Summary
Out-hospital cardiac arrest (OHCA) is a multi-factor disease. Many studies have correlated OHCA with a patient’s lifestyle; unfortunately, less evidence highlights the correlation with meteorological factors. Methods: Analysis of 23959 OHCA rescue performed by the emergency medical system (EMS) of Lombardy Region, the most Italian populated region, in 2018 and 2019, the pre-pandemic era through a retrospective observational cohort study. The aim of the study consists on evaluating the probability of Return Of Spontaneous Circulation (ROSC) during months to highlight potential seasonal impact in ROSC achievement. In March and April, we highlight an increase of ROSC (OR: 1.20 95% CI 1.04-1.31; p < 0.001) compared to other months. During March and April, we highlight an increase of public access defibrillation (PAD) (3.5% vs 2.5%; p < 0.001), and a reduction of overage time of first vehicle on scene (11.5 vs 11.8; p < 0.001) and age of patient (73.5 vs 74.2; p < 0.01). Finally, we highlight a slight reduction of cancer patient (1.6% vs 1.1%; p = 0.01). We didn’t register significant differences in the other variables analyzed as: onset place, sex, rescue team and the patient’s death before the rescue arrive. We highlight a difference in ROSC probability during the first month of spring. We register few differences in patient characteristics and EMS rescue, though just PAD use and age clinically impact OHCA patients. In this study, we are unable to fully understand the modification of the probability of ROSC in these months. Even though four variables have a statistically significant difference, they can’t fully explain this modification. Different variables like meteorological and seasonal factor must be considered. We propose more research on this item.
Keywords: Resuscitation, Emergency medical system, Environmental pollution
Introduction
Out Hospital Cardiac arrest (OHCA), which is the cessation of cardiac mechanical activity in a person outside of a hospital setting, is a severe event with a high incidence (50 to 120 per 100.000 people) and a low survival rate worldwide (7%) [1]. Return of spontaneous circulation (ROSC) is correlated to many demographic variables [2, 3], like time of the Emergency medical system (EMS) rescue [4], layperson training [5, 6] and the protocol used by EMS [7, 8].
Environmental factors could modify the ROSC rate [9, 10]. Although little evidence has been published, that’s why is challenging to find a clear correlation between the high number of environmental variables and OHCA.
Unfortunately, in the last three years, the research in the medical emergency was focused on Covid impact [11, 12] and the modification of EMS [11] and the collateral damage of COVID [13-17]. We highlight plenty of research focused on OHCA epidemiology, COVID [18-21] and other clinical aspects [22].
Despite some evidence correlating the meteorological factors and air pollutants with the incidence of OHCA [22-24], an increase of PM2.5 and average temperature are correlated with a rise in daily OHCA [23, 25].
Lombardy is the largest Italian region, with 9.96 million inhabitants and an area of 23 863 km2. All missions are coordinated by a single Regional Agency, AREU, which coordinates the rescue through wheeled vehicles or helicopters. AREU’s tecniques processed about 1 million calls in one years and in 800.000 call a vehicle was sent to rescue the patient AREU consist of 265 ambulances with a crew of 2-3 rescuers, 50 Intermediate Rescue Vehicles with a nurse, 59 Advanced Rescue Vehicles and 5 helicopters [26], nurse and doctor are trained by ACLS course [27-28]. All mission data are record in one single register, call EmMa (Emergency Management) [29].
The aim of the study consists on analyzing the impact during months of ROSC achievement, to highlight a potential seasonal link with meteorological factors.
Methods
STUDY DESIGN
The study is a retrospective observational cohort, it was conducted following the principles of the Helsinki declaration and was approved by the AREU Data Protection Officer in July 2022.
The Lombardy AREU headquarters register provided data analysis. The data analysis process was conducted employing the SAS-AREU portal. The portal contains all data regarding emergency calls, and the scenarios involving OHCA were selected.
The monthly diagnoses of OHCA in two years, from 1 January 2018 to 31 December 2019, was selected in SAS-AREU Database.
DATA
We used fourteen variables registered in the SAS-AREU database. The correlation between variables and ROSC was controlled in previous research. The variables were sex, age, timing of rescue, the onset of the event, type of rescue time and signs of death.
Data are available on AREU website. It is possible to find “OHCA” records in the SAS-AREU portal. The portal contains all the data related to emergency calls; it has been selected all the scenarios involving OHCA.
At every 118 call, performed in Lombardy Region, the EMS receiver automatically opens a record in SAS-AREU, the caller introduces the demographic characteristics and information about the main clinical problem of the patient. In case of OHCA patients, MSB (basic life supper vehicle) and an MSA (advanced cardiovascular vehicle) are sent to the scene. The vehicle has a GPS tracker, and an automatic system which records the timing of rescue. During the rescue procedure, the MSB or MSA operator informs the medical director of the operation center with all other information to define the clinical status of the patient and the correct hospital. All data are correctly recorded in the SAS-AREU database. All data are necessary to identify the appropriate hospital Hub, while the GPS tracker automatically records logistic data.
STATISTICAL EVALUATION
We compared the characteristic of rescue in April and March with other months of the year in 2018 and 2019. The categorical variables are presented as numbers and percentage, and the continuous variables are presented as mean and standard deviation (SD). The categorical variables were analyzed by Z test for proportion and Odds Ratio (OR) with relative Confidence interval (CI) 95%. Continuous variables were tested for normality by means of the Kolmogorov-Smirnov test and the appropriate analysis for Z test for means. Differences were considered significant when p < 0.05. Otherwise, they were considered non-significant (NS). The Prism 8.0.1 statistical software (GraphPad Software LLC, San Diego, CA, USA) was used for this aim.
Results
A total of 23959 OHCA ware analyzed, all event occurred in Lombardy region in the two years of analyses. 11663 (48.7%) was rescue by EMS in 2018 and 12296 (51.3%) was rescue in 2019.
Table I summarizes the comparison of rescues during March and April in 2018 and 2019 compared to all other months in 2018 and 2019. The average age (73.5 vs 74.2; p = 0.01) and the time of the first vehicle on scene (11.8 vs 11.5; p = 0.0006) in March and April were significant low than other months.
Tab. I.
Comparison of overage age and overage time of rescue.
| 2018-2019 | March-April | p-value | |
|---|---|---|---|
| Age (SD) | 74.2 (16.6) | 73.5 (16.5) | < 0.01 |
| Overage time of First vehicle (SD) | 11.8 (6.5) | 11.5 (5.3) | < 0.01 |
| Overage Time hospital arrived (SD) | 53.2 (24.3) | 52.4 (22.6) | 0.046 |
No difference was highlight in the overage time of hospital arrival.
Table II shows the analyzed ROSC variables. The significant differences are recorded for the use of the Pads, which is greater during the spring (3.5% vs 2.5%; p = 0.0005), and there is also a reduction in OHCA for patients diagnosed with neoplastic disease (1.6% vs 1.1%; p = 0.01).
Tab. II.
Demographic variables.
| 2018-2019 Without March-April N (%) | 2018-2019 March-April N (%) | p-value | |
|---|---|---|---|
| Number of OHCA | 20038 (80.4%) | 3921 (19.6%) | |
| ROSC | 1686 (8.4%) | 380 (9.7%) | < 0.01 |
| Female | 7811 (39.0%) | 1526 (38.9%) | 0.47 |
| RCP layperson | 4320 (21.6%) | 876 (22.3%) | 0.14 |
| PAD | 509 (2.5%) | 136 (3.5%) | < 0.001 |
| no MSI | 16991 (84.8%) | 3338 (85.1%) | 0.29 |
| no MSA | 7951 (39.7%) | 1546 (39.4%) | 0.38 |
| Death people | 2793 (13.9%) | 516 (13.2%) | 0.10 |
| Workplace | 914 (4.6%) | 190 (4.9%) | 0.22 |
| Open place | 1010 (5.0%) | 203 (5.2%) | 0.36 |
| Traumatic event | 1377 (6.9%) | 284 (7.2%) | 0.20 |
| Neoplastic patient | 313 (1.6%) | 43 (1.1%) | 0.01 |
| PAD: Public access defibrillation; MSI: Vehicle with a Nurse; MSA: Vehicle with a doctor and a nurse; Death people: a person with clear sign of death (i.e. Decapitation). | |||
Figure 1 shows the percentage of ROSC on the total of OHCAs; there is an increase in the months of March and April compared to the other months of the year. The value reaches 9.2% in March and 10.3% in April. In the two months, in the years of follow-up, the ROSC significant increased (OR: 1.20 95% CI 1.04-1.31; p < 0.001).
Fig. 1.
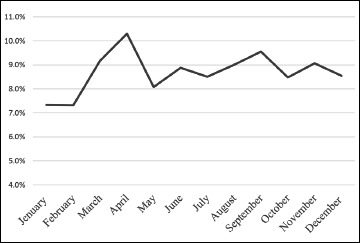
Percentage of ROSC on total of monthly OHCA in 2018 and 2019.
Noteworthy, four variables have a significant difference in the months of March and April. The most relevant was a major use of PAD OR 1.38 (CI 95% 1.14-1.67; p < 0.001) and the reduction of the average time of the first vehicle on scene (11.8 vs 11.5; p < 0.001), average age (73.5 vs 74.2; p = 0.01) and a slight reduction of cancer patient (1.6% vs 1.1%; p = 0.01).
Discussion
In accordance with the aim, we analyzed the ROSC in different months over the two years. We highlight an increase in ROSC during March and April in 2018 and 2019, as shown in Figure 1.
We analyzed 14 variables, all registered in AREU’s database, as shown in Table I and Table II. All 14 variables, as evidenced in previous research, by McNally B. et al. [29], are correlated with the probability of ROSC.
Despite the statistical significance of the four variables, just the use of PAD and the average age of the patient have the major clinical impact, in fact, the other two variables, first ambulance on scena and percentage of oncology patients, were lightly changed, and the impact on ROSC was irrelevant.
Furthermore, could be difficult interpret as the increase of ROSC in the first month of spring. In fact, there wasn’t a reason for the reduction of average age, maybe meteorological and seasonal factors could alter the epidemiology of OHCA how highlight by Kim JH et al [23], but more research must be implemented on this topic for coordinate new public health project to increase ROSC.
No less significant is the increase of PAD’s use; in fact, during the spring season, we didn’t register a modification of OHCA location, no significant modification was registered in the workplace or in a closed place area, where the number of mandatory PAD is high. This point should be the focus of future research. In fact, we must identify a reason for this phenomenon to achieve the possibility of increasing the use of Pad in OHCA.
Different factors, including environmental ones, can cause OHCA, often they are unknown, and the scientific community should reconsider those issues related to OHCA epidemiology. Great attention has been paid to COVID-19 and OHCA reports in recent years, but it is necessary to take a step back and analyze the pre-pandemic data in order to study the environmental factors that may contribute to OHCA.
This study adds two key aspects to OHCA’s research. The first aspect consists in changing the focus of COVID-19 impact on OHCA epidemiology, and reconsidering the pre pandemic issues, like the influence of external factors, or the meteorological impact on the ROSC. The second aspect concerns a legislative matter. As a matter of fact, after the Italian Legislative degree (D Lgsl 81/08), D Lgsl 158/12 and D Lgsl 116/21, the ROSC study became important to highlight the impact of this law on OHCA’s patient outcome. The implication of the seasonal correlation between OHCA and ROSC should be investigated in order to highlight the possible link with pollution or other events unknown in this research. The research on OHCA during spring season might underline a difference in the rescue condition or the clinical characteristic of the patient, which can help future policy.
Conclusion
During the first month of spring, we measured an increase in ROSC probability in the Lombardy region. This phenomenon is correlated with the increasing in Pads used by the layperson and a reduction of the arriving time of the first vehicle on scene. However, this change could not completely justify the ROSC increase. Seasonal or meteorological phenomena could influence OHCA epidemiology.
The study of the phenomenon is an important public health’s concern. In fact, a deep analysis of clinical patients, or meteorological factors could highlight new variables for the ROSC achievement in patients affected by OHCA. The second study’s aim is to bring attention back to the pre COVID-19 pandemic types of studies, and the impact of the environment on the development of the disease in addition to COVID-19.
Acknowledgments
The authors are sincerely grateful to Elisa Pes (elisa-pes@hotmail.it) for the language revision of the manuscript.
Conflict of interest statement
All authors declare no conflicts of interest.
Funding
The Working Group did not receive any funds.
Authors’ contributions
GS, CS and GMS conceived and designed the study. GS, AA collected and analyzed the data. GS drafted the first version of the manuscript. All authors edited, revised the manuscript, and approved the final version before submission.
Figures and tables
References
- [1].Lim ZJ, Ponnapa Reddy M, Afroz A, Billah B, Shekar K, Subramaniam A. Incidence and outcome of out-of-hospital cardiac arrests in the COVID-19 era: A systematic review and meta-analysis. Resuscitation 2020;157:248-58. https://doi.org/10.1016/j.resuscitation.2020.10.025 10.1016/j.resuscitation.2020.10.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Lim GH, Seow E. Resuscitation for patients with out-of-hospital cardiac arrest: Singapore. Prehosp Disaster Med 2002;17:96-101. https://doi.org/10.1017/s1049023x00000248 10.1017/s1049023x00000248 [DOI] [PubMed] [Google Scholar]
- [3].Mayr NP, Mayr T, Tassani P, Martin K. Use of automated external defibrillators in the occupational setting in Germany: a pilot study. J Occup Environ Med 2012;54:789-91. https://doi.org/10.1097/JOM.0b013e318256f65c 10.1097/JOM.0b013e318256f65c [DOI] [PubMed] [Google Scholar]
- [4].Villa GF, Kette F, Balzarini F, Riccò M, Manera M, Solaro N, Pagliosa A, Zoli A, Migliori M, Sechi GM, Odone A, Signorelli C. Out-of-hospital cardiac arrest (OHCA) Survey in Lombardy: data analysis through prospective short time period assessment. Acta Biomed 2019;90(9-S):64-70. https://doi.org/10.23750/abm.v90i9-S.8710 10.23750/abm.v90i9-S.8710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Tay PJM, Pek PP, Fan Q, Ng YY, Leong BS, Gan HN, Mao DR, Chia MYC, Cheah SO, Doctor N, Tham LP, Ong MEH. Effectiveness of a community based out-of-hospital cardiac arrest (OHCA) interventional bundle: Results of a pilot study. Resuscitation 2020;146:220-8. https://doi.org/10.1016/j.resuscitation.2019.10.015 10.1016/j.resuscitation.2019.10.015 [DOI] [PubMed] [Google Scholar]
- [6].Lukić A, Lulić I, Lulić D, Ognjanović Z, Cerovečki D, Telebar S, Mašić I. Analysis of out-of-hospital cardiac arrest in Croatia – survival, bystander cardiopulmonary resuscitation, and impact of physician’s experience on cardiac arrest management: a single center observational study. Croat Med J 2016;57:591-600. https://doi.org/10.3325/cmj.2016.57.591 10.3325/cmj.2016.57.591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Fukuda T, Ohashi-Fukuda N, Kondo Y, Hayashida K, Kukita I. Association of Prehospital Advanced Life Support by Physician With Survival After Out-of-Hospital Cardiac Arrest With Blunt Trauma Following Traffic Collisions: Japanese Registry-Based Study. JAMA Surg 2018;153:e180674. https://doi.org/10.1001/jamasurg.2018.0674 10.1001/jamasurg.2018.0674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ong MEH, Chan YH, Ang HY, Lim SH, Tan KL. Resuscitation of out-of-hospital cardiac arrest by Asian primary health-care physicians. Resuscitation 2005;65:191-5. https://doi.org/10.1016/j.resuscitation.2004.11.021 10.1016/j.resuscitation.2004.11.021 [DOI] [PubMed] [Google Scholar]
- [9].Tobaldini E, Iodice S, Bonora R, Bonzini M, Brambilla A, Sesana G, Bollati V, Montano N. Out-of-hospital cardiac arrests in a large metropolitan area: synergistic effect of exposure to air particulates and high temperature. Eur J Prev Cardiol 2020:513-9. https://doi.org/10.1177/2047487319862063 10.1177/2047487319862063 [DOI] [PubMed] [Google Scholar]
- [10].Zhao B, Johnston FH, Salimi F, Kurabayashi M, Negishi K. Short-term exposure to ambient fine particulate matter and out-of-hospital cardiac arrest: a nationwide case-crossover study in Japan. Lancet Planet Health 2020;4:e15-e23. https://doi.org/10.1016/S2542-5196(19)30262-1 10.1016/S2542-5196(19)30262-1 [DOI] [PubMed] [Google Scholar]
- [11].Stirparo G, Ristagno G, Bellini L, Bonora R, Pagliosa A, Migliari M, Andreassi A, Signorelli C, Sechi GM, Fagoni N. Changes to the Major Trauma Pre-Hospital Emergency Medical System Network before and during the 2019 COVID-19 Pandemic. J Clin Med 2022;11:6748. https://doi.org/10.3390/jcm11226748 10.3390/jcm11226748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Signorelli C, Odone A, Stirparo G, Cereda D, Gramegna M, Trivelli M, Rezza G. SARS-CoV-2 transmission in the Lombardy Region: the increase of household contagion and its implication for containment measures. Acta Biomed 2020;91:e2020195. https://doi.org/10.23750/abm.v91i4.10994 10.23750/abm.v91i4.10994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Stirparo G, Bellini L, Fagoni N, Compatti S, Botteri M, Villa GF, Sironi S, Signorelli C, Sechi GM, Zoli A. Missed training, collateral damage from COVID-19? Disaster Med Public Health Prep 2022:1-8. https://doi.org/10.1017/dmp.2022.14 10.1017/dmp.2022.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Caminiti C, Maglietta G, Meschi T, Ticinesi A, Silva M, Sverzellati N. Effects of the COVID-19 Epidemic on Hospital Admissions for Non-Communicable Diseases in a Large Italian University-Hospital: A Descriptive Case-Series Study. J Clin Med 2021;10:880. https://doi.org/10.3390/jcm10040880 10.3390/jcm10040880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Diegoli H, Magalhães PSC, Martins SCO, Moro CHC, França PHC, Safanelli J, Nagel V, Venancio VG, Liberato RB, Longo AL. Decrease in Hospital Admissions for Transient Ischemic Attack, Mild, and Moderate Stroke During the COVID-19 Era. Stroke 2020;51:2315-21. https://doi.org/10.1161/STROKEAHA.120.030481 10.1161/STROKEAHA.120.030481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Fagoni N, Perone G, Villa GF, Celi S, Bera P, Sechi GM, Mare C, Zoli A, Botteri M. The Lombardy Emergency Medical System Faced with COVID-19: The Impact of Out-of-Hospital Outbreak. Prehosp Emerg Care 2021;25:1-7. https://doi.org/10.1080/10903127.2020.1824051 10.1080/10903127.2020.1824051 [DOI] [PubMed] [Google Scholar]
- [17].Stirparo G, Bellini L, Ristagno G, Bonora R, Pagliosa A, Migliari M, Andreassi A, Signorelli C, Sechi GM, Fagoni N. The Impact of COVID-19 on Lombardy Region ST-Elevation Myocardial Infarction Emergency Medical System Network – A Three-Year Study. J Clin Med 2022;11:5718. https://doi.org/10.3390/jcm11195718 10.3390/jcm11195718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, Klersy C, Palo A, Contri E, Ronchi V, Beretta G, Reali F, Parogni P, Facchin F, Bua D, Rizzi U, Bussi D, Ruggeri S, Oltrona Visconti L, Savastano S, Lombardia CARe Researchers . Out-of-Hospital Cardiac Arrest during the COVID-19 Outbreak in Italy. N Engl J Med 2020;383:496-8. https://doi.org/10.1056/NEJMc2010418 10.1056/NEJMc2010418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, Palo A, Contri E, Ronchi V, Beretta G, Reali F, Parogni PP, Facchin F, Rizzi U, Bussi D, Ruggeri S, Oltrona Visconti L, Savastano S, all the Lombardia CARe researchers . Treatment of out-of-hospital cardiac arrest in the COVID-19 era: A 100 days experience from the Lombardy region. PLoS One 2020;15:e0241028. https://doi.org/10.1371/journal.pone.0241028 10.1371/journal.pone.0241028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Scquizzato T, Landoni G, Paoli A, Lembo R, Fominskiy E, Kuzovlev A, Likhvantsev V, Zangrillo A. Effects of COVID-19 pandemic on out-of-hospital cardiac arrests: A systematic review. Resuscitation 2020;157:241-7. https://doi.org/10.1016/j.resuscitation.2020.10.020 10.1016/j.resuscitation.2020.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Stirparo G, Fagoni N, Bellini L, Oradini-Alacreu A, Migliari M, Villa GF, Botteri M, Signorelli C, Sechi GM, Zoli A. Cardiopulmonary resuscitation missed by bystanders: Collateral damage of coronavirus disease 2019. Acta Anaesthesiol Scand 2022;66:1124-9. https://doi.org/10.1111/aas.14117 10.1111/aas.14117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Cheng FJ, Wu KH, Hung SC, Lee KH, Lee CW, Liu KY, Hsu PC. Association between ambient air pollution and out-of-hospital cardiac arrest: are there potentially susceptible groups? J Expo Sci Environ Epidemiol 2020;30:641-9. https://doi.org/10.1038/s41370-019-0140-7 10.1038/s41370-019-0140-7 [DOI] [PubMed] [Google Scholar]
- [23].Kim JH, Hong J, Jung J, Im JS. Effect of meteorological factors and air pollutants on out-of-hospital cardiac arrests: A time series analysis. Heart 2020;106:1218-27. https://doi.org/10.1136/heartjnl-2019-316452 10.1136/heartjnl-2019-316452 [DOI] [PubMed] [Google Scholar]
- [24].Haikerwal A, Akram M, Del Monaco A, Smith K, Sim MR, Meyer M, Tonkin AM, Abramson MJ, Dennekamp M. Impact of Fine Particulate Matter (PM2.5) Exposure During Wildfires on Cardiovascular Health Outcomes. J Am Heart Assoc 2015;4:e001653. https://doi.org/10.1161/JAHA.114.001653 10.1161/JAHA.114.001653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Gentile FR, Primi R, Baldi E, Compagnoni S, Mare C, Contri E, Reali F, Bussi D, Facchin F, Currao A, Bendotti S, Savastano S, Lombardia CARe researchers . Out-of-hospital cardiac arrest and ambient air pollution: A dose-effect relationship and an association with OHCA incidence. PLoS One 2021;16:e0256526. https://doi.org/10.1371/journal.pone.0256526 10.1371/journal.pone.0256526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Botteri M, Celi S, Perone G, Prati E, Bera P, Villa GF, Mare C, Sechi GM, Zoli A, Fagoni N. Effectiveness of massive transfusion protocol activation in pre-hospital setting for major trauma. Injury 2022;53:1581-6. https://doi.org/10.1016/j.injury.2021.12.047 10.1016/j.injury.2021.12.047 [DOI] [PubMed] [Google Scholar]
- [27].Stirparo G, Gambolò L, Bellini L, Medioli F, Bertuol M, Guasconi M, Sulla F, Artioli G, Sarli L. Satisfaction evaluation for ACLS training. Acta Biomed 2022;93:e2022260. https://doi.org/10.23750/abm.v93i3.13337 10.23750/abm.v93i3.13337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Stirparo G, Solla D, Gambolò L, Bellini L, Mantovanelli L, Trapani M, Pregliasco FE, Sarli L, Signorelli C. SIMED-New Doc course, a matter of reflection. Acta Biomed 2023;94:e2023035. https://doi.org/10.23750/abm.v94i1.13959 10.23750/abm.v94i1.13959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Stirparo G, Pireddu R, Kacerik E, Scognamiglio T, Andreassi A, Sechi GM, Zoli A, Signorelli C. Stroke and the need for immediate assistance at the place of onset: the future of mandatory training for lay people in Italy. Ann Ig 2022. https://doi.org/10.7416/ai.2022.2553 10.7416/ai.2022.2553 [DOI] [PubMed] [Google Scholar]


