Abstract
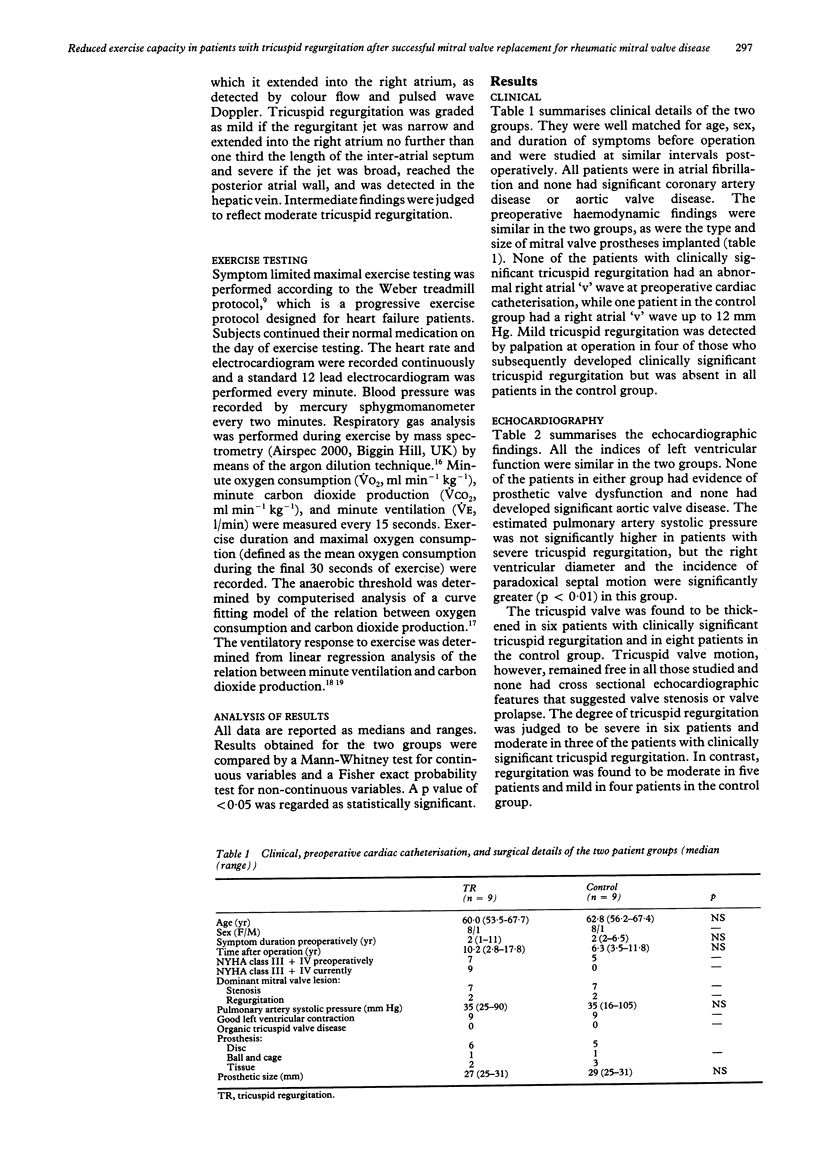
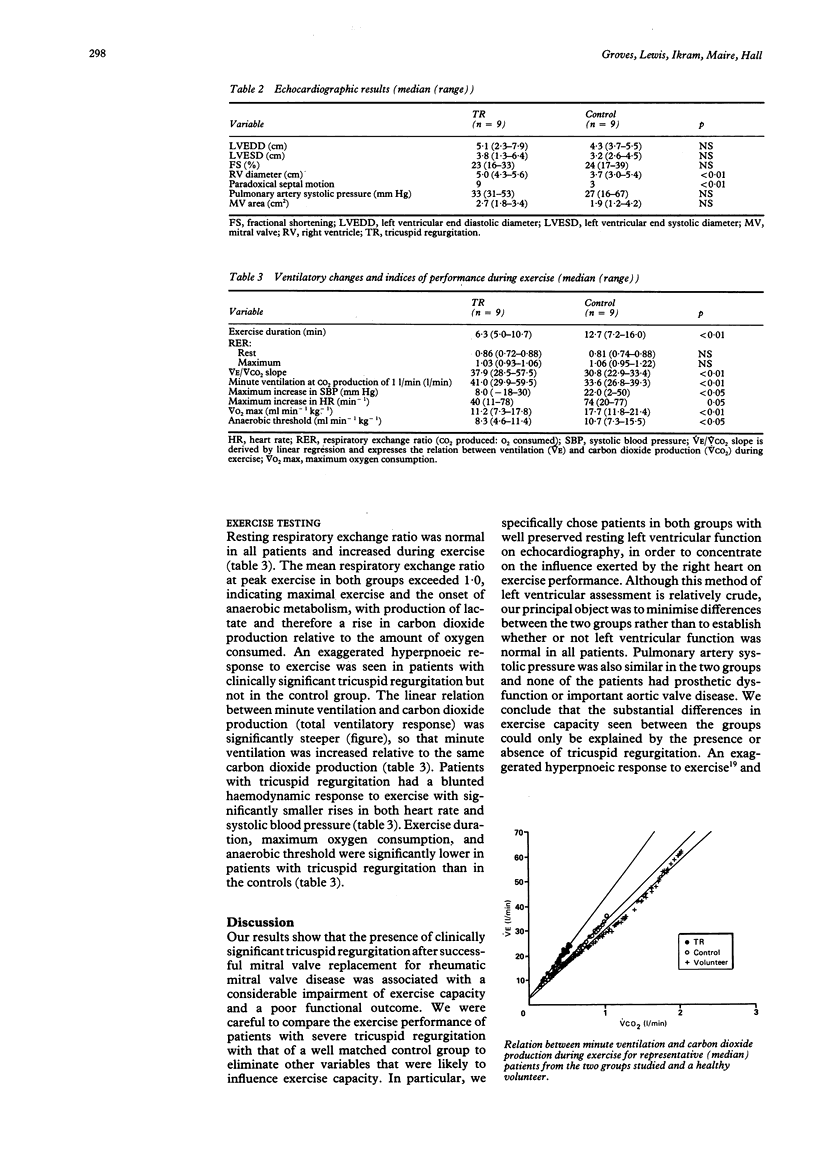
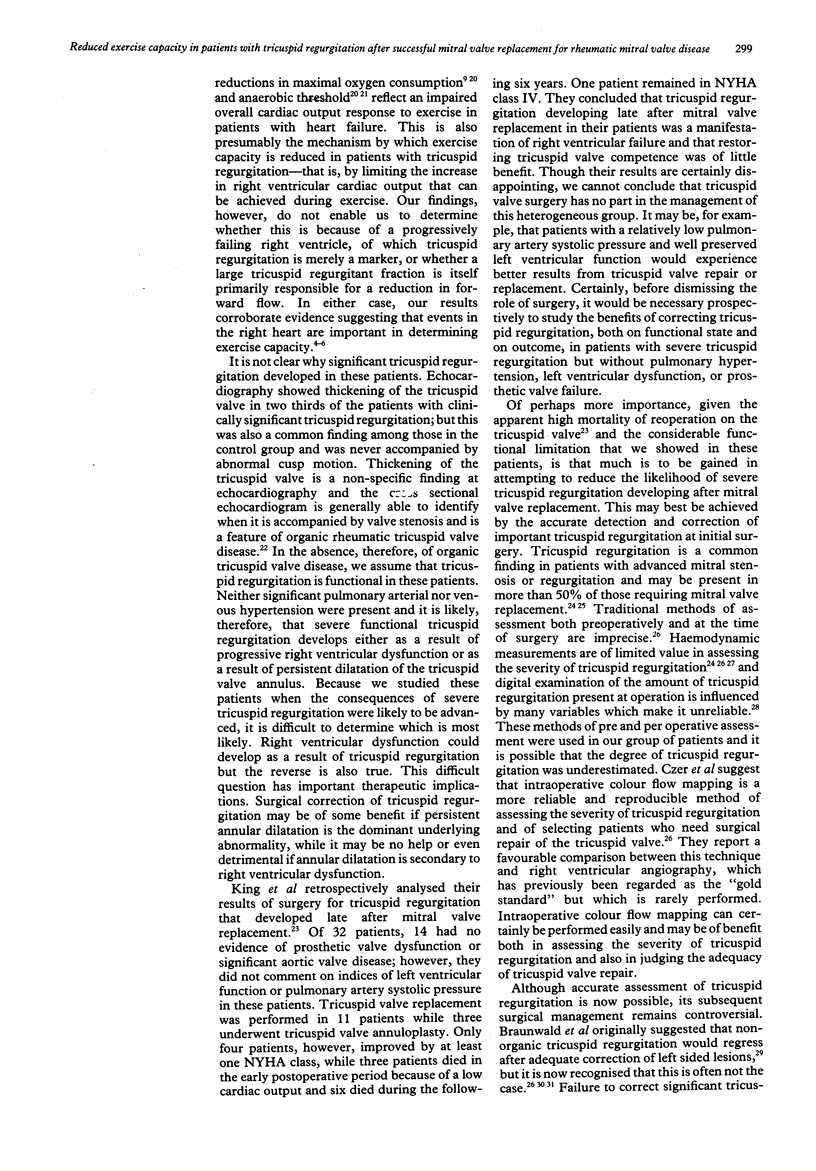
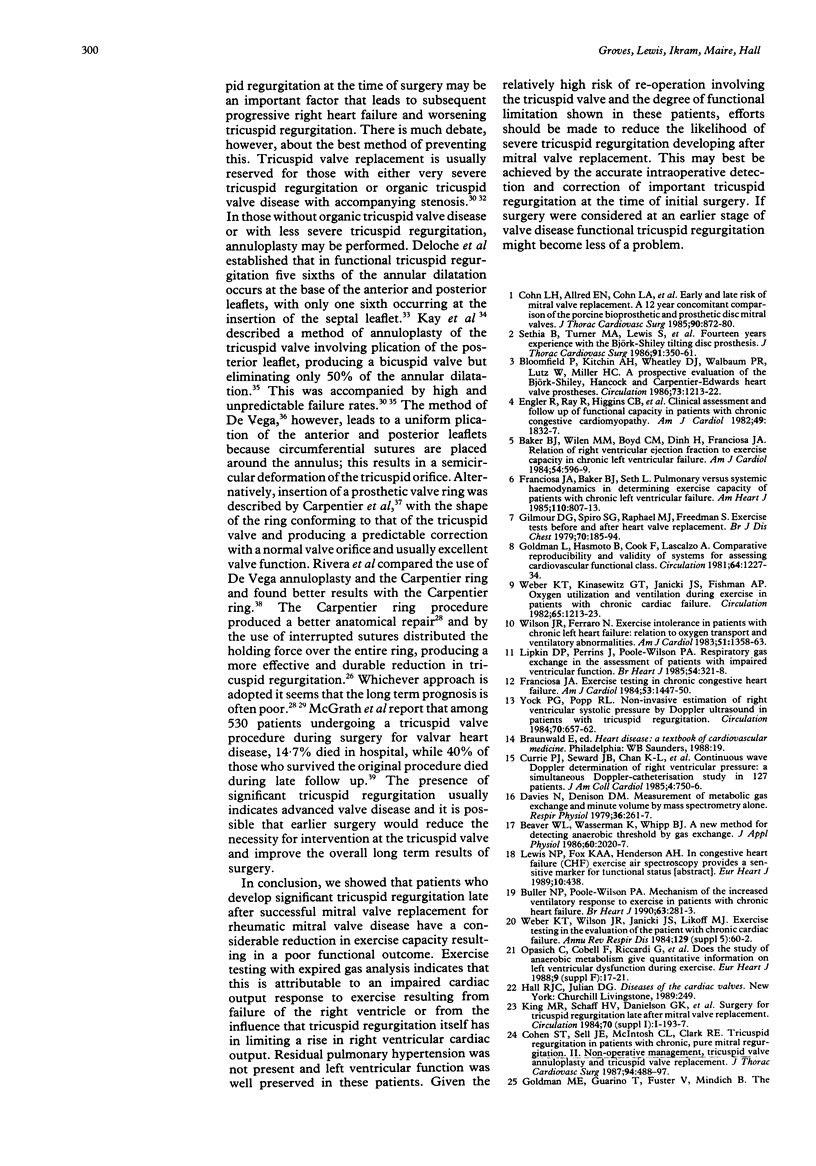
OBJECTIVE--To determine how severe tricuspid regurgitation influences exercise capacity and functional state in patients who have undergone successful mitral valve replacement for rheumatic mitral valve disease. DESIGN--9 patients in whom clinically significant tricuspid regurgitation developed late after mitral valve replacement were compared with 9 patients with no clinical evidence of tricuspid regurgitation. The two groups were matched for preoperative clinical and haemodynamic variables. Patients were assessed by conventional echocardiography, Doppler echocardiography, and a maximal treadmill exercise test in which expired gas was monitored by mass spectrometry. SETTING--University Hospital of Wales, Cardiff. SUBJECTS--18 patients who had been reviewed regularly since mitral valve replacement. MAIN OUTCOME MEASURE--Objective indices of exercise performance including exercise duration, maximal oxygen consumption, anaerobic threshold, and ventilatory response to exercise. RESULTS--Mitral valve prosthetic function was normal in all patients and estimated pulmonary artery systolic pressure and left ventricular function were similar in the two groups. Right ventricular diameter (median (range) 5.0 (4.3-5.6) v 3.7 (3.0-5.4) cm, p less than 0.01) and the incidence of paradoxical septal motion (9/9 v 3/9, p less than 0.01) were greater in the group with severe tricuspid regurgitation. Exercise performance--assessed by exercise duration (6.3 (5.0-10.7) v 12.7 (7.2-16.0) min, p less than 0.01), maximum oxygen consumption (11.2 (7.3-17.8) v 17.7 (11.8-21.4) ml min-1 kg-1, p less than 0.01), and anaerobic threshold (8.3 (4.6-11.4) v 0.7 (7.3-15.5) ml min-1 kg-1, p less than 0.05)--was significantly reduced in the group with severe tricuspid regurgitation. The ventilatory response to exercise was greater in patients with tricuspid regurgitation (minute ventilation at the same minute carbon dioxide production (41.0 (29.9-59.5) v 33.6 (26.8-39.3) l/min, p less than 0.01). CONCLUSIONS--Clinically significant tricuspid regurgitation may develop late after successful mitral valve replacement and in the absence of residual pulmonary hypertension, prosthetic dysfunction, or significant left ventricular impairment. Patients in whom severe tricuspid regurgitation developed had a considerable reduction in exercise capacity caused by an impaired cardiac output response to exercise and therefore experienced a poor functional outcome. The extent to which this was attributable to the tricuspid regurgitation itself or alternatively to the consequences of right ventricular dysfunction was not clear and requires further investigation.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baker B. J., Wilen M. M., Boyd C. M., Dinh H., Franciosa J. A. Relation of right ventricular ejection fraction to exercise capacity in chronic left ventricular failure. Am J Cardiol. 1984 Sep 1;54(6):596–599. doi: 10.1016/0002-9149(84)90256-x. [DOI] [PubMed] [Google Scholar]
- Beaver W. L., Wasserman K., Whipp B. J. A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol (1985) 1986 Jun;60(6):2020–2027. doi: 10.1152/jappl.1986.60.6.2020. [DOI] [PubMed] [Google Scholar]
- Bloomfield P., Kitchin A. H., Wheatley D. J., Walbaum P. R., Lutz W., Miller H. C. A prospective evaluation of the Björk-Shiley, Hancock, and Carpentier-Edwards heart valve prostheses. Circulation. 1986 Jun;73(6):1213–1222. doi: 10.1161/01.cir.73.6.1213. [DOI] [PubMed] [Google Scholar]
- Buller N. P., Poole-Wilson P. A. Mechanism of the increased ventilatory response to exercise in patients with chronic heart failure. Br Heart J. 1990 May;63(5):281–283. doi: 10.1136/hrt.63.5.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cairns K. B., Kloster F. E., Bristow J. D., Lees M. H., Griswold H. E. Problems in the hemodynamic diagnosis of tricuspid insufficiency. Am Heart J. 1968 Feb;75(2):173–179. doi: 10.1016/s0002-8703(68)90061-6. [DOI] [PubMed] [Google Scholar]
- Carpentier A., Deloche A., Dauptain J., Soyer R., Blondeau P., Piwnica A., Dubost C., McGoon D. C. A new reconstructive operation for correction of mitral and tricuspid insufficiency. J Thorac Cardiovasc Surg. 1971 Jan;61(1):1–13. [PubMed] [Google Scholar]
- Cohen S. R., Sell J. E., McIntosh C. L., Clark R. E. Tricuspid regurgitation in patients with acquired, chronic, pure mitral regurgitation. II. Nonoperative management, tricuspid valve annuloplasty, and tricuspid valve replacement. J Thorac Cardiovasc Surg. 1987 Oct;94(4):488–497. [PubMed] [Google Scholar]
- Cohn L. H., Allred E. N., Cohn L. A., Austin J. C., Sabik J., DiSesa V. J., Shemin R. J., Collins J. J., Jr Early and late risk of mitral valve replacement. A 12 year concomitant comparison of the porcine bioprosthetic and prosthetic disc mitral valves. J Thorac Cardiovasc Surg. 1985 Dec;90(6):872–881. [PubMed] [Google Scholar]
- Currie P. J., Seward J. B., Chan K. L., Fyfe D. A., Hagler D. J., Mair D. D., Reeder G. S., Nishimura R. A., Tajik A. J. Continuous wave Doppler determination of right ventricular pressure: a simultaneous Doppler-catheterization study in 127 patients. J Am Coll Cardiol. 1985 Oct;6(4):750–756. doi: 10.1016/s0735-1097(85)80477-0. [DOI] [PubMed] [Google Scholar]
- Czer L. S., Maurer G., Bolger A., DeRobertis M., Kleinman J., Gray R. J., Chaux A., Matloff J. M. Tricuspid valve repair. Operative and follow-up evaluation by Doppler color flow mapping. J Thorac Cardiovasc Surg. 1989 Jul;98(1):101–111. [PubMed] [Google Scholar]
- Davies N. J., Denison D. M. The measurement of metabolic gas exchange and minute volume by mass spectrometry alone. Respir Physiol. 1979 Feb;36(2):261–267. doi: 10.1016/0034-5687(79)90029-x. [DOI] [PubMed] [Google Scholar]
- De Vega N. G. La anuloplastia selectiva, regulable y permanente. Una técnica original para el tratamiento de la insuficiencia tricúspide. Rev Esp Cardiol. 1972 Nov-Dec;25(6):555–556. [PubMed] [Google Scholar]
- Deloche A., Guerinon J., Fabiani J. N., Morillo F., Caramanian M., Carpentier A., Maurice P., Dubost C. Etude anatomique des valvulopathies rhumatismales tricuspidiennes: Application à l'étude des différentes valvuloplasties. Ann Chir Thorac Cardiovasc. 1973 Oct;12(4):343–349. [PubMed] [Google Scholar]
- Duran C. M., Pomar J. L., Colman T., Figueroa A., Revuelta J. M., Ubago J. L. Is tricuspid valve repair necessary? J Thorac Cardiovasc Surg. 1980 Dec;80(6):849–860. [PubMed] [Google Scholar]
- Engler R., Ray R., Higgins C. B., McNally C., Buxton W. H., Bhargava V., Shabetai R. Clinical assessment and follow-up of functional capacity in patients with chronic congestive cardiomyopathy. Am J Cardiol. 1982 Jun;49(8):1832–1837. doi: 10.1016/0002-9149(82)90199-0. [DOI] [PubMed] [Google Scholar]
- Franciosa J. A., Baker B. J., Seth L. Pulmonary versus systemic hemodynamics in determining exercise capacity of patients with chronic left ventricular failure. Am Heart J. 1985 Oct;110(4):807–813. doi: 10.1016/0002-8703(85)90461-2. [DOI] [PubMed] [Google Scholar]
- Franciosa J. A. Exercise testing in chronic congestive heart failure. Am J Cardiol. 1984 May 15;53(10):1447–1450. doi: 10.1016/s0002-9149(84)91041-5. [DOI] [PubMed] [Google Scholar]
- Gilmour D. G., Spiro S. G., Raphael M. J., Freedman S. Exercise tests before and after heart valve replacement. Br J Dis Chest. 1976 Jul;70(3):185–194. doi: 10.1016/0007-0971(76)90028-0. [DOI] [PubMed] [Google Scholar]
- Goldman L., Hashimoto B., Cook E. F., Loscalzo A. Comparative reproducibility and validity of systems for assessing cardiovascular functional class: advantages of a new specific activity scale. Circulation. 1981 Dec;64(6):1227–1234. doi: 10.1161/01.cir.64.6.1227. [DOI] [PubMed] [Google Scholar]
- Goldman M. E., Guarino T., Fuster V., Mindich B. The necessity for tricuspid valve repair can be determined intraoperatively by two-dimensional echocardiography. J Thorac Cardiovasc Surg. 1987 Oct;94(4):542–550. [PubMed] [Google Scholar]
- Grondin P., Meere C., Limet R., Lopez-Bescos L., Delcan J. L., Rivera R. Carpentier's annulus and De Vegas annuloplasty. The end of the tricuspid challenge. J Thorac Cardiovasc Surg. 1975 Nov;70(5):852–861. [PubMed] [Google Scholar]
- KAY J. H., MASELLI-CAMPAGNA G., TSUJI K. K. SURGICAL TREATMENT OF TRICUSPID INSUFFICIENCY. Ann Surg. 1965 Jul;162:53–58. doi: 10.1097/00000658-196507000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipkin D. P., Perrins J., Poole-Wilson P. A. Respiratory gas exchange in the assessment of patients with impaired ventricular function. Br Heart J. 1985 Sep;54(3):321–328. doi: 10.1136/hrt.54.3.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath L. B., Gonzalez-Lavin L., Bailey B. M., Grunkemeier G. L., Fernandez J., Laub G. W. Tricuspid valve operations in 530 patients. Twenty-five-year assessment of early and late phase events. J Thorac Cardiovasc Surg. 1990 Jan;99(1):124–133. [PubMed] [Google Scholar]
- Mullany C. J., Gersh B. J., Orszulak T. A., Schaff H. V., Puga F. J., Ilstrup D. M., Pluth J. R., Danielson G. K. Repair of tricuspid valve insufficiency in patients undergoing double (aortic and mitral) valve replacement. Perioperative mortality and long-term (1 to 20 years) follow-up in 109 patients. J Thorac Cardiovasc Surg. 1987 Nov;94(5):740–748. [PubMed] [Google Scholar]
- Opasich C., Cobelli F., Riccardi G., La Rovere M. T., Calsamiglia G., Specchia G. Does the study of anaerobic metabolism give quantitative information on left ventricular dysfunction during exercise? Eur Heart J. 1988 Apr;9 (Suppl F):17–21. doi: 10.1093/eurheartj/9.suppl_f.17. [DOI] [PubMed] [Google Scholar]
- Pritchett E. L., Smith M. S., McCarthy E. A., Lee K. L. The spontaneous occurrence of paroxysmal supraventricular tachycardia. Circulation. 1984 Jul;70(1):1–6. doi: 10.1161/01.cir.70.1.1. [DOI] [PubMed] [Google Scholar]
- Rivera R., Duran E., Ajuria M. Carpentier's flexible ring versus De Vega's annuloplasty. A prospective randomized study. J Thorac Cardiovasc Surg. 1985 Feb;89(2):196–203. [PubMed] [Google Scholar]
- Sethia B., Turner M. A., Lewis S., Rodger R. A., Bain W. H. Fourteen years' experience with the Björk-Shiley tilting disc prosthesis. J Thorac Cardiovasc Surg. 1986 Mar;91(3):350–361. [PubMed] [Google Scholar]
- Weber K. T., Kinasewitz G. T., Janicki J. S., Fishman A. P. Oxygen utilization and ventilation during exercise in patients with chronic cardiac failure. Circulation. 1982 Jun;65(6):1213–1223. doi: 10.1161/01.cir.65.6.1213. [DOI] [PubMed] [Google Scholar]
- Wilson J. R., Ferraro N. Exercise intolerance in patients with chronic left heart failure: relation to oxygen transport and ventilatory abnormalities. Am J Cardiol. 1983 May 1;51(8):1358–1363. doi: 10.1016/0002-9149(83)90312-0. [DOI] [PubMed] [Google Scholar]
- Yock P. G., Popp R. L. Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation. 1984 Oct;70(4):657–662. doi: 10.1161/01.cir.70.4.657. [DOI] [PubMed] [Google Scholar]