Summary
Background
The phenotype of combined heavy alcohol consumption and obesity has the potential to pose as a considerable health burden in the U.S. No studies using nationally representative data in the U.S. have reported their secular joint prevalence trends. We estimated the prevalence and examined the joint trends of heavy alcohol use and obesity over time among adult U.S. men and women in different age groups and according to race/ethnicity.
Methods
Using data from 10 cycles of the U.S. National Health and Nutrition Examination Survey (NHANES) from 1999 to 2020, we examined secular trends in the combined phenotype of heavy drinking and obesity overall and by age-group, sex, and race/ethnicity. The main outcome measures were prevalence of heavy alcohol consumption (>14 drinks/week in men and >7 drinks/week in women) and obesity (BMI ≥30).
Findings
In 45,292 adults (22,684 men, mean age 49.26 years; and 22,608 women, mean age 49.86), the overall weighted prevalence of combined heavy alcohol drinking and obesity increased from 1.8% (95% CI: 1.2%, 3.1%) in 1999–2000 to 3.1% (95% CI: 2.7%, 3.7%) in 2017–2020 representing an increase of 72% over time. In the joinpoint regression, the combined phenotype of heavy alcohol consumption and obesity increased by 3.25% (95% CI: 1.67%, 4.85%) per year overall from 1999 to 2017. An increasing trend of 9.94% (95% CI: 2.37%, 18.06%) per year was observed among adults aged between 40 and 59 years from 2007 onwards. Prevalence of heavy alcohol consumption in obesity increased at a faster rate among women (APC, 3.96%; 95% CI: 2.14%, 5.82%) than men (APC, 2.47%; 95% CI: 0.63%, 4.35%), and increased among non-Hispanic Whites (APC, 4.12%; 95% CI: 1.50%, 6.82%) and non-Hispanic Blacks (APC, 2.78%; 95% CI: 0.47%, 5.14%), but not Hispanics.
Interpretation
The prevalence of combined heavy alcohol consumption and obesity increased overall in the U.S., but the rate of increase differed by age, sex, and race/ethnic groups. Given their independent and potential synergistic effects on premature mortality, public health policies on alcohol consumption need to reflect the background obesity epidemic.
Funding
Cancer Prevention & Research Institute of Texas (CPRIT) for the Systems Epidemiology of Cancer Training (SECT) Program (RP210037; PI: A. Thrift).
Keywords: Burden, Trends, Obesity, Overweight, Alcohol consumption, Joinpoint regression
Research in context.
Evidence before this study
Prior population-based studies have reported increasing prevalence of obesity as well as on the alcohol consumption trends among the general U.S. adult population. These studies have used several nationally representative databases such as National Health and Nutrition Examination Survey, National Health Interview Survey, National Longitudinal Study of Adolescent to Adult Health, and Global Burden of Disease Study. However, the combined prevalence trends of alcohol consumption and obesity in the U.S. general population has not been reported previously.
Added value of this study
In this large nationally representative population-based study of 45,292 men and women, the overall prevalence of combined heavy alcohol consumption and obesity in the U.S. increased by over 70% from 1999 to 2020. The prevalence of combined heavy alcohol consumption and obesity increased by 3–4% annually in non-Hispanic Whites and non-Hispanic Blacks but remained stable among the Hispanic adult population. Over the last two decades, the prevalence of heavy drinking has increased in obese U.S. population, and given the potential for synergistic effects on premature deaths, guidelines for safe drinking thresholds need to take into account the background prevalence of obesity.
Implications of all the available evidence
The hypothesis that alcohol in moderation confers health benefits has implications for estimations of national level burden of ill-effects of obesity. The longtime debate on the consumption of low-moderate alcohol use on health outcomes have been narrowed in through recent studies by recommending that the level of alcohol consumption that minimizes health loss is ‘zero standard drinks’ per day. The apparent contradiction in findings across existing studies highlights the need for continuous revisions of public health guidelines for alcohol consumption reduction and obesity prevention based on evolving scientific evidence.
Introduction
Worldwide, an estimated 5.3% of all deaths (3 million deaths every year) and 5.1% of global disability-adjusted life-years are attributable to excessive alcohol use.1 Each year in the United States between 2015 and 2019, excessive alcohol use led to more than 140,000 deaths and 3.6 million years of potential life lost, shortening the lives of those who died by an average of 26 years.2 According to recent reports by the World Obesity Federation, it is projected that about one billion people will be living with obesity by 2030 worldwide, including 1 in 5 women and 1 in 7 men.3,4 About 65% of adults in the U.S. are overweight or obese, and majority keep gaining weight throughout adulthood.5,6 In 2019, an estimated 5.02 million deaths and 160 million disability-adjusted life-years around the world were attributable to high body mass index (BMI > 25).7
As such, major public health institutions have developed and implemented policies aimed at reducing harmful alcohol use and controlling obesity. Alcohol consumption guidelines are instituted at drinking risk thresholds associated with the lowest risk of mortality. Nonetheless, guidelines and threshold for ‘safe drinking’ vary substantially across the globe and are frequently revised. In the U.S., to reduce the risk of alcohol-related harms, recent guidelines recommend that adults of legal drinking age can choose not to drink, or to drink in moderation by limiting intake to 2 drinks or less in a day for men and 1 drink or less in a day for women.8 To reverse the obesity epidemic, the focus is on supporting healthy eating and active living.
In addition to their independent effects, joint exposure to excess alcohol consumption and obesity may act synergistically to confer especially high risk for adverse health outcomes, including chronic diseases, cancer, and premature mortality.5,9 In a recent study from the United Kingdom, being overweight or obese amplified the harmful effects of alcohol on risks of liver disease incidence and mortality.10 The study reported that the alcohol consumption above the guidelines for individuals who were overweight or obese conferred 1.5-fold–2-fold higher risk of liver disease incidence and mortality compared to healthy weight participants. Likewise, in a recent study from the U.S., there was also evidence for supra-additive interaction between obesity and heavy drinking on liver-related mortality.11 These studies therefore allude that ‘safe drinking’ levels may need to be revisited in the context of growing population that are overweight or obese.
Thus, the phenotype of heavy alcohol consumption and high BMI has the potential to pose as a considerable health burden. However, the extent of the problem overall and in sociodemographic sub-groups of the U.S. population have not been previously reported. Here, we used a nationally representative dataset from National Health and Nutrition Examination Survey (NHANES), to estimate prevalence and analyse joint trends of alcohol use and BMI over time. We examined these trends overall and within important subgroups of the U.S. population.
Methods
Study population
We used data from 10 cycles of NHANES (1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, 2009–2010, 2011–2012, 2013–2014, 2015–2016, and 2017–2020). NHANES is a nationally representative sample of the non-institutionalized U.S. population. Individuals who are residents in nursing homes, members of the armed forces, those who are institutionalized, and U.S. citizens living outside the U.S. were excluded. NHANES combines in-person interviews that capture data through multiple study surveys and physical examination via mobile examination centers (MEC). Ethics approval for this survey was provided by National Center for Health Statistics Research Ethics Review Board and all adult participants in the surveys provided written consent (https://www.cdc.gov/nchs/nhanes/irba98.htm).
Demographic data
We obtained data on age in years (categorized as 18–39, 40–59, and ≥60 years), sex, and race/ethnicity (non-Hispanic White [NHW], non-Hispanic Black [NHB], and Hispanics). These categories follow the analytic guidelines as laid down for each of the NHANES cycles.12 We combined NHANES demographic data for each of the 10 cycles for variables on age, sex and race/ethnicity. We limited our analyses on the most detailed public use demographic dataset on race/ethnicity that did not include the restricted data files on American Indian/Alaska Native (AIAN).13 Since NHANES recorded the less-detailed measure on non-Hispanic Asians and collapsed it into ‘Other Race’ category that also included non-specific multi-racial groups,14 we excluded this group from the current analyses due to small number of participants.
Alcohol consumption
As part of MEC, for each survey cycle, data on lifetime and current alcohol use is collected (i.e., alcohol use over the past 12 months) for respondents aged ≥20 (from 1999 to 2010) and ≥18 (from 2011 to 2020) years using the Alcohol Use Questionnaire.13 In the NHANES Questionnaire dataset with information on both drinkers and non-drinkers, pregnant women were excluded from analysis as they did not complete the alcohol survey. Among ever drinkers, we calculated their average drinks per week from total drinks per year divided by total drinking days per year. Drinking status categories used sex-specific thresholds according to definition of alcohol use by the National Institute on Alcohol and Alcoholism: non-drinkers, low-moderate drinkers (≤14 drinks/week for men and ≤7 drinks/week for women), and heavy drinkers (>14 drinks/week for men and >7 drinks/week for women).15
Obesity
In all the survey cycles, anthropometric measurements of weight and height were measured in MEC using standardised techniques and equipment by trained professionals.13 We retrieved this information from the NHANES Examination dataset. For participants in this survey aged ≥18 years, weight categories were defined according to clinical guidelines for Body Mass Index (BMI): healthy weight (18.5–24.9), overweight (25–29.9), and obese (≥30).16
Statistical analyses
We examined (1) secular trends in prevalence of alcohol use (non-drinkers, low-moderate drinkers, and heavy drinkers) according to BMI category (healthy weight, overweight, and obese) overall and by age-group, sex, and race/ethnicity, and (2) secular trends in the combined phenotype of heavy drinking and obesity. Complex survey sample design was incorporated in the standard error estimates and all statistical testing. NHANES datasets contain the design variables such as stratification and cluster variable information that is necessary for conducting complex sample data analysis. Each case was recognised by a unique case sequence identification number that was used to match information for cases from Demographic, Questionnaire, and Examination datasets wherein missing data was also identified (See Fig. 1). We used sample weights provided by National Center for Health Statistics to account for the survey design and oversampling in populations during the survey cycles.17 For all survey cycles, sampling weights accounted for unequal probabilities of selection (resulting from the sample design and planned oversampling of certain subgroups) and were adjusted for nonresponse. The 2-year sample weights were used for all NHANES survey cycles except for NHANES 2017–2020 pre-pandemic data where the special sample weights were used. The weighted analyses were carried out using SPSS Complex Sample Analysis (IBM SPSS 2022 Version 28.0, Armonk, NY). We also conducted a sensitivity analysis whereby we examined secular trends in the prevalence of combined heavy alcohol consumption use and obesity excluding the 2017–2020 survey cycle.
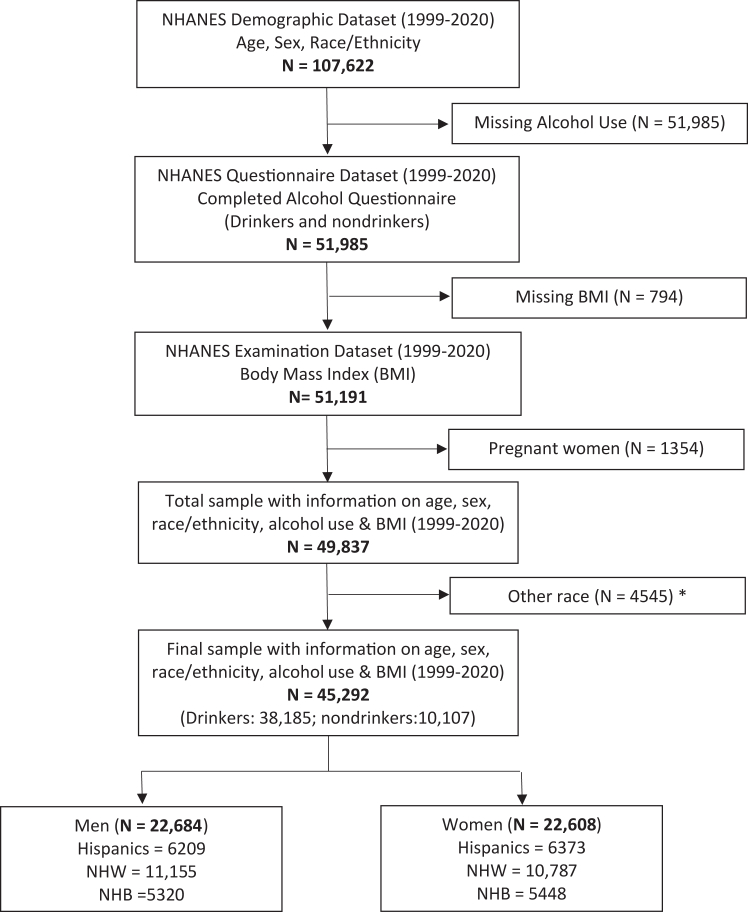
Fig. 1.
Consolidated Standards of Reporting (CONSORT) diagram describing the flow of participants selected for inclusion in the study from National Health and Nutrition Examination Survey (1999–2020). Three datasets (Demographic, Questionnaire and Examination) for each of the 10 survey cycles were matched and combined to arrive at the final sample of 45,292 with complete information on age, sex, race/ethnicity, alcohol use (drinkers and nondrinkers), and body mass index (BMI). Pregnant women and those missing BMI were excluded. Other race categories such as non-Hispanic Asians including non-Hispanic multi racial groups and American Indians and Native Alaskans were also excluded.
We used joinpoint regression to analyse trends over time and to detect, if present, joinpoints (i.e., inflection points) when the trend significantly changed. This approach first identified by Kim et al., is commonly used when temporal trend of a given quantity such as prevalence is of interest.18, 19, 20 By using prevalence as input, this method identifies the start and end year when a trend change is produced, and then it calculates the annual percentage change (APC) in prevalence between trend-change points. It also estimates the average annual percentage change (AAPC) in the whole period studied.
To estimate APC in the prevalence estimates, we fit a least squares regression to the natural logarithm of the prevalence. The regression line required a maximum of two joinpoints and a minimum of four observations between those joinpoints.18 For each joinpoints combination, we used Monte Carlo permutation tests to examine trends, and the best fitted trend line for the data was selected.21 We used Joinpoint Trend analysis Software (Version 4.9, National Cancer Institute, Bethesda, MD) to estimate APC values for each linear segment along with the values of AAPC between 1999 and 2020. For AAPC computation, a weighted average of the slope coefficients of the underlying joinpoint regression line was used with the weights equal to the length of each segment over the interval.19 A parallelism test was used to examine whether the slopes of the change in trend between groups were similar (or not) in direction. A statistically significant p-value on this test indicates that the two trends in terms of APCs compared were statistically significantly different from each other.22 All tests were two-sided with a statistical significance level of α = 0.05.
Role of the funding source
This work was funded (in part) by a Research Training Award from the Cancer Prevention & Research Institute of Texas (CPRIT) for the Systems Epidemiology of Cancer Training (SECT) Program (RP210037; PI: A. Thrift). The funders have no role in the study design; data collection, analysis, and interpretation; manuscript preparation or the decision to submit the manuscript.
Results
We identified 45,292 (22,684 men, mean age 49.26 years; and 22,608 women, mean age 49.86 years) adults in the NHANES combined data from 1999 to 2020 that had complete information on demographic, alcohol use (drinkers and non-drinkers) and BMI variables (Fig. 1). The unweighted sample sizes of survey respondents by race/ethnicity, age group and sex are shown in Table 1 (as well as in Supplementary Table S1).
Table 1.
Sample sizes in NHANES survey cycles according to race/ethnicity and age groups in men and women.
| Race/Ethnicity |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Non-Hispanic Whites |
Non-Hispanic Blacks |
Hispanics |
||||||||
| 18–39 | 40–59 | ≥60 | 18–39 | 40–59 | ≥60 | 18–39 | 40–59 | ≥60 | ||
| All groups | N = 45,292 | (n = 6479) | (n = 6660) | (n = 8803) | (n = 3638) | (n = 3640) | (n = 3490) | (n = 4736) | (n = 4068) | (n = 3778) |
| 1999–2000 | 3762 | 496 | 497 | 770 | 235 | 244 | 251 | 429 | 398 | 442 |
| 2001–2002 | 4036 | 607 | 758 | 848 | 274 | 282 | 236 | 419 | 344 | 268 |
| 2003–2004 | 3880 | 605 | 625 | 964 | 286 | 273 | 223 | 299 | 243 | 362 |
| 2005–2006 | 3844 | 572 | 673 | 810 | 310 | 328 | 271 | 390 | 272 | 218 |
| 2007–2008 | 4921 | 665 | 741 | 1035 | 341 | 334 | 367 | 537 | 501 | 400 |
| 2009–2010 | 4972 | 751 | 818 | 992 | 294 | 333 | 290 | 524 | 550 | 420 |
| 2011–2012 | 4089 | 636 | 528 | 651 | 454 | 424 | 425 | 394 | 291 | 286 |
| 2013–2014 | 4578 | 770 | 707 | 808 | 390 | 335 | 346 | 485 | 407 | 330 |
| 2015–2016 | 4360 | 528 | 500 | 675 | 379 | 380 | 322 | 572 | 471 | 533 |
| 2017–2020 | 6850 | 849 | 813 | 1250 | 675 | 707 | 759 | 687 | 591 | 519 |
| Men | N = 22,684 | (n = 3366) | (n = 3352) | (n = 4437) | (n = 1827) | (n = 1726) | (n = 1767) | (n = 2452) | (n = 1951) | (n = 1806) |
| 1999–2000 | 1887 | 267 | 258 | 398 | 116 | 117 | 115 | 220 | 176 | 220 |
| 2001–2002 | 2068 | 300 | 397 | 419 | 138 | 155 | 119 | 236 | 182 | 122 |
| 2003–2004 | 1971 | 318 | 313 | 482 | 156 | 130 | 102 | 163 | 126 | 181 |
| 2005–2006 | 2008 | 310 | 349 | 423 | 165 | 151 | 143 | 216 | 140 | 111 |
| 2007–2008 | 2443 | 354 | 365 | 532 | 175 | 152 | 180 | 258 | 253 | 174 |
| 2009–2010 | 2480 | 369 | 407 | 499 | 144 | 178 | 147 | 274 | 274 | 188 |
| 2011–2012 | 2065 | 349 | 274 | 317 | 242 | 180 | 209 | 210 | 142 | 142 |
| 2013–2014 | 2230 | 417 | 332 | 365 | 196 | 159 | 184 | 224 | 195 | 158 |
| 2015–2016 | 2133 | 271 | 251 | 353 | 187 | 173 | 168 | 290 | 195 | 245 |
| 2017–2020 | 3399 | 411 | 406 | 649 | 308 | 331 | 400 | 361 | 268 | 265 |
| Women | N = 22,608 | (n = 3113) | (n = 3308) | (n = 4366) | (n = 1811) | (n = 1914) | (n = 1723) | (n = 2284) | (n = 2117) | (n = 1972) |
| 1999–2000 | 1875 | 229 | 239 | 372 | 119 | 127 | 136 | 209 | 222 | 222 |
| 2001–2002 | 1968 | 307 | 361 | 429 | 136 | 127 | 117 | 183 | 162 | 146 |
| 2003–2004 | 1909 | 287 | 312 | 482 | 130 | 143 | 121 | 136 | 117 | 181 |
| 2005–2006 | 1836 | 262 | 324 | 387 | 145 | 177 | 128 | 174 | 132 | 107 |
| 2007–2008 | 2478 | 311 | 376 | 503 | 166 | 182 | 187 | 279 | 248 | 226 |
| 2009–2010 | 2492 | 382 | 411 | 493 | 150 | 155 | 143 | 250 | 276 | 232 |
| 2011–2012 | 2024 | 287 | 254 | 334 | 212 | 244 | 216 | 184 | 149 | 144 |
| 2013–2014 | 2348 | 353 | 375 | 443 | 194 | 176 | 162 | 261 | 212 | 172 |
| 2015–2016 | 2227 | 257 | 249 | 322 | 192 | 207 | 154 | 282 | 276 | 288 |
| 2017–2020 | 3451 | 438 | 407 | 601 | 367 | 376 | 359 | 326 | 323 | 254 |
Heavy drinking prevalence and obesity in 1999–2020
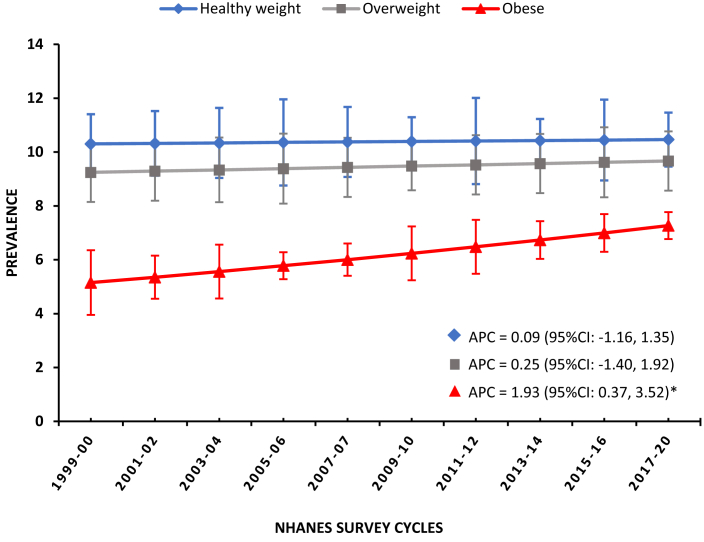
Weighted estimates of prevalence of alcohol use in BMI categories are shown in Table 2. The estimated prevalence of non-drinkers among healthy weight individuals remained stable from 1999–2000 to 2017–2020 (21.2% [n = 347] to 22.9% [n = 612]) but decreased among overweight and obese adults. Among obese individuals, the proportion who were non-drinkers decreased significantly from 37.1% (95% CI: 32.7%, 41.7%; n = 543) in 1999–2000 to 23.4% (95% CI: 21.3%, 25.8%; n = 1011) in 2017–2020 as indicated by non-overlapping confidence intervals. Concurrently, the prevalence of heavy alcohol use among obese adults increased albeit with overlapping confidence intervals from 5.9% (95% CI: 4.0%, 8.7%; n = 66) in 1999–2000 to 7.5% (95% CI: 6.5%, 8.6%; n = 220) in 2017–2020. In the joinpoint regression, the overall prevalence of heavy alcohol drinkers increased by almost 2% per year (APC, 1.93%; 95% CI: 0.37%, 3.52%) between 1999 and 2017 driven by obese adults (Fig. 2 and Table 3). Conversely, rates of heavy alcohol use remained stable among healthy weight (APC, 0.09%; p = 0.88) and overweight (APC, 0.25%; p = 0.74) adults. The trends of heavy alcohol consumption in different BMI groups varied by age group, sex and race/ethnicity. When examined separately, heavy alcohol use increased only in obese adults aged 40–59 years (APC, 7.21%; 95% CI: 1.62%, 13.11%) between 2005 and 2017, obese women (APC, 2.62%; 95% CI: 0.46%, 4.82%) and obese NHWs (APC, 1.93%; 95% CI: 0.36%, 3.53%) between 1999 and 2017 (Table 3). The only sub-group with significant linear declining prevalence of heavy alcohol use was observed among healthy weight Hispanics, where prevalence decreased by over 3% per year between 1999 and 2017 (APC, −3.20%; 95% CI: −5.61%, −0.73%).
Table 2.
Overall weighted prevalence of alcohol use categories among adults stratified by BMI status: NHANES 1999–2020.
| BMI status | Year | Nondrinkers |
Low-moderate drinkers |
Heavy drinkers |
|||
|---|---|---|---|---|---|---|---|
| % | (95% CI) | % | (95% CI) | % | (95% CI) | ||
| Healthy weight | |||||||
| 1999–2000 | 21.2 | (18.6, 24.1) | 67.8 | (65.2, 70.3) | 11.0 | (9.0, 13.3) | |
| 2001–2002 | 24.6 | (18.2, 32.4) | 66.3 | (59.4, 72.6) | 9.0 | (6.9, 11.7) | |
| 2003–2004 | 25.5 | (20.2, 31.7) | 65.4 | (60.2, 70.3) | 9.1 | (6.8, 11.9) | |
| 2005–2006 | 25.6 | (21.5, 30.1) | 62.0 | (58.3, 65.6) | 12.5 | (9.6, 16.0) | |
| 2007–2008 | 25.0 | (21.2, 29.2) | 64.7 | (61.4, 67.9) | 10.3 | (8.0, 13.1) | |
| 2009–2010 | 22.4 | (19.7, 25.4) | 67.4 | (64.4, 70.3) | 10.2 | (8.4, 12.2) | |
| 2011–2012 | 21.6 | (17.7, 26.0) | 66.9 | (61.9, 71.6) | 11.5 | (8.6, 15.1) | |
| 2013–2014 | 23.2 | (18.3, 28.9) | 67.1 | (62.0, 71.9) | 9.7 | (8.2, 11.5) | |
| 2015–2016 | 23.6 | (20.1, 27.5) | 67.0 | (61.9, 71.7) | 9.4 | (6.8, 12.8) | |
| 2017–2020 | 22.9 | (20.1, 26.0) | 65.9 | (61.9, 69.8) | 11.2 | (9.3, 13.4) | |
| Overweight | |||||||
| 1999–2000 | 26.9 | (23.8, 30.2) | 63.5 | (60.1, 66.8) | 9.6 | (7.6, 12.1) | |
| 2001–2002 | 27.5 | (22.2, 33.6) | 63.0 | (56.9, 68.8) | 9.4 | (7.6, 11.7) | |
| 2003–2004 | 30.4 | (25.8, 35.5) | 62.0 | (57.9, 66.0) | 7.6 | (5.5, 10.3) | |
| 2005–2006 | 26.5 | (22.2, 31.3) | 62.2 | (57.4, 66.7) | 11.3 | (9.0, 14.2) | |
| 2007–2008 | 28.2 | (23.5, 33.5) | 63.6 | (58.5, 68.4) | 8.2 | (6.4, 10.3) | |
| 2009–2010 | 23.4 | (21.5, 25.4) | 67.1 | (64.5, 69.6) | 9.5 | (7.9, 11.5) | |
| 2011–2012 | 23.7 | (20.2, 27.7) | 66.3 | (62.3, 70.1) | 10.0 | (8.1, 12.2) | |
| 2013–2014 | 27.0 | (21.6, 33.1) | 64.8 | (59.6, 69.7) | 8.2 | (6.4, 10.5) | |
| 2015–2016 | 26.6 | (22.5, 31.2) | 65.7 | (60.7, 70.3) | 7.7 | (5.5, 10.7) | |
| 2017–2020 | 23.3 | (21.6, 25.1) | 65.9 | (63.3, 68.4) | 10.8 | (9.0, 12.9) | |
| Obese | |||||||
| 1999–2000 | 37.1 | (32.7, 41.7) | 57.0 | (52.1, 61.8) | 5.9 | (4.0, 8.7) | |
| 2001–2002 | 36.8 | (28.3, 46.2) | 57.0 | (48.5, 65.1) | 6.2 | (4.8, 7.9) | |
| 2003–2004 | 35.5 | (29.5, 42.0) | 59.0 | (53.1, 64.7) | 5.5 | (3.8, 7.8) | |
| 2005–2006 | 31.6 | (28.1, 35.3) | 63.3 | (59.5, 67.0) | 5.1 | (4.2, 6.2) | |
| 2007–2008 | 34.9 | (30.2, 40.0) | 60.1 | (55.4, 64.6) | 5.0 | (3.9, 6.4) | |
| 2009–2010 | 30.1 | (27.3, 33.0) | 62.7 | (60.1, 65.2) | 7.2 | (5.5, 9.4) | |
| 2011–2012 | 30.4 | (27.2, 33.7) | 61.9 | (58.9, 64.9) | 7.7 | (6.0, 9.8) | |
| 2013–2014 | 30.5 | (25.4, 36.2) | 63.2 | (57.9, 68.1) | 6.3 | (5.1, 7.8) | |
| 2015–2016 | 28.9 | (26.8, 31.0) | 64.5 | (62.1, 66.9) | 6.6 | (5.3, 8.2) | |
| 2017–2020 | 23.4 | (21.3, 25.8) | 69.1 | (66.4, 71.6) | 7.5 | (6.5, 8.6) | |
Fig. 2.
Weighted prevalence of heavy drinking with annual percentage change (APC) from 1999 to 2020 stratified by healthy weight, overweight and obese U.S. population. ∗Statistically significant increasing trend at α = 0.05.
Table 3.
Weighted prevalence of heavy drinking and annual percentage change (APC) overall and by age group, sex, and race/ethnicity: NHANES 1999–2020.
| Population | Cases | Weighted prevalence | Joinpoint segmenta |
APC (95% CI) | p | |
|---|---|---|---|---|---|---|
| Year start | Year end | |||||
| Overall | ||||||
| Healthy weight | 1202 | 10.4 (9.6, 11.2) | 1999 | 2017 | 0.09 (−1.16, 1.35) | 0.88 |
| Overweight | 1232 | 9.2 (8.6, 9.9) | 1999 | 2017 | 0.25 (−1.40, 1.92) | 0.74 |
| Obese | 1039 | 6.4 (5.9, 6.9) | 1999 | 2017 | 1.93 (0.37, 3.52) | 0.02 |
| Age-groups | ||||||
| 18–39 | ||||||
| Healthy weight | 497 | 9.5 (8.5, 10.7) | 1999 | 2017 | −1.04 (−2.79, 0.74) | 0.21 |
| Overweight | 419 | 10.1 (9.1, 11.2) | 1999 | 2017 | −1.11 (−2.78, 0.58) | 0.17 |
| Obese | 374 | 7.1 (6.3, 8.0) | 1999 | 2017 | 0.14 (−3.61, 4.03) | 0.94 |
| 40–59 | ||||||
| Healthy weight | 425 | 13.4 (11.8, 15.3) | 1999 | 2017 | 1.06 (−0.91, 3.06) | 0.25 |
| Overweight | 489 | 10.3 (9.2, 11.5) | 1999 | 2017 | 0.81 (−1.03, 2.69) | 0.34 |
| Obeseb | 422 | 7.0 (6.1, 8.0) | 1999 | 2005 | −10.52 (−28.23, 11.57) | 0.25 |
| 2005 | 2017 | 7.21 (1.62, 13.11) | 0.02 | |||
| ≥60 | ||||||
| Healthy weight | 280 | 7.7 (6.6, 9.0) | 1999 | 2017 | 4.06 (−0.04, 8.32) | 0.05 |
| Overweight | 324 | 6.6 (5.7, 7.7) | 1999 | 2017 | 2.02 (−1.62, 5.80) | 0.24 |
| Obese | 243 | 4.6 (3.7, 5.6) | 1999 | 2017 | 2.69 (−0.53, 6.02) | 0.09 |
| Sex | ||||||
| Men | ||||||
| Healthy weight | 673 | 11.6 (10.6, 12.7) | 1999 | 2017 | −0.47 (−2.04, 1.12) | 0.51 |
| Overweight | 835 | 10.5 (9.7, 11.5) | 1999 | 2017 | −0.39 (−2.96, 2.26) | 0.74 |
| Obese | 639 | 8.3 (7.5, 9.1) | 1999 | 2017 | 0.59 (−1.18, 2.39) | 0.46 |
| Women | ||||||
| Healthy weight | 529 | 9.4 (8.4, 10.6) | 1999 | 2017 | 0.85 (−0.44, 2.15) | 0.17 |
| Overweight | 397 | 7.5 (6.5, 8.5) | 1999 | 2017 | 1.82 (−0.80, 4.51) | 0.15 |
| Obese | 400 | 4.7 (4.1, 5.4) | 1999 | 2017 | 2.62 (0.46, 4.82) | 0.02 |
| Race/Ethnicity | ||||||
| NHWc | ||||||
| Healthy weight | 699 | 11.8 (10.8, 13.0) | 1999 | 2017 | 0.09 (−1.16, 1.35) | 0.88 |
| Overweight | 694 | 10.4 (9.6, 11.4) | 1999 | 2017 | 0.25 (−1.40, 1.92) | 0.74 |
| Obese | 460 | 6.7 (6.1, 7.4) | 1999 | 2017 | 1.93 (0.36, 3.53) | 0.02 |
| NHBd | ||||||
| Healthy weight | 250 | 9.6 (8.5, 10.8) | 1999 | 2017 | 0.82 (−2.86, 4.63) | 0.63 |
| Overweight | 211 | 7.2 (6.2, 8.3) | 1999 | 2017 | 1.34 (−2.30, 5.11) | 0.43 |
| Obese | 271 | 5.7 (4.9, 6.5) | 1999 | 2017 | 2.20 (−0.12, 4.56) | 0.06 |
| Hispanics | ||||||
| Healthy weight | 163 | 6.2 (5.2, 7.3) | 1999 | 2017 | −3.20 (−5.61, −0.73) | 0.02 |
| Overweight | 263 | 6.1 (5.3, 7.0) | 1999 | 2017 | 1.50 (−2.51, 5.69) | 0.42 |
| Obese | 257 | 5.7 (5.0, 6.5) | 1999 | 2017 | −0.08 (−4.47, 4.52) | 0.97 |
Survey periods are represented by first year e.g., Year-start 1999 (1999–2000 Survey Cycle) and Year-end 2017 (2017–2020 Survey Cycle).
Average annual percentage change (AAPC) for obese heavy drinkers aged 40–59-year-old: 0.55% (95% CI: −0.25%, 1.35%).
Non-Hispanic White.
Non-Hispanic Black.
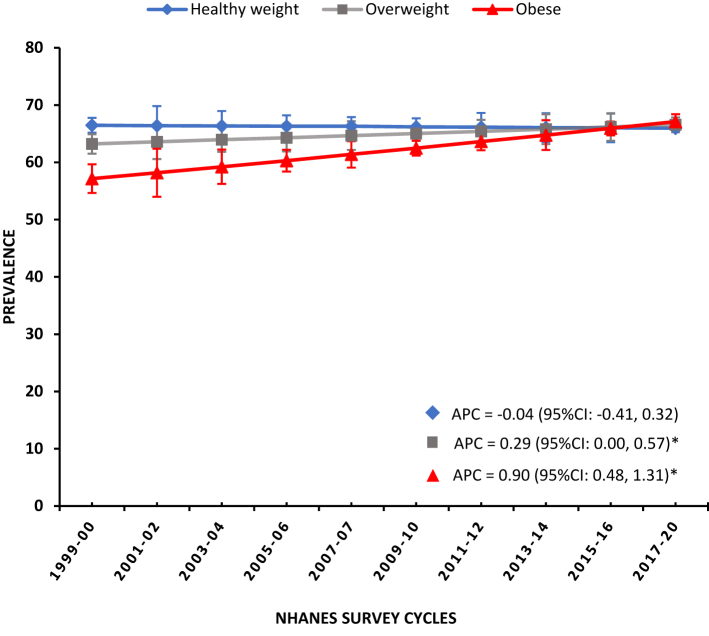
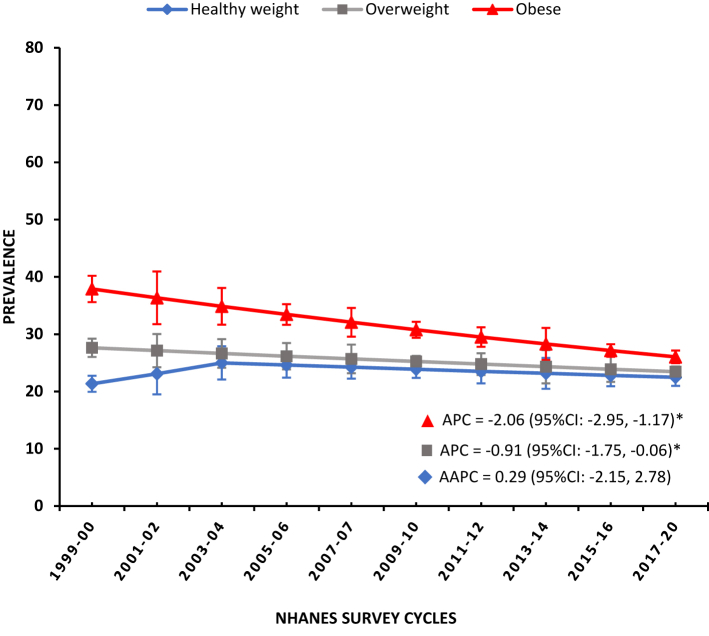
Similarly, Fig. 3 shows that the prevalence of low-moderate drinkers increased by 0.29% per year among overweight (95% CI: 0.00%, 0.57%) and by almost 1% per year among obese individuals (APC, 0.90%; 95% CI: 0.48%, 1.31%) between 1999 and 2017. Like heavy alcohol consumption in obese 40–59-year-old (Table 3), rates of low-moderate alcohol use increased in this group (APC, 1.09%; 95% CI: 0.42%, 1.76%). And an increase was also noted in obese men and women, NHWs, NHBs and Hispanics (Supplementary Table S2). For non-drinkers, among both overweight and obese categories, an overall trend shows a significant decline in the prevalence between 1999 and 2017 (Fig. 4) albeit with a higher decline of over 2% per year observed in obese individuals (APC, −2.06%; 95% CI: −2.95%, −1.17%). This decline was observed in obese individuals across age categories, sex and among race/ethnicity (Supplementary Table S3).
Fig. 3.
Weighted prevalence of low-moderate drinking with annual percentage change (APC) from 1999 to 2020 stratified by healthy weight, overweight and obese U.S. population. ∗Statistically significant increasing trend at α = 0.05.
Fig. 4.
Weighted prevalence of nondrinkers with annual percentage change (APC) and average annual percentage change (AAPC) from 1999 to 2020 stratified by healthy weight, overweight and obese U.S. population. ∗Statistically significant declining trend at α = 0.05.
The overall prevalence of the phenotype of adults who are both obese and are heavy drinkers increased from 1.8% (95% CI: 1.2%, 2.6%) in 1999–2000 to 3.1% (95% CI: 2.7%, 3.7%) in 2017–2020 representing an increase of approximately 72% (Supplementary Table S4). The joinpoint regression also shows that the overall prevalence of combined heavy drinking and obesity from 1999 to 2017 increased by 3.25% (95% CI: 1.67%, 4.85%) per year (Table 4). A notable observation is a significant increase of 9.94% in 40–59 year old that was preceded by a non-significant declining trend. The increasing trends were observed in both men and women albeit higher rate of change in women (APC, 3.96%; 95% CI: 2.14%, 5.82%) compared to men (APC, 2.47%; 95% CI: 0.63%, 4.35%). Parallelism test however indicated that the trends were not different between men and women. A significant increasing linear trend was observed among NHWs (APC, 4.12%; 95% CI: 1.50%, 6.82%) and NHBs (APC, 2.78%; 95% CI: 0.47%, 5.14%) but not Hispanics between 1999 and 2017.
Table 4.
Weighted prevalence of combined obesity and heavy drinking and annual percentage change (APC) overall and by age group, sex, and race/ethnicity: NHANES 1999–2020.
| Population | Weighted prevalence | Joinpoint segmenta |
APC (95% CI) | p | |
|---|---|---|---|---|---|
| Year start | Year end | ||||
| Overall | 2.3 (2.1, 2.5) | 1999 | 2017 | 3.25 (1.67, 4.85) | 0.00 |
| Age-groups | |||||
| 18–39 | 2.2 (2.0, 2.5) | 1999 | 2017 | 1.81 (−2.71, 6.54) | 0.39 |
| 40–59b | 2.7 (2.4, 3.1) | 1999 | 2007 | −4.58 (−16.35, 8.84) | 0.40 |
| 2007 | 2017 | 9.94 (2.37, 18.06) | 0.02 | ||
| ≥60 | 1.7 (1.4, 2.1) | 1999 | 2017 | 4.18 (0.81, 7.67) | 0.02 |
| Sex | |||||
| Men | 1.8 (1.5, 2.0) | 1999 | 2017 | 2.47 (0.63, 4.35) | 0.02 |
| Women | 2.8 (2.5, 3.1) | 1999 | 2017 | 3.96 (2.14, 5.82) | 0.00 |
| Race/Ethnicity | |||||
| NHWc | 2.3 (2.1, 2.6) | 1999 | 2017 | 4.12 (1.50, 6.82) | 0.01 |
| NHBd | 2.6 (2.2, 3.0) | 1999 | 2017 | 2.78 (0.47, 5.14) | 0.02 |
| Hispanics | 2.2 (1.9, 3.8) | 1999 | 2017 | 2.57 (−3.56, 9.10) | 0.37 |
Survey periods are represented by first year e.g., Year-start 1999 (1999–2000 Survey Cycle); Year-end 2017 (2017–2020 Survey Cycle).
AAPC for combined obese heavy drinkers aged 40–59-year-old: 3.23% (95% CI: −2.19%, 8.94%).
Non-Hispanic White.
Non-Hispanic Black.
In the sensitivity analysis removing the 2017–2020 survey cycle, rates of heavy alcohol use were again stable among healthy weight (APC, −0.36%; p = 0.604) and overweight (APC, −0.59%; p = 0.509) adults. For obese adults, the increasing trend of heavy drinking was no longer statistically significant (APC, 1.47%; 95% CI: −0.81%, 3.80%). However, the joinpoint regression again showed that the overall prevalence of combined heavy drinking and obesity has increased over time (APC, 2.77%; 95% CI: 0.72%, 4.86%; p = 0.015).
Discussion
In this population-based study, we report an overall increase in prevalence of heavy alcohol consumption in the obese adult U.S. population. The proportion of the U.S. adult population who are both heavy drinkers and obese increased from 1.8% in 1999–2000 to 3.1% in 2017–2020, representing an increase of 72% (or 3.25% per year). The rate of increase was most striking among individuals aged 40–59, where prevalence of this phenotype increased by almost 10% per year from 2007 to 2017. We showed that prevalence of combined trends increased at a faster rate among women compared to men and increased in NHWs and NHBs but not among Hispanics. Similarly, the prevalence of low-moderate drinkers among obese individuals also increased. In contrast, we found an annual decline in the prevalence of non-drinkers in the U.S. obese population.
Although the prior population-based studies have reported on trends in obesity among the U.S. adults23, 24, 25 and also reported the frequency of alcohol use and its association with obesity,11,26 studies reporting combined alcohol consumption and obesity trends are scarce. It is essential to understand this combined phenotype due to its potential detrimental health implications.9 Although, some studies suggested that low to moderate drinking reduces the likelihood of obesity,27 the current data showed increasing trends of low-moderate drinking with obesity across gender and race/ethnic groups. The hypothesis that alcohol in moderation confers health benefits has implications for estimations of national level burden of ill-effects of obesity.28, 29, 30, 31 The long-time debate on the consumption of low-moderate alcohol use on health outcomes have been narrowed in by the recent Global Burden of Disease (GBD) Study by recommending that the level of alcohol consumption that minimizes health loss is ‘zero standard drinks’ per day.32 The apparent contradiction in findings across existing studies highlights the significance of the need for continuous revisions of public health guidelines for alcohol consumption reduction and obesity prevention based on evolving scientific evidence.
Our study reports overall declining prevalence trends of non-drinkers in obese individuals, and almost uniformly across age groups, gender, and race/ethnicity. A previous population-based study has suggested an increase in alcohol abstinence among young adults between 2002 and 2018.33 We found a significant linear declining trend of non-drinkers among obese adults of ≥40 years, although the decrease was not significant for younger individuals aged 18–39 years. The trends in the current analysis are based specifically on non-drinkers defined as someone who responded in negative to even having at least 12 drinks of any type of alcoholic beverage in their entire life. This contrasts with studies where abstention from alcohol among young individuals and others is defined as ‘non-drinking’ but where former drinkers have not been separated from abstainers in the analysis.31
Previous cross-sectional studies of middle-aged individuals have shown that the strongest influence of alcohol on BMI is observed among those who are non-smokers.34,35 A noticeable finding in the current report is a very high annual increasing trend of combined heavy alcohol consumption and obesity in the middle age group of 40–59 in 10-year period from 2007 to 2017, preceded by a non-significant declining trend between 1999 and 2007. This could be related to changing lifestyle across decades. For example, the changing trend could be due to potential confounding effects of the implementation of tobacco smoking cessation programs and those who quit smoking,36,37 reducing the prevalence of non-smokers and possibly influencing the trend after 2007. Another explanation is the possibility of changes in the type of alcohol consumed in the two time periods where those who report spirit drinking tended to be heavier in weight than beer and wine drinkers.34,35
In addition, we found sex and racial/ethnic differences in the trends of combined alcohol consumption and obesity phenotype over time. For example, there was a higher rate of increase among women compared to men, consistent with the NHANES U.S. specific estimates,24,38 GBD7 and Non Communicable Disease Risk Factor Collaboration (NCD-RisC).39 Obesity impacts health outcomes across reproductive lifespan among women; and alcohol consumption remains an important predictor.40 Much of these results underscore ongoing global obesity pandemic and variations between men and women.24 Although studies have also reported greater burdens of obesity among racially minoritized populations,41 our data showed increasing rates among NHWs and NHBs but not Hispanics. Many obesity interventions are race-specific, targeting minority populations who, over the years, have had the greatest burdens of obesity.42,43
There are several limitations to using NHANES, a repeated cross-sectional survey. Different participants were randomly sampled from the population at several time points. Thus, unlike in longitudinal studies, it is not possible to track within-person changes in weight and drinking behaviour over time. Given the cross-sectional study design, we could not provide any definitive explanation for causes behind the observed trends. We may have underestimated alcohol consumption due to misclassification from self-reported drinking in the NHANES alcohol use questions. Nonetheless, our study has internal validity in terms of the trend assessments. Also, the length of the last survey period of 2017–2020 is not the same as the rest of survey cycles starting from 1999 since the program suspended field operations in March 2020 due to the coronavirus disease 2019 (COVID-19) pandemic. The data collected from 2019 to March 2020 were combined with data from the 2017–2018 cycle to form a nationally representative sample of 2017-March 2020 pre-pandemic data.44 However, in order to make valid comparisons, NHANES allowed use of special sample weights for combined 2017–2020 data. Finally, although sampling weights adjust for nonresponse and missing data, residual bias may remain due to incomplete nonresponse adjustments and may vary with changing response rates.17,38 These results from NHANES cannot be applied or generalized to populations outside the U.S. due to socioeconomic and cultural differences that emerge as predictors of obesity and heavy consumption behaviours. However, population-based surveys like NHANES can allow an important cumulative snapshot of time to speculate on factors influencing the joint trends27 that can then be extrapolated to the general population in the U.S. for informing public health policy on weight reduction and assist in revising alcohol consumption guidelines.
It is important to acknowledge that there are direct and indirect drivers that can lead to higher trends in heavy alcohol consumption and weight gain e.g., psychological stress and depression, as well as physical inactivity, oxidation capacity, adipose signalling and genetics. Like in all observational studies, our analyses cannot attribute any causation due to general lack of information on these potential drivers of the observed trends. Alcohol induced abdominal fat mass is an important pathophysiological entity that leads to several metabolic conditions in alcohol consumers such as hypercholesterolemia, hypertension, glucose intolerance, and insulin resistance.45 Recent evidence also suggests that an important contributor to the obesity epidemic from 2009 onwards is the rising prevalence of obesogenic medications in the U.S. adult population who are already overweight and obese, and that it disproportionally affects individuals with lower socioeconomic status.46,47 While these studies have suggested better non-obesogenic alternative medications, more studies are needed to follow closer scrutiny of medical regimens to avoid weight gain secondary to these medications for the control of obesity epidemic.
Our current analyses also shows that the weighted prevalence of combined heavy alcohol consumption and obesity increased from 2009 to 2010 onwards and that it coincided with the U.S. economic recession during 2008–2009.48 In our study while linking this observed trend, in particular among 40–59 year age group with economic recession remains speculative in nature, it is plausible in light of ‘provocation hypothesis’ proposed by Catalano49,50 which postulates that heavy consumption of alcohol increase during the recession as people cope with insecurity and stress of job loss and foreclosures. Studies using nationally representative data have also reported a relationship between the economic downturn in the U.S. with heavy alcohol use and how this crisis influenced drinking trends.51 During the time of this recession, the rates of abstinence from alcohol increased among younger adults. The overall total alcohol consumption also increased, which was driven by an increase in the number of heavy drinkers with a decline in the number of light drinkers. These results are consistent with our findings and needs to be further built upon to understand how macroeconomic conditions during recession impact the alcohol consumption trends in obese men and women among different race/ethnic groups.
The results of our study should also be interpreted with caution due to possibility of potential implications of conducting multiple comparisons without appropriate corrections. Future studies should consider using corrections for the multiple comparison by adjusting the significance level. It is important however to note that while adjusting for multiple comparison can help control the type I error rate, it may also reduce the power of the study to detect true effects.52 Hence researchers must strike a balance between controlling the type I error rate and maintaining adequate power to detect true effects.
In summary, the prevalence of combined heavy alcohol consumption and obesity among the U.S. adults has increased dramatically over the last two decades; however, secular trends varied across age groups, sex, and race/ethnicity. Conversely, rates of non-drinking have decreased, particularly among obese middle-aged adults and NHWs and NHBs. These findings have important implications considering increasing public and academic debate regarding threshold levels of safe drinking and claimed health benefits from consumption of alcohol in relatively low-moderate doses that also necessitates revision of public health guidelines on alcohol consumption.31,53 Further investigations are needed to inform strategic and effective public health policy development around alcohol use in the context of the now high levels of obesity in the U.S. population.
Contributors
SAR had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. SAR analysed and drafted the manuscript with APT and were involved in the study conception. IOS participated in the critical revision of the manuscript. APT obtained funding for the study and had final responsibility to decide to submit for publication.
Data sharing statement
The data was retrieved from publicly available resources and can be accessed from National Center for Health Statistics of Center for Disease Control and Prevention through https://www.cdc.gov/nchs/nhanes/index.htm.
Declaration of interests
None reported.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lana.2023.100525.
Appendix A. Supplementary data
References
- 1.World Health Organization Key facts alcohol. https://www.who.int/news-room/fact-sheets/detail/alcohol
- 2.Centers for Disease Control and Prevention Alcohol use and your health. https://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm
- 3.World Obesity Federation World obesity atlas 2022. https://www.worldobesity.org/resources/resource-library/world-obesity-atlas-2022
- 4.Inoue Y., Qin B., Poti J., Sokol R., Gordon-Larsen P. Epidemiology of obesity in adults: latest trends. Curr Obes Rep. 2018;7(4):276–288. doi: 10.1007/s13679-018-0317-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang L., Lee I.M., Manson J.E., Buring J.E., Sesso H.D. Alcohol consumption, weight gain, and risk of becoming overweight in middle-aged and older women. Arch Intern Med. 2010;170(5):453–461. doi: 10.1001/archinternmed.2009.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fazzino T.L., Fleming K., Sher K.J., Sullivan D.K., Befort C. Heavy drinking in young adulthood increases risk of transitioning to obesity. Am J Prev Med. 2017;53(2):169–175. doi: 10.1016/j.amepre.2017.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.United States Department of Agriculture Dietary guidelines for Americans, 2020-2025. https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf
- 9.White G.E., Mair C., Richardson G.A., Courcoulas A.P., King W.C. Alcohol use among U.S. adults by weight status and weight loss attempt: NHANES, 2011-2016. Am J Prev Med. 2019;57(2):220–230. doi: 10.1016/j.amepre.2019.03.025. [DOI] [PubMed] [Google Scholar]
- 10.Inan-Eroglu E., Huang B.H., Ahmadi M.N., Johnson N., El-Omar E.M., Stamatakis E. Joint associations of adiposity and alcohol consumption with liver disease-related morbidity and mortality risk: findings from the UK Biobank. Eur J Clin Nutr. 2022;76(1):74–83. doi: 10.1038/s41430-021-00923-4. [DOI] [PubMed] [Google Scholar]
- 11.Patra J., Buckley C., Kerr W.C., Brennan A., Purshouse R.C., Rehm J. Impact of body mass and alcohol consumption on all-cause and liver mortality in 240 000 adults in the United States. Drug Alcohol Rev. 2021;40(6):1061–1070. doi: 10.1111/dar.13265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson C.L., Dohrmann S.M., Burt V.L., Mohadjer L.K. National health and nutrition examination survey: sample design, 2011-2014. Vital Health Stat. 2014;2(162):1–33. [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention About NHANES. https://www.cdc.gov/nchs/nhanes/about_nhanes.htm
- 14.Ponce N., Becker T., Babey S., et al. Improving data capacity for American Indian/Alaska Native (AIAN) populations in federal health surveys. Final report October 2019, Office of the Assistant Secretary for Planning and Evaluation. https://aspe.hhs.gov/sites/default/files/private/pdf/263361/improving-data-capacity-aian.pdf
- 15.National Institute on Alcohol Abuse and Alcoholism Drinking levels defined. https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking#:∼:text=NIAAA%20defines%20heavy%20drinking%20as,than%207%20drinks%20per%20week
- 16.Jensen M.D., Ryan D.H., Apovian C.M., et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25 Pt B):2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention NHANES module 3: weighting. https://wwwn.cdc.gov/nchs/nhanes/tutorials/module3.aspx
- 18.Yu B.B.M., Kim H.J., Feuer E.J. Estimating joinpoints in continuous time scale for multiple change-point models. Comput Stat Data Anal. 2007;51(5):2420–2427. [Google Scholar]
- 19.Kim H.J., Fay M.P., Feuer E.J., Midthune D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 20.Rea F., Pagan E., Compagnoni M.M., et al. Joinpoint regression analysis with time-on-study as time-scale. Application to three Italian population-based cohort studies. Epidemiol Biom Public Health. 2017;14(3):e126161–e126168. [Google Scholar]
- 21.Clegg L.X., Hankey B.F., Tiwari R., Feuer E.J., Edwards B.K. Estimating average annual per cent change in trend analysis. Stat Med. 2009;28(29):3670–3682. doi: 10.1002/sim.3733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim H.J., Fay M.P., Yu B., Barrett M.J., Feuer E.J. Comparability of segmented line regression models. Biometrics. 2004;60(4):1005–1014. doi: 10.1111/j.0006-341X.2004.00256.x. [DOI] [PubMed] [Google Scholar]
- 23.Flegal K.M., Carroll M.D., Kit B.K., Ogden C.L. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 24.Flegal K.M., Kruszon-Moran D., Carroll M.D., Fryar C.D., Ogden C.L. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ogden C.L., Fryar C.D., Martin C.B., et al. Trends in obesity prevalence by race and Hispanic origin-1999-2000 to 2017-2018. JAMA. 2020;324(12):1208–1210. doi: 10.1001/jama.2020.14590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Masum M., Howard J.T., Grigsby T.J. Combined alcohol use and weight status effects on mortality risk among adults: analysis of the National Health Interview Survey linked mortality files, 2001-2015. Drug Alcohol Depend. 2022;230 doi: 10.1016/j.drugalcdep.2021.109206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chakraborty S. Analysis of NHANES 1999-2002 data reveals noteworthy association of alcohol consumption with obesity. Ann Gastroenterol. 2014;27(3):250–257. [PMC free article] [PubMed] [Google Scholar]
- 28.Chikritzhs T., Stockwell T., Naimi T., Andreasson S., Dangardt F., Liang W. Has the leaning tower of presumed health benefits from ‘moderate’ alcohol use finally collapsed? Addiction. 2015;110(5):726–727. doi: 10.1111/add.12828. [DOI] [PubMed] [Google Scholar]
- 29.Chikritzhs T.N., Naimi T.S., Stockwell T.R., Liang W. Mendelian randomisation meta-analysis sheds doubt on protective associations between 'moderate' alcohol consumption and coronary heart disease. Evid Based Med. 2015;20(1):38. doi: 10.1136/ebmed-2014-110086. [DOI] [PubMed] [Google Scholar]
- 30.Holmes M.V., Dale C.E., Zuccolo L., et al. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ. 2014;349 doi: 10.1136/bmj.g4164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stockwell T., Zhao J., Panwar S., Roemer A., Naimi T., Chikritzhs T. Do "Moderate" drinkers have reduced mortality risk? A systematic review and meta-analysis of alcohol consumption and all-cause mortality. J Stud Alcohol Drugs. 2016;77(2):185–198. doi: 10.15288/jsad.2016.77.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.GBD 2020 Alcohol Collaborators Population-level risks of alcohol consumption by amount, geography, age, sex, and year: a systematic analysis for the Global Burden of Disease Study 2020. Lancet. 2022;400(10347):185–235. doi: 10.1016/S0140-6736(22)00847-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCabe S.E., Arterberry B.J., Dickinson K., et al. Assessment of changes in alcohol and marijuana abstinence, co-use, and use disorders among US young adults from 2002 to 2018. JAMA Pediatr. 2021;175(1):64–72. doi: 10.1001/jamapediatrics.2020.3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wannamethee S.G., Field A.E., Colditz G.A., Rimm E.B. Alcohol intake and 8-year weight gain in women: a prospective study. Obes Res. 2004;12(9):1386–1396. doi: 10.1038/oby.2004.175. [DOI] [PubMed] [Google Scholar]
- 35.Wannamethee S.G., Shaper A.G. Alcohol, body weight, and weight gain in middle-aged men. Am J Clin Nutr. 2003;77(5):1312–1317. doi: 10.1093/ajcn/77.5.1312. [DOI] [PubMed] [Google Scholar]
- 36.Aubin H.J., Farley A., Lycett D., Lahmek P., Aveyard P. Weight gain in smokers after quitting cigarettes: meta-analysis. BMJ. 2012;345 doi: 10.1136/bmj.e4439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Inoue-Choi M., Freedman N.D. When to adjust for potentially confounding variables-reply. JAMA Intern Med. 2017;177(6):892. doi: 10.1001/jamainternmed.2017.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hales C.M., Fryar C.D., Carroll M.D., Freedman D.S., Aoki Y., Ogden C.L. Differences in obesity prevalence by demographic characteristics and urbanization level among adults in the United States, 2013-2016. JAMA. 2018;319(23):2419–2429. doi: 10.1001/jama.2018.7270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.National Communicable Disease Risk Factor Collaboration Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCarty C.A., Kosterman R., Mason W.A., et al. Longitudinal associations among depression, obesity and alcohol use disorders in young adulthood. Gen Hosp Psychiatry. 2009;31(5):442–450. doi: 10.1016/j.genhosppsych.2009.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hill S.E., Bell C., Bowie J.V., et al. Differences in obesity among men of diverse racial and ethnic background. Am J Mens Health. 2017;11(4):984–989. doi: 10.1177/1557988315580348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Petersen R., Pan L., Blanck H.M. Racial and ethnic disparities in adult obesity in the United States: CDC's tracking to inform state and local action. Prev Chronic Dis. 2019;16 doi: 10.5888/pcd16.180579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang L., Southerland J., Wang K., et al. Ethnic differences in risk factors for obesity among adults in California, the United States. J Obes. 2017;2017 doi: 10.1155/2017/2427483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention NHANES 2017-March 2020 pre-pandemic. https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?cycle=2017-2020
- 45.Sutter P.M. Is alcohol consumption a risk factor for weight gain and obesity? Crit Rev Clin Lab Sci. 2005;42(3):197–227. doi: 10.1080/10408360590913542. [DOI] [PubMed] [Google Scholar]
- 46.Lyu B., Chang A.R., Inker L.A., Selvin E., Grams M.E., Shin J.I. Socioeconomic status and use of obesogenic and anti-obesity medications in the United States: a population-based study. Lancet Reg Health Am. 2022;11 doi: 10.1016/j.lana.2022.100249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hales C.M., Gu Q., Ogden C.L., Yanovski S.Z. Use of prescription medications associated with weight gain among US adults, 1999-2018: a nationally representative survey. Obesity. 2022;30(1):229–239. doi: 10.1002/oby.23299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mulia N., Zemore S.E., Murphy R., Liu H., Catalano R. Economic loss and alcohol consumption and problems during the 2008 to 2009 U.S. recession. Alcohol Clin Exp Res. 2014;38(4):1026–1034. doi: 10.1111/acer.12301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Catalano R. An emerging theory of the effect of economic contraction on alcohol abuse in the United States. Soc Justice Res. 1997;10:191–201. [Google Scholar]
- 50.Catalano R., Dooley D., Wilson G., Hough R. Job loss and alcohol abuse: a test using data from the epidemiologic catchment area project. J Health Soc Behav. 1993;34(3):215–225. [PubMed] [Google Scholar]
- 51.Bor J., Basu S., Coutts A., McKee M., Stuckler D. Alcohol use during the great recession of 2008-2009. Alcohol Alcohol. 2013;48(3):343–348. doi: 10.1093/alcalc/agt002. [DOI] [PubMed] [Google Scholar]
- 52.Savitz D.A., Olshan A.F. Multiple comparisons and related issues in the interpretation of epidemiologic data. Am J Epidemiol. 1995;142(9):904–908. doi: 10.1093/oxfordjournals.aje.a117737. [DOI] [PubMed] [Google Scholar]
- 53.Gilmore W., Chikritzhs T., Stockwell T., Jernigan D., Naimi T., Gilmore I. Alcohol: taking a population perspective. Nat Rev Gastroenterol Hepatol. 2016;13(7):426–434. doi: 10.1038/nrgastro.2016.70. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.