Abstract
Background
Thiazolidinediones, commonly used antidiabetic medications, have been associated with an increased risk of development of diabetic macular oedema and increased vascular endothelial cell permeability. Macular neovascularisation in age-related macular degeneration (AMD) and associated fluid leakage may be influenced by thiazolidinediones. This study aims to determine the association between thiazolidinedione usage and retinal morphological outcomes or visual acuity (VA) in patients treated with bevacizumab or ranibizumab for neovascular AMD (nAMD).
Methods
Secondary analysis of data from the Comparison of Age-related Macular Degeneration Treatments Trials. Participant self-reported diabetes status and thiazolidinedione usage at baseline. VA, intraretinal, subretinal and subretinal pigment epithelium fluid, and foveal thickness of retinal layers were evaluated at baseline and during 2-year follow-up. Comparisons of outcomes between thiazolidinedione usage groups were adjusted by macular neovascularisation lesion type in multivariable regression models.
Results
Patients taking thiazolidinedione (n=30) had lower adjusted mean VA score at baseline (difference −6.2 letters; p=0.02), greater proportion with intraretinal fluid (IRF) at year 2 (75% vs 50%, adjusted OR 2.8; p=0.04), greater mean decrease in subretinal tissue complex thickness from baseline at year 1 (difference −75.1 um; p=0.02) and greater mean decrease in subretinal thickness at year 1 (difference −41.9 um; p=0.001) and year 2 (difference −43.3 um; p=0.001).
Conclusions
In this exploratory analysis, patients with diabetes taking thiazolidinediones and treated with bevacizumab or ranibizumab for nAMD had worse baseline mean VA, greater reductions in subretinal and subretinal tissue complex thickness from baseline, and greater proportions with IRF comparing to patients not taking thiazolidinediones.
Trial registration number
INTRODUCTION
Thiazolidinediones, such as rosiglitazone and pioglitazone, improve glycaemic control in patients with diabetes through activation of the gamma isoform of the peroxisome proliferator-activated nuclear receptor (PPARγ), which improves insulin sensitivity and alters transcription of genes regulating systemic glucose levels.1 PPARγ activity has been observed in vascular endothelial cells and is thought to increase vascular endothelial permeability.1 These drugs produce numerous physiologic effects such as increasing endothelial cell permeability,1 increasing serum VEGF levels, reducing suppressor-of-cytokine-signalling-3 (SOCS3), tumour necrosis factor alpha (TNF-α) and C reactive protein (CRP) levels, upregulating insulin-growth-factor-binding-protein-3 (IGFBP-3) and inhibiting diabetes-induced apoptosis in retinal neurons.2–4 Considering these myriad effects, there are multiple potential pathways by which thiazolidinediones could prove either beneficial or detrimental to the retina of people affected by diabetes or other types of neovascular disease.
An association between thiazolidinedione use and an increased risk of diabetic macular oedema has been reported.5 6 It is not known whether the off-target effects of thiazolidinediones might influence neovascular conditions other than diabetic retinopathy such as neovascular age-related macular degeneration (nAMD). This information would be important given the general prevalence of diabetes and its association with nAMD, which has been consistently observed in cross-sectional studies.7 Potential effects of thiazolidinediones on AMD have been studied with in vitro or in situ models but not in patients.8 Therefore, we assessed the association of thiazolidinedione usage with retinal morphology and visual acuity (VA) in participants with diabetes who received antivascular endothelial growth factor (anti-VEGF) treatment for nAMD in the Comparison of Age-Related Macular Degeneration Treatments Trials (CATT).
METHODS
This study is a secondary analysis of data from a cohort within a randomised clinical trialThe trial was conducted in accordance with the tenets of the Declaration of Helsinki and the Health Insurance Portability and Accountability Act. Detailed descriptions of the design and methods of the CATT are provided in previous reports.5
We use the term nAMD so as to include retinal angiomatous proliferation (type 3 macular neovascularisation, characterised by intraretinal neovascularisation), in addition to types 1 and 2 macular neovascularisation (defined by the presence of choroidal neovascularisation) in place of choroidal neovascularisation, which was used in previous CATT reports.9 Macular atrophy is used in place of geographic atrophy to describe areas of well-circumscribed retinal pigment epithelium (RPE) atrophy.10 CATT enrolment criteria were age of 50 years or older, treatment-na’fve, active nAMD in the study eye with absence of foveal macular atrophy, and study eye VA of 20/25–20/320. The nAMD activity was determined by leakage on fluorescein angiography and fluid within or beneath the retina or beneath the RPE on time-domain optical coherence tomography (OCT). Baseline medical history and medication use were self-reported by the patient. Only patients reporting a diagnosis of diabetes mellitus were included in this analysis.
Masked, certified readers at the Duke University OCT Reading Center independently evaluated OCT scans for the presence and location (foveal vs extrafoveal) of intraretinal fluid (IRF), subretinal fluid (SRF) and sub-RPE fluid. Thickness of retinal layers at the foveal centre were measured. Characteristics of macular neovascularisation such as lesion type and area were determined based on fundus photographs and fluorescein angiogram by readers in the reading centre. A senior reader resolved discrepancies between readers.
Baseline participant characteristics including age, gender, smoking status, hypertension and macular neovascularisation lesion characteristics were compared between participants taking vs not taking thiazolidinediones. Proportions with fluid, mean thickness of retinal layers and mean VA (ETDRS letters) at the baseline, year 1 and year 2 visits were compared between patients taking vs not taking thiazolidinediones and adjusted by baseline macular neovascularisation lesion type in logistic regression models for binary outcomes and linear regression models for continuous outcomes. Statistical analysis was performed with SAS V.9.4 (SAS Institute) and R (R Foundation for Statistical Computing, Vienna, Austria). Two-sided p values <0.05 were considered statistically significant.
RESULTS
Among 1185 participants in the CATT, 207 (17.5%) had diabetes at baseline and 30 (14.5%) of them were taking thiazolidinediones. Baseline demographic and macular neovascularisation lesion characteristics were similar between participants taking vs not taking thiazolidinediones (all p≤0.12; table 1). Participants taking thiazolidinediones had lower baseline VA score (55.2 vs 61.4 letters, p=0.02), and the difference remained significant after adjustment by macular neovascularisation lesion type (mean difference −6.2 letters; 95% CI (−11.2 to −0.8); p=0.02). Among 112 participants assigned anti-VEGF treatment as-needed, those taking (N=22) and not taking thiazolidinediones (N=90) received a similar mean number of injections through year 1 (6.1 vs 6.9; p=0.36) and year 2 (10.1 vs 11.8; p=0.30).
Table 1.
Baseline demographic and ocular characteristics in patients with and without baseline thiazolidinedione use
| Baseline characteristics | Thiazolidinedione usage at baseline | P value* | |
|---|---|---|---|
| No (N=177) | Yes (N=30) | ||
| Age (years), mean (SE) | 77.6 (0.5) | 77.9 (1.3) | 0.81 |
| Gender, female (%) | 88 (53.0) | 16 (61.5) | 0.42 |
| Hypertension (%) | 133 (80.1) | 23 (88.5) | 0.42 |
| Cigarette smoking | 0.53 | ||
| Never | 71 (42.8) | 14 (53.8) | |
| Quit | 83 (50.0) | 11 (42.3) | |
| Current | 12 (7.2) | 1 (3.8) | |
| Area (disc area) of macular neovascularisation, mean (SE) | 1.5 (0.1) | 2.1 (0.4) | 0.13 |
| Presence of retinal angiomatous proliferation, n (%) | 19 (10.7) | 4 (13.3) | 0.75 |
| Macular neovascularisation type, n (%) | 0.33 | ||
| Predominantly or minimally classic | 58 (33.3) | 7 (24.1) | |
| Occult only | 116 (66.7) | 22 (75.9) | |
| IRF presence, n (%) | 119 (69.6) | 20 (66.7) | 0.75 |
| SRF presence, n (%) | 149 (85.1) | 29 (96.7) | 0.14 |
| Sub-RPE fluid presence, n (%) | 92 (56.8) | 16 (55.2) | 0.87 |
| Retinal thickness at foveal centre (μm), mean (SE) | 216.3 (8.6) | 204.6 (20.9) | 0.61 |
| SRF thickness at foveal centre (μm), mean (SE) | 23.8 (4.6) | 47.3 (11.1) | 0.12 |
| Subretinal tissue complex thickness at foveal centre (μm), mean (SE) | 219.1 (13.6) | 266.9 (32.9) | 0.34 |
| Visual acuity (letters): mean (SE) | 61.4 (1.0) | 55.2 (2.4) | 0.02 |
P value calculated based on χ2 test Fisher’s exact test and two-sample t-test as appropriate.
IRF, intraretinal fluid; RPE, retinal pigment epithelium; SRF, subretinal fluid.
Adjusted VA score (letters) and change in VA were similar between thiazolidinedione takers versus non-takers at years 1 and 2 (all p≤0.27; table 2). Presence of SRF and sub-RPE fluid were similar at years 1 and 2 between takers versus non-takers (all p≤0.06). Proportions with IRF were higher in thiazolidinedione takers at both year 1 (64% vs 44.2%, p=0.10) and year 2 (75% vs 50%, p=0.04) and after adjustment for lesion type at year 2 (adjusted OR 2.8; 95% CI (1.0 to 8.0); p=0.04). Retinal, subretinal and subretinal tissue complex thicknesses at years 1 and 2 were similar between takers versus non-takers (all p≤0.13, table 2). Thiazolidinedione usage was associated with a greater decrease in SRF thickness at year 1 (adjusted mean difference −41.9 um; 95% CI (−66.7 to −17.0); p=0.001) and year 2 (adjusted mean difference −43.3 um (−69.5 to −17.2); p=0.001). Thiazolidinedione usage was associated with a greater mean decrease in subretinal tissue complex thickness at year 1 (difference −75.1 um; 95% CI (−139.8 to −10.4); p=0.02) and year 2 (difference −67.0 um; 95% CI (−135.4 to 1.4); p=0.06). The changes in SRF and subretinal tissue complex thickness from week 24 to year 2 were similar between thiazolidinedione takers versus non-takers (figure 1). Between year 1 and year 2, mean retinal thickness increased slightly in participants taking thiazolidinediones while remaining stable in non-takers.
Table 2.
Associations between baseline use of thiazolidinedione with fluid status, retinal thickness and visual acuity at year 1 and year 2
| Outcomes at year 1 or 2 | Year 1 |
Year 2 |
||||||
|---|---|---|---|---|---|---|---|---|
| Not Taking (N=166) | Taking (N=26) | Adjusted OR (95% CI)* | P value | Not Taking (N=151) | Taking (N=26) | Adjusted OR (95% CI)* | P value* | |
| IRF presence, n (%) | 72 (44.2) | 16 (64.0) | 2.1 (0.9 to 5.0) | 0.10 | 74 (50.0) | 18 (75.0) | 2.8 (1.0 to 7.5) | 0.04 |
|
| ||||||||
| SRF presence, n (%) | 56 (34.6) | 5 (21.7) | 0.5 (0.2 to 1.6) | 0.25 | 58 (40.3) | 5 (20.0) | 0.4 (0.1 to 1.1) | 0.06 |
|
| ||||||||
| Sub-RPE fluid presence, n (%) | 54 (34.6) | 5 (23.8) | 0.6 (0.2 to 1.7) | 0.31 | 56 (40.0) | 10 (41.7) | 1.2 (0.5 to 2.8) | 0.75 |
| Adjusted Difference (95% CI)* | P value | Adjusted Difference (95% CI)* | P value | |||||
|
| ||||||||
| Retinal thickness at foveal centre (μm), mean (SE) | 151.9 (4.1) | 136.6 (10.2) | −13.2 (−35.0 to 8.5) | 0.23 | 151.5 (5.1) | 149.8 (12.4) | 1.3 (−25.6 to 28.1) | 0.93 |
|
| ||||||||
| SRF thickness at foveal centre (μm), mean (SE) | 8.8 (2.3) | 1.8 (5.9) | −7.5 (−20.2 to 5.2) | 0.25 | 8.1 (2.1) | 0.0 (5.1) | −8.5 (−19.5 to 2.5) | 0.13 |
|
| ||||||||
| Subretinal tissue complex thickness at foveal centre (μm), mean (SE) | 143.7 (10.4) | 127.6 (26.3) | −20.7 (−77.6 to 36.2) | 0.48 | 137.3 (10.3) | 123.0 (25.2) | −18.1 (−72.8 to 36.7) | 0.52 |
|
| ||||||||
| Change in retinal thickness at foveal centre from baseline (μm), mean (SE) | −68.3 (9.3) | −60.5 (23.3) | 8.5 (−41.8 to 58.8) | 0.74 | −72.2 (10.8) | −37.6 (26.4) | 36.9 (−20.4 to 94.1) | 0.21 |
|
| ||||||||
| Change in SRF thickness at foveal centre from baseline (μm), mean (SE) | −11.8 (4.6) | −51.7 (11.5) | −41.9 (−66.7 to to 17.0) | 0.001 | −14.3 (4.9) | −55.6 (12.1) | −43.3 (−69.5 to to 17.2) | 0.001 |
|
| ||||||||
| Change in subretinal tissue complex thickness at foveal centre from baseline (μm), mean (SE) | −76.4 (12.1) | −157.9 (30.3) | −75.1 (−139.8 to to 10.4) | 0.02 | −77.4 (13.1) | −149.3 (32.0) | −67.0 (−135.4 to 1.4) | 0.056 |
|
| ||||||||
| Visual acuity (letters): mean (SE) | 68.0 (1.3) | 65.3 (3.3) | −2.7 (−9.7 to 4.4) | 0.46 | 66.6 (1.5) | 62.5 (3.6) | −4.4 (−12.2 to 3.4) | 0.27 |
|
| ||||||||
| Change in visual acuity from baseline (letters): mean (SE) | 6.7 (1.0) | 10.1 (2.6) | 3.0 (−2.7 to 8.6) | 0.30 | 5.1 (1.3) | 7.2 (3.0) | 1.6 (−5.0 to 8.2) | 0.64 |
ORs and differences are for participants taking versus not taking thiazolidinediones and adjusted by macular neovascularisation lesion type as a covariate in regression models.
IRF, intraretinal fluid; RPE, retinal pigment epithelium; SRF, subretinal fluid.
Figure 1.
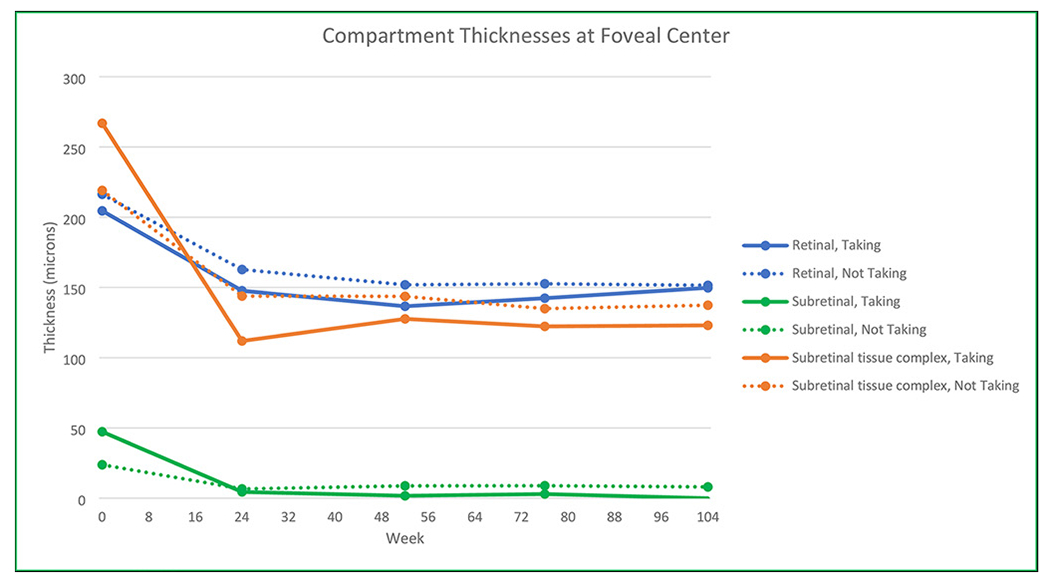
Retinal, subretinal fluid and subretinal tissue complex thickness at the foveal centre over time stratified by baseline use of thiazolidinedione. Mean thickness values of the retina, subretinal fluid and subretinal tissue complex compartments at the foveal centre are shown for key timepoints from baseline to week 104. Mean thickness values are stratified by patients taking (solid lines, N=151) and not taking thiazolidinediones at baseline (dashed lines, N=26).
DISCUSSION
We observed several differences in retinal anatomy among patients with diabetes taking thiazolidinediones when compared with patients with diabetes not taking them. Participants taking thiazolidinediones had similar mean SRF and subretinal tissue complex thicknesses at baseline compared with non-takers but had greater reductions in SRF and sub-RPE fluid thickness after anti-VEGF therapy initiation. Participants taking thiazolidinediones had worse mean baseline VA score, but similar VA score at year 1 and year 2 compared with non-takers. Finally, thiazolidinedione usage was associated with an increased risk of IRF at year 2.
Studies investigating the role of PPAR-γ signalling in AMD are sparse and focused on in vitro or in situ models. Herzlich et al found that human retinas with wet and dry AMD have increased PPAR-γ expression compared with age-matched healthy retinas and higher VEGF levels. These results were replicated in vitro when ARPE19 cells, a human RPE cell line commonly used as a model to study AMD, were exposed to H2O2-induced oxidative stress.8 While the clinical effects of TZDs on eyes with nAMD are unstudied, usage of this drug class has previously been associated with diabetic macular oedema (DME). Fong et al found that patients with diabetes taking thiazolidinediones were more likely to develop DME in a cohort study of 996 cases of new-onset DME after adjusting for age, glycaemic control and insulin usage.5 A larger retrospective cohort study of the Health Improvement Network database involving 103 368 patients with type 2 diabetes found an association between thiazolidinedione usage and DME following adjustment for confounding factors known to influence diabetic retinopathy at both 1-year and 10-year follow-ups.6 It must be noted, however, that the association between thiazolidinedione usage and DME has not been replicated in other retrospective analyses, such as the Action to Control Cardiovascular Risk in Diabetes (ACCORD) Eye Study.11 Thiazolidinediones have multiple effects which may predispose to a greater amount of vascular leakage or promote angiogenesis. Rosiglitazone has been found to increase VEGF expression and vascular permeability in human umbilical vein endothelial cells in vitro.12 Systemically, thiazolidinediones increase serum levels of VEGF and expand the plasma volume.13 14 Through VEGF-induced augmentation of vascular permeability and altered haemodynamics, thiazolidinediones could induce greater amounts of leakage from a persistent or recurrent neovascular membrane, leading to the greater incidence of IRF at follow-up observed in the CATT. Given that IRF has been associated with poor VA and increased risk of macular atrophy in large-scale clinical trials of anti-VEGF therapy for nAMD,15–17 a greater incidence of IRF among participants taking thiazolidinediones may herald later poor visual and anatomic outcomes.
Interestingly, thiazolidinediones have been shown in some studies to produce antiangiogenic rather than proangiogenic effects. In endometrial cells, thiazolidinediones inhibited VEGF gene promoter activity and expression.18 Thiazolidinediones administered intravitreally in animal models have inhibited VEGF-induced proliferation and migration of choroidal endothelial cells and retinal pigment epithelium.19 Whether thiazolidinediones act as an inhibitor or promoter of angiogenesis may depend on cell type, and it is unclear which effect, if any, predominates in vivo for the retinal tissues of patients with diabetes or nAMD. The greater reductions in fluid thickness from baseline observed in CATT participants taking thiazolidinediones suggest that their nAMD lesions are equally or more responsive to initiation of anti-VEGF therapy. If thiazolidinediones did hypothetically synergise with anti-VEGF therapy, resulting in a greater drying of the retina, the higher incidence of IRF we observe with their usage could result from degenerative cystic change rather than ongoing leakage. In the CATT and IVAN trials, greater fluctuations in the combined foveal centre point thicknesses (FCPT) of the retinal, subretinal and sub-RPE compartments have been correlated to poorer VA and the development of macular atrophy and fibrosis.20 The greater reductions in subretinal and subretinal tissue complex thickness observed in participants taking thiazolidinediones could promote retinal damage and cystic degeneration via greater FCPT fluctuations over time.
Thiazolidinediones might also influence macular neovascularisation lesions by anti-inflammatory effect, as demonstrated by in vitro and in vivo studies. Decreased circulating levels of the pro-inflammatory cytokine TNF-α have been found in patients treated with pioglitazone, while diabetic atherosclerotic plaques in patients treated with rosiglitazone contained lower concentrations of TNF-α and other inflammatory cytokines.21 22 TNF-α increases VEGF secretion by human RPE cells and choroidal fibroblasts and may therefore play a role in initiating retinal neovascularisation.23 Although TNF-inhibiting therapy for the treatment of nAMD has not been well tolerated,24 thiazolidinediones may nevertheless dampen the inflammatory milieu involved in the pathogenesis of nAMD and thereby alter the disease course. Overall, the effects of thiazolidinediones are numerous, complex and not well understood. Additional studies should be conducted to characterise their risk-benefit profile in the setting of nAMD as well as other diseases involving neovascularisation.
This study has several limitations. The analysis is post hoc and observational rather than based on randomised assignment to drug exposure or placebo group and cannot establish causality between thiazolidinedione usage and the reported findings. All OCT scans acquired in the first year of the CATT were time-domain and only a minority (22.6%) acquired in the second year were spectral-domain. Due to the lower resolution of time-domain OCT images, it is possible that some small collections of fluid may have been missed during grading, or that similarly appearing but distinct anatomic features such as outer retinal tubulations may have been misinterpreted as retinal fluid.25 The number of patients taking thiazolidinediones at the study baseline was small, limiting the statistical power of the analysis. Lastly, measurement of fluid thickness and retinal thickness was performed only at the foveal centre.
CONCLUSIONS
In this exploratory analysis, CATT participants with diabetes taking thiazolidinediones at baseline had greater reductions in SRF and subretinal tissue complex thickness from baseline, worse baseline VA and a greater proportion with IRF after 2 years of treatment. Additional studies are warranted to confirm these findings and characterise the effects of thiazolidinediones in neovascular ocular diseases.
Key messages.
What is already known on this topic
Thiazolidinediones have been associated with an increased risk of development of diabetic macular edema and may increase vascular endothelial cell permeability.
What this study adds
In this post-hoc analysis of participants with diabetes in the Comparison of Age-related Macular Degeneration Treatments Trials, we found thiazolidinedione usage was associated with worse baseline visual acuity, greater decreases in subretinal fluid and subretinal tissue complex thickness, and a greater proportion with intraretinal fluid at 2 years.
How this study might affect research, practice or policy
Additional studies are warranted to confirm these findings and characterize the effects of thiazolidinediones in neovascular ocular diseases.
Funding
This study was supported by cooperative agreements U10 EY017823, U10 EY017825, U10 EY017826, U10 EY017828 and R21EY023689 from the National Eye Institute, National Institutes of Health, and Department of Health and Human Services. ClinicalTrials.gov number: NCT00593450.
Collaborators
Credit Roster for the Comparison of AMD Treatments Trials: Clinical Centers (Ordered by Number of Patients Enrolled): Certified Roles at Clinical Centers: Clinic Coordinator (CC), Data Entry Staff (DE), Participating Ophthalmologist (O), Ophthalmic Photographer (OP); Optical Coherent Tomography Technician (OCT), Principal Investigator (PI), Refractionist (R), Visual Acuity Examiner (VA). VitreoRetinal Surgery, PA (Edina, MN): David F. Williams, MD (PI); Sara Beardsley, COA (VA/R); Steven Bennett, MD (O); Herbert Cantrill, MD (O); Carmen Chan-Tram, COA (VA/R); Holly Cheshier, CRA, COT, OCTC (OP); John Davies, MD (O); Sundeep Dev, MD (O); Julianne Enloe, CCRP, COA (CC); Gennaro Follano (OP/OCT); Peggy Gilbert, COA (VA/R); Jill Johnson, MD (O); Tori Jones, COA (OCT); Lisa Mayleben, COMT (CC/VA/R/OCT); Robert Mittra, MD (O); Martha Moos, COMT, OSA (VA/R); Ryan Neist, COMT (VA/R); Neal Oestreich, COT (CC); Polly Quiram, MD (O); Robert Ramsay, MD (O); Edwin Ryan, MD (O); Stephanie Schindeldecker, OA (VA/R); Trenise Steele, COA (VA); Jessica Tonsfeldt, AO (OP); Shelly Valardi, COT (VA/R). Texas Retina Associates (Dallas, TX): Gary Edd Fish, MD (PI); Hank A. Aguado, CRA (OP/OCT); Sally Arceneaux (CC/VA/R); Jean Arnwine (CC); Kim Bell, COA (VA/R); Tina Bell (CC/OCT); Bob Boleman (OP); Patricia Bradley, COT (CC); David Callanan, MD (O); Lori Coors, MD (O); Jodi Creighton, COA (VA/R); Kimberly Cummings (OP/OCT); Christopher Dock (OCT); Karen Duignan, COT (VA/R); Dwain Fuller, MD (O); Keith Gray (OP/OCT); Betsy Hendrix, COT, ROUB (OCT); Nicholas Hesse (OCT); Diana Jaramillo, COA (OCT); Bradley Jost, MD (O); Sandy Lash (VA/R); Laura Lonsdale, CCRP (DE); Michael Mackens (OP/OCT); Karin Mutz, COA (CC); Michael Potts (VA/R); Brenda Sanchez (VA/R); William Snyder, MD (O); Wayne Solley, MD (O); Carrie Tarter (VA/R); Robert Wang, MD (O); Patrick Williams, MD (O). Southeastern Retina Associates (Knoxville, TN): Stephen L. Perkins, MD (PI); Nicholas Anderson, MD (O); Ann Arnold, COT (VA/R); Paul Blais (OP/OCT); Joseph Googe, MD (O); Tina T. Higdon, (CC); Cecile Hunt (VA/R); Mary Johnson, COA (VA/R); James Miller, MD (O); Misty Moore (VA/R); Charity K. Morris, RN (CC); Christopher Morris (OCT); Sarah Oelrich, COT (OP/OCT); Kristina Oliver, COA (VA/R); Vicky Seitz, COT (VA/R); Jerry Whetstone (OP/OCT). Retina Vitreous Consultants (Pittsburgh, PA): Bernard H. Doft (PI); Jay Bedel, RN, (CC); Robert Bergren, MD (O); Ann Borthwick (VA/R); Paul Conrad, MD, PHD (O); Christina Fulwylie (VA/R); Willia Ingram (DE); Shawnique Latham (VA/R); Gina Lester (VA/R); Judy Liu, MD (O); Louis Lobes, MD (O); Nicole M. Lucko, (CC); Lori Merlotti, MS, CCRC (CC); Karl Olsen, MD (O); Danielle Puskas, COA (VA/R); Pamela Rath, MD (O); Lynn Schueckler (OCT); Christina Schultz (CC/VA/R); Heather Shultz (OP/OCT); David Steinberg, CRA (OP/OCT); Avni Vyas, MD (O); Kim Whale (VA/R); Kimberly Yeckel, COA, COT (VA/R). Ingalls Memorial Hospital/Illinois Retina Associates (Harvey, IL): David H. Orth, MD (PI); Linda S. Arredondo, RN (CC/VA); Susan Brown (VA/R); Barbara J. Ciscato (CC/VA); Joseph M. Civantos, MD (O); Celeste Figliulo (VA/R); Sohail Hasan, MD (O); Belinda Kosinski, COA (VA/R); Dan Muir (OP/OCT); Kiersten Nelson (OP/OCT); Kirk Packo, MD (O); John S. Pollack, MD (O); Kourous Rezaei, MD (O); Gina Shelton (VA); Shannya Townsend-Patrick (OP/OCT); Marian Walsh, CRA (OP/OCT). West Coast Retina Medical Group, Inc. (San Francisco, CA): H. Richard McDonald, MD (PI); Nina Ansari (VA/R/OCT); Amanda Bye, (OP/OCT); Arthur D. Fu, MD (O); Sean Grout (OP/OCT); Chad Indermill (OCT); Robert N. Johnson, MD (O); J. Michael Jumper, MD (O); Silvia Linares (VA/R); Brandon J. Lujan, MD (O); Ames Munden (OP/OCT); Rosa Rodriguez (CC); Jennifer M. Rose (CC); Brandi Teske, COA (VA/R); Yesmin Urias (OCT); Stephen Young (OP/OCT). Retina Northwest, P.C. (Portland, OR): Richard F. Dreyer, MD (PI); Howard Daniel (OP/OCT); Michele Connaughton, CRA (OP/OCT); Irvin Handelman, MD (O); Stephen Hobbs (VA/R/OCT); Christine Hoerner (OP/OCT); Dawn Hudson (VA/R/OCT); Marcia Kopfer, COT (CC/VA/R/OCT); Michael Lee, MD (O); Craig Lemley, MD (O); Joe Logan, COA (OP/OCT); Colin Ma, MD (O); Christophe Mallet (VA/R); Amanda Milliron (VA/R); Mark Peters, MD (O); Harry Wohlsein, COA (OP). Retinal Consultants Medical Group, Inc. (Sacramento, CA): Joel A. Pearlman, MD, PHD (PI); Margo Andrews (OP); Melissa Bartlett (OCT); Nanette Carlson (CC/OCT); Emily Cox (VA/R); Robert Equi, MD (O); Marta Gonzalez (VA/R); Sophia Griffin (OP/OCT); Fran Hogue (VA/R); Lance Kennedy (OP/OCT); Lana Kryuchkov (OCT); Carmen Lopez (VA/R); Danny Lopez (OP/OCT); Bertha Luevano (VA/R); Erin McKenna, (CC); Arun Patel, MD (O); Brian Reed, MD (O); Nyla Secor (CC/OCT); Iris R. Sison (CC); Tony Tsai, MD (O); Nina Varghis, (CC); Brooke Waller (OCT); Robert Wendel, MD (O); Reina Yebra (OCT). Retina Vitreous Center, PA (New Brunswick, NJ): Daniel B. Roth, MD (PI); Jane Deinzer, RN (VA/R); Howard Fine, MD MHSC (O); Flory Green (VA/R); Stuart Green, MD (O); Bruce Keyser, MD (O); Steven Leff, MD (O); Amy Leviton (VA/R); Amy Martir (OCT); Kristin Mosenthine (VA/R/OCT); Starr Muscle, RN (CC); Linda Okoren (VA/R); Sandy Parker (VA/R); Jonathan Prenner, MD (O); Nancy Price (CC); Deana Rogers (OP/OCT); Linda Rosas (OP/OCT); Alex Schlosser (OP/OCT); Loretta Studenko (DE); Thea Tantum (CC); Harold Wheatley, MD (O). Vision Research Foundation/Associated Retinal Consultants, P.C. (Royal Oak, MI): Michael T. Trese, MD (PI); Thomas Aaberg, MD (O); Denis Bezaire, CRA (OP/OCT); Craig Bridges, CRA (OP/OCT); Doug Bryant, CRA (OP/OCT); Antonio Capone, MD (O); Michelle Coleman, RN (CC); Christina Consolo, CRA, COT (OP/OCT); Cindy Cook, RN (CC); Candice DuLong (VA/R); Bruce Garretson, MD (O); Tracy Grooten (VA/R); Julie Hammersley, RN (CC); Tarek Hassan, MD (O); Heather Jessick (OP/OCT); Nanette Jones (VA/R/OP/OCT); Crystal Kinsman (VA/R); Jennifer Krumlauf (VA/R); Sandy Lewis, COT (VA/R/OP/OCT); Heather Locke (VA/R); Alan Margherio, MD (O); Debra Markus, COT (CC/VA/R/OP/OCT); Tanya Marsh, COA (OP/OCT); Serena Neal (CC); Amy Noffke, MD (O); Kean Oh, MD (O); Clarence Pence (OP/OCT); Lisa Preston (VA/R); Paul Raphaelian, MD (O); Virginia R. Regan, RN, CCRP (VA/R); Peter Roberts (OP/OCT); Alan Ruby, MD (O); Ramin Sarrafizadeh, MD, PHD (O); Marissa Scherf (OP/OCT); Sarita Scott (VA/R); Scott Sneed, MD (O); Lisa Staples (CC); Brad Terry (VA/R/OP/OCT); Matthew T. Trese (OCT); Joan Videtich, RN (VA/R); George Williams, MD (O); Mary Zajechowski, COT, CCRC (CC/VA/R). Barnes Retina Institute (St. Louis, MO): Daniel P. Joseph, MD (PI); Kevin Blinder, MD (O); Lynda Boyd, COT (VA/R); Sarah Buckley (OP/OCT); Meaghan Crow (VA/R); Amanda Dinatale, (OCT); Nicholas Engelbrecht, MD (O); Bridget Forke (OP/OCT); Dana Gabel (OP/OCT); Gilbert Grand, MD (O); Jennifer Grillion-Cerone (VA/R); Nancy Holekamp, MD (O); charlotte Kelly, COA (VA/R); Ginny Nobel, COT (CC); Kelly Pepple (VA/R); Matt Raeber, (OP/OCT); P. Kumar Rao, MD (O); Tammy Ressel, COT (VA/R); Steven Schremp (OCT); Merrilee Sgorlon (VA/R); Shantia Shears, MA (CC); Matthew Thomas, MD (O); Cathy Timma (VA/R); Annette Vaughn,(OP/OCT); Carolyn Walters, COT (CC/VA/R); Rhonda Weeks, CRC (CC/VA/R); Jarrod Wehmeier (OP/OCT); Tim Wright (OCT). The Retina Group of Washington (Chevy Chase, MD): Daniel M. Berinstein, MD (PI); Aida Ayyad (VA/R); Mohammed K. Barazi, MD (O); Erica Bickhart (VA/R); Lisa Byank, MA (CC); Alysia Cronise, COA (VA/R); Vanessa Denny (VA/R); Courtney Dunn (VA/R); Michael Flory (OP/OCT); Robert Frantz (OP/OCT); Richard A. Garfinkel, MD (O); William Gilbert, MD (O); Michael M. Lai, MD, PHD (O); Alexander Melamud, MD (O); Janine Newgen (VA/R); Shamekia Newton (CC); Debbie Oliver (CC); Michael Osman, MD (O); Reginald Sanders, MD (O); Manfred von Fricken, MD (O). Retinal Consultants of Arizona (Phoenix, AZ): Pravin Dugel, MD (PI); Sandra Arenas (CC); Gabe Balea (OCT); Dayna Bartoli (OP/OCT); John Bucci (OP/OCT); Jennifer A. Cornelius (CC); Scheleen Dickens, (CC); Don Doherty (OP/OCT); Heather Dunlap, COA (VA/R); David Goldenberg, MD (O); Karim Jamal, MD (O); Norma Jimenez (OP/OCT); Nicole Kavanagh (VA/R); Derek Kunimoto, MD (O); John Martin (OP/OCT); Jessica Miner, RN (VA/R); Sarah Mobley, CCRC (CC/VA/R); Donald Park, MD (O); Edward Quinlan, MD (O); Jack Sipperley, MD (O); Carol Slagle (R); Danielle Smith (OP/OCT); Rohana Yager, COA (OCT). Casey Eye Institute (Portland, OR): Christina J. Flaxel, MD (PI); Steven Bailey, MD (O); Peter Francis, MD, PHD (O); Chris Howell, (OCT); Thomas Hwang, MD (O); Shirley Ira, COT (VA/R); Michael Klein, MD (O); Andreas Lauer, MD (O); Teresa Liesegang, COT (CC/VA/R); Ann Lundquist, (CC/VA/R); Sarah Nolte (DE); Susan K. Nolte (VA/R); Scott Pickell (OP/OCT); Susan Pope, COT (VA/R); Joseph Rossi (OP/OCT); Mitchell Schain (VA/R); Peter Steinkamp, MS (OP/OCT); Maureen D. Toomey (CC/VA/R); Debora Vahrenwald, COT (VA/R); Kelly West (OP/OCT). Emory Eye Center (Atlanta, GA): Baker Hubbard, MD (PI); Stacey Andelman, MMSC, COMT (CC/VA/R); Chris Bergstrom, MD (O); Judy Brower, COMT (CC/VA/R); Blaine Cribbs, MD (O); Linda Curtis (VA/R); Jannah Dobbs (OP/OCT); Lindreth DuBois, MED, MMSC, CO, COMT (CC/VA/R); Jessica Gaultney (OCT); Deborah Gibbs, COMT, CCRC (VA/R); Debora Jordan, CRA (OP/OCT); Donna Leef, MMSC, COMT (VA/R); Daniel F. Martin, MD (O); Robert Myles, CRA (OP); Timothy Olsen, MD (O); Bryan Schwent, MD (O); Sunil Srivastava, MD (O); Rhonda Waldron, MMSC, COMT, CRA, RDMS (OCT). Charlotte Eye, Ear, Nose & Throat Associates/Southeast Clinical Research (Charlotte, NC): Andrew N. Antoszyk, MD (PI); Uma Balasubramaniam, COA (OCT); Danielle Brooks, CCRP (VA/R); Justin Brown, MD (O); David Browning, MD, PHD (O); Loraine Clark, COA (OP/OCT); Sarah Ennis, CCRC (VA/R); Jennifer V. Helms, CCRC,(CC); Jenna Herby, CCRC (CC); Angie Karow, CCRP (VA/R); Pearl Leotaud, CRA (OP/OCT); Caterina Massimino (OCT); Donna McClain, COA (OP/OCT); Michael McOwen, CRA (OP/OCT); Jennifer Mindel, CRA, COA (OP/OCT); Candace Pereira, CRC (CC); Rachel Pierce, COA (VA/R); Michele Powers (OP/OCT); Angela Price, MPH, CCRC (CC); Jason Rohrer (CC); Jason Sanders, MD (O). California Retina Consultants (Santa Barbara, CA): Robert L. Avery, MD (PI); Kelly Avery (VA/R); Jessica Basefsky (CC/OCT); Liz Beckner (OP); Alessandro Castellarin, MD (O); Stephen Couvillion, MD (O); Jack Giust (CC/OCT); Matthew Giust (OP); Maan Nasir, MD (O); Dante Pieramici, MD (O); Melvin Rabena (VA/R); Sarah Risard (VA/R/OCT/DE); Robert See, MD (O); Jerry Smith (VA/R). Mayo Clinic (Rochester, MN): Sophie J. Bakri, MD (PI); Nakhleh Abu-Yaghi, MD (O); Andrew Barkmeier, MD (O); Karin Berg, COA (VA); Jean Burrington, COA (VA/R); Albert Edwards, MD (O); Shannon Goddard, COA (OP/OCT); Shannon Howard (VA/R); Raymond Iezzi, MD (O); Denise Lewison, COA (OP/OCT); Thomas Link, CRA (OP/OCT); Colin A. McCannel, MD (O); Joan Overend (VA/R); John Pach, MD (O); Margaret Ruszczyk, CCRP (CC); Ryan Shultz, MD (O); Cindy Stephan, COT (VA/R); Diane Vogen (CC). Dean A. McGee Eye Institute (Oklahoma City, OK): Reagan H. Bradford Jr, MD (PI); Vanessa Bergman, COA, CCRC (CC); Russ Burris (OP/OCT); Amanda Butt, CRA (OP/OCT); Beth Daniels, COA (CC); Connie Dwiggins, CCRC (CC); Stephen Fransen, MD (O); Tiffany Guerrero (CC/DE); Darin Haivala, MD (O); Amy Harris (CC); Sonny Icks (CC/DE); Ronald Kingsley, MD (O); Rob Richmond (OP/OCT); Brittany Ross (VA/R); Kammerin White, CCRC (VA/R); Misty Youngberg, COA, CCRC (VA/R). Ophthalmic Consultants of Boston (Boston, MA): Trexler M. Topping, MD (PI); Steve Bennett (OCT); Sandy Chong (VA/R); Tina Cleary, MD (O); Emily Corey (VA/R); Dennis Donovan (OP/OCT); Albert Frederick, MD (O); Lesley Freese (CC/VA/R); Margaret Graham (OP/OCT); Natalya Gud, COA (VA/R); Taneika Howard (VA/R); Mike Jones (OP/OCT); Michael Morley, MD (O); Katie Moses (VA/R); Jen Stone (VA/R); Robin Ty, COA (VA/R); Torsten Wiegand, PHD, MD (O); Lindsey Williams (CC); Beth Winder (CC). Tennessee Retina, P.C. (Nashville, TN): Carl C. Awh, MD (PI); Everton Arrindell, MD (O); Dena Beck (OCT); Brandon Busbee, MD (O); Amy Dilback (OP/OCT); Sara Downs (VA/R); Allison Guidry, COA (VA/R); Gary Gutow, MD (O); Jackey Hardin (VA/R); Sarah Hines, COA (CC); Emily Hutchins (VA/R); Kim LaCivita, MA (OP/OCT); Ashley Lester (OCT); Larry Malott (OP/OCT); MaryAnn McCain, RN, CNOR (CC); Jayme Miracle (VA/R); Kenneth Moffat, MD (O); Lacy Palazzotta (VA/R); Kelly Robinson, COA (VA/R); Peter Sonkin, MD (O); Alecia Travis (OP/OCT); RoyTrent Wallace, MD (O); Kelly J. Winters, COA (CC); Julia Wray (OP/OCT). Retina Associates Southwest, P.C. (Tucson, AZ): April E. Harris, MD (PI); Mari Bunnell (OCT); Katrina Crooks (VA/R); Rebecca Fitzgerald, CCRC (CC); Cameron Javid, MD (O); Corin Kew (VA/R); Erica Kill, VAE (VA/R); Patricia Kline (VA/R); Janet Kreienkamp (VA/R); RoyAnn Moore, OMA (CC/OCT); Egbert Saavedra, MD (O); LuAnne Taylor, CSC (CC/OCT); Mark Walsh, MD (O); Larry Wilson (OP). Midwest Eye Institute (Indianapolis, IN): Thomas A. Ciulla, MD (PI); Ellen Coyle, COMT (VA/R); Tonya Harrington, COA (VA/R); Charlotte Harris, COA (VA); Raj Maturi, MD (O); Stephanie Morrow, COA (OP); Jennifer Savage, COA (VA); Bethany Sink, COA (VA/R); Tom Steele, CRA (OP); Neelam Thukral, CCRC (CC/OCT); Janet Wilburn, COA (CC). National Ophthalmic Research Institute (Fort Myers, FL): Joseph P. Walker, MD (PI); Jennifer Banks (VA/R); Debbie Ciampaglia (OP/OCT); Danielle Dyshanowitz (VA/R); Jennifer Frederick, CRC (CC); A. Tom Ghuman, MD (O); Richard Grodin, MD (O); Cheryl Kiesel, CCRC (CC); Eileen Knips, RN, CCRC, CRA (OP/OCT); Crystal Peters, CCRC (CC); Paul Raskauskas, MD (O); Etienne Schoeman (OP/OCT); Ashish Sharma, MD (O); Glenn Wing, MD (O). University of Wisconsin Madison (Madison, WI): Suresh R. Chandra, MD (PI); Michael Altaweel, MD (O); Barbara Blodi, MD (O); Kathryn Burke, BA (VA/R); Kristine A. Dietzman, (CC); Justin Gottlieb, MD (O); Gene Knutson (OP/OCT); Denise Krolnik (OP/OCT); T. Michael Nork, MD (O); Shelly Olson (VA/R); John Peterson, CRA (OP/OCT); Sandra Reed (OP/OCT); Barbara Soderling (VA/R); Guy Somers (VA/R); Thomas Stevens, MD (O); Angela Wealti, (CC). Duke University Eye Center (Durham, NC): Srilaxmi Bearelly, MD (PI); Brenda Branchaud (VA/R); Joyce W. Bryant, COT, CPT (CC/VA/R); Sara Crowell (CC/VA); Sharon Fekrat, MD (O); Merritt Gammage (OP/OCT); Cheala Harrison, COA (VA/R); Sarah Jones (VA); Noreen McClain, COT, CPT, CCRC (VA/R); Brooks McCuen, MD (O); Prithvi Mruthyunjaya, MD (O); Jeanne Queen, CPT (OP/OCT); Neeru Sarin, MBBS (VA/R); Cindy Skalak, RN, COT (VA/R); Marriner Skelly, CRA (OP/OCT); Ivan Suner, MD (O); Ronnie Tomany (OP/OCT); Lauren Welch (OP/OCT). University of California-Davis Medical Center (Sacramento, CA): Susanna S. Park, MD, PHD (PI); Allison Cassidy (VA/R); Karishma Chandra (OP/OCT); Idalew Good (VA/R); Katrina Imson (CC); Sashi Kaur (OP/OCT); Helen Metzler, COA, CCRP (CC/VA/R); Lawrence Morse, MD, PHD (O); Ellen Redenbo, ROUB (OP/OCT); Marisa Salvador (VA/R); David Telander, MD (O); Mark Thomas, CRA (OCT); Cindy Wallace, COA (CC). University of Louisville School of Medicine, KY (Louisville, KY): Charles C. Barr, MD (PI); Amanda Battcher (VA/R); Michelle Bottorff, COA (CC/OCT); Mary Chasteen (VA/R); Kelly Clark (VA/R); Diane Denning, COT (OCT); Amy Schultz (OP); Evie Tempel, CRA, COA (OP); Greg K. Whittington, MPS, PSY (CC). Retina Associates of Kentucky (Lexington, KY): Thomas W. Stone, MD (PI); Todd Blevins (OP/OCT); Michelle Buck, COT, (VA/R/OCT); Lynn Cruz, COT (CC); Wanda Heath (VA/R); Diana Holcomb (VA/R); Rick Isernhagen, MD (O); Terri Kidd, COA (OCT); John Kitchens, MD (O); Cathy Sears, CST, COA (VA/R); Ed Slade, CRA, COA (OP/OCT); Jeanne Van Arsdall, COA (VA/R); Brenda VanHoose, COA (VA/R); Jenny Wolfe, RN (CC); William Wood, MD (O). Colorado Retina Associates (Denver, CO): John Zilis, MD (PI); Carol Crooks, COA (VA/R); Larry Disney (VA/R); Mimi Liu, MD (O); Stephen Petty, MD (O); Sandra Sall, ROUB, COA (CC/VA/R/OP/OCT). University of Iowa Hospitals & Clinics (Iowa City, IA): James C. Folk, MD (PI); Tracy Aly, CRA (OP/OCT); Abby Brotherton (VA); Douglas Critser, CRA (OP/OCT); Connie J. Hinz, COT, CCRC (CC/VA/R); Stefani Karakas, CRA (OP/OCT); Cheyanne Lester (VA/R); Cindy Montague, CRA (OP/OCT); Stephen Russell, MD (O); Heather Stockman (VA/R); Barbara Taylor, CCRC (VA/R); Randy Verdick, FOPS (OP/OCT). Retina Specialists (Towson, MD): John T. Thompson, MD (PI) ; Barbara Connell (VA/R); Maryanth Constantine (CC); John L. Davis Jr (VA/R); Gwen Holsapple (VA/R); Lisa Hunter (OP/OCT); C. Nicki Lenane (CC/VA/R/OCT); Robin Mitchell (CC); Leslie Russel, CRA (OP/OCT); Raymond Sjaarda, MD (O). Retina Consultants of Houston (Houston, TX): David M. Brown, MD (PI); Matthew Benz, MD (O); Llewellyn Burns (OCT); JoLene G. Carranza, COA, CCRC (CC); Richard Fish, MD (O); Debra Goates (VA/R); Shayla Hay (VA/R); Theresa Jeffers, COT (VA/R); Eric Kegley, CRA, COA (OP/OCT); Dallas Kubecka (VA/R); Stacy McGilvra (VA/R); Beau Richter (OCT); Veronica Sneed, COA (VA/R); Cary Stoever (OCT); Isabell Tellez (VA/R); Tien Wong, MD (O). Massachusetts Eye & Ear Infirmary/Harvard Vanguard Medical Associates (Boston, MA): Ivana Kim, MD (PI); Christopher Andreoli, MD (O); Leslie Barresi, CRA, COA, OCT-C (VA/OP/OCT); Sarah Brett (OP); Charlene Callahan (OP); Karen Capaccioli (OCT); William Carli, COA (VA/R/OCT); Matthew Coppola, COA (VA); Nicholas Emmanuel (CC); Claudia Evans, OD (VA/R); Anna Fagan, COA (VA/R); Marcia Grillo (OCT); John Head, CRA, OCT-C (OP/OCT); Troy Kieser, COA, OCT-C (CC/VA/R); Ursula Lord, OD (VA/R); Edward Miretsky (CC); Kate Palitsch (OCT); Todd Petrin, RN (OCT); Liz Reader (CC); Svetlana Reznichenko, COA (VA); Mary Robertson, COA (VA); Demetrios Vavvas, MD, PHD (O). Palmetto Retina Center (West Columbia, SC): John Wells, MD (PI); Cassie Cahill (VA/R); W. Lloyd Clark, MD (O); Kayla Henry (VA/R); David Johnson, MD (O); Peggy Miller (CC/VA/R); LaDetrick Oliver, COT (OP/OCT); Robbin Spivey (OP/OCT); Mallie Taylor (CC). Retina and Vitreous of Texas (Houston, TX): Michael Lambert, MD (PI); Kris Chase (OP/OCT); Debbie Fredrickson, COA (VA/R); Joseph Khawly, MD, FACS (O); Valerie Lazarte (VA/R); Donald Lowd (OP/OCT); Pam Miller (CC); Arthur Willis, MD (O). Long Island Vitreoretinal Consultants (Great Neck, NY): Philip J. Ferrone, MD (PI); Miguel Almonte (OCT); Rachel Arnott, (CC); Ingrid Aviles (VA/R/OCT); Sheri Carbon (VA/R); Michael Chitjian (OP/OCT); Kristen DAmore (CC); Christin Elliott (VA/R); David Fastenberg, MD (O); Barry Golub, MD (O); Kenneth Graham, MD (O); AnnMarie Lavorna (CC); Laura Murphy (VA/R); Amanda Palomo (VA/R); Christina Puglisi (VA/R); David Rhee, MD (O); Juan Romero, MD (O); Brett Rosenblatt, MD (O); Glenda Salcedo (OP/OCT); Marianne Schlameuss, RN (CC); Eric Shakin, MD (O); Vasanti Sookhai (VA/R). Wills Eye Institute (Philadelphia, PA): Richard Kaiser, MD (PI); Elizabeth Affel, MS, OCT-C (OCT); Gary Brown, MD (O); Christina Centinaro (CC); Deborah Fine, COA (OCT); Mitchell Fineman, MD (O); Michele Formoso (CC); Sunir Garg, MD (O); Lisa Grande (VA/R); Carolyn Herbert (VA/R); Allen Ho, MD (O); Jason Hsu, MD (O); Maryann Jay (OCT); Lisa Lavetsky (OCT); Elaine Liebenbaum (OP); Joseph Maguire, MD (O); Julia Monsonego (OP); Lucia O’Connor (OCT); Carl Regillo, MD (O); Maria Rosario (DE); Marc Spirn, MD (O); James Vander, MD (O); Jennifer Walsh (VA/R). Ohio State University Eye Physicians & Surgeons-Retina Division (Dublin, OH): Frederick H. Davidorf, MD (PI); Amanda Barnett (OP/OCT); Susie Chang, MD (O); John Christoforidis, MD (O); Joy Elliott (CC); Heather Justice (VA/R); Alan Letson, MD (O); Kathryne McKinney, COMT (CC); Jeri Perry, COT (VA/R); Jill A. Salerno, COA (CC); Scott Savage (OP); Stephen Shelley (OCT). Retina Associates of Cleveland (Beachwood, OH): Lawrence J. Singerman, MD (PI);Joseph Coney, MD (O); John DuBois (OP/OCT); Kimberly DuBois, LPN, CCRP, COA (VA/R); Gregg Greanoff, CRA (OP/OCT); Dianne Himmelman, RN, CCRC (CC); Mary Ilc, COT (VA/R); Elizabeth Mcnamara (VA/R/OP); Michael Novak, MD (O); Scott Pendergast, MD (O); Susan Rath, PA-C (CC); Sheila Smith-Brewer, CRA (OP/OCT); Vivian Tanner, COT, CCRP (VA/R); Diane E. Weiss, RN, (CC); Hernando Zegarra, MD (O). Retina Group of Florida (Fort Lauderdale, FL): Lawrence Halperin, MD (PI); Patricia Aramayo (OCT); Mandeep Dhalla, MD (O); Brian Fernandez, MD (OP/OCT); Cindy Fernandez, MD (CC); Jaclyn Lopez (CC); Monica Lopez (OCT); Jamie Mariano, COA (VA/R); Kellie Murphy, COA (OCT); Clifford Sherley, COA (VA/R); Rita Veksler, COA (OP/OCT). Retina-Vitreous Associates Medical Group (Beverly Hills, CA): Firas Rahhal, MD (PI); Razmig Babikian (DE); David Boyer, MD (O); Sepideh Hami (DE); Jeff Kessinger (OP/OCT); Janet Kurokouchi (CC); Saba Mukarram (VA/R); Sarah Pachman (VA/R); Eric Protacio (OCT); Julio Sierra (VA/R); Homayoun Tabandeh, MD, MS, FRCP (O); Adam Zamboni (VA/R). Elman Retina Group, P.A. (Baltimore, MD): Michael Elman, MD (PI); Tammy Butcher (CC); Theresa Cain (OP/OCT); Teresa Coffey, COA (VA/R); Dena Firestone (VA/R); Nancy Gore (VA/R); Pamela Singletary (VA/R); Peter Sotirakos (OP/OCT); JoAnn Starr (CC). University of North Carolina at chapel Hill (Chapel Hill, NC): Travis A. Meredith, MD (PI); Cassandra J. Barnhart, MPH (CC/VA/R); Debra Cantrell, COA (VA/R/OP/OCT); RonaLyn Esquejo-Leon (OP/OCT); Odette Houghton, MD (O); Harpreet Kaur (VA/R); Fatoumatta NDure, COA (CC). Ophthalmologists Enrolling Patients but No Longer Affiliated with a CATT Center: Ronald Glatzer, MD (O); Leonard Joffe, MD (O); Reid Schindler, MD (O). Resource Centers: Chairman’s Office (Cleveland Clinic, Cleveland, OH): Daniel F. Martin, MD (Chair); Stuart L. Fine, MD (Vice-Chair; University of Colorado, Denver CO); Marilyn Katz (Executive Assistant). Coordinating Center (University of Pennsylvania, Philadelphia, PA): Maureen G. Maguire, PhD (PI); Mary Brightwell-Arnold, SCP (Systems Analyst); Ruchira Glaser, MD (Medical Monitor); Judith Hall (Protocol Monitor); Sandra Harkins (Staff Assistant); Jiayan Huang, MS (Biostatistician); Alexander Khvatov, MS (Systems Analyst); Kathy McWilliams, CCRP (Protocol Monitor); Susan K. Nolte (Protocol Monitor); Ellen Peskin, MA, CCRP (Project Director); Maxwell Pistilli, MS, MEd (Biostatistician); Susan Ryan (Financial Administrator); Allison Schnader (Administrative Coordinator); Gui-shuang Ying, PhD (Senior Biostatistician). OCT Reading Center (Duke University, Durham, NC): Glenn Jaffe, MD (PI); Jennifer Afrani-Sakyi (CATT PowerPoint Presentations); Brannon Balsley (OCT Technician Certifications); Linda S. Bennett (Project Manager); Adam Brooks (Reader/SD-Reader); Adrienne Brower-Lingsch (Reader); Lori Bruce (Data Verification); Russell Burns (Senior Technical Analyst/Senior Reader/SD Reader/OCT Technician Certifications); Dee Busian (Reader); John Choong (Reader); Lindsey Cloaninger (Reader Reliability Studies/Document Creation/CATT PPT Files); Francis Char DeCroos (Research Associate); Emily DuBois (Data Entry); Mays El-Dairi (Reader/SD-Reader); Sarah Gach (Reader); Katelyn Hall (Reader Reliability Studies/Data Verification/Document Creation); Terry Hawks (Reader); ChengChenh Huang (Reader); Cindy Heydary (Senior Reader/Quality Assurance Coordinator/SD Reader/Data Verification); Alexander Ho (Reader, Transcription); Shashi Kini (Data Entry/Transcription); Michelle McCall (Data Verification); Daaimah Muhammad (Reader Feedback); Jayne Nicholson (Data Verification); Jeanne Queen (Reader/SD-Reader); Pamela Rieves (Transcription); Kelly Shields (Senior Reader); Cindy Skalak (Reader); Adam Specker (Reader); Sandra Stinnett (Biostatistician); Sujatha Subramaniam (Reader); Patrick Tenbrink (Reader); Cynthia Toth, MD (Director of Grading); Aaron Towe (Reader); Kimberly Welch (Data Verification); Natasha Williams (Data Verification); Katrina Winter (Senior Reader); Ellen Young (Senior Project Manager). Fundus Photograph Reading Center (University of Pennsylvania, Philadelphia, PA): Juan E. Grunwald, MD (PI); Judith Alexander (Director); Ebenezer Daniel, MBBS, MS, MPH, PhD (Director); Elisabeth Flannagan (Administrative Coordinator); E. Revell Martin (Reader); Candace Parker (Reader); Krista Sepielli (Reader); Tom Shannon (Systems Analyst); Claressa Whearry (Data Coordinator). National Eye Institute, National Institutes of Health: Maryann Redford, DDS, MPH (Program Officer). Committees: Executive Committee: Daniel F. Martin, MD (chair); Robert L. Avery, MD; Sophie J. Bakri, MD; Ebenezer Daniel, MBBS, MS, MPH; Stuart L. Fine, MD; Juan E. Grunwald, MD; Glenn Jaffe, MD, Marcia R. Kopfer, BS, COT; Maureen G. Maguire, PhD; Travis A. Meredith, MD; Ellen Peskin, MA, CCRP; Maryann Redford, DDS, MPH; David F. Williams, MD. Operations Committee: Daniel F. Martin, MD (chair); Linda S. Bennett; Ebenezer Daniel, MBBS, MS, MPH; Frederick L. Ferris III, MD; Stuart L. Fine, MD; Juan E. Grunwald, MD; Glenn Jaffe, MD; Maureen G. Maguire, PhD; Ellen Peskin, MA, CCRP; Maryann Redford, DDS, MPH; Cynthia Toth, MD. Clinic Monitoring Committee: Ellen Peskin, MA, CCRP (chair); Mary Brightwell-Arnold, SCP; Joan DuPont; Maureen G. Maguire, PhD; Kathy McWilliams, CCRP; Susan K. Nolte. Data and Safety Monitoring Committee: Lawrence M. Friedman, MD (chair); Susan B. Bressler, MD; David L. DeMets, PhD; Martin Friedlander, MD, PhD; Mark W. Johnson, MD; Anne Lindblad, PhD; Douglas W. Losordo, MD, FACC; Franklin G. Miller, PhD.
Footnotes
Competing interests ED is a consultant to Novartis International AG. MGM serves on a data and safety monitoring committee for Genentech/Roche. GJ has a consultancy relationship with Alcon/Novartis, Genentech/Roche, Neurotech, EyePoint Pharmaceuticals and Adverum. G-SY is a consultant to Chengdu Kanghong Biotech, Ziemer Ophthalmic Systems AG and Synergy Research.
Additional supplemental material is published online only. To view, please visit the journal online (http://dx.doi.org/10.1136/bjophthalmol-2021-320665).
Patient consent for publication Consent obtained directly from patient(s)
Ethics approval The trial protocol was approved by the institutional review boards of all clinical centres participating in the CATT, and patients provided written, informed consent for participation.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data is available at the following website: https://hyperprod.cceb.med.upenn.edu/catt/catt_index.php
REFERENCES
- 1.Idris I, Gray S, Donnelly R. Rosiglitazone and pulmonary oedema: an acute dose-dependent effect on human endothelial cell permeability. Diabetologia 2003;46:288–90. [DOI] [PubMed] [Google Scholar]
- 2.Jiang Y, Thakran S, Bheemreddy R, et al. Pioglitazone normalizes insulin signaling in the diabetic rat retina through reduction in tumor necrosis factor α and suppressor of cytokine signaling 3. J Biol Chem 2014;289:26395–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vijay SK, Mishra M, Kumar H, et al. Effect of pioglitazone and rosiglitazone on mediators of endothelial dysfunction, markers of angiogenesis and inflammatory cytokines in type-2 diabetes. Acta Diabetol 2009;46:27–33. [DOI] [PubMed] [Google Scholar]
- 4.Thakran S, Zhang Q, Morales-Tirado V, et al. Pioglitazone restores IGFBP-3 levels through DNA pK in retinal endothelial cells cultured in hyperglycemic conditions. Invest Ophthalmol Vis Sci 2014;56:177–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Idris I, Warren G, Donnelly R. Association between thiazolidinedione treatment and risk of macular edema among patients with type 2 diabetes. Arch Intern Med 2012;172:1005–11. [DOI] [PubMed] [Google Scholar]
- 6.Fong DS, Contreras R. Glitazone use associated with diabetic macular edema. Am J Ophthalmol 2009;147:583–6. [DOI] [PubMed] [Google Scholar]
- 7.Chen X, Rong SS, Xu Q, et al. Diabetes mellitus and risk of age-related macular degeneration: a systematic review and meta-analysis. PLoS One 2014;9:e108196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herzlich AA, Ding X, Shen D, et al. Peroxisome proliferator-activated receptor expression in murine models and humans with age-related macular degeneration. Open Biol J 2009;2:141–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CATT Research Group, Martin DF, Maguire MG, et al. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med 2011;364:1897–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spaide RF, Jaffe GJ, Sarraf D, et al. Consensus Nomenclature for reporting neovascular age-related macular degeneration data: consensus on neovascular age-related macular degeneration nomenclature Study Group. Ophthalmology 2020;127:616–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ambrosius WT, Danis RP, Goff DC, et al. Lack of association between thiazolidinediones and macular edema in type 2 diabetes: the Accord eye substudy. Arch Ophthalmol 2010;128:312–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ku YH, Cho B-J, Kim MJ, et al. Rosiglitazone increases endothelial cell migration and vascular permeability through Akt phosphorylation. BMC Pharmacol Toxicol 2017;18:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Emoto M, Anno T, Sato Y, et al. Troglitazone treatment increases plasma vascular endothelial growth factor in diabetic patients and its mRNA in 3T3-L1 adipocytes. Diabetes 2001;50:1166–70. [DOI] [PubMed] [Google Scholar]
- 14.Karalliedde J, Buckingham R, Starkie M, et al. Effect of various diuretic treatments on rosiglitazone-induced fluid retention. J Am Soc Nephrol 2006;17:3482–90. [DOI] [PubMed] [Google Scholar]
- 15.Sadda SR, Tuomi LL, Ding B, et al. Macular atrophy in the harbor study for neovascular age-related macular degeneration. Ophthalmology 2018;125:878–86. [DOI] [PubMed] [Google Scholar]
- 16.Sharma S, Toth CA, Daniel E, et al. Macular morphology and visual acuity in the second year of the comparison of age-related macular degeneration treatments trials. Ophthalmology 2016;123:865–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grunwald JE, Daniel E, Huang J, et al. Risk of geographic atrophy in the comparison of age-related macular degeneration treatments trials. Ophthalmology 2014;121:150–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peeters LLH, Vigne J-L, Tee MK, et al. Ppar gamma represses VEGF expression in human endometrial cells: implications for uterine angiogenesis. Angiogenesis 2005;8:373–9. [DOI] [PubMed] [Google Scholar]
- 19.Murata T, He S, Hangai M, et al. Peroxisome proliferator-activated receptor-gamma ligands inhibit choroidal neovascularization. Invest Ophthalmol Vis Sci 2000;41:2309–17. [PubMed] [Google Scholar]
- 20.Evans RN, Reeves BC, Maguire MG, et al. Associations of variation in retinal thickness with visual acuity and anatomic outcomes in eyes with neovascular age-related macular degeneration lesions treated with anti-vascular endothelial growth factor agents. JAMA Ophthalmol 2020;138:1043–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shimizu H, Oh-I S, Tsuchiya T, et al. Pioglitazone increases circulating adiponectin levels and subsequently reduces TNF-alpha levels in type 2 diabetic patients: a randomized study. Diabet Med 2006;23:253–7. [DOI] [PubMed] [Google Scholar]
- 22.Marfella R, D’Amico M, Esposito K, et al. The ubiquitin-proteasome system and inflammatory activity in diabetic atherosclerotic plaques: effects of rosiglitazone treatment. Diabetes 2006;55:622–32. [DOI] [PubMed] [Google Scholar]
- 23.Nagineni CN, Kommineni VK, William A, et al. Regulation of VEGF expression in human retinal cells by cytokines: implications for the role of inflammation in age-related macular degeneration. J Cell Physiol 2012;227:116–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giganti M, Beer PM, Lemanski N, et al. Adverse events after intravitreal infliximab (remicade). Retina 2010;30:71–80. [DOI] [PubMed] [Google Scholar]
- 25.Folgar FA, Jaffe GJ, Ying GS. Comparison of age-related macular degeneration treatments trials research Group. Comparison of optical coherence tomography assessments in the comparison of age-related macular degeneration treatments trials. Ophthalmology 2014;121:1956–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available at the following website: https://hyperprod.cceb.med.upenn.edu/catt/catt_index.php


