Abstract
Introduction
Nonunion of long bones is a major complication following fractures that requires a substantial amount of investment both monetary and time from patients and surgeons. The need to comprehensively understand the complications, outcomes and distraction capability is profound, which necessitates a review of current evidence on special fixators used for distraction. The current systematic review aims to study the available literature on distraction osteogenesis using special fixators (Ilizarov and Limb Reconstruction System) in the management of nonunion (infected and non-infected).
Methods
Cochrane Library, PubMed, Scopus were searched until January 2022. The review included all original studies which used Ilizarov or Monorail Fixators/LRS in the treatment of nonunion of long bones. The quality of studies was assessed using the Modified Coleman Methodology Score.
Results
A total of 35 original studies with Ilizarov (n = 29) and LRS (n = 8) were selected including two comparative studies. The pooled data meta-analysis and the subgroup analysis of these studies found both Ilizarov and LRS fixator yield similar functional outcomes for the treatment of long bones nonunion.
Conclusion
The review was conducted to understand the scenario of nonunion in long bones. Pin tract infection is found to be the most common complication followed by adjacent joint stiffness and deformity. In our review we observed that both external fixator time and index were lower in LRS compared to Ilizarov group. Further RCT are required comparing Ilizarov and LRS fixators to effectively comment upon the superiority of the implants.
Keywords: Non-union, ASAMI Score, Ilizarov, Monorail fixators, LRS, Long bone, Complications
1. Introduction
Nonunion of long bones is a major complication following fractures that requires a substantial amount of investment both monetary and time from patients and surgeons alike for treatment.1, 2, 3 Infected nonunions further curtail the progress and leads to multiple procedures, including debridement, bone transport, or bone grafting.4 The general consensus in literature favors to the use of radical debridement of necrotic bone and soft tissue followed by external fixation.5
Nonunions (infected or non-infected) persistently produce gap defects due to the necrotic bone at the ends.5 Currently, there exist multiple methods for the management of nonunions. Among them, the most commonly used methods are Distraction Osteogenesis with external fixation, Masquelet technique, Huntington method, and bone grafting.6,7 Distraction osteogenesis is currently the most preferred method of treatment in gap nonunions, using a corticotomy and gradually distracting.7,8 The construct is held by Ilizarov special ring fixators or the newer Limb Reconstruction System (LRS) or the hybrid fixators.8
There is a volume of literature on the clinical outcomes and complications, however, some lacunae still exist in the literature to comprehensively assess the expected outcome and complications. Peng Yin et al. in their review, used 24 studies (n = 590) to assess the outcomes using ASAMI scores and noted that Ilizarov methods had high rates of good bone formation and high functional scores.9 The review failed to include all the available literature and comment on overall outcomes. Moreover, the outcomes of LRS in nonunions were not studied.9 The need to comprehensively understand the complications, outcomes and distraction capability is profound, which necessitates a review of current evidence on special fixators used for distraction.
The current systematic review aims to study the available literature on distraction osteogenesis using special fixators (Ilizarov and LRS) in the management of nonunion (infected and non-infected). The interests of outcomes for the study were complications, distraction capability, and outcomes in terms of The Association for the Study and Application of Methods of Ilizarov (ASAMI) functional and bone scores.
2. Material and methods
The current review and meta-analysis were performed in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.10
3. Literature search and study selection
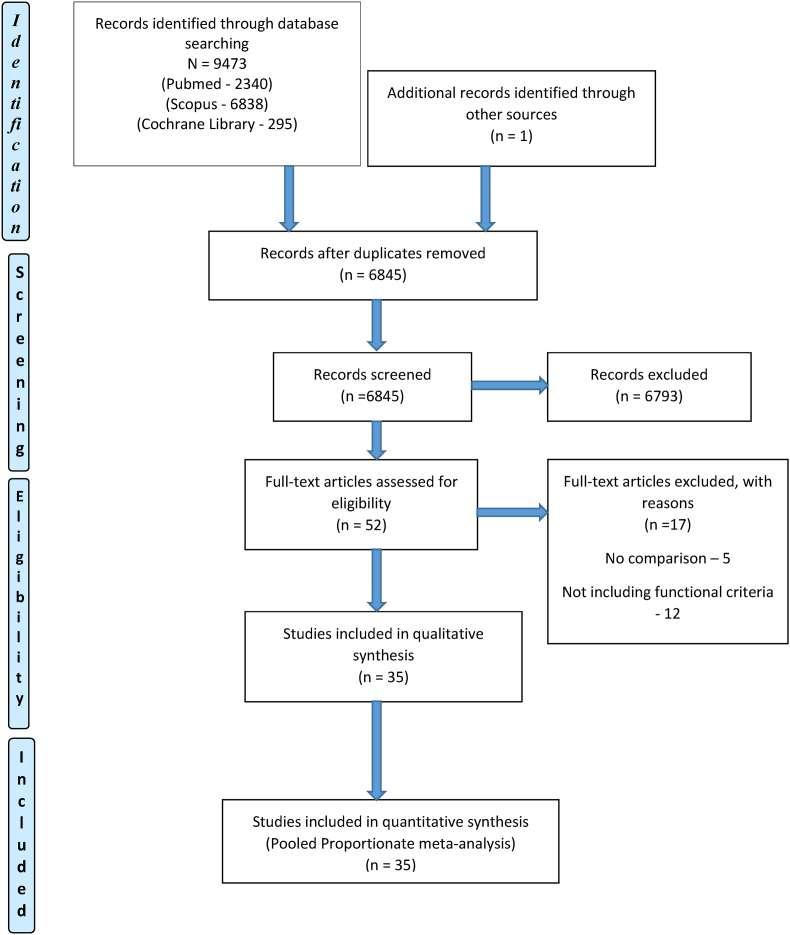
The online databases platform Pubmed, Scopus, and Cochrane library were searched by three authors. The last date of the search was 31/01/2022, and all the databases were searched from 01/01/2001 to the above specified time. The search terms used where “Nonunion”, “Non-union”, “Ilizarov”, “Ilizarov method” or “Ilizarov methods”, and “Ilizarov technique” or “Ilizarov techniques”, “LRS”, “Limb reconstruction system”, “Femur”, “Tibia”, “Humerus”, “Long bone”, “outcome”, “complication”, “functional score” with Boolean operators “AND” and “OR”. The flow diagram representing the search is shown in Fig. 1. The abstracts were identified first by the above-mentioned search methods and were assessed for eligibility based on the criteria mentioned below. The shortlisted abstracts were followed up for full texts and again assessed for eligibility. An additional search of the reference list of the finalized articles was searched for further relevant studies. The process was repeated two times, and the senior author had final say regarding discrepancies between the authors.
Fig. 1.
PRISMA chart.
4. Eligibility criteria
The review used the following eligibility criteria for articles selection: (1) Target population: patients with nonunion of humerus, tibia, and femur; (2) Intervention: Ilizarov methods and LRS, including bone transport, acute compression and lengthening, and compression osteosynthesis; (3) Studies with any of the two mentioned outcomes were included. Outcomes: bone union, bone evaluated by ASAMI (rated as excellent, good, fair and poor), and functional results evaluated by ASAMI (rated as excellent, good, fair and poor), complications, external fixation time and external fixation index. (4) Follow-up of >2 years; (5) All types of articles excluding case reports, case series with less than three patients, biomechanical studies, expert opinions, letters to editors, or editorials and review or non-English language. Duplicate or multiple publications of the same study were excluded.
5. Data extraction and statistical analysis
Three authors extracted the data using a standardized form. The following data were extracted from each included study: first author, year of publication, journal, study location, study design, level of evidence, technique, sample size, mean age, mean previous surgical procedures (number of the procedure the patient underwent before the enrolling into the study), mean bone defects, mean length of follow-up, bone results evaluated by ASAMI, functional results evaluated by ASAMI, complications per patient, external fixation time (months of treatment time), and external fixation index (days of treatment time divided by centimeters of the bone defect), and complications as events. The continuous variables were extracted and expressed as mean ± standard deviation. In case of missing data, the authors were contacted for the specific information, and the articles were excluded if responses were not obtained. Disagreements between the authors were discussed, and the senior author took the final decision.
Bone results was evaluated based on union, infection, deformity, and limb length discrepancy as excellent: union without infection, <7° deformity, and <2.5 cm limb length inequality; good: union with 2 of the above criteria; fair: union with one of the above criteria; poor: nonunion or re-fracture, and none of the above criteria fulfilled11
The functional result was evaluated according to 5 adverse criteria: (1) observable limp, (2) stiffness of knee or hip (loss of >70° of knee flexion or >15° of knee extension), (3) loss of >50% of hip motion when compared with the normal contralateral side, (4) severe sympathetic dystrophy, pain that reduced activity or disturbed sleep, and (5) inactivity (unemployment or inability to return to daily activities). (11) Provided the patient was active, the result was deemed excellent if the other four criteria were also absent, good if one or 2 of the other criteria were present, and fair if 3 or 4 of them prevailed. The result was deemed poor if the patient was inactive, regardless of the other criteria.
The review and meta-analysis were done using the Medcalc version 20.211. The random-effects model was taken for pooled estimates in the meta-analysis, assuming the heterogeneity in the methods and techniques and that the included studies represent a random sample from the larger population of such studies wherein each study has its own underlying effect size. The heterogeneity of the sample was assessed with the I2 statistic, with values of 25, 50, and 75% considered as low, moderate, and high heterogeneity, respectively.12 Other major data extracted in this study were recorded and statistically analyzed using weighted means based on the sample size in each study by Medcalc version 20.211, including the number of patients, mean age, mean previous surgical procedures, mean bone defects, mean length of follow-up, bone union, complications per patient, external fixation time (EFT), and external fixation index (EFI). If the standard deviation was not mentioned in the study, it was calculated using the range of values as per Hozo et al.13
6. Quality assessment
Two authors assessed the quality of the studies included in the review. Modified Coleman Methodology Score (MCMS) was used for the analysis, and it consisted of 10 (7 + 3) parameters for which each item had an individual score based on the reported outcome.14 The score was not used as an exclusion criterion for the selected articles. The senior author had final say regarding discrepancies between the authors, if any, by discussion to reach a consensus.
7. Results
7.1. Study characteristics
The initial literature search identified 9473 relevant records published from 01 January 2001 to 31 January 2022, out of which duplicates were removed, and a total of 35 original studies with Ilizarov (n = 29) and LRS (n = 8) were selected using the criteria mentioned above with two comparative studies. Twenty-four were retrospective, and eleven were prospective studies. The review found two studies that compared LRS vs. Ilizarov meeting the inclusion criteria4,7
The review included a total of 1391 patients, of which 1181 underwent Ilizarov and 210 underwent LRS. The study demographics have been listed in Table 1. The mean age of patients was 37.42 years. 1104 were males, and 287 were females, with one study failing to mention sex of the study participants.15
Table 1.
Study characteristics of Ilizarov and LRS group.
| ILIZAROV DATA | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Author (year) | Study design | Sample size (n) | M/F (n) | Age (year) | Site of Intervention (N) | MPSP (n) | Mean bone defects (cm) | Technique/Procedure | Mean follow up (month) | MCMS |
| V Barbarossa (2001) | Prospective | 30 | 24/6 | 39.4± 14.4 (25–80) | Femur | 4.4 ± NS | 6.3 ± NS | Ilizarov | NS (24–126) | 66 |
| David W. Sanders (2002) | retrospective | 19 | 12/3 (1 loss of f/u and 3 amputated NS) | 45 ± NS (20–78) | Tibia | NS | 8 ± NS (4.5–12) | Ilizarov | 39 ± NS | 50 |
| S Patil (2006) | Retrospective | 41 | 35/5 | 41 ± NS (10–73) | 36 Tibia 5 Femur | 3 ± NS (1–10) | NS | Ilizarov | 61.1 ± NS | 66 |
| A Krishnan (2006) | Retrospective | 20 | 17/3 | 38.4 ± NS (18–65) | Femur | 4.4±2 (1–9) | NS | Ilizarov | 62.8±25 | 54 |
| MP Magadum (2006) | Retrospective | 27 | 27/0 | 39±14 (15–65) | Tibia | 2 ± NS (1–4) | NS | Ilizarov | 27 ± NS (25–39) | 58 |
| Dror Paley (2006) | Retrospective | 21 | 12/9 | 40 ± NS (12–63) | Tibia | NS | NS | Ilizarov | 83.4 ± NS (26–144) | 63 |
| Ranjit Baruah (2007) | Retrospective | 50 | 45/5 | NS (18–56) | Tibia | NS | 3.5 ± NS (2–9) | Ilizarov | NS (24–72) | 59 |
| M. Trigui (2008) | Retrospective | 9 | 5/4 | 20 ± NS | 8 Tibia 1 Femur |
NS | 4.1 ± NS (2–8) | Ilizarov | 28 ± NS | 53 |
| Khaled M Emara (2008) | Prospective | 33 | 22/11 | 2 ± NS | Tibia | NS | 6 ± NS | Ilizarov | 36 ± NS (22–48) | 68 |
| S. Robert Rozbruch (2008) | Retrospective | 38 | 30/8 | 43 ± NS (8−72) | Tibia | 4 ± NS (0−20) | 5.9 ± NS (1.5–16) | Ilizarov | 37 ± NS (15–63) | 58 |
| Michael D. Mckee (2008) | Retrospective | 11 | 8/3 | 43.7 ± NS (30–71) | Tibia | 4.5 ± NS (2–12) | NS | Ilizarov | 41 ± NS (24–82) | 56 |
| Francesco Sala (2011) | Retrospective | 12 | 8/4 | 44 ± NS (19–79) | Tibial | 4.66 ± NS | 8.06±2.6 (3.0–12.0) | Ilizarov | 24.6±4.7 (18–32) | 50 |
| M Sayed (2013) | Retrospective | 20 | 19/1 | 37.45 ± NS | Femur | 1.95±1.05 (1–5) | NS | Ilizarov | 36.65±15.8 (25–82) | 62 |
| P Yin (2014) | Retrospective | 66 | 62/4 | 37.06 ± NS | Tibia | NS | 6.27 ± NS (3–13) | Ilizarov | 25.91 ± NS | 63 |
| Chang Seon Oh (2015) | Retrospective | 7 | 6/1 | 14.4 ± NS (4.8–36.9) | 5 Tibia 2 Femur | NS | 7.3 ± NS (5.1–12.1) | Ilizarov | 106.2 ± NS | 59 |
| Peng Yin (2015) | Retrospective | 72 | 92/18 | 38.90 ± NS | Tibias | 2.61 ± NS (1–8) | 6.15 ± NS (3−13) | Ilizarov | 23.12 ± NS (14–46) | 60 |
| Ramji Lal Sahu (2016) | Prospective | 60 | 50/10 | 37.5 ± NS (25–45) | Tibia | 3.5 ± NS (2–5) | 3 ± NS (2–5) | Ilizarov | 36 ± NS (26–50) | 71 |
| Kemal Aktuglu (2016) | Retrospective | 24 | 21/3 | 35.04±17.19 (8–69) | Tibia | 3.64±2.66 (range, 0–11). | 7.01±2.88 (5–18) | Ilizarov | 74.08±24.17 | 53 |
| R Rohilla (2016) | Prospective | 35 | 32/3 | 33.2 ± NS (18–64) | Tibia | 1 ± NS | 5.84 ± NS (3–9) | I-Ilizarov | 33.8 ± NS | 79 |
| Martin McNally (2017) | Prospective | 79 | 61/18 | 43.0 ± NS | Tibia | 2.2 ± NS (1–5) | 4.93 ± NS | Ilizarov | 40.8 ± NS (6–131) | 71 |
| Gamal Ahmed Hosny (2018) | Retrospective | 144 | 87/57 | 44.48 ± NS | 18 Humerus | 4.35±1.21 (2–6) | 5.98 ± NS (3−10) | Ilizarov | 51.05 ± NS | 60 |
| 52 Femur | ||||||||||
| 74 Tibia | ||||||||||
| K Bhowmick (2018) | Retrospective | 8 | 7/1 | 41 ± NS (22–57) | Tibia | All 8 underwent 1 procedure | NS | Ilizarov | 33±35.05 (12–20) | 62 |
| S Fahad (2019) | Retrospective | 51 | 41/10 | 45.65±16.69 | Tibia | 2 ± NS (1–4) | 3.5 ± NS (2–5) | Ilizarov | 36.84 ± NS | 69 |
| G Testa (2020) | Retrospective | 26 | 20/6 | 51.3±15.3 (22–68) | Tibia | All 26 underwent 1 procedure | NS | Ilizarov | 28.25 ± NS (9–42.75) | 62 |
| I Sigmund (2020) | Prospective | 47 ASR: 20, BT: 27 | NS | ASR: 48.9 ± NS (21–78), | Tibia | ASR: 2.9 ± NS (1–5) | ASR: 4.0 ± NS (2–5) | Ilizarov | 37.9 ± NS (16–128) | 79 |
| NS | BT: 50.9 ± NS (29–75), | BT: 2.7 ± NS (1–6) | BT: 5.9 ± NS (3–10) | |||||||
| R K Baruah (2020) | Retrospective | 86 | 72/24 | NS (18–65) | Tibia | 5 ± NS | 5.04 ± NS (3–9) | Ilizarov | 24 ± NS | 69 |
| Gamal Ahmed Hosny (2020) | Retrospective | 13 | 11/2 | 9.1 ± NS (2–14.5) | Femur | 3.3 ± NS | NS | Ilizarov | 60.15 ± NS | 65 |
| A Chalak (2021) | Retrospective | 30 | 16/14 | 39.27 ± NS (10–66), | Tibia | 16 underwent 1 procedure | 7.17 ± NS (2–12) | Ilizarov | 39.36 ± NS (24–54) | 69 |
| Lukasz Szelereski (2021) | Retrospective | 102 | 76/26 | 46.7 ± NS (11–84) | Tibia | NS | NS | Ilizarov | 84 ± NS (24–144) | 65 |
| LRS DATA | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Author (year) | Study design | Sample size (n) | M/F (n) | Age (year) | Site of intervention (n) | MPSP (n) | Mean bone defects (cm) | Technique/Procedure | Mean follow up (month) | MCMS |
| Hiranaya Seenappa (2013) | Prospective | 30 | 28/2 | 29.28 ± NS (19–66) | 16 Tibia, | 2.67 ± NS (0–10) | 5.06 ± NS (1–10) | LRS | 27 ± NS (14–41) | 66 |
| 10 Femur, | ||||||||||
| 4 Humerus | ||||||||||
| Peng Yin (2015) | Retrospective | 38 | 92/18 | 38.90 ± NS | Femur | 2.61 ± NS (1–8) | 6.15 ± NS (3−13) | Monorail | 23.12 ± NS (14–46) | 60 |
| R Rohilla (2016) | Prospective | 35 | 30/5 | 29.3 ± NS (18–65) | Tibia | 1 ± NS | 5.78 ± NS (3–10) | LRS | 32.6 ± NS | 79 |
| Qun Jhang (2017) | Retrospective | 41 | 31/10 | 44 ± NS (26–76) | Femur | NS | 10.1 ± NS (6–17) | LRS | 35 ± NS (20–60) | 61 |
| S Gupta (2018) | Retrospective | 14 | 13/1 | 38.1 ± NS | Tibia | NS | 6.4±1.3 | LRS | 33.2 ± NS (24–50) | 60 |
| Xun Chen (2019) | Prospective | 23 | 19/4 | 37.8 ± NS (19–54) | Tibia | 2.5 ± NS (2–4) | 6.5 ± NS (5.2–8.1) | LRS | 57.6 ± NS (36–72) | 62 |
| N Kushwaha (2020) | Prospective | 21 | 19/2 | 29.43±14.07 | Tibia | NS | NS | LRS | 29.5 ± NS (16–50) | 76 |
| Victor Lu (2021) | Retrospective | 8 | 8/0 | 37.75 ± NS | femur | 4.5 ± NS | 9.69 ± NS | Rail Fixator | 57 ± NS | 50 |
ASR, Acute Shortening and Relengthening; BT, Bone Transport; MPSP, Mean previous surgical procedures; MCMS, Modified Coleman Methodology score; NS, Not Specified; LRS, Limb Reconstruction System.
7.2. Quality assessment
The quality assessment revealed that the average MCMS score was 65, of which 30 studies scored between 55 and 69 (Fair group), and five studies showed scores between 70 and 84 (Good Group). Details have been tabulated in Table 1.
7.3. Mean previous surgical procedures
A total of 25 studies reported on the mean previous surgical procedures patients underwent before being part of the study. The Ilizarov group noted 3.18 mean previous surgical procedures in 21 studies,4,7,15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32 whereas the LRS group noted a mean of 2.30 procedures in 5 studies.4,7,33, 34, 35 Details have been tabulated in Table 1.
7.4. Mean bone defect
A total of 25 studies reported on the mean bone defects in patients before being part of the study. The Ilizarov group noted a mean of 5.43 cm in 19 studies,4,7,20,21,24, 25, 26, 27,29,31,32,36, 37, 38, 39, 40, 41 whereas the LRS group noted a mean of 6.97 cm in 7 studies4,7,33, 34, 35,42,43 Details have been tabulated in Table 1.
7.5. External fixator index (day/cm)
Twenty-one studies reported on the External fixator index, including the comparative study. 16 studies in the Ilizarov group with the average being 54.46 day/cm,4,7,15,18,24, 25, 26,29,31,32,37, 38, 39, 40, 41,44 while in the LRS group, seven studies reported on the outcome with the average being 43.64 day/cm.4,7,33, 34, 35,42,43 Details have been tabulated in Table 2.
Table 2.
Functional Outcome of Studies in Ilizarov and LRS group.
| ILIZAROV DATA | |||||||
|---|---|---|---|---|---|---|---|
| Author (year) | ASAMI (bone results) – E/G/F/P | E + G | ASAMI (functional results) – E/G/F/P | E + G | External fixator time (month) | External fixator index (day/cm) | Complications per patient (number of complications/sample size) |
| V Barbarossa (2001) | 13/9/2/5 with 1 amputation | 22/30 | 5/10/8/6 (1 failure) | 15/30 | NS | NS | 87/30 = 2.9 |
| David W. Sanders (2002) | NS | NS | 9/4/1/5 | 13/19 | NS | NS | 18/19 = 0.94 |
| S Patil (2006) | 17/14/4/6 | 31/41 | 14/14/2/4 | 28/41 | 14.1 ± NS | NS | 56/41 = 1.36 |
| A Krishnan (2006) | 13/4/1/1 | 17/20 | 3/9/3/5 | 12/20 | 7.8±4.13 | 38.3±1.6 (36–42) | 71/20 = 3.55 |
| MP Magadum (2006) | 19/5/0/1 | 24/27 | 15/8/1/1 | 23/27 | 6.3 ± NS (4−12) | NS | 25/27 = 0.92 |
| Dror Paley (2006) | 10/9/1/1 | 19/21 | 15/3/2/1 | 18/21 | 7.8 ± NS | 75 ± NS | 61/21 = 2.9 |
| Ranjit Baruah (2007) | 24/24/0/2 | 48/50 | 23/22/2/2 | 45/50 | 6.08 ± NS | 51.9 ± NS | 33/50 = 0.66 |
| Khaled M Emara (2008) | IMN – 17/0/0/0 Without IMN – 15/1/0/0 | 33/33 | IMN – 13/2/2/0 Without IMN – 12/1/3/0 | 28/33 | With IMN-3.1 ± NS | With IMN- 16.5 ± NS | 10/33 = 0.3 |
| Without IMN – 8.5 ± NS | Without IMN -45 ± NS | ||||||
| S. Robert Rozbruch (2008) | 24/12/0/2 | 36/38 | 20/14/2/2 | 34/38 | 9.6 ± NS (3.9–23.8) | NS | 24/38 = 0.63 |
| Michael D. McKee (2008) | NS | NS | 9/1/1/0 | 10/11 | 6.5 ± NS (1.75–10.5) | NS | 25/11 = 2.27 |
| M. Trigui (2008) | 3/4/2/0 | 7/9 | 1/8/0/0 | 9/9 | 9 ± NS | 57 ± NS | 18/9 = 2 |
| Francesco Sala (2011) | 10/2/0/0 | 12/12 | 6/5/1/0 | 11/12 | 15.16 ± NS | NS | 24/12 = 2 |
| M Sayed (2013) | 10/6/1/3 | 16/20 | 4/13/3/0 | 17/20 | 8.03±2.774 (5–15) | NS | 63/20 = 3.15 |
| P Yin (2014) | 44/15/5/2 | 59/66 | 24/26/10/0 | 50/66 | NS | 41.4 ± NS (34.5–47.4) | NS |
| Chang Seon Oh (2015) | 6/1/0/0 | 7/7 | 6/1/0/0 | 7/7 | 6.18 ± NS | 26.0 ± NS (19.8–32.5) | 3/7 = 0.42 |
| Peng Yin (2015) | 46/17/7/2 | 63/72 | 25/27/13/0 | 52/72 | 2.3 ± NS | 44.4 ± NS (34.5–50.1) | 192/110: 1.74 |
| Ramji Lal Sahu (2016) | 50/7/2/1 | 57/60 | 45/10/3/2 | 55/60 | 12 ± NS (8–14) | 120 ± NS | 69/60 = 1.15 |
| Kemal Aktuglu (2016) | 12/8/2/2 | 20/24 | 14/9/1/0 | 23/24 | 11.69±2.97 (8.7–20.9) | 52 ± NS (34.8–62.8) | 28/24 = 1.66 |
| R Rohilla (2016) | I-21/12/0/2 | 33/35 | I-16/17/1/1 | 33/35 | 11.1 ± NS | 63.6 ± NS | I-60/35 = 1.71 |
| Martin McNally (2017) | 74/3/0/2 | 77/79 | 55/16/6/1 (1 amputation) | 71/79 | 7.5 ± NS | 45.6 ± NS | 18/79 = 0.23 |
| Gamal Ahmed Hosny (2018) | 109/26/3/6 | 135/144 | 91/38/12/3 | 129/144 | 9.12±2.27 (6–16) | NS | 35/144 = 0.24 |
| K Bhowmick (2018) | 8/0/0/0 | 8/8 | 5/3/0/0 | 8/8 | 11.5±8.03 (3–30) | NS | 8/8 = 1 |
| S Fahad (2019) | 22/19/7/3 | 41/51 | 24/21/4/2 | 45/51 | 10 ± NS | 60 ± NS (45–120) | 24/51 = 0.47 |
| G Testa (2020) | 10/12/4/0 | 22/26 | 16/9/1/0 | 25/26 | 9.8±2.3 (6–13) | NS | 6/26 = 0.23 |
| I Sigmund (2020) | ASR: 18/2/0/0 BT: 22/5/0/0 | 47/47 | ASR: 12/7/1/0 BT: 19/6/2/0 | 44/47 | ASR: 8.8 ± NS (5−16) | ASR: 60 ± NS (39–84) | 31/47 = 0.6531 |
| BT: 10.3 (7–17) | BT: 54 ± NS (27–81) | ||||||
| R K Baruah (2020) | 16/42/18/10 | 58/86 | 13/44/22/7 | 57/86 | 6.8 ± NS | 40.5 ± NS | 51/86 = 0.6 |
| Gamal Ahmed Hosny (2020) | 8/3/1/1 | 11/13 | 9/3/1/0 | 12/13 | 5.3 ± NS | NS | 18/13 = 1.4 |
| A Chalak (2021) | 27/2/1/0 | 29/30 | 28/2/0/0 | 30/30 | 11.43 ± NS | 51.3 ± NS (35–105) | 20/30 = 0.66 |
| Lukasz Szelereski (2021) | 88/9/0/5 | 97/102 | 67/30/0/5 | 97/102 | 8.3 ± NS | NS | 5/102 = 0.05 |
| LRS DATA | |||||||
|---|---|---|---|---|---|---|---|
| Author (year) | ASAMI (bone results) – E/G/F/P | E + G | ASAMI (functional results) – E/G/F/P | E + G | External fixator time (month) | External fixator index (day/cm) | Complications per patient (number of complications/sample size) |
| Seenappa (2013) | 22/3/0/3 | 25/30 | 11/14/0/0 (Failure-3) | 25/30 | 9.68 ± NS | 57.3 ± NS | 50/30 = 1.66 |
| Peng Yin (2015) | 22/11/5/0 | 33/38 | 12/15/8/0 | 27/38 | 64.45 ± NS (45–86) | 45 ± NS (38.4–51.3) | 192/110: 1.74 |
| Rohilla (2016) | 14/15/3/3 | 29/35 | 22/10/0/3 | 32/35 | 10.5 ± NS | 63.3 ± NS | II-70/35 = 2 |
| Jhang (2017) | 30/6/5/0 | 36/41 | 21/9/7/4 | 30/41 | 13.3 ± NS | 39 ± NS | 58/41 = 1.41 |
| Gupta (2018) | 14/0/0/0 | 14/14 | 8/6/0/0 | 14/14 | 4.5 ± NS | 21.2 ± NS | 7/14 = 0.5 |
| Chen (2019) | 15/8/0/0 | 23/23 | 18/5/0/0 | 23/23 | 3.26 ± NS | 22.4 ± NS | 5/23 = 0.22 |
| Kushwaha (2020) | 9/10/2/0 | 19/21 | 11/9/1/0 | 20/21 | 11.2 ± NS (6–18) | NS | 10/21 = 0.47 |
| Victor Lu (2021) | 4/2/0/2 | 6/8 | NS | NS | 2.29 ± NS | 24 ± NS (11.2–42.0) | 17/8 = 2.125 |
ASAMI, The Association For The Study And Application Of Methods Of Ilizarov; E/G/F/P/F, Excellent/Good/Fair/Poor/Failure; EFT, External fixation time; EFI, External fixation index.
7.6. External fixator time (month)
Thirty-two studies reported on the follow-up, including the comparative study. Twenty-six studies were in the Ilizarov group,4,7,15,17, 18, 19, 20, 21,23, 24, 25, 26, 27, 28, 29, 30, 31, 32,37, 38, 39,41,44,45 with the average being 8.52 months, while in the LRS group, all studies reported on the outcome with the average being 7.98 months.4,7,33, 34, 35,42,43,46 Details have been tabulated in Table 2.
7.7. Follow up
Thirty-three studies reported on the follow-up, including the comparative study. Twenty-seven studies in the Ilizarov group with the average follow-up being 41.03 months,4,7,15,17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32,36, 37, 38, 39, 40, 41,44,45 while in the LRS group, all studies reported the outcome with an average of 33.95 months.4,7,33, 34, 35,42,43,46 Details have been tabulated in Table 1.
7.8. Outcome assessment
The review included studies with a standardized protocol for reporting the outcomes. The Association for the Study and Application of Methods of Ilizarov (ASAMI) scoring system in which Bone and Functional results were assessed separately.
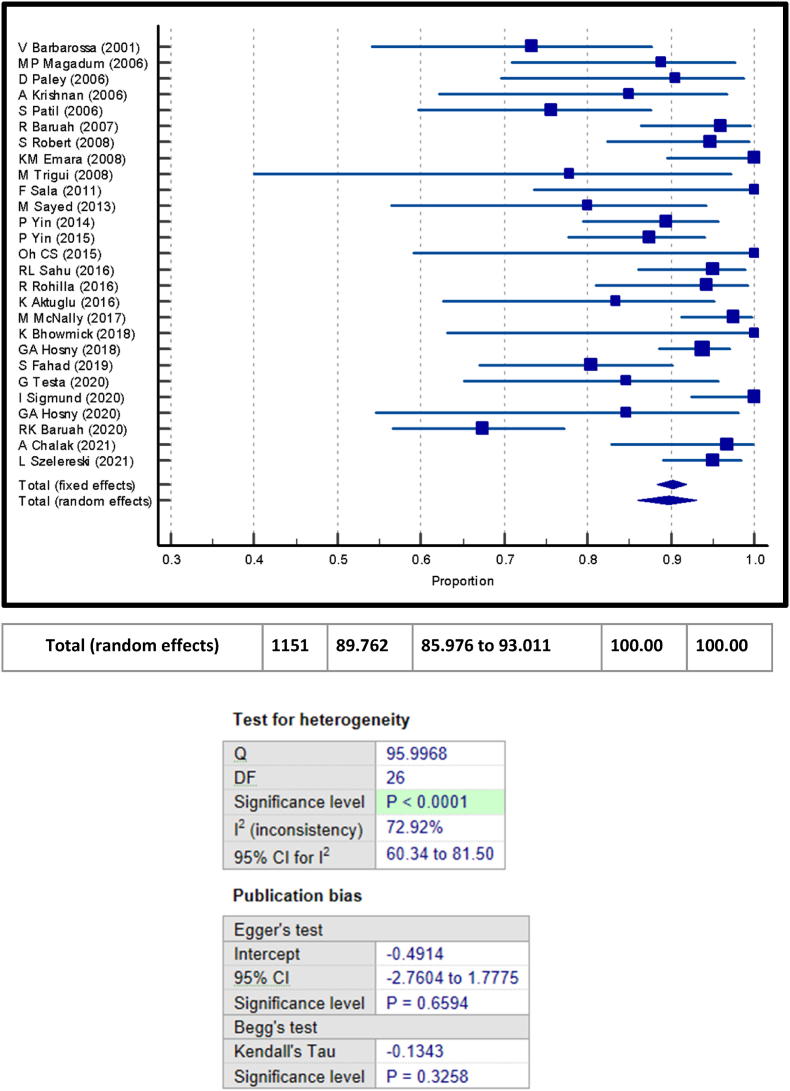
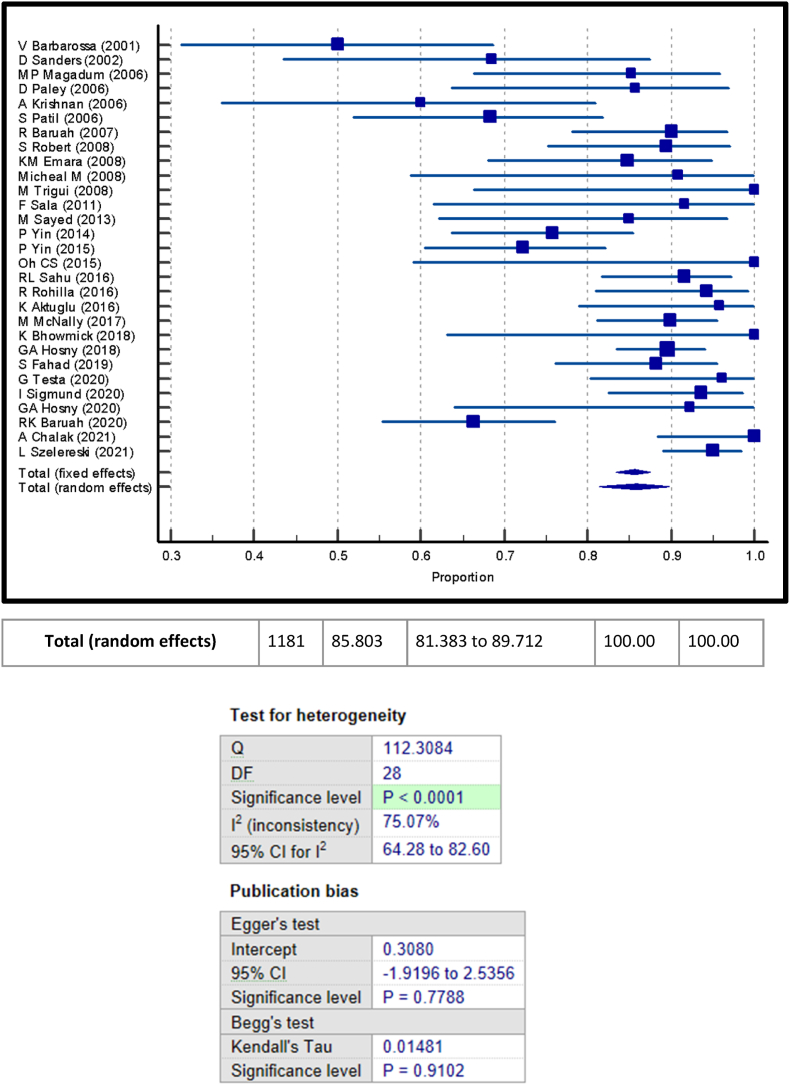
Total of 27 studies reported on the ASAMI Bone results in the Ilizarov group,4,7,15, 16, 17, 18, 19, 20, 21,23, 24, 25, 26, 27, 28, 29, 30, 31, 32,37, 38, 39, 40, 41,44,45 with a total of 1029 patients reported with excellent to good results among the 1170 total number of patients accounting for about 89.31% of patients. In the LRS group, all studies reported on the ASAMI Bone results with a total of 185 patients reported with excellent to good results among the 210 total number of patients accounting for about 88.3% of patients.4,7,33, 34, 35,42,43,46
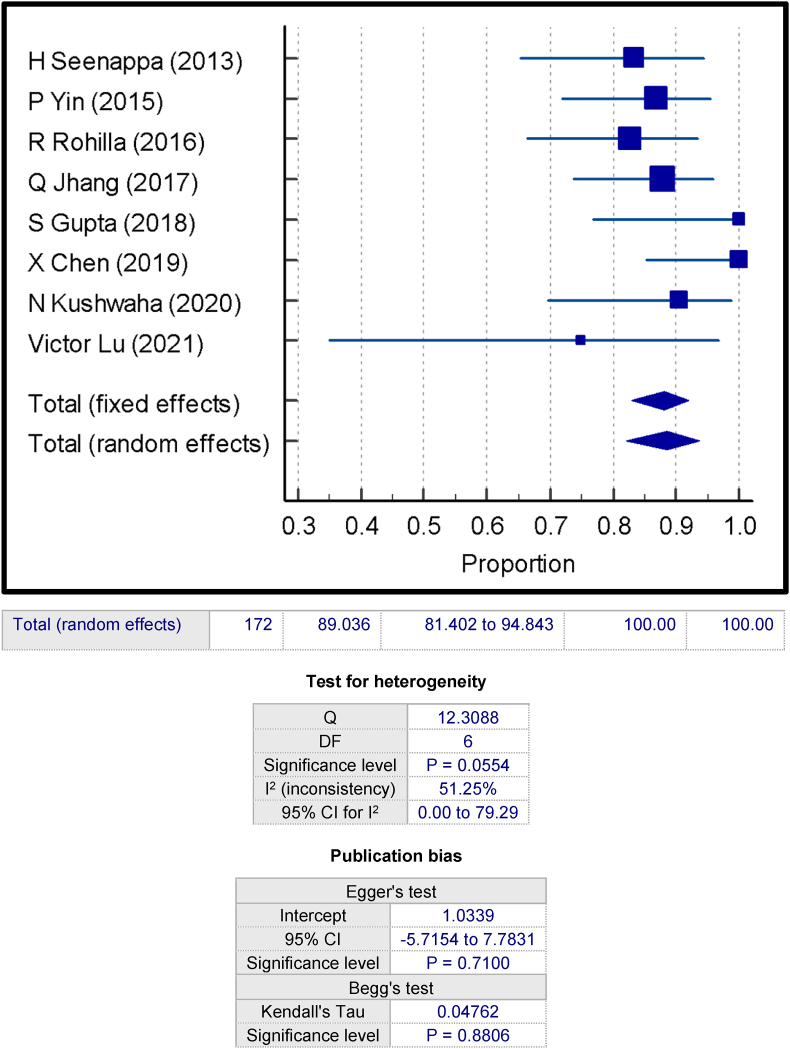
Total of 29 studies reported on the ASAMI Functional results in the Ilizarov group with a total of 1001 patients reported with excellent to good results among the 1181 total number of patients accounting for about 85.87% patients.4,7,15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32,36, 37, 38, 39, 40, 41,44,45 In the LRS group, a total of 7 studies reported on the ASAMI Functional results with a total of 171 patients reported with excellent to good results among the 210 total number of patients accounting for about 87.74% of patients.4,7,33,34,42,43,46
The results have been tabulated in Table 2, and the proportion meta-analysis is in Fig. 2, Fig. 3, Fig. 4, Fig. 5. Proportion meta-analysis for both bone and functional results showed significant level of test of heterogeneity in ilizarov group (p < 0.0001) compared to LRS group.
Fig. 2.
Proportion meta-analysis of ASAMI bone score - ilizarov.
Fig. 3.
Proportion meta-analysis of ASAMI Functional Score - Ilizarov.
Fig. 4.
Proportion meta-analysis of ASAMI bone score - LRS
Fig. 5.
Proportion meta-analysis of ASAMI Functional Score – LRS.
7.9. Complications
The complications noted were subgrouped into implant-related complications, adjacent joint-related complications, Nerve injuries, bone-related complications, Limb length discrepancy, nonunion, other infection, intractable pain, and Miscellaneous.
Of all the complications, implant related complications were most common in all studies and among both groups. Among the implant-related complications - Pin Tract Infection accounted for almost 90% and was the most common individual complication which almost all patients suffered during the postoperative period, which was managed conservatively by changing the dressing regularly, and few required further surgical management.4,7,15, 16, 17, 18, 19,21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37,39,41, 42, 43, 44,46
The 2nd most common complication noted was adjacent joint stiffness, managed by physiotherapy, and few requiring further surgical management.4,16, 17, 18, 19,21, 22, 23, 24, 25,27,28,31,33,36,37,39,42
All complications were noted and tabulated individually and as complications per patient in Table 2, Table 3 and a graphical representation in Fig. 6, Fig. 7.
Table 3.
Complications of Ilizarov and LRS group.
| ILIZAROV DATA | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Author (Year) | Implant Related Complications | Adjacent Joint Complications | Nerve Injuries | Bone Related Complications | LLD | Nonunion | Infection | Intractable Pain | Others |
| V Barbarossa (2001) | PTI - 1 | Stiffness – 15 | Dysesthesia - 3 | Refracture - 1 | LLD - 6 | Nonunion −4 | Intractable Pain - 2 | Mental Depression - 3 | |
| Axial Deviation - 13 | Amputation - 1 | ||||||||
| David W. Sanders (2002) | PTI - 10 | Stiffness – 3 | Nerve Palsy - 1 | LLD - 2 | Nonunion −1 | Leg Abscess - 1 | Osteopenia - 7 | ||
| Deformity - 3 | |||||||||
| S Patil (2006) | PTI - 41 Wire Break - 1 | Equinus Contracture −1 | Poor Regenerate - 3 | Amputation - 1 | Persistent Infection – 2 | DVT – 1 | |||
| Refracture - 2 | Chronic OM – 2 | ||||||||
| Fracture Of Regenerate - 1 | Septic Arthritis - 1 | ||||||||
| A Krishnan (2006) | PTI - 11 | Joint Stiffness – 11 | Refracture - 1 | LLD - 1 | Nonunion −1 Amputation - 1 | Intractable Pain - 3 | Severe Dystrophy – 7 | ||
| Angular Deformity – 1 | Delayed Consolidation – 2 | Weight Loss – 9 | |||||||
| Axial Deviation – 14 | Premature Consolidation - 1 | Depression - 3 | |||||||
| Edema – 5 | |||||||||
| MP Magadum (2006) | PTI – 21 Wire Loosening – 0 | Deformity – 2 | Refracture - 0 | Nonunion −1 Amputation - 1 | |||||
| Dror Paley (2006) | PTI - 27 Pin Breakage - 1 | Knee Effusion - 1 | Nerve Palsy - 2 | Premature Consolidation - 4 | LLD - 1 | Infection −7 | |||
| Axial Deviation −13 | Delayed Consolidation - 2 | ||||||||
| Ranjit Baruah (2007) | PTI – 5 | Equinus Deformity - 2 | Delayed Consolidation - 7 | Nonunion −4 | Aneurysm - 1 Interposition Of Soft Tissue - 6 | ||||
| Early Consolidation - 1 | |||||||||
| Refracture - 2 | |||||||||
| Hyporegenerate - 4 | |||||||||
| Khaled M Emara (2008) | PTI -3 | Joint Stiffness - 2 | Unplanned Surgery - 2 | ||||||
| Pin Loosening −1 | |||||||||
| Broken Nail – 2 (In IMN Group) | |||||||||
| S. Robert Rozbruch (2008) | Nonunion - 11 Amputation - 2 |
Infection - 11 | |||||||
| Michael D. McKee (2008) | PTI - 4 | Osteoarthritis – 3 | Nerve Palsy - 2 | Translation - 1 | LLD - 2 | Amputation- 1 | Osteomyelitis - 2 | Intractable Pain - 1 | |
| Ankle fusion – 1 | |||||||||
| Deformity - 2 | Refracture - 1 | Cellulitis - 2 | |||||||
| Angular deformity - 4 | |||||||||
| M. Trigui (2008) | Axial Deviation - 4 | LLD - 6 | Nonunion −0 | Infection - 0 | |||||
| Francesco Sala (2011) | PTI - 10 | Equinus - 3 | LLD - 2 | Pseudoaneurysm - 1 | |||||
| M Sayed (2013) | PTI – 16 | Joint Stiffness – 12 | Refracture - 1 | LLD - 4 | Nonunion −2 | Persistent Infection – 1 | Intractable Pain - 3 | Depression - 3 | |
| Pin Loosening – 2 | Deformity – 8 | ||||||||
| Frame Adjustment - 2 | Edema – 5 | ||||||||
| P Yin (2014) | Nonunion −0 | Infection – 0 | |||||||
| Chang Seon Oh (2015) | PTI - 1 | Nonunion −1 | Recurrence Of Tumor - 1 | ||||||
| Peng Yin (2015) | PTI - 46 Wire loosening - 4 | Axial deviation - 20 | Refracture - 2 | LLD - 2 | Nonunion −7 | Local inflammation - 66 | |||
| Ramji Lal Sahu (2016) | PTI - 60 | Equinus - 4 | Soft Tissue Dystrophy - 3 | ||||||
| Angular Deformity - 2 | |||||||||
| Kemal Aktuglu (2016) | PTI - 17 | Stiffness - 5 Equinus - 3 | Angulation - 5 | LLD - 6 | Nonunion −1 | Skin Tethered - 7 Soft Tissue Injury – 11 | |||
| R Rohilla (2016) | PTI - 21 | Joint Stiffness −14 | LLD - 3 | ||||||
| Broken Screw −2 | Angular Deformity - 4 | ||||||||
| Martin Mcnally (2017) | PTI – 3 Broken Wire - 4 | Refracture - 8 | LLD -3 | ||||||
| Gamal Ahmed Hosny (2018) | PTI - 11 | Deformity - 3 | Nerve Palsy - 2 | Lengthening - 2 | LLD - 4 | Nonunion −3 | NS | ||
| K Bhowmick (2018) | PTI –1 | Deformity – 2 Axial Deviation −1 | Refracture - 1 | Nonunion −2 | Soft Tissue Infection – 1 | ||||
| S Fahad (2019) | PTI – 9 | LLD - 7 | Nonunion −2 | Re- Infection – 1 | |||||
| Pin Loosening – 2 | Amputation - 1 | Leg Abcess −1 | |||||||
| Screw Broken −1 | Septic Arthritis - 1 | ||||||||
| R K Baruah (2020) | PTI - 23 | Equinus - 3 | Nerve Palsy - 2 | Delayed Consolidation - 10 | Nonunion −2 | False Aneurysm −1 | |||
| Soft Tissue Interposition - 10 | |||||||||
| G Testa (2020) | PTI – 3 | ||||||||
| K-Wire Break −1 | |||||||||
| Screw Break −2 | |||||||||
| I Sigmund (2020) | PTI – 22 Pin Removal – 1 | Deformity – 0 | Premature Consolidation - 2 | LLD - 0 | Painful Thethred Skin −1 | ||||
| Gamal Ahmed Hosny (2020) | PTI – 9 | Joint Stiffness – 2 | Delayed Union - 1 | LLD - 3 | |||||
| Angular Deformity – 2 | Refracture - 1 | ||||||||
| A Chalak (2021) | PTI - 5 | Soft Tissue Invagination At The Docking Site - 2 | |||||||
| Lukasz Szelereski (2021) | Refracture - 5 | ||||||||
| LRS DATA | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Author (Year) | Implant Related Complications | Adjacent Joint Complications | Nerve Injuries | Bone Related Complications | LLD | Nonunion | Infection | Intractable Pain | Others |
| Hiranaya Seenappa (2013) | PTI - 22 | Joint Stiffness - 13 | Refracture - 1 | LLD - 4 | |||||
| Pin Loosening - 8 | Angular Deformity - 2 | ||||||||
| Peng Yin (2015) | PTI - 24 | Axial deviation - 12 | Refracture - 2 (in total) | LLD - 2 | Nonunion −5 | Local inflammation: 66 (in total) | |||
| Wire loosening - 4 | |||||||||
| R Rohilla (2016) | PTI - 30 | Joint Stiffness - 8 | LLD - 6 | ||||||
| Pin Loosening - 1 | Angular Deformity - 3 | ||||||||
| Qun Jhang (2017) | PTI - 23 | Joint Stiffness - 14 | Refracture - 1 | Nonunion −5 | Bone grafting - 1 | ||||
| Pin Loosening - 2 | Angular Deformity - 3 | ||||||||
| S Gupta (2018) | PTI - 5 | ||||||||
| Xun Chen (2019) | PTI - 5 | ||||||||
| N Kushwaha (2020) | PTI - 4 | Refracture - 1 | Persistent Infection – 5 | ||||||
| Victor Lu (2021) | PTI - 5 | Osteoarthritis - 1 | Nonunion −2 | Osteomyelitis - 2 | Intractable Pain - 1 | Myositis Ossificans - 1 | |||
B/K, Below Knee; DVT, Deep Vein thrombosis; LLD, Limb Length Discrepancy; OM, Osteomyelitis, PTI – Pin tract infection.
Fig. 6.
Complication per patient – Ilizarov.
Fig. 7.
Complication per patient - LRS.
8. Discussion
Long bone defects with no union that may or may not be segmental require appropriate treatment for adequate outcomes.47, 48, 49 Distraction osteogenesis by Ilizarov or monorail fixator, masquelet technique, and vascularized fibular grafting are currently the methods to treat segmental long bone defects.6, 7, 8 The use of monorail fixators has risen in the last decade and is employed in many cases of nonunions. The Ilizarov fixators are the mainstay of treatment. The bone transport can be performed with both systems. However, both the modes of fixation have some biomechanical differences. Ilizarov due to its 3 dimensional fixation with tensioned wire/pins provides uniform loading where as LRS due to its uniplanar fixation has a cantilever effect at fracture site. The current review focuses on both LRS and Ilizarov fixators in the nonunion of long bones separately.
In our study, we found that the overall complication rate with the use of Ilizarov was 89.4%. The most common complication was pin tract infection. The rest of the complications were joint stiffness, angular deformity, wire breakage, nonunion, refracture, amputation. Multiple studies have highlighted the advantages, such as better bone and functional results with a low rate of refracture, infectious recurrence, and amputation.49, 50, 51, 52 The ring fixator with multiple rings and wires is prone to pin tract infection and pin breakage. The study noted pin tract related complication as most common.53,54 The rate of refracture and amputation were 2.05% and 0.65%, respectively, in the Ilizarov group, which was less than 4% and 4% reported by Ying P et al.9 and 5% and 2.9% reported by Papakostidis et al.55 The incidence of deformity of long bones in LRS was 7.4%. The analysis showed most common complication was pin tract infection, with an incidence of nearly 90% in both treatment arms, which was similar to that reported by Papakostidis et al. and Ying P et al.9,55, 56
The average external fixator time was 8.52 months with Ilizarov and 7.98 months with LRS, both being lower than that reported in the meta-analysis on Ilizarov fixator in segmental long bone defect by Ying P et al., which was 10.69 months.9 The external fixator index is the time required to cover the bone gap present. EFI in Ilizarov and LRS group was respectively 54.46 days/cm and 43.64 days/cm, which was less than that reported in the study by Ying P et al.9 Treatment with LRS appears to have less fixator time which may increase compliance in the long term.
Outcome assessment was done by ASAMI functional score in all of the studies on Ilizarov and seven studies on LRS fixator, whereas ASAMI bone score was used in 27 studies on Ilizarov and eight studies on LRS. In the Ilizarov group, 85.87% reported excellent to good results as compared to the LRS group, where 87.74% reported excellent to good results on ASAMI functional scoring showing the use of both Ilizarov and LRS have a comparable functional outcome in patients. Similar was the case with the ASAMI bone score, where both groups had similar results, 89.31%, and 88.3% had excellent to a good outcome in Ilizarov and LRS groups, respectively.
To our best knowledge, this is the first systematic review involving both Ilizarov and LRS fixator for long bone nonunion, where we studied 1219 patients treated with Ilizarov fixator and 282 patients with LRS fixator. Ying P et al., in their review, looked at Ilizarov fixator in 590 patients9
Overall, the treatment arms were similar in terms of functional and bone outcomes. Pin tract infection was the most common complication in both groups. However, joint stiffness was more frequent in the LRS group, and deformity was more common with the Ilizarov fixator. So clinically, both Ilizarov and LRS fixator yield similar results in the management of long bone nonunion.
Our study does have its limitations. The review included a mixture of study designs. Ideally, one would survive for randomized controlled trials for accurate results. The literature currently lacks such studies. Second, there were very few studies comparing Ilizarov vs LRS methods. Such comparative studies are the need of the day. Third, even though a thorough search was conducted, a few studies might be missed. Fourth, the protocol for this systematic review was not preregistered or published.
9. Conclusion
The review was conducted to understand the scenario of nonunion in long bones. We found that both Ilizarov and LRS fixator yield similar clinical results for the treatment of long bones nonunion. Pin tract infection is found to be the most common complication followed by adjacent joint stiffness and deformity. In our review we observed that both external fixator time and index were lower in LRS. Further RCT are required comparing Ilizarov and LRS fixators to effectively comment upon the superiority of the implants.
Consent to participants
Not Applicable.
Consent to publish
All authors have read the final prepared draft of the manuscript and approve this version, in its current format if considered further for publication.
Financial support and sponsorship
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Availability of data and materials
All included studies used in this retrospective study are available online. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. Data regarding this study is not available in any electronic databases.
Informed consent
Not Applicable.
Ethics approval
Approval from the institutional ethics committee was not required for this review article.
Authors contribution
V.M − Conceptualization, project administration Planning of study, literature search, writing the manuscript, quality assessment of the included studies.
B.S.R - Data curation, outcome assessment, manuscript preparation.
B.B – Formal analysis, Data management, manuscript preparation.
A.R- Methodology, Literature search, writing the manuscript, quality assessment of the included studies.
M.D - Quality assessment of the included studies, writing and revising the manuscript, Correspondence.
A.K.S.G - Data management, outcome assessment, revising the manuscript.
Declaration of competing interest
All authors declare that they do not have any competing interest, concerning this research, authorship, and/or publication of this article.
Acknowledgement
None.
Abbreviation
- LRS
Limb Reconstruction System
- MPSP
Mean previous surgical procedures
- ASAMI
The Association For The Study And Application Of Methods Of Ilizarov
- E/G/F/P/F
Excellent/Good/Fair/Poor/Failure
- EFT
External fixation time
- EFI
External fixation index
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- ASR
Acute Shortening and Relengthening
- BT
Bone Transport
- MCMS
Modified Coleman Methodology score
- RCT
Randomized Control Trial
- PTI
Pin tract infection
Contributor Information
Vikas Maheshwari, Email: 111vikasmaheshwari@gmail.com.
Balgovind S. Raja, Email: balgovindsraja@gmail.com.
Bom Bahadur, Email: iambbk001@gmail.com.
Anil Regmi, Email: regmiaanil@gmail.com.
Mohit Dhingra, Email: modisbanu77@gmail.com.
Aditya K.S. Gowda, Email: adityajr.orth@aiimsrishikesh.edu.in.
References
- 1.Nicholson J., Makaram N., Simpson A., Keating J. Fracture nonunion in long bones: a literature review of risk factors and surgical management. Injury. 2021;52 doi: 10.1016/j.injury.2020.11.029. S3–11. [DOI] [PubMed] [Google Scholar]
- 2.Stewart S. Fracture non-union: a review of clinical challenges and future research needs. Malays Orthop J. 2019;13(2):1–10. doi: 10.5704/MOJ.1907.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ekegren C.L., Edwards E.R., De Steiger R., Gabbe B.J. Incidence, costs and predictors of non-union, delayed union and mal-union following long bone fracture. Int J Environ Res Publ Health. 2018;15(12):2845. doi: 10.3390/ijerph15122845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yin P., Zhang L., Li T., et al. Infected nonunion of tibia and femur treated by bone transport. J Orthop Surg. 2015;10(1):49. doi: 10.1186/s13018-015-0189-5. 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El-Rosasy M., Mahmoud A., El-Gebaly O., Lashin A., Rodriguez-Collazo E. Debridement technique and dead space management for infected non-union of the tibia. Int J Orthoplast Surg. 2019;2(1):29+. [Google Scholar]
- 6.Gowtham Ram P. Madras Medical College; Chennai: 2019. Prospective Analysis of Outcome in the Management of Post Traumatic Bone Defects in Tibia by Masquelet Technique. [Google Scholar]
- 7.Rohilla R., Wadhwani J., Devgan A., Singh R., Khanna M. Prospective randomised comparison of ring versus rail fixator in infected gap nonunion of tibia treated with distraction osteogenesis. Bone Jt J. 2016;98-B(10):1399–1405. doi: 10.1302/0301-620X.98B10.37946. [DOI] [PubMed] [Google Scholar]
- 8.Pal C.P., Kumar H., Kumar D., Dinkar K.S., Mittal V., Singh N.K. Comparative study of the results of compound tibial shaft fractures treated by Ilizarov ring fixators and limb reconstruction system fixators. Chin J Traumatol. 2015;18(6):347–351. doi: 10.1016/j.cjtee.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 9.Yin P., Ji Q., Li T., et al. A systematic review and meta-analysis of ilizarov methods in the treatment of infected nonunion of tibia and femur. PLoS One. 2015;10(11) doi: 10.1371/journal.pone.0141973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 11.Paley D., Catagni M.A., Argnani F., Villa A., Bijnedetti G.B., Cattaneo R. Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res. 1989;241:146–165. [PubMed] [Google Scholar]
- 12.Cucherat M, Boissel JP, Leizorovicz A, Haugh MC. EasyMA (1997) a program for the meta-analysis of clinical trials. Comput Methods Progr Biomed, 53(3):187–190. [DOI] [PubMed]
- 13.Hozo S.P., Djulbegovic B., Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;20(5):13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jakobsen R.B., Engebretsen L., Slauterbeck J.R. An analysis of the quality of cartilage repair studies. JBJS. 2005;87(10):2232–2239. doi: 10.2106/JBJS.D.02904. [DOI] [PubMed] [Google Scholar]
- 15.Sigmund I.K., Ferguson J., Govaert G.A.M., Stubbs D., McNally M.A. Comparison of ilizarov bifocal, acute shortening and relengthening with bone transport in the treatment of infected, segmental defects of the tibia. J Clin Med. 2020;9(2):279. doi: 10.3390/jcm9020279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barbarossa V., Matković B.R., Vucić N., Bielen M., Gluhinić M. Treatment of osteomyelitis and infected non-union of the femur by a modified Ilizarov technique: follow-up study. Croat Med J. 2001;42(6):634–641. [PubMed] [Google Scholar]
- 17.Patil S., Montgomery R. Management of complex tibial and femoral nonunion using the Ilizarov technique, and its cost implications. J Bone Joint Surg Br. 2006;88(7):928–932. doi: 10.1302/0301-620X.88B7.17639. [DOI] [PubMed] [Google Scholar]
- 18.Krishnan A., Pamecha C., Patwa J.J. Modified Ilizarov technique for infected nonunion of the femur: the principle of distraction-compression osteogenesis. J Orthop Surg Hong Kong. 2006;14(3):265–272. doi: 10.1177/230949900601400307. [DOI] [PubMed] [Google Scholar]
- 19.Magadum M., Yadav C.B., Phaneesha M., Ramesh L. Acute compression and lengthening by the ilizarov technique for infected nonunion of the tibia with large bone defects. J Orthop Surg. 2006;14(3):273–279. doi: 10.1177/230949900601400308. [DOI] [PubMed] [Google Scholar]
- 20.Rozbruch S.R., Pugsley J.S., Fragomen A.T., Ilizarov S. Repair of tibial nonunions and bone defects with the Taylor Spatial Frame. J Orthop Trauma. 2008;22(2):88–95. doi: 10.1097/BOT.0b013e318162ab49. [DOI] [PubMed] [Google Scholar]
- 21.Sala F., Thabet A.M., Castelli F., et al. Bone transport for postinfectious segmental tibial bone defects with a combined Ilizarov/taylor spatial frame technique. J Orthop Trauma. 2011;25(3):162–168. doi: 10.1097/BOT.0b013e3181e5e160. [DOI] [PubMed] [Google Scholar]
- 22.McKee M.D., Yoo D.J., Zdero R., et al. Combined single-stage osseous and soft tissue reconstruction of the tibia with the Ilizarov method and tissue transfer. J Orthop Trauma. 2008;22(3):183–189. doi: 10.1097/BOT.0b013e3181678a64. [DOI] [PubMed] [Google Scholar]
- 23.El-Sayed M.M.H., Gaballah S., Hosny G., Hafez K. Management of infected nonunion of the femur in adults using the Ilizarov technique. Eur Orthop Traumatol. 2014;5(3):285–291. [Google Scholar]
- 24.Sahu R.L., Ranjan R. Treatment of complex nonunion of the shaft of the tibia using Ilizarov technique and its functional outcome. Niger Med J J Niger Med Assoc. 2016;57(2):129–133. doi: 10.4103/0300-1652.182076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aktuglu K., Günay H., Alakbarov J. Monofocal bone transport technique for bone defects greater than 5 cm in tibia: our experience in a case series of 24 patients. Injury. 2016;47(suppl 6) doi: 10.1016/S0020-1383(16)30838-5. S40–6. [DOI] [PubMed] [Google Scholar]
- 26.McNally M., Ferguson J., Kugan R., Stubbs D. Ilizarov treatment protocols in the management of infected nonunion of the tibia. J Orthop Trauma. 2017;31(Suppl 5):S47–S54. doi: 10.1097/BOT.0000000000000987. [DOI] [PubMed] [Google Scholar]
- 27.Hosny G.A., Ahmed A.S.A.A., Hussein M.A.E. Clinical outcomes with the corticotomy-first technique associated with the Ilizarov method for the management of the septic long bones non-union. Int Orthop. 2018;42(12):2933–2939. doi: 10.1007/s00264-018-3924-9. [DOI] [PubMed] [Google Scholar]
- 28.Bhowmick K., Boopalan P.R.J.V.C., Gunasekeran C., Livingston A., Jepegnanam T.S. Management of chronic infected intra-articular fractures of the proximal tibia with ilizarov ring fixation. J Knee Surg. 2020;33(2):213–222. doi: 10.1055/s-0038-1677512. [DOI] [PubMed] [Google Scholar]
- 29.Fahad S., Habib A., Awais M., Umer M., Rashid H. Infected non-union of tibia treated with ilizarov external fixator: our experience. Malays Orthop J. 2019;13(1):36–41. doi: 10.5704/MOJ.1903.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Testa G., Vescio A., Aloj D.C., et al. Treatment of infected tibial non-unions with ilizarov technique: a case series. J Clin Med. 2020;9(5):1352. doi: 10.3390/jcm9051352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baruah R., Baruah J., Shyam-Sunder S. Acute shortening and Re-lengthening (ASRL) in infected non-union of tibia - advantages revisited. Malays Orthop J. 2020;14(2):47–56. doi: 10.5704/MOJ.2007.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hosny G.A., Ahmed A.S.A.A. Paediatric infected femoral nonunion; mid-term results of a rare problem with a single-stage treatment and up to eleven and half years follow-up. Int Orthop. 2020;44(3):503–509. doi: 10.1007/s00264-019-04464-1. [DOI] [PubMed] [Google Scholar]
- 33.Singh S., Shetty S., Kale S., Singh P., Ghodke A. A Novel technique of three-ring Ilizarov fixator frame in gap non-union of tibia. J Clin Orthop Trauma. 2021;23 doi: 10.1016/j.jcot.2021.101639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seenappa H.K., Shukla M.K., Narasimhaiah M. Management of complex long bone nonunions using limb reconstruction system. Indian J Orthop. 2013;47(6):602–607. doi: 10.4103/0019-5413.121590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen X., Zhang W., Yu Z., Wang Y., Zhang S., Song T. Application of bone transport with unilateral external fixator combined with locked plate internal fixation in treatment of infected tibial nonunion. Chin J Reparative Reconstr Surg. 2019;33(3):328–331. doi: 10.7507/1002-1892.201811024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lu V., Zhang J., Zhou A., Krkovic M. Management of post-traumatic femoral defects with a monorail external fixator over an intramedullary nail. Eur J Orthop Surg Traumatol Orthop Traumatol. 2022;32(6):1119–1126. doi: 10.1007/s00590-021-03082-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sanders D.W., Galpin R.D., Hosseini M., MacLeod M.D. Morbidity resulting from the treatment of tibial nonunion with the Ilizarov frame. Can J Surg J Can Chir. 2002;45(3):196–200. [PMC free article] [PubMed] [Google Scholar]
- 38.Baruah R.K. Ilizarov methodology for infected non union of the Tibia: classic circular transfixion wire assembly vs. hybrid assembly. Indian J Orthop. 2007;41(3):198–203. doi: 10.4103/0019-5413.33682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Trigui M., Ayadi K., Ellouze Z., Gdoura F., Zribi M., Keskes H. Treatment of bone loss in limbs by bone transport] Rev Chir Orthop Reparatrice Appar Mot. 2008;94(7):628–634. doi: 10.1016/j.rco.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 40.Emara K.M., Allam M.F. Ilizarov external fixation and then nailing in management of infected nonunions of the tibial shaft. J Trauma. 2008;65(3):685–691. doi: 10.1097/TA.0b013e3181569ecc. [DOI] [PubMed] [Google Scholar]
- 41.Yin P., Zhang Q., Mao Z., Li T., Zhang L., Tang P. The treatment of infected tibial nonunion by bone transport using the Ilizarov external fixator and a systematic review of infected tibial nonunion treated by Ilizarov methods. Acta Orthop Belg. 2014;80(3):426–435. [PubMed] [Google Scholar]
- 42.Oh C.S., Jung S.T., Cho Y.J., Ahn Y.S., Na B.R. Bone transport for reconstruction in benign bone tumors. Clin Orthop Surg. 2015;7(2):248–253. doi: 10.4055/cios.2015.7.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang Q., Zhang W., Zhang Z., et al. Femoral nonunion with segmental bone defect treated by distraction osteogenesis with monolateral external fixation. J Orthop Surg. 2017;25;12(1):183. doi: 10.1186/s13018-017-0684-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gupta S., Malhotra A., Mittal N., Garg S.K., Jindal R., Kansay R. The management of infected nonunion of tibia with a segmental defect using simultaneous fixation with a monorail fixator and a locked plate. Bone Jt J. 2018;100-B(8):1094–1099. doi: 10.1302/0301-620X.100B8.BJJ-2017-1442.R1. [DOI] [PubMed] [Google Scholar]
- 45.Paley D., Lamm B.M., Katsenis D., Bhave A., Herzenberg J.E. Treatment of malunion and nonunion at the site of an ankle fusion with the Ilizarov apparatus. Surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1 Pt 1):119–134. doi: 10.2106/JBJS.E.00862. [DOI] [PubMed] [Google Scholar]
- 46.Ł Szelerski, Pajchert Kozłowska A., Żarek S., et al. A new criterion for assessing Ilizarov treatment outcomes in nonunion of the tibia. Arch Orthop Trauma Surg. 2021;141(5):879–889. doi: 10.1007/s00402-020-03571-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Singh Kushwaha N., Mahendra M., Kumar DrS., Sinha S., Singh A., Sharma V. Infected non union of tibia managed by limb reconstruction system- A prospective cohort study. J Clin Diagn Res. 2020;1:14. [Google Scholar]
- 48.Lasanianos N.G., Kanakaris N.K., Giannoudis P.V. Current management of long bone large segmental defects. Orthop Traumatol. 2010;24(2):149–163. [Google Scholar]
- 49.Kadhim M., Holmes L., Gesheff M.G., Conway J.D. Treatment options for nonunion with segmental bone defects: systematic review and quantitative evidence synthesis. J Orthop Trauma. 2017;31(2):111–119. doi: 10.1097/BOT.0000000000000700. [DOI] [PubMed] [Google Scholar]
- 50.Giannoudis P.V., Harwood P.J., Tosounidis T., Kanakaris N.K. Restoration of long bone defects treated with the induced membrane technique: protocol and outcomes. Injury. 2016;47:S53–S61. doi: 10.1016/S0020-1383(16)30840-3. [DOI] [PubMed] [Google Scholar]
- 51.Bumbaširević M., Tomić S., Lešić A., Milošević I., Atkinson H.D.E. War-related infected tibial nonunion with bone and soft-tissue loss treated with bone transport using the Ilizarov method. Arch Orthop Trauma Surg. 2010;130(6):739–749. doi: 10.1007/s00402-009-1014-6. [DOI] [PubMed] [Google Scholar]
- 52.Maini L., Chadha M., Vishwanath J., Kapoor S., Mehtani A., Dhaon B.K. The Ilizarov method in infected nonunion of fractures. Injury. 2000;31(7):509–517. doi: 10.1016/s0020-1383(00)00036-x. [DOI] [PubMed] [Google Scholar]
- 53.Aktuglu K., Erol K., Vahabi A. Ilizarov bone transport and treatment of critical-sized tibial bone defects: a narrative review. J Orthop Traumatol. 2019;20(1):22. doi: 10.1186/s10195-019-0527-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rogers L.C., Bevilacqua N.J., Frykberg R.G., Armstrong D.G. Predictors of postoperative complications of ilizarov external ring fixators in the foot and ankle. J Foot Ankle Surg. 2007;46(5):372–375. doi: 10.1053/j.jfas.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 55.Papakostidis C., Bhandari M., Giannoudis P.V. Distraction osteogenesis in the treatment of long bone defects of the lower limbs. Bone Jt J. 2013;95-B(12):1673–1680. doi: 10.1302/0301-620X.95B12.32385. [DOI] [PubMed] [Google Scholar]
- 56.Khan M.S., Rashid H., Umer M., Qadir I., Hafeez K., Iqbal A. Salvage of infected non-union of the tibia with an ilizarov ring fixator. J Orthop Surg. 2015;23(1):52–55. doi: 10.1177/230949901502300112. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All included studies used in this retrospective study are available online. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. Data regarding this study is not available in any electronic databases.