Abstract
This study aimed to examine the extent to which illness beliefs, coping styles, pain acceptance, pain catastrophizing, and psychological distress mediate the relationship between fibromyalgia symptoms and quality of life (QoL) in a female cohort diagnosed with Fibromyalgia (n = 151). Measures used included the Revised Fibromyalgia Impact Questionnaire, Carver Brief COPE scale, Chronic Pain Acceptance Questionnaire Revised, Pain Catastrophizing Scale, Brief Illness Perceptions Questionnaire, Depression and Anxiety Stress Scales, and European Health Interview Survey Quality of Life 8-item Index. Using structural equation modelling, the final model indicated that fibromyalgia symptom severity had a significant direct influence on illness perceptions and psychological distress. In turn, illness perceptions had a significant direct influence on maladaptive coping, pain catastrophizing, pain acceptance, and QoL. Pain catastrophizing and maladaptive coping influenced psychological distress, and in turn distress impacted QoL. Acceptance of pain was found to be influenced by maladaptive coping and in turn acceptance of pain influenced QoL.
Keywords: Fibromyalgia, Common sense model, Psychological distress, Quality of life
Fibromyalgia (FM) is a painful medical condition associated with poor treatment outcomes and quality of life (QoL) (Arnold et al., 2011; Choy et al., 2010; Clark et al., 2013; Skaer & Kwong, 2017). Compared to other pain-related illnesses, autoimmune disorders, and the general public, individuals with FM report higher psychological distress (Capraro et al., 2012; Lami et al., 2018; McInnis et al., 2014; Schaefer et al., 2016; Toussaint et al., 2019). Additionally, higher FM symptoms have been shown to relate to greater psychological distress (PD) and poorer QoL (De Souza Santos Berber et al., 2005; Lee et al., 2017; Schaefer et al., 2011; Toussaint et al., 2017).
FM-cohort studies have demonstrated that illness beliefs and coping strategies can significant impact psychological distress, functional impairment, and pain intensity (Alok et al., 2014; Boehm et al., 2011; Cui et al., 2009; Smith et al., 2009; Stuifbergen et al., 2006).
Given the significant individual and societal burdens associated with FM and the limited efficacy of current standard diagnosis and treatment (Chandran et al., 2012; Choy et al., 2010; Clark et al., 2013; Guymer et al., 2016; Skaer & Kwong, 2017; Vervoort et al., 2016; Walitt et al., 2015), further research is needed to understand the degree to which modifiable psychosocial mediators of adaption (such as acceptance, coping strategies, and pain catastrophizing) influence physical and mental health and QoL outcomes.
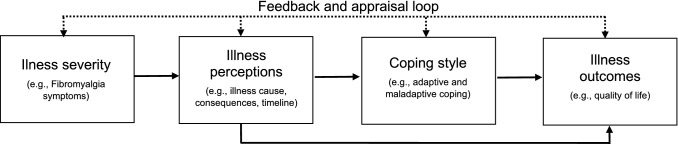
The Common Sense Model (CSM; Leventhal et al., 1980; See Fig. 1) is a well-established and valuable theoretical model that posits illness severity influences illness perceptions (e.g. beliefs about the cause, consequences). Additionally, illness perceptions act as a mediator between illness severity and illness outcomes (e.g. psychological distress and QoL) and influence the coping strategies utilized by individuals to manage the impact of their illness and perceptions on illness outcomes (Hagger & Orbell, 2003; Hagger et al., 2017). To date, substantial evidence supports the model across multiple chronic illness conditions (see Hagger & Orbell, 2003, for review); however, no research has utilized the CSM in a FM cohort.
Fig. 1.
The common sense model (Hagger & Orbell, 2003), adapted by Knowles et al. (2011)
Other psychological variables identified in the FM literature which may also be useful to extend the CSM include pain acceptance and pain catastrophizing. Research has demonstrated that greater pain acceptance (the willingness to live with pain without trying to change, avoid, or reduce it, McCracken, 1999) is associated with reduced psychological distress, while pain catastrophizing (the exaggerated and negative appraisal or actual or anticipated painful experiences) is associated with increased distress and pain-related disability, and poorer QoL in FM populations (Burckhardt et al., 1997; Edwards et al., 2006; Lami et al., 2018; Rodero et al., 2011).
The current literature suggests that despite strong evidence of associations between illness severity, illness perceptions, pain acceptance, pain catastrophizing, coping styles, psychological distress, and QoL in FM, no study to the authors’ knowledge has evaluated these psychosocial variables together in a FM cohort. Using structural equation modelling (SEM), the aim of the study was to extend the CSM to explore the potential interrelationships between these variables in a FM cohort. It was hypothesized that consistent with the posits of the CSM that illness perceptions, pain acceptance, pain catastrophizing, and coping styles would mediate the relationship between FM symptoms and patient-reported outcomes (psychological distress and QoL).
Methods
Participants
A total of 151 participants with a mean age of 45.98 years (SD = 10.57) completed a self-administered online questionnaire. Of the 151 participants, the majority of participants were married (39.07%) or single (23.18%), lived with a partner (60.26%) or alone (29.14%), lived in their own home (44.37%) or in private rental (38.41%), were on a pension (27.15%) or unemployed (37.75%).
On average, participants had experienced symptoms of FM for 11.58 years (SD = 10.75), with 58.90% having experienced fibromyalgia symptoms for more than 5 years. Seventy-seven per cent of participants reported taking medication to help manage the fibromyalgia symptoms. Comorbidity in the participant cohort was also high with 83.44% reported being diagnosed with another physical health condition, with the most common being arthritis (26.49%) and chronic fatigue syndrome (8.61%).
Measures
The Revised Fibromyalgia Impact Questionnaire (FIQ-R) (Bennett et al., 2009). The FIQ-R is a 21-item scale (zero to ten response format) used to measure the functional impact, the overall impact of symptoms, and the intensity of symptoms. An overall score (0–100) was obtained by weighting the subscale scores and summing them together with higher scores indicating a greater perceived impact of fibromyalgia symptoms. An error was made when administering the questionnaire, as participants were asked to rate their symptom severity from none to a lot instead of the individualized answers to the questionnaire. Cronbach alpha analysis indicated that the modified scale had strong internal consistency (0.89).
The Brief Illness Perception Questionnaire (BIPQ) (Broadbent et al., 2006). The BIPQ is an eight-item scale (zero to ten response format) used to measure cognitive and emotional representations of illness. Consistent with previous research to improve scale consistency Knowles et al. (2011), an exploratory actor analysis using Principal Axis Factoring method with an Oblimin rotation and Cronbach alpha with item-if-deleted analysis recommend the removal of the question “How well do you feel you understand your illness?” (item 7). The remove resulted in a 7-item scale (Cronbach alpha: 0.67) with an overall score obtained by adding all the items together (reversing items three and four). Total scores range from zero to 70 with higher scores indicating a more threatening view of illness.
The Brief Coping Operations Preference Enquiry (Brief COPE; Carver, 1997). The Brief COPE is a 28 item (zero to three response format) that assesses fourteen conceptually different coping response types. Consistent with recommendations by the scale author (Carver, 1997) and previous research (Knowles, et al., 2011), an exploratory factor analysis using the Principal Axis Factoring method with an Oblimin rotation and Cronbach alpha with item-if-deleted analysis was conducted on the scale. Review of the scree plot and pattern matrix suggested a two-factor structure solution. Consistent with previous research (Carver, 1997; Knowles et al., 2011; Knowles, Cook, & Tribbick, 2013), two subscales descriptors (i.e. maladaptive and adaptive coping styles) were used in the study. Maladaptive coping styles refer to items that had an adverse relationship with psychosocial outcomes. Maladaptive coping was composed of 9 items: “I’ve been saying to myself “this isn’t real””, “I’ve been using alcohol or other drugs to make myself feel better”, “I’ve been refusing to believe that it has happened”, “I’ve been saying things to let my unpleasant feeling escape”, “I’ve been using alcohol or other drugs to help me get through it”, “I’ve been criticizing myself”, “I’ve been giving up the attempt to cope”, “I’ve been doing something to think about it less, such as going to the movies, watching TV, reading, daydreaming, sleeping, or shopping”, and “I’ve been blaming myself for things that happened”. Adaptive coping styles refer to items that had a beneficial relationship with psychosocial outcomes and was comprised of 15 items: “I’ve been concentrating my efforts on doing something about the situation I’m in”, “I’ve been getting emotional support from others”, “I’ve been taking action to try and make the situation better”, “I’ve been getting help and advice from other people”, “I’ve been trying to see it in a different light, to make it seem more positive”, “I’ve been trying to come up with a strategy about what to do”, “I’ve been getting comfort and understanding from someone”, “I’ve been looking for something good in what is happening”, “I’ve been making jokes about it”, “I’ve been trying to find comfort in my religion or spiritual beliefs”, “I’ve been trying to get advice or help from other people about what to do”, “I’ve been learning to live with it”, “I’ve been thinking hard about what steps to take”, “I’ve been praying or meditating”, and “I’ve been making fun of the situation”. Factor analysis also suggested the removal of items 1, 6, 20, and 21. Each of the subscale scores is obtained by averaging the items, with higher scores indicating a greater engagement in maladaptive or adaptive coping styles. Maladaptive and adaptive coping were found to have strong internal consistencies (Cronbach alpha 0.75 and 0.86 respectively).
Chronic Pain Acceptance Questionnaire—Revised (CPAQ-R) (McCracken et al., 2004). The CPAQ-R is a 20-item scale (zero to six response format) used to measure acceptance of pain. An overall score is obtained by adding the items together. Total scores range from zero to 120 with higher scores indicating greater level of acceptance. Cronbach alpha analysis indicated the modified scale had acceptable internal consistency (0.73).
Pain Catastrophizing Scale (PCS) (Sullivan et al., 1995). The PCS is a 13-item scale (zero to four response format) used to measure the degree to which the participant engages in thoughts or feelings that may catastrophize their level of pain. An overall score is obtained by adding the items together. Total scores range from zero to 52 with higher scores indicating greater level of pain catastrophizing. Cronbach alpha analysis indicated that the modified scale had strong internal consistency (0.93).
Depression Anxiety Stress Scale (DASS) (Lovibond & Lovibond, 1996). The DASS is a 21-item scale (zero to three response format) used to measure stress, anxiety, and depression levels. An overall score is obtained by adding the items together and multiplying them by two. Total scores range from 0 to 126, with higher scores indicating greater psychological distress. Cronbach alpha analysis indicated that the modified scale had strong internal consistency (0.93).
The European Health Interview Survey-Quality of Life 8-item Index (EUR0HIS-QoL 8-item index) (Nosikov & Gudex, 2003; Schmidt et al., 2005). The EUROHIS-QoL is an eight-item scale (zero to five response format) used to measure QoL across psychological, physical, social, and environmental domains. An overall score is obtained by adding scores across the items together. Total scores range from eight to 40 with higher scores indicating better QoL. Cronbach alpha analysis indicated the modified scale had strong internal consistency (0.83).
Procedure
Participants were recruited through FM-related social media (e.g. Australian Fibromyalgia online Facebook forum) and were invited to complete a 20-min online survey. Inclusion criteria were being aged 18 years or older and having a diagnosis of Fibromyalgia. Research was approved by Swinburne University of Technology’s Human Research Ethics Committee (SUHREC). Informed consent was obtained from all research participants. Data were collected from 7 to 9 August 2018.
Statistical analyses
The data for the present research were analysed using IBM Statistical Package for Social Sciences (SPSS) Version 25. Preliminary data screening was conducted to ensure suitability of the data for further analysis. Analysis of missing values revealed that data were missing completely at random, Little's MCAR test = 7516.83 (8199), p > 0.05. There were 26 cases with missing values of over 30%, and these were removed due to the large sample size, consistent with recommendations by Tabachnick and Fiddell (2013), leaving 151 cases for the analysis. Expectation Maximization process was used to replace missing data in the remaining cases (Tabachnick & Fidell, 2013).
Exploratory analysis and visual inspection of the data indicated that all the study variables met the necessary assumptions for statistical analysis (e.g. normality, linearity). Correlational analyses were undertaken to compare the relationship between the study variables. A SEM was specified using the AMOS (Version 27) by an iterative process of adding pathways and removing variables that did not add significantly to the model’s fit. As recommended by Hu and Bentler (1999), pathways were added or removed based on inspection of standardized residuals, AMOS modification indices, the CSM, and prior research on psychosocial factors relating to FM, and a significant improvement in fit (Chi-square goodness of fit test [χ2] p > 0.05; Normed Chi square [χ2/N] = 1–3, Tucker–Lewis index [TLI] > 0.95, Steiger-Lind Root-Mean-Square Error of Approximation [RMSEA] < 0.08, and Standardized Root–Mean-Squared Residual [SRMR] < 0.06).
Results
As shown in Table 1 (descriptive and correlational analyses), greater FM symptom severity was associated significantly with poorer illness perceptions and QoL, less pain acceptance, and greater engagement in maladaptive coping, pain catastrophizing, and psychological distress. Poorer illness perceptions were associated significantly with less pain acceptance, greater engagement in maladaptive coping, pain catastrophizing and greater psychological distress, and poorer QoL. Adaptive coping was found only significantly relate to pain acceptance, suggesting that higher engagement in adaptive coping is associated with greater pain acceptance. In contrast, engagement in maladaptive coping was associated significantly with greater pain catastrophizing and psychological distress and poorer QoL. Higher pain acceptance was associated significantly with higher QoL, while engagement in pain catastrophizing was associated significantly with greater psychological distress and poorer QoL.
Table 1.
Pearson Correlations (and significance values) and descriptive values of CSM variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | Means (SD) | |
|---|---|---|---|---|---|---|---|---|
| 1. FM symptom severity (FIQ-R) | – | 67.00 (14.62) | ||||||
| 2. Illness perceptions (BIPQ) | .60** | – | 54.56 (8.19) | |||||
| 3. Pain acceptance (CPAQ-R) | − .22** | − .30** | – | 52.08 (11.95) | ||||
| 4. Pain catastrophizing (PCS) | .45** | .55** | .02 | – | 26.35 (12.10) | |||
| 5. Maladaptive coping (COPE) | .32** | .37** | .12 | .51** | – | 1.83 (.57) | ||
| 6. Adaptive coping (COPE) | .10 | .01 | .28** | .02 | .09 | – | 2.29 (.55) | |
| 7. Psychological distress (DASS-21) | .62** | .49** | .04 | .65** | .64** | .04 | – | 55.50 (27.13) |
| 8. QoL (EUR0HIS-QOL) | − .50** | − .51** | .44** | − .33** | − .24** | .16 | − .44** | 18.07 (5.52) |
*p < .05; ** p < .01
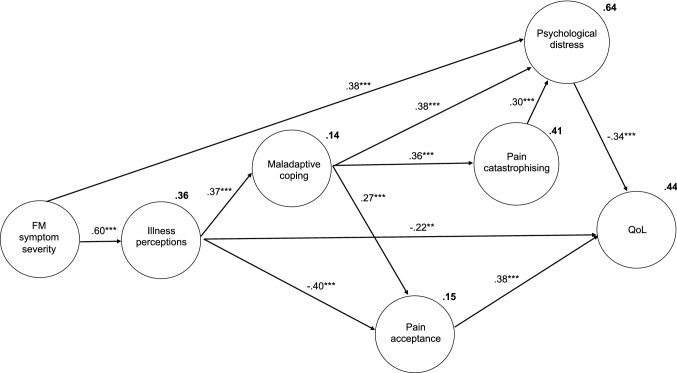
To evaluate the hypothesis, a model of the study variables was conducted. Based on an iterative process guided by Hu and Bentler (1999), adaptive coping and all demographic variables were removed from the model. The final model (see Fig. 1) demonstrated an excellent fit (χ2 (9) = 15.57, p = 0.08, χ2/N = 1.73, CFI = 0.985, TLI = 0.965, RMSEA = 0.070, SRMR = 0.048). The total amount of variance accounted for in each of the variables was also good, 36% of illness perceptions, 14% of maladaptive coping, 15% of pain acceptance, 41% of pain catastrophizing, 64% of psychological distress, and 44% of QoL.
Consistent with the CSM and the study hypotheses, FM symptom severity had a significant direct influence on illness perceptions (β = 0.60, p < 0.001) and psychological distress (β = 0.38, p < 0.001). Illness perceptions had a significant direct influence on maladaptive coping (β = 0.37, p < 0.001), pain catastrophizing (β = 0.42, p < 0.001), pain acceptance (β = − 0.40, p < 0.001), and QoL (β = − 0.22, p < 0.01). Pain catastrophizing and maladaptive coping influenced psychological distress (β = 0.30, p < 0.001, β = 0.38, p < 0.001, respectively), and in turn distress impacted QoL (β = − 0.34, p < 0.001). Acceptance of pain was influenced by maladaptive coping (β = 0.27, p < 0.001) and in turn acceptance of pain influenced QoL (β = 0.38, p < 0.001) (Fig. 2).
Fig. 2.
Final extended CSM (note: only latent variables presented with error terms removed; **p < 0.01, ***p < 0.001)
Discussion
Given a high proportion of people diagnosed with FM are women (Yunus et al., 2000), understanding the unique experiences of women who have FM is important to improve health outcomes, as has previously been done in other female-based FM studies (Capraro et al., 2012; McInnis et al., 2014; Stuifbergen et al., 2006). Consistent with past research, this study observed that an increase in FM severity was associated with more negative illness perceptions (Stuifbergen et al., 2006; Van Wilgen et al., 2008), higher pain catastrophizing (Lami et al., 2018), lower pain acceptance (Lami et al., 2018; Rodero et al., 2011), poorer QoL, and higher psychological distress (De Souza Santos Berber et al., 2005; Lee et al., 2017; Schaefer et al., 2011; Toussaint et al., 2017). The results support the study hypothesis that illness perceptions, pain acceptance, pain catastrophizing, and coping styles mediated the relationship between FM symptom severity and patient-reported outcomes (PD and QoL).
The current study is the first to validate the CSM using SEM to simultaneously evaluate the interactions between FM severity, illness perceptions, pain acceptance, pain catastrophizing, coping strategies, psychological distress, and QoL. Consistent with the principles and past research involving the CSM (Hagger & Orbell, 2003; Leventhal et al., 1980), the study found that the severity of FM directly and indirectly influenced psychological distress and QoL. This indirect influence occurred via illness perceptions, and consequent maladaptive coping and pain acceptance. These findings are consistent with previous research demonstrating that illness perceptions act as a mediator between illness severity and QoL (Hagger & Orbell, 2003). The finding is also consistent with FM-based research which demonstrated a relationship between illness severity and illness perceptions (Stuifbergen et al., 2006), and illness severity and QoL (Lee et al., 2017; Schaefer et al., 2011), and illness perceptions and QoL (Capraro et al., 2012; Van Wilgen et al., 2008). Additionally, the study found illness perceptions directly and indirectly influenced QoL via pain catastrophizing, pain acceptance, maladaptive coping, and psychological distress. These findings support the previous research involving FM cohorts which has identified QoL being influenced by pain catastrophizing (Burckhardt et al., 1997; Galvez-Sánchez et al., 2020) and psychological distress (Lee et al., 2017). Prior studies have identified QoL being influenced by pain acceptance in paediatric chronic pain cohorts (McGarrigle et al., 2020) and maladaptive coping in chronic illness cohorts such as diabetes and endometriosis (González-Echevarría et al., 2019; Knowles et al., 2020) but have not specifically been investigated in FM cohorts.
This study highlights the importance of working with individuals living with FM to adapt their perceptions (e.g. how much control and understanding they have of FM, the extent to which their identity is linked to FM diagnosis) of their illness as a way of improving QoL. In addition to addressing comorbid psychological distress, improvement in QoL is likely to be enhanced through reducing pain catastrophizing and promoting strategies to increase pain acceptance. It is noted that while leading pain societies currently recommend the use of cognitive-behavioural therapy in their multicomponent treatment plan for FM (Thieme et al., 2017), the role of increasing pain acceptance has not yet been incorporated into recommendations.
Limitations of this study include self-reported FM diagnosis and severity, and potential for self-selection bias. As data were collected from a FM female-specific online group, results may not reflect the experience of people with more mild symptoms who do not utilize the group. Additionally, as fatigue and cognitive impairment are common components of FM (Arnold et al., 2011), the results may not reflect the experiences of people who experience more severe and debilitating symptoms for whom answering 135 questions may be challenging. The number of participants in this study was below the recommended sample size (> 200) generally recommended when using SEM (Hair et al., 2010); however, the study was based on a validated theoretical model. Due to the administrative error relating to the naming of the anchor points for the FIQ-R, the validity of the scale may have been compromised. Although a factor analysis was completed and the FIQ-R demonstrated a strong internal consistency, further research is needed to replicate the study using the original scale. Further, as the study was cross-sectional, true causal relationships cannot be established. Future research should seek to replicate and extend the current study’s findings within an interventional repeated measures design to explore and evaluate true causality of the study variables and their role in impacting QoL in FM cohorts. Finally, future research should seek to replicate this study and extend it by assessing for potential differences across males and females.
In conclusion, this is the first study to validate the complete CSM in a female cohort with FM using SEM. The findings from this study provides evidence for the interactions between self-reported FM symptom severity, illness perceptions, maladaptive coping, pain acceptance, pain catastrophizing, psychological distress, and QoL. Consistent with the CSM, illness perceptions mediated the relationship between FM severity and QoL, and both pain acceptance and maladaptive coping mediated the relationship between illness perceptions and QoL, and maladaptive coping mediated the relationship between illness perceptions and psychological distress. The study findings suggest that future interventional studies aimed at enhancing QoL in FM cohorts should target psychological variables such as pain acceptance, pain catastrophizing, and maladaptive coping strategies, and illness perceptions.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by KD and SK. The first draft of the manuscript was written by KD, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. No funding was received for conducting this study.
Data Availability
The summary data generated during and/or analysed during the current study are available from the corresponding author on reasonable request and after relevant ethical approval.
Code Availability
Not applicable.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Patients signed informed consent regarding publishing their data.
Ethical Approval
The questionnaire and methodology for this study was approved by the Human Research Ethics committee of Swinburne University of Technology (Ethics Approval Number: 2018/114).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Alok R, Das SK, Agarwal GG, Tiwari SC, Salwahan L, Srivastava R. Problem-focused coping and self-efficacy as correlates of quality of life and severity of fibromyalgia in primary fibromyalgia patients. Journal of Clinical Rheumatology. 2014;20(6):314–316. doi: 10.1097/RHU.0000000000000130. [DOI] [PubMed] [Google Scholar]
- Arnold LM, Clauw DJ, McCarberg BH. Improving the recognition and diagnosis of fibromyalgia. Mayo Clinic Proceedings. 2011;86(5):457–464. doi: 10.4065/mcp.2010.0738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett RM, Friend R, Jones KD, Ward R, Han BK, Ross RL. The revised fibromyalgia impact questionnaire (FIQR): Validation and psychometric properties. Arthritis Research & Therapy. 2009;11(4):R120. doi: 10.1186/ar2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehm A, Eisenberg E, Lampel S. The contribution of social capital and coping strategies to functioning and quality of life of patients with fibromyalgia. Clinical Journal of Pain. 2011;27(3):233–239. doi: 10.1097/AJP.0b013e3181fdabcf. [DOI] [PubMed] [Google Scholar]
- Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. Journal of Psychosomatic Research. 2006;60(6):631–637. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- Burckhardt CS, Clark SR, O'Reilly CA, Bennett RM. Pain-coping Strategies of women with fibromyalgia: Relationship to pain, fatigue, and quality of life. Journal of Musculoskeletal Pain. 1997;5(3):5–21. doi: 10.1300/J094v05n03_02. [DOI] [Google Scholar]
- Capraro M, Dalla Valle M, Podswiadek M, de Sandre P, Sgnaolin E, Ferrari R. The role of illness perception and emotions on quality of life in fibromyalgia compared with other chronic pain conditions. Reumatismo. 2012;64(3):142–150. doi: 10.4081/reumatismo.2012.142. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’too long: Consider the brief cope. International Journal of Behavioral Medicine. 1997;4(1):92. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Chandran, A., Schaefer, C., Ryan, K., Baik, R., McNett, M., & Zlateva, G. (2012). The comparative economic burden of mild, moderate, and severe fibromyalgia: Results from a retrospective chart review and cross-sectional survey of working-age U.S. adults. Journal of Managed Care Pharmacy, 18(6), 415–426. 10.18553/jmcp.2012.18.6.415 [DOI] [PMC free article] [PubMed]
- Choy E, Perrot S, Leon T, Kaplan J, Petersel D, Ginovker A, Kramer E. A patient survey of the impact of fibromyalgia and the journey to diagnosis. BMC Health Services Research. 2010 doi: 10.1186/1472-6963-10-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark P, Paiva ES, Ginovker A, Salomón PA. A patient and physician survey of fibromyalgia across Latin America and Europe. BMC Musculoskeletal Disorders. 2013 doi: 10.1186/1471-2474-14-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui J, Matsushima E, Aso K, Masuda A, Makita K. Psychological features and coping styles in patients with chronic pain. Psychiatry and Clinical Neurosciences. 2009;63(2):147–152. doi: 10.1111/j.1440-1819.2009.01934.x. [DOI] [PubMed] [Google Scholar]
- Berber DSS, Kupek, E., & Berber, S. C. Prevalence of depression and its relationship with quality of life in patients with fibromyalgia syndrome. Revista Brasileira De Reumatologia. 2005;45(2):47–54. doi: 10.1590/S0482-50042005000200002. [DOI] [Google Scholar]
- Edwards RR, Bingham Iii CO, Bathon J, Haythornthwaite JA. Catastrophizing and pain in arthritis, fibromyalgia, and other rheumatic diseases. Arthritis Care and Research. 2006;55(2):325–332. doi: 10.1002/art.21865. [DOI] [PubMed] [Google Scholar]
- Galvez-Sánchez CM, Montoro CI, Duschek S, del Paso GAR. Pain catastrophizing mediates the negative influence of pain and trait-anxiety on health-related quality of life in fibromyalgia. Quality of Life Research. 2020;29(7):1871–1881. doi: 10.1007/s11136-020-02457-x. [DOI] [PubMed] [Google Scholar]
- González-Echevarría AM, Rosario E, Acevedo S, Flores I. Impact of coping strategies on quality of life of adolescents and young women with endometriosis. Journal of Psychosomatic Obstetrics & Gynecology. 2019;40(2):138–145. doi: 10.1080/0167482X.2018.1450384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guymer EK, Littlejohn GO, Brand CK, Kwiatek RA. Fibromyalgia onset has a high impact on work ability in Australians. Internal Medicine Journal. 2016;46(9):1069–1074. doi: 10.1111/imj.13135. [DOI] [PubMed] [Google Scholar]
- Hagger MS, Koch S, Chatzisarantis NLD, Orbell S. The common sense model of self-regulation: Meta-analysis and test of a process model. Psychological Bulletin. 2017;143(11):1117–1154. doi: 10.1037/bul0000118. [DOI] [PubMed] [Google Scholar]
- Hagger MS, Orbell S. A meta-analytic review of the common-sense model of illness representations. Psychology and Health. 2003;18(2):141–184. doi: 10.1080/088704403100081321. [DOI] [Google Scholar]
- Hair JF, Anderson RE, Babin BJ, Black WC. Multivariate data analysis: A global perspective. Pearson; 2010. [Google Scholar]
- Hu L, t., & Bentler, P. M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Knowles SR, Apputhurai P, O’Brien CL, Ski CF, Thompson DR, Castle DJ. Exploring the relationships between illness perceptions, self-efficacy, coping strategies, psychological distress and quality of life in a cohort of adults with diabetes mellitus. Psychology, Health & Medicine. 2020;25(2):214–228. doi: 10.1080/13548506.2019.1695865. [DOI] [PubMed] [Google Scholar]
- Knowles SR, Wilson JL, Connell WR, Kamm MA. Preliminary examination of the relations between disease activity, illness perceptions, coping strategies, and psychological morbidity in Crohn's disease guided by the common sense model of illness. Inflammatory Bowel Diseases. 2011;17(12):2551–2557. doi: 10.1002/ibd.21650. [DOI] [PubMed] [Google Scholar]
- Lami MJ, Martínez MP, Miró E, Sánchez AI, Guzmán MA. Catastrophizing, acceptance, and coping as mediators between pain and emotional distress and disability in fibromyalgia. Journal of Clinical Psychology in Medical Settings. 2018 doi: 10.1007/s10880-018-9543-1. [DOI] [PubMed] [Google Scholar]
- Lee JW, Lee KE, Park DJ, Kim SH, Nah SS, Lee JH, Kim SK, Lee YA, Hong SJ, Kim HS, Lee HS. Determinants of quality of life in patients with fibromyalgia: A structural equation modeling approach. PLoS ONE. 2017 doi: 10.1371/journal.pone.0171186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal H, Meyer D, Nerenz D. The common sense representation of illness danger. Contributions to Medical Psychology. 1980;2:7–30. [Google Scholar]
- Lovibond, S. H., & Lovibond, P. F. (1996). Manual for the depression anxiety stress scales. Psychology Foundation of Australia.
- McCracken LM. Behavioral constituents of chronic pain acceptance: Results from factor analysis of the chronic pain acceptance questionnaire. Journal of Back and Musculoskeletal Rehabilitation. 1999;13(2–3):93–100. doi: 10.3233/BMR-1999-132-306. [DOI] [Google Scholar]
- McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: Component analysis and a revised assessment method. Pain. 2004;107(1–2):159–166. doi: 10.1016/j.pain.2003.10.012. [DOI] [PubMed] [Google Scholar]
- McGarrigle L, Wesson C, DeAmicis L, Connoly S, Ferreira N. Psychological mediators in the relationship between paediatric chronic pain and adjustment: An investigation of acceptance, catastrophising and kinesiophobia. Journal of Contextual Behavioral Science. 2020;18:294–305. doi: 10.1016/j.jcbs.2020.10.009. [DOI] [Google Scholar]
- McInnis OA, Matheson K, Anisman H. Living with the unexplained: Coping, distress, and depression among women with chronic fatigue syndrome and/or fibromyalgia compared to an autoimmune disorder. Anxiety, Stress and Coping. 2014;27(6):601–618. doi: 10.1080/10615806.2014.888060. [DOI] [PubMed] [Google Scholar]
- Nosikov, A., & Gudex, C. (2003). Development of a common instrument for quality of life. EUROHIS: Developing common instruments for health surveys, 57, 145.
- Rodero B, Casanueva B, Luciano JV, Gili M, Serrano-Blanco A, García-Campayo J. Relationship between behavioural coping strategies and acceptance in patients with fibromyalgia syndrome: Elucidating targets of interventions. BMC Musculoskeletal Disorders. 2011 doi: 10.1186/1471-2474-12-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer C, Chandran A, Hufstader M, Baik R, McNett M, Goldenberg D, Gerwin R, Zlateva G. The comparative burden of mild, moderate and severe Fibromyalgia: Results from a cross-sectional survey in the United States. Health and Quality of Life Outcomes. 2011 doi: 10.1186/1477-7525-9-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer C, Mann R, Masters ET, Cappelleri JC, Daniel SR, Zlateva G, McElroy HJ, Chandran AB, Adams EH, Assaf AR, McNett M. The comparative burden of chronic widespread pain and fibromyalgia in the United States. Pain Practice. 2016;16(5):565–579. doi: 10.1111/papr.12302. [DOI] [PubMed] [Google Scholar]
- Schmidt S, Mühlan H, Power M. The EUROHIS-QOL 8-item index: Psychometric results of a cross-cultural field study. European Journal of Public Health. 2005;16(4):420–428. doi: 10.1093/eurpub/cki155. [DOI] [PubMed] [Google Scholar]
- Skaer TL, Kwong WJ. Illness perceptions and burden of disease in fibromyalgia. Expert Review of Pharmacoeconomics and Outcomes Research. 2017;17(1):9–15. doi: 10.1080/14737167.2017.1270207. [DOI] [PubMed] [Google Scholar]
- Smith WR, Strachan ED, Buchwald D. Coping, self-efficacy and psychiatric history in patients with both chronic widespread pain and chronic fatigue. General Hospital Psychiatry. 2009;31(4):347–352. doi: 10.1016/j.genhosppsych.2009.03.012. [DOI] [PubMed] [Google Scholar]
- Stuifbergen AK, Phillips L, Voelmeck W, Browder R. Illness perceptions and related outcomes among women with fibromyalgia syndrome. Women's Health Issues. 2006;16(6):353–360. doi: 10.1016/j.whi.2006.05.003. [DOI] [PubMed] [Google Scholar]
- Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: Development and validation. Psychological Assessment. 1995;7(4):524. doi: 10.1037/1040-3590.7.4.524. [DOI] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. Pearson Education UK; 2013. [Google Scholar]
- Thieme K, Mathys M, Turk DC. Evidenced-based guidelines on the treatment of fibromyalgia patients: Are they consistent and if not, why not? Have effective psychological treatments been overlooked? Journal of Pain. 2017;18(7):747–756. doi: 10.1016/j.jpain.2016.12.006. [DOI] [PubMed] [Google Scholar]
- Toussaint L, Sirois F, Hirsch J, Kohls N, Weber A, Schelling J, Vajda C, Offenbäecher M. Anger rumination mediates differences between fibromyalgia patients and healthy controls on mental health and quality of life. Personality and Mental Health. 2019 doi: 10.1002/pmh.1445. [DOI] [PubMed] [Google Scholar]
- Toussaint L, Sirois F, Hirsch J, Weber A, Vajda C, Schelling J, Kohls N, Offenbacher M. Gratitude mediates quality of life differences between fibromyalgia patients and healthy controls. Quality of Life Research. 2017;26(9):2449–2457. doi: 10.1007/s11136-017-1604-7. [DOI] [PubMed] [Google Scholar]
- Van Wilgen CP, Van Ittersum MW, Kaptein AA, Van Wijhe M. Illness perceptions in patients with fibromyalgia and their relationship to quality of life and catastrophizing. Arthritis and Rheumatism. 2008;58(11):3618–3626. doi: 10.1002/art.23959. [DOI] [PubMed] [Google Scholar]
- Vervoort VM, Vriezekolk JE, Olde Hartman TC, Cats HA, van Helmond T, van der Laan WH, Geenen R, van den Ende CH. Cost of illness and illness perceptions in patients with fibromyalgia. Clinical and Experimental Rheumatology. 2016;34:74–82. [PubMed] [Google Scholar]
- Walitt B, Nahin RL, Katz RS, Bergman MJ, Wolfe F. The prevalence and characteristics of fibromyalgia in the 2012 national health interview survey. PLoS ONE. 2015 doi: 10.1371/journal.pone.0138024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yunus MB, Inanici F, Aldag JC, Mangold RF. Fibromyalgia in men: Comparison of clinical features with women. The Journal of Rheumatology. 2000;27(2):485–490. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The summary data generated during and/or analysed during the current study are available from the corresponding author on reasonable request and after relevant ethical approval.
Not applicable.