Summary
Introduction
The Karnataka State Reserve Police (KSRP) is a state-level police force in India. Good Oral Health-Related Quality of Life (OHRQoL) among them is quintessential for the welfare of the society. The aim of the study was to assess the impact of dental caries and periodontal disease on the OHRQoL among the Karnataka State Reserve Police (KSRP) stationed in Belagavi, India.
Methods
A cross-sectional design was used with a total sample size of 720. The personnel were recruited by simple random sampling. The Oral Health Impact Profile 14 (OHIP 14) was used to assess OHRQoL in 7 domains. The intra-examiner reliability for World Health Organisation (WHO) oral assessment form 2013 was assessed using Kappa statistics and was found to be 0.86. Dentition and periodontal status were recorded using the same. Statistical analysis was performed using descriptive statistics, Analysis of variance (ANOVA), Pearson’s coefficient of correlation and multiple linear regression analysis.
Results
Physical pain and psychological discomfort had the highest mean scores among the seven domains of OHIP-14. Constables had higher mean OHIP-14 scores among the study population. A significant positive correlation was found between oral health parameters with the domains of OHIP-14. The highest dependence on the socio-demographic and oral health predictors were found in the domains of physical pain (44.2%), psychological discomfort (38.3%), and physical disability (30.5%).
Conclusions
The study revealed that dental caries and periodontal disease had a significant impact on OHRQoL among reserve police personnel and the OHRQoL was poor particularly among the lower ranked personnel.
Keywords: Dental caries, Oral health, Police, Periodontal diseases, Quality of Life
Introduction
Oral health is closely linked to overall health [1]. According to World Health Organisation (WHO), nearly 3.5 billion people worldwide are affected by oral diseases, with a high prevalence in middle-income countries like India [2]. Nearly 29% of world population have dental caries in their permanent teeth, with a total of over 2 billion reported cases worldwide. Similarly, periodontal disease is also particularly common, with over 1 billion cases worldwide and a peak prevalence of 19% in adults over the age of 55 years [2]. These oral diseases can significantly impact the Quality of Life (QoL) of an individual.
Certain occupations may elevate the likelihood of oral health diseases due to the nature of the work [3]. Physical demands of certain jobs may hinder oral hygiene practices leading to poor oral health. One such strenuous occupation is policing. A police personnel’s job is typically classified as a blue-collar job and involves maintaining law and order, protecting the public, and enforcing laws. Studies conducted among police personnel of Indian states have reported increased psychological distress among them [4, 5]. Long work hours, exposure to traumatic events, and public scrutiny can contribute to post-traumatic stress and lower QoL further [6]. Due to the high stress levels associated with their job, they may tend to engage in habits such as using tobacco in various forms [7]. These habits may increase the risk of periodontal disease and oral cancer.
The concept of QoL was introduced by economist A.C. Pigou in 1920 [8]. David Locker’s model considers health and QoL as multifaceted, subjective, and influenced by various factors. He emphasizes the link between overall health and oral health [9]. Oral Health-Related Quality of Life (OHRQoL) measures the impact of oral health on an individual’s overall well-being and daily life [10]. Poor oral health may lower OHRQoL due to pain, difficulty in eating and speaking, and self-consciousness about appearance. Previous systematic reviews have shown that dental pain and periodontitis can negatively impact OHRQoL [11, 12]. The Oral Health Impact Profile (OHIP) by G D Slade, is a validated and widely used instrument for measuring OHRQoL and is based on Locker’s model. It assesses how oral health problems affect various aspects of daily life [13].
Karnataka State Reserve Police (KSRP) is a state-level police force with fourteen battalions that supplement the regular police force as and when needed. The second battalion is located in Belagavi district consisting of male and female personnel. They have the same training and responsibilities as regular personnel [14]. Although there have been previous studies conducted on the oral health and OHRQoL of police personnel in India, this study contributes significantly to the existing knowledge by focusing exclusively on reserve police personnel. It provides unique insights into the oral health and OHRQoL of this population, which has not been previously explored in the literature [15, 16]. This study was done to address the hypothesis that dental caries and periodontal disease have a significant impact on the OHRQoL among KSRP personnel stationed in Belagavi, India. The objectives of study this were to evaluate the OHRQoL of KSRP personnel using the OHIP-14 questionnaire. To determine if there are any significant differences in OHRQoL among the police force based on their rank. To investigate the association between oral health parameters and their OHRQoL.
Material and methods
This cross-sectional study followed STROBE recommendations and was conducted from September to December 2022 among KSRP unit in Belagavi district. Eligible participants were police personnel deployed at KSRP Belagavi unit during the study period, and those who refused informed consent were excluded.
The Institutional Research and Ethics Committee issued the ethical clearance (Ref no: 1538) and the study adhered to all the ethical requirements. Prior to the start of the study, an official permission was acquired from the office of the superintendent of police at KSRP, Belagavi unit. All participants read and signed a written informed consent document before commencing the study.
A single examiner was standardised and calibrated to ensure consistent assessment by a panel of experts prior to the start of the study. The intra-examiner reliability was assessed using Kappa statistics for WHO Oral Health Assessment Form (2013) and the Kappa coefficient value was found to be 0.86 [17]. A pilot study was carried out to estimate the prevalence of dental caries and periodontal disease among 40 police personnel. It also assessed questionnaire comprehension and response time. From the pilot study, the prevalence of dental caries and periodontal disease was estimated to be 72.1% and 83.6% respectively. Based on these findings, the minimum sample size was estimated to be 688 with type I (α) error = 0.05 and Power (1-β) = 0.95 using G*Power statistical software (Ver. 3.1.9.4). During the period of study, the list of police personnel who were deployed at the KSRP unit in Belagavi was obtained and it was used as the sampling frame. A final sample size of 720 was set and the participants were recruited by simple random sampling using the random number table method.
The study involved conducting an oral examination followed by completion of a physical copy of questionnaire. The questionnaire utilized for the survey was the OHIP-14, which was made available in both English and the local language, Kannada. To ensure linguistic validity, it was translated into Kannada by back-translation method and was verified using a language expert. An expert committee performed a cross-cultural adaptation on the translated version, which aimed to establish equivalence between the source and target versions in four areas: semantic, idiomatic, experiential, and conceptual [18]. The higher ranked personnel received the questionnaire in English while the lower ranked personnel received the questionnaire in the regional language. This approach ensured that the questionnaire was suitable for all ranks and that the results obtained were reliable. Although the OHIP-14 is a brief questionnaire, it has demonstrated strong reliability and sensitivity, with satisfactory cross-cultural consistency over other instruments such as Oral Impacts on Daily Performance (OIDP) to assess the OHRQoL [19, 20].
Demographic details like age, sex, designation, and education were recorded in the first part of the questionnaire. The second part consisted of OHIP-14 questionnaire to assess OHRQoL in seven domains [21]. Each of the seven domains had two questions, which were close ended. Responses were recorded on a 5-point Likert scale, with higher scores indicating lower OHRQoL. The total OHIP-14 score ranged from 0 to 56, with individual domain score ranging from 0 to 8 [10]. DMFT (Decayed, Missing Filled Teeth) and periodontal status (gingival bleeding, pockets, and loss of attachment) were recorded using the WHO Oral Health Assessment Form (2013). On pre-determined dates, the oral examination was carried out at the KSRP health centre, Belagavi in a designated space provided by the officials, in adherence to standardized procedures and protocols. Data was collected in batches and a type III examination carried out under natural light.
STATISTICAL ANALYSIS
IBM SPSS Statistics (Version 21.0) was used for statistical analysis. Descriptive statistics were computed using Microsoft Excel 2019, including percentages, means, and standard deviations. The Kolmogorov-Smirnov test determined data distribution normality. Analysis of Variance (ANOVA) was used to check for significant differences, while Karl Pearson coefficient of correlation and multiple linear regression were performed for study variables. Level of significance and confidence levels were set at 5% and 95%, respectively.
Results
Among the 720 study participants, majority of the participants were constables (35.6%) and head constables (24.4%), while 10.6% were inspectors. The mean age of the study participants was 39.48 ± 10.65 (Tab. I). Table II depicts the frequency distribution of responses to all OHIP-14 questions and their mean values. Among the seven domains of OHIP-14, physical pain and psychological discomfort had the highest mean scores of 3.10 ± 1.64 and 3.01 ± 1.82 respectively. The OHIP-14 scores were highest for constables (22.43 ± 4.84) and lowest for inspectors (7.71 ± 3.01) (Tab. III). The mean OHIP-14 score among the study population was 18.74 ± 7.69 and there was a statistically significant difference among the five ranks of police personnel when ANOVA test was applied (P ≤ 0.001). The prevalence of dental caries among the study participants was 84.2%. Figure 1 illustrates the distribution of mean DMFT scores among the participants. It was observed that constables and head constables had higher mean DMFT scores of 5.62 ± 2.97 and 5.39 ± 2.96 respectively, while inspectors had a lower score of 3.66 ± 2.70. Figure 2 illustrates the prevalence of various periodontal conditions among the population. The prevalence of gingival bleeding, periodontal pockets, and loss of attachment (LoA) were 71%, 63% and 69% respectively. Figure 3 illustrates the kernel density estimate of the OHIP-14 scores among the participants.
Tab. I.
Distribution of study population by gender, age and educational level.
| Sociodemographic characteristics | Constables n (%) | Head Constables n (%) | Assistant Sub Inspectors n (%) | Sub Inspectors n (%) | Inspectors n (%) | Total n (%) |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Male | 118 (46.1%) | 137 (77.8%) | 96 (82.8%) | 77 (80.2%) | 76 (100%) | 504 (70.0%) |
| Female | 138 (53.9%) | 39 (22.2%) | 20 (17.2%) | 19 (19.8%) | 0 (0.0%) | 216 (30.0%) |
| Age Groups | ||||||
| 21-30 | 116 (45.3%) | 39 (22.2%) | 20 (17.2%) | 0 (0%) | 0 (0.0%) | 175 (24.3%) |
| 31-40 | 60 (23.4%) | 59 (33.5%) | 19 (16.4%) | 76 (79.2%) | 38 (50.0%) | 252 (35.0%) |
| 41-50 | 20 (7.8%) | 58 (33.0%) | 20 (17.2%) | 20 (20.8%) | 19 (25.0%) | 137 (19.0%) |
| 51-60 | 60 (23.4%) | 20 (11.4%) | 57 (49.1%) | 0 (0.0%) | 19 (25.0%) | 156 (21.7%) |
| Educational Level | ||||||
| Graduate | 0 (0.0%) | 0 (0.0%) | 20 (17.2%) | 57 (59.4%) | 57 (75.0%) | 174 (24.2%) |
| Diploma / Intermediate | 40 (15.6%) | 39 (22.2%) | 57 (49.1%) | 20 (20.8%) | 19 (25.0%) | 135 (18.8%) |
| High School | 216 (84.4%) | 137 (77.8%) | 39 (33.6%) | 19 (19.8%) | 0 (0.0%) | 411 (57.1%) |
| Total | 256 (100%) | 176 (100%) | 116 (100%) | 96 (100%) | 76 (100%) | 720 (100%) |
| All values are expressed as frequency with percentages (in parentheses). | ||||||
Tab. II.
Distribution of responses to individual OHIP-14 questions and their mean scores.
| OHIP-14 Questions | 5 Point Likert Scale | |||||
|---|---|---|---|---|---|---|
| Never (0) | Rarely (1) | Occasionally (2) | Frequently (3) | Very often (4) | Mean ± SD | |
| Have you had trouble pronouncing any words because of problems with your teeth or mouth? | 134 (18.6%) | 291 (40.4) | 217 (30.1%) | 59 (8.2%) | 19 (2.6%) | 1.36 ± 0.96 |
| Have you felt that your sense of taste has worsened because of problems with your teeth or mouth? | 95 (13.2%) | 292 (40.6%) | 274 (38.1%) | 54 (7.5%) | 5 (0.7%) | 1.42 ± 0.84 |
| Have you had painful aching in your mouth? | 190 (26.4%) | 139 (19.3%) | 312 (43.3%) | 76 (10.6%) | 3 (0.4%) | 1.39 ± 1.00 |
| Have you found it uncomfortable to eat any foods because of problems with your teeth or mouth? | 76 (10.6%) | 156 (21.7%) | 409 (56.8%) | 59 (8.2%) | 20 (2.8%) | 1.71 ± 0.87 |
| Have you been self-conscious because of your teeth or mouth? | 58 (8.1%) | 330 (45.8%) | 214 (29.7%) | 78 (10.8%) | 40 (5.6%) | 1.60 ± 0.98 |
| Have you felt tense because of problems with your teeth or mouth? | 211 (29.3) | 216 (30%) | 139 (19.3%) | 97 (13.5%) | 57 (7.9%) | 1.41 ± 1.25 |
| Has been your diet been unsatisfactory because of problems with your teeth of mouth? | 254 (35.3%) | 213 (29.6%) | 155 (21.5%) | 78 (10.8%) | 20 (2.8%) | 1.17 ± 1.11 |
| Have you had to interrupt meals because of problems with your teeth or mouth? | 175 (24.3%) | 175 (24.3%) | 156 (21.7%) | 211 (29.3%) | 3 (0.4%) | 1.57 ± 1.16 |
| Have you found it difficult to relax because of problems with your teeth or mouth? | 114 (15.8%) | 312 (43.3%) | 140 (19.4%) | 135 (18.8%) | 19 (2.6%) | 1.50 ± 1.06 |
| Have you been a bit embarrassed because of problems with your teeth or mouth? | 152 (21.1%) | 333 (46.3%) | 196 (27.2%) | 37 (5.1%) | 2 (0.3%) | 1.17 ± 0.83 |
| Have you been a bit embarrassed because of problems with your teeth or mouth? | 135 (18.8%) | 368 (51.1%) | 217 (30.1%) | 4 (0.6%) | 1 (0.1%) | 1.12 ± 0.71 |
| Have you had difficulty doing your usual jobs because of problems with your teeth or mouth? | 133 (18.5%) | 350 (48.6%) | 178 (24.7%) | 39 (5.4%) | 20 (2.8%) | 1.25 ± 0.91 |
| Have you felt that life in general was less satisfying because of problems with your teeth or mouth? | 179 (24.9%) | 351 (48.8%) | 133 (18.5%) | 55 (7.6%) | 2 (0.3%) | 1.10 ± 0.87 |
| Have you been totally unable to function because of problems with your teeth or mouth? | 235 (32.6%) | 328 (45.6%) | 99 (13.8%) | 57 (7.9%) | 1 (0.1%) | 0.97 ± 0.89 |
| All values are expressed as frequency with percentages (in parentheses); SD: Standard deviation. | ||||||
Tab. III.
Mean scores of the seven domains of OHIP-14 among the study subjects.
| Domains of OHIP | Constables | Head Constables | Assistant Sub Inspectors | Sub Inspectors | Inspectors | Total |
|---|---|---|---|---|---|---|
| Functional limitation | 3.32 ± 1.54 | 3.22 ± 1.39 | 3.02 ± 1.16 | 1.63 ± 1.52 | 1.00 ± 1.01 | 2.78 ± 1.61 |
| Physical pain | 3.55 ± 1.70 | 3.32 ± 0.82 | 3.70 ± 1.81 | 2.04 ± 1.72 | 1.50 ± 0.50 | 3.10 ± 1.64 |
| Psychological discomfort | 3.90 ± 1.64 | 3.87 ± 1.52 | 2.53 ± 1.51 | 1.41 ± 0.49 | 0.75 ± 0.44 | 3.01 ± 1.82 |
| Physical disability | 3.38 ± 1.80 | 2.99 ± 2.18 | 3.34 ± 2.17 | 1.61 ± 1.36 | 0.50 ± 0.87 | 2.74 ± 2.08 |
| Psychological disability | 3.25 ± 1.29 | 3.55 ± 1.27 | 2.34 ± 2.13 | 1.43 ± 1.38 | 0.75 ± 0.44 | 2.67 ± 1.70 |
| Social disability | 2.80 ± 1.53 | 3.01 ± 1.28 | 1.86 ± 1.24 | 1.60 ± 0.49 | 1.25 ± 0.83 | 2.38 ± 1.41 |
| Handicap | 2.23 ± 1.26 | 2.27 ± 1.57 | 2.04 ± 2.01 | 1.40 ± 1.12 | 1.96 ± 1.15 | 2.07 ± 1.48 |
| Total OHIP-14 Score | 22.43 ± 4.84 | 22.23 ± 5.18 | 18.82 ± 8.41 | 11.11 ± 5.18 | 7.71 ± 3.01 | 18.74 ± 7.69 |
| All values are expressed in Mean ± Standard Deviation (SD). | ||||||
Fig. 1.
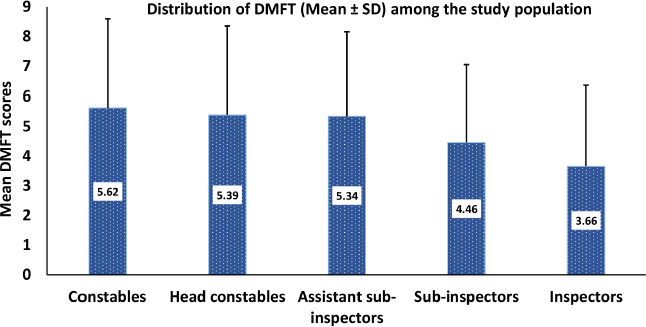
Distribution of DMFT (Decayed, Missing and Filled Teeth) among the study population in Mean and SD (Standard deviation).
Fig. 2.
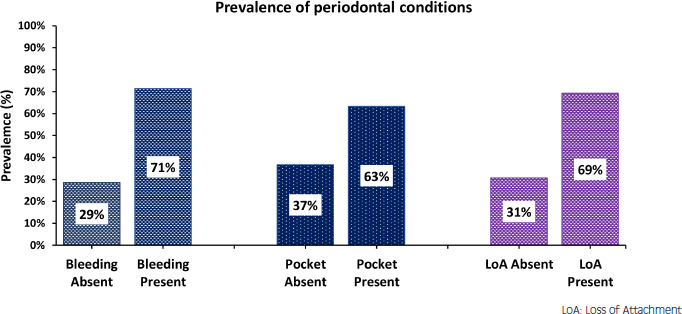
Prevalence of periodontal conditions among the study participants;.
Fig. 3.
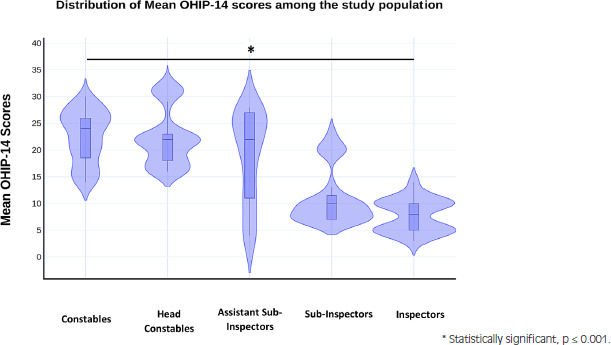
Violin plot showing the distribution of OHIP-14 scores among the study population. Statistical test used: Analysis of Variance (ANOVA).
RELATIONSHIP BETWEEN THE DOMAINS OF OHIP-14 AND VARIOUS ORAL HEALTH PARAMETERS USING PEARSON’S COEFFICIENT OF CORRELATION
Table IV depicts the field-wise correlation data of the study variables using Pearson’s coefficient of correlation. DMFT showed maximum positive correlations that were statistically significant at p ≤ 0.001 with four domains of OHIP-14, followed by the decayed component (DT) which were significantly correlated with two. There was a negative correlation seen between filled teeth and domain physical pain at P ≤ 0.05. High loss of attachment (LoA) scores were positively correlated with the domain physical pain at P ≤ 0.001. Other periodontal components also had significant positive correlations with some of the domains of OHIP-14. The missing component did not show any statistically significant correlations.
Tab. IV.
Correlation between clinical variables and domains of OHIP-14.
| Domains of OHIP | DT | MT | FT | DMFT | Bleeding | Deep Pockets (> 6 mm) | High LoA |
|---|---|---|---|---|---|---|---|
| Functional limitation | 0.093* | 0.050 | -0.022 | 0.102** | 0.044 | 0.032 | 0.009 |
| Physical pain | 0.093* | 0.061 | -0.083* | 0.109** | 0.082* | 0.075* | 0.139** |
| Psychological discomfort | 0.098** | 0.060 | -0.006 | 0.118** | 0.061 | 0.055 | 0.078* |
| Physical disability | 0.080* | 0.008 | -0.020 | 0.074* | 0.054 | 0.058 | 0.083* |
| Psychological disability | 0.123** | 0.073 | -0.033 | 0.136** | 0.047 | 0.035 | 0.006 |
| Social disability | 0.042 | 0.050 | 0.017 | 0.068 | 0.008 | 0.010 | 0.001 |
| Handicap | 0.072 | 0.015 | -0.052 | 0.055 | 0.025 | 0.062 | 0.047 |
| The statistical test used: Pearson’s coefficient of correlation. * Significant at 0.05 level. ** Significant at 0.001 level. DT: Decayed teeth; MT: Missing teeth; FT: Filled teeth; LoA: Loss of attachment. | |||||||
RELATIONSHIP BETWEEN THE DOMAINS OF OHIP-14 AND VARIOUS STUDY VARIABLES USING MULTIPLE LINEAR REGRESSION ANALYSIS
Table V summarizes all the multiple regression analysis models performed using the seven domains of OHIP-14 as the dependent variable and the predictors: age, education, designation of police personnel and prevalence of caries and periodontal disease. The highest dependence on these predictors were found in the domains of physical pain (44.2%), psychological discomfort (38.3%), and physical disability (30.5%), while the lowest dependence were seen with handicap (17.0%) and social disability (10.8%). Table VI presents the regression equation of all the multiple regression analysis models performed in the study.
Tab. V.
Association between domains of OHIP-14 as dependent variable and various study variables as predictors.
| Dependent Variable | Coefficient (r) | Coefficient of determination (R2) | F | p | Standard error of estimate |
|---|---|---|---|---|---|
| Functional limitation | 0.484 | 0.235 | 43.798 | < 0.001* | 1.403 |
| Physical pain | 0.665 | 0.442 | 112.951 | < 0.001* | 1.365 |
| Psychological discomfort | 0.619 | 0.383 | 88.513 | < 0.001* | 1.628 |
| Physical disability | 0.553 | 0.305 | 62.797 | < 0.001* | 1.412 |
| Psychological disability | 0.483 | 0.234 | 43.514 | < 0.001* | 1.230 |
| Social disability | 0.329 | 0.108 | 17.349 | < 0.001* | 1.398 |
| Handicap | 0.412 | 0.170 | 29.236 | < 0.001* | 1.493 |
| The statistical analysis used: Multivariate linear regression; Level of significance: * P ≤ 0.05 is considered statistically significant: Dependent Variable: Domains of OHIP-14; Predictors: (Constant), Age, Education, Designation, Caries Prevalence, Periodontal disease prevalence. | |||||
Tab. VI.
Regression equation of all the models with domains of OHIP-14 as dependent variable and various study variables as predictors.
| Domains of OHIP | Regression equation |
|---|---|
| Functional limitation (Y1) | Y1 = 0.788 + (0.057) X1 + (0.258) X2 + (0.650) X3 + (0.025) X4 + (0.124) X5 |
| Physical pain (Y2) | Y2 = 1.435 + (0.316) X1 + (0.421) X2 + (0.944) X3 + (0.052) X4 + (0.234) X5 |
| Psychological discomfort (Y3) | Y3 = 0.995 + (0.542) X1 + (1.080) X2 + (0.129) X3 + (0.030) X4 + (0.029) X5 |
| Physical disability (Y4) | Y4 = 1.284 + (0.308) X1 + (0.109) X2 + (0.633) X3 + (0.087) X4 + (0.005) X5 |
| Psychological disability (Y5) | Y5 = 1.182 + (0.049) X1 + (0.499) X2 + (0.620) X3 + (0.043) X4 + (0.070) X5 |
| Social disability (Y6) | Y6 = 1.870 + (0.296) X1 + (0.246) X2 + (0.098) X3 + (0.011) X4 + (0.026) X5 |
| Handicap (Y7) | Y7 = 2.097 + (0.218) X1 + (0.098) X2 + (0.465) X3 + (0.020) X4 + (0.085) X5 |
| Predictors: X1 = Age; X2 = Education; X3 = Designation; X4 = Caries Prevalence; X5 = Periodontal disease prevalence. | |
Discussion
Oral health is an important factor in the overall QoL. India ranks 54th in the QoL Index 2023 [22]. In a recent study conducted on QoL, nearly one out of two (46.2%) Indian adults has poor QoL [23]. Good QoL among police personnel is quintessential for the welfare of the society. The purpose of this study was to investigate if there is any impact of oral health parameters on the seven domains of QoL among the reserve police force of Belagavi district.
Blue collared jobs such as policing take a toll on an individual’s health. They are prone to systemic as well as oral diseases [3, 24]. The demanding physical work and long hours can lead to poor oral hygiene habits, which can increase the risk of dental caries and periodontal disease. Previous studies conducted among police personnel in India and other parts of Southwest Asia reported that the oral health among this population were not up to the required standards [25, 26]. In this study, the prevalence of dental caries was found to be high (84.2%) and comparatively, the lower ranked personnel had higher DMFT scores. These findings were comparable to Maurya et al. [25] and Basavaraj et al. [27], however it was contradicting Singh et al. [28]. Dental caries is a multifactorial disease. It may be associated with factors such as poor oral hygiene, increased amounts of sugars in diet, lack of awareness and low socioeconomic status among this population. A previous study conducted by Mythri et al. [29] at KSRP unit in Tumkur district revealed that the there was a significant disparity between oral health awareness and practices among the personnel. Lower-ranked police personnel may consume refreshments high in fermentable sugars during duty hours when exposed to prolonged sunlight. Dehydration under the sun can cause decreased salivary flow. This combination can increase the risk of developing dental caries. Additionally, due to their low socioeconomic status, these personnel have limited access to good oral healthcare services to maintain their oral health [30, 31].
The prevalence of periodontal diseases were also high among them, analogous to findings reported by Rajagopalachari et al. [16] and Majeed et al. [26]. Inadequate oral hygiene practices can contribute to the build-up of bacterial plaque and calculus, which in turn can result in gingival bleeding. Due to stress and irregular work hours, there is also increased use of tobacco among them. A higher prevalence of deleterious habits such as tobacco chewing was reported among police personnel, by Dilip C.L in Karnataka [32]. These habits can affect the periodontium leading to conditions such as gingival recession, pocket formation, and bone loss. Periodontal disease, if left untreated, can lead to tooth and bone loss, and increased risk of systemic conditions [15].
The OHRQoL was assessed in seven dimensions using OHIP-14 questionnaire [19, 33]. In this study the police personnel had a lower OHRQoL, especially in the domains physical pain and psychological discomfort, as evidenced by the higher mean scores observed in these two domains. The OHRQoL worsens with the pain and discomfort caused by decayed teeth. Dental caries when progressed deeper towards to the pulp can cause major pain affecting the OHRQoL of an individual [11]. The decayed component and DMFT showed significant positive correlations with the domains of OHIP-14, similar to findings reported by Rajagopalachari et al. [16]. These findings indicate that, as the number of decayed teeth increases the OHRQoL declines among these personnel. Educational qualifications of an individual play a key role in maintaining a good oral health [34]. In this study, it was observed that personnel with higher education had lower DMFT scores and better OHRQoL, especially the inspectors. This study also reported that, the filled component showed negative correlations with OHIP-14 domains, indicating that treating the decayed teeth has improved the OHRQoL among these personnel, by reducing their pain and associated symptoms. However, these findings were at contradiction to that of Rajagopalachari et al. [16], where no such negative correlation was reported. The pain caused by periodontal disease is milder compared to dental caries [28]. But increase in prevalence of periodontal disease among these police personnel may still affect the OHRQoL [12]. Halitosis caused by periodontal disease can also negatively impact the OHRQoL as evidenced in the systematic review by Cassiano et al. [35]. In this study, it was found that periodontal diseases showed significant correlations with physical pain and disability, and psychological discomfort.
In this study, it was seen that five domains of OHIP-14 showed significant relationship with oral health variables. Physical pain, and psychological discomfort showed the most significant correlations, followed by physical and psychological disability, and functional limitation. The mean scores for social disability and handicap were low and had no similar significant relationships with any of the oral health parameters. These findings were synonymous with studies by Rajagopalachari et al. [16] and Fotedar et al. [36]. It shows that the existence of oral disorders did not cause any significant handicap or social disadvantage among this population, however it significantly affected the physical, psychological, and functional dimensions of OHRQoL. When total OHIP-14 scores were considered, it was observed that the inspectors and other higher ranked personnel had better OHRQoL than lower ranked constables. Multiple linear regression analysis performed in this study revealed that factors such as age, education, designation, and prevalence of oral disease had a major influence on OHRQoL. These findings highlight that socioeconomic status and education play key roles in the OHRQoL of these police personnel [34]. The personnel with higher ranks had good education and better socioeconomic status due to which they could cater to their oral health needs on time, thereby having a better OHRQoL.
Some of the ways to tackle this oral health challenge are health education programs targeting police personnel on proper brushing techniques and other oral hygiene practices. This should be complemented by diet counselling and emphasizing the importance of avoiding fermentable sugars between meals. Routine dental check-ups are required among this population, followed by preventive dental treatments such as pit and fissure sealant application and fluoride varnish, to reduce the incidence of initial enamel caries. Individual-level restorative dental treatments, particularly among lower-ranked personnel, may be beneficial in improving OHRQoL, as restoring teeth had a significant positive impact on OHRQoL. These personnel should be made aware of the different treatment modalities, such as removable and fixed prosthesis and dental implants that are available to them, to prevent disability caused by tooth loss. Additionally, tobacco counselling and education on the ill effects of tobacco are necessary interventions. Health insurance schemes, such as the one implemented in the state of Odisha, which covers systemic as well as oral diseases, should be considered to improve the QoL and working efficiency of police personnel in Karnataka [37]. Occupational health and safety standards set by the International Labor Organization can help to ensure their well-being while on the job, covering areas such as physical and psychological health, risk assessment, and emergency preparedness [38]. This study highlights a significant public health problem present in this population, and addressing it requires a comprehensive approach involving collaboration between individuals, organizations, and government agencies. This approach can address the underlying social determinants of oral health and target this vulnerable population of police personnel.
Cross-sectional studies such as this, involves studying a population at a specific point in time. The limitation of this study being the inability to establish cause and effect relationships, as seen in other cross-sectional studies. Perhaps, a longitudinal study would be beneficial in establishing that relationship among the various study variables.
Conclusion
The results of this study reveal that dental caries and periodontal disease had a significant impact on the OHRQoL of reserve police personnel in Belagavi and the OHRQoL among them was poor particularly among the lower ranked personnel. Poor oral health among them had a negative influence on their daily life experiences, including physical, emotional, and social well-being. These findings highlight the need for interventions such as regular dental check-ups, oral hygiene education and providing access to preventative and restorative dental treatments specifically targeting the lower ranked police personnel.
Acknowledgments
The authors extend their gratitude to David Coutinho, Ram Surath Kumar K, Atrey J. Pai Khot and Rhea Vas for their significant contributions to the quality of the manuscript. The authors also thank G M Sampada and Erika Mendonca for their assistance in carrying out the study.
Conflict of interest statement
There were no conflict of interests associated with this original research.
Authors’ contributions
NSV, AA: conceptualization; ASV, PC: data curation; NSV, ASV: formal analysis; NSV,ASV, PC: investigation; NSV, MAS, SJ, AA: methodology; NSV, SJ, AA: project administration; NSV, SJ, AVA: resources; MAS, SJ, AVA: software; AA, SJ, RS: supervision; AVA, SJ, RS: validation; NSV, ASV, PC,RS: writing-original draft; NSV, ASV, PC,RS, SJ, AA, MAS: writing-review & editing.
Figures and tables
References
- [1].Swaminathan K, Ananthan V, Haridoss S, Thomas E. Correlation Between Body Mass Index and Dental Caries Among Three- to 12-Year-Old Schoolchildren in India: A Cross-Sectional Study. Cureus 2019;11:e5421. https://doi.org/10.7759/cureus.5421 10.7759/cureus.5421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Global oral health status report: towards universal health coverage for oral health by 2030. Available at: https://www.who.int/publications-detail-redirect/9789240061484 (Accessed on: 4/1/2023).
- [3].Varkey NS, Vas R, Uppala H, Vas NV, Jalihal S, Ankola AV, Ram SKK. Dental caries, oral hygiene status and treatment needs of fishermen and non-fishermen population in South Goa, India. Int Marit Health 2022;73:125-32. https://doi.org/10.5603/imh.2022.0025 10.5603/imh.2022.0025 [DOI] [PubMed] [Google Scholar]
- [4].Parsekar SS, Singh MM, Bhumika TV. Occupation-related psychological distress among police constables of Udupi taluk, Karnataka: A cross-sectional study. Indian J Occup Environ Med 2015;19:80-3. https://doi.org/10.4103/0019-5278.165329 10.4103/0019-5278.165329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kaur R, Chodagiri VK, Reddi NK. A Psychological Study of Stress, Personality and Coping in Police Personnel. Indian J Psychol Med 2013;35:141-7. https://doi.org/10.4103/0253-7176.116240 10.4103/0253-7176.116240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Oh HK, Jang CY, Ko MS. Factors influencing post-traumatic stress disorder among police officers in South Korea. Front Public Health 2022;10:1024284. https://doi.org/10.3389/fpubh.2022.1024284 10.3389/fpubh.2022.1024284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Singh A, Bhambal A, Saxena S, Tiwari V, Tiwari U. Frequency of Addictive Habits and its Association with Oral Diseases Among a Cross Section of Indian Police Personnel Connotation. J Coll Physicians Surg Pak 2016;26:403-7. [PubMed] [Google Scholar]
- [8].Pigou AC. The economics of welfare. London: Macmillan & Co, Limited; 1920. [Google Scholar]
- [9].Locker D. Measuring oral health: a conceptual framework. Community Dent Health 1988;5:3-18. [PubMed] [Google Scholar]
- [10].Malicka B, Skośkiewicz-Malinowska K, Kaczmarek U. The impact of socioeconomic status, general health and oral health on Health-Related Quality of Life, Oral Health-Related Quality of Life and mental health among Polish older adults. BMC Geriatr 2022;22:2. https://doi.org/10.1186/s12877-021-02716-7 10.1186/s12877-021-02716-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Barasuol JC, Santos PS, Moccelini BS, Magno MB, Bolan M, Martins-Júnior PA, Maia LC, Cardoso M. Association between dental pain and oral health-related quality of life in children and adolescents: A systematic review and meta-analysis. Community Dent Oral Epidemiol 2020;48:257-63. https://doi.org/10.1111/cdoe.12535 10.1111/cdoe.12535 [DOI] [PubMed] [Google Scholar]
- [12].Paśnik-Chwalik B, Konopka T. Impact of periodontitis on the Oral Health Impact Profile: A systematic review and meta-analysis. Dent Med Probl 2020;57:423-31. https://doi.org/10.17219/dmp/125028 10.17219/dmp/125028 [DOI] [PubMed] [Google Scholar]
- [13].Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health 1994;11:3-11. [PubMed] [Google Scholar]
- [14].Karnataka State Police. Available at: https://ksp.karnataka.gov.in/page/About%20Us/Organization/en (Accessed on: 4/1/2023).
- [15].Abhishek KN, Jain J, Shamarao S, Khanapure SC. Impact of periodontal status on oral health-related quality of life among police personnel in Virajpet, India. J Investig Clin Dent 2016;7:193-7. https://doi.org/10.1111/jicd.12139 10.1111/jicd.12139 [DOI] [PubMed] [Google Scholar]
- [16].Rajagopalachari US, Puranik MP, Sonde L. Impact of oral health on quality of life among police personnel in Bengaluru City, India: A cross-sectional survey. J Indian Assoc Public Health Dent 2015;13:42-7. https://doi.org/10.4103/2319-5932.153584 10.4103/2319-5932.153584 [DOI] [Google Scholar]
- [17].Oral health surveys: basic methods. 5th ed. Available at: https://www.who.int/publications-detail-redirect/9789241548649 (Accessed on: 27/1/2022).
- [18].Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000;25:3186-91. https://doi.org/10.1097/00007632-200012150-00014 10.1097/00007632-200012150-00014 [DOI] [PubMed] [Google Scholar]
- [19].Montero-Martín J, Bravo-Pérez M, Albaladejo-Martínez A, Hernández-Martín LA, Rosel-Gallardo EM. Validation the Oral Health Impact Profile (OHIP-14sp) for adults in Spain. Med Oral Patol Oral Cir Bucal 2009;14:E44-50. [PubMed] [Google Scholar]
- [20].Robinson PG, Gibson B, Khan FA, Birnbaum W. A comparison of OHIP 14 and OIDP as interviews and questionnaires. Community Dent Health 2001;18:144-9. [PubMed] [Google Scholar]
- [21].Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol 1997;25:284-90. https://doi.org/10.1111/j.1600-0528.1997.tb00941.x 10.1111/j.1600-0528.1997.tb00941.x [DOI] [PubMed] [Google Scholar]
- [22].Quality of Life Index by Country 2023. Available at: https://www.numbeo.com/quality-of-life/rankings_by_country.jsp (Accessed on: 8/1/2023).
- [23].Nearly one in two Indian adults have poor quality of life as per a study launched during The Protein Week 2021. Danone India. Available at: https://www.danone.in/press/nearly-one-in-two-indian-adults-have-poor-quality-of-life-as-per-a-study-launched-during-the-protein-week-2021/ (Accessed on: 8/1/2023). [Google Scholar]
- [24].Lee JH, Hwang SY, Kim EJ, Kim MJ. Comparison of risk factors between prehypertension and hypertension in Korean male industrial workers. Public Health Nurs Boston Mass 2006;23:314-23. https://doi.org/10.1111/j.1525-1446.2006.00567.x 10.1111/j.1525-1446.2006.00567.x [DOI] [PubMed] [Google Scholar]
- [25].Maurya R, Kundu D, Singh H, Mishra H. Oral Health Status, Dental Caries Experience & Treatment Needs of Population of Jammu City. Int J Oral Health Dent 2016;1:164-7. https://doi.org/10.5958/2395-499x.2015.00004.0 10.5958/2395-499x.2015.00004.0 [DOI] [Google Scholar]
- [26].Majeed MM, Ahmed N, Uzair M, Ghandhi D, Bashir TF, Khalid Z. Oral Health Status and Treatment Needs of Police Personnel in Karachi. Pak J Public Health 2020;10:96-102. https://doi.org/10.32413/pjph.v10i2.590 10.32413/pjph.v10i2.590 [DOI] [Google Scholar]
- [27].Basavaraj P. Dental caries experience and periodontal status of police personnel in Ghaziabad city. J Indian Assoc Public Health Dent 2011;9:44-50. [Google Scholar]
- [28].Singh A, Bhambal A, Saxena S, Tiwari V, Tiwari U. Assessment of dentition status and treatment needs of police personnel in Bhopal city, Central India. Int J Med Sci Public Health 2015;4:829-34. https://doi.org/10.5455/ijmsph.2015.11012015171 10.5455/ijmsph.2015.11012015171 [DOI] [Google Scholar]
- [29].Mythri H, Bharteesh JV. Awareness Regarding Oral Health & COTPA Act – 2003 among Karnataka State Reserve Police (KSRP) Stationed In Tumkur; a Brief Report. Int J Health Sci Res 2019;9:93-7. [Google Scholar]
- [30].Peršić Bukmir R, Paljević E, Pezelj-Ribarić S, Brekalo Pršo I. Association of the self-reported socioeconomic and health status with untreated dental caries and the oral hygiene level in adult patients. Dent Med Probl 2022;59:539-45. https://doi.org/10.17219/dmp/138908 10.17219/dmp/138908 [DOI] [PubMed] [Google Scholar]
- [31].Lima LJS, da Consolação Soares ME, Moreira LV, Ramos-Jorge J, Ramos-Jorge ML, Marques LS, Fernandes IB. Family income modifies the association between frequent sugar intake and dental caries. Int J Paediatr Dent 2023;00:1-8. https://doi.org/10.1111/ipd.13053 10.1111/ipd.13053 [DOI] [PubMed] [Google Scholar]
- [32].Dilip CL. Health status, treatment requirements, knowledge and attitude towards oral health of police recruits in Karnataka. J Indian Assoc Public Health Dent 2005;5:20-35. [Google Scholar]
- [33].Acharya S. Oral health-related quality of life and its associated factors in an Indian adult population. Oral Health Prev Dent 2008;6:175-84. [PubMed] [Google Scholar]
- [34].Costa SM, Martins CC, Bonfim M de LC, Zina LG, Paiva SM, Pordeus IA, Abreu M. H. A systematic review of socioeconomic indicators and dental caries in adults. Int J Environ Res Public Health 2012;9:3540-74. https://doi.org/10.3390/ijerph9103540 10.3390/ijerph9103540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Schertel Cassiano L, Abdullahi F, Leite FRM, López R, Peres MA, Nascimento GG. The association between halitosis and oral-health-related quality of life: A systematic review and meta-analysis. J Clin Periodontol 2021;48:1458-69. https://doi.org/10.1111/jcpe.13530 10.1111/jcpe.13530 [DOI] [PubMed] [Google Scholar]
- [36].Fotedar S, Sharma KR, Fotedar V, Bhardwaj V, Chauhan A, Manchanda K. Relationship between oral health status and oral health related quality of life in adults attending H.P Government Dental College, Shimla, Himachal Pradesh--India. Oral Health Dent Manag 2014;13:661-5. [PubMed] [Google Scholar]
- [37].Odisha police plan health insurance cover for cops. The Times of India. Available at: https://timesofindia.indiatimes.com/city/bhubaneswar/odisha-police-plan-health-insurance-cover-for-cops/articleshow/64321532.cms (Accessed on: 14/1/2023).
- [38].International Labour Standards on Occupational Safety and Health. Available at: https://www.ilo.org/global/standards/subjects-covered-by-international-labour-standards/occupational-safety-and-health/lang--en/index.htm (Accessed on: 14/1/2023).


