Abstract
Background
Endoscopic treatment for achalasia (POEM) is a recently introduced technique that incorporates the concepts of natural orifice transluminal surgery. Although pediatric achalasia is rare, POEM has been episodically used in children since 2012. Despite this procedure entails many implications for airway management and mechanical ventilation, evidences about anesthesiologic management are very poor. We conducted this retrospective study to pay attention on the clinical challenge for pediatric anesthesiologists. We put special emphasis on the risk in intubation maneuvers and in ventilation settings.
Results
We retrieved data on children 18 years old and younger who underwent POEM in a single tertiary referral endoscopic center between 2012 and 2021. Demographics, clinical history, fasting status, anesthesia induction, airway management, anesthesia maintenance, timing of anesthesia and procedure, PONV, and pain treatment and adverse events were retrieved from the original database.
Thirty-one patients (3–18 years) undergoing POEM for achalasia were analyzed. In 30 of the 31 patients, rapid sequence induction was performed. All patients manifested consequences of endoscopic CO2 insufflation and most of them required a new ventilator approach. No life-threatening adverse events have been detected.
Conclusions
POEM procedure seems to be characterized by a low-risk profile, but specials precaution must be taken. The inhalation risk is actually due to the high rate of full esophagus patients, even if the Rapid Sequence Induction was effective in preventing ab ingestis pneumonia. Mechanical ventilation may be difficult during the tunnelization step. Future prospective trials will be necessary to individuate the better choices in such a special setting.
Keywords: Pediatric anesthesia, Endoscopy, Adverse events, Rapid sequence induction, Mechanical ventilation
Introduction
Peroral endoscopy myotomy (POEM) is a new endoscopic technique for the treatment of achalasia, which encompasses the concepts of natural orifice transluminal endoscopic surgery [1].
Since the first human case was performed in Japan in 2008 [2], this procedure has been successfully tested on more than 5000 adult patients nowadays. Although pediatric achalasia is rare, POEM has also been successfully used for the treatment of symptomatic children since 2012 [3].
POEM combines the benefits of a minimally invasive, endoscopic, transoral procedure, with the long-term efficacy of a surgical myotomy, so for achalasia disorder, it has emerged as a first-line treatment [4]. The procedure includes incision of the esophageal mucosa, dissection of the submucosa facilitated by insufflation of carbon dioxide (CO2), and myotomy of the esophageal muscular layer and requires special and often challenging anesthesiological management [5–7].
Esophageal clearance is severely compromised, and frequently, at the time of surgery, esophagus is still full of food. Furthermore, during the procedure, large volumes of carbon dioxide are inflated through the submucosal space into the mediastinum and the abdominal cavity, with possibly severe impairment of ventilation due to subcutaneous emphysema, capnomediastinum, capnoperitoneum, and pneumothorax [8].
Some studies about anesthesiological management are extrapolated from adult literature, while in the pediatric field the evidence is very poor, existing with only a few reports, focused on surgical procedures.
We perform a retrospective chart review about the anesthesiological management of 31 children who underwent POEM in a single center: we underline the clinical challenge in the perioperative period focusing on the risk in intubation maneuvers and ventilation management.
Materials and methods
This retrospective study was approved by local IRB (prot.5486/14). All the patients underwent POEM at a single tertiary referral endoscopic center between January 2012 and December 2021. They were retrospectively identified from a prospectively collected database. Patients, who were younger than 18 years old at the time of the procedure, were included in this study.
Demographics, clinical history, fasting status, anesthesia induction, airway management, anesthesia maintenance, the timing of anesthesia and procedure, post-operative nausea and vomiting (PONV), pain treatment, and adverse events were retrieved from the original database and medical charts.
Data were collected in a prospective database (Microsoft Excel) and password protected. Parametric data were presented as mean data and range. Based on the small size of our sample, and on the descriptive presentation of data, statistical analysis for determination of risk odd ratio for each factor was not allowed. The study was conducted following the ethical principles outlined in the Declaration of Helsinki.
Results
We collected a total of 31 patients. The firsts 6 procedures were scheduled in the operating room, but since 2013 POEM was performed exclusively in an endoscopic suite.
Preclinical assessment at the hospitalization the day before the procedure is summarized in Table 1. American Society of Anesthesiologists (ASA) class was assessed as II in 25 patients for the only presence of achalasia and nutritional status, as III in 6 patients for other pathologies (1 Down Syndrome affected by major heart disease; 1 hemiplegia due to oncologic neurosurgery; 4 chronic pulmonary disease, related with esophageal reflux). Preoperative preparation in the ward was standardized, similarly to our adult patients [9].
Table 1.
Demographic and procedural data
| 31 patients data | ||
|---|---|---|
| Number | Range | |
| M/F | 18/13 | |
| Age (years) | 11.8 | (3–18) |
| Weight (kg) | 39.1 | (11–75) |
| Height (cm) | 154.6 | (95–183) |
| ASA III/II (excepted for malnutrition) | 6/25 | |
| Timing of surgery (min)a | 49.3 | (14–82) |
| Timing of anesthesia (min)a | 109.6 | (60–165) |
| Timing of discharge (min)a | 66 | (48–90) |
aThis value excluded 2 procedures aborted before conclusions due to surgical issue
After two days of a clear liquid diet, the 24 h before the procedure adult patients could take just water, while an intravenous glucose solution assured the caloric intake in smaller patients (10/31, 32%).
On the day of the procedure, the antibiotic prophylaxis with clindamycin 20 mg/kg (600 mg maximum) and Cefazolin 30 mg/kg (2 g maximum) was administered iv 30 min before the beginning.
As in adults, a precautionary nasogastric tube was not placed before the procedure, except in one child, but no esophagus content was found.
Anesthesia induction was performed by intravenous drugs in all patients: in one case the anesthesiologist performed a standard induction with propofol, cis-atracurium, and fentanyl; in the other cases a rapid sequence induction (RSI), administering propofol (30/30), rocuronium (26/30) or succinylcholine (4/30) and fentanyl (15/30), remifentanil (4/30) or both (11/30), was preferred. Intubation was easily performed (Cormack 1 was reported in all patients) and no episode of ab ingestis pneumonia occurred. However, in 4 patients (12.9%), the laryngoscopy revealed the presence of some residue in the pharynx, and in 15 patients (48.4%), the endoscopy reported food debris.
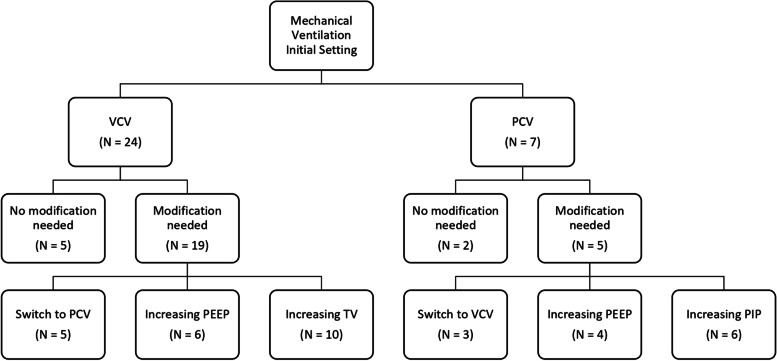
General anesthesia was maintained with sevoflurane (25/31, 80.64%), desflurane (5/31, 16.1%), or propofol-target controlled infusion (1/31, 3.2%). Mechanical ventilation setup was volume controlled (VCV) (24/31, 77.42%) and pressure controlled (PCV) (7/31, 22.58%). In all patients, a standard positive end-expiratory pressure (PEEP) of 4–5 cm H2O was ensured.
In addition to opiates chosen for the induction, analgesia was improved by acetaminophen (31/31, 100%) and tramadol (12/31, 38.7%), while the PONV prophylaxis was ensured with iv dexamethasone before induction.
Two procedure was aborted because of technical difficulties in submucosal tunnelization, due to fibrosis. There was no anesthesiological indication to discontinue the procedure. However, many cases required adjustments in ventilation, because of an increase in peak inspiratory pressure (maximum value reported was 32 mmHg over the PEEP) or in EtCO2 values (maximum value reported was 60 mmHg) during the submucosal tunneling.
All patients manifested some transient signs of endoscopic CO2 insufflation (pneumomediastinum, pneumoperitoneum, and subcutaneous emphysema) but no one required any clinical therapy. Neither tension pneumothorax nor other life-threatening events were reported.
The mean time of surgery was 49.3 +/− 17 min, with an extubation time of 11 +/− 4 min. Once extubated all patients were observed in the recovery room for a mean period of 66 +/− 24 min. Mild analgesic rescue (tramadol) was administered in 7 patients (22.58%), while 1 received a stronger opiate (3.22%) (morphine). PONV occurred in 5 patients (16.13%), but it was effectively treated with ondansetron. No emergence agitation was reported. One case of transient bronchospasm without desaturation occurred in the recovery room, but therapy with salbutamol puffs and betamethasone iv quickly restored the normal pulmonary function.
All patients were regularly transferred to the ward and started feeding within 48 h, with discharge scheduled for the second postoperative day. A mild case of ab ingestis occurred in a 3-year-old baby in the second postoperative day, delaying discharge to the 8th day.
Discussion
POEM procedure requires a specific anesthesiologic approach concerning strategy, risk, and possible adverse events. In 2014, Tanaka et al. made suggestions for adults [10], even though the first prospective study dates from 2015 [5], while in children the experience with this new procedure is limited (Table 2).
Table 2.
Literature data about POEM in pediatric population
| Pts | Mean age (years) | Symptoms duration (months) | Timing of procedure (min) | Procedural adverse events | Occupant days | |
|---|---|---|---|---|---|---|
|
Maselli R Endoscopy [3] |
1 | 3 | No data | 190 | None | No data |
|
Familiari P J Ped Gastr Nut [11] |
3 | 9.5 (9–11) | 17(3–36) | 60.6 (49–76) | 1 Mucosal Perforation | 5 (4–7) |
|
Li C J Ped Surg [12] |
9 | 14.1 (10–17) | 26.4 (6–60) | 56.7 (45–105) |
1 esophagitis 1 subcutaneous emphysema |
No data |
|
Tang X Pediatr Surg Int [13] |
5 | 14.7 (12–17) | 6.3 (1.5–12) | 56 (40–90) | None | 7 (5–13) |
|
Caldaro T J Pediatr Surg [14] |
9 | 12.2 (6–17) | No data | 62 (49–74) |
1 pneumoperitoneum 1 perforation 1 GERD |
4.1 (2–7) |
|
Chen W Gatroint End [15] |
27 | 13.8 (6–17) | 17 (0.2–36) | 39.4 (21–90) |
1 pneumothorax 2 pneumoperitoneum 5 mucosal perforation 1 fever 2 severe pain 4 GERD |
3.2 (1–7) |
|
Filser J Eur J Ped Surg Rep [16] |
1 | 10 | 18 | 93 | None | 3 |
|
Petrosyan J Pediatr Surg [17] |
2 | No data | No data | No data |
1 pneumothorax 1 GERD |
No data |
GERD Gastroesophageal reflux disease
This procedure has been seldom implemented in young patients for prudential reasons, but the good outcomes experienced in adult patients have led endoscopists to apply POEM also to younger patients.
The first point to be assessed is the risk of regurgitation at induction of anesthesia. To avoid aspiration literature suggests a pre-surgery liquid diet, withholding oral intake 24 h before, antacid therapy, and the use of rapid sequence induction [8]. Despite the fasting, in all patients with achalasia, residual food debris should always be suspected. Indeed, in our series, only 52% of patients had the esophagus completely empty at the beginning of the procedure.
Moreover, in children, prolonged fasting can lead to ketoacidosis and hypoglycemia [18], further worsening a nutritional status already debilitated by previous dysphagia [19]. Right now, there is no evidence that this approach improves esophageal clearance.
Although medical therapy has been demonstrated efficient in the reduction of lower esophageal sphincter (LES) pressure [20, 21], children were never premedicated. A pre-procedural treatment with nifedipine [22] or nitrates [23] could be useful in emptying improvement, but there is evidence neither on this approach.
In some centers, an active draining of esophageal content is performed in children as well as in adult patients. In our series, only one anesthesiologist chose to place preoperatively an orogastric tube. In all other cases (30/31), the performer deemed that the risk of the tube positioning outweighed the benefits. Indeed, the esophageal content could be either liquid (i.e., secretion, saliva) or solid (food debris), so no withdrawable. On the contrary, it should be taken into account the real risk of esophageal perforation [24], also considering the esophageal muscular wall alterations.
Performing an esophagoscopy for evacuation of solid esophageal contents within a few hours before POEM is suggested in adults [8–10]. Nabi et al. described a pre-operative endoscopy in children under light sedation [25], but the poor compliance of pediatric patients would require higher doses of sedative drugs, with a bigger risk for airway protection. Furthermore, the traditional fear of inhalation at induction must be reconsidered. Warner et al. evaluated pulmonary aspiration of gastric contents during the perioperative period in infants and children in 63.180 general anesthesia. Among them, only 24 children inhaled (0.04%) and only 3 patients required mechanical ventilation for more than 48 h [26].
At odds with the previous data, there is even more evidence that the traditional fear of inhalation of food debris, could be disproportionate. Some authors questioned even the rapid sequence induction for the high risk of vomiting in children [27]. The more recent review by Engelhardt et al. confirms the meager number of pulmonary aspirations, as well as highlights the risk linked to hypoxia and traumatic tracheal intubation when this technique is transferred directly into pediatric anesthesia practice [28].
The attitude of our group was more traditional, usually (30/31) preferring the RSI. No complication has been observed, even in smaller children. Sellick maneuver (cricoid pressure to occlude the esophagus during induction) was not performed because, despite current adult guidelines, studies on the pediatric population do not seem to show benefit in preventing regurgitation and potential risk in the airway management [29].
Some considerations are worth to be done about the ventilatory approach. Throughout the entire procedure, a continuous insufflation is performed to achieve a good display of the endoscopic field. Especially during the tunnelization step, when the esophageal wall is dissected, the gas insufflated cross in the points of least resistance, producing pneumediastinum, pneumoperitoneum, and subcutaneous emphysema. Since children’s anatomy is characterized by a smaller abdominal/thoracic cavity, a minimal increase in abdominal pressures could compromise diaphragmatic breathing [30].
In our series, all patients needed some revisions in the ventilator setting regardless of whether volume-controlled ventilation or pressure-controlled ventilation had been applied.
The better mechanical ventilation strategy for a normal pediatric lung is not still defined. Many papers only recognized the pathologic status [31] and most of them were published more than two decades ago [32]. Some indications can be obtained by authors who analyzed the patient’s outcome after several changes in mechanical ventilatory approaches [33], but as for pediatric mechanical ventilation, there is not any scientific evidence, so the anesthesiological management must be driven by personal experience and data from adults [34].
This lack of evidence appears in the extreme variability of the mechanical ventilation approach in our sample, especially when the anesthesiologist has to consider the continuous CO2 insufflation generated by the endoscope. At the beginning of the procedure, VCV was the preferred approach in most of the cases (24/31) and a minimal PEEP (4–5 cm H2O) was ensured in all patients.
Based on the data from the anesthetic chart, the entire sample needed some adjustment in ventilation parameters during the tunnelization and the myotomy. This appears as the most difficult step in ventilation control, due to some alterations in the compliance of the respiratory system. In adults, Tanaka et al. observed an increase of EtCO2 in all patients (until 50 mmHg) but no elevation of inspiratory pressure during mechanical ventilation was reported [10].
In our series both parameters were compromised, suggesting that the differences existing in the pediatric chest wall, compared with adults, [35] were involved. Clinical treatment is extremely variable as results in Fig. 1. Despite this “Brownian motion” profile, no adverse events occurred, suggesting that the ventilator mode used does not have a strong impact on the respiratory adverse events. It is also worth noting that Plateau Pressure (Pplat) was never reported in clinical charts. Although a value above 35 cm H2O in adults is strongly correlated with barotrauma [36], no anesthesiologist used Pplat to guide mechanical ventilation.
Fig. 1.
Modification in mechanical ventilation setting
Some authors tried to evaluate whether the pneumomediastinum and pneumoperitoneum occur using the postoperative CT scan. Abnormal findings were frequently identified on radiological examination, but no correlation was found with the development of complications [37]. Hence, none of these conditions have any real clinical impact on the outcome.
Indeed, at our center, it is not common to perform some types of radiological exams in the postoperative period, especially in pediatric patients.
According to the limited duration of the POEM procedure, the management of analgesia involves the use of short-acting drugs. During the stay in the Recovery Room (mean time 66 min), only 25.8% (8/31) patients required an analgesic rescue (7 with weak opioids and 1 with strong opioids), while 16.1% (5/19?) required an intravenous therapy for PONV.
No serious or life-threatening adverse events have been reported. Only two major complications (supposedly linked to achalasia) occurred, but without sequelae. The length of hospitalization (3 days for each patient) was coherent with literature data, which show a period between 1 and 5 days for the uncomplicated procedures [38].
Considering the level of evidence in our retrospective analysis, the POEM procedure seems to be characterized by a low-risk profile, also in children and adolescents. No serious adverse events occurred and the anesthesiological requirements are within the reach of most of the pediatric anesthesiologists. Thanks to a proper scheduling system in a well-equipped endoscopic suite, instead of an operating room, any difficulties were encountered. Moreover, the execution of the procedure in a more friendly environment is probably positive in reducing the psychological impact on children and their parents.
About anesthesiological issues, data that emerged from our case series are quite comforting. The inhalation risk is due to the high rate of full esophagus patients, but the RSI was effective in preventing ab ingestis pneumonia.
The mechanical ventilation may be difficult during the tunnelization step, but in any case, the procedure had to be delayed or stopped. According to literature, there is no recommendation on optimal intraoperative ventilation strategy. The set tidal volume or inspiratory pressures need to be changed according to EtCO2 and Pplat, while a certain level of PEEP in the range of 4–8 cmH20 is necessary to prevent atelectasis.
Our experience would like to help fill the gap in pediatric management, reporting a significant case series, even considering the rarity of achalasia, mostly in children. However, considering the lack of evidence and the limited sample, we cannot make general recommendations. Future prospective trials are necessary to find better options in a such special setting.
Clinical trial registration number
Not applicable.
Abbreviations
- ASA
American Society of Anesthesiology
- CO2
Carbon dioxide
- EtCO2
End-tidal CO2
- GERD
Gastroesophageal reflux disease
- PCV
Pressure controlled ventilation
- PEEP
Positive end-expiratory pressure
- POEM
Peroral endoscopy myotomy
- PONV
Post-operative nausea and vomiting
- RSI
Rapid sequence induction
- SD
Standard deviation
Authors’ contributions
Fabio Sbaraglia and Pietro Familiari contributed to the conceptualization, investigation, supervision, writing—first draft, review, and editing. Federica Maiellare and Marco Mecarello contributed to the statistical analysis and writing—review and editing. Annamaria Scarano, Demetrio Del Prete, Rosa Lamacchia, and Federica Antonicelli contributed to the conceptualization, investigation, and editing. Marco Rossi contributed to the conceptualization and writing—review and editing. All the authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
Support was provided solely from institutional and/or departmental sources.
Availability of data and materials
All data are available under request to the corresponding author.
Declarations
Ethics approval and consent to participate
IRB Number 5486/14 Comitato Etico UCSC Rome Italy. This research accomplishes with all the international requirements for ethics in research.
Competing interests
No potential conflict of interest relevant to this article was reported.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Eleftheriadis N, Inoue H, Ikeda H, Onimaru M, Maselli R, Santi G. Submucosal tunnel endoscopy: peroral endoscopic myotomy and peroral endoscopic tumor resection. World J Gastrointest Endosc. 2016;8(2):86–103. doi: 10.4253/wjge.v8.i2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42(4):265–271. doi: 10.1055/s-0029-1244080. [DOI] [PubMed] [Google Scholar]
- 3.Maselli R, Inoue H, Misawa M, Ikeda H, Hosoya T, Onimaru M, et al. Peroral endoscopic myotomy (POEM) in a 3-year-old girl with severe growth retardation, achalasia, and Down syndrome. Endoscopy. 2012;44 Suppl 2 UCTN:E285–E287. doi: 10.1055/s-0032-1309924. [DOI] [PubMed] [Google Scholar]
- 4.Kim JY, Min YW. Peroral endoscopic myotomy for esophageal motility disorders. Clin Endosc. 2020;53(6):638–645. doi: 10.5946/ce.2020.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang D, Pannu D, Zhang Q, White JD, Draganov PV. Evaluation of anesthesia management, feasibility and efficacy of peroral endoscopic myotomy (POEM) for achalasia performed in the endoscopy unit. Endosc Int Open. 2015;3(4):E289–E295. doi: 10.1055/s-0034-1391965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goudra B, Singh PM, Gouda G, Sinha AC. Peroral endoscopic myotomy-initial experience with anesthetic management of 24 procedures and systematic review. Anesth Essays Res. 2016;10(2):297–300. doi: 10.4103/0259-1162.171462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jayan N, Jacob JS, Mathew M, Mukkada RJ. Anesthesia for peroral endoscopic myotomy: a retrospective case series. J Anaesthesiol Clin Pharmacol. 2016;32(3):379–381. doi: 10.4103/0970-9185.188829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Löser B, Werner YB, Punke MA, Saugel B, Haas S, Reuter DA, et al. Anesthetic considerations for patients with esophageal achalasia undergoing peroral endoscopic myotomy: a retrospective case series review. Can J Anaesth. 2017;64(5):480–488. doi: 10.1007/s12630-017-0820-5. [DOI] [PubMed] [Google Scholar]
- 9.Familiari P, Gigante G, Marchese M, Boskoski I, Tringali A, Perri V, et al. Peroral endoscopic myotomy for esophageal achalasia: outcomes of the first 100 patients with short-term follow-up. Ann Surg. 2016;263(1):82–87. doi: 10.1097/SLA.0000000000000992. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka E, Murata H, Minami H, Sumikawa K. Anesthetic management of peroral endoscopic myotomy for esophageal achalasia: a retrospective case series. J Anesth. 2014;28(3):456–459. doi: 10.1007/s00540-013-1735-0. [DOI] [PubMed] [Google Scholar]
- 11.Familiari P, Marchese M, Gigante G, Boskoski I, Tringali A, Perri V, et al. Peroral endoscopic myotomy for the treatment of achalasia in children. J Pediatr Gastroenterol Nutr. 2013;57(6):794–797. doi: 10.1097/MPG.0b013e3182a803f7. [DOI] [PubMed] [Google Scholar]
- 12.Li C, Tan Y, Wang X, Liu D. Peroral endoscopic myotomy for treatment of achalasia in children and adolescents. J Pediatr Surg. 2015;50(1):201–205. doi: 10.1016/j.jpedsurg.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 13.Tang X, Gong W, Deng Z, Zhou J, Ren Y, Zhang Q, et al. Usefulness of peroral endoscopic myotomy for treating achalasia in children: experience from a single center. Pediatr Surg Int. 2015;31(7):633–638. doi: 10.1007/s00383-015-3717-9. [DOI] [PubMed] [Google Scholar]
- 14.Caldaro T, Familiari P, Romeo EF, Gigante G, Marchese M, Contini AC, et al. Treatment of esophageal achalasia in children: today and tomorrow. J Pediatr Surg. 2015;50(5):726–730. doi: 10.1016/j.jpedsurg.2015.02.047. [DOI] [PubMed] [Google Scholar]
- 15.Chen WF, Li QL, Zhou PH, Yao LQ, Xu MD, Zhang YQ, et al. Long-term outcomes of peroral endoscopic myotomy for achalasia in pediatric patients: a prospective, single-center study. Gastrointest Endosc. 2015;81(1):91–100. doi: 10.1016/j.gie.2014.06.035. [DOI] [PubMed] [Google Scholar]
- 16.Filser J, Dick A, Meyer T, Germer CT, von Rahden BH. Peroral endoscopic myotomy for the treatment of achalasia in a 10-year-old male patient. Eur J Pediatr Surg Rep. 2015;3(1):18–22. doi: 10.1055/s-0034-1372461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Petrosyan M, Khalafallah AM, Guzzetta PC, Sandler AD, Darbari A, Kane TD. Surgical management of esophageal achalasia: evolution of an institutional approach to minimally invasive repair. J Pediatr Surg. 2016;51(10):1619–1622. doi: 10.1016/j.jpedsurg.2016.05.015. [DOI] [PubMed] [Google Scholar]
- 18.Dennhardt N, Beck C, Huber D, Nickel K, Sander B, Witt LH, et al. Impact of preoperative fasting times on blood glucose concentration, ketone bodies and acid-base balance in children younger than 36 months: a prospective observational study. Eur J Anaesthesiol. 2015;32(12):857–861. doi: 10.1097/EJA.0000000000000330. [DOI] [PubMed] [Google Scholar]
- 19.Smits M, van Lennep M, Vrijlandt R, Benninga M, Oors J, Houwen R, et al. Pediatric achalasia in the Netherlands: incidence, clinical course, and quality of life. J Pediatr. 2016;169:110–5.e3. doi: 10.1016/j.jpeds.2015.10.057. [DOI] [PubMed] [Google Scholar]
- 20.Traube M, Hongo M, Magyar L, McCallum RW. Effects of nifedipine in achalasia and in patients with high-amplitude peristaltic esophageal contractions. JAMA. 1984;252(13):1733–1736. doi: 10.1001/jama.1984.03350130047033. [DOI] [PubMed] [Google Scholar]
- 21.Orlando RC, Bozymski EM. Clinical and manometric effects of nitroglycerin in diffuse esophageal spasm. N Engl J Med. 1973;289(1):23–25. doi: 10.1056/NEJM197307052890106. [DOI] [PubMed] [Google Scholar]
- 22.Maksimak M, Perlmutter DH, Winter HS. The use of nifedipine for the treatment of achalasia in children. J Pediatr Gastroenterol Nutr. 1986;5:883–886. doi: 10.1097/00005176-198611000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Wen ZH, Gardener E, Wang YP (2004) Nitrates for achalasia. Cochrane Database Syst Rev. 2004;2004(1):CD002299. [DOI] [PMC free article] [PubMed]
- 24.Gander JW, Berdon WE, Cowles RA. Iatrogenic esophageal perforation in children. Pediatr Surg Int. 2009;25(5):395–401. doi: 10.1007/s00383-009-2362-6. [DOI] [PubMed] [Google Scholar]
- 25.Nabi Z, Ramchandani M, Chavan R, Darisetty S, Kalapala R, Shava U, et al. Outcome of peroral endoscopic myotomy in children with achalasia. Surg Endosc. 2019;33(11):3656–3664. doi: 10.1007/s00464-018-06654-1. [DOI] [PubMed] [Google Scholar]
- 26.Warner MA, Warner ME, Warner DO, Warner LO, Warner EJ. Perioperative pulmonary aspiration in infants and children. Anesthesiol. 1999;90:66–71. doi: 10.1097/00000542-199901000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Scrimgeour GE, Leather NW, Perry RS, Pappachan JV, Baldock AJ. Gas induction for pyloromyotomy. Paediatr Anaesth. 2015;25(7):677–680. doi: 10.1111/pan.12633. [DOI] [PubMed] [Google Scholar]
- 28.Engelhardt T. Rapid sequence induction has no use in pediatric anesthesia. Paediatr Anaesth. 2015;25(1):5–8. doi: 10.1111/pan.12544. [DOI] [PubMed] [Google Scholar]
- 29.Kojima T, Harwayne-Gidansky L, Shenoi A, Owen E, Napolitano N, Rehder K, et al. Cricoid pressure during induction for tracheal intubation in critically ill children: a report from National Emergency Airway Registry for Children. Pediatr Clin Care Med. 2018;19(6):528–537. doi: 10.1097/PCC.0000000000001531. [DOI] [PubMed] [Google Scholar]
- 30.Halachmi S, El-Ghoneimi A, Bissonnette B, Zaarour C, Bagli DJ, McLorie GA, et al. Hemodynamic and respiratory effect of pediatric urological laparoscopic surgery: a retrospective study. J Urol. 2003;170(4 Pt 2):1651–1654. doi: 10.1097/01.ju.0000084146.25552.9c. [DOI] [PubMed] [Google Scholar]
- 31.Conti G, Piastra M. Mechanical ventilation for children. Curr Opin Crit Care. 2016;22(1):60–66. doi: 10.1097/MCC.0000000000000271. [DOI] [PubMed] [Google Scholar]
- 32.Benjamin PK, Thompson JE, O’Rourke PP. Complications of mechanical ventilation in a children’s hospital multidisciplinary intensive care unit. Respir Care. 1990;35:873–878. [PubMed] [Google Scholar]
- 33.Albuali WH, Singh RN, Fraser DD, Seabrook JA, Kavanagh BP, Parshuram CS, et al. Have changes in ventilation practice improved outcome in children with acute lung injury? Pediatr Crit Care Med. 2007;8:324–330. doi: 10.1097/01.PCC.0000269390.48450.AF. [DOI] [PubMed] [Google Scholar]
- 34.Kneyber MC. Intraoperative mechanical ventilation for the pediatric patient. Best Pract Res Clin Anaesthesiol. 2015;29(3):371–379. doi: 10.1016/j.bpa.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 35.Papastamelos C, Panitch HB, England SE, et al. Developmental changes in chest wall compliance in infancy and early childhood. J Appl Physiol. 1995;78:179–184. doi: 10.1152/jappl.1995.78.1.179. [DOI] [PubMed] [Google Scholar]
- 36.Boussarsar M, Thierry G, Jaber S, Roudot-Thoraval F, Lemaire F, Brochard L. Relationship between ventilatory settings and barotrauma in the acute respiratory distress syndrome. Intensive Care Med. 2002;28(4):406–413. doi: 10.1007/s00134-001-1178-1. [DOI] [PubMed] [Google Scholar]
- 37.Yang S, Zeng MS, Zhang ZY, Zhang HL, Liang L, Zhang XW. Pneumomediastinum and pneumoperitoneum on computed tomography after peroral endoscopic myotomy (POEM): postoperative changes or complications? Acta Radiol. 2015;56(10):1216–1221. doi: 10.1177/0284185114551399. [DOI] [PubMed] [Google Scholar]
- 38.Stavropoulos SN, Modayil RJ, Friedel D, Savides T. The International Per Oral Endoscopic Myotomy Survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc. 2013;27:3322–3338. doi: 10.1007/s00464-013-2913-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available under request to the corresponding author.