Abstract
Background
Previous studies have suggested links between anxiety response to the novel coronavirus (COVID-19) and depression symptoms in general population. However, a symptom-level investigation has not been reported.
Objective
This study aimed to use network analysis to identify central symptoms and bridge symptoms that link COVID-19 anxiety and depression.
Methods
Data from 1788 participants were analyzed. Coronavirus anxiety and depression symptoms were measured using the Stress and Anxiety to Viral Epidemics-6 Items Scale and the Patient Health Questionnaire-9, respectively. Network analysis was performed using R.
Results
The results revealed ‘thoughts of suicide or self-harm’ from Patient Health Questionnaire-9 and ‘worry about others avoiding me’ from Stress and Anxiety to Viral Epidemics-6 Items Scale as bridge symptoms. Findings suggest direct relationship between fear of social isolation and thoughts of suicide or self-harm. ‘Feeling tired with little energy’ and ‘trouble concentrating’ are strongly linked to ‘thoughts of suicide or self-harm’, suggesting these symptoms as risk factors for suicidal or self-injurious thoughts during the pandemic.
Conclusions
The findings suggest fear of social isolation as a risk factor for developing thoughts of suicide or self-harm. These results should be taken into account during evaluation of risk of suicide or mental health interventions for the pandemic.
Key words: COVID-19, anxiety, depression, network analysis, suicidal thoughts, social isolation
Introduction
The novel coronavirus (COVID-19) began to spread in early 2020, causing numerous public health issues, among which includes mental health problems. Aside from COVID-19, worsening of psychological health has also been reported from previous epidemics such as the Middle East respiratory syndrome and severe acute respiratory syndrome.1 , 2 Commonly reported psychological responses to COVID-19 and its spread include depression, anxiety, phobia, and insomnia.3 A meta-analysis reported the prevalence of anxiety and depression during the COVID-19 pandemic to be 31.9 and 33.7%, respectively.4 Increased development of psychological symptoms during virus outbreak were reported in a variety of population, including children and adolescents,5 elderly,6 and healthcare workers.7 Among various psychological consequence of the viral epidemic, depression carries important clinical significances. It is one of the leading causes of disability and increases risk of developing chronic medical illnesses such as diabetes, hypertension, and cerebrovascular diseases.8 Depression is also associated with worse status of overall health when comorbid with chronic diseases9 and poorer quality of life in patients with chronic diseases.10 More importantly, it has been consistently reported that depression increases mortality in the general population and clinical samples.11 , 12
Research has identified various factors that cause an increase in depression symptoms during viral pandemic. Gender, marital status, financial worries, and personality traits have been reported as an individual factor.13, 14, 15 Others directly related to the disease include worries about stigmatization, infection, isolation, and job security.14 Numerous studies have reported the link between depression and anxiety about the viral pandemic on a general level. For example, one study has revealed a significant association between worry about COVID-19 and psychological distress, including anxiety and depression.16 Another study has revealed positive correlations of trait health anxiety with anxiety and depression.17 However, despite various reports, no study has investigated how pandemic-related worries and depression are associated at a symptom level. Examining the symptom-level association helps clarify their link, providing insight into how pandemic-related worries cause depression. Furthermore, it also allows us to identify target symptoms of effective psychological intervention for preventing development of clinical depression.
Network analysis is a novel statistical analysis method that is currently widely used to analyze psychiatric disorders and their symptoms and is a suitable method for analysis of symptom interactions. Network analysis provides rich information regarding the extent of effect exerted by certain symptoms within the network. Node centrality indices, for example, enable identification of significant symptoms with respect to their statistical characteristics. Centrality indices include strength, closeness, and betweenness. Strength centrality identifies how strongly a node is related to its adjacent nodes; closeness centrality identifies a node's average distance to other nodes; and betweenness centrality identifies how frequently a node lies on the connection between two nodes.18 Centrality indices are unique tools that can be used to support interpretation of the resulting network. Centrality indices are distinctive indices that can make network analysis a valuable tool even in clinical practice. For example, one study has successfully developed and implemented personalized network-based treatments based on the most central features present in one's eating disorder.19 Therefore, network analysis can offer valuable insights that otherwise cannot be obtained using methods such as linear regression.
In addition, using network analysis, recent literature has enabled the identification of symptoms that bridge different groups of symptoms. For example, certain depression symptoms may have stronger connections with COVID-19-related worries than others and can be identified as bridge symptoms. Similar to centrality indices, bridge nodes can be characterized using bridge centrality.20 Bridge centrality, coined by Jones et al. (2021), is defined in the same regard as node centrality but within a context of symptom group. Bridge centrality is particularly effective in comorbidity research investigating specific symptoms that play a central role in the intertwining of symptom communities. Identification of bridge centrality helps identify symptoms that are particularly more influential than others within a network and helps provide a nuanced understanding. As such, bridge symptoms may help provide insight into underlying mechanisms and contribute to development of theories and interventions.
The purpose of this study is to employ network analysis and bridge analysis to investigate the network structure and bridge symptoms of depression and COVID-19-related worries. This will provide insight into how depression symptoms and COVID-19 worries are related on a symptom level, detailing how specific symptoms are involved in the intertwinement. Based on previous studies, we hypothesized that overall, significant correlations between worry about COVID-19 and depression symptoms would emerge,16 , 17 with items linked to social stigmatization and isolation (e.g., “worry about others avoiding me”) to have a high bridge centrality values.14
Materials and Methods
Study Design and Participants
This is a prospective study using an online survey that was conducted to explore the association between viral anxiety and depression in COVID-19 among the general population in South Korea. It was conducted via an anonymous online survey system of the professional research company, EMBRAIN (www.embrain.com). We collected 1009 (study 1 from January 14–20, 2021), 400 (study 2 from November 9–15, 2021), and 400 (study 3 from January 10–18, 2022) participants (total 1809) from the 14 million general population panels registered in the survey company. Participants voluntarily participated in this study by answering yes to the question, “Do you voluntarily participate in this survey, and do you agree to use your responses for research purpose?” before they started the survey. Twenty-one participants who indicated that they had been infected with COVID-19 were excluded from the analysis to improve homogeneity of participants and generalizability of the results to an uninfected general population. As a result, data from 1788 participants were used for analysis. All participants completed the Stress and Anxiety to Viral Epidemics-6 Items Scale (SAVE-6) and Patient Health Questionnaire-9 (PHQ-9). The e-survey forms were developed according to the Checklist for Reporting Results of Internet e-Surveys guidelines,21 and investigators (S.C. and S.S.) checked usability and technical functionality of the e-surveys before implementation. The survey company delivered the data to investigators after excluding identifiable information.
The protocols of the studies were approved by the Institutional Review Board of Sungshin Women's University, Seoul, South Korea (study 1: SSWUIRB-2020-040) and Asan Medical Center, Seoul, South Korea (study 2: 2021–1490, study 3: 2021–1755), and obtaining written informed consent was waived. Finally, the protocol for analyzing the data combined of three dataset was approved by the Institutional Review Board of Asan Medical Center (S2022-0741).
Measures
The Stress and Anxiety to Viral Epidemics-6 Items Scale (SAVE-6)
The SAVE-6 scale is a self-report scale consisting of six items that measure anxiety about viral epidemics. It is derived from the SAVE-9 scale, which includes anxiety about viral epidemic as well as additional three items measuring work-related stress among healthcare workers about the viral epidemic.22 All items are rated on a five-point Likert scale, ranging from 0 (never) to 4 (always). Higher scores indicate higher anxiety experienced due to viral epidemic. The SAVE-6 scale has been validated on the general population in many countries, showing good internal consistencies.22, 23, 24, 25 The internal consistency from the current study was 0.82.
Patient Health Questionnaire-9 (PHQ-9)
The PHQ-9 scale measures levels of depression based on individual symptoms. It consists of nine items, each measuring a symptom of depression, such as loss of interest and suicidal thoughts. Each item is rated on a 4-point Likert scale, ranging from 0 (not at all) to 3 (nearly every day). Higher scores reflect higher symptom severity. This study used a Korean-validated version of the PHQ-9, where its internal consistency was reported to be 0.86.26 The internal consistency from the current study was 0.89.
Statistical Analysis
Network Estimation
Basic descriptive statistics such as gender ratio, means and standard deviations of age, SAVE-6, and PHQ-9 were calculated using IBM SPSS Statistics for Windows, Version 27.0 (IBM Corp, Armonk, N.Y., USA).
Network analysis was conducted using the qgraph package in R.27 Each item, corresponding to a single symptom, was regarded as a node in the network. As a result, the network contained 15 total nodes. As each symptom was rated on an ordinal scale, polychoric correlations between item ratings were computed as edges to construct the network. Partial correlation coefficients near 0 were excluded from the network using the graphic least absolute shrinkage and selection operator estimator.
Centrality indices of strength, closeness, and betweenness were calculated for each node. To assess the stability, correlation stability coefficients (CS-coefficients) were calculated for each centrality index using bootstrap methods implemented by bootnet package.28 The CS-coefficient is obtained by first calculating correlations between the original centrality index value and centrality index of subsets obtained via bootstrapping. Then, given a condition where this correlation is 0.7 or higher, CS-coefficient is the maximum proportion of samples that can be dropped to retain the correlation at a 95% probability. A simulation study suggests that interpretation of the centrality index should be done for CS-coefficients at least above 0.25.28 In addition, each edge was bootstrapped with 1000 samples to determine their accuracies. Bootstrapped difference tests were performed to compare each edge weight against others. Significant differences would indicate the edge weight of the particular is significantly stronger than others. These results were summarized into a single figure using the plot function to provide an overall image reference as to which edge weight significantly differs from the other.
Bridge Centrality
Bridge centrality indices, bridge strength, bridge closeness, and bridge betweenness were computed using the bridge function from the package, networktools.20 , 29 Bridge strength of a node is defined as the sum of its connections to adjacent nodes in another symptom group. For this study, the bridge strength of a depression symptom is the sum of its connections to nodes of COVID-19-related worries. Bridge closeness is the average distance of a node to nodes in another symptom group. For this study, bridge closeness of a depression symptom is its average distance to nodes of COVID-19-related worries. Bridge betweenness is how frequently a node lies on the shortest path between two nodes, where each of these two nodes are from different symptom groups (i.e., depression symptoms and COVID-19-related worries).20 Similar to centrality indices, their CS-coefficients were calculated using bootnet to determine their interpretability.
Results
Descriptive Statistics
Gender proportions, means, and standard deviations of age, SAVE-6, and PHQ-9 are listed in Table 1 . There were similar number of men and women and the mean age was 43.84 years. The mean score of SAVE-6 and PHQ-9 were 14.62 and 5.92, respectively.
Table 1.
Descriptive Information of Gender, Age, COVID-19 Questions, SAVE-6, and PHQ-9 of the Sample (N = 1788)
| Variable | Value |
|---|---|
| Gender | |
| Males (%) | 911 (51.0%) |
| Females (%) | 877 (49.0%) |
| Mean age (SD) | 43.84 (12.90) |
| Below 20 (%) | 11 (0.6%) |
| 20 to 29 (%) | 330 (18.5%) |
| 30 to 39 (%) | 341 (19.1%) |
| 40 to 49 (%) | 415 (23.2%) |
| Above 50 (%) | 691 (38.6%) |
| COVID-19 questions | |
| Did you experience being quarantined for having been infected with COVID-19? (Yes) | 178 (10.0%) |
| SAVE-6 mean (SD) | 14.62 (4.54) |
| PHQ-9 mean (SD) | 5.92 (5.25) |
SD = standard deviation.
Network Estimation
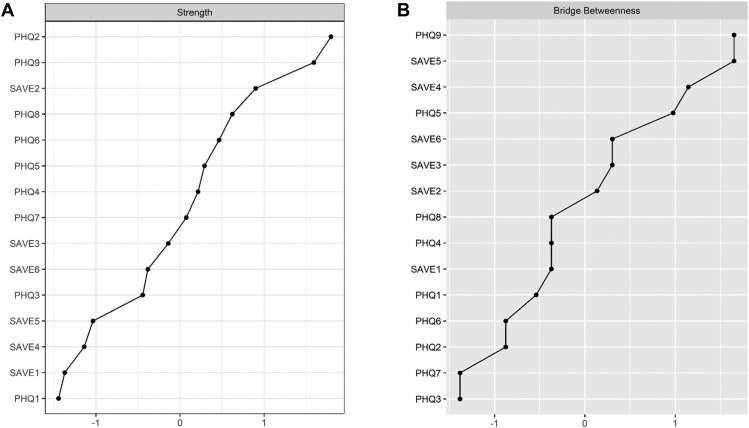
The overall network consisting of SAVE-6 and PHQ-9 items is illustrated in Figure 1 . CS-coefficients for centralities of strength, closeness, and betweenness were 0.67, 0.13, and 0.05, respectively. As such, only strength centrality, a measure of how strong a node is associated with its adjacent nodes, was interpreted.28 Figure 2 A depicts strength of each node. In particular, PHQ2, PHQ9, and SAVE2 had the largest strength values among others. In addition, the results for bootstrapped difference tests for edges are illustrated in Figure 3 . As can be seen, most edges connecting nodes within the same scale are significantly different from others. Some of the first few edges are PHQ1—PHQ2, SAVE1—SAVE2, PHQ8—PHQ9, and PHQ3—PHQ4, visible via an abundant number of black-colored squares, indicating a significant difference between the edge in comparison. Of note, the first interscale edge that appears to be significantly stronger than others is SAVE5—PHQ9.
Figure 1.
Estimated Network of SAVE-6 and PHQ-9. Orange nodes indicate SAVE-6 items, and blue nodes indicate PHQ-9 items. Lines connecting the nodes are edges. Line thickness and gradient correspond to edge-weights. Green lines indicate positive correlations, and red lines indicate negative correlations.
Figure 2.
Strength and Bridge Betweenness Centralities of SAVE-6 and PHQ-9 items. (A) illustrates values for strength centrality, and (B) illustrates bridge betweenness centrality. Items are listed in a descending order from top to bottom, from nodes with largest centrality value to smallest centrality value. All values are standardized
Figure 3.
Results for Bootstrapped Difference Tests of First 32 Edges, Ordered by Weight. Black boxes indicate edges that significantly differ from the other, and gray boxes indicate otherwise. Diagonal boxes indicate strength and direction of the focal edge. Blue boxes are positive, while red boxes are negative. Edges are listed in a descending order from positive to negative values. For ease of understanding, only the first 32 edges are listed. The full figure can be accessed via Supplementary Material 1
Bridge Centrality
As for bridge centralities, only bridge betweenness reached an appropriate CS-coefficient value of 0.28. As such, only bridge-betweenness was interpreted. Bridge betweenness is an index of how frequently a node appears in an intercommunity link from one node to another,20 and a symptom with high bridge betweenness index is considered crucial when explaining the link from one symptom community to another. Figure 2B shows that two items, item 9 from PHQ-9 (PHQ9) and item 5 from SAVE-6 (SAVE5), had the largest bridge betweenness. This indicates that when two nodes from different symptom communities are connected, PHQ9 or SAVE5 occur the most within the connections.
Discussion
This study employed network analysis on depression symptoms and COVID-19 worries measured by PHQ-9 and SAVE-6 in an uninfected general population. Bridge symptoms were identified using bridge analysis. The main results are as follows. First, ‘thoughts of suicide or self-harm’ (PHQ9) had highest bridge betweenness value, suggesting that this symptom is a central symptom in the relationship between COVID-19-related worries and depression symptoms. Similarly, ‘worry about others avoiding me after risk of infection has been minimized’ (SAVE5) also had a high bridge betweenness value. In addition, the edge connecting PHQ9 and SAVE5 had the strongest edge weight among intercommunity edges. Finally, high strength centralities were observed for PHQ-9 items, where ‘thoughts of suicide or self-harm’ were strongly linked to ‘feeling tired with little energy’ (PHQ6) and ‘trouble concentrating’ (PHQ8). Some implications about the current pandemic situation and psychopathology are discussed.
A main finding of this study is high bridge betweenness of ‘thoughts of suicide/self-harm’. High bridge betweenness indicates that thoughts of suicide/self-harm play significant role in funneling depression symptoms from COVID-related worries. This result is in line with studies reporting associations between COVID-19 pandemic and increased risk of thoughts of suicide/self-harm.30 , 31 Such association was also observed in previous cases of epidemics. For example, increased suicide rates have been observed during post–severe acute respiratory syndrome and post–Middle East respiratory syndrome period.32 , 33 It is also notable that aside other major symptoms of depression such as ‘feeling down, depressed, and hopeless’ (PHQ1), and ‘loss of interest’ (PHQ2), suicidal/self-injurious thoughts were revealed as the bridge symptom to COVID-19 worries. Together, these results imply that instead of having severe depression symptoms as mediators, thoughts of suicide/self-harm may be a direct psychological response to the pandemic. This emphasizes the need to examine the mechanism of how COVID-19-related worries may affect thoughts of suicide/self-harm. For example, suicidal thoughts can be directly derived from the fear of consequence of viral infection, which can be exaggerated by inadequate health information. It has also been reported that some individuals have shown suicidal thoughts from experiencing fear from insecurity caused by the pandemic, or being forced to stay home with problematic family issues.34 Longitudinal studies may be helpful to examine the detailed mechanism of how COVID-19 worries may lead to thoughts about suicide/self-harm. However, it should also be noted that there is a possibility that individuals who exhibit thoughts of suicide/self-harm due to severe depression may also be more susceptible to experiencing more COVID-19-related worries, thus leading to high bridge-betweenness. To this end, research may be conducted on how the impact of pandemic or epidemic may differ on individuals with mental disorders and healthy individuals.
In addition, ‘worry about others avoiding me after risk of infection has been minimized’ (SAVE5) also emerged as a node with high bridge betweenness. Prior to interpretation, it is important to note that this item connotes fear for continuation of social isolation even after the pandemic has been controlled. It is interesting that this node showed increased association with depression symptoms rather than those directly associated with one's health, such as fear of infection or loss of health. This is in contrast with a study using clinical sample, where health worries were associated with psychopathology symptoms.35 However, in our sample of uninfected general population, health worry ‘afraid of worsening health because of virus’ (SAVE2) was a central symptom only within the SAVE-6 community, as evidenced by its high strength centrality and edge-weights (Figure 3). Instead, social worry (SAVE5) emerged as a bridge symptom with depression symptoms. This result is significant, because it suggests that in an uninfected population, fear of social isolation, regardless of the pandemic being under control, can contribute to increased thoughts of suicide/self-harm as well as other depression symptoms. To this regard, recent studies have reported that loneliness and isolation caused by COVID-19-related restrictions are linked to thoughts of suicide/self-harm.30 , 36 This adds to the growing body of studies on risk factors for suicidal/self-injurious thoughts as a result of pandemic measures. Understanding the COVID-19-related risk factors of suicide and self-harm may facilitate setting intervention targets for those with declined mental health during pandemic times. Our result suggests that fear of social isolation is a serious issue that needs to be addressed, especially for population at risk, such as financially strained individuals.30 In addition, these findings can be utilized to help develop strategies to prevent disease transmission while reducing social isolation during future outbreaks of another epidemic or pandemic. One possible example could be to establish online social supports to help individuals in home quarantine feel less socially isolated.37 To this regard, future studies could assess whether providing social support services or encouragement of online communication during isolation results in decrease in depression incidence.
Thoughts of suicide/self-harm appeared to play a significant role within the depression symptom community. This can be inferred by its high strength due to strong links between other depression symptoms illustrated in Figure 3, such as ‘trouble concentrating’ (PHQ8) and ‘feeling tired with little energy’ (PHQ6). It should be noted that previous studies have reported core symptoms of depression, such as ‘feeling down, depressed, and hopeless’ (PHQ1), and ‘loss of interest’ (PHQ2) to be predictors of suicidal thoughts,38 , 39 which differs with our results. The difference can be attributed to the target sample of the studies, as this study sampled general population, whereas the aforementioned studies were conducted on clinically depressed samples. It could also possibly be because of the added COVID-19 context. Indeed, one study reported energy loss to be a central depression symptom in the general population during COVID-19 pandemic, which supports our findings.40 In addition, functional impairments (e.g., work functioning impairment) caused by COVID-19 anxiety may also contribute to lack of energy and concentration difficulties.41 These results suggest ‘feeling tired with little energy’, and ‘trouble concentrating’ are risk factors to be considered when evaluating suicidal/self-injurious thoughts during the pandemic.
The limitations of this study are as follows. First, this study employed a nondirected network on cross-sectional data. Therefore, associations between nodes can be bidirectional, which widens possible number of interpretations. To address this issue, directed networks can be constructed using longitudinal data in future studies to determine the causal direction of symptoms. Second, this study was conducted on Korean participants, limiting generalizability of results in other countries with different cultural backgrounds. Collectivistic cultures tend to value belongingness, which could have possibly contributed to the result linking ‘worry about others avoiding me’ and depression symptoms. Third, it should be noted that our network showed an overall modest link between depression symptoms and COVID-19-related worries. This may be because our study was not conducted on a clinical sample. To this end, future studies may yield meaningful results when conducted on a clinically depressed sample. In addition, it should be emphasized that the results should be accepted with caution, as the methodology of using psychometric networks have yet been rigorously tested to support its robustness and reliability.42 Finally, while COVID-19 tests were performed rigorously, it should be noted that there is a possibility of asymptomatic COVID-19 infections among some participants. As research has suggested evidence of physiologically produced mood symptoms due to COVID-19 such as depression,43 the possibility that undetected COVID-19 may have influenced reports of depression symptoms among the participants should be considered.
Conclusion
Despite the limitations, the findings from this study are significant for the following reasons. We revealed that suicidal/self-injurious thoughts and fear of social isolation bridged depression symptoms and COVID-19-related worries in an uninfected general population. These results encourage investigation of how COVID-19-related worries may affect thoughts of suicide/self-harm. In addition, it also highlights the significance of fear of social isolation as a risk factor for depression symptoms in a nonclinical population. Next, risk factors for suicidal/self-injurious thoughts during the current pandemic situation were identified. In sum, our findings contribute to expansion of understanding risk factors associated with thoughts of suicide/self-harm during the pandemic. The results suggest that fear of social isolation should be thoroughly considered when evaluating mental health, even after COVID-19 risk has been minimized.
Footnotes
Ethical Publication Statement: The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Funding: This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Data Availability: The data that support findings of this study are available upon request from the corresponding authors.
Supplementary data related to this article can be found at 10.1016/j.jaclp.2023.06.002.
Supplementary data
Supplementary Figure 1.
References
- 1.Lee D., Lee J.H., Jeon K., Lee N., Sim M. Psychological responses among Korean middle east respiratory syndrome survivors and bereaved families. Disaster Med Public Health Prep. 2022;16:1077–1082. doi: 10.1017/dmp.2021.32. [DOI] [PubMed] [Google Scholar]
- 2.Khan S., Siddique R., Xiaoyan W., et al. Mental health consequences of infections by coronaviruses including severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Brain and Behavior. 2021;11 doi: 10.1002/brb3.1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salari N., Hosseinian-Far A., Jalali R., et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. 2020;16:57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Miranda D.M., Athanasio B.D., Oliveira A.C.S., Simoes-e-Silva A.C. How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disast Risk Re. 2020;51 doi: 10.1016/j.ijdrr.2020.101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yildirim H., Isik K., Aylaz R. The effect of anxiety levels of elderly people in quarantine on depression during covid-19 pandemic. Soc Work Public Hlth. 2021;36:194–204. doi: 10.1080/19371918.2020.1868372. [DOI] [PubMed] [Google Scholar]
- 7.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vos T., Barber R.M., Bell B., et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moussavi S., Chatterji S., Verdes E., Tandon A., Patel V., Ustun B. Depression, chronic diseases, and decrements in health: results from the world health surveys. Lancet. 2007;370:851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 10.Gallegos-Carrillo K., García-Peña C., Mudgal J., Romero X., Durán-Arenas L., Salmerón J. Role of depressive symptoms and comorbid chronic disease on health-related quality of life among community-dwelling older adults. J Psychosom Res. 2009;66:127–135. doi: 10.1016/j.jpsychores.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Cuijpers P., Vogelzangs N., Twisk J., Kleiboer A., Li J., Penninx B.W. Comprehensive meta-analysis of excess mortality in depression in the general community versus patients with specific illnesses. Am J Psychiatr. 2014;171:453–462. doi: 10.1176/appi.ajp.2013.13030325. [DOI] [PubMed] [Google Scholar]
- 12.Walker E.R., McGee R.E., Druss B.G. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatr. 2015;72:334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nikcevic A.V., Marino C., Kolubinski D.C., Leach D., Spada M.M. Modelling the contribution of the big five personality traits, health anxiety, and COVID-19 psychological distress to generalised anxiety and depressive symptoms during the COVID-19 pandemic. J Affect Disorders. 2021;279:578–584. doi: 10.1016/j.jad.2020.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McPherson K.E., McAloney-Kocaman K., McGlinchey E., Faeth P., Armour C. Longitudinal analysis of the UK COVID-19 Psychological wellbeing study: trajectories of anxiety, depression and COVID-19-related stress symptomology. Psychiat Res. 2021;304 doi: 10.1016/j.psychres.2021.114138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCracken L.M., Badinlou F., Buhrman M., Brocki K.C. Psychological impact of COVID-19 in the Swedish population: depression, anxiety, and insomnia and their associations to risk and vulnerability factors. Eur Psychiat. 2020;63:e81. doi: 10.1192/j.eurpsy.2020.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kibbey M.M., Fedorenko E.J., Farris S.G. Anxiety, depression, and health anxiety in undergraduate students living in initial US outbreak "hotspot" during COVID-19 pandemic. Cogn Behav Ther. 2021;50:409–421. doi: 10.1080/16506073.2020.1853805. [DOI] [PubMed] [Google Scholar]
- 17.Landi G., Pakenham K.I., Boccolini G., Grandi S., Tossani E. Health anxiety and mental health outcome during COVID-19 lockdown in Italy: the mediating and moderating roles of psychological flexibility. Front Psychol. 2020;11:2195. doi: 10.3389/fpsyg.2020.02195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McNally R.J. Can network analysis transform psychopathology? Behav Res Ther. 2016;86:95–104. doi: 10.1016/j.brat.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 19.Levinson C.A., Williams B.M., Christian C., et al. Personalizing eating disorder treatment using idiographic models: an open series trial. J Consult Clin Psychol. 2023;91:14–28. doi: 10.1037/ccp0000785. [DOI] [PubMed] [Google Scholar]
- 20.Jones P.J., Ma R.F., McNally R.J. Bridge centrality: a network APPROACH TO UNDERSTANDing comorbidity. Multivar Behav Res. 2021;56:353–367. doi: 10.1080/00273171.2019.1614898. [DOI] [PubMed] [Google Scholar]
- 21.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of Internet e-surveys (CHERRIES) J Med Internet Res. 2004;6:12–16. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chung S., Ahn M.H., Lee S., Kang S., Suh S., Shin Y.W. The stress and anxiety to viral epidemics-6 items (SAVE-6) scale: a New Instrument for assessing the anxiety response of general population to the viral epidemic during the COVID-19 pandemic. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.669606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Okajima I., Chung S., Suh S. Validation of the Japanese version of Stress and Anxiety to Viral Epidemics-9 (SAVE-9) and relationship among stress, insomnia, anxiety, and depression in healthcare workers exposed to coronavirus disease 2019. Sleep Med. 2021;84:397–402. doi: 10.1016/j.sleep.2021.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moraleda-Cibrian M., Ahmed O., Albares-Tendero J., Chung S. Validity and reliability of the stress and anxiety to viral epidemics-6 (SAVE-6) scale to measure viral anxiety of healthcare workers in Spain during the COVID-19 pandemic. Front Psychiatry. 2022;12 doi: 10.3389/fpsyt.2021.796225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahmed O., Hossain K.N., Hiramoni F.A., Siddique R.F., Chung S. Psychometric properties of the Bangla version of the stress and anxiety to viral epidemics-6 items scale among the general population in Bangladesh. Front Psychiatry. 2022;13 doi: 10.3389/fpsyt.2022.804162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Han C.S., Jo S.A., Kwak J.H., et al. Validation of the patient health questionnaire-9 Korean version in the elderly population: the ansan geriatric study. Compr Psychiat. 2008;49:218–223. doi: 10.1016/j.comppsych.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 27.Epskamp S., Cramer A.O.J., Waldorp L.J., Schmittmann V.D., Borsboom D. Qgraph: network visualizations of relationships in psychometric data. J Stat Softw. 2012;48:1–18. [Google Scholar]
- 28.Epskamp S., Borsboom D., Fried E.I. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. 2018;50:195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jones P.J., Mair P., Riemann B.C., Mugno B.L., McNally R.J. A network perspective on comorbid depression in adolescents with obsessive-compulsive disorder. J Anxiety Disord. 2018;53:1–8. doi: 10.1016/j.janxdis.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 30.Elbogen E.B., Lanier M., Blakey S.M., Wagner H.R., Tsai J. Suicidal ideation and thoughts of self-harm during the COVID-19 pandemic: the role of COVID-19-related stress, social isolation, and financial strain. Depress Anxiety. 2021;38:739–748. doi: 10.1002/da.23162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hawton K., Lascelles K., Brand F., et al. Self-harm and the COVID-19 pandemic: a study of factors contributing to self-harm during lockdown restrictions. J Psychiatr Res. 2021;137:437–443. doi: 10.1016/j.jpsychires.2021.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ahn S.H., Kim J.L., Kim J.R., et al. Association between chronic fatigue syndrome and suicidality among survivors of Middle East respiratory syndrome over a 2-year follow-up period. J Psychiatr Res. 2021;137:1–6. doi: 10.1016/j.jpsychires.2021.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cheung Y.T., Chau P.H., Yip P.S.F. A revisit on older adults suicides and severe acute respiratory syndrome (SARS) epidemic in Hong Kong. Int J Geriatr Psych. 2008;23:1231–1238. doi: 10.1002/gps.2056. [DOI] [PubMed] [Google Scholar]
- 34.Son C., Hegde S., Smith A., Wang X.M., Sasangohao F. Effects of COVID-19 on College students' mental health in the United States: interview survey study. J Med Internet Res. 2020;22 doi: 10.2196/21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim S.T., Seo J.H., Lee S., et al. Dysfunctional coronavirus anxiety in nonpsychotic psychiatric outpatients during the COVID-19 pandemic: A network analysis. Depress Anxiety. 2022;39:556–563. doi: 10.1002/da.23256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fortgang R.G., Wang S.B., Millner A.J., et al. Increase in suicidal Thinking during COVID-19. Clin Psychol Sci. 2021;9:482–488. doi: 10.1177/2167702621993857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hwang T.J., Rabheru K., Peisah C., Reichman W., Ikeda M. Loneliness and social isolation during the COVID-19 pandemic. Int Psychogeriatr. 2020;32:1217–1220. doi: 10.1017/S1041610220000988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schneider B., Philipp M., Muller M.J. Psychopathological predictors of suicide in patients with major depression during a 5-year follow-up. Eur Psychiat. 2001;16:283–288. doi: 10.1016/s0924-9338(01)00579-x. [DOI] [PubMed] [Google Scholar]
- 39.Takeuchi T., Nakao M. The relationship between suicidal ideation and symptoms of depression in Japanese workers: a cross-sectional study. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-003643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cheung T., Jin Y., Lam S., et al. Network analysis of depressive symptoms in Hong Kong residents during the COVID-19 pandemic. Transl Psychiat. 2021;11 doi: 10.1038/s41398-021-01543-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gallagher M.W., Zvolensky M.J., Long L.J., Rogers A.H., Garey L. The impact of covid-19 experiences and associated stress on anxiety, depression, and functional impairment in American adults. Cognitive Ther Res. 2020;44:1043–1051. doi: 10.1007/s10608-020-10143-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Neal Z.P., Forbes M.K., Neal J.W., et al. Critiques of network analysis of multivariate data in psychological science. Nat Rev Method Primers. 2022 [Google Scholar]
- 43.Troyer E.A., Kohn J.N., Hong S.Z. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020;87:34–39. doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]