Abstract
Children with Fetal Alcohol Spectrum Disorders (FASD) have significant social skills deficits. The efficacy of a Child Friendship Training (CFT) versus a Delayed Treatment Control (DTC) was assessed for 100 children ages 6 to 12 years with FASD. Children in the CFT showed clear evidence of improvement in their knowledge of appropriate social behavior; and, according to parent report, CFT resulted in improved social skills and fewer problem behaviors when compared to DTC. These gains were maintained at 3-month follow up. After receiving treatment, the DTC group exhibited similar improvement. Teachers did not report improvement as a function of social skills treatment. Findings suggest that children with FASD benefit from CFT but these social skills gains may not be observed in the classroom.
Keywords: Fetal Alcohol Spectrum Disorders, Social Skills Training
In 1996, the Institute of Medicine (IOM; Stratton, Howe, & Battaglia, 1996) released a report containing broadly defined diagnostic criteria for Fetal Alcohol Syndrome (FAS), partial FAS, Alcohol-Related Birth Defects (ARBD), and Alcohol-Related Neurodevelopmental Disorders (ARND). These diagnostic categories represent a continuum of effects and are subsumed under the term Fetal Alcohol Spectrum Disorders (FASD; Streissguth & O’Malley, 2000). It is estimated that, in the United States, about 1 in 100 children born each year has FASD, resulting in substantial life-long impairments in neurocognitive and socioemotional development (May & Gossage, 2001).
Studies reveal that children with FASD have multiple developmental deficits including inattention and hyperactivity, poor language performance, as well as problems in memory and executive functioning (for review see Mattson & Riley, 1998; Rasmussen, 2005; Streissguth & O’Malley, 2000). Alarmingly, these neurocognitive deficits have been documented even in the offspring of women who drank light to moderate amounts of alcohol and who do not meet criteria for a diagnosis of FAS (Jacobson & Jacobson, 2002; O’Connor, Sigman, & Kasari, 1993; Sood, Delancy-Black, Covington et al., 2001).
Likely as a consequence of the primary deficits described, children with FASD exhibit considerable social impairment. Problems understanding social cues, indiscriminant social behavior, and difficulty communicating in social contexts are reported (Streissguth, 1997). Both caregivers (Roebuck, Mattson, & Riley, 1999) and teachers (Brown et al., 1991) have rated children with prenatal exposure to alcohol as having poorer social skills than unexposed children, even after controlling for differences in cognitive functioning (Thomas, Kelly, Mattson, & Riley, 1998; Whaley, O’Connor, & Gunderson, 2001). Furthermore, studies of adolescents and adults with FASD indicate that social skills deficits continue into adulthood (Carmichael-Olson, Feldman, Streissguth, Sampson, & Bookstein, 1998).
Why Social Competence is Important
In typically developing children, best friends promote the development of social competence (Nelson & Aboud, 1985). In contrast, children with poor social skills acquire negative reputations among peers concomitant with social rejection (Frankel & Feinberg, 2002). Having one or two best friends is important to later adjustment, can buffer the impact of stressful life events, and correlates positively with self-esteem and negatively with anxious and depressive symptoms (Buhrmester, 1990; Frankel & Myatt, 1996). The association between poor peer relationships and both juvenile delinquency and early school drop out also has been well documented (Paetsch & Bertrand, 1997; Patterson, Forgatch, Yoerger, & Stoolmiller, 1998).
Regarding children with FASD specifically, research suggests that exposed children without mental retardation may be at greatest risk for poor adaptation. In a study using parent report, alcohol exposed children with less cognitive impairment were found to be more likely than children with mental retardation to exhibit antisocial behavior, lack of consideration for the rights and feelings of others, and resistance to limits and requests of authority figures (Roebuck et al., 1999). Additionally, children with exposure but without FAS are more likely to have conduct problems suggestive of early delinquency when compared to children with the full syndrome (Schonfeld, Mattson, & Riley, 2005). These findings are consistent with the high rate of delinquency and school failure found in alcohol-exposed adolescents with higher IQs but without FAS (Streissguth, Barr, Kogan, & Bookstein, 1996). Given the high percentage of individuals with prenatal exposure to alcohol who have significant social problems as they grow older, it is important to begin early promote adequate social problem solving and competence.
Previous Research on Efficacy of Social Skills Training with Children
Research on the efficacy of social skills training for children with high incidence disabilities reveals considerable variability in outcomes (for review see Gresham, Sugai, & Horner, 2001). Various meta-analyses suggest that, in many studies, social skills training has not produced large, long-term, or generalized changes in social competence. The most successful programs appear to include a combination of modeling and rehearsal (with coaching and performance feedback); provide treatment prior to adolescence; use socially valid outcome measures; and translate socially skill behaviors to naturalistic settings.
The Need for Parent Involvement and Education in Treatment Programs
Parent involvement has been notably absent from most social skills training interventions, which may also explain the lack of generalization found in many of these studies (Gresham et al., 2001). It is reasonable to expect that parent involvement would enhance treatment generalization, especially since parents typically play a major role in arranging and supervising children’s play experiences. Available evidence suggests that parent involvement is essential in helping children develop positive peer relationships (Parke, Neville, Burks, Boyum, & Carson, 1994). For example, young children exhibit higher rates of cooperation, turn taking, and longer play encounters when actively supervised by an adult than when playing without assistance (Bhavnagri & Parke, 1991); and children with parents who facilitate contact with peers have more consistent play partners than children of parents who are less active in initiating peer contacts (Frankel, Myatt, Cantwell, & Feinberg, 1997a, 1997b; Ladd, Profilet, & Hart, 1992).
More so than unexposed children, children with prenatal alcohol exposure present with complex problems requiring the assistance of their parents in guiding their play and in arranging opportunities for peer interactions. Clinical reports from parents reveal that these children often have poor strategies for entering and maintaining successful play interactions. Problems in impulse control and low frustration tolerance make it difficult for them to ignore teasing and avoid conflict situations (Streissguth & O’Malley, 2000). For these reasons, treatment facilitated by parents is especially important for children with FASD in order to help them to generalize skills learned to naturalistic settings.
Purpose of the Present Research
In order to assist children with FASD to achieve more success in peer friendships, the aims of the current study were: (1) To examine the impact of parent-assisted Children’s Friendship Training (CFT; Frankel & Myatt, 2003) compared to a Delayed Treatment Control (DTC) on the social skills of children with a history of prenatal alcohol exposure; and (2) To examine the maintenance of social skills gains over a 3-month period. The innovation afforded by this study is in its reliance on parents as facilitators of social competence in their children and in its use with a unique sample of children with developmental disabilities. No previous studies have systematically implemented social skills training for children with FASD and, to our knowledge, this is the first controlled study of its kind on this population.
Method
The study was conducted at the University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior. Prior to the initiation of the study, the UCLA and the Centers for Disease Control and Prevention Institutional Review Boards approved all procedures and a Certificate of Confidentiality was obtained from the National Institute of Alcohol Abuse and Alcoholism. Participants were recruited through letters mailed to local health care and community providers (e.g., pediatricians, YMCA, schools) and flyers posted within the UCLA Semel Institute, medical center, and the community. Interested families contacted the project coordinator who conducted a screening interview by telephone to determine initial eligibility. Informed consent was obtained from the parent (s) and assent from children ≥7 years of age.
Participants
Participants were recruited from February 2003 to February 2005. Children were eligible if they were between 6 and 12 years of age, had documented prenatal alcohol exposure, measurable social skills deficits (− 1 standard deviation below the mean) on the Socialization domain of the Vineland Adaptive Behavior Scales (VABS; Sparrow, Balla, & Cicchetti, 1984), and a verbal IQ of ≥ 701 on the Kaufman Brief Intelligence Test (K-BIT; Kaufman & Kaufman, 1990). Children were not admitted if they had major sensory or motor deficits, or a past diagnosis of mental retardation or pervasive developmental disorder. No parent could be currently abusing alcohol as measured by the Alcohol Use Disorders Identification Test (AUDIT; Babor, De la Fuente, Saunders, & Grant, 1989).
Recruitment efforts yielded a total of 183 families who agreed to be screened for initial eligibility. Following screening, 126 children met initial eligibility requirements. Failure to meet these requirements included alcohol exposure levels too low (n = 28), no reliable documentation of alcohol exposure (n = 19), a previous diagnosis of mental retardation (n = 4) or pervasive developmental disorder (n = 6). Of the 126 children who were scheduled for final eligibility, 20 families did not keep their appointments. These families did not differ from the final sample families on variables of child age, gender, or ethnicity. Of the 106 who came in for final eligibility assessment, 6 children were deemed ineligible for participation. Two children were excluded because they met criteria for pervasive developmental disorder, one child had an IQ < 55 on the K-BIT, one child did not have social skills deficits as defined by the VABS, and the mothers of two children reported less drinking (below eligibility criterion) when questioned during final eligibility testing than they did during initial screening. A total of 100 children met final eligibility requirements and all families agreed to participate. See Tables 1 and 2.
Table 1.
Sample Characteristics and Comparison of Children’s Friendship Training (CF) and Delayed Treatment Control (DTC) Conditions
| Variables | Total Sample (N = 100) |
CFT (n = 51) |
DTC (n = 49) |
|---|---|---|---|
| Ethnicity (%) | |||
| White, Non Hispanic | 54.0 | 56.9 | 51.0 |
| Black, Non Hispanic | 17.0 | 11.8 | 22.4 |
| Hispanic | 17.0 | 19.6 | 14.3 |
| Asian | 2.0 | 2.0 | 2.0 |
| Mixed | 10.0 | 9.8 | 10.2 |
| Child Gender-Males (%) | 51.0 | 56.9 | 44.9 |
| Child Age in Years (M, SD) | 8.59 (1.56) | 8.32 (1.47) | 8.66 (1.65) |
| Child Composite IQ (M, SD) a | 97.24 (14.83) | 95.53 (17.14) | 99.02 (11.88) |
| Child Verbal IQ b | 93.58 (14.73) | 92.59 (16.78) | 94.61 (12.32) |
| Child Socialization c | 62.83 (8.04) | 63.53 (7.97) | 62.10 (8.14) |
| Biological Mother (%) | 21.0 | 17.6 | 24.5 |
| Number of Placements (M, SD) | 2.18 (0.20) | 2.29 (0.28) | 2.06 (0.27) |
| Primary Caregiver Married/Partner (%) | 62.0 | 62.8 | 61.2 |
| Primary Caregiver Yrs Education (M, SD) | 16.28 (0.26) | 16.43 (0.35) | 16.12 (0.39) |
| FAS/Partial FAS Present (%) | 56.0 | 52.9 | 59.8 |
Kaufman Brief Intelligence Test Composite IQ
Kaufman Vocabulary Subtest
Vineland Socialization Standard Score
Table 2.
Comparison of Children’s Friendship Training (CF) and Delayed Treatment Control (DTC) Conditions on Baseline Social Skills and Problem Behaviors
| Variables | Total Sample (N = 100) |
CFT (n = 51) |
DTC (n = 49) |
|---|---|---|---|
| Child Knowledge of Social Skills | 11.15 (2.38) | 11.08 (2.42) | 11.22 (2.37) |
| SSRS Social Skills, Parent a | 73.80 (13.09) | 75.22 (14.33) | 72.33 (11.63) |
| SSRS Problem Behaviors, Parent | 123.66 (13.94) | 122.80 (14.63) | 124.55 (13.28) |
| SSRS Social Skills, Teacher | 87.79 (13.05) | 89.94 (11.45) | 85.54 (14.31) |
| SSRS Problem Behaviors, Teacher | 114.12 (15.32) | 112.76 (15.06) | 115.54 (15.62) |
SSRS-Social Skills Rating System
FASD Diagnosis
Every child received a physical examination to assess for the presence of the diagnostic features of FASD using the Diagnostic Guide for Fetal Alcohol Syndrome (FAS) and Related Conditions (Astley, 2004). This system uses a 4-digit diagnostic code reflecting the magnitude of expression of four key diagnostic features of FAS: (1) growth deficiency; (2) the FAS facial phenotype, including short palpebral fissures, flat philtrum, and thin upper lip; (3) CNS dysfunction; and (4) gestational alcohol exposure. Using this code, the magnitude of expression of each feature was ranked independently on a 4-point Likert scale with 1 reflecting complete absence of the FAS feature and 4 reflecting the full manifestation of the feature. The study physician administered this examination after achieving reliability with the senior study clinician who was trained by Dr. Astley. The physician was unaware of the children’s group assignment.
History on prenatal alcohol exposure was obtained from the biological mothers using the Health Interview for Women (O'Connor et al., 2002). For adopted or foster children, medical or legal records documenting known exposure or reliable collateral reports by others who had observed the mother drinking during pregnancy were obtained. Based on this documentation, all children except three 2 were assigned ratings of 3 (“some risk”) or 4 (“high risk”) in the prenatal alcohol exposure category.
After the 4-digit code for each participant was calculated, participant diagnosis was converted to fit the IOM criteria according to the guidelines developed by Dr. Astley (personal communication). Using this conversion, 12% of children were diagnosed with FAS, 44% with Partial FAS, and 44% with ARND. No child met criteria for ARBD.
Study Design and Procedures
A 2-group Child Friendship Training (CFT) or Delayed Treatment Control (DTC) longitudinal design was used. Each consecutive set of 14 to 16 eligible children formed a cohort. After completing all pretreatment assessments, the children within a cohort were assigned, in alternating sequence, to one of the two study conditions (child 1 CFT, child 2 DTC, child 3 CFT, child 4 DTC, etc.), with an attempt to equate groups on gender and ethnicity. In addition, families having two children in the study were allowed to have both children in the same condition (n = 5 in CFT and n = 6 in DTC). Each cohort averaged approximately 7-8 children in each condition. The CFT group received 12 sessions, of 90 minutes in length, delivered over the course of 12 weeks. Parents attended separate concurrent sessions in which they were instructed on key social skills being taught to their children. Incentives included weekly pizza dinners, free baby-sitting for siblings, and $30 for completion of study assessments. On completion of the 12-week intervention, participants in the CFT condition were administered a post treatment assessment. Children for whom treatment had been delayed (DTC) then received the social skills training.3 After completing treatment, the DTC participants were assessed (post treatment). At the same time, the CFT group completed a 3-month follow up assessment.
Treatment Content
The CFT procedure used in this study and all its social skills components are based on social learning theory, have been validated empirically, and have been successfully implemented for children between the ages of 6 and 12 years in multiple clinical contexts (Frankel, 2005). Research has demonstrated that child and parent behaviors within certain critical situations discriminate accepted from rejected children. These critical situations are: (1) social network formation with the aid of the parent (Parke et al., 1994); (2) informational exchange with peers leading to common-ground activities (Black & Hazen, 1990); (3) entry into a group of children already at play (Frankel, 2005); (4) in-home play dates (Frankel & Myatt, 2003); and (5) conflict avoidance and negotiation (Rose & Asher, 1999). The key features of CFT were taught through instruction on simple rules of social behavior; modeling, rehearsal, and performance feedback during treatment sessions; rehearsal at home; homework assignments; and coaching by parents during play with a peer (Elliot & Gresham, 1993). See Table 3 for a description of sessions.
Table 3.
Description of Child and Parent Treatment Sessions
| Session | Topic Child Group |
Goals – Child Group | Topic Parent Group |
Goals – Parent Group |
|---|---|---|---|---|
| 1 | Rules of the group; elements of good communication | Children learn and practice elements of good communication by introducing themselves to one another | Goals and methods of treatment; limitations of intervention: what not to expect | Parents learn about importance of their role in the intervention; group leader reviews context and stability of sociometric categories |
| 2 | Having a conversation | Children learn how to exchange information, good and bad places to make friends | Having a conversation | Parents learn how to help their child develop two-way conversation skills, and how to better communicate with their child |
| 3 | Joining a group of children already at play: “slipping in” | Children learn when, where, and how to “slip in” or join a group of children already at play | Supporting child friendships | Parents learn about appropriate settings for play dates; sources of potential playmates; importance of adequate time availability for play dates |
| 4 | Joining a group of children already at play: “slipping in” | Children learn more techniques for group entry, reasons for rejection from group entry, and what to do in response to rejection | Joining a group of children already at play: “slipping in” | Parents learn when, where, and how their children should “slip in” to a group of children already at play, and importance of their child taking “no” for an answer |
| 5 | How to be a good sport | Children learn and practice basic rules of being a good sport | Joining a group of children already at play: “slipping in” | Parents learn how to help their child practice “slipping in” outside of the session |
| 6 | How to be a good sport | Children learn to praise other children, techniques of persuasion and negotiation. Children practice praising one another while playing games, and negotiating changes in games when they become bored | Appropriate games for play dates | Parents learn appropriate games and games to exclude for indoor and outdoor play |
| 7 | Rules of being a good host | Children learn and practice rules of being the "host" during interactive indoor games | Play dates | Parents learn about sources for potential playmates for their child and physical resources for play dates. Parents learn about their responsibilities for the play date |
| 8 | How to handle teasing | Children learn and practice strategies for reacting neutrally or humorously to teasing, so as to reduce the likelihood of further teasing | How to handle teasing | Parents learn about effective strategies their child can use to handle teasing and are instructed on appropriate role play for practice |
| 9 | Unjustified accusations | Children learn how to handle situations when unjustly accused of bad behavior by an adult | How to handle other adults complaining about child’s behavior | Parents learn how to respond appropriately and effectively to other adults who complain about their child’s behavior so as to minimize their child getting a negative reputation |
| 10 | How to be a good winner | Children learn and practice rules of being a good winner | How to be a good winner | Parents learn rules of being a good winner and how to encourage their child’s practice of those rules |
| 11 | Bullies and conflict situations | Children learn how to avoid conflict and have the opportunity to practice strategies for conflict resolution | Bullies and conflict situations | Parents learn how to support their child’s use of strategies for defusing confrontations with another child |
| 12 | Graduation | Post treatment evaluation, graduation ceremony, and party for the children and their parents | Graduation | Parents complete post treatment evaluation and participate in the child’s graduation ceremony and party |
Therapist Training
Five clinical psychology graduate students provided treatment. The first task of training was to educate the therapists about the developmental challenges faced by children with FASD. This training was followed by the social skills treatment training that began with instruction on the development of children’s friendships, the theoretical and empirical rationale underlying the treatment protocol, and a review of the elements of the CFT adapted for children with FASD. Concomitantly, group leaders became familiar with the treatment by assisting more experienced group leaders in either the parent or child sessions as “coaches” during one complete 12-week treatment cycle with non-participant children. Group leaders then conducted either a child or parent group according to the training they had received.
Treatment Integrity
Treatment integrity was insured consistent with the guidelines of Moncher and Prinz (1991) and was monitored through the use of trained and qualified group leaders, standardized treatment manuals, ongoing weekly supervision, and live monitoring of sessions. Fidelity checklists covering the primary content of the protocol were created for each treatment session. Undergraduate psychology students, trained to reliability, served as coders and coded all sessions live. If a group leader failed to cover any primary content, the coder reminded them during the sessions. Using this method, no substantial deviations from the treatment protocol were noted.
Measures
Eligibility Measures
Health Interview for Women.
All biological mothers were interviewed using the Health Interview for Women (O’Connor, Kogan, & Findlay, 2002), which yields standard measures of the average number of drinks per drinking occasion and the frequencies of those occasions.4 Criteria for alcohol exposure was ≥ 7 drinks per week or ≥ 3 drinks per drinking occasion. In a recent study by Barr and Streissguth (2001), a cut point of ≥ 7 drinks per week had 100% sensitivity and 83% specificity for diagnosis of FASD. In other studies, a cut point of ≥ 3 drinks per drinking occasion has been a statistically significant predictor of behavioral teratogenesis (O’Connor, Sigman & Kasari, 1993; Sood et al., 2001).
Review of Medical Records.
If the biological mother was not available, medical, adoption, or other legal records were obtained documenting prenatal alcohol exposure. Although detailed information regarding exact quantity and frequency of maternal alcohol use was not always available, the records did provide sufficient information to meet the diagnostic criteria outlined in the Diagnostic Guide (Astley, 2004). Examples of such documentation included medical records that indicated the biological mother was intoxicated at delivery, or records indicating that the mother was observed to drink heavily during pregnancy by a reliable collateral source (i.e. grandparent, spouse) or was a registered alcoholic (Russia).
Vineland Adaptive Behavior Scales, Survey Form (VABS)
To qualify for the study, children had to score −1 standard deviation below the mean on the Socialization Scale of the VABS (Sparrow et al., 1984). The VABS is for individuals from birth through 18 years to measure parent assessment of child functioning in communication, self help, social, and motor skills. For children 6 years and older, the motor scale is not scored. The median split-half coefficient for the Socialization Scale is .89 for 6 to 12 year olds and test-retest reliability is .89.
Kaufman Brief Intelligence Test (K-BIT).
The K-BIT is a brief, individually administered measure of verbal and nonverbal intelligence (Kaufman & Kaufman, 1990) composed of two subtests: Vocabulary and Matrices. The Vocabulary subtest was used as an eligibility criterion to ensure that study participants could understand the verbal components of the treatment. The split-half reliability coefficients for the Vocabulary IQ score for children aged 6 to 12 years averages .91 with test-retest reliability of .86 and construct validity with the WISC-R of .78.
Alcohol Use Disorders Identification Test (AUDIT).
The AUDIT, developed by the World Health Organization, was used to assess high risk drinking status of parents or caregivers desiring study participation (Babor et al., 1989). The AUDIT contains 10 items and has been shown to have high sensitivity and specificity (with a weighted score >8) in a six-nation validation trial using heavy drinking as the criterion (Saunders, Aasland, Babor, De la Fuente, & Grant, 1993).
Outcome Measures
Test of Social Skills Knowledge (TSSK).
The TSSK is a 17-item forced choice criterion-based measure designed to assess children’s social skills knowledge (Frankel, 1994). The items, which were read to the child, directly relate to the social skills taught during the CFT intervention. This measure and similar measures have been used successfully in evaluating treatment gains in other studies of social skills training (Frankel & Myatt, 2003; Pfiffner & McBurnett, 1997). Scores range from 0 to 17 with a higher score reflecting higher social skills knowledge.
Social Skills Rating System (SSRS-P and SSRS-T).
Social skills were evaluated with the Social Skills Rating System Parent (SSRS-P) and Teacher (SSRS-T) Forms (Gresham & Elliott, 1990). Two scales comprise the SSRS: Social Skills and Problem Behaviors, presented as standard scores (M = 100; SD = 15). There is an Academic Competence Scale on the teacher version of the SSRS that was not used in this study. The Social Skills scale measures cooperation, assertion, responsibility (parent version only), and self-control. Lower scores represent poorer social functioning. The Problem Behaviors scale measures internalizing, externalizing, and hyperactivity. Higher scores represent greater problem behaviors. The SSRS has high criterion related validity, correlating significantly with other established measures of child social and problem behaviors. The SSRS has high internal consistency (Cronbach’s alpha = .87-.94) and test-retest reliability for parent (.65 and .87) and teacher (.84 and .85) ratings.
Data Analysis Plan
Data analyses were conducted using SPSS Statistical Analysis software (13.0). The children’s knowledge of social skills measure (TSSK), the parent (SSRS-P) and teacher (SSRS-T) measures were assessed at baseline (T1), at the end of the 12-week treatment (T2), and, for the CFT condition, at 3-month follow up (T3). The short-term efficacy of the treatment (Aim 1) was evaluated with separate analyses of covariance (ANCOVA), performed at the group level, using the post treatment (T2) TSSK, parent or teacher SSRS scores as outcome variables. Treatment (CFT versus DTC) was the grouping factor, and baseline scores (T1) on the TSSK, SSRS parent or teacher ratings were used as the primary covariates. Group leader, cohort (i.e., replication), child gender and ethnicity were evaluated in preliminary analyses of models as possible additional covariates. Other possible covariates included child age, IQ, home placement (biological or non biological parent), number of placements, FASD diagnosis, primary caregiver marital status and education. Effect size of treatment was determined by calculating the mean difference between the CFT and DTC groups on each of the three post treatment outcomes (T2) and dividing each difference score by the pooled standard deviation across the groups (Cohen, 1988). The long-term effect of treatment on outcome variables (Aim 2) was evaluated with two-tailed pairwise t tests (T2-T3, T1-T3) on the scores of participants in the CFT condition. Effect sizes for the change over time of the CFT group were estimated by computing the mean change score for each of the pairwise comparisons and dividing by the pooled standard deviation within each pair. Following treatment, these comparisons were repeated for participants in the DTC condition with the exception that there was no 3-month follow up for this group. Sample size was determined using conventional power analyses. With two-tailed alpha = .05 and a sample size = 100, power is .81 to detect a conventional “medium” effect (d = .50) in a two-group ANCOVA with the addition of a baseline covariate accounting for 25% of the variance (i.e. a baseline-post treatment correlation of r = .50).
Results
Participant Attrition
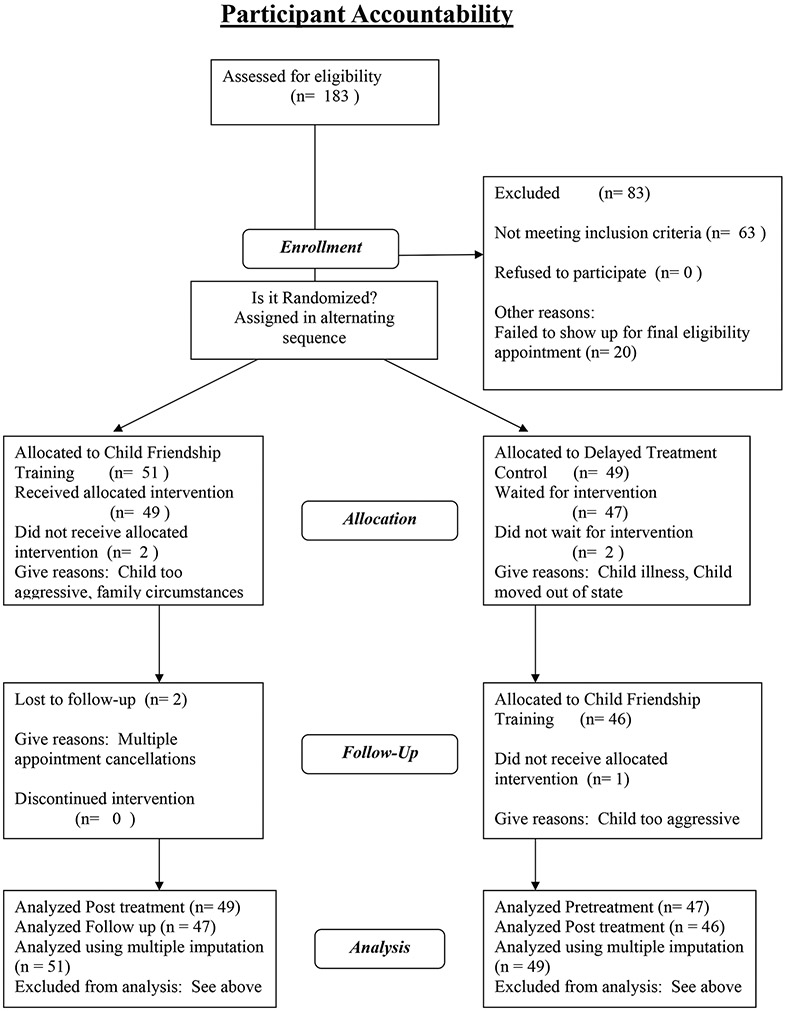
Of the 100 children who were recruited for study, 51 were assigned to the CFT condition and 49 were assigned to the DTC condition. Of that number, 96 children completed the baseline and 12-week post treatment or wait phases of the study (CFT n = 49; DTC n = 47). Two children did not start treatment because of illness or family circumstances (CFT n = 1; DTC n = 1) and two were asked to leave the program because of significant aggressive behavior that could not be safely monitored in the groups (CFT n = 1; DTC n = 1). At the conclusion of the study, 47 children (92%) completed the 3-month follow up assessment in the CFT condition. One sibling pair did not complete the assessment because of multiple failures to show up for their appointment resulting in too great a lapse in time. In the DTC condition, 46 (94%) of the children completed the post treatment assessment following friendship training. One child did not start treatment because the family moved from the area. All analyses were intention to treat and included all participants with outcome data; however, to check for possible effects of missing data on the results, supplemental analyses were done on each of the outcome measures using multiple imputation (Rubin, 1987). As expected, these supplemental analyses were not meaningfully different from the primary analyses, and are not reported further.
Baseline Comparison of CFT to DTC
Chi Square and independent t-tests revealed no statistically significant differences at baseline between the CFT and DTC conditions on study demographic variables or on measures of social skills and problem behaviors. See Tables 1 and 2.
Comparison of CFT to DTC
Children’s Report of Social Skills Knowledge.
To examine the impact of social skills training on children with FASD, a 2 Condition (CFT, DTC) ANCOVA design was used. Analyses were conducted on the scores derived from the Test of Social Skills Knowledge (TSSK) completed by the children. The post treatment score (T2) was the dependent variable and the baseline score (T1) was used as a covariate to control for initial levels. Analyses of variance (ANOVA) and simple correlations revealed no significant associations between variables of group leader, cohort, child gender or ethnicity, home placement, number of placements, caregiver marital status or education and social skills knowledge. As expected, child IQ (r = .43, p < .003) and age (r = .23, p < .03) were related to outcome. In addition, a diagnosis of FAS versus partial FAS/ARND was negatively associated with knowledge of social skills (F (1, 94) = 4.31, p < .05) and so was included in data analysis. After controlling for these variables, the analysis yielded a significant group effect with the children in the CFT showing significantly improved knowledge of appropriate social skills compared to children in the DTC group, F (1, 90) = 57.12, p < .0001, d = 1.28. See Table 4.
Table 4.
Comparison of Children’s Friendship Training (CFT) to Delayed Treatment Control (DTC)
| T1 | T2d | T3e | ||||
|---|---|---|---|---|---|---|
| CFT | DTC | CFT | DTC | CFT | DTC | |
| Variables |
M (SD) n = 51 |
M (SD) n = 49 |
M (SD) n = 49 |
M (SD) n = 47 |
M (SD) n = 47 |
M (SD) n = 46 |
| Child | ||||||
| TSSKa | 11.1 (2.4) | 11.2 (2.4) | 15.0 (2.0) | 12.3 (2.4) | 15.3 (1.4) | 14.9 (2.1) |
| Parent | ||||||
| SSRS-SS b | 75.2 (14.3) | 72.3 (11.6) | 84.4 (14.7) | 77.0 (13.5) | 89.4 (17.4) | 85.2 (15.9) |
| SSRS-PB c | 122.8 (14.6) | 124.6 (13.3) | 116.6 (15.5) | 122.6 (14.1) | 115.0 (15.8) | 118.3 (13.5) |
| Variables |
M (SD) n = 50 |
M (SD) n = 48 |
M (SD) n = 48 |
M (SD) n = 46 |
M (SD) n = 43 |
M (SD) n = 43 |
| Teacher | ||||||
| SSRS-SS | 89.9 (11.5) | 85.5 (14.3) | 89.1 (12.5) | 88.2 (10.5) | 92.0 (11.1) | 90.4 (12.3) |
| SSRS-PB | 112.8 (15.1) | 115.5 (15.6) | 112.4 (12.8) | 113.0 (15.6) | 109.1 (13.3) | 113.1 (13.4) |
Test of Social Skills Knowledge
Social Skills Rating System-Social Skills
Social Skills Rating System-Problem Behaviors
CFT Post treatment; DTC pretreatment
CFT 3-Month Follow up; DTC Post treatment
Parent Report of Social Skills and Problem Behaviors.
A 2 Condition (CFT, DTC) ANCOVA design was used for testing the hypothesis that the groups would differ on parent-reported outcome measures post treatment. Analyses were conducted on the standard scores derived from parent ratings on the SSRS Social Skills and Problem Behaviors scales. The post treatment scores (T2) were the dependent variables and the baseline scores (T1) were used as covariates to control for initial levels. Demographic, child and caregiver characteristics, group leader, and cohort proved to be unnecessary as covariates since they were unrelated to the outcome variables. Analyses revealed statistically significant condition effects for both Social Skills and Problem Behaviors, respectively, F (1, 93) = 5.03, p < .03, d = .52 and F (1, 93) = 4.05, p < .05, d = .40. Children in the CFT condition showed significantly improved social skills and decreased problem behaviors compared to the children in the DTC condition. See Table 4.
Teacher Report of Social Skills and Problem Behaviors.
Examination of possible covariates to outcome on the teacher rated SSRS Social Skills and Problem Behaviors scales revealed that only child IQ was statistically related to outcome (r = .29, p < .01, Social Skills; r = −.27, p < .01, Problem Behaviors). After controlling for child IQ and baseline levels, teacher ratings revealed no treatment effects post treatment. See Table 4.
CFT Treatment Effects at 3-month Follow Up
Children’s Report of Social Skills Knowledge.
To examine the maintenance of social skill knowledge over a 3-month period following treatment, data from children in the CFT condition were analyzed using two-tailed pairwise t tests. The DTC group received treatment during this time period so could not be used as a comparison group. Change scores across two time periods, post treatment to 3-month follow up (T2-T3) and baseline to 3 month follow up (T1-T3), constituted the dependent variables for the outcome measure (TSSK). Results indicated that children’s knowledge not only significantly improved following treatment but also was maintained over the 3- month follow up period (T2 to T3, t (48) = 1.07, p < .29, d = .16; T1-T3, t (48) = 11.83, p < .0001, d = 1.73). See Table 4.
Parent Report of Social Skills and Problem Behaviors.
To examine the maintenance of social skill gains and the reduction in problem behaviors at follow up, ratings (SSRS Social Skills and Problem Behaviors standard scores) from parents of the children in the CFT condition were analyzed as described above. Results indicated that social skills gains increased over time, and gains in problem behaviors, while not improving significantly from T2 to T3, were maintained over time (Social Skills: T2 to T3, t (48) = 3.35, p < .002, d = .49; T1-T3, t (48) = 7.89, p < .0001, d = 1.15; Problem Behaviors: T2 to T3, t (48) = 1.48, p < .15, d = .22; T1-T3, t (48) = 4.55, p < .0001, d = .66). See Table 4.
Teacher Report of Social Skills and Problem Behaviors.
Teachers saw little change in social skills in the CFT group from T2 to T3; however, there was a trend for an effect of treatment in the right direction at the 3-month follow up (T1-T3, ps < .14, d = .22 for Social Skills and d =.24 for Problem Behaviors). See Table 4.
DTC Treatment Outcomes
Similar to findings reported for the CFT group, following treatment, the children in the DTC group exhibited a statistically significant increase in their social skills knowledge as measured by the TSSK (T2-T3), t (45) = 6.26 p < .0001, d = .92; and, according to parent report, an increase in their social skills, t (45) = 2.86 p < .006, d = .42, and a decrease in problem behaviors, t (45) = 2.63 p < .01, d = .39. ANCOVAs on outcome variables, controlling for pretreatment levels (T1 for CFT and T2 for DTC), revealed that the CFT and the DTC groups were comparable after having received treatment (ps ns). Consistent with findings for the CFT group, teachers did not report a statistically significant improvement in social skills or a significant decrease in problem behaviors in the DTC group following treatment. See Table 4.
Clinical Significance
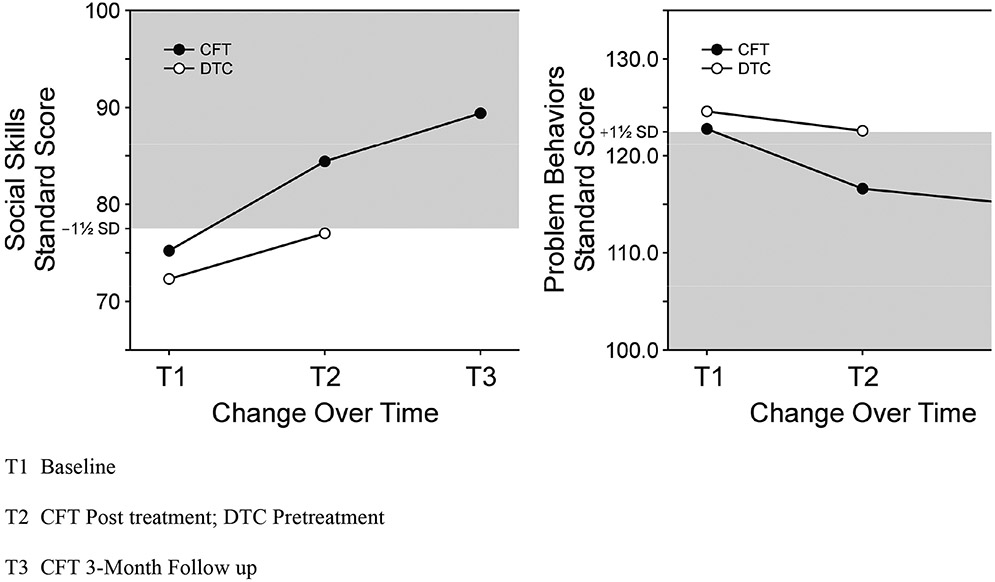
Beyond statistical significance, it is important to address the clinical significance of findings. One approach to clinical significance testing is normative comparisons in which the findings are defined as end-state functioning that falls within a normative range on important outcome variables (Kendall, Marrs-Garcia, Nath, & Sheldrick, 1999). Statistical norms are available for the SSRS Social Skills and Problem Behavior scales and so were used in comparison tests between the mean scores of the CFT group and the standardized normative sample. We conducted one-tailed z tests using 1½ standard deviations around the normative mean as the range of closeness (standard score = 77.5 to 122.5). For post treatment Social Skills (T2), a standard score of 77.5 was chosen as lower limit of the normative range. On this scale, C.E.z = 3.18, p < .001 and tradz = 7.19, p < .001, one tailed. From these results we conclude that, following treatment, the CFT group was clinically equivalent to the normative group; however, there was still a statistically significant difference between the CFT post treatment mean and the normative mean (M = 100). Similar results were found for the Problem Behaviors scale using a standard score of 122.5 as the upper limit of the normative range, C.E.z = 2.70, p < .01, tradz = 7.64, p < .001, one tailed. At 3-month follow up, sample scores continued to fall within the normative ranges but were still significantly different from the normative sample mean. See Figure 1.
Figure 1.
Parent Report of Change in Social Skills and Problem Behaviors following Children ’s Friendship Training (CFT) in Comparison to Delayed Treatment Control (DTC)
Discussion
Children with FASD who participated in social skills training showed clear evidence of improvement in their knowledge of appropriate social behavior post treatment, and this improvement was retained over a 3-month follow up period. Moreover, according to parents, CFT was also effective in increasing social skills and decreasing problem behaviors in sample children. Overall statistically significant differences between the CFT and the DTC groups immediately following treatment were found, and for the CFT group, these gains were maintained over time according to parent reports. Importantly, social skills improved significantly from post treatment to 3-month follow up, suggesting that children were continuing to benefit from the intervention targeting social skills performance. Similar gains were reported for the children in the DTC group following treatment suggesting that waiting 3 months for treatment was not detrimental. Study findings are consistent with those reported by Frankel and associates using CFT for children with and without ADHD (Frankel, 2005; Frankel et al., 1997a; Frankel et al., 1997b). In contrast to previous results using CFT, teachers of children in the present sample reported no improvement for the CFT or the DTC group following treatment.
Failure to find statistically significant generalization of effects to the classroom merits some discussion. Close inspection of the baseline ratings by the teachers revealed that they tended to rate sample children as functioning within the average ranges in social skills and problem behaviors suggesting that teachers did not perceive significant problems in social competence in sample children even at baseline. Frequency counts revealed that teachers rated only 19% of the sample as having social skills scores and only 34 % as having behavior problems scores in the clinical range as defined in this study as between 1½ standard deviations below or above the normative mean, respectively. The reason for this finding may be that teachers focus less on child social skills and focus instead on behaviors related to successful classroom functioning. Since this program was not designed to address those behaviors that are important for classroom success, teachers may not have recognized or even observed changes in the behaviors targeted in this intervention. Indeed, the social skills targeted by CFT, such as trading information to establish common interests or peer group entry, are skills that are more likely to be enacted on the playground or during unstructured time in the classroom, periods when teachers may be less likely to be closely observing student behavior. Moreover, a positive association was found between child IQ and teacher rated social skills, suggesting that teachers rated more intelligent children as making more significant social skills gains regardless of treatment condition.
Alternatively, the parents who participated in the CFT treatment may have overestimated changes in their children simply as a function of being involved in treatment. Although this is a plausible explanation for the difference seen between the parent and teacher outcomes, the fact that children in the treatment condition demonstrated a significant increase in their knowledge of the social rules of behavior that was retained over the follow up period suggests that they did learn socially appropriate behaviors as a function of treatment. In addition, our own observations from week to week of the children in the CFT group and their own and parent reports of successful completion of their social skills homework as well as high attendance (94% of parents attended 8 or more sessions) suggested that children were, in fact, using the strategies that they had learned in treatment and were achieving success in their social interactions and in their ability to deal with conflict situations.
The results of clinical significance testing were mixed. Findings suggested that, although the scores of the children in the CFT group met criteria for clinical equivalency with the normative sample following treatment, their scores were still considerably different compared to the standardized mean of the normative sample, particularly with regard to problem behaviors. These findings are not surprising in light of the fact that children with FASD are characterized as having significant brain pathology that may restrict the degree of improvement they can achieve from this type of psychosocial intervention. Although we attempted to modify the treatment protocol to address primary neurocognitive deficits seen in children with FASD, it is possible that additional refinements of the intervention techniques will further enhance its efficacy with this population. Additionally, it may be useful to examine whether adjunctive therapies such as parent training for problematic behaviors or psychopharmacological interventions might improve treatment outcomes.
Limitations
The conclusions of this study need to be considered in the context of some methodological issues. The lack of concordance between parent and teacher ratings of child social performance represents a limitation of the study and future research would ideally measure social skills at school in more naturalistic settings such as during unstructured classroom time and on the playground.
In addition, some factors restrict our ability to generalize study findings to larger populations of children with FASD. First, it was necessary to work only with children with verbal IQs of 70 or above because the treatment required that the children understand the instructions provided during the didactic portions of the sessions. This necessarily limited the generalizability of the study to some children with prenatal alcohol exposure. In the future, further modifications of the protocol could be made to accommodate children functioning in the moderate to mild range of mental retardation as social skills are extremely important for these children in order to foster more positive social adaptations. Second, the study sample was composed of volunteers who were actively seeking help for their children and who were highly motivated to participate as evidenced by the low rate of study attrition. Although this may represent a potential limitation with regard to generalization to other children with FASD and their families, research shows that the children with FASD who have the best prognoses are those who are identified early, who come from stable supportive homes, and who receive intervention early in life (Streissguth, 1997). Given the requirement of parent involvement for the success of the present treatment, we would expect that it is those highly motivated families who would benefit most from this particular intervention.
Future Directions
This study represents the first controlled treatment for improving the social functioning of children with FASD. As such, it represents a promising intervention for these children who experience multiple failures in social interaction leading to poor peer choices and, for some, juvenile delinquency. However, the treatment was performed in a highly controlled university setting, and thus the next step in determining its effectiveness would be to test the treatment on children enrolling in more typical community based programs. Given the high rates of mental health problems among children with FASD (Streissguth, et al., 1996), these children are likely to be seen for treatment in these community settings. Providing increased access to interventions that have been empirically demonstrated to be efficacious with this population would be a critical step toward reducing some of the devastating secondary disabilities faced by children with FASD and in helping their families facilitate change.
Footnotes
Based upon research reported by Sampson, Streissguth, Bookstein, and Barr, (2000) on the IQ score distribution of a large sample of children with prenatal alcohol exposure, a cut point of ≥ 70 would allow 73% of children with FAS and 91% of children with Partial FAS and ARND to participate in the study. For a minority of children recently adopted from Russia (n = 3/13), verbal IQs lower than 70 were accepted if a 95% confidence interval around this score included 70 and if estimates of their nonverbal IQs on the K-BIT were greater than 70.
Three children in the study were assigned a score of 2 (“unknown risk”) in the prenatal alcohol exposure category of the Diagnostic Guide (Astley, 2004). These children were abandoned at birth with no documentation regarding their prenatal history. However, these children presented with either a diagnosis of FAS from a pediatric geneticist or had features consistent with prenatal alcohol exposure (e.g., facial dysmorphology, central nervous system dysfunction). Additionally, other disorders that might resemble FAS (e.g., certain genetic syndromes) had been ruled out during medical or psychiatric evaluations they had received prior to enrollment in the current study.
Children in the DTC condition were yoked in time with the children in the CFT condition and we decided that it would be unethical to deny treatment to the DTC families for 6 months.
One drink was considered to be .60 ounces of absolute alcohol (i.e. one 12-ounce can of beer containing 5% absolute alcohol was considered 1 drink). All alcohol levels obtained were considered estimates of actual exposure because they were based on maternal self-report.
References
- Astley SJ (2004). Diagnostic Guide for Fetal Alcohol Spectrum Disorders: The 4-Digit Diagnostic Code-Third Edition. Seattle, WA: University of Washington. [Google Scholar]
- Babor TF, De la Fuente R, Saunders J, & Grant M (1989). AUDIT: The alcohol use disorders identification test. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Barr HM, & Streissguth AP (2001). Identifying maternal self-reported alcohol use associated with fetal alcohol spectrum disorders, Alcohol: Clinical and Experimental Research, 25 (2), 283–287. [PubMed] [Google Scholar]
- Bhavnagri N, & Parke RD (1991). Parents as direct facilitators of children's peer Relationships: Effects of age of child and sex of parent. Journal of Personal and Social Relationships, 8, 423–440. [Google Scholar]
- Black B, & Hazen NL (1990). Social status and patterns of communication in acquainted and unacquainted preschool children. Developmental Psychology, 26, 379–387. [Google Scholar]
- Brown RT, Coles CD, Smith IE, Platzman KA, Silverstein J, Erikson S, et al. (1991). Effects of prenatal alcohol exposure at school age. II: Attention and behavior. Neurotoxicology and Teratology, 13, 369–376. [DOI] [PubMed] [Google Scholar]
- Buhrmester D (1990). Intimacy of friendship, interpersonal competence, and adjustment during preadolescence and adolescence. Child Development, 61, 1101–1111. [PubMed] [Google Scholar]
- Carmichael-Olson H, Morse BA, & Huffine C (1998). Development and psychopathology: Fetal alcohol syndrome and related conditions. Seminars in Clinical Neuropsychiatry, 3, 262–284. [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analyses for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Elliot SN, & Gresham FM (1993). Social skills intervention for children. Behavior Modification. (pp. 287–313). New York: Sage Publications, Inc. [DOI] [PubMed] [Google Scholar]
- Frankel F (1994). Test of Social Skills Knowledge. Unpublished manuscript. [Google Scholar]
- Frankel F (2005). Parent-assisted children's friendship training. In Hibbs ED & Jensen PS (Eds.), Psychosocial treatments for child and adolescent disorders: Empirically based approaches. (pp 693–715). Washington, D.C.: American Psychological Association. [Google Scholar]
- Frankel F, & Feinberg D (2002). Social problems associated with ADHD vs ODD in children referred for friendship problems. Child Psychiatry & Human Development, 33(2), 125–146. [DOI] [PubMed] [Google Scholar]
- Frankel F, & Myatt R (1996). Self-esteem, social competence, and psychopathology in boys without friends. Personality and Individual Differences, 20, 401–407. [Google Scholar]
- Frankel F, & Myatt R (2003). Children’s Friendship Training. New York: Brunner-Routledge Publishers. [Google Scholar]
- Frankel F, Myatt R, & Cantwell DP (1995). Training outpatient boys to conform with the social ecology of popular peers: Effects on parent and teacher ratings. Journal of Clinical Child Psychology, 24, 300–310. [Google Scholar]
- Frankel F, Myatt R, Cantwell DP, & Feinberg DT (1997a). Use of child behavior checklist and DSM-III-R diagnosis in predicting outcome of children’s social skills training. Journal of Behavior Therapy and Experimental Psychiatry, 28, 149–161. [DOI] [PubMed] [Google Scholar]
- Frankel F, Myatt R, Cantwell DP, & Feinberg DT (1997b). Parent-assisted children’s social skills training: Effects on children with and without attention-deficit hyperactivity disorder. Journal of the Academy of Child and Adolescent Psychiatry, 36, 1056–1064. [DOI] [PubMed] [Google Scholar]
- Gresham FM, & Elliott S (1990). The Social Skills Rating System. MN: American Guidance Service. [Google Scholar]
- Gresham FM, Sugai G, & Horner RH (2001). Interpreting outcomes of social skills training for students with high-incidence disabilities. Exceptional Children, 67, 331–350. [Google Scholar]
- Jacobson JL, & Jacobson SW (2002). Effects of prenatal alcohol exposure on child development. Alcohol Research and Health, 26, 282–286. [PMC free article] [PubMed] [Google Scholar]
- Kaufman AS, & Kaufman NL (1990). Kaufman Brief Intelligence Test (K-BIT). Circle Pines, Minnesota: American Guidance Service. [Google Scholar]
- Kendall RC, Marrs-Garcia A, Nath SR, & Sheldrick RC (1999). Normative comparisons for the evaluation of clinical significance. Journal of Consulting and clinical Psychology, 67, 285–299. [DOI] [PubMed] [Google Scholar]
- Ladd GW, Profilet SM, & Hart CH (1992). Parents’ management of children’s peer relations: Facilitating and supervising children’s activities in the peer culture. In Parke R & Ladd G (Eds.), Family-peer Relationships: Modes of Linkage (pp. 215–253). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Mattson SN, & Riley EP (1998). A review of the neurobehavioral deficits in children with fetal alcohol syndrome or prenatal exposure to alcohol. Alcoholism: Clinical and Experimental Research, 22, 279–294. [DOI] [PubMed] [Google Scholar]
- May PA, & Gossage JP (2001). Estimating the prevalence of fetal alcohol syndrome: A summary. Alcohol Research and Health, 25, 159–167. [PMC free article] [PubMed] [Google Scholar]
- Moncher FJ, & Prinz RJ (1991). Treatment fidelity in outcome studies. Clinical Psychology Review, 11, 247–266. [Google Scholar]
- Nelson J, & Aboud FE (1985). The resolution of social conflict between friends. Child Development, 56, 1009–1017. [Google Scholar]
- O’Connor MJ, Kogan N, & Findlay R (2002). Prenatal alcohol exposure and attachment behavior in children. Alcoholism: Clinical and Experimental Research, 26(10), 1592–1602. [DOI] [PubMed] [Google Scholar]
- O'Connor MJ, Sigman M, & Kasari C (1993). Interactional model for the association among maternal alcohol consumption, mother-infant characteristics and infant cognitive development. Infant Behavior and Development, 16, 177–192. [Google Scholar]
- Paetsch JJ, & Bertrand LD (1997). The relationship between peer, social, and school factors, and delinquency among youth. Journal of School Health, 67(1), 27–33. [DOI] [PubMed] [Google Scholar]
- Parke RD, Neville B, Burks VM, Boyum LA, & Carson JL (1994). Family-Peer Relationship: A Tripartite Model. In Parke RD & Kellam SG (Eds.), Exploring Family Relationships with Other Social Contexts (pp. 115–145). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Patterson GR, Forgatch MS, Yoerger KL, & Stoolmiller M (1998). Variables that initiate and maintain and early-onset trajectory for juvenile offending. Development and Psychopathology, 10, 531–547. [DOI] [PubMed] [Google Scholar]
- Pfiffner LJ, & McBurnett K (1997). Social skills training with parent generalization: Treatment effects for children with attention deficit disorder. Journal of Consulting and Clinical Psychology, 65(5), 749–757. [DOI] [PubMed] [Google Scholar]
- Rasmussen C (2005). Executive functioning and working memory in fetal alcohol spectrum disorder. Alcoholism: Clinical and Experimental Research, 29(8), 1359–1367. [DOI] [PubMed] [Google Scholar]
- Roebuck TM, Mattson SN, & Riley EP (1999). Behavioral and psychosocial profiles of alcohol exposed children. Alcoholism: Clinical and Experimental Research, 23, 1070–1076. [PubMed] [Google Scholar]
- Rose AJ, & Asher SR (1999). Children’s goals and strategies in response to conflicts within a friendship. Developmental Psychology, 35, 69–79. [DOI] [PubMed] [Google Scholar]
- Rubin DB (1987). Multiple Imputation for Nonresponse in Surveys, NY: John Wiley & Sons, Inc. [Google Scholar]
- Sampson PD, Streissguth AP, Bookstein F, & Barr HM (2000). On categorizations in analyses of alcohol teratogenesis. Environmental Health Perspectives, 108, 421–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De la Fuente R, & Grant M (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT). Addiction, 88, 791–804. [DOI] [PubMed] [Google Scholar]
- Schonfeld AM, Mattson SN, & Riley EP (2005). Moral maturity and delinquency after prenatal alcohol exposure. Journal of Studies on Alcohol, 66, 545–554. [DOI] [PubMed] [Google Scholar]
- Sood B, Delancey-Black V, Covington C et al. , (2001). Prenatal alcohol exposure and childhood behavior at age 6 to 7 years: I. Dose-response effect. Pediatrics, 108(2), 1–9. [DOI] [PubMed] [Google Scholar]
- Sparrow S, Balla D, & Cicchetti DV (1984). The Vineland Adaptive Behavior Scales. Circle Pines, Minnesota: American Guidance Service. [Google Scholar]
- Stratton K, Howe C, & Battaglia F (Eds.). (1996). Fetal Alcohol Syndrome: Diagnosis, Epidemiology, Prevention, and Treatment. Washington, D.C.: Institute of Medicine, National Academy Press. [Google Scholar]
- Streissguth AP (1997). Fetal Alcohol Syndrome. Baltimore, MD: Paul Brooks. [Google Scholar]
- Streissguth AP, Barr HM, Kogan J, & Bookstein FL (1996). Understanding the Occurrence of Secondary Disabilities in Clients with Fetal Alcohol Syndrome (FAS) and Fetal Alcohol Effects (FAE): Final Report to the Center for Disease Control. Seattle: University of Washington, Fetal Alcohol and Drug Unit. [Google Scholar]
- Streissguth AP, & O’Malley K (2000). Neuropsychiatric implications and long-term consequences of fetal alcohol spectrum disorders. Seminars in Clinical Neuropsychiatry, 5(3), 177–190. [DOI] [PubMed] [Google Scholar]
- Thomas SE, Kelly SJ, Mattson SN, & Riley EP (1998). Comparison of social abilities of children with fetal alcohol syndrome to those of children with similar IQ scores and normal controls. Alcoholism: Clinical and Experimental Research, 22, 528–533. [PubMed] [Google Scholar]
- Whaley SE, O’Connor MJ, & Gunderson B (2001). Comparison of the adaptive functioning of children prenatally exposed to alcohol to a nonexposed clinical sample. Alcoholism: Clinical and Experimental Research, 25(7), 118–124. [PubMed] [Google Scholar]