Abstract
To highlight a rare case of inner ear barotrauma as a post-operative complication following robot-assisted radical prostatectomy (RARP). A 65-year-old man diagnosed with localised prostate carcinoma underwent elective RARP in a steep Trendelenburg position. Postoperatively, the patient complained of bothersome dizziness and spinning of surroundings associated with nausea. The patient was diagnosed to have vestibular symptoms secondary to inner ear barotrauma. He was started on prochlorperazine 12.5 mg and antibiotics, following which the patient improved. Vestibular rehabilitation exercises were taught to the patient. After 3 days of treatment, the patient did well with no episodes of dizziness. The patient was discharged on tablet cinnarizine 25 mg thrice daily for a week. On follow-up, the patient is asymptomatic. Inner ear barotrauma can be a rare complication of a combination of prolonged steep Trendelenburg during robotic surgery and pneumoperitoneum. Only further reporting of such incidents can help determine predisposing factors and precautions for preventing such incidents.
Keywords: Complications, inner ear barotrauma, robot-assisted radical prostatectomy, steep Trendelenburg position, vestibular symptoms
INTRODUCTION
Robot-assisted surgery has brought a new revolution with a significant reduction in technical challenges and the learning curve for minimally invasive surgery. Robot-assisted prostatectomy is presently the gold standard for carcinoma prostate.[1] However, with the introduction of the robot, there have been many considerations such as specialised patient positioning and longer surgical times. Longer operative times in Trendelenburg positions are fraught with increased intracerebral pressure, middle ear pressure and intraocular pressure. Patients with morbid obesity, ophthalmic problems and decreased cardiopulmonary reserve are more at risk of these intra-operative and post-operative complications.[2] We describe a rare case of inner ear barotrauma as a post-operative complication following robot-assisted radical prostatectomy (RARP).
CASE REPORT
A 65-year-old man with no comorbidities and a diagnosis of localised prostate carcinoma was admitted for elective RARP. There were no prior otological complaints, and he could perform all his daily activities by himself. General physical examinations were within the normal limits. The abdomen was soft, non-tender and digital rectal examination revealed a right lobe’s Grade 2 prostate with a hard nodule. Transrectal ultrasound-guided biopsy showed prostatic adenocarcinoma with a Gleason score of 3 + 3. Further staging on magnetic resonance imaging revealed a T2aN0M0 prostate cancer prostate-specific antigen of 22 ng/ml. As per patient preference and with informed consent patient underwent RARP.
Propofol, fentanyl and vecuronium were used during anaesthesia induction and muscle relaxation. Anaesthesia was maintained with nitrous oxide and sevoflurane. For RARP, the patient was placed in a steep Trendelenburg position (>30°). The total console time was 4 h. RARP and bilateral standard pelvic lymph node dissection (B/L SPLND) were done, and the procedure went uneventful [Figure 1]. The patient’s systolic blood pressure was between 110 and 140 during the procedure.
Figure 1.
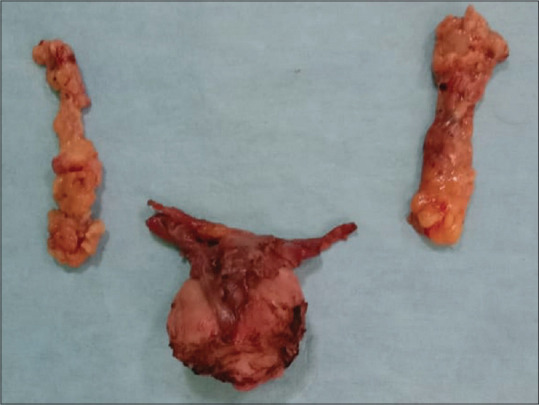
Specimen of robot-assisted radical prostatectomy and standard bilateral pelvic lymph node dissection
Twelve hours postoperatively, the patient complained of bothersome dizziness and spinning of surroundings associated with nausea. There were no complaints of decreased hearing or headache. Neurological evaluation was normal. Ear-nose-throat (ENT) consult was taken. Otoscopic examination revealed an intact bilateral tympanic membrane with no nystagmus. Rinne’s test was positive on the right side and inconclusive on the left side. Weber’s test was lateralsed to the right ear. The audiometric test done suggested bilateral mild sensorineural hearing loss [Figure 2]. Impedance audiometry was suggestive of Type A pattern bilaterally and absented bilateral acoustic reflexes. A non-contact tonometer showed left and right eye pressures of 16.7 and 17.3 mmHg on ophthalmological examination, respectively. The rest of the ophthalmological examination was within the normal limits. Based on clinical examination and evaluation, the patient was diagnosed to have mainly vestibular symptoms secondary to inner ear barotrauma. He was started on prochlorperazine 12.5 mg and antibiotics, following which the patient improved. Vestibular rehabilitation exercises were taught to the patient in the head, eye and shoulder movements.
Figure 2.
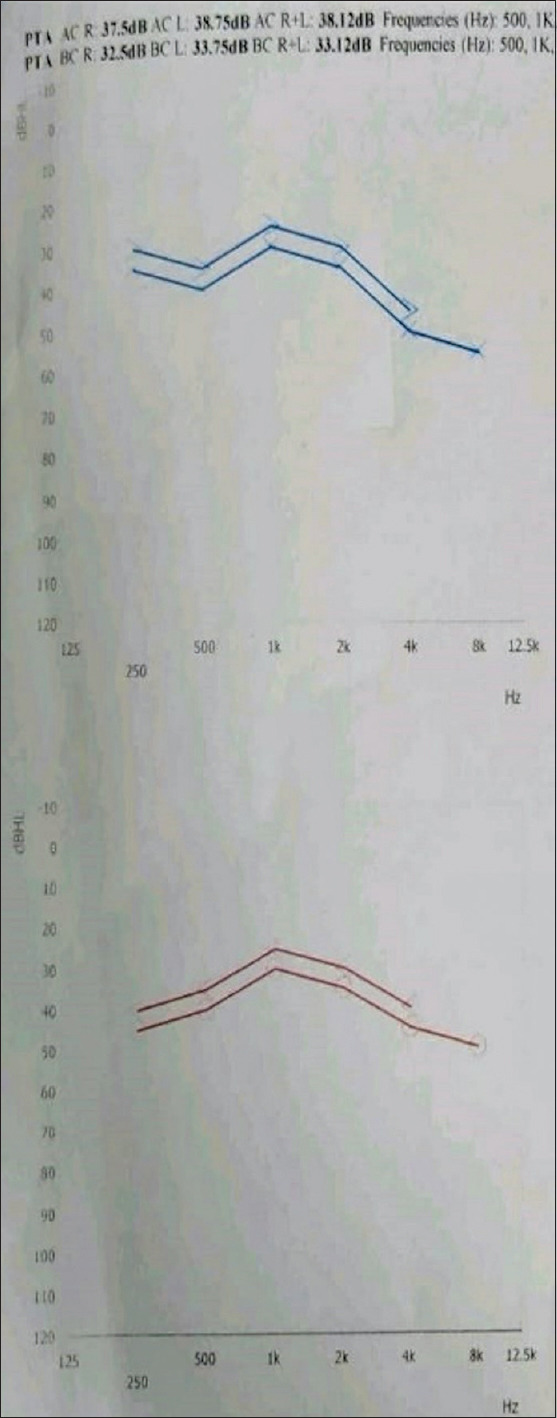
Audiometry showing bilateral mild sensorineural hearing loss (Impedance audiometry bilateral A Type, bilateral acoustic reflexes absent)
After 3 days of treatment, the patient did well with no episodes of dizziness. The patient was then started on tablet cinnarizine 25 mg thrice daily. The patient was discharged on the postoperative day (POD) 7 on oral medication and advised to perform vestibular rehabilitation exercises. The medication was stopped after 1 week. Histopathology showed prostatic acinar adenocarcinoma, pT2N0. Foley’s catheter was removed on POD 10. In 1 year, the patient is doing well and has achieved day and night time continence.
DISCUSSION
The steep Trendelenburg position helps in optimal surgical exposure in radical prostatectomy. However, the steep Trendelenburg position combined with pneumoperitoneum induces significant cardiovascular, respiratory and cerebrovascular changes.[1] The Trendelenburg position results in increased venous return, which increases the mean arterial pressure. This increases the cardiac output transiently, which returns to normal within 10 min in an average healthy adult.[2] Pneumoperitoneum with Trendelenburg position decreases the functional residual capacity and decreases lung compliance. These can cause a mild decrease in the partial pressure of arterial oxygen. However, all these return to normal with a neutral position. Numerous cases of ischemic optic neuropathy have been reported related to increased venous pressure and interstitial edema, which causes decreased blood flow.[2] Steep Trendelenburg position and pneumoperitoneum increase intraocular pressure (IOP), leading to cerebral oedema. Prolonged steep Trendelenburg position for 7–10 h might result in cerebral oedema and neurological damage.[3] The increase in IOP can lead to vision loss, optic neuropathy and retinal detachment. Risk factors associated are pre-existing ocular disease or glaucoma. Patients with any ocular risk factors should be evaluated by an ophthalmologist preoperatively.[3]
Steep Trendelenburg position and pneumoperitoneum could significantly increase middle ear pressure and continue postoperatively. The response is related to the time and degree of Trendelenburg position and CO2 diffusion to the middle ear. The changes in middle ear pressure can result in prolonged postoperative nausea, vomiting, rupture of membranes and nerve damage. Pre-operative evaluation should include any history of ear-related diseases, and if present, it should be evaluated by an ENT consult.[3]
The most commonly reported complication related to the ear is bleeding from the ear. The pathophysiology described in the literature is increased arterial and venous pressures resulting in rupture of subcutaneous vessels. A steep Trendelenburg position for a prolonged duration might also result in benign paroxysmal positional vertigo. Otoconia dislodgement to the most dependent areas of semicircular canals in the inner ear in this vertical position might trigger this episode of benign paroxysmal positional vertigo.[2]
The history and physical examination were directed to rule out any central or peripheral cause of vertigo. Ear, eye, neurological and cardiac examination should be directed to find the cause of vertigo. The most common differential diagnosis of vertigo is labyrinthitis, vestibular neuronitis, benign paroxysmal positional vertigo, inner ear barotrauma and Meniere’s disease. Most cases are usually benign, but central causes should also be kept in mind while evaluating a cerebrovascular accident, tumour, and a perilymphatic fistula. Inner ear barotrauma includes intralabyrinthine membrane tear, perilymph fistula and inner ear haemorrhage.[4] Determining the cause in many cases is difficult. Barotrauma can be associated with hearing loss, as was present in this index case. The treatment should be directed towards a specific aetiology. The recommended management option is conservative in inner ear barotrauma. Medications should be used only in the acute setting, as was given in this index case. Prolonged medicines should be avoided, and the patient should be warned about the side effects of these medications, such as drowsiness, dry mouth and blurred vision. Prochlorperazine may also cause seizures. Lifestyle changes, including salt restriction and avoiding coffee and alcohol, should be advised. Vestibular rehabilitation exercise and balance stabilisation exercise are essential in preventing recurrences. Surgery might be needed in cases with severe and persisting symptoms.[4]
The limited literature might be due to under-reporting and rare presentations of acute labyrinthitis post robotic and laparoscopic surgery in the steep Trendelenburg position. The factors responsible are still unclear, such as predisposing factors, duration of surgery and the degree of steep Trendelenburg position. The use of nitrous oxide with pneumoperitoneum might be another reason, leading to barotrauma in the index patient. Due to nitrous oxide’s greater blood solubility, it enters closed gas cavities quicker than nitrogen is eliminated, resulting in the expansion of air or low-solubility gas-filled cavities. Nitrous gas is relatively contraindicated in intestinal, laparoscopic, middle ear and ocular surgery due to these risks.[5]
Measures that need to be taken to decrease the incidence of this complication:
Pre-operative risk factors such as ear disease and eye diseases
Minimising the operative time
Minimising the pneumoperitoneum
Minimum Trendelenburg position to keep the operative field clear of the small bowel
Nitrous oxide should be used with caution in robotic surgeries.
CONCLUSION
Complications due to the steep Trendelenburg position during robotic procedures are not uncommon. Inner ear barotrauma can be a rare complication of a combination of prolonged steep Trendelenburg during robotic surgery. Only further reporting of such incidents can help determine predisposing factors and precautions for preventing such incidents.
Consent
I hereby give my consent for images or other clinical information relating to my case to be reported in a medical publication. I understand that my name and initials will not be published and that efforts will be made to conceal my identity, but that anonymity cannot be guaranteed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kalmar AF, Foubert L, Hendrickx JF, Mottrie A, Absalom A, Mortier EP, et al. Influence of steep Trendelenburg position and CO2 pneumoperitoneum on cardiovascular, cerebrovascular, and respiratory homeostasis during robotic prostatectomy. Br J Anaesth. 2010;104:433–9. doi: 10.1093/bja/aeq018. [DOI] [PubMed] [Google Scholar]
- 2.Arvizo C, Mehta ST, Yunker A. Adverse events related to Trendelenburg position during laparoscopic surgery:Recommendations and review of the literature. Curr Opin Obstet Gynecol. 2018;30:272–8. doi: 10.1097/GCO.0000000000000471. [DOI] [PubMed] [Google Scholar]
- 3.Balbay MD, Koc E, Canda AE. Robot-assisted radical cystectomy:Patient selection and special considerations. Robot Surg. 2017;4:101–6. doi: 10.2147/RSRR.S119858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elliott EJ, Smart DR. The assessment and management of inner ear barotrauma in divers and recommendations for returning to diving. Diving Hyperb Med. 2014;44:208–22. [PubMed] [Google Scholar]
- 5.Brown SM, Sneyd JR. Nitrous oxide in modern anaesthetic practice. BJA Educ. 2016;16:87–91. [Google Scholar]


