Abstract
Introduction:
Although stress has been associated with eating behaviors, such as overeating and eating less healthy foods, the relationships between specific types of parent stressors and fast-food consumption in parents and young children have not been well studied. We hypothesized that parent perceived stress, parenting stress, and household chaos would be positively associated with fast-food consumption for parents and their young children.
Methods:
Parents of 2–5 year olds and with Body Mass Index > 27 kg/m2 (N=234, parent mean age: 34.3 (±5.7); child age: 44.9 (±13.8) months; 65.8% from two parent households) completed surveys on parent perceived stress, parenting stress, household chaos, and their fast-food intake and that of their child.
Results:
In separate regression models, controlling for covariates, parent perceived stress (β=0.21, p<0.01; R2=0.10, p<0.01), parenting stress (β=0.26, p<0.01; R2=0.13, p<0.01), and household chaos (β=0.25, p<0.01; R2=0.12, p<0.01) were each significantly associated with parent fast-food consumption, and separately with child fast-food consumption [Parent perceived stress (β=0.05, p=0.02; R2=0.14, p<0.01); parenting stress (β=0.14, p=0.03; R2=0.14, p<0.01); parent fast-food consumption (β=0.40, p<0.01; R2=0.27, p<0.01)]. However, combined final models showed parenting stress (p < 0.01) as the only significant predictor of parent fast-food consumption, which in turn was the only significant predictor of child fast-food consumption (p < 0.01).
Discussion:
The findings support the inclusion of parenting stress interventions that target fast-food eating behaviors in parents, which may in turn, reduce fast-food intake in their young children.
Keywords: stress, parenting stress, fast food, child nutrition, household chaos
1. Introduction
Frequent consumption of fast-food is a potential pathway to increased risk of health problems including obesity in adults (Fryar et al., 2013; Rosenheck, 2008), and is a source of higher caloric intake with poor nutritional quality for children (Powell & Nguyen, 2013). It is important to assess fast-food consumption in parents and their young children because food preference patterns are often set early in children’s lives within a familial context (Cooke, 2007; van’t Riet et al., 2011). Although multiple biopsychosocial factors contribute to health problems such as obesity risk across generations including genetics (Soubry et al., 2015), environment (Keane et al., 2012), and behavioral patterns such as nutritional intake (Sahoo et al., 2015), far less research has examined effects of environmental factors specifically on fast-food intake. Moreover, these impacts have rarely been investigated in parents and their young children within the same study. The Theory of Planned Behavior, which assumes that behavioral intentions result from an evaluation of the risks and benefits of specific behaviors, is widely used to predict health behaviors (Ajzen, 1991). Some behaviors such as smoking, drinking, exercise, and diet have received the attention of psychological research for their clear contradiction to this theory. However, the association between planned behavior and healthy intentions can be heavily influenced by stress (Louis et al., 2009). Therefore, we aimed to assess perceived stress as a key environmental factor for its association with food choices, specifically fast-food consumption.
Prior research has identified associations between stress and diet, including higher consumption of high-fat foods (Baskind et al., 2019), higher stress-related craving of highly palatable foods (Sinha et al., 2019), lower consumption of fruits and vegetables (Khaled et al., 2020), and the use of food as a coping mechanism (Mason et al., 2019). Parent perceived stress and parenting stressors include specific challenges related to child-caretaking, household responsibilities, parent employment and partner relationships, and maintaining their own health and wellbeing. Higher parent stress is associated with lower availability of fruits, vegetables, and healthy beverages in the home (Jang et al., 2021). Meal preparation at home may be particularly stressful for parents due to time constraints and chaotic stucture in the home (Beshara et al., 2010). Household chaos, characterized by dyfunction, disorganization, and lack of structure in the home (Evans et al., 2005), is associated with childhood malnutrition and weight gain (Anderson & Whitaker, 2010), though findings are inconsistent (Bates et al., 2018). The parent and family chaos factors may be viewed also within the family stress model framework (Masarik & Conger, 2017), which purports that parent and family stressors may affect child and adolescent development primarily through parents’ psychological distress, interparental relationship/marital problems, and disrupted parenting. Extending this model, we can assess how parenting stress and household chaos may be associated with parent and family health behaviors.
Stress is a multidimensional complex phenomenon. Psychological stress is innately tied to an individual’s perception of threat and resources available that would allow them to cope with the perceived stressor (Lazarus & Folkman, 1984). Therefore, when assessing psychosocial stress, it is important to consider how different aspects of a stressor may be perceived as more or less stressful to the individual based on their perceived threat and available resources. For example, assessment of perceived stress may not distinguish between specific perceived parent stress (e.g. related to finances or work) and those related to chaos in the family environment or stress related to parenting responsibiities, thereby possibly missing specific aspects of stress that may contrbute to parent and child health behaviors. While perceived parent stress captures overall sense of threats and stress and one’s abilties to control and manage the stress as measured by the Perceived Stress Scale (PSS; Cohen et al., 1983), the stress related to parenting a small child, such as the demand of attending to all aspects of child care may not be experienced by parents as the same as work, finacial or marital stress. Similarly household chaos which encompasses household hubbub, disorganization, hurriedness, covering multiple things at once may not be perceived by parents as an inability to manage the multiple demands but rather just busyness and having multiple household demands. Although previous studies have assessed specific individual factors that may contribute to parenting stress and child health behaviors (Gouveia, et al., 2019; Jang, et al., 2021), including economic hardship (Schuler, et al., 2020) and parenting style (Park & Walton-Moss, 2012), few studies have used multiple measures of stress in the same sample to assess how different stressors impact parent and child fast-food consumption.
The purpose of this study was to assess associations among parent perceived stress, parenting stress, household chaos, and fast-food consumption in parents and separately in their young children aged 2–5 years old. We hypothesized significant and positive associations between greater parent perceived stress, higher parenting stress, and greater household chaos and greater fast-food consumption for both parents and their children. We also hypothesized a significant and positive association between parent fast-food consumption and child fast-food consumption.
2. Methods
2.1. Participants
Participants were recruited from the surrounding local communities in the greater New Haven area between late 2019 through early 2022. Inclusion criteria for study participation were adults (18 or older), with a body mass index (BMI) over 27 kg/m2 and were the primary caretakers of a child between the ages of two and five years old. Many participants could not accurately provide an exact yearly income, and therefore we opted for endorsement of an income range. We had 7 different income ranges, from <$15,000 to > $100,00. Income requirements for poverty levels were calculated based on the number of people in the household (adults and children) using national guidelines (https://aspe.hhs.gov/topics/poverty-economic-mobility/poverty-guidelines/prior-hhs-poverty-guidelines-federal-register-references/2021-poverty-guidelines). The poverty level was translated into the income ranges we had (e.g., if someone’s poverty level was $16,000, they fit into the $15,000-$24,9999 range). Their actual income range was then compared to the income needed. If the difference between these two values was 0 or negative (for instance someone earned <$15,000 but needed at least $16,000 to meet poverty level requirements), they were classified as “at or below poverty.” However, if they exceeded the needed income they were “above poverty.” Exclusion criteria were medical or psychiatric illness that required acute medical care, acute psychiatric symptoms (suicidal / homicidal ideations), pervasive developmental disorder in the child, or an active alcohol or substance use disorder based on the Structured Clinical Interview for DSM-IV (SCID-IV) and positive drug testing by urine toxicology. Participants with past or currently stable in treatment for any medical or non-psychotic psychiatric illnesses were not excluded. The inclusion and exclusion criteria for this study were based on the needs for a larger trial utilizing this data. The study was approved by the University Institutional Review Board (IRB) and all parents signed written informed consent.
2.2. Measures
2.2.1. Independent Variables
Parent Perceived Stress.
The Perceived Stress Scale (PSS; Cohen et al., 1983) was used to assess the frequency in which the participants have felt stressed or unable to cope with their stress within the last month. The PSS is a 14-item self-report scale with items such as “How often have you been upset because of something that happened unexpectedly?” The items are rated on a scale from 0= “Never” to 4 = “Very often”. Total scores were calculated by summing the responses, with higher scores indicating higher levels of perceived stress. The PSS has excellent test reliability and construct validity. Previous studies have reported high internal consistency of the PSS with Cronbach’s alpha coefficient of 0.78, .91, and 0.91 in their three independent samples (Cohen & Janiki, 2012). The Cronbach’s alpha for the current sample was 0.87.
Parenting Stress.
The Parenting Stress Index short form (PSI-SF; Haskett et al., 2006) was used to assess stress derived from the parent-child system. The PSI-SF is a 36-item self-assessment that is directly pulled from the full-length Parent Stress Index 120-item assessment (Abidin,1995; Johnson, 2015). The scale includes items such as “I feel trapped by my responsibilities as a parent.” The items are rated on a scale ranging from 1 = “Strongly agree” to 5 = “Strongly disagree.” Items are reverse coded so that a higher score indicates higher levels of parent stress. The PSI-SF demonstrates strong internal consistency and validity (Haskett et al., 2006; Lee et al., 2016). The Cronbach’s alpha for the total scale for the current sample was 0.92.
Household Chaos.
The Confusion, Hubbub, and Order Scale (CHAOS; Matheny et al., 1995) was used to measure the degree of a chaotic home environment and child environmental confusion. The CHAOS consists of 15 items such as “No matter what our family plans, it usually doesn’t seem to work out.” The participants responded to each statement utilizing a four-point Likert scale ranging from 1 = “Very much like your own home” to 4 = “Not at all like your own home” to indicate how much the statement reflects their home life. Total scores were reverse coded and calculated by summing the responses, with higher scores indicating higher levels of home chaos. The CHAOS has been validated and broadly used in assessing the home environment of children and adolescents (Evans et al. 2005; Jaffee et al. 2012), with strong reported retest reliability (0.79) in the sample of 123 families (Matheny et al., 1995). The Cronbach’s alpha for the current sample was 0.85.
2.2.2. Dependent Variables
Parent Fast-food Consumption.
To assess the frequency in which parents consumed fast-food and restaurant food, a mean of two items from a self-report nutrition questionnaire adapted from the Harvard Nurses’ Health Study was used (Varraso et al., 2007). These items have been validated and used by the Center for Disease Control (CDC) in the National Health and Nutrition Examination Survey Questionnaire. The items ask how often the parents “ate fast-food” and “ate out” the items were scored as: 0 = “never”, 1 = “<1/month”, 2 = “1–3/month”, 3 = “1/week”, 4 = “2–4/week”, 5 = “5–6/week”, 6 = “1/day”, and 7 = “2–3/day.”
Child Fast-food Consumption.
To assess the frequency in which children consumed fast-food, one item from a self-report food frequency questionnaire (FFQ) was used (Flood et al., 2014). The FFQ has been validated for use in child populations for measuring food consumption (Bell et al., 2013; Mubarik et al., 2018). The item asked parents to report the number of times per week (potential for multiple times per day) the child consumed a meal or snack “such as burgers, pizza, chicken or fries from places like McDonalds, Burger King, Pizza Hut, KFC, Popeyes or local take-away food places?”
2.3. Data Analysis Plan
SPSS version 28 (IBM Corp., Armonk, NY) was used for all data cleaning and analysis. Missing data was handled using case wise exclusion for each variable used in the analysis. Bivariate Pearson correlations, t-tests, and analysis of variance (ANOVA) were computed to examine associations between variables of interest and demographic information to identify the potential for necessary covariates. The demographic variables that were significantly correlated with the variables of interest and had theoretical support were included as covariates in the models.
Three multiple linear regression models were conducted to separately examine the associations between parent perceived stress, parenting stress, and household chaos with fast-food consumption among the parents. Four multiple linear regression models were conducted to separately examine the associations between parent perceived stress, parenting stress, chaos, and parent fast-food consumption with child fast-food consumption. To correct for multiple comparisons, the Bonferroni method was used, and new alpha level was set to 0.007. The Bonferroni correction was used at the model p level (i.e., if the total models did not meet this threshold, we did not look at the terms). Finally, two multiple linear regression models were conducted to assess the strongest association with fast-food consumption (parent and child, respectively) when all variables were included together in the same model. Upon consideration of dependent variable distributions and model metrics, multiple linear regressions were conducted, model assumptions for linear regression were met by assessing model residuals for each dependent variable, and both variables followed a normal distribution. Although the child fast-food intake is a count variable, the data followed a normal distribution. For the parent fast-food consumption variable, although the initial two items were ordinal variables, we average them to get our final score. In doing so, we have some values that are decimals (e.g., 1.5). The data presented no issues or violations with any assumptions of normality necessary for regression analyses. Additionally, despite the independent variables being correlated to each other, there were no issues with multicollinearity in any of the regression models; all variance inflation factors (VIF) were below 2.5.
3. Results
The sample comprised 234 parent and child dyads, parents aged 20 to 49 years (mean age 34.3; SD=5.7), 46.6% were non-Hispanic White, 23.9% were Non-Hispanic Black, 25.2% were Hispanic, and 4.3% identified as other. Approximately 94% of the sample were biological mothers of the child, 60.3% had a college degree or higher, and 65.8% were married or living with a life-partner. The average number of adults living in the household was 2.00 (SD = 0.68), ranging from 1 to 5. The sample enrolled prior to March 2020 and during the coronavirus pandemic until early 2022 were not significantly different on demographic, predictor and outcomes variables. For more information about the sample, including child demographics, see Table 1.
Table 1.
Characteristics of Participants
| Variable (N = 234) | Mean (SD) or N (%) |
|---|---|
| Parent Age (years) | 34.33 (5.74) |
| Parent Relation to Child | |
| Biological Mother | 218 (93.2%) |
| Parent Race/Ethnicity | |
| Non-Hispanic White | 109 (46.6%) |
| Non-Hispanic Black | 56 (23.9%) |
| Hispanic | 59 (25.2%) |
| Other | 10 (4.3%) |
| Relative Poverty (based on location and household size) | |
| At or Below Poverty Line | 49 (20.9%) |
| Parent Education | |
| High School/GED or less | 27 (11.5%) |
| Some College/Tech or Trade School | 66 (28.2%) |
| College Degree or higher | 141 (60.3%) |
| Parent BMI (kg/m2) | 34.76 (6.74) |
| Parent Marital Status | |
| Married/Remarried/Life Partner | 154 (65.8%) |
| Single/Divorced/Separated | 80 (34.2%) |
| Number of adults in household | 2.00 (0.68) |
| Parent Perceived Stress | 24.62 (8.21) |
| Parenting Stress | 78.77 (19.04) |
| Household Chaos | 31.76 (8.37) |
| Parent Fast-food | 3.63 (2.53) |
| Child Sex | |
| Male | 119 (50.9%) |
| Child BMI Percentile | 58.61 (35.67) |
| Child Fast-food | 1.00 (1.03) |
3.1. Bivariate Analyses
There were no statistically significant associations between sample characteristics and parent fast-food consumption at the p< 0.05 level, except for parent age (r = −.15, p < 0.05) and for the number of adults living in the household (r = −.03, p <0.05). There were no statistically significant associations between sample characteristics and child fast-food consumptions at the p< 0.05 level, except child age (r = .23 , p < 0.01).
Parent perceived stress was significantly correlated with parenting stress (PSI) (r = .62, p < .01) and with household chaos (r = .60, p < 0.01). Parent fast-food consumption was significantly and positively correlated with parent perceived stress (r = .15, p < 0.05), parenting stress (r = .23, p < 0.01), and household chaos (r = .18, p < 0.01). Furthermore, there was a significant and positive correlation between parent fast-food consumption and child fast-food consumption (r = .45, p < 0.01). See Table 2 for association between demographics and variables of interest.
Table 2.
Pearson Correlation
| Variable | P. Age | P. BMI | C. Age | C. BMI% | Adults | PSS | PSI | Chaos | P. Fast-food |
|---|---|---|---|---|---|---|---|---|---|
| 1. Parent Age | -- | ||||||||
| 2. Parent BMI | −0.13 | -- | |||||||
| 3. Child age (months) | 0.19 ** | −0.04 | -- | ||||||
| 4. Child BMI % | −0.13 | 0.14 * | 0.74 ** | -- | |||||
| 5. adults in house | 0.07 | 0.00 | −0.01 | 0.03 | -- | ||||
| 5. PSS | 0.01 | −0.04 | 0.08 | −0.04 | 0.14 * | -- | |||
| 6. PSI | −0.01 | −0.05 | 0.07 | −0.02 | 0.08 | 0.62 ** | -- | ||
| 7. Chaos | 0.16 * | −0.04 | 0.06 | 0.00 | 0.18 ** | 0.60 ** | 0.55 ** | -- | |
| 8. Parent Fast-food | −0.13* | −0.02 | 0.06 | 0.01 | −0.13* | 0.15 * | 0.23 ** | 0.18 ** | -- |
| 9. Child Fast-food | −0.05 | 0.03 | 0.23 ** | −0.10 | −0.11 | 0.10 | 0.12 | 0.05 | 0.45 ** |
p <0.01
p < 0.05
Based on correlation results with the current sample and prior theoretical support, parent age, parent BMI, marital status, and the number of adults living in the household were included as covariates for the models with parent fast-food consumption as the dependent variable. Child age, child BMI, parent marital status, and the number of adults living in the household were included as covariates in models with the child fast-food consumption as the dependent variable.
3.2. Significant associations between parent perceived stress, parenting stress, household chaos, and parent fast-food consumption
As shown in Table 3, after accounting for covariates, parent perceived stress was significantly and positively associated with parent fast-food consumption (R2 = 0.10; β = 0.21, p < 0.01). This was also the case for parenting stress (R2 = 0.13; β = 0.26, p < 0.01) and CHAOS (R2 = 0.12; β = 0.25, p < 0.01) in the association with parent fast-food consumption. In the final model, we included all three independent variables (R2 = 0.14, F (7, 226) = 5.35, p < 0.01), and, of the four covariates and three independent variables, parent marital status (β = 0.21, p < 0.01) and parenting stress (β = 0.17, p < 0.05) were significant. Figure 1 illustrates the association between parenting stress and parent fast-food consumption controlling for all other variables.
Table 3.
Four regression models with parent fast-food consumption as the dependent variable.
| R2 = 0.10** | R2 = 0.13** | R2 = 0.12** | R2 = 0.14 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE B | B | SE B | B | SE B | B | SE B | |||||
| Primary Outcome(s) | PSS | 0.07** | 0.02 | PSI | 0.03** | 0.01 | CHAOS | 0.08** | 0.02 | PSS | 0.01 | 0.03 |
| PSI | 0.02* | 0.01 | ||||||||||
| CHAOS | 0.04 | 0.03 | ||||||||||
| Covariates | Parent BMI | −0.02 | 0.02 | −0.01 | 0.02 | −0.02 | 0.02 | −0.01 | 0.02 | |||
| Parent age | −0.04 | 0.03 | −0.04 | 0.03 | −0.06* | 0.03 | −0.05 | 0.03 | ||||
| Parent Marital Status | 1.21** | 0.25 | 1.10** | 0.36 | 1.08** | 0.36 | 1.14** | 0.36 | ||||
| Adults in the home | −0.28 | 0.25 | −0.27 | 0.25 | −0.35 | 0.25 | −0.33 | 0.25 | ||||
p<0.05
p<.01
Note: The first three models have the independent variable of interest entered independently. The last model has all three independent variables entered together with parenting stress significantly associated with parent fast-food consumption after controlling for parent age, parent BMI, parent marital status, and number of adults in the household.
Figure 1. Significant association between parenting stress and parent fast-food consumption.
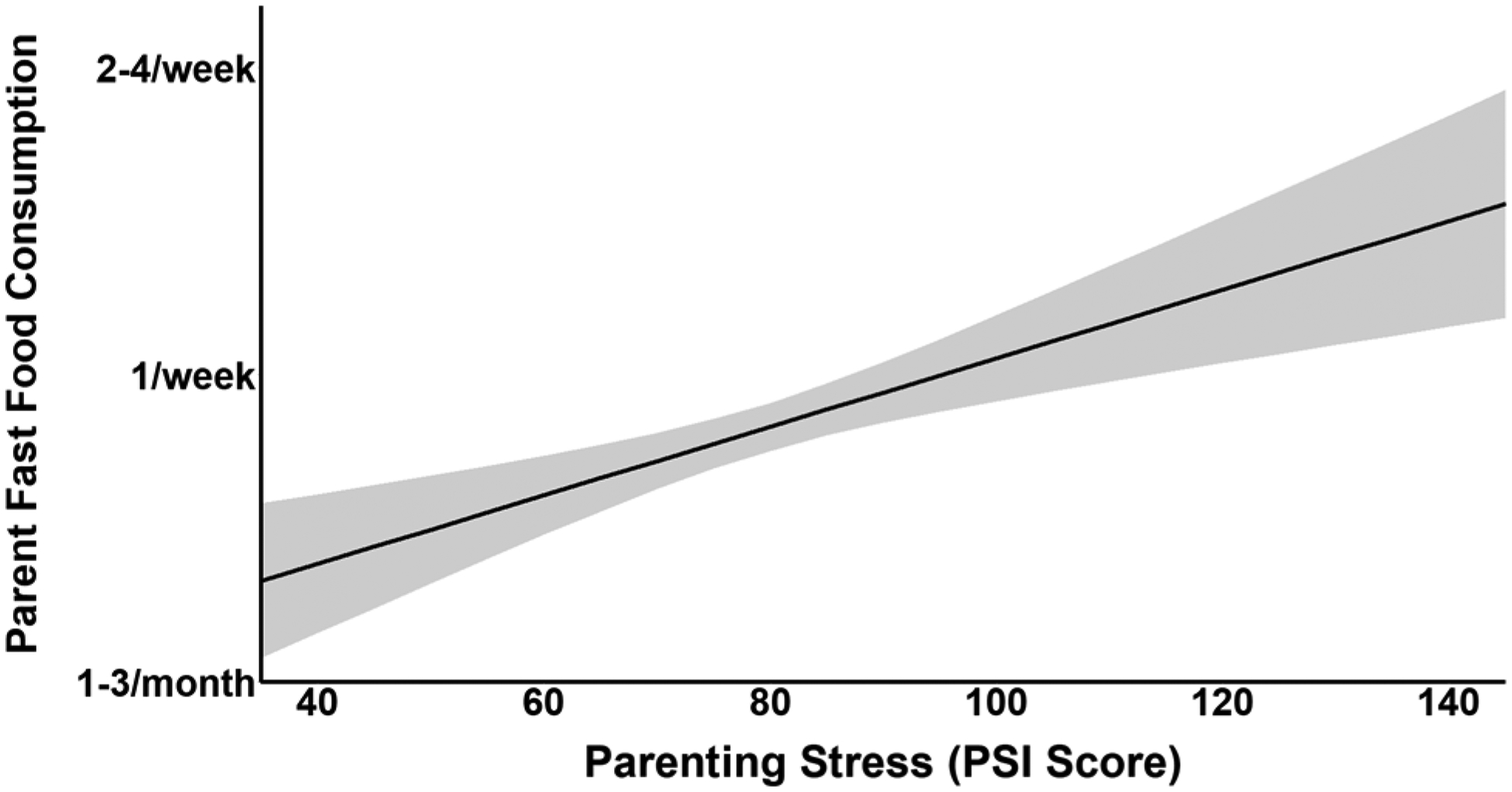
Note: This figure illustrates the final model in which parenting stress as the independent variable was significantly associated with parent fast-food consumption (R2 = 0.14, F (7,226) = 5.35, p < 0.01; β = 0.17, p < 0.05) after controlling for parent age, parent BMI, parent marital status, and number of adults in the household. The shaded gray area is the standard error of the model coefficient.
3.3. Significant associations between parent stress and child fast-food consumption
As shown in Table 4, after accounting for covariates, parent perceived stress was significantly positively associated with child fast-food consumption (R2 = 0.14, F (5, 228) = 7.55, p < 0.01; β = 0.21, β = 0.15, p < 0.05). This was also the case for parenting stress (R2 = 0.14, F (5, 228) = 7.39, p < 0.01; β = 0.14, p < 0.05) and parent fast-food consumption (R2 = 0.27, F (5, 228) = 17.16, p < 0.01; β = 0.40, p < 0.01) in the association with child fast-food consumption. Household chaos was not significantly associated with child fast-food consumption after controlling for covariates. The final model was significant (R2 = 0.28, F (8, 225) = 10.98, p < 0.01), and, of the four covariates and four independent variables, child age (β = 0.23, p < 0.01), parent marital status (β = 0.18, p < 0.01) and parent fast-food consumption (β = 0.39, p < 0.01) were significant. Figure 2 illustrates the association between parenting fast-food consumption and child fast-food consumption controlling for all other variables.
Table 4.
Four regression models with child fast-food consumption as the dependent variable.
| R2 = 0.14** | R2 = 0.14** | R2 = 0.27** | R2 = 0.28** | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE B | B | SE B | B | SE B | B | SE B | |||||
| Primary Outcome(s) | PSS | 0.02* | 0.01 | PSI | 0.01* | <0.01 | Parent Fast-Food | 0.16** | 0.02 | PSS | 0.01 | 0.01 |
| PSI | <0.01 | <0.01 | ||||||||||
| CHAOS | −0.01 | 0.01 | ||||||||||
| Parent FF | 0.16** | 0.03 | ||||||||||
| Covariates | Child BMI | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | |||
| Child age | 0.02** | 0.01 | 0.02** | 0.01 | 0.02** | 0.01 | 0.02* | 0.01 | ||||
| Parent Marital Status | 0.58** | 0.15 | 0.54** | 0.15 | 0.35* | 0.14 | 0.38** | 0.14 | ||||
| Adults in the home | 0.02 | 0.01 | −0.06 | 0.10 | −0.01 | 0.09 | −0.01 | 0.09 | ||||
p<0.05
p<.01
Note: The first three models have the independent variable of interest entered independently, the model with chaos as the independent variable was not significant and therefore not included. The last model has all four independent variables entered together with parenting fast-food consumption significantly associated with child fast-food consumption after controlling for child age, child BMI, parent marital status, and number of adults in the household.
Figure 2. Significant association between parent fast-food consumption and child fast-food consumption.
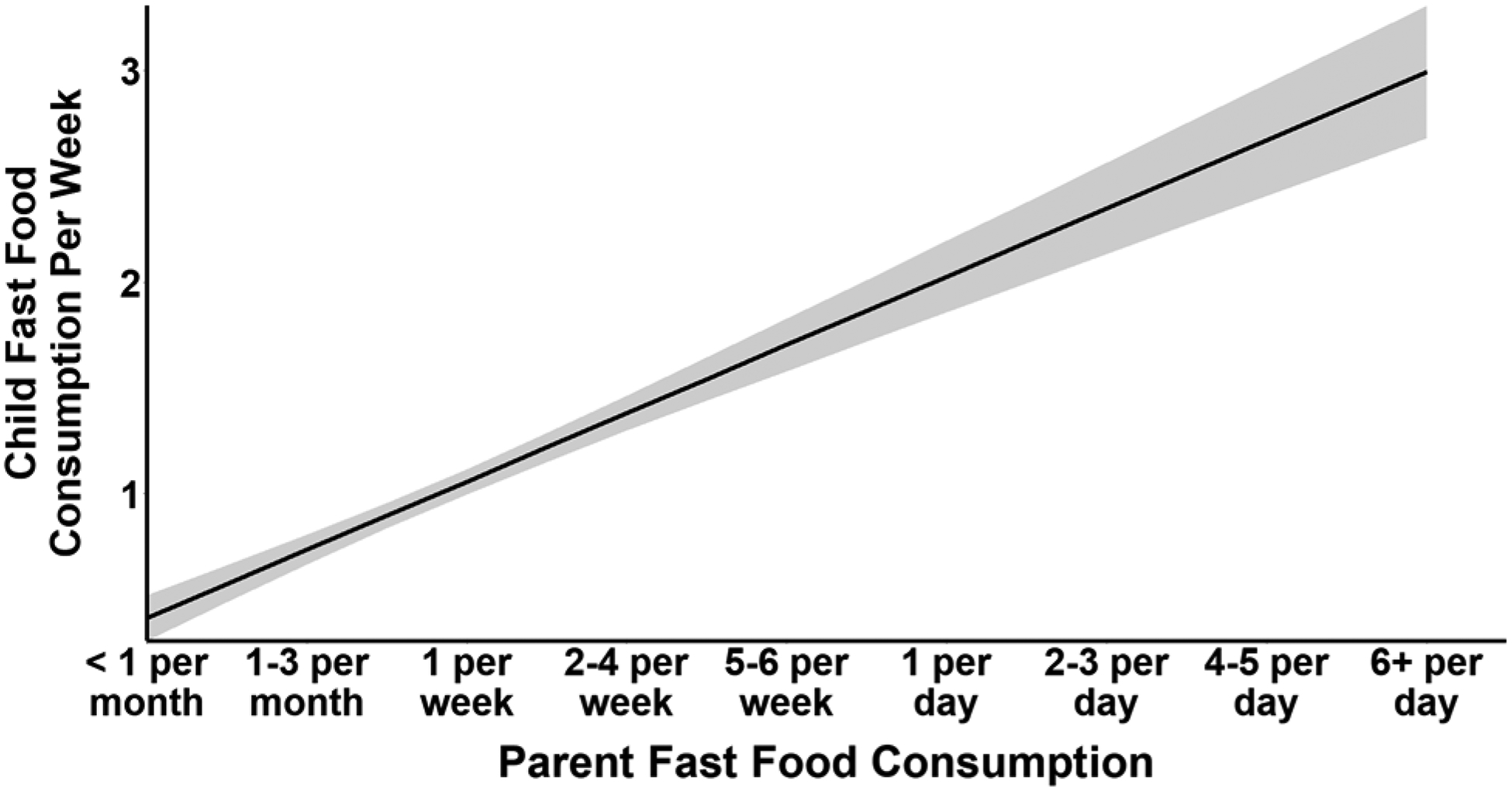
Note: This figure illustrates the model with parent fast-food consumption as the independent variable was significantly associated with child fast-food consumption (R2 = 0.28, F (8,225) = 10.98, p < 0.01; β = 0.39, p < 0.01) after controlling for child age, child BMI, parent marital status, and number of adults in the household. The shaded gray area is the standard error of the model coefficient.
4. Discussion
This study included a large group of community parent-young child dyads and uniquely compared the association of parent perceived stress, parenting stress and household chaos with parent and child fast-food consumption. While previous work has assessed parent stressors such as work, economic hardship and marital problems and association with fast-food intake, no previous research included each of the constructs of parent stress, parenting stress and household chaos. As hypothesized, we found parent perceived stress was significantly associated with both parenting stress and household chaos. Interestingly, while each of these measures were also significantly positively associated with parent fast-food consumption, only parent perceived stress, parenting stress, and parent fast-food consumption, but not household chaos, were significantly associated with child fast-food consumption when assessed separately in regression models. In final models inclusive of these signfiicant predictor variables, we found parenting stress was associated with parent fast-food consumption beyond what was explained by parent perceived stress and household chaos, and parent fast-food consumption was associated with child fast-food consumption beyond what was explained by parent perceived stress and parenting stress. These findings suggest that household chaos maybe less influential in impacting young childrens’ fast-food intake than parenting stress and parent fast-food intake. Of course, parent fast-food intake which is a key contributor to child fast-food intake was influenced by all three stress predictors. Thus, current findings suggest that targeting parent and parenting stress as well as household chaos with parent stress reduction interventions could have a positive impact on fast-food intake of parents and children.
Results of the present study provide a novel perspective on the distinct roles parent stress and parenting stress perform in parents’ decision-making process regarding fast food consumption and providing it to their children. Although previous work has documented the association between stress and fast-food consumption, parenting-specific stress has not been well-explored. For example, higher work-life stress was associated with higher fast-food consumption among U.S. parents, but the study did not assess parenting stress or child fast-food consumption (Bauer et al., 2012). Additionally, much of the prior work has lacked nutritional data from parent- child dyads. Previously, in a small qualitative study of 12 Norwegian families, Alm and Olsen (2017) found that on days when parents reported time stress (constraints on their time), they would typically serve convenience foods to the family for dinner. However, convenience food rarely included fast-food or restaurant take-out, they usually consisted of easily prepared fish and vegetables (Alm & Olsen, 2017). This may be a cultural difference between Norwegian and American families and the public opinion of fast-food being much more negative in Norway. Notably, this earlier work did not separately evaluate parenting stress, instead measuring concepts such as work stress or time stress. Current results support the importance of measuring multiple facets of life stress, including stress unique to parenting as well as household chaos. Although parenting stress was significantly correlated with parent perceived stress in the present study, the two constructs varied in their associations with other variables. Parents experiencing higher parenting stress, potentially due to child negative emotional reactivity, may be using fast-food as a soothing mechanism. Stifter and colleagues (2011) found that mothers who used food to soothe rated themselves lower in parenting self-efficacy and their children higher in temperamental negativity. This previous work would support the notion that focusing on adaptive stress coping and alternate self-soothing practices could improve the nutritional intake of their young children. Interventions that incorporate the theory of planned behavior could identify and improve learning and use of specific adaptive psychosocial skills for stress coping and also work towards healthy nutritional goals for the family.
We found a significant association between parent fast-food consumption and child fast-food consumption, which supported our second hypothesis. Prior literature suggests children, especially young children, eat similar food to their parents (Birch & Anzman, 2010). Preschool aged children are a particularly important demographic to capture because this is a critical age when children begin to develop eating habits and food preferences, largely shaped by foods they are exposed to at this age (Benton, 2004; Beckerman, et al., 2017). Parks and colleagues (2012) also found a direct association between parent-perceived stress and child fast-food consumption, but they did not test whether parent fast-food consumption may account for the association between parent stress and child fast-food consumption.
We also found significant associations between marital status and fast-food consumption, suggesting that two-parent households (married, remarried, or life-partner) consumed less fast-food for the parents and the children. Interestingly, two-parent households were also associated with great perceived stress and household chaos, but not greater parenting stress. This may suggest that although two-parent households may report greater overall parent stress and household chaos, two parents in a family may provide greater parenting stress buffering that in turn may serve as a protective factor specifically related to lower fast-food consumption. In a recent systematic review, Duriancik and Goff (2019) found greater risk of obesity in children from single parent households, hypothesizing that higher time demands for household responsibilities relative to dual parent households led to fewer homecooked and shared family meals. Furthermore, understanding the home environmental factors that are predictive of fast-food consumption may help tailor interventions to be relevant and acceptable among the most at-risk family groups. Daniels and Glorieux (2015) found that older, lower-educated, non-working and traditional nuclear households spent a larger portion of their food budget on ‘shortcut’ ingredients. Future research may explore how to group fast-food items with convenience “shortcut” foods and at-home processed foods.
The current findings contribute to an emerging literature in support of early childhood interventions for the development of healthy eating behaviors, with consensus on the importance of family-based programs for long-lasting healthy weight maintenance (Institute of Medicine, 2011). Although there is a well-established literature on the need of early interventions in the development of healthy eating behaviors, this literature rarely includes parent stress and parenting stress management as a component of early interventions for health eating behaviors. There is little research on incorporating parent factors, such as parent stress, parenting stress, and household chaos, to address self-regulation and decisions of healthy food choices for parents and their young children. A recent community-based weight loss intervention in mothers with BMIs in the overweight range (Chang et al., 2014) found that the efficacy of the intervention on reducing fast-food intake was mediated by perceived stress, suggesting that reducing parent perceived stress may be key to reducing fast-food intake (Chang et al., 2020). In a preliminary intervention study, we found that a novel mindfulness-based parent stress reduction intervention that targeted stress reduction and increases in healthy behavioral food choices for the parent and their young families was associated with improved child BMI outcomes (Jastreboff et al., 2018). Such programs that target both stress reduction combined with the need for healthy behavioral food choices, in addition to healthy nutrition and physical activity psychoeducation, could be of benefit in lowering fast-food consumption in both the parent and their young children.
Results from the present study should be interpreted considering certain limitations. First, a cross-sectional design does not permit us to draw any causal inferences, and we cannot distinguish between confounding and partial mediation in the model adjusted for all variables of interest. Second, this study only assessed fast-food consumption, and did not investigate other potentially problematic nutritional behaviors, such as frequent consumption of low-nutrient, highly processed foods at home. Parents may be preparing frozen processed foods at home that may not be captured in the current data. However, prior research has documented the health consequences associated with frequent consumption of fast-food (Rosenheck, 2008), suggesting that even altering this specific aspect of parents and their young child’s diets could have an impact on their health. Third, considering the potential limitation of using 1–2 item measurements of fast-food intake, we also acknowledge the need for broader metrics for fast-food measures (i.e., multiple measures of items in an instrument). Fourth, the sample only included parents with a BMI greater than 27 kg/m2, and these findings may not be generalizable to populations with lower BMIs. And lastly, our study included only one child per family and was comprised of mostly biological mothers to the child. Future work should examine the relationships between specific stressors and fast-food intake amongst other caregivers.
In conclusion, young children are often not in control of their meal selection and rely on their caretakers to provide meals, which are typically alike to meals consumed by the caregiver. Fast-food consumption typically comprises of high-fat, high-sugar or high-calorie highly processed foods (Powell & Nguyen, 2013). Frequent intake of these foods may place consumers at greater risk of obesity, weight gain, and other health issues, possibly creating life-long consequences for children. A central and concerning finding from this study suggests that parent perceived stress, parenting stress, and household chaos are each associated with, and may be contributing to, higher consumption of fast-food for young children. Therefore, addressing parenting stress and behavioral food choices for the parent and the family, as well as the link among parent stress, chaos, and parenting stress, could increase healthy food intake and reduce fast-food intake among parents and their young children to improve healthy nutrition and reduced obesity risk in families.
Highlights.
Perceived stress and parenting stress were associated with child fast-food consumption
Parent fast-food consumption was associated with child fast-food consumption
Parenting stress was associated with parent fast-food consumption
Current findings highlight a role for parent stress in child fast-food consumption
Funding:
NIH/NIDDK Grant # 5R01DK117651 (PIs: R.S., A.M.J., & W.K.S.) NIH/NCATS Grant # 5TL1TR001864 (PIs: L.C., R.S. & E.S.)
Conflicts of interest/Competing Interests:
Financial interests: Author (A.M.J), has received research support from American Diabetes Association, Novo Nordisk, and Eli Lilly. No other authors have any relevant financial or non-financial interest to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Institutional Review Board (IRB) Human Investigation Committee #2000023271) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate: All participants read and signed an informed consent form after discussing the study with trained research assistants.
Consent for publication: All participant read and signed a consent form allowing us to publish their de-identified aggregated data.
Declaration of Interest
The authors have no other relevant financial or non-financial interest to declare.
Availability of data and material:
The data is part of a large ongoing NIH-funded clinical trial. At the completion of the clinical trial, requests for data sharing can be submitting to the PI (Rajita Sinha)
References
- Abidin RR (1995). Manual for the parenting stress index. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Alm S, & Olsen SO (2017). Coping with time pressure and stress: consequences for families’ food consumption. Journal of consumer policy, 40(1), 105–123. [Google Scholar]
- Anderson SE, & Whitaker RC (2010). Household routines and obesity in US preschool-aged children. Pediatrics, 125(3), 420–428. [DOI] [PubMed] [Google Scholar]
- Bahreynian M, Qorbani M, Khaniabadi BM, Motlagh ME, Safari O, Asayesh H, & Kelishadi R (2017). Association between obesity and parental weight status in children and adolescents. Journal of clinical research in pediatric endocrinology, 9(2), 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baskind MJ, Taveras EM, Gerber MW, Fiechtner L, Horan C, & Sharifi M (2019). Parent-perceived stress and its association with children’s weight and obesity-related behaviors. Preventing Chronic Disease, 16: E39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates CR, Buscemi J, Nicholson LM, Cory M, Jagpal A, & Bohnert AM (2018). Links between the organization of the family home environment and child obesity: A systematic review. Obesity Reviews, 19(5), 716–727. [DOI] [PubMed] [Google Scholar]
- Bauer KW, Hearst MO, Escoto K, Berge JM, & Neumark-Sztainer D (2012). Parental employment and work family stress: Associations with family food environments. Social Science & Medicine, 75(3), 496–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckerman JP, Alike Q, Lovin E, Tamez M, & Mattei J (2017). The development and public health implications of food preferences in children. Frontiers in nutrition, 4, 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell LK, Golley RK, & Magarey AM (2013). Short tools to assess young children’s dietary intake: a systematic review focusing on application to dietary index research. Journal of obesity, 709626. doi: 10.1155/2013/709626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benton D (2004). Role of parents in the determination of the food preferences of children and the development of obesity. International Journal of Obesity, 28(7), 858–869. [DOI] [PubMed] [Google Scholar]
- Beshara M, Hutchinson A, & Wilson C (2010). Preparing meals under time stress. The experience of working mothers. Appetite, 55(3), 695–700. [DOI] [PubMed] [Google Scholar]
- Birch LL, & Anzman SL (2010). Learning to eat in an obesogenic environment: A developmental systems perspective on childhood obesity. Child Development Perspectives, 4(2), 138–143. [Google Scholar]
- Block JP, He Y, Zaslavsky AM, Ding L, & Ayanian JZ (2009). Psychosocial stress and change in weight among US adults. American Journal of Epidemiology, 170(2), 181–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan L, Walkley J, Wilks R, Fraser SF, & Greenway K (2013). Physiological and behavioural outcomes of a randomized controlled trial of a cognitive behavioural lifestyle intervention for overweight and obese adolescents. Obesity research & clinical practice, 7(1), e23–41. 10.1016/j.orcp.2012.02.0102012.02.010 [DOI] [PubMed] [Google Scholar]
- Burgess E, Hassmén P, Welvaert M, & Pumpa KL (2017). Behavioural treatment strategies improve adherence to lifestyle intervention programmes in adults with obesity: A systematic review and meta-analysis. Clinical Obesity, 7, 105–114. 10.1111/cob.12180 [DOI] [PubMed] [Google Scholar]
- Chang MW, Brown R, & Wegener DT (2020). Perceived Stress Can Mediate the Associations between a Lifestyle Intervention and Fat and Fast-Food Intakes. Nutrients, 12(12), 3606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang MW, Nitzke S, Brown R, & Resnicow K (2014). A community-based prevention of weight gain intervention (Mothers In Motion) among young low-income overweight and obese mothers: design and rationale. BMC public health, 14(1), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, & Janicki- Deverts DENISE (2012). Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. Journal of Applied Social Psychology, 42(6), 1320–1334. [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 385–396. [PubMed] [Google Scholar]
- Cooke L (2007). The importance of exposure for healthy eating in childhood: A review. Journal of Human Nutrition and Dietetics, 20(4), 294–301. [DOI] [PubMed] [Google Scholar]
- Daniels S, & Glorieux I (2015). Convenience, food and family lives. A socio-typological study of household food expenditures in 21st-century Belgium. Appetite, 94, 54–61. [DOI] [PubMed] [Google Scholar]
- Duriancik DM, & Goff CR (2019). Children of single-parent households are at a higher risk of obesity: A systematic review. Journal of Child Health Care, 23(3), 358–369. [DOI] [PubMed] [Google Scholar]
- Evans GW, Gonnella C, Marcynyszyn LA, Gentile L, & Salpekar N (2005). The role of chaos in poverty and children’s socioemotional adjustment. Psychological science, 16(7), 560–565. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, & Johnson CL (2002). Prevalence and trends in obesity among US adults, 1999–2000. JAMA, 288(14), 1723–1727. [DOI] [PubMed] [Google Scholar]
- Flood VM, Wen LM, Hardy LL, Rissel C, Simpson JM, & Baur LA (2014). Reliability and validity of a short FFQ for assessing the dietary habits of 2–5-year-old children, Sydney, Australia. Public health nutrition, 17(3), 498–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman DS, Mei Z, Srinivasan SR, Berenson GS, & Dietz WH (2007). Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. The Journal of Pediatrics, 150(1), 12–17. [DOI] [PubMed] [Google Scholar]
- Fryar CD, & Ervin RB (2013). Caloric intake from fast-food among adults: United States, 2007–2010 (No. 114). US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. [Google Scholar]
- Gouveia MJ, Canavarro MC, & Moreira H (2019). How can mindful parenting be related to emotional eating and overeating in childhood and adolescence? The mediating role of parenting stress and parental child-feeding practices. Appetite, 138, 102–114. [DOI] [PubMed] [Google Scholar]
- Gundersen C, Lohman BJ, Garasky S, Stewart S, & Eisenmann J (2008). Food security, maternal stressors, and overweight among low-income US children: results from the National Health and Nutrition Examination Survey (1999–2002). Pediatrics, 122(3), e529–e540. [DOI] [PubMed] [Google Scholar]
- Haskett ME, Ahern LS, Ward CS, & Allaire JC (2006). Factor structure and validity of the parenting stress index-short form. Journal of Clinical Child & Adolescent Psychology, 35(2), 302–312. [DOI] [PubMed] [Google Scholar]
- IBM Corp. (2020). IBM SPSS statistics for windows, version 27.0. Armonk, NY: IBM Corp. [Google Scholar]
- Institute of Medicine. (2011). Early childhood obesity prevention policies. Washington, DC: The National Academies Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jafee SR, Hanscombe KB, Haworth CMA, Davis OSP, & Plomin R (2012). Chaotic homes and children’s disruptive behavior. Psychological Science, 239(6), 643–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang M, Brown R, & Vang PY (2021). The Relationships Between Parental Stress, Home Food Environment, and Child Diet Patterns in Families of Preschool Children. American Journal of Health Promotion, 35(1), 131–139. 10.1177/0890117120929541 [DOI] [PubMed] [Google Scholar]
- Jastreboff AM, Chaplin TM, Finnie S, Savoye M, Stults-Kolehmainen M, Silverman WK, & Sinha R (2018). Preventing childhood obesity through a mindfulness-based parent stress intervention: A randomized pilot study. The Journal of Pediatrics, 202, 136–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson AO (2015). Test Review: Parenting Stress Index, Fourth Edition (PSI-4). Journal of Psychoeducational Assessment, 33(7), 698–702. 10.1177/0734282914556069 [DOI] [Google Scholar]
- Keane E, Layte R, Harrington J, Kearney PM, & Perry IJ (2012). Measured parental weight status and familial socio-economic status correlates with childhood overweight and obesity at age 9. PloS one, 7(8), e43503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khaled K, Tsofliou F, Hundley V, Helmreich R, & Almilaji O (2020). Perceived stress and diet quality in women of reproductive age: A systematic review and meta-analysis. Nutrition Journal, 19(1), 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS, & Folkman S (1984). Stress, appraisal, and coping. Springer publishing company. [Google Scholar]
- Lee SJ, Gopalan G, & Harrington D (2016). Validation of the parenting stress index–short form with minority caregivers. Research on Social Work Practice, 26(4), 429–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masarik AS, & Conger RD (2017). Stress and child development: A review of the Family Stress Model. Current Opinion in Psychology, 13, 85–90. [DOI] [PubMed] [Google Scholar]
- Mason TB, O’Connor SG, Schembre SM, Huh J, Chu D, & Dunton GF (2019). Momentary affect, stress coping, and food intake in mother–child dyads. Health Psychology, 38(3), 238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheny AP Jr, Wachs TD, Ludwig JL, & Phillips K (1995). Bringing order out of chaos: Psychometric characteristics of the confusion, hubbub, and order scale. Journal of Applied Developmental Psychology, 16(3), 429–444. [Google Scholar]
- Mozaffarian D, Hao T, Rimm EB, Willett WC, & Hu FB (2011). Changes in diet and lifestyle and long-term weight gain in women and men. New England Journal of Medicine, 364(25), 2392–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mubarik F, Warren J, Abrahamse M, Brown JE, & Muhardi L (2018). Methodological considerations for the design of food frequency questionnaires for toddlers. Pakistan Journal of Nutrition, 17, 102–115. doi: 10.3923/pjn.2018.102.115 [DOI] [Google Scholar]
- National Health and Nutrition Examination Survey (NHANES). 2009 – 2010 Data Documentation, Codebook, and Frequencies for NHANES Physical Activity Items. 2011, September: http://www.cdc.gov/nchs/nhanes/nhanes2009-2010/PAQ_F.htm#PAD590.
- Park H, & Walton-Moss B (2012). Parenting style, parenting stress, and children’s health-related behaviors. Journal of Developmental & Behavioral Pediatrics, 33(6), 495–503. [DOI] [PubMed] [Google Scholar]
- Parks EP, Kumanyika S, Moore RH, Stettler N, Wrotniak BH, & Kazak A (2012). Influence of stress in parents on child obesity and related behaviors. Pediatrics, 130(5), e1096–e1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LM, & Nguyen BT (2013). Fast-food and full-service restaurant consumption among children and adolescents: effect on energy, beverage, and nutrient intake. JAMA pediatrics, 167(1), 14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenheck R (2008). Fast-food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk. Obesity reviews, 9(6), 535–547. [DOI] [PubMed] [Google Scholar]
- Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, & Bhadoria AS (2015). Childhood obesity: causes and consequences. Journal of Family Medicine and Primary Care, 4(2), 187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savoye M, Nowicka P, Shaw M, Yu S, Dziura J, Chavent G, O’Malley G, Serrecchia JB, Tamborlane WV, & Caprio S (2011). Long-term results of an obesity program in an ethnically diverse pediatric population. Pediatrics, 127(3), 402–410. 10.1542/peds.2010-0697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler BR, Daundasekara SS, Hernandez DC, Dumenci L, Clark M, Fisher JO, & Miller AL (2020). Economic hardship and child intake of foods high in saturated fats and added sugars: the mediating role of parenting stress among high-risk families. Public Health Nutrition, 23(15), 2781–2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirley K, Rutfield R, Hall N, Fedor N, McCaughey VK, & Zajac K (2015). Combinations of obesity prevention strategies in US elementary schools: a critical review. The Journal of Primary Prevention, 36(1), 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soubry A, Murphy SK, Wang F, Huang Z, Vidal AC, Fuemmeler BF, … & Hoyo C (2015). Newborns of obese parents have altered DNA methylation patterns at imprinted genes. International Journal of Obesity, 39(4), 650–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stifter CA, Anzman-Frasca S, Birch LL, & Voegtline K (2011). Parent use of food to soothe infant/toddler distress and child weight status. An exploratory study. Appetite, 57(3), 693–699. [DOI] [PubMed] [Google Scholar]
- Wilson SM, & Sato AF (2014). Stress and pediatric obesity: what we know and where to go. Stress and Health, 30(2), 91–102. [DOI] [PubMed] [Google Scholar]
- van’t Riet J, Sijtsema SJ, Dagevos H, & De Bruijn GJ (2011). The importance of habits in eating behaviour. An overview and recommendations for future research. Appetite, 57(3), 585–596. [DOI] [PubMed] [Google Scholar]
- Varraso R, Fung TT, Barr RG, Hu FB, Willett W, & Camargo CA Jr (2007). Prospective study of dietary patterns and chronic obstructive pulmonary disease among US women. The American Journal of Clinical Nutrition, 86(2), 488–495. [DOI] [PMC free article] [PubMed] [Google Scholar]


