nat Commun 2021, 12, 7217. doi: 10.1038/s41467-021-27410-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dan JM, Mateus J, Kato Y, Hastie KM, Yu ED, Faliti CE, et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science 2021, 371(6529), eabf4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ogbe A, Kronsteiner B, Skelly DT, Pace M, Brown A, Adland E, et al.; Oxford Immunology Network Covid-19 Response T Cell Consortium. T cell assays differentiate clinical and subclinical SARS-CoV-2 infections from cross-reactive antiviral responses. Nat Commun 2021, 12, 2055. doi: 10.1038/s41467-021-21856-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Payne RP, Longet S, Austin JA, Skelly DT, Dejnirattisai W, Adele S, et al.; PITCH Consortium. Immunogenicity of standard and extended dosing intervals of BNT162b2 mRNA vaccine. Cell 2021, 184, 5699–714.e11. doi: 10.1016/j.cell.2021.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Skelly DT, Harding AC, Gilbert-Jaramillo J, Knight ML, Longet S, Brown A, et al.; Medawar Laboratory Team. Two doses of SARS-CoV-2 vaccination induce robust immune responses to emerging SARS-CoV-2 variants of concern. Nat Commun 2021, 12, 5061. doi: 10.1038/s41467-021-25167-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tarke A, Coelho CH, Zhang Z, Dan JM, Yu ED, Methot N, et al. SARS-CoV-2 vaccination induces immunological T cell memory able to cross-recognize variants from Alpha to Omicron. Cell 2022, 185, 847–59.e11. doi: 10.1016/j.cell.2022.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tomic A, Skelly DT, Ogbe A, O’Connor D, Pace M, Adland E, et al.; OPTIC Clinical Group. Divergent trajectories of antiviral memory after SARS-CoV-2 infection. Nat Commun 2022, 13, 1251. doi: 10.1038/s41467-022-28898-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tan AT, Lim JM, Le Bert N, Kunasegaran K, Chia A, Qui MD, et al. Rapid measurement of SARS-CoV-2 spike T cells in whole blood from vaccinated and naturally infected individuals. J Clin Invest 2021, 131(17), e152379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Le Bert N, Clapham HE, Tan AT, Chia WN, Tham CYL, Lim JM, et al. Highly functional virus-specific cellular immune response in asymptomatic SARS-CoV-2 infection. J Exp Med 2021, 218(5), e20202617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Le Bert N, Tan AT, Kunasegaran K, Tham CYL, Hafezi M, Chia A, et al. SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls. Nature 2020, 584, 457–62. doi: 10.1038/s41586-020-2550-z. [DOI] [PubMed] [Google Scholar]
- 12. Bilich T, Med ST, Bilich T, Nelde A, Heitmann JS, Maringer Y, et al. Coronavirus T cell and antibody kinetics delineate SARS-CoV-2 peptides mediating long-term immune responses in COVID-19 convalescent individuals. Sci Trans Med 2021, 7517, 17–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cohen KW, Linderman SL, Moodie Z, Czartoski J, Lai L, Mantus G, et al. Longitudinal analysis shows durable and broad immune memory after SARS-CoV-2 infection with persisting antibody responses and memory B and T cells. Cell Rep Med 2021, 2, 100354. doi: 10.1016/j.xcrm.2021.100354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Grifoni A, Weiskopf D, Ramirez SI, Mateus J, Dan JM, Moderbacher CR, et al. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell 2020, 181, 1489–501.e15. doi: 10.1016/j.cell.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rodda LB, Netland J, Shehata L, Pruner KB, Morawski PA, Thouvenel CD, et al. Functional SARS-CoV-2-specific immune memory persists after Mild COVID-19. Cell 2021, 184, 169–83.e17. doi: 10.1016/j.cell.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zuo J, Dowell AC, Pearce H, Verma K, Long HM, Begum J, et al. Robust SARS-CoV-2-specific T cell immunity is maintained at 6 months following primary infection. Nat Immunol 2021, 22, 620–6. doi: 10.1038/s41590-021-00902-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Angyal A, Longet S, Moore SC, Payne RP, Harding A, Tipton T, et al.; PITCH Consortium. T-cell and antibody responses to first BNT162b2 vaccine dose in previously infected and SARS-CoV-2-naive UK health-care workers: a multicentre prospective cohort study. Lancet Microbe 2022, 3, e21–31. doi: 10.1016/S2666-5247(21)00275-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ewer KJ, Barrett JR, Belij-rammerstorfer S, Sharpe H, Makinson R, Morter R, et al.; Oxford COVID Vaccine Trial Group. T cell and antibody responses induced by a single dose of ChAdOx1 nCoV-19 (AZD1222) vaccine in a phase 1/2 clinical trial. Nat Med 2021, 27, 270–8. doi: 10.1038/s41591-020-01194-5. [DOI] [PubMed] [Google Scholar]
- 19. Folegatti PM, Ewer KJ, Aley PK, Angus B, Becker S, Belij-Rammerstorfer S, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/ 2, single-blind, randomised controlled trial. Lancet 2020, 396, 467–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mateus J, Dan JM, Zhang Z, Moderbacher CR, Lammers M, Goodwin B, et al. Low-dose mRNA-1273 COVID-19 vaccine generates durable memory enhanced by cross-reactive T cells. Science 2021, 374, 1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jaganathan S, Stieber F, Rao SN, Manissero D, Boyle J.. Preliminary evaluation of QuantiFERON SARS-CoV-2 and QIAreach anti-SARS-CoV-2 total test in recently vaccinated individuals. Infect Dis Ther 2021, 10, 2765–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bonelli MM, Mrak D, Perkmann T, Haslacher H, Aletaha D.. SARS-CoV-2 vaccination in rituximab-treated patients: evidence for impaired humoral but inducible cellular immune response. Ann Rheum Dis 2021, 80, 1355–6. doi: 10.1136/annrheumdis-2021-220408. [DOI] [PubMed] [Google Scholar]
- 23. Krüttgen A, Klingel H, Haase G, Haefner H, Imöhl M, Kleines M.. Evaluation of the QuantiFERON SARS-CoV-2 interferon-ɣ release assay in mRNA-1273 vaccinated health care workers. J Virol Methods 2021, 298, 114295. doi: 10.1016/j.jviromet.2021.114295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Martínez-Gallo M, Esperalba J, Pujol-Borrell R, Sandá V, Arrese-Muñoz I, Fernández-Naval C, et al. Commercialized kits to assess T-cell responses against SARS-CoV-2 S peptides. A pilot study in health care workers. Med Clin 2021, doi:S0025–7753(21)00529-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tychala A, Meletis G, Katsimpourlia E, Gkeka I, Dimitriadou R, Sidiropoulou E, et al. Evaluation of the QuantiFERON SARS-CoV-2 assay to assess cellular immunogenicity of the BNT162b2 mRNA COVID-19 vaccine in individuals with low and high humoral response. Hum Vaccin Immunother 2021, 17(12), 1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Van Praet JT, Vandecasteele S, De Roo A, De Vriese AS, Reynders M.. Humoral and cellular immunogenicity of the BNT162b2 messenger RNA Coronavirus disease 2019 vaccine in nursing home residents. Clin Infect Dis 2021, 73, 2145–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Aiello A, Coppola A, Vanini V, Petrone L, Cuzzi G, Salmi A, et al. Accuracy of QuantiFERON SARS-CoV-2 research use only assay and characterization of the CD4+ and CD8+ T cell-SARS-CoV-2 response: comparison with a homemade interferon-γ release assay. Int J Infect Dis 2022, 122, 841–9. doi: 10.1016/j.ijid.2022.07.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tormo N, Giménez E, Martínez-Navarro M, Albert E, Navalpotro D, Torres I, et al. Performance comparison of a flow cytometry immunoassay for intracellular cytokine staining and the QuantiFERON® SARS-CoV-2 test for detection and quantification of SARS-CoV-2-Spike-reactive-IFN-γ -producing T cells after COVID-19 vaccination. Eur J Clin Microbiol Infect Dis 2022, 41, 657–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Barreiro P, Sanz JC, San Román J, Pérez-Abeledo M, Carretero M, Megías G, et al. A pilot study for the evaluation of an Interferon Gamma Release Assay (IGRA) to measure T-cell immune responses after SARS-CoV-2iInfection or vaccination in a unique cloistered cohort. J Clin Microbiol 2022, 60, e0219921. doi: 10.1128/jcm.02199-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Phillips E, Adele S, Malone T, Deeks A, Stafford L, Dobson SL, et al. Comparison of two T cell assays to evaluate T cell responses to SARS-CoV-2 following vaccination in naïve and convalescent healthcare workers. medRxiv 2022; doi: 10.1101/2022.02.05.22270447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Variants: distribution of case data, 9th July 2021 [Internet]. https://www.gov.uk/government/publications/covid-19-variants-genomically-confirmed-case-numbers/variants-distribution-of-case-data-9-july-2021 (19 April 2022, date last accessed).
- 32. McMahan K, Yu J, Mercado NB, Loos C, Tostanoski LH, Chandrashekar A, et al. Correlates of protection against SARS-CoV-2 in rhesus macaques. Nature 2021, 590, 630–4. doi: 10.1038/s41586-020-03041-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Molodtsov IA, Kegeles E, Mitin AN, Mityaeva O, Musatova OE, Panova AE, et al. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)–Specific T Cells and Antibodies in Coronavirus Disease 2019 (COVID-19) protection: a prospective study. Clin Infect Dis 2022, 12, ciac278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kundu R, Narean JS, Wang L, Fenn J, Pillay T, Fernandez ND, et al. Cross-reactive memory T cells associate with protection against SARS-CoV-2 infection in COVID-19 contacts. Nat Commun 2022, 13, 80. doi: 10.1038/s41467-021-27674-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Swadling L, Diniz MO, Schmidt NM, Amin OE, Chandran A, Shaw E, et al.; COVIDsortium Investigators. Pre-existing polymerase-specific T cells expand in abortive seronegative SARS-CoV-2. Nature 2022, 601, 110–7. doi: 10.1038/s41586-021-04186-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Whitworth HS, Scott M, Connell DW, Dongés B, Lalvani A.. IGRAs--the gateway to T cell based TB diagnosis. Methods 2013, 61, 52–62. doi: 10.1016/j.ymeth.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 37. Zhang Z, Mateus J, Coelho CH, Dan JM, Moderbacher CR, Gálvez RI, et al. Humoral and cellular immune memory to four COVID-19 vaccines. Cell 2022, 185, 2434–51.e17. doi: 10.1016/j.cell.2022.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Moore SC, Kronsteiner B, Longet S, Adele S, Deeks AS, Liu C, et al. Evolution of long-term hybrid immunity in healthcare workers after different COVID-19 vaccination regimens: a longitudinal observational cohort study. medRxiv 2022; doi: 10.1101/2022.06.06.22275865. [DOI] [Google Scholar]
- 39. Rydyznski Moderbacher C, Ramirez SI, Dan JM, Grifoni A, Hastie KM, Weiskopf D, et al. Antigen-specific adaptive immunity to SARS-CoV-2 in acute COVID-19 and associations with age and disease severity. Cell 2020, 183, 996–1012.e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tan AT, Linster M, Tan CW, Le Bert N, Chia WN, Kunasegaran K, et al. Early induction of functional SARS-CoV-2-specific T cells associates with rapid viral clearance and mild disease in COVID-19 patients. Cell Rep 2021, 34, 108728. doi: 10.1016/j.celrep.2021.108728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Karlsson AC, Martin JN, Younger SR, Bredt BM, Epling L, Ronquillo R, et al. Comparison of the ELISPOT and cytokine flow cytometry assays for the enumeration of antigen-specific T cells. J Immunol Methods 2003, 283, 141–53. doi: 10.1016/j.jim.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 42. Tanguay S, Killion JJ.. Direct comparison of ELISPOT and ELISA-based assays for detection of individual cytokine-secreting cells. Lymphokine Cytokine Res 1994, 13, 259–63. [PubMed] [Google Scholar]
- 43. De Marco L, D’Orso S, Pirronello M, Verdiani A, Termine A, Fabrizio C, et al. Preserved T cell reactivity to the SARS-CoV-2 Omicron variant indicates continued protection in vaccinated individuals. bioRxiv 2021; doi: 10.1101/2021.12.30.474453 [DOI] [Google Scholar]
- 44. GeurtsvanKessel CH, Geers D, Schmitz KS, Mykytyn AZ, Lamers MM, Bogers S, et al. Divergent SARS CoV-2 Omicron-reactive T- and B cell responses in COVID-19 vaccine recipients. Sci Immunol 2022, 7(69), eabo2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Keeton R, Tincho MB, Ngomti A, Baguma R, Benede N, Suzuki A, et al. SARS-CoV-2 spike T cell responses induced upon vaccination or infection remain robust against Omicron. medRxiv 2021, 1. doi: 10.1101/2021.12.26.21268380. [DOI] [Google Scholar]
- 46. Madelon N, Heikkilä N, Sabater Royo I, Fontannaz P, Breville G, Lauper K, et al. Omicron-specific cytotoxic T-cell responses after a third dose of mRNA Covid-19 vaccine among patients with multiple sclerosis treated with Ocrelizumab. JAMA Neurol 2022, 10, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tarke A, Sidney J, Methot N, Yu ED, Zhang Y, Dan JM, et al. Impact of SARS-CoV-2 variants on the total CD4(+) and CD8(+) T cell reactivity in infected or vaccinated individuals. Cell Rep Med 2021, 2, 100355. doi: 10.1016/j.xcrm.2021.100355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Liu C, Ginn HM, Dejnirattisai W, Supasa P, Wang B, Tuekprakhon A, et al. Reduced neutralization of SARS-CoV-2 B.1.617 by vaccine and convalescent serum. Cell 2021, 184, 4220–36.e13. doi: 10.1016/j.cell.2021.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Gao Y, Cai C, Grifoni A, Müller TR, Niessl J, Olofsson A, et al. Ancestral SARS-CoV-2-specific T cells cross-recognize the Omicron variant. Nat Med 2022, 28, 472–6. doi: 10.1038/s41591-022-01700-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Parry H, Bruton R, Stephens C, Brown K, Amirthalingam G, Otter A, et al. Differential immunogenicity of BNT162b2 or ChAdOx1 vaccines after extended-interval homologous dual vaccination in older people. Immun Ageing 2021, 18, 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kearns P, Siebert S, Willicombe M, Gaskell C, Kirkham A, Pirrie S, et al. Examining the immunological effects of CoVID-19 vaccination in patients with conditions potentially leading to diminished immune response capacity – The OCTAVE Trial. SSRN Electron J 2021, 1–25. doi: 10.2139/ssrn.3910058. [DOI] [Google Scholar]
- 52. Prendecki M, Thomson T, Clarke CL, Martin P, Gleeson S, De Aguiar RC, et al.; Imperial Renal COVID-19 vaccine study group in collaboration with the OCTAVE Study Consortium. Immunological responses to SARS-CoV-2 vaccines in kidney transplant recipients. Lancet 2021, 398, 1482–4. doi: 10.1016/S0140-6736(21)02096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and Supplementary material.