Abstract
Genitourinary tuberculosis is a rare form of extrapulmonary tuberculosis that affects the kidneys, ureters, prostate, vas deferens, seminal vesicles, testes, and epididymis.
Testicular tuberculosis is a very unusual form, We report a rare case of unilateral testicular tuberculosis that manifested as orchi-epididymitis. The main treatment for urogenital tuberculosis is antituberculosis therapy, possibly combined with surgery.
Keys words: Tuberculosis, Testicular swelling, HIV epidemic, Granulomatous infection
1. Introduction
Pulmonary tuberculosis is the most common form of the disease. The incidence of extrapulmonary tuberculosis has increased over the last few decades mainly due to the HIV epidemic, Genital tuberculosis is rare and testicular tuberculosis is even more unusual.
The most common mechanism of testicular disease caused by tuberculosis is retrograde extension of the infection from the prostate and seminal vesicles, as well as hematogenous diffusion1 dissemination by the pelvic lymphatic system has been considered2
2. Case report
A 41-year-old man, married with 5 children, presented with testicular pain and right testicular swelling for 3 months with a fever of 38° without sinus or scrotal ulceration. He had no history of respiratory symptoms, anorexia, and significant weight loss.
Clinical examination found a febrile patient at 38° with multiple right inguinal lymph nodes, not painful firm and hypertrophied.
The left scrotum was normal, while the right scrotum was painful enlarged with inflammatory signs and a right testicular swelling was 2 cm It was painful, solid, not attached to the scrotal skin. There was no discharge sinus or scrotal ulceration.
In view of this, the patient presented with orchitis, the biological blood test and a cytobacteriological examination of the urine (ECBU) were completed and antibiotics were started to treat the orchitis. The evolution was marked by the persistence of nocturnal fever pain and inflammatory signs, which motivated the completion of the etiologic assessment.
The cytobacteriological examination of the urine was sterile with a high level of leukocyturia, the biological assessment showed a hyperleukocytosis with lymphocytic predominance creatinine: 10 mg/l, ASAT and ALAT are normal.
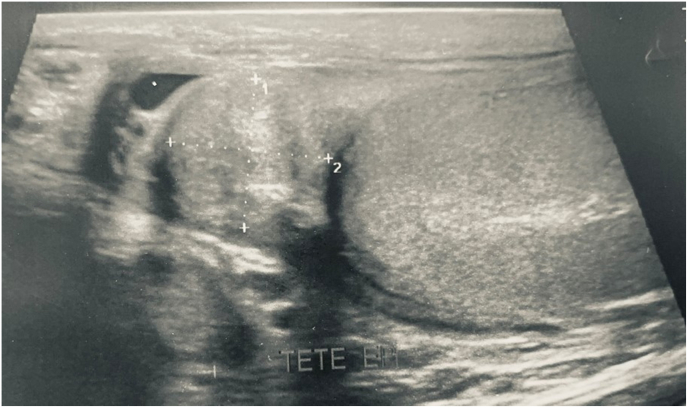
Ultrasound showed a right para-testicular nodule (18 mm) (Fig. 1) the left testis was without abnormality. Testicular tumor markers were β human chorionic gonadotropin <1.5 mIU/mL (N: 0–5), alpha fetoprotein 4.32 ng/mL (N: 0–13.4), and lactate dehydrogenase 173 U/L (N: 125–243). The testicular tumor markers were negative and the ultrasound was not indicative of tumor pathology.
Fig. 1.
Ultrasound showed a right para-testicular nodule (18 mm).
Direct examination for BAAR in urine and semen was negative the spermogram performed showed oligo-spermia. Human Immunodeficiency Virus (HIV), Venereal Disease Research Laboratory (VDRL), Hepatitis B, Hepatitis C, Chlamydia, and Gonorrhea tests were negative.
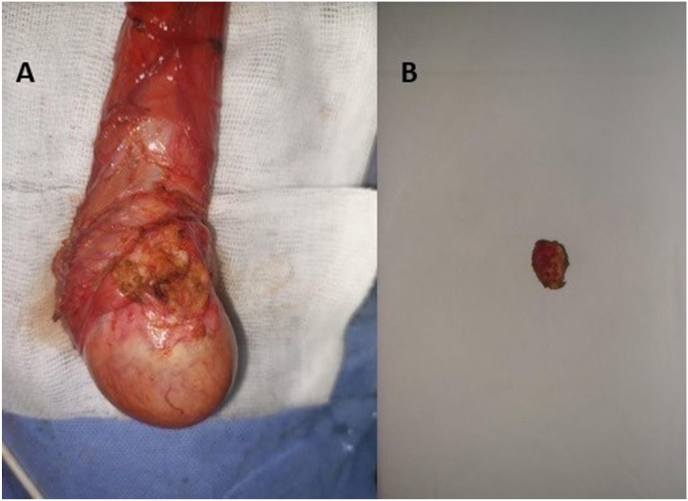
A surgical exploration was performed with resection of the right paratesticular nodule (Fig. 2) without orchiectomy.
Fig. 2.
-A) Image of the testicle after nodule resection -B) operative image showing the resected para-testicular nodule.
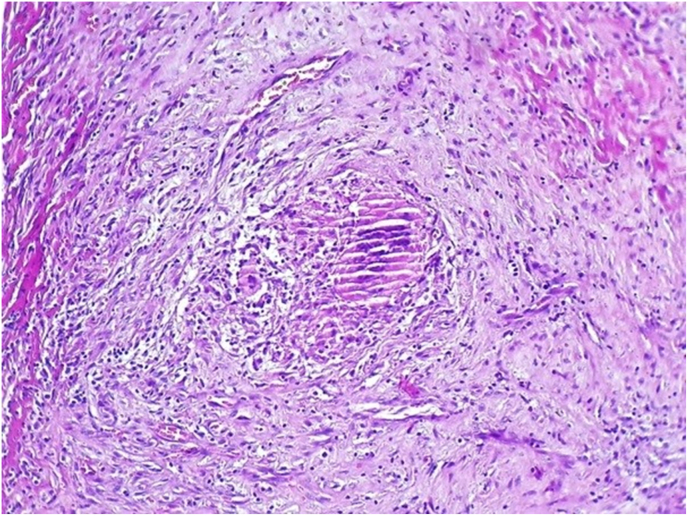
The histological examination of the surgical specimen showed a granulomatous reaction composed of multiple epithelioid cells and multinucleated giant cells surrounded by a lymphocytic infiltrate suggesting testicular tuberculosis (Fig. 3). The diagnosis adopted is an isolated testicular tuberculosis with reactive inguinal adenopathy.
Fig. 3.
Histological examination of the biopsy shows a granulomatous reaction composed of multiple epithelioid cells and multinucleated giant cells, surrounded by a lymphocytic infiltrate (H&E, x100).
The endoscopic examination of the lower urinary tract was normal, a uroscanner was also performed was without particularity. The pulmonary radiography did not show any abnormality.
Our patient has no history of antituberculosis treatment. Pharmacological treatment of tuberculosis was started for our patient, including Isoniazid 300 mg, Rifampicin 600 mg, Pyrazinamide 2000 mg and Ethambutol 1200 mg daily for 2 months Isoniazid and rifampin was maintained for an additional 6 months the evolution after the administration of the treatment was favorable, we also note a disappearance of inguinal lymph nodes at the end of the treatment.
The diagnosis was based on histology, the context and improvement under antibiotics
3. Discussion
Since the advent of HIV infection, tuberculosis has been on the rise worldwide, particularly in developing countries. The disease is most often found in the lungs. All organs may be affected (epididymis and/or testis) during hematogenous, lymphatic, or contiguous dissemination. Isolated genital tuberculosis is rare.
The mode of dissemination of tuberculosis bacilli in the genitalia is controversial, In most cases, tuberculous epididymo-orchitis develops from retrograde dissemination of tubercle bacilli from the infected urinary tract to the prostate by reflux, continued by a ductal propagation towards the seminal vesicle, the vas deferens and the epididymis.3 Tuberculosis bacilli can also penetrate the organism by the blood and lymphatic tracts, it should be noted that tuberculous orchitis without epididymal disease is very unusual, which is reported in our case.
Urogenital tuberculosis, it is more common in men than in women. It usually presents with urinary symptoms that occur in more advanced disease. Male urogenital tuberculosis can usually affect the epididymis and seminal vesicles more than the prostate.
The principal problem of extra pulmonary tuberculosis and particularly genital tuberculosis is in the diagnosis which is often difficult and late in the absence of other evocative localizations, of a notion of contagion or of a history of tuberculosis. The most frequent presentation is a chronic epididymitis possibly an orchitis evolving in a little painful context except in case of superinfection, associated more or less with signs of tuberculosis impregnation.
In the presence of orchitis, without any notion of genital trauma in a subject in full genital activity, the diagnosis is immediately oriented towards sexually transmitted germs which are responsible in 35% of cases, or towards the usual germs of urogenital infection in 25% of cases.4 Other germs, including Mycobacterium tuberculosis, are implicated in 10% of cases. Tuberculosis is responsible for only 2–3% of epididymitis. It is the absence of response to antibiotic treatment or an incomplete response (in the case of superinfection) that most often leads to the diagnosis of tuberculosis as described in our case.
Untreated or incorrectly treated genital tuberculosis has serious consequences on the life of the couple, as it is often complicated by impaired fertility such as oligospermia or azoospermia due to reversible or irreversible organic damage to the genital organs.
The principal treatment for urogenital tuberculosis is antituberculosis chemotherapy, an induction treatment period of 2 months of daily isoniazid, rifampicin, pyrazinamide and ethambutol is followed by a period of 4 or 7 months of daily isoniazid and rifampicin treatment, in endemic regions such as ours, patients with a chronic epididymitis or scrotal mass must be examined for tuberculosis.
4. Conclusion
Tuberculosis can currently present as isolated genital involvement, Tuberculous etiology should be suspected and explored in all cases of persistent orchi-epididymitis, especially in patients with immunosuppression, General evaluation, to identify other bacillary locations is necessary.
Declaration of competing interest
The authors declare that there is no conflict of interests regarding the publication of this article.
References
- 1.Muttarak M., Wilfred P.G.C., Lojanapiwat B., Chaiwun B. Tuberculous epididymitis and epididymo-orchitis. Am J Roentgenol. 2001;176:1459–1466. doi: 10.2214/ajr.176.6.1761459. [DOI] [PubMed] [Google Scholar]
- 2.Muttarak M., Wilfred P.G.C. Case 91: tuberculous epididymo-orchitis. Radiology. 2006;238:748–751. doi: 10.1148/radiol.2382031851. 2. MBBS, FRCP, FRCR. [DOI] [PubMed] [Google Scholar]
- 3.Wise G.J., Shteynshlyuger A. An update on lower urinary tract tuberculosis. Curr Urol Rep. 2008;9:305–313. doi: 10.1007/s11934-008-0053-9. [DOI] [PubMed] [Google Scholar]
- 4.Delaviere D., Fournier G., Et Mangin P. Orchi-épididymites - editions techniques. Encycl. Méd. Chir. (Paris - France), Nephrologie - Urologie. 1992;18635 A 10:11p. [Google Scholar]