Abstract
Despite emerging evidence that food insecurity (FI) is associated with elevated rates of eating pathology, little is known about the lasting impact of FI on eating behaviors. Studies that have explored the association between FI during childhood and eating behavior in adulthood have not accounted for current FI. The present study explored differences in disordered eating (DE) and related appetitive traits among four groups of cisgender female mothers: individuals who (1) endorsed childhood FI only (n=96), (2) endorsed current FI only (n=134), (3) endorsed both childhood and current FI (n=257), and (4) denied both childhood and current FI (n=146). Participants responded to online questionnaires including items from the USDA Household Food Security Survey Module, the 7-item Eating Disorder Examination-Questionnaire, the Eating Disorder Diagnostic Scale, and the Adult Eating Behavior Questionnaire. Adjusting for age and race/ethnicity, ANCOVAs explored mean differences between groups in DE and appetitive traits, and a modified Poisson regression model examined differences in binge-eating prevalence across the four FI groups. The “current FI only” group consistently endorsed the highest levels of DE and related appetitive traits followed by the “current and childhood FI” group, suggesting newly food-insecure women may be at highest risk for DE. Interestingly, across almost all constructs, the “childhood FI only” group did not differ significantly from the “no FI” group. These findings suggest that improved access to food may help offset risk for adult DE related to experiences of FI in childhood.
In adults, current food insecurity (FI; i.e., a lack of access, or worry about continued access, to adequate food for an active, healthy lifestyle) has been consistently related to disordered eating (DE) symptoms, including weight and shape concerns, fear of weight gain, and intentional restriction for weight loss,1,2 but most robustly to binge eating and inappropriate compensatory behaviors.3–6 To date, much of the work linking FI to DE has examined current FI in cross-sectional datasets. Thus, the impact of FI on eating behaviors across time is still relatively unknown. Approximately 1 in 8 US households with children are affected by FI,7 highlighting the need to understand the impact of FI early in life on adult eating behavior. Children living in food-insecure households are more likely than food-secure peers to be described by their parents as having elevated responsiveness to food (e.g., motivation to eat triggered by the availability of food or reminders of food), food enjoyment, and emotional overeating.8,9 These appetitive traits are linked to risk for weight gain across the lifespan9 and DE in adults.10,11 Children in FI households are known to be at elevated risk for higher body mass index (BMI) after adjusting for other socioeconomic factors.12 Overweight and obesity in childhood are linked to increased risk for the development of DE during puberty or later in life.13–16 Thus, the full impact of childhood FI on eating behavior may not become apparent until individuals have passed through puberty and early adulthood, developmental periods when incidence of DE increases.17–19
Six studies have explored the impact of prior FI on current DE. Two studies explored the relationship cross-sectionally using college undergraduates’ retrospective report of FI before age 18. Within both studies, experiencing FI before beginning college was associated with elevated symptoms of DE (e.g., overall DE20 and preoccupation with food, but not binge eating or hiding food21). However, these analyses did not adjust for the impact of current FI, and given the often chronic nature of poverty and FI, it is not possible to determine whether the increased levels of DE in the FI-exposed participants were attributable to the developmental impact of past FI or the direct impact of current FI.
Three sets of analyses, all using data from Project EAT (Eating and Activity over Time), explored the longitudinal relationship between FI and DE from adolescence to adulthood. Consistent results emerged from two different Project EAT cohorts: after adjusting for sociodemographic factors, FI in adolescence predicted higher rates of binge eating in late adolescence and young adulthood.4,12,22 Adolescent FI was also examined as a longitudinal predictor of other DE symptoms and behaviors, but no significant associations were observed with young adult disordered weight-control behaviors (e.g., vomiting) or chronic dieting4,12. Despite methodological strengths including large, population-based cohorts and longitudinal data analysis adjusting for a range of DE behaviors and socioeconomic variables, these analyses did not adjust for current FI at the timepoint when binge-eating risk or incidence was assessed.
To our knowledge, only one study has explored the relationship between FI and DE in a model that included both past and current FI as predictors. Using the same cohort as Hooper et al.,12 Larson and colleagues23 found that adjusting for severe FI in adolescence did not significantly attenuate or change the cross-sectional relationship between young adult FI and binge eating, which was again more common among emerging adults with current FI compared to food-secure peers. Notably, while this study demonstrates the robust nature of the association between current FI and binge eating, it does not directly explore whether the experience of childhood FI is associated with later DE when FI is not present.
To our knowledge, no study exploring the impact of FI during childhood on eating behavior in adulthood has controlled for current FI when exploring these relationships. Although the experience of FI is often transient and episodic, FI tracks strongly with low income, low educational attainment, and other indicators of economic marginalization across all stages of life.24,25 Thus, there is a strong likelihood that a large percentage of individuals who experienced FI before 18 years of age remain at risk for FI in adulthood. To isolate the relationship between childhood FI and adult DE, it is necessary to assess and control for concurrent adult FI. More replication is also needed, as four of six studies exploring this relationship used data from Project EAT cohorts, which, though diverse, are drawn from the same geographic region. Further, given that children start developing their relationship with food at an early age, the experience of childhood FI could also influence the development of various appetitive traits. Thus, exploration of a variety of DE symptoms and appetitive traits in adulthood is needed to understand the scope of eating behaviors associated with FI.
Past studies have explored the association between childhood FI and adult eating behaviors exclusively in young adulthood, a period of high risk for experiencing FI. The present study explored FI in another high-risk group, mothers living in households with young children26. Parents may be at elevated risk for experiencing FI due to the cost of rearing children and the tendency for parents to attempt to buffer the effects of FI from their children. Indeed, 34% of caregivers (compared to 4.9% of their children) endorsed skipping meals or eating less when the family had run out of food or money to buy food on the National Longitudinal Survey of Children and Youth (NLSCY)27 . Further, studies have highlighted that low-income mothers compromise their nutritional intake to preserve food access for their children26.
The current study explored differences in DE and related appetitive traits between four groups of mothers of 6–11-year-old children: (1) individuals who endorsed childhood FI only, (2) individuals who endorsed current FI only, (3) individuals who endorsed both childhood and current FI, and (4) individuals who denied childhood and current FI. By comparing levels of DE and appetitive traits across these groups, we aimed to explore the differential relationship between DE and FI that is childhood-limited, adulthood-limited, or recurrent. We hypothesized that (1) mothers who experienced both childhood and current FI would endorse the highest levels of DE and DE-related appetitive traits, whereas (2) mothers who denied childhood and current FI would endorse the lowest levels. Comparisons between the childhood FI-only and current FI-only groups were exploratory.
Methods
Participants
Our sample included 633 cisgender female mothers (mean age=34.77, SD=7.40) recruited using Amazon’s Mechanical Turk (MTurk) for an online study about the “impact of food availability on eating and feeding behaviors”. Given our primary research questions, we recruited approximately half the sample to have experienced FI during childhood, and the other half to have denied experiencing FI during childhood. A secondary aim of the data collection included exploring the influence of FI on parent feeding practices; thus, an additional inclusion criterion was having at least one child between the ages of 6–11 years. Only women were recruited due to the higher prevalence of ED pathology in women28 and the higher likelihood that mothers would be directly involved in feeding their children.
Participants were compensated $5 for the completion of the study, which, on average, took 28.49 minutes (SD=22.31) to complete. To ensure data quality, MTurk worker qualifications included a Human Intelligence Task (HIT) approval rate of greater than 95% (number of approved HITs that a worker has completed) and number of HITs approved greater than 100 (number of HITs that a worker has successfully completed since registering with MTurk). These requirements are consistent with other studies using MTurk samples (i.e., ≥90% approval rate, ≥100 approved HITs)29. Participants also needed to reside within the United States. Participants provided online informed consent at the beginning of the study. All study procedures were approved by the University of Chicago’s Institutional Review Board.
The full sample collected included 805 mothers. Six quality checks that asked participants to select the sentence that does not make semantic sense (e.g., “Planes yell on the dream”) from a set of four syntactically correct sentences (“Boats are sailing on the lake”) were administered throughout the study. The average completion time of the survey did not differ by the number of quality checks missed with one exception. Next, the internal consistency of well-validated, reliable measures (that include reverse-scored items) was explored by the number of missed quality checks. Cronbach’s alphas decreased when including individuals who missed four or more quality checks. Thus, our final analytic sample excludes those who missed at least four of six quality checks (n=171) and one individual who had missing data assessing current FI (n=1) for a total of 633 women. Our sample was economically diverse with 18.0% reporting a household income<$30,000, 40.6% between $30,000 and $59,999, 23.1% between $60,000 and $89,999, and 18.3%≥$90,000. Participants predominantly identified as non-Hispanic (82.0%) and White (77.4%), followed by participants who identified as African American (18.3%), Asian (3.8%), American Indian/Alaskan Native (3.2%), Native Hawaiian/Pacific Islander (1.1%), and those who preferred not to provide their race or ethnicity (1.3% and 2.4%, respectively).
Measures
Childhood and Current Food Security Status.
Three gateway items from the USDA Household Food Security Survey Module30 were used to assess childhood and current food security. Specifically, participants were asked to select whether the following statements were “often true”, “sometimes true”, or “never true”: “We worried whether our food would run out before we got money to buy more”, “The food that we bought just didn’t last, and we didn’t have money to get more”, and “We couldn’t afford to eat balanced meals”. When assessing childhood food security status, participants were instructed to “… think back to your childhood, when you were living with your parents or the guardians who raised you. Indicate whether the following statements were true during any point in your childhood.” When assessing current food security, participants were asked to respond to these three items based on the last 12 months.
For both childhood and current FI, participants who endorsed “never true” for all three statements were considered “food secure”, whereas participants who endorsed either “sometimes true” or “often true” for any of the three items were considered “food insecure”. Participants were then divided into four FI groups: (1) those who denied both childhood and current FI (“No FI”, n=146), (2) those who endorsed only childhood FI (“Childhood FI only”, n=96), (3) those who endorsed only current FI (“Current FI only”, n=134), and (4) those who endorsed both childhood and current FI (“Childhood & Current FI”, n=257).
Disordered Eating.
The brief Eating Disorder Examination Questionnaire (EDE-Q) consists of seven items from the EDE-Q that assess dietary restraint, weight/shape overvaluation, and body dissatisfaction, as well as a global score.31 The brief EDE-Q has been validated as a standalone measure,32 and studies demonstrate good convergent and discriminant validity compared to other eating disorder measures.33 Cronbach’s alpha in the current sample ranged from 0.92–0.93.
Binge Eating.
Two dichotomous (yes/no) questions from the Eating Disorder Diagnostic Scale for the DSM-5 (EDDS-5)34 assessed binge eating. Participants who responded affirmatively to both questions: “During the past 3 months have there been times when you have eaten what other people would regard as an unusually large amount of food (e.g., a pint of ice cream) given the circumstances?” and “During the times when you ate an unusually large amount of food, did you experience a loss of control (e.g., felt you couldn’t stop eating or control what or how much you were eating)?” were coded as endorsing binge eating. The EDDS based on the DSM-IV has demonstrated good reliability, criterion validity with interview-based assessments, and convergent validity with eating pathology risk factors.35
Appetitive Traits.
The Adult Eating Behavior Questionnaire (AEBQ)11 is a 35-item self-report questionnaire that assesses appetitive traits in adults. Items are rated on a 5-point Likert scale ranging from strongly disagree to strongly agree, and yield scores for eight traits: enjoyment of food, emotional overeating, emotional undereating, food fussiness, food responsiveness, slowness in eating, hunger, and satiety responsiveness. The AEBQ demonstrated good factor structure, test re-test reliability (0.73–0.91) and internal consistency (0.75–0.90).11 Cronbach’s alpha in the current sample ranged from 0.71–0.91.
Statistical Analyses
One-way analyses of covariance (ANCOVAs) were used to examine mean differences between the four FI groups in DE (i.e., restraint, overvaluation, and body dissatisfaction) and appetitive traits (i.e., emotional overeating, food responsiveness, satiety responsiveness, hunger, emotional undereating, food fussiness, enjoyment of food, and slow eating). Age, race, and ethnicity were included as covariates, as each was theorized to act as a confounder of the associations of interest. Post-hoc Tukey contrasts were performed to explore pairwise comparisons between groups.
A modified Poisson regression model (i.e., with robust standard errors36) adjusted for age, race, and ethnicity was conducted to examine differences in the prevalence of binge eating between the four FI groups. Pairwise comparisons were examined by changing the reference category for FI group in the regression model.
Results
Results from the one-way ANCOVAs are presented in Table 1 and Figures 1–2. For all DE outcomes and the majority of appetitive traits, significant group differences were indicated (p’s<.01). Largely, the “Current FI only” group demonstrated the highest endorsement of DE and appetitive traits, followed by the “Current & Childhood FI group”. There were no significant differences between the “No FI” and “Childhood FI only” groups for most DE and appetitive traits. The only exception was satiety responsiveness, for which the “Childhood FI only” group endorsed lower levels than the “No FI” group. Notably, the “Current FI” group demonstrated significantly higher endorsement compared to the “Current & Childhood FI” group on EDEQ Total Score, restraint, emotional overeating, satiety responsiveness, and emotional undereating. No significant differences were observed between these two groups on overvaluation, body dissatisfaction, food responsiveness, hunger, food fussiness, enjoyment of food, and slow eating.
Table 1.
One-Way Analyses of Covariance in Disordered Eating and Appetitive Traits based on Food Security Status (N=633)
| No FI History(a) | Childhood FI only(b) | Current FI only(c) | Current & Childhood FI(d) | F(3, 613) | Eta-Squared | |
|---|---|---|---|---|---|---|
| (n=146) M(SD) | (n=96) M(SD) | (n=134) M(SD) | (n=257) M(SD) | |||
| Eating Disorder Examination Questionnaire-Brief | ||||||
| Total Score | 2.45 (2.18, 2.73)c*** | 2.11 (1.76, 2.46)c***d** | 3.33 (3.03, 3.63)a***b***d* | 2.86 (2.65, 3.07)b**c* | 12.69*** | .07 (.03, .10) |
| Restraint | 2.35 (2.02, 2.67)c** | 2.01 (1.61, 2.42)c*** | 3.03 (2.68, 3.38)a**b***d** | 2.35 (2.11, 2.60)c** | 6.45*** | .04 (.01, .07) |
| Overvaluation | 2.40 (2.08, 2.72)c***d** | 2.16 (1.75, 2.56)c***d*** | 3.39 (3.04, 3.73)a***b*** | 3.13 (2.88, 3.37)a**b*** | 12.42*** | .06 (.03, .10) |
| Body Dissatisfaction | 2.67 (2.35, 2.98)c***d** | 2.21 (1.81, 2.61)c***d*** | 3.73 (3.39, 4.07)a***b*** | 3.35 (3.10, 3.59)a**b*** | 15.90*** | .08 (.04. .12) |
| Adult Eating Behavior Questionnaire | ||||||
| Food Responsiveness | 3.01 (2.87, 3.16)c***d** | 2.90 (2.72, 3.08)c***d*** | 3.41 (3.25, 3.56)a***b*** | 3.27 (3.16, 3.38)a**b*** | 10.69*** | .06 (.02, .09) |
| Satiety Responsiveness | 3.03 (2.88, 3.18)b*c* | 2.74 (2.55, 2.93)a*c*** | 3.31 (3.15, 3.47)a*b***d*** | 2.87 (2.76, 2.99)c*** | 11.92*** | .08 (.04, .11) |
| Emotional Overeating | 2.71 (2.52, 2.90)c*** | 2.46 (2.22, 2.69)c***d*** | 3.39 (3.19, 3.59)a***b***d** | 2.89 (2.74, 3.03)b***c** | 15.18*** | .09 (.05, .13) |
| Emotional Undereating | 3.00 (2.82, 3.19)c*** | 2.96 (2.73, 3.19)c** | 3.45 (3.25, 3.65)a***b**d*** | 2.91 (2.76, 3.05)c*** | 8.56*** | .05 (.02,.09) |
| Hunger | 2.81 (2.67, 2.95)c***d** | 2.70 (2.52, 2.88)c***d*** | 3.29 (3.14, 3.44)a***b*** | 3.06 (2.95, 3.16)a**b*** | 13.29*** | .08 (.04, .11) |
| Food Fussiness | 2.38 (2.24, 2.52) | 2.13 (1.95, 2.30)c** | 2.57 (2.42, 2.72)b** | 2.42 (2.31, 2.52) | 4.35** | .03 (.01, .06) |
| Enjoyment of Food | 4.07 (3.95, 4.19)c* | 4.14 (3.99, 4.29)c* | 3.84 (3.71, 3.97)a*b* | 3.94 (3.85, 4.03) | 4.10** | .02 (.00, .04) |
| Slow Eating | 2.92 (2.77, 3.07) | 2.82 (2.63, 3.01) | 3.00 (2.83, 3.16) | 2.85 (2.73, 2.96) | 1.92 | .02 (.00, .03) |
Note. Both childhood and current food security status were evaluated using three items from the USDA Household Food Security Survey Module. Age and race/ethnicity were included as covariates.
Superscript letters reflect significant differences (*p-value < .05, **p-value < .01, ***p-value < .001) with one of the other groups with “a” denoting the No FI History, “b” denoting the Childhood FI only group, “c” denoting the Current FI only group, and “d” denoting the Current & Childhood FI.
Figure 1.
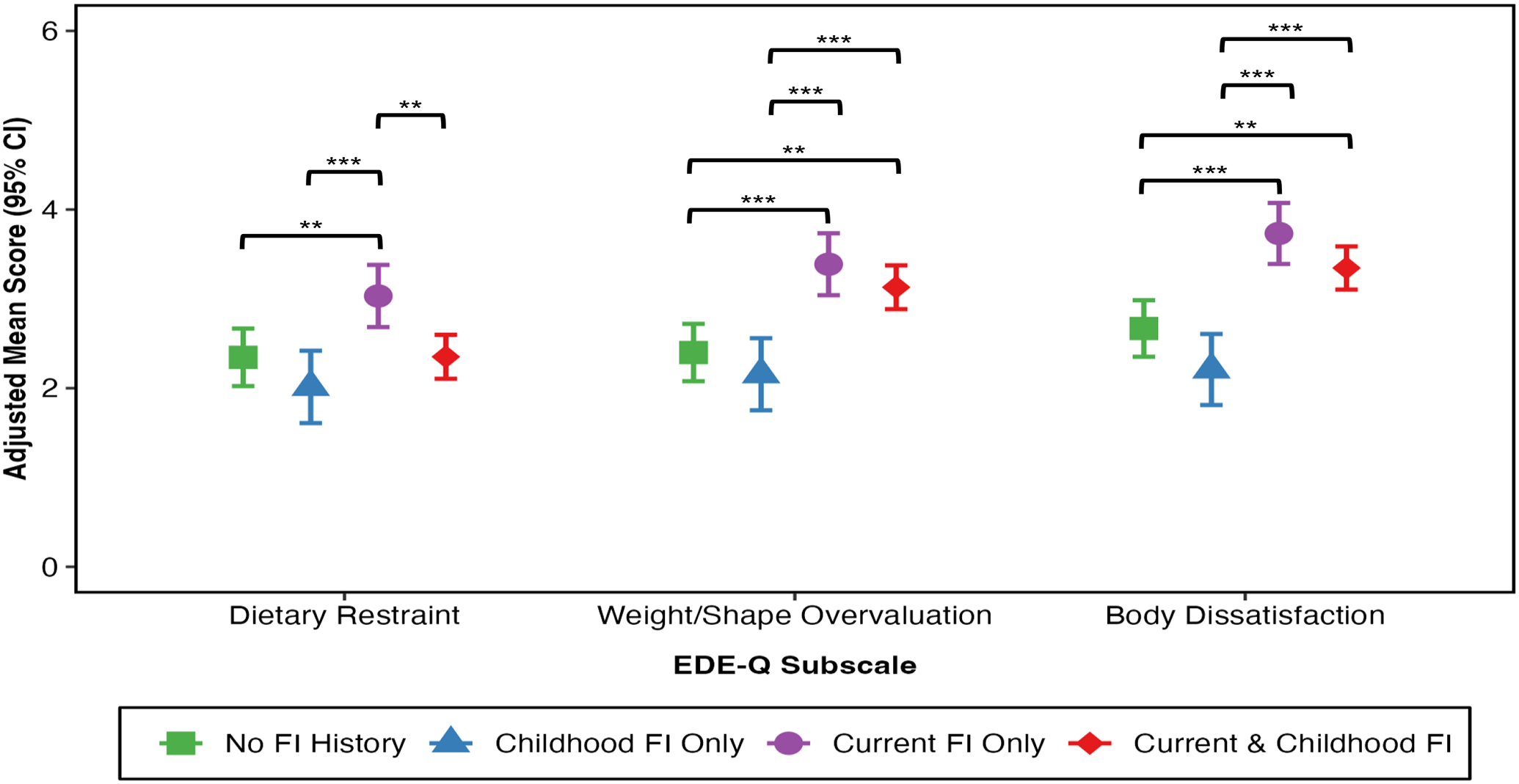
Mean EDE-Q subscale scores by food insecurity group, adjusted for age and race/ethnicity (error bars indicate 95% confidence intervals; ** p < .01, *** p < .001)
Figure 2.
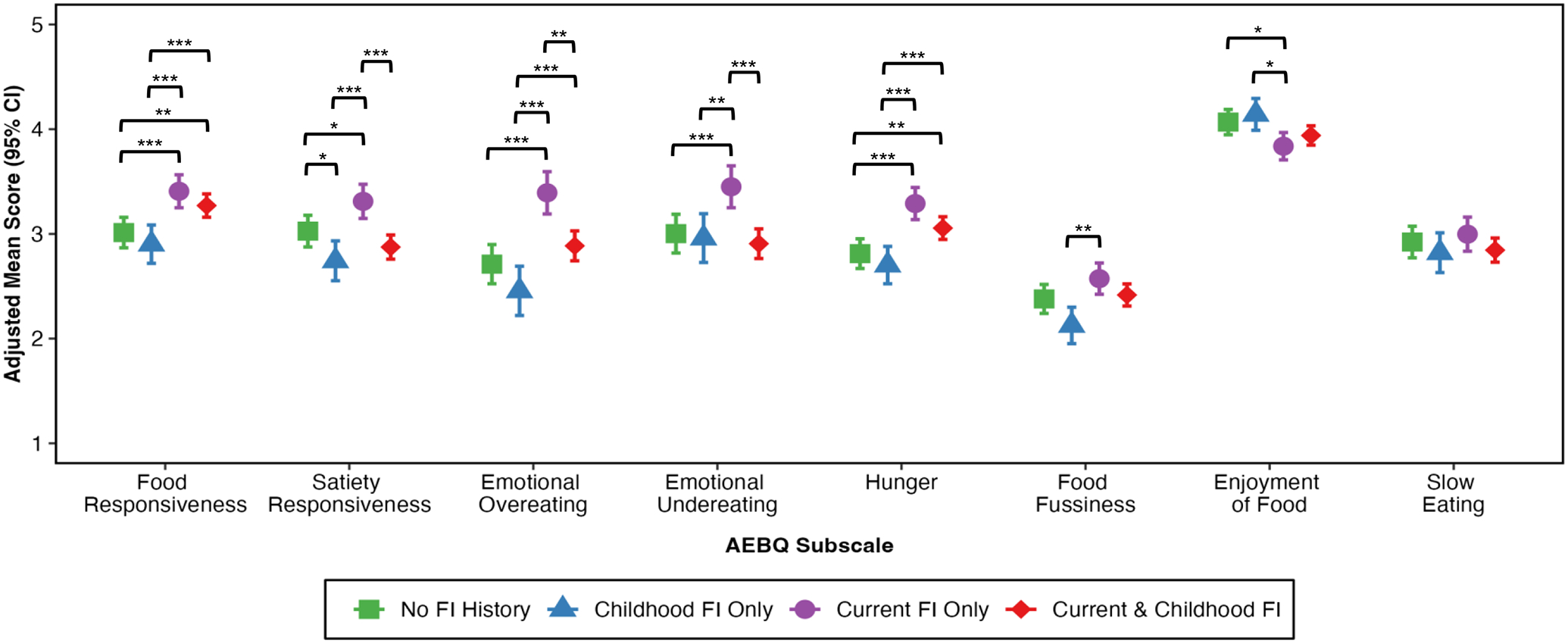
Mean AEBQ subscale scores by food insecurity group, adjusted for age and race/ethnicity (error bars indicate 95% confidence intervals; * p < .05, ** p < .01, *** p < .001)
Two exceptions to this pattern included the enjoyment of food subscale, which demonstrated the inverse pattern. Specifically, those experiencing “Current FI only” demonstrated the lowest endorsement of enjoyment of food with similar levels of enjoyment of food indicated for the “No FI”, “Childhood FI only”, and “Current & Childhood FI” groups. The second exception was for the slow eating subscale, which exhibited no significant differences among groups.
The prevalence of binge eating differed significantly by FI group after adjusting for age and race/ethnicity, X2(3, N=633) = 35.73, p <.001. Specifically, the prevalence of binge eating in the “Current FI only” group was 1.83 (95% confidence interval [CI]: 1.35, 2.49) times as high as that in the “No FI” group, 2.78 (95% CI: 1.72, 4.50) times as high as that in the “Childhood FI only” group, and 1.84 (95% CI: 1.41, 2.38) times as high as that in the “Current & Childhood FI” group (see Figure 3). Each of these group differences in prevalence of binge eating was significant at p<.001.
Figure 3.
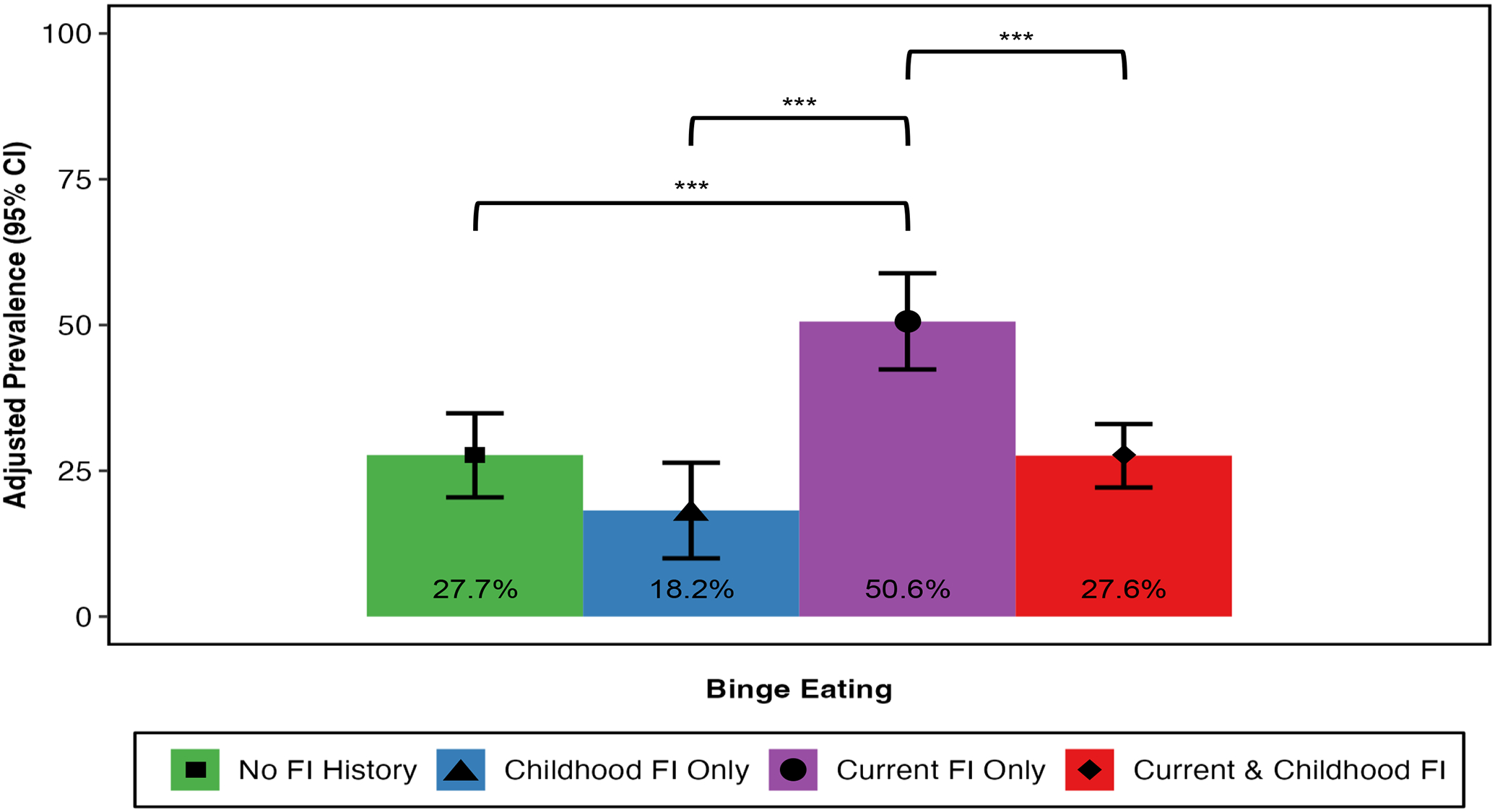
Predicted prevalence of binge eating by food insecurity group, adjusted for age and race/ethnicity (error bars indicate 95% confidence intervals; *** p < .001)
Discussion
To advance understanding of how childhood FI may influence adult eating behavior, this study examined differences in DE and related appetitive traits by current FI status and childhood FI history among mothers. While results pertaining to current FI were consistent with prior studies documenting a cross-sectional link between FI and DE,5 consideration of childhood FI history yielded more nuanced findings. Contrary to our hypotheses, results indicated that the highest levels of DE and related appetitive traits generally were observed in women experiencing current FI without a history of childhood FI, with the next highest levels observed in those who reported both current and childhood FI. Differences between these two groups were more apparent for measures of behavior (e.g., dietary restraint, binge eating, emotional overeating, emotional undereating) than those of cognitively-oriented constructs (e.g., weight/shape overvaluation, body dissatisfaction). These findings may reflect that women with recurrent exposure to FI may be more connected to resources or have found coping strategies to alleviate some of the behavioral DE symptoms, but not the cognitive symptoms. Further, newer experiences with FI could also reflect the existence of a recent and ongoing stressor that led to current FI (e.g., divorce, illness, job loss, etc.). Thus, the possibility of compounding stressors and/or the lack of connection to resources related to FI may explain the higher levels of DE and DE-related appetitive traits in the “Current FI only” group relative to those who experience FI more chronically.
Also counter to our hypotheses, currently food-secure women with a history of childhood FI did not exhibit significantly elevated levels of any aspect of DE or appetitive traits relative to women with no FI history, with one exception. Women who endorsed childhood FI reported significantly lower satiety responsiveness than women who denied both current and childhood FI, indicating that those with childhood FI may have more difficulty recognizing when they feel full. Women with both current and childhood FI exposure reported similar levels of satiety responsiveness compared to women with childhood-limited FI.
A possible explanation for why women exposed to FI during childhood, regardless of current food security status, may endorse lower satiety responsiveness is that children in food insecure households are more likely to be encouraged to “clean their plate,” and have fewer opportunities to self-regulate eating based on satiety cues. Numerous studies, including both observational and experimental designs, have found that encouraging preschool and school-aged children to ignore satiety cues in favor of external cues (e.g., the amount of food served) is associated with diminished responsiveness to internal satiety signals.37,38 Although these feeding practices have been found to be common in general samples,39,40 there is some indication that they are more common in FI households, which could help to explain the current finding that childhood FI is specifically linked to low satiety responsiveness in adults. For example, one qualitative study of parents of children 5–7 years old found that less than a third of food-secure families required their children to finish all the food on their plates compared to approximately half of food-insecure families, and that parents in food-insecure families were more likely to perceive their role in family mealtimes as ensuring that their child ate enough food.41 Food-insecure parents cited family anxiety about food waste and protecting children from hunger as reasons for their encouragement of clean plates.42
Interestingly, within our study, women currently experiencing FI with no history of childhood FI reported the highest levels of satiety responsiveness (i.e., endorsed becoming full more easily and before a meal is finished). While reasons for this elevation are unclear, it is possible that the preoccupation with food that is reported in food-insecure populations21 may lead individuals (without a prior history of disrupted satiety responsiveness) to attend more closely to their satiety cues. Longitudinal studies are needed to better understand how unreliable access to food affects satiety responsiveness over time.
Finally, enjoyment of food seemed to exhibit a different pattern of results compared to DE and other appetitive traits explored. Specifically, women experiencing current FI reported significantly lower levels of enjoyment of food compared to women in the “No FI” group and women who endorsed “Childhood FI only”. No significant difference was observed between the “Current FI only” group and “Current & Childhood FI” groups. Items on the enjoyment of food scale include “I look forward to mealtimes”. Given the stress associated with the experience of FI43, it is possible that individuals experiencing current FI, regardless of the experience of childhood FI, view food and mealtime as less pleasurable. A similar pattern emerged for food fussiness, a measure of limited dietary variety and reluctance to try new foods (e.g., selective eating). None of the FI-exposed groups differed from the no-FI group on this variable, but participants with current FI only endorsed slightly higher food fussiness compared to the childhood-only FI participants. Some have suggested that childhood FI may be a risk factor for the development of selective eating, which in turn can lead to symptoms of Avoidant/Restrictive Food Intake Disorder.44,45 Research suggests that it can take as many as 20 exposures to a novel food before children are willing to incorporate it into their diets.46 Families with FI report difficulties with exposing their children to a variety of foods, or hesitancy to serve foods that the child might not accept,42 but no available evidence supports the hypothesis that FI is concurrently related to selective eating. Indeed, several studies have failed to find an association between concurrent childhood FI and childhood food selectivity.47,48 Notably, however, our effect sizes were small for both enjoyment of food and food fussiness.
Although the present study has several strengths (e.g., large sample, exploration of DE and appetitive traits, independent assessment of childhood and current FI), it also has limitations. First, the evaluation of childhood FI relied on three retrospective items. There may be bias in retrospective reporting, which may be particularly true for childhood FI given that parents often attempt to buffer the effects of FI from their children.49 Thus, participants may have been unaware of the extent to which their parents were concerned about food access when they were children. Second, both current and childhood food security status were evaluated dichotomously, whereas it is recognized that FI exists on a spectrum. Further research examining a more nuanced view of past and current FI (e.g., duration, severity) is needed. Similarly, binge eating was assessed dichotomously using two items from the EDDS-5 that have not been explored for psychometric qualities. Thus, future research using more nuanced and well-established measures of binge eating is needed. Third, the present study collected data using Amazon’s Mechanical Turk. While quality checks and worker requirements were used to ensure data quality, there has been debate within the field regarding the use of MTurk.50,51 Our data quality checks and screening processes are consistent with recommendations for collecting quality data, and screening for poor-quality data, on MTurk.52 Fourth, our sample included data from mothers who had at least one child aged 6–11, which may have limited generalizability to all parents or all adult women. Fifth, while the brief EDE-Q has been demonstrated as appropriate for use in food-insecure samples (i.e., no differential item functioning between food insecure and food secure samples53), similar exploration of the psychometric properties of items on the AEBQ has yet to be conducted. Sixth, the present study did not control for SES, and thus it is unclear whether FI specifically or disadvantage more broadly drives the relationship between FI and DE. Finally, the cross-sectional nature of the present study precludes our ability to establish temporality. Longitudinal studies are needed to further delineate how the experience of FI is associated with DE overtime.
This study was the first to our knowledge to explore the association between childhood FI and adulthood eating behaviors accounting for current FI. Despite consistent emerging evidence of associations between current FI and DE, this study suggests that the experience of FI in childhood is not linked with elevated eating pathology during adulthood in the absence of current FI, as women with childhood-limited exposure to FI reported similar levels of DE and appetitive traits to women with no experience of FI. Further, exposure to both childhood and current FI was not associated with worse DE-related outcomes than current FI only. These findings were consistent across multiple measures of DE cognitions, behaviors, and related traits, and highlight a continued need for assessment of DE in individuals and communities at highest risk for FI, particularly those who are newly food insecure. Further, there may be policy-related future directions as our findings provide preliminary support for optimism that improving access to food may help offset risk for adult DE related to experiences of FI in childhood.
Highlights.
Childhood food insecurity was not associated with elevated adult disordered eating (DE)
Individuals experiencing current food insecurity exhibited the highest levels of DE
Results were largely consistent across a range of DE constructs and appetitive traits
Funding:
Drs. Shannon O’Connor, Hana Zickgraf, and Vivienne Hazzard were supported by the National Institute of Mental Health under award number T32 MH082761. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Mental Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest/Competing interests:
Authors have no conflicts to declare.
Ethics Approval: This study was reviewed and approved by the University of Chicago Institutional Review Board.
Consent to Participate: Informed consent was obtained from all participants included in the study.
Data Availability Statement:
The data generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.Becker CB, Middlemass K, Taylor B, Johnson C & Gomez F Food insecurity and eating disorder pathology. International Journal of Eating Disorders 50, 1031–1040 (2017). 10.1002/eat.22735 [DOI] [PubMed] [Google Scholar]
- 2.Becker CB, Middlemass KM, Gomez F & Martinez-Abrego A Eating disorder pathology among individuals living with food insecurity: A replication study. Clinical Psychological Science 7, 1144–1158 (2019). 10.1177/2167702619851811 [DOI] [Google Scholar]
- 3.Hazzard VM et al. Food insecurity and its associations with bulimic-spectrum eating disorders, mood disorders, and anxiety disorders in a nationally representative sample of U.S. adults. Soc Psychiatry Psychiatr Epidemiol 57, 1483–1490 (2022). 10.1007/s00127-021-02126-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hazzard VM et al. Associations between severe food insecurity and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. Prev Med 154, 106895 (2022). 10.1016/j.ypmed.2021.106895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hazzard VM, Loth KA, Hooper L & Becker CB Food Insecurity and Eating Disorders: a Review of Emerging Evidence. Curr Psychiatry Rep 22, 74 (2020). 10.1007/s11920-020-01200-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christensen KA et al. Food insecurity associated with elevated eating disorder symptoms, impairment, and eating disorder diagnoses in an American University student sample before and during the beginning of the COVID-19 pandemic. Int J Eat Disord 54, 1213–1223 (2021). 10.1002/eat.23517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coleman-Jensen A, Rabbitt MP, Gregory CA & Singh A Household food security in the United States in 2021. Amber Waves: The Economics of Food, Farming, Natural Resources, and Rural America 2022 (2022). [Google Scholar]
- 8.Eagleton SG, Na M & Savage JS Food insecurity is associated with higher food responsiveness in low-income children: The moderating role of parent stress and family functioning. Pediatr Obes 17, e12837 (2022). 10.1111/ijpo.12837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher JO et al. Characteristics of eating behavior profiles among preschoolers with low-income backgrounds: a person-centered analysis. Int J Behav Nutr Phys Act 19, 91 (2022). 10.1186/s12966-022-01323-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.He J, Sun S, Zickgraf HF, Ellis JM & Fan X Assessing Appetitive Traits Among Chinese Young Adults Using the Adult Eating Behavior Questionnaire: Factor Structure, Gender Invariance and Latent Mean Differences, and Associations With BMI. Assessment 28, 877–889 (2021). 10.1177/1073191119864642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hunot C et al. Appetitive traits and relationships with BMI in adults: Development of the Adult Eating Behaviour Questionnaire. Appetite 105, 356–363 (2016). 10.1016/j.appet.2016.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hooper L, Mason SM, Telke S, Larson N & Neumark-Sztainer D Experiencing Household Food Insecurity During Adolescence Predicts Disordered Eating and Elevated Body Mass Index 8 Years Later. J Adolesc Health 70, 788–795 (2022). 10.1016/j.jadohealth.2021.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cena H et al. Association of a history of childhood-onset obesity and dieting with eating disorders. Eat Disord 25, 216–229 (2017). 10.1080/10640266.2017.1279905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Markowitz JT, Lowe MR, Volkening LK & Laffel LM Self-reported history of overweight and its relationship to disordered eating in adolescent girls with Type 1 diabetes. Diabet Med 26, 1165–1171 (2009). 10.1111/j.1464-5491.2009.02844.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rancourt D & McCullough MB Overlap in Eating Disorders and Obesity in Adolescence. Current Diabetes Reports 15, 78 (2015). 10.1007/s11892-015-0645-y [DOI] [PubMed] [Google Scholar]
- 16.Sim LA, Lebow J & Billings M Eating disorders in adolescents with a history of obesity. Pediatrics 132, e1026–1030 (2013). 10.1542/peds.2012-3940 [DOI] [PubMed] [Google Scholar]
- 17.Marzilli E, Cerniglia L & Cimino S A narrative review of binge eating disorder in adolescence: prevalence, impact, and psychological treatment strategies. Adolesc Health Med Ther 9, 17–30 (2018). 10.2147/ahmt.S148050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hudson JI, Hiripi E, Pope HG Jr. & Kessler RC The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry 61, 348–358 (2007). 10.1016/j.biopsych.2006.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Slane JD, Klump KL, McGue M & Iacono WG Developmental trajectories of disordered eating from early adolescence to young adulthood: a longitudinal study. Int J Eat Disord 47, 793–801 (2014). 10.1002/eat.22329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Darling KE, Fahrenkamp AJ, Wilson SM, D’Auria AL & Sato AF Physical and mental health outcomes associated with prior food insecurity among young adults. Journal of Health Psychology 22, 572–581 (2015). 10.1177/1359105315609087 [DOI] [PubMed] [Google Scholar]
- 21.Poll KL, Holben DH, Valliant M & Joung HD Food insecurity is associated with disordered eating behaviors in NCAA division 1 male collegiate athletes. J Am Coll Health 68, 105–109 (2020). 10.1080/07448481.2018.1529035 [DOI] [PubMed] [Google Scholar]
- 22.West CE, Goldschmidt AB, Mason SM & Neumark‐Sztainer D Differences in risk factors for binge eating by socioeconomic status in a community‐based sample of adolescents: Findings from project EAT. International Journal of Eating Disorders 52, 659–668 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Larson N, Laska MN & Neumark-Sztainer D Food Insecurity, Diet Quality, Home Food Availability, and Health Risk Behaviors Among Emerging Adults: Findings From the EAT 2010–2018 Study. Am J Public Health 110, 1422–1428 (2020). 10.2105/AJPH.2020.305783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamelin A-M, Habicht J-P & Beaudry M Food Insecurity: Consequences for the Household and Broader Social Implications. The Journal of Nutrition 129, 525S–528S (1999). 10.1093/jn/129.2.525S [DOI] [PubMed] [Google Scholar]
- 25.Rose D Economic Determinants and Dietary Consequences of Food Insecurity in the United States. The Journal of Nutrition 129, 517S–520S (1999). 10.1093/jn/129.2.517S [DOI] [PubMed] [Google Scholar]
- 26.McIntyre L et al. Do low-income lone mothers compromise their nutrition to feed their children? Cmaj 168, 686–691 (2003). [PMC free article] [PubMed] [Google Scholar]
- 27.McIntyre L, Connor SK & Warren J Child hunger in Canada: Results of the 1994 National Longitudinal Survey of Children and Youth. CANADIAN MEDICAL ASSOCIATION JOURNAL 163, 961–965 (2000). [PMC free article] [PubMed] [Google Scholar]
- 28.American Psychiatric, A. & American Psychiatric, A. Diagnostic and statistical manual of mental disorders : DSM-5. 5th edn, xliv, 947 pages ; 26 cm (American Psychiatric Association, 2013). [Google Scholar]
- 29.Chmielewski M & Kucker SC An MTurk crisis? Shifts in data quality and the impact on study results. Social Psychological and Personality Science 11, 464–473 (2020). [Google Scholar]
- 30.Carlson SJ, Andrews MS & Bickel GW Measuring food insecurity and hunger in the United States: development of a national benchmark measure and prevalence estimates. The Journal of nutrition 129, 510S–516S (1999). [DOI] [PubMed] [Google Scholar]
- 31.Grilo CM et al. Factor Structure of the Eating Disorder Examination Interview in Patients With Binge-eating Disorder. Obesity 18, 977–981 (2010). 10.1038/oby.2009.321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jenkins PE & Davey E The brief (seven-item) eating disorder examination-questionnaire: Evaluation of a non-nested version in men and women. International Journal of Eating Disorders 53, 1809–1817 (2020). 10.1002/eat.23360 [DOI] [PubMed] [Google Scholar]
- 33.Grilo CM, Reas DL, Hopwood CJ & Crosby RD Factor Structure and Construct Validity of the Eating Disorder Examination-Questionnaire in College Students: Further Support for a Modified Brief Version. INTERNATIONAL JOURNAL OF EATING DISORDERS 48, 284–289 (2015). 10.1002/eat.22358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stice E, Telch CF & Rizvi SL Development and validation of the Eating Disorder Diagnostic Scale: a brief self-report measure of anorexia, bulimia, and binge-eating disorder. Psychol Assess 12, 123–131 (2000). 10.1037//1040-3590.12.2.123 [DOI] [PubMed] [Google Scholar]
- 35.Stice E, Fisher M & Martinez E Eating disorder diagnostic scale: additional evidence of reliability and validity. Psychological assessment 16, 60 (2004). [DOI] [PubMed] [Google Scholar]
- 36.Zou G A modified poisson regression approach to prospective studies with binary data. American journal of epidemiology 159, 702–706 (2004). 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 37.Bilman E, van Kleef E & van Trijp H External cues challenging the internal appetite control system-Overview and practical implications. Crit Rev Food Sci Nutr 57, 2825–2834 (2017). 10.1080/10408398.2015.1073140 [DOI] [PubMed] [Google Scholar]
- 38.Birch LL, McPhee L, Shoba BC, Steinberg L & Krehbiel R “Clean up your plate”: Effects of child feeding practices on the conditioning of meal size. Learning and motivation (Print) 18, 301–317 (1987). [Google Scholar]
- 39.Fletcher J, Branen LJ & Lawrence A Late adolescents’ perceptions of their caregiver’s feeding styles and practices and those they will use with their own children. Adolescence 32, 287–298 (1997). [PubMed] [Google Scholar]
- 40.Orrell-Valente JK et al. “Just three more bites”: An observational analysis of parents’ socialization of children’s eating at mealtime. Appetite 48, 37–45 (2007). 10.1016/j.appet.2006.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Trofholz AC, Tate A, Keithahn H, de Brito JN, Loth K, Fertig A, & Berge JM (2021). Family meal characteristics in racially/ethnically diverse and immigrant/refugee households by household food security status: A mixed methods study. Appetite, 157, 105000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Trofholz A et al. Ecological Momentary Assessment of Weight-Related Behaviors in the Home Environment of Children From Low-Income and Racially and Ethnically Diverse Households: Development and Usability Study. JMIR Res Protoc 10, e30525 (2021). 10.2196/30525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pourmotabbed A et al. Food insecurity and mental health: a systematic review and meta-analysis. Public Health Nutrition 23, 1778–1790 (2020). 10.1017/S136898001900435X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thomas JJ et al. Avoidant/Restrictive Food Intake Disorder: a Three-Dimensional Model of Neurobiology with Implications for Etiology and Treatment. Curr Psychiatry Rep 19, 54 (2017). 10.1007/s11920-017-0795-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zickgraf HF, Murray HB, Kratz HE & Franklin ME Characteristics of outpatients diagnosed with the selective/neophobic presentation of avoidant/restrictive food intake disorder. Int J Eat Disord 52, 367–377 (2019). 10.1002/eat.23013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cooke L The importance of exposure for healthy eating in childhood: a review. J Hum Nutr Diet 20, 294–301 (2007). 10.1111/j.1365-277X.2007.00804.x [DOI] [PubMed] [Google Scholar]
- 47.Brown CL et al. Association of Picky Eating With Weight Status and Dietary Quality Among Low-Income Preschoolers. Academic Pediatrics 18, 334–341 (2018). 10.1016/j.acap.2017.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Berge JM et al. Associations between parental stress, parent feeding practices, and child eating behaviors within the context of food insecurity. Prev Med Rep 19, 101146 (2020). 10.1016/j.pmedr.2020.101146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Landry MJ et al. Child Compared with Parent Perceptions of Child-Level Food Security. Current Developments in Nutrition 3, nzz106 (2019). 10.1093/cdn/nzz106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Burnette CB et al. Concerns and recommendations for using Amazon MTurk for eating disorder research. International Journal of Eating Disorders 55, 263–272 (2022). 10.1002/eat.23614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vogel M, Krüger J & Junne F Eating disorder related research using Amazon Mechanical Turk (MTurk): Friend or foe?: Commentary on Burnette et al (2021). International Journal of Eating Disorders 55, 285–287 (2022). [DOI] [PubMed] [Google Scholar]
- 52.Chmielewski M & Kucker SC An MTurk Crisis? Shifts in Data Quality and the Impact on Study Results. Social Psychological and Personality Science 11, 464–473 (2019). 10.1177/1948550619875149 [DOI] [Google Scholar]
- 53.O’Connor SM, Hazzard VM & Zickgraf HF Exploring differential item functioning on eating disorder measures by food security status. Eating and weight disorders : EWD 27, 1449–1455 (2022). 10.1007/s40519-021-01289-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data generated and/or analyzed during the current study are available from the corresponding author on reasonable request.


