Abstract
Background
Social frailty is one type of frailty. Physical frailty with cardiovascular and cerebrovascular diseases (CCVD) have been studied a lot, but less research on social frailty.
Objectives
To study the prevalence, related risk factors and regional differences of social frailty with CCVD in Chinese older adults.
Methods
SSAPUR was a national cross-sectional survey. Participants aged 60 years or older were recruited in August 2015. Demographic data and information regarding family, health and medical conditions, living environment conditions, social participation, spiritual and cultural life, and health condition were obtained. Social frailty was assessed in five areas (HALFE Social Frailty Index) including inability to help others, limited social participation, loneliness, financial difficulty, and living alone. The prevalence of CCVD with social frailty, related risk factors and regional differences in CCVD with social frailty were studied.
Results
A total of 222,179 participants were enrolled. 28.4% of them had CCVD history. The prevalence of social frailty in the CCVD group was 16.03%. In CCVD participants, compared with the group without social frailty, there were significant differences in gender, age, urban–rural distribution, ethnicity, marital status, and education levels in the social frailty group. Significant differences were also found in physical exercise participation, health status, cataract, hypertension, diabetes mellitus, hospitalization within 1 year, self-assessed health status, crutch or wheelchair usage, urinary and fecal incontinence, need for care from others, fall history, housing satisfaction, and self-assessed happiness in the social frailty group. Women with CCVD had a higher prevalence of social frailty than men. By age in CCVD with social frailty, the highest prevalence was found in participants 75–79 years old. The prevalence of CCVD was significant difference between social frailty in urban and rural group. The prevalence of social frailty with CCVD was significantly different in different regions. The highest prevalence was 20.4% in southwest area, and the lowest prevalence was 12.5% in northeast with area.
Conclusion
The prevalence of social frailty among the CCVD older adults is high. Factors such as gender, age, region, urban–rural residence, and the state of the disease may be associated with social frailty.
Keywords: social frailty, cardiovascular and cerebrovascular disease, Chinese, healthy aging, older adults
Introduction
It is estimated that over 300 million Chinese people will be 60 years of age or older by 2025 (1). With this aging demographic, the prevalence of chronic diseases like cardiovascular and cerebrovascular diseases (CCVDs) and frailty will increase. CCVDs are a major cause of death among Chinese people, adding to the public health burden in China (2). Frailty describes a state of vulnerability due to an age-related decline in several physiological systems (3) and is associated with a considerably increased risk of falling, disability, hospitalization, and mortality (4, 5). Frailty has become a major public health concern in the current context of aging due to its impact on the older adults access’s to medical resources and age-related services. Frailty has received notable attention in the healthcare community in recent years due to its potentially adverse consequences for the older adults and society as a whole.
Existing research on risk factors of frailty mainly focuses on sociodemographic, physiological, and biological risk factors (6–11). In recent years, frailty has evolved from a concept focused on physical frailty to one that encompasses multiple health aspects (physical, psychological, and social) (12–21). Physical frailty indicates physical vulnerability, whereas social frailty is conceptualized as being at risk of losing or having lost sufficient social support, activities, or resources required to fulfill basic social needs (12, 15, 16, 20, 22–35). Several instruments have previously been used to assess social frailty among community-dwelling older adults, most commonly evaluating social activities, social support, social networks, loneliness, and living alone (12, 16, 20, 22, 25, 36–49). One study reported a nearly 30% overlap between physical and social frailty (24). Social frailty is a risk factor for long-term mortality and disability, and has a prevalence of approximately 18%–30% among community-dwelling older adults (24, 50–52). Research on social frailty is important, particularly in the context of situations such as quarantine or physical isolation, which have recently arisen due to the COVID-19 pandemic (32, 37, 53).
Frailty is believed to have a bidirectional effect on cardiovascular diseases (32, 33). Emerging evidence suggests that frailty is a risk factor for CCVDs, even after accounting for subclinical atherosclerosis (27). Conversely, CCVD risk factors and risk scores may predict frailty (33, 34): frailty is associated with a higher risk of CCVD prevalence (18). Therefore, frailty can be considered both a consequence of and a potential risk factor for CCVDs (18, 27, 33, 35, 37, 41, 42). Existing reports on the prevalence of frailty in the older adults with CCVDs are based on a unidimensional view of frailty in which only physical deficits are considered when determining frailty. The prevalence of social frailty in Chinese older adults with CCVDs has not been reported. Regional differences in the prevalence of social frailty may exist in the older adults in China. Therefore, the characteristics of the older adults with CCVDs combined with social frailty need to be investigated. This study uses data from the fourth Sample Survey of the Aged Population in Urban/Rural China (SSAPUR) conducted in 2015 and provides reference information for early interventions for CCVD patients with social frailty.
Materials and methods
Study population
Data were obtained from the database of the fourth SSAPUR, conducted by the China National Committee on Ageing in 2015. Chinese citizens aged 60 or above were surveyed to compile the largest database of older people in China. The sampling method of the survey was introduced in a previous study (43). The SSAPUR covered 31 provinces, autonomous regions, municipalities, and the Xinjiang Production and Construction Corps, including 466 counties (districts), 1,864 townships (sub-districts), and 7,456 village (residential) committees. The questionnaire covered nine domains: demographic information, family situation, health status, healthcare and nursing services, economic status, social activity, living environment, and spiritual and cultural life (including psychological status), and was divided into simplified and detailed forms, as introduced in a previous study (43). CCVDs included coronary heart disease, angina pectoris, and stroke as self-reported by the participants.
The research protocol was approved by the National Bureau of Statistics (No. [2014] 87) and the Ethics Committee of the Beijing Hospital (2021BJYYEC-294-01). All participants provided written informed consent before completing the questionnaire. The number of collected samples was 2,24,142.
Definition of social frailty
Social frailty screening questionnaire: HALFE scale
To identify and assess social frailty, we considered five categories based on previous studies (7, 12–16, 21, 22, 44–50): inability to help others, limited social participation, loneliness, financial difficulty, and living alone. “HALFE” is an acronym for these five components: Help, pArticipation, Loneliness, Financial situation, and living alonE. The ability to help others was measured by asking participants if they were able to help their friends or family within the past 12 months. If participants responded “no,” the item was scored 1. Limited social participation was assessed by asking participants if they had engaged in any social or leisure activities in the past 12 months. If participants responded “no,” the item was scored 1. Loneliness was scored 1 if participants responded “yes” to feeling lonely. The financial situation was divided into five grades: very wealthy, relatively wealthy, basically enough, relatively difficult, or very difficult. Financial difficulty was scored 1 if participants had a “relatively difficult” or “very difficult” financial situation. Living alone was scored 1 if the participants lived alone. The total score on the HALFE scale ranges from 0 to 5, with a total score ≥ 3 indicating social frailty.
Statistical analysis
The characteristics of subjects with and without social frailty were compared using one-way analysis of variance (ANOVA) for normal-distributed quantitative data and the Chi-square test for categorical data. Multivariate logistic regression was performed to estimate the adjusted odds ratios and 95% confidence intervals (CIs) of variables associated with social frailty. p-value < 0.05 was chosen as the threshold for statistical significance. All statistical analyses were performed using SPSS 24.0 (IBM Corp., Armonk, NY, United States).
Results
Prevalence of social frailty in CCVD group and non-CCVD group
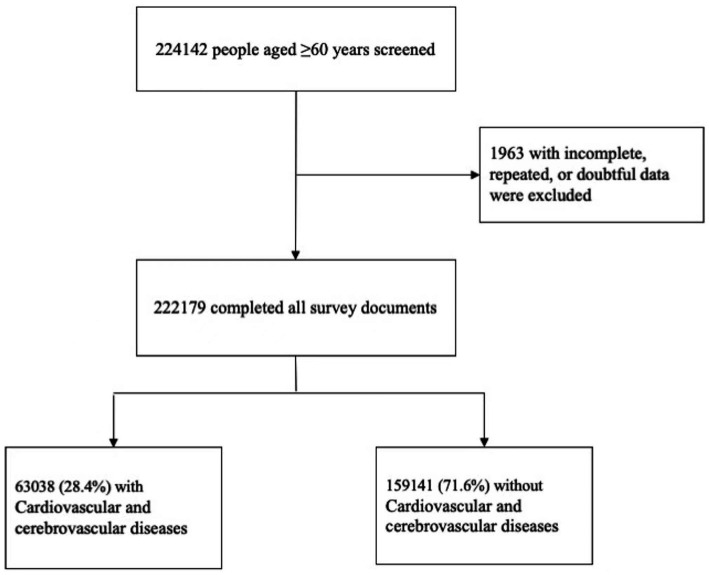
Data of 2,24,142 participants were collected from SSAPUR 2015. After excluding 1,963 cases with missing, doubtful, or duplicate data, 2,22,179 cases were included in the final analysis. Among the participants, 63,038 (28.4%) had a history of CCVDs and 1,59,141 (71.6%) did not have CCVDs (Figure 1).
Figure 1.
Study flowchart.
The prevalence of social frailty was 16.03% in the CCVD group and 14.9% in the non-CCVD group, with significant differences between the two groups (p < 0.001). There were significant differences in gender, age, urban–rural distribution, ethnicity, marital status, and education levels in the CCVD group with social frailty than without social frailty (Table 1). Women with CCVDs had a higher prevalence of social frailty than men with CCVDs (Table 1).
Table 1.
The prevalence of social frailty status based on demographic information in the group with and without CCVD.
| Non-CCVD | CCVD | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-SF n (%) | SF n (%) | Total | χ2 | P-value | Non-SF n (%) | SF n (%) | Total | χ2 | P-value | ||
| Gender | Female | 68,501 (85.4) | 11,740 (14.6) | 80,241 | 7.108 | 0.008 | 29,891 (83.5) | 5,906 (16.5) | 35,797 | 12.692 | <0.001 |
| Male | 66,981 (84.9) | 11,919 (15.1) | 78,900 | 23,033 (84.6) | 4,208 (15.4) | 27,241 | |||||
| Ethnicity | Han ethnic group | 127,156 (85.4) | 21,652 (14.6) | 148,808 | 181.274 | <0.001 | 50,182 (84.1) | 9,512 (15.9) | 59,694 | 10.052 | 0.002 |
| Non-Han ethnic group | 8,326 (80.6) | 2007 (19.4) | 10,333 | 2,742 (82.0) | 602(18.0) | 3,344 | |||||
| Educational levels | Non-Illiteracy | 97,973 (86.9) | 14,786 (13.1) | 112,759 | 940.187 | <0.001 | 37,746 (85.5) | 6,400 (14.5) | 44,146 | 261.693 | <0.001 |
| Illiteracy | 37,509 (80.9) | 8,873 (19.1) | 46,382 | 15,178 (80.3) | 3,714 (19.7) | 18,892 | |||||
| Marriage status | Spousal presence | 106,132 (90.9) | 10,605 (9.1) | 116,737 | 11573.141 | <0.001 | 39,572 (89.2) | 4,808 (10.8) | 44,380 | 3022.222 | <0.001 |
| Single | 29,350 (69.2) | 13,054 (30.8) | 42,404 | 13,352 (71.6) | 5,306 (28.4) | 18,658 | |||||
| Age | 60–64 | 49,270 (87.5) | 7,011 (12.5) | 56,281 | 588.488 | <0.001 | 14,229 (84.4) | 2,627 (15.6) | 16,856 | 48.623 | <0.001 |
| 65–69 | 32,286 (85.5) | 5,470 (14.5) | 37,756 | 12,363 (83.9) | 2,366 (16.1) | 14,729 | |||||
| 70–74 | 21,029 (83.3) | 4,231 (16.7) | 25,260 | 9,712 (82.9) | 2009 (17.1) | 11,721 | |||||
| 75–79 | 15,841 (81.7) | 3,541 (18.3) | 19,382 | 7,981 (82.7) | 1,671 (17.3) | 9,652 | |||||
| 80–84 | 10,352 (82.3) | 2,221 (17.7) | 12,573 | 5,583 (85.4) | 953 (14.6) | 6,536 | |||||
| 85 and over | 6,704 (85.0) | 1,185 (15.0) | 7,889 | 3,056 (86.2) | 488 (13.8) | 3,544 | |||||
| Urban/ rural |
Urban | 72,454 (89.5) | 8,506 (10.5) | 80,960 | 2475.505 | <0.001 | 30,613 (88.2) | 4,087 (11.8) | 34,700 | 1042.973 | <0.001 |
| Rural | 83,028 (80.6) | 15,153 (19.4) | 78,181 | 22,311 (78.7) | 6,027 (21.3) | 28,338 | |||||
CCVD, cardiovascular and cerebrovascular diseases; SF, social frailty.
Significant differences were also found in physical exercise participation, health status, the prevalence of cataract, hypertension, and diabetes mellitus, hospitalization within 1 year, self-assessed health status, crutch or wheelchair usage, urinary and fecal incontinence, need for care from others, fall history, housing satisfaction, and self-assessed happiness in the CCVD group with social frailty (Table 2). However, no significant differences were found in cataract and hypertension prevalence in the non-CCVD group with social frailty compared with the non-CCVD participants without social frailty (Table 2).
Table 2.
The prevalence of social frailty status based on health/medical conditions and social participation in the group with and without CCVD.
| Non-CCVD | CCVD | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-SF n (%) | SF n (%) | Total | χ2 | P-value | Non-SF n (%) | SF n (%) | Total | χ2 | P-value | ||
| Physical exercise | Once a week or more | 64,133 (87.8) | 8,886 (12.2) | 73,019 | 775.593 | <0.001 | 24,899 (85.9) | 4,103 (14.1) | 29,002 | 143.500 | <0.001 |
| No | 71,349 (82.2) | 14,773 (17.2) | 86,122 | 28,025 (82.3) | 6,011 (17.7) | 34,036 | |||||
| Cataract/ glaucoma |
No | 114,566 (85.2) | 19,931(14.8) | 134,497 | 0.526 | 0.468 | 44,893 (84.3) | 8,373 (15.7) | 53,266 | 63.240 | <0.001 |
| Yes | 20,916 (84.9) | 3,728 (15.1) | 24,644 | 8,031 (82.2) | 1741 (17.8) | 9,772 | |||||
| Hypertension | No | 92,897 (85.1) | 16,308 (14.9) | 109,205 | 1.223 | 0.269 | 21,784 (82.0) | 4,769 (18.0) | 26,553 | 125.0.034 | <0.001 |
| Yes | 42,585(85.3) | 7,351 (14.7) | 49,936 | 31,140 (85.4) | 5,345 (14.6) | 36,485 | |||||
| Diabetes mellitus | No | 125,578 (80.6) | 22,182 (19.4) | 147,760 | 34.556 | <0.001 | 39,820 (82.0) | 8,736 (18.0) | 48,556 | 594.997 | <0.001 |
| Yes | 9,904 (87.0) | 1,477 (13.0) | 11,381 | 13,104 (90.5) | 1,378 (9.5) | 14,482 | |||||
| Osteopathy | No | 80,719 (87.8) | 11,183 (12.2) | 91,902 | 1251.268 | <0.001 | 31,751 (87.3) | 4,617 (12.7) | 36,368 | 715.773 | <0.001 |
| Yes | 54,763 (81.4) | 12,476 (18.6) | 67,239 | 21,173 (79.4) | 5,497 (20.6) | 26,670 | |||||
| Cancer | No | 134,023 (85.2) | 23,307 (14.8) | 157,330 | 30.229 | <0.001 | 52,417 (84.0) | 9,967 (16.0) | 62,384 | 20.302 | <0.001 |
| Yes | 1,459 (80.6) | 352 (19.4) | 1811 | 507 (77.5) | 147 (22.5) | 654 | |||||
| Lung diseases | No | 124,464 (85.8) | 20,612 (14.2) | 145,076 | 563.182 | <0.001 | 46,823 (84.9) | 8,327 (15.1) | 55,150 | 292.468 | <0.001 |
| Yes | 11,018 (78.3) | 3,047 (21.7) | 14,065 | 6,101 (77.3) | 1787 (22.7) | 7,888 | |||||
| Dentures | No | 101,075 (85.0) | 17,803 (15.0) | 118,878 | 4.424 | 0.035 | 39,671 (84.4) | 7,318 (15.6) | 46,989 | 30.323 | <0.001 |
| Yes | 34,407 (85.5) | 5,856 (14.5) | 40,263 | 13,253 (82.6) | 2,796 (17.4) | 16,049 | |||||
| Crutching using | No | 124,022 (85.4) | 21,244 (14.6) | 145,266 | 77.404 | <0.001 | 48,584 (84.2) | 9,090 (15.8) | 57,674 | 40.382 | <0.001 |
| Yes | 11,460 (82.6) | 2,415 (17.4) | 13,875 | 4,340 (80.9) | 1,024 (19.1) | 5,364 | |||||
| Wheel chairs using | No | 132,991 (85.1) | 23,303 (14.9) | 156,294 | 12.782 | <0.001 | 51,889 (83.9) | 9,954 (16.1) | 61,843 | 6.375 | 0.012 |
| Yes | 2,491 (87.5) | 356 (12.5) | 2,847 | 1,035 (86.6) | 160 (13.4) | 1,195 | |||||
| Hospitalization within 1 year | No | 106,361 (86.1) | 17,224 (13.9) | 123,585 | 377.772 | <0.001 | 31,871 (85.5) | 5,400 (14.5) | 37,271 | 163.853 | <0.001 |
| Once or more | 29,121 (81.9) | 6,435 (18.1) | 35,556 | 21,053 (81.7) | 4,714 (18.3) | 25,767 | |||||
| Self-awareness of healthy | Healthy | 123,738 (86.6) | 19,157 (13.4) | 142,895 | 2358.570 | <0.001 | 40,721 (86.3) | 6,443 (13.7) | 47,164 | 789.891 | <0.001 |
| Unhealthy | 11,744 (72.3) | 4,502 (27.7) | 16,246 | 12,203 (76.9) | 3,671 (23.1) | 15,874 | |||||
| Fecal incontinence | No | 128,018 (85.2) | 22,223 (14.8) | 1,150,241 | 11.979 | 0.001 | 41,820 (82.7) | 8,748 (17.3) | 50,568 | 2,980,991 | <0.001 |
| Yes | 7,464 (83.9) | 1,436 (16.1) | 8,900 | 11,104 (89.0) | 1,366 (11.0) | 12,470 | |||||
| Urinary incontinence | No | 125,671 (85.4) | 21,525 (14.6) | 147,196 | 91.743 | <0.001 | 39,822 (82.9) | 8,221 (17.1) | 48,043 | 170.852 | <0.001 |
| Yes | 9,811 (82.1) | 2,134 (17.9) | 11,945 | 13,102 (87.4) | 1893 (12.6) | 14,995 | |||||
| Supporting supplies Hearing aids | No | 133,481 (85.1) | 23,331 (14.9) | 156,812 | 1.146 | 0.284 | 52,079 (84.0) | 9,946 (16.0) | 62,025 | 0.223 | 0.637 |
| Yes | 2001 (85.9) | 328 (14.1) | 2,329 | 845 (83.4) | 168 (16.6) | 1,013 | |||||
| Diapers | No | 134,236 (85.1) | 23,441 (14.9) | 157,677 | 0.001 | 0.979 | 52,431 (84.0) | 10,009 (16.0) | 62,440 | 1.028 | 0.311 |
| Yes | 1,246 (85.1) | 218 (14.9) | 1,464 | 493 (82.4) | 105 (17.6) | 598 | |||||
| Need care from others | No | 116,947 (85.5) | 19,801 (14.5) | 136,748 | 114.864 | <0.001 | 45,046 (84.3) | 8,405 (15.7) | 53,451 | 26.653 | <0.001 |
| Yes | 18,535 (82.8) | 3,858 (17.2) | 22,393 | 7,878 (82.2) | 1709 (17.8) | 9,587 | |||||
| Number of chronic diseases | Less than 2 | 95,184 (86.9) | 14,339 (13.1) | 109,523 | 873.913 | <0.001 | 8,771 (86.2) | 1,409 (13.8) | 10,180 | 43.759 | <0.001 |
| 2 or more | 40,298 (81.2) | 9,320 (18.8) | 49,618 | 44,153 (83.5) | 8,705 (16.5) | 52,858 | |||||
| Falls | No | 117,686 (86.4) | 18,482 (13.6) | 136,168 | 1247.462 | <0.001 | 41,231 (85.8) | 6,799 (14.2) | 48,030 | 534.171 | <0.001 |
| Yes | 17,796 (77.5) | 5,177 (22.5) | 22,973 | 11,693 (77.9) | 3,315 (22.1) | 15,008 | |||||
| Housing satisfaction | Satisfied | 121,007 (87.2) | 17,745 (12.8) | 138,752 | 3693.782 | <0.001 | 45,552 (86.0) | 7,408 (14.0) | 52,960 | 1039.944 | <0.001 |
| Dissatisfied | 14,475 (71.0) | 5,914 (29.0) | 20,389 | 7,372 (73.1) | 2,706 (26.9) | 10,078 | |||||
| Happiness | Happy | 127,448 (85.6) | 21,517 (14.4) | 148,965 | 328.350 | <0.001 | 49,733 (84.4) | 9,215 (15.6) | 58,948 | 114.418 | <0.001 |
| Unhappy | 8,034 (79.0) | 2,142 (21.0) | 10,176 | 3,191 (78.0) | 899 (22.0) | 4,090 | |||||
| Self-care ability | Fully independent | 117,378 (86.2) | 18,768 (13.8) | 136,146 | 870.731 | <0.001 | 38,998 (85.0) | 6,864 (15.0) | 45,862 | 145.117 | <0.001 |
| Dependent | 18,104 (78.7) | 4,891 (21.3) | 22,995 | 13,926 (81.1) | 3,250 (18.9) | 17,176 | |||||
CCVD, cardiovascular and cerebrovascular diseases; SF, social frailty.
Sub-group analysis of the prevalence of social frailty in CCVD patients
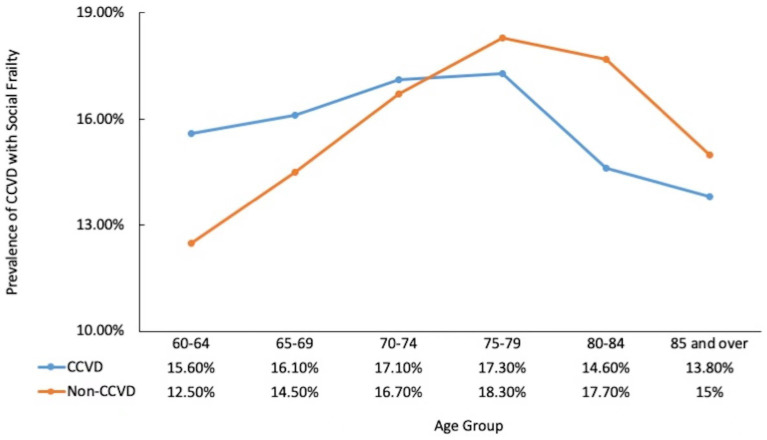
The highest prevalence of social frailty in the CCVD group was observed in participants aged 75–79. For participants aged below 75, the prevalence of social frailty was higher in the CCVD group than in the non-CCVD group, and the prevalence rate increased with age. The opposite trend was observed in participants aged above 75, with less prevalence of social frailty in the CCVD group than in the non-CCVD group, and the prevalence rate decreased with age (see Table 3; Figure 2 for details).
Table 3.
The prevalence of social frailty in the group with and without CCVD by ages.
| Non-CCVD | CCVD | |||
|---|---|---|---|---|
| Age group | Prevalence of SF | CI (%) | Prevalence of SF | CI (%) |
| 60–64 | 12.5% | 12.19–12.74 | 15.6% | 15.04–16.14 |
| 65–69 | 14.5% | 14.14–14.85 | 16.1% | 15.48–16.66 |
| 70–74 | 16.7% | 16.29–17.22 | 17.1% | 16.47–17.83 |
| 75–79 | 18.3% | 17.73–18.82 | 17.3% | 16.57–18.08 |
| 80–84 | 17.7% | 17.00–18.34 | 14.6% | 13.75–15.46 |
| 85 and over | 15.0% | 14.25–15.83 | 13.8% | 12.67–14.94 |
CCVD, cardiovascular and cerebrovascular diseases.
Figure 2.
Prevalence of social frailty by age and CCVD status CCVD, cardiovascular and cerebrovascular diseases.
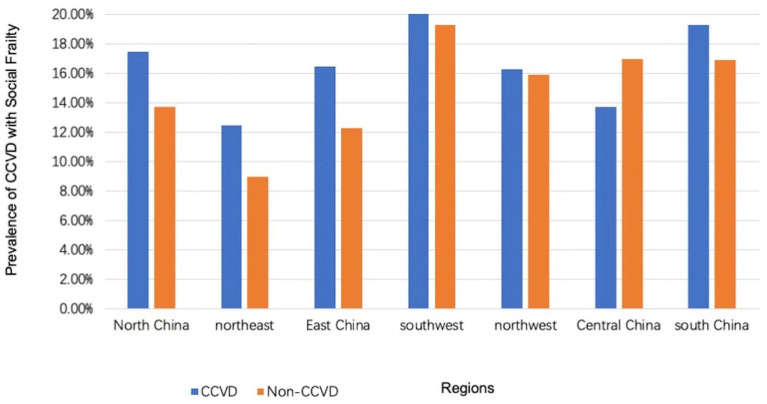
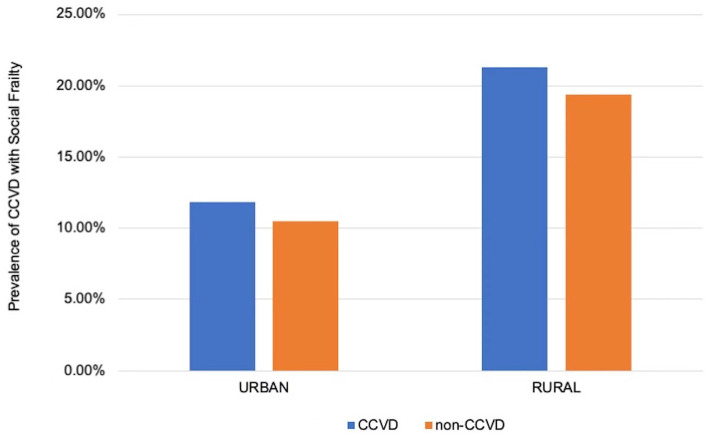
There existed significant differences in the prevalence of social frailty in CCVD patients with hypertension and CCVD patients with diabetes. The prevalence of social frailty in CCVD patients also varied based on region (p < 0.001, see Table 4; Figure 3 for details): Southwest China had the highest prevalence of social frailty (20.4%) and the Northeast had the lowest prevalence rate (12.5%). The prevalence of social frailty combined with CCVDs was 11.8% in urban areas and 21.3% in rural areas, with significant differences (see Figure 4).
Table 4.
The prevalence of social frailty in different regions in the group with and without CCVD.
| Non-CCVD | CCVD | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Non-SF n (%) | SF n (%) | Total | χ2 | P-value | Non-SF n (%) | SF n (%) | Total | χ2 | P-value | |
| North China | 13,640(86.3) | 2,171(13.7) | 15,811 | 1175.768 | 0.000 | 7,383(82.5) | 1,562(17.5) | 8,945 | 275.231 | 0.000 |
| Northeast China | 10,123(91.0) | 1,003(9.0) | 11,126 | 6,521(87.5) | 929(12.5) | 7,450 | ||||
| East China | 47,436(87.7) | 6,678(12.3) | 54,114 | 13,424(83.5) | 2,651(16.5) | 16,075 | ||||
| Southwest China | 23,112(80.7) | 5,518(19.3) | 28,630 | 5,778(79.6) | 1,478(20.4) | 7,256 | ||||
| Northwest China | 7,445(84.1) | 1,407(15.9) | 8,852 | 3,816(83.7) | 742(16.3) | 4,558 | ||||
| Central China | 17,236(83.0) | 3,537(17.0) | 20,773 | 13,436(86.3) | 2,173(13.7) | 15,573 | ||||
| South China | 16,490(83.1) | 3,345(16.9) | 19,835 | 2,566(80.7) | 615(19.3) | 3,181 | ||||
CCVD, cardiovascular and cerebrovascular diseases.
Figure 3.
Prevalence of social frailty in the group with and without CCVD in different regions of China CCVD, cardiovascular and cerebrovascular diseases.
Figure 4.
Prevalence of social frailty in the group with and without CCVD in urban and rural area of China CCVD, cardiovascular and cerebrovascular diseases.
Multivariate regression analysis showed that gender, age, educational level, marital status, living in an urban vs. rural environment, physical exercise, number of comorbid chronic diseases, lung diseases, cancer, wheelchair usage, fecal incontinence, fall history, housing satisfaction, self-assessed happiness, and self-care ability were all associated with social frailty in CCVD patients (see Table 5).
Table 5.
Factors associated with social frailty in the group with CCVD.
| Variables | Comparison | Groups | Chi-square value | P-value | OR | 95%CI |
|---|---|---|---|---|---|---|
| Gender | Female | Male | 139.871 | <0.001 | 1.356 | 1.290–1.427 |
| Educational levels | Illiteracy | Non-Illiteracy | 10.691 | 0.001 | 1.094 | 1.037–1.115 |
| Marriage status | Single | Spousal presence | 3195.182 | <0.001 | 4.389 | 4.170–4.620 |
| Age | 85 and over | 60–64 | 304.836 | <0.001 | 0.349 | 0.310–0.393 |
| 65–69 | 261.724 | <0.001 | 0.378 | 0.337–0.426 | ||
| 70–74 | 215.989 | <0.001 | 0.416 | 0.370–0.467 | ||
| 75–79 | 133.836 | <0.001 | 0.502 | 0.446–0.564 | ||
| 80–84 | 24.167 | <0.001 | 0.733 | 0.647–0.830 | ||
| Urban or rural area | Rural | Urban | 575.700 | <0.001 | 1.815 | 1.729–1.906 |
| Physical exercise | Once a week or more | No | 4.341 | 0.037 | 0.949 | 0.903–0.997 |
| Number of chronic diseases | 2 or more | Less than 2 | 6.363 | 0.012 | 1.114 | 1.024–1.212 |
| Wheel chairs using | Yes | No | 4.729 | 0.030 | 0.822 | 0.688–0.981 |
| Housing satisfaction | Dissatisfied | Satisfied | 733.424 | <0.001 | 2.126 | 2.013–2.245 |
| Cataract/ glaucoma | Yes | No | 9.300 | 0.002 | 1.100 | 1.035–1.169 |
| Hypertension | Yes | No | 18.498 | <0.001 | 0.889 | 0.843–0.938 |
| Diabetes mellitus | Yes | No | 171.904 | <0.001 | 0.626 | 0.583–0.671 |
| Osteopathy | Yes | No | 169.766 | <0.001 | 1.430 | 1.355–1.509 |
| Lung diseases | Yes | No | 67.305 | <0.001 | 1.306 | 1.226–1.392 |
| Cancer | Yes | No | 22.781 | <0.001 | 1.624 | 1.331–1.982 |
| Dentures | Yes | No | 6.180 | 0.013 | 1.068 | 1.014–1.124 |
| Fecal incontinence | Yes | No | 120.794 | <0.001 | 0.676 | 0.630–0.724 |
| Falls | Yes | No | 189.009 | <0.001 | 1.435 | 1.363–1.510 |
| Happiness | Unhappy | Happy | 38.299 | <0.001 | 1.303 | 1.199–1.418 |
| Self-care ability | Dependent | Fully independent | 12.624 | <0.001 | 1.103 | 1.045–1.164 |
CCVD, cardiovascular and cerebrovascular diseases; SF, social frailty.
Discussion
To the best of our knowledge, this study conducts the most extensive survey on social frailty among the older adults in urban and rural China to date. The study investigated the prevalence of social frailty in the older adults with CCVDs in China and identified health risk factors and socioeconomic factors associated with social frailty.
The findings showed that 16.03% of the older adults with CCVDs also suffered from social frailty. This confirms that CCVDs and frailty are common among community-dwelling older adults. Age is a significant predictor of frailty. Thinuan et al. showed that age was associated with a higher prevalence of prefrailty and frailty. Frailty, in turn, is associated with an increased occurrence of CCVDs (32, 33, 35). This study showed that the prevalence of social frailty combined with CCVDs varied with age: social frailty increased with age till 80 years, after which it decreased with age. The highest prevalence of social frailty was observed in participants with CCVDs aged 75–79 years, which may be because many older adults with CCVDs and social frailty do not survive to be 80. Social frailty is associated with lower dietary intake, poor diet quality, and poor nutrition among community-dwelling older men, which in turn are associated with physical frailty, cognitive decline, hospitalization, and mortality (20–26). The prevalence of social frailty decreased in those with CCVDs aged 80 and beyond, possibly because older adults require more companionship, are less likely to live alone, and have more social interactions, reducing the prevalence of social frailty.
Regarding gender, in the case of the CCVD group, the prevalence of social frailty was higher in women than in men, whereas, for non-CCVD participants, the prevalence of social frailty was higher in men than in women. The prevalence of social frailty in patients with heart failure can be as high as 66.5% (33). Some studies have shown that the prevalence of heart failure is higher in older adults women than in older adults men: heart failure prevalence is 10 per 1,000 people after the age of 65 years, with 8.6% of men and 11.5% of women aged > 80 years afflicted with heart failure (32, 33). Men diagnosed with frailty syndrome are more likely to suffer from heart failure than women (35). Thus, the relationship between gender and social frailty needs further study.
Furthermore, the survey showed a significant difference in the prevalence of social frailty combined with CCVDs across different regions in mainland China. According to the China Cardiovascular Health Report 2016, the prevalence of CCVDs is significantly higher in the north than in the south, with the highest prevalence rate in Northeast China, followed by North China, and a lower prevalence rate in South China, Central China, East China, Northwest China, and Southwest China. As for the prevalence of social frailty in the older adults with CCVDs, Southwest China had the highest prevalence rate of 20.4%, and the Northeast had the lowest prevalence rate of 12.5%. These differences may be related to cultural factors and social economies of the regions and need further exploration.
The findings also showed a significant difference in the prevalence of social frailty among the older adults with CCVDs between urban and rural areas in mainland China, with a significantly higher prevalence in rural people than in urban people. This difference may be related to the overall higher economic and cultural levels and living conditions associated with urban environments. Therefore, eliminating the urban–rural gap and economic development are critical to alleviating social frailty.
An interesting phenomenon is the occurrence of social frailty in hypertensive older adults. Hypertension is one of the most important risk factors for CCVDs and its prevalence increases with age, affecting endothelial function and leading to oxidative stress, inflammation, and atherosclerosis. For non-CCVD older adults, the prevalence of social frailty in those with and without hypertension was 14.7% and 14.9%, respectively, without significant differences. For the older adults with CCVDs, the prevalence of social frailty in those with and without hypertension was 14.6% and 18.0%, respectively, with a significant difference. This may be related to the long medical history of patients with hypertension, and their increased awareness of the need for long-term medication, follow-up, monitoring, and exercise.
Hyperglycemia is one of the most common comorbidities in older adults, driving inflammation and oxidative stress, leading to endothelial dysfunction, with a negative impact on frail patients. Hyperglycemia is frequently observed in frail older adults and is an independent predictor of poor health outcomes. High glucose levels may increase the risk of frailty in older adults, causing physical impairment in frail hypertensive older adults (5, 39, 54). However, in this study, for the non-CCVD group, the prevalence of social frailty with and without diabetes was 13% and 19.4%, respectively, with significant differences. For the older adults with CCVDs, the prevalence of social frailty with and without diabetes was 9.5% and 18.0%, respectively. The lower prevalence of social frailty among diabetes patients may be because treatment for diabetes requires keeping a close watch over one’s blood sugar levels with a combination of medications, exercise, and diet. Patients with diabetes go to the hospital every few months to see their doctors, talk with other diabetes patients, and often participate in sports activities, which increases their social participation, thus lowering the risk of social frailty.
The findings of this study have important implications for clinical practice. More research is required on social frailty as it influences health outcomes through health behaviors and lifestyles. Social frailty cannot be screened or treated simply with medications but requires comprehensive attention to the social environment; thus, it is necessary to pay attention to social frailty in older adults and actively manage consequent problems and implement relevant interventions (32, 33, 35, 55).
The study also has some limitations. Firstly, the data on CCVDs were self-reported and might be subject to memory bias. Secondly, owing to the cross-sectional design of the study, causality could not be explored. This should be investigated in a future prospective study. Thirdly, the categories of social frailty were based on recent studies rather than an established method. Therefore, future research on instrument development to measure social frailty is needed.
Conclusion
This study shows that there is a high prevalence of social frailty among the older adults with CCVDs in China. Factors such as gender, age, region, urban–rural residence, and the state of the disease influence the prevalence of social frailty. Future research should further study the relevant factors affecting the occurrence and development of social frailty and its relationship with physical frailty to improve frailty prognosis and the quality of life of older patients with CCVDs.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
XQ and NJ wrote the various drafts of the manuscript. XQ, LM, and PZ conducted the statistical analyses, with advice from JH, JmL, JS, XZ, HL and JuL were involved in data interpretation. DL, QZ, JuL, and XQ conceived and designed this study. Drafts of the manuscript were revised for important scientifific content by XQ, NJ, JH, LM, PZ, JmL, JS, XZ, HL, QZ, JuL and DL. DL is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors gave final approval of the version to be published.
Funding
The present study was funded by the National Key R&D Program of China (grant nos. 2020YFC2003000 and 2020YFC2003001). DL has full access to all study data and has final responsibility for the decision to submit for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1022208/full#supplementary-material
References
- 1.Eggleston K, Ling L, Qingyue M, Lindelow M, Wagstaff A. Health service delivery in China: a literature review. Health Econ. (2008) 17:149–65. doi: 10.1002/hec.1306, PMID: [DOI] [PubMed] [Google Scholar]
- 2.The Writing Committee of the Report on Cardiovascular Health and Diseases in China . Report on Cardiovascular Health and Diseases in China 2021: An updated summary. Chin Circ J. (2022) 2022:553–78. doi: 10.3969/j.issn.1000-3614.2022.06.001 [DOI] [Google Scholar]
- 3.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. (2001) 56:M146–57. doi: 10.1093/gerona/56.3.m146 [DOI] [PubMed] [Google Scholar]
- 4.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in older people. Lancet. (2013) 381:752–62. doi: 10.1016/s0140-6736(12)62167-9, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. (2019) 394:1365–75. doi: 10.1016/S0140-6736(19)31786-6 [DOI] [PubMed] [Google Scholar]
- 6.Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. (2012) 60:1487–92. doi: 10.1111/j.1532-5415.2012.04054.x, PMID: [DOI] [PubMed] [Google Scholar]
- 7.Gale CR, Mõttus R, Deary IJ, Cooper C, Sayer AA. Personality and risk of frailty: the English longitudinal study of ageing. Ann Behav Med. (2017) 51:128–36. doi: 10.1007/s12160-016-9833-5, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feng Z, Lugtenberg M, Franse C, Fang X, Hu S, Jin C, et al. Risk factors and protective factors associated with incident or increase of frailty among community-dwelling older adults: a systematic review of longitudinal studies. PLoS One. (2017) 12:e0178383. doi: 10.1371/journal.pone.0178383, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang SF, Yang RS, Nieh HM, Wen GM. Prevalence and risk factors of frailty phenotype among vulnerable solitary elderly individuals. Int J Nurs Pract. (2015) 21:321–7. doi: 10.1111/ijn.12280, PMID: [DOI] [PubMed] [Google Scholar]
- 10.Ng TP, Feng L, Nyunt MS, Larbi A, Yap KB. Frailty in older persons: multisystem risk factors and the frailty risk index (FRI). J Am Med Dir Assoc. (2014) 15:635–42. doi: 10.1016/j.jamda.2014.03.008, PMID: [DOI] [PubMed] [Google Scholar]
- 11.Santos-Eggimann B, Cuénoud P, Spagnoli J, Junod J. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. J Gerontol A Biol Sci Med Sci. (2009) 64:675–81. doi: 10.1093/gerona/glp012, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gobbens RJ, van Assen MA, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Determinants of frailty. J Am Med Dir Assoc. (2010) 11:356–64. doi: 10.1016/j.jamda.2009.11.008 [DOI] [PubMed] [Google Scholar]
- 13.Nagai K, Tamaki K, Kusunoki H, Wada Y, Tsuji S, Itoh M, et al. Physical frailty predicts the development of social frailty: a prospective cohort study. BMC Geriatr. (2020) 20:403. doi: 10.1186/s12877-020-01814-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ge L, Yap CW, Heng BH. Associations of social isolation, social participation, and loneliness with frailty in older adults in Singapore: a panel data analysis. BMC Geriatr. (2022) 22:26. doi: 10.1186/s12877-021-02745-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bunt S, Steverink N, Olthof J, van der Schans CP, Hobbelen JSM. Social frailty in older adults: a scoping review. Eur J Ageing. (2017) 14:323–34. doi: 10.1007/s10433-017-0414-7, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Makizako H, Tsutsumimoto K, Shimada H, Arai H. Social frailty among community-dwelling older adults: recommended assessments and implications. Ann Geriatr Med Res. (2018) 22:3–8. doi: 10.4235/agmr.2018.22.1.3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ding YY, Kuha J, Murphy M. Pathways from physical frailty to activity limitation in older people: identifying moderators and mediators in the English longitudinal study of ageing. Exp Gerontol. (2017) 98:169–76. doi: 10.1016/j.exger.2017.08.029, PMID: [DOI] [PubMed] [Google Scholar]
- 18.Hou Y, Xu C, Lu Q, Zhang Y, Cao Z, Li S, et al. Associations of frailty with cardiovascular disease and life expectancy: a prospective cohort study. Arch Gerontol Geriatr. (2022) 99:104598. doi: 10.1016/j.archger.2021.104598, PMID: [DOI] [PubMed] [Google Scholar]
- 19.Shen C, Rolls E, Cheng W, Kang J, Dong G, Xie C, et al. Associations of social isolation and loneliness with later dementia. Neurology. (2022) 99:e164–75. doi: 10.1212/wnl.0000000000200583, PMID: [DOI] [PubMed] [Google Scholar]
- 20.Makizako H, Shimada H, Tsutsumimoto K, Lee S, Doi T, Nakakubo S, et al. Social frailty in community-dwelling older adults as a risk factor for disability. J Am Med Dir Assoc. (2015) 16:1003.e7–1003.e11. doi: 10.1016/j.jamda.2015.08.023 [DOI] [PubMed] [Google Scholar]
- 21.Ma L, Sun F, Tang Z. Social frailty is associated with physical functioning, cognition, and depression, and predicts mortality. J Nutr Health Aging. (2018) 22:989–95. doi: 10.1007/s12603-018-1054-0, PMID: [DOI] [PubMed] [Google Scholar]
- 22.Tsutsumimoto K, Doi T, Makizako H, Hotta R, Nakakubo S, Makino K, et al. Association of Social Frailty with both Cognitive and Physical Deficits among Older People. J Am Med Dir Assoc. (2017) 18:603–7. doi: 10.1016/j.jamda.2017.02.004, PMID: [DOI] [PubMed] [Google Scholar]
- 23.Makizako H, Shimada H, Doi T, Tsutsumimoto K, Hotta R, Nakakubo S, et al. Social frailty leads to the development of physical frailty among physically non-frail adults: a four-year follow-up longitudinal cohort study. Int J Environ Res Public Health. (2018) 15:490. doi: 10.3390/ijerph15030490, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yamada M, Arai H. Social frailty predicts incident disability and mortality among community-dwelling Japanese older adults. J Am Med Dir Assoc. (2018) 19:1099–103. doi: 10.1016/j.jamda.2018.09.013, PMID: [DOI] [PubMed] [Google Scholar]
- 25.Teo N, Gao Q, Nyunt MSZ, Wee SL, Ng TP. Social frailty and functional disability: findings from the Singapore longitudinal ageing studies. J Am Med Dir Assoc. (2017) 18:637.e13–9. doi: 10.1016/j.jamda.2017.04.015, PMID: [DOI] [PubMed] [Google Scholar]
- 26.Makizako H, Kubozono T, Kiyama R, Takenaka T, Kuwahata S, Tabira T, et al. Associations of social frailty with loss of muscle mass and muscle weakness among community-dwelling older adults. Geriatr Gerontol Int. (2019) 19:76–80. doi: 10.1111/ggi.13571, PMID: [DOI] [PubMed] [Google Scholar]
- 27.Veronese N, Sigeirsdottir K, Eiriksdottir G, Marques EA, Chalhoub D, Phillips CL, et al. Frailty and risk of cardiovascular diseases in older persons: the age. Gene/Environ Suscept-Reykjavik Study Rejuvenation Res. (2017) 20:517–24. doi: 10.1089/rej.2016.1905, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kulmala J, Nykänen I, Hartikainen S. Frailty as a predictor of all-cause mortality in older men and women. Geriatr Gerontol Int. (2014) 14:899–905. doi: 10.1111/ggi.12190, PMID: [DOI] [PubMed] [Google Scholar]
- 29.Armstrong JJ, Andrew MK, Mitnitski A, Launer LJ, White LR, Rockwood K. Social vulnerability and survival across levels of frailty in the Honolulu-Asia aging study. Age Ageing. (2015) 44:709–12. doi: 10.1093/ageing/afv016, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Andrew MK, Mitnitski AB, Rockwood K. Social vulnerability, frailty and mortality in elderly people. PLoS One. (2008) 3:e2232. doi: 10.1371/journal.pone.0002232, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wallace LM, Theou O, Pena F, Rockwood K, Andrew MK. Social vulnerability as a predictor of mortality and disability: cross-country differences in the survey of health, aging, and retirement in Europe (SHARE). Aging Clin Exp Res. (2015) 27:365–72. doi: 10.1007/s40520-014-0271-6, PMID: [DOI] [PubMed] [Google Scholar]
- 32.Keshvani N, Pandey A. Beyond physical impairment: the role of social frailty in heart failure. J Am Heart Assoc. (2021) 10:e022187. doi: 10.1161/JAHA.121.022187, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jujo K, Kagiyama N, Saito K, Kamiya K, Saito H, Ogasahara Y, et al. Impact of social frailty in hospitalized elderly patients with heart failure: a FRAGILE-HF registry subanalysis. J Am Heart Assoc. (2021) 10:e019954. doi: 10.1161/JAHA.120.019954, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ko Y, Lee K. Social frailty and health-related quality of life in community-dwelling older adults. Int J Environ Res Public Health. (2022) 19:5659. doi: 10.3390/ijerph19095659, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Uchmanowicz I, Pasieczna AH, Wójta-Kempa M, Gobbens RJJ, Młynarska A, Faulkner KM, et al. Physical, psychological and social frailty are predictive of heart failure: a cross-sectional study. J Clin Med. (2022) 11:565. doi: 10.3390/jcm11030565, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Inoue T, Maeda K, Satake S, Matsui Y, Arai H. Osteosarcopenia, the co-existence of osteoporosis and sarcopenia, is associated with social frailty in older adults. Aging Clin Exp Res. (2022) 34:535–43. doi: 10.1007/s40520-021-01968-y, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mone P, Pansini A, Frullone S, de Donato A, Buonincontri V, De Blasiis P, et al. Physical decline and cognitive impairment in frail hypertensive elders during COVID-19. Eur J Intern Med. (2022) 99:89–92. doi: 10.1016/j.ejim.2022.03.012, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang CH, Okada K, Matsushita E, Uno C, Satake S, Arakawa Martins B, et al. Sex-specific association between social frailty and diet quality, diet quantity, and nutrition in community-dwelling elderly. Nutrients. (2020) 12:2845. doi: 10.3390/nu12092845, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mone P, De Gennaro S, Frullone S, Marro A, Santulli G. Hyperglycemia drives the transition from pre-frailty to frailty: the Monteforte study. Eur J Intern Med. (2023) 111:135–7. doi: 10.1016/j.ejim.2023.01.006, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boreskie KF, Rose AV, Hay JL, Kehler DS, Costa EC, Moffatt TL, et al. Frailty status and cardiovascular disease risk profile in middle-aged and older females. Exp Gerontol. (2020) 140:111061. doi: 10.1016/j.exger.2020.111061, PMID: [DOI] [PubMed] [Google Scholar]
- 41.Kleipool EE, Hoogendijk EO, Trappenburg MC, Handoko ML, Huisman M, Peters MJ, et al. Frailty in older adults with cardiovascular disease: cause, effect or both? Aging Dis. (2018) 9:489–97. doi: 10.14336/ad.2017.1125, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bouillon K, Batty GD, Hamer M, Sabia S, Shipley MJ, Britton A, et al. Cardiovascular disease risk scores in identifying future frailty: the Whitehall II prospective cohort study. Heart. (2013) 99:737–42. doi: 10.1136/heartjnl-2012-302922, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zeng X, Jia N, Meng L, Shi J, Li Y, Hu X, et al. A study on the prevalence and related factors of frailty and pre-frailty in the older population with diabetes in China: a national cross-sectional study. Front Public Health. (2022) 10:996190. doi: 10.3389/fpubh.2022.996190, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yoo M, Kim S, Kim BS, Yoo J, Lee S, Jang HC, et al. Moderate hearing loss is related with social frailty in a community-dwelling older adults: the Korean frailty and aging cohort study (KFACS). Arch Gerontol Geriatr. (2019) 83:126–30. doi: 10.1016/j.archger.2019.04.004, PMID: [DOI] [PubMed] [Google Scholar]
- 45.Gobbens RJ, van Assen MA. The prediction of quality of life by physical, psychological and social components of frailty in community-dwelling older people. Qual Life Res. (2014) 23:2289–300. doi: 10.1007/s11136-014-0672-1, PMID: [DOI] [PubMed] [Google Scholar]
- 46.Gobbens RJJ, van Assen M. Associations between multidimensional frailty and quality of life among Dutch older people. Arch Gerontol Geriatr. (2017) 73:69–76. doi: 10.1016/j.archger.2017.07.007, PMID: [DOI] [PubMed] [Google Scholar]
- 47.Takabayashi K, Ikuta A, Okazaki Y, Ogami M, Iwatsu K, Matsumura K, et al. Clinical characteristics and social frailty of super-elderly patients with heart failure—the Kitakawachi clinical background and outcome of heart failure registry. Circ J. (2016) 81:69–76. doi: 10.1253/circj.CJ-16-0914, PMID: [DOI] [PubMed] [Google Scholar]
- 48.Garre-Olmo J, Calvó-Perxas L, López-Pousa S, de Gracia BM, Vilalta-Franch J. Prevalence of frailty phenotypes and risk of mortality in a community-dwelling elderly cohort. Age Ageing. (2013) 42:46–51. doi: 10.1093/ageing/afs047, PMID: [DOI] [PubMed] [Google Scholar]
- 49.Ko H, Jung S. Association of Social Frailty with physical health, cognitive function, psychological health, and life satisfaction in community-dwelling older Koreans. Int J Environ Res Public Health. (2021) 18:818. doi: 10.3390/ijerph18020818, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tsutsumimoto K, Doi T, Makizako H, Hotta R, Nakakubo S, Kim M, et al. Social frailty has a stronger impact on the onset of depressive symptoms than physical frailty or cognitive impairment: a 4-year follow-up longitudinal cohort study. J Am Med Dir Assoc. (2018) 19:504–10. doi: 10.1016/j.jamda.2018.02.008 [DOI] [PubMed] [Google Scholar]
- 51.Bessa B, Ribeiro O, Coelho T. Assessing the social dimension of frailty in old age: a systematic review. Arch Gerontol Geriatr. (2018) 78:101–13. doi: 10.1016/j.archger.2018.06.005, PMID: [DOI] [PubMed] [Google Scholar]
- 52.Pek K, Chew J, Lim JP, Yew S, Tan CN, Yeo A, et al. Social frailty is independently associated with mood, nutrition, physical performance, and physical activity: insights from a theory-guided approach. Int J Environ Res Public Health. (2020) 17:4239. doi: 10.3390/ijerph17124239, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Smith BJ, Lim MH. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res Pract. (2020) 30:3022008. doi: 10.17061/phrp3022008, PMID: [DOI] [PubMed] [Google Scholar]
- 54.Pansini A, Lombardi A, Morgante M, Frullone S, Marro A, Rizzo M, et al. Hyperglycemia and physical impairment in frail hypertensive older adults. Front Endocrinol. (2022) 13:831556. doi: 10.3389/fendo.2022.831556, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jang AR, Won CW, Sagong H, Bae E, Park H, Yoon JY. Social factors predicting improvement of frailty in community-dwelling older adults: Korean frailty and aging cohort study. Geriatr Gerontol Int. (2021) 21:465–71. doi: 10.1111/ggi.14160, PMID: [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.