Abstract
Background:
Dentists play an important role in caries prevention by delivering preventive care, educating patients, and buying related products; it is critical to recognize what they know and believe about caries prevention, as well as how they use caries prevention interventions.
Materials and Methods:
A descriptive cross-sectional study was conducted in South India between January 2021 and February 2021 to determine the dentists' knowledge, attitude, and practice of prescribing preventive strategies and remineralizing agents for caries prevention. A questionnaire including 11 self-administered, prestructured questions was made and distributed through electronic media. Chi-square test was done. The test significance value was taken as 0.05.
Results:
A total of 252 dental practitioners participated in the study. The majority of general dentists and specialists followed all the measures such as pit and fissure sealants, fluoride application, counseling patients about oral hygiene maintenance, and regular recall after 6 months to 1 year (P > 0.05). Fluoridated remineralization strategy was found to be the most prescribed (69%) strategy for caries prevention. A significant number of dentists think fluoridated mineralization strategies will remain prevalent (P < 0.05). Younger dentists find practicing preventive dentistry more feasible compared to dentists with greater years of experience (P < 0.05).
Conclusion:
Dentists across the country are well aware, have sufficient knowledge, and prescribe preventive strategies such as fluoride application, pit and fissure sealants, regular oral health checkups, and counsel the patients about the importance of oral health but there is a lack of implementation of these preventive strategies in everyday practice.
Keywords: Oral health, pit and fissure sealants, preventive dentistry, remineralization formulations, toothpaste
INTRODUCTION
People all over the world are vulnerable to dental caries throughout their lives, making it one of the most prevalent preventable oral diseases.[1,2,3] It is the leading cause of tooth loss and oral pain.[2,4] Caries can be halted and possibly reversed in their early stages, but it is rarely self-limiting, and if not treated properly, they can intensify until the tooth is lost.[2,5] Dental caries is caused by acidic by-products of bacteria fermentation of dietary carbohydrates that cause localized degradation of susceptible dental hard tissues.[2,5] Carious demineralization effects are visible on hard dental tissues, but the disease process begins inside the bacterial biofilm (dental plaque) that covers a tooth surface. Dental caries is a multifactorial disease that begins with microbiological changes inside the complex biofilm and is influenced by salivary flow and composition, fluoride exposure, sugar intake, and preventive practices (cleaning teeth). The disease is initially reversible and can be stopped at any stage, even if some dentin or enamel has been lost (cavitation), as long as enough biofilm is removed. In most people, dental caries is a chronic condition that develops slowly. The disease can be seen on the smooth, pitted, and fissured surfaces of primary and permanent teeth, as well as the crown (coronal caries) and root (root caries).[6]
Oral diseases affect about 3.5 billion people worldwide, according to the Global Burden of Disease Study 2017, with caries of permanent teeth being the most prevalent condition. Caries of permanent teeth affect an estimated 2.3 billion people worldwide, whereas caries of primary teeth affect over 530 million children.[7] These results highlight the importance of treating dental caries based on an individual's risk level and taking specific precautions for those who are at a high risk of developing the disease. The persistence of a high global disease burden demands renewed and increased professional efforts at the individual- and population-level prevention.[8]
In the past, cavities were filled as soon as they were discovered; now, the indications for restorative treatment have narrowed; plaque reduction steps are used instead of restorative treatment to facilitate remineralization and reversal of the dental caries process. A patient with active caries lesions requires a combination of individual-level measures to minimize the risk of caries and prevent future caries lesions, as well as tooth-level strategies to prevent future caries lesions.[9] Caries prevention has historically meant preventing caries initiation, also known as primary prevention. Caries care/management/control now encompasses primary, secondary, and tertiary prevention, as well as nonoperative and operative procedures.[10] Preventive measures such as maintenance of oral hygiene, counseling/awareness about oral hygiene, fluoride application (professionally applied and at-home measures), use of pit and fissure sealants, resin infiltration, and remineralizing agents are being promoted.
The application of a thin physical barrier over a clinically sound caries predilection site to prevent the initiation of a caries lesion is known as preventive sealant/sealing. Resin composite or glass ionomer cement (GIC) can be used to fill pits, fissures, and fossae.[10] Diet, which is the leading cause of dental caries, is also linked to obesity, heart disease, diabetes, and some cancers. Improvements in a variety of chronic conditions should be more efficiently and effectively achieved by directing action toward common risk factors and their underlying social determinants.[11] It is reasonable to encourage a reduction in sugar consumption, both in terms of frequency and total amount.[12,13] Research on the oral health effects of fluoride started around 100 years ago.[14] Topical fluorides generally fall into two categories: (a) self-applied – e.g., toothpaste and mouth rinse and (b) professionally applied – e.g., solutions, gels, foams, and varnish. Professionally applied fluoride varnish, gel, and foam are high-concentration fluoride vehicles which are applied by health-care professionals intermittently for caries prevention.[15] Brushing with fluoride toothpaste has been considered being near to an ideal public health technique because it is convenient, economical, culturally acceptable, and widely used.[16]
The American Dental Association (ADA) recently published recommendations for nonrestorative treatment methods. Silver diamine fluoride (SDF), when applied every 6–12 months, has been demonstrated to be effective at halting advanced cavitated caries lesions at all coronal and root surfaces, as well as noncavitated root caries lesions, in both primary and permanent teeth. Occlusal noncavitated caries lesions in primary and permanent teeth can be effectively managed with sealants alone or in combination with 5% NaF varnishes. Five percentage NaF varnish, resin infiltration, sealant, or a combination of the above are recommended for noncavitated carious lesions on the proximal surface of primary and permanent teeth. Professionally applied 1.23% acidulated phosphate fluoride gel or 5% NaF varnish applied every 3–6 months is effective for managing noncavited caries lesions on the occlusal, facial, or lingual coronal surfaces of primary and permanent teeth. For root surface cavitated and noncavitated caries lesion management, a 5000-ppm fluoride dentifrice or gel (1.1% sodium fluoride [NaF]) applied at least once per day is effective.[9]
Dentists play an important role in caries prevention by delivering preventive care, educating patients, and buying related products; it is critical to recognize what they know and believe about caries prevention, as well as how they use caries prevention interventions.[17] Hence, the aim of this study was to determine the knowledge, attitude, and practice of preventive strategies by dentists for caries prevention.
MATERIALS AND METHODS
A descriptive cross-sectional study was conducted in South India between January 2021 and February 2021 to determine the dentists' knowledge, attitude, and practice of prescribing preventive strategies and remineralizing agents for caries prevention. Ethical approval from the review board of Saveetha Institute of Medical and Technical Sciences, Chennai, India, was taken to conduct the study.
The questionnaire included 11 self-administered, prestructured questions. (Refer supplementary data) The questionnaire was divided into two sections, which collected the information as follows: The first part assessed the demographic details of the respondents comprising 5 questions – gender, age, qualification, designation, and years of experience in the profession. The second part was made up of 11 questions which focused on knowledge-based (3) questions regarding preventive care options, attitude-based (4) questions eliciting what the dentists feel about such strategies, and practice-based (4) questions to judge whether they incorporate these strategies in their daily practice.
The questionnaire was prepared on Google Forms and distributed through electronic media across the country. Two hundred and fifty-two responses were generated. The data collection and tabulation were done in Google Sheets and were then analyzed using Statistical Packages for the Social Sciences (SPSS), version 25.0 software (SPSS Inc., Chicago, USA).
RESULTS
The questionnaire's face validity was checked by a focus group discussion by a panel of five experts in the field, who agreed that the test is a valid measure of the concept which is being measured. The content validity of the instrument was evaluated, which indicates a determination of whether the instrument contained all applicable or important domains or not. Based on the opinions of three blinded raters, the mean content validity ratio was determined to be 0.87. A previously validated questionnaire was pilot tested among a convenience group of 15 dentists before finalization. Following the completion of the pilot answer format, each respondent was interviewed to obtain input on the questionnaire's overall acceptability in terms of duration, language, clarity, and adequacy. The questionnaire's internal reliability was found to be good, with a Cronbach's coefficient of 0.88. The required improvements were implemented before the key study based on the findings of this review.
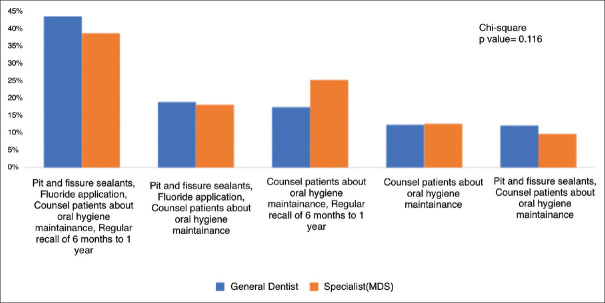
A total of 252 dental practitioners participated in the study. Out of all the participants, 88 (34.9%) were male whereas 164 (64.1%) were females [Figure 1]. The qualifications of the respondents were as follows: 145 (57.5%) of them were general dentists and 107 (42.5%) of them were specialists (MDS)[Figure 2]. Majority of dentists were clinicians (67.5%) while 9.1% were both academicians and clinicians [Figure 3]. Figure 4 shows that most of the participants (90%) have <5 years of experience.
Figure 1.
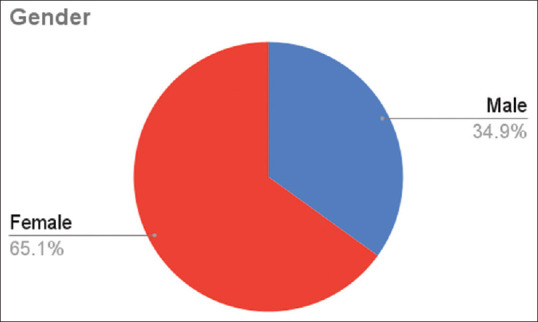
Distribution of participants according to gender.
Figure 2.
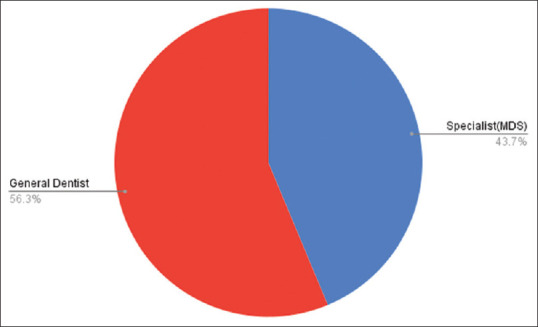
Distribution of participants according to qualification.
Figure 3.
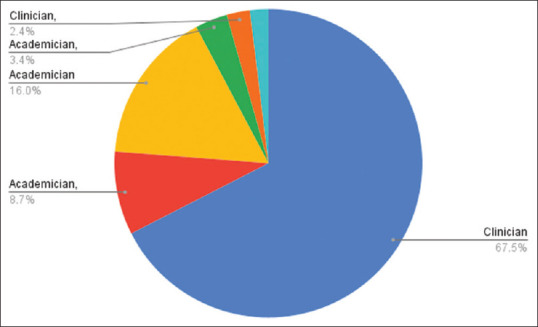
Distribution of participants according to the designation.
Figure 4.
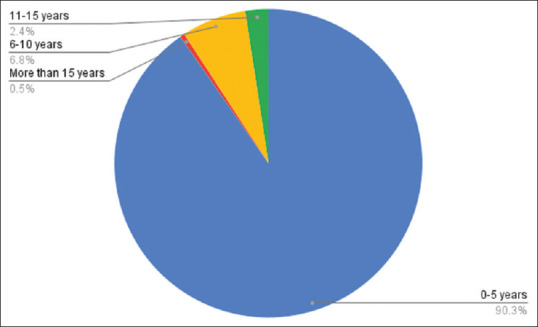
Distribution of participants according to years of experience.
When dentists were asked about what preventive measures they practice the most, the majority of general dentists and specialists followed all the measures such as pit and fissure sealants, fluoride application, counseling patients about oral hygiene maintenance, and regular recall after 6 months to 1 year. Fluoridated remineralization strategy was found to be the most prescribed (69%) strategy for caries prevention [Figure 5].
Figure 5.
Preventive strategies usually followed by general dentists and specialists.
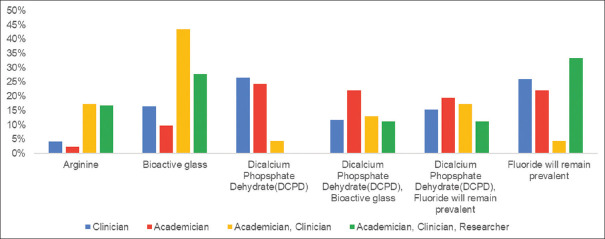
Dentists were asked about what remineralizing agent in toothpaste had the maximum scope of development in the future. According to most academicians, clinicians, and researchers, fluoride will remain prevalent compared to other remineralizing agents such as bioactive glass, dicalcium dihydrate, and arginine [Figure 6].
Figure 6.
Opinion of researchers, academicians, and clinicians on toothpaste ingredients having maximum scope of development in future.
Regarding the feasibility of practicing preventive dentistry, most dentists with 0–15 years of experience responded that it was feasible (60%) to practice preventive dentistry in daily clinical life, while about 25% of dentists with an experience of 11–15 years think it is not feasible [Figure 7]. According to more than 50% of dentists, the most common difficulty in practicing preventive dentistry is patient compliance [Figure 8]. About 82.8% of dentists think pit and fissure sealants can be used in case of initial enamel margin breakdown, whereas 17.2% think it cannot be used. The most commonly used pit and fissure sealants among dentists were resin-based cement (51.6%), followed by GIC (39.1%), no use of sealants (6.3%), and other sealants (3.1%). While 39.5% of dentists used fluoride varnishes on exposed root surfaces, whereas 39.8% said they do not use varnishes. About 17.2% used both fluoride and chlorhexidine varnishes and only 7% used chlorhexidine varnishes.
Figure 7.
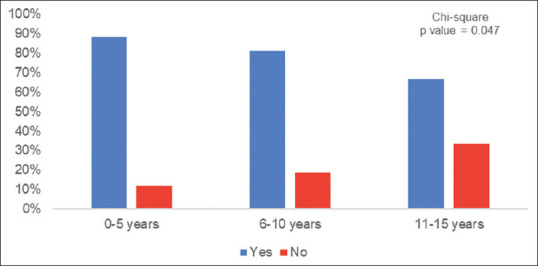
Feasibility of practicing preventive strategies in dental practice.
Figure 8.
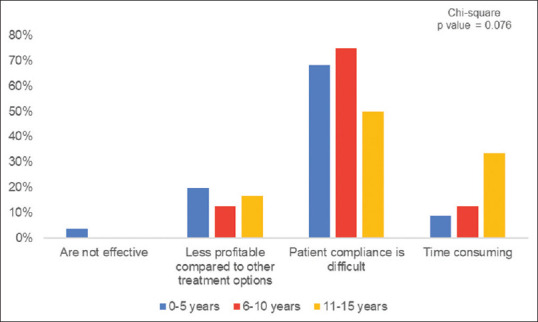
Difficulties in practicing preventive strategies.
The most commonly prescribed formulation by general dentists and specialists was toothpaste, followed by the combination of toothpaste and mouth rinses whereas varnishes and toothpaste are the least prescribed [Figure 9]. Meaning of the term “remineralizing agents,” according to 53.7% of respondents was materials that restore the minerals in demineralized structure and those that cause deposition of calcium and phosphate in demineralized enamel. Colgate was the most prescribed toothpaste by academicians, clinicians, and researchers [Figure 10].
Figure 9.
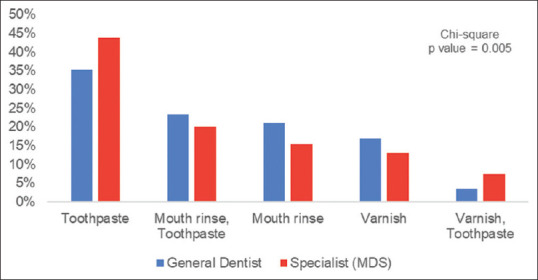
Most commonly prescribed demineralization formulation by dentists and specialists.
Figure 10.
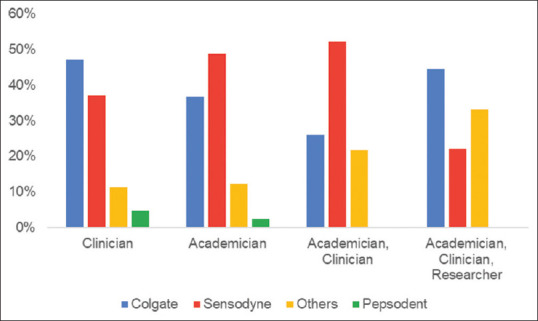
Most commonly prescribed toothpaste by clinicians, practitioners, and researchers.
DISCUSSION
This is the first survey in South India to review data from a random sample of dentists regarding the practice of preventive dentistry. The importance of oral health promotion and prevention in reducing disease burden and improving quality of life cannot be underestimated. Early and regular preventive dental treatment, fluoridation, and sealants are cost-effective ways to reduce disease burden and related costs.[18] To avoid oral diseases and maintain good oral health, prevention is essential. Lack of access to preventive dental care almost often leads to fast fixes that are both short-lived and expensive, especially among low-income children and their families who lack the financial means to access dental care. Professionals, people, and society as a whole are all responsible for this aspect of dentistry. Dentists are in a unique position to assist their patients in reducing the burden of oral disease and adopting good oral hygiene habits.
In conglomeration, the findings show favorable awareness and attitude, as well as effective use of sealants, topical fluoride, and various preventive procedures. These findings were in agreement with the findings of a study carried out by Riley et al.,[19] which reported the practice of sealants and topical fluoride as 69% and 82%, respectively. Similar findings were found in studies by Bhardwaj et al. and Patil et al.[20,21]
In a study by Bhardwaj et al., more than 50% of dentists could integrate preventive dental procedures in their routine dental practice.[21] These results were similar to our study where 85.4% of dentists suggested it was feasible to practice preventive dentistry. These results are in contrast to the study by Arheiam et al., where the majority of participants admitted to being unable to learn practical skills to practice preventive dentistry.[22] Younger dentists were seen to prefer preventive dentistry more compared to practitioners with more experience. This may be due to insufficient preventive strategies earlier or due to difficulties faced by practitioners over the years of practice.
Patient compliance was found to be the most common limitation in practicing preventive dentistry, followed by less revenue generated through this practice. In a similar study, a lack of positive attitude or some sort of barrier or difficulty was seen in the dentist's ability to practice preventive dentistry.[23] There is a need to spread awareness and sensitize patients about the effectiveness and importance of preventive dentistry.
According to 82.8% of dentists, pit and fissure sealants can be used in initial enamel breakdown. Sealant application is a preventive conservative technique that involves introducing sealants into the pits and fissures of caries-prone teeth; the sealant then micromechanically binds to the tooth, creating a physical barrier that prevents bacteria away from their source of nutrients.[24]
The type of pit and fissure sealant most commonly used according to this study is resin-based sealants (51.5%). The GI sealant was shown to be an effective measure in caries prevention, although it had a significantly lower retention rate compared to resin based sealants according to a study by Haznedaroğlu et al.[25] In a recent update, the ADA recommendations, in collaboration with the American Academy of Pediatric Dentistry, could not draw any conclusion as to which of the two sealant materials was better due to the very low quality of the evidence available. GI persists in the deepest areas of the fissures, even though it is not clinically visible, which may explain why GIC has a caries-preventive effect despite not being as retentive as resin-based sealers.[26]
About 39.8% of dentists do not use varnish on exposed tooth surfaces in elderly patients while 35.5% use fluoride varnishes. Chlorhexidine varnishes were preferred by only 7% of dentists. A Systematic review and meta-analysis by Meyer-Lueckel et al. found that as compared to fluoride toothpaste or a placebo, professionally applied chlorhexidine varnish or SDF appeared to be more effective at preventing root caries.[27] This finding highlights dentists' lack of awareness about alternatives to fluoride varnishes such as chlorhexidine varnish or SDF, which are more effective at preventing root caries than traditional fluorides. Fluoridated remineralization strategies were preferred or prescribed more often than nonfluoridated strategies. Fluoride formulations were initially the only material used, and they responded by restoring hydroxyapatite crystals and providing the requisite ions that had been missing from the lattice network. Later studies were able to successfully implement newer biomimetic remineralization products capable of producing apatite crystals within totally demineralized collagen fibers.[28] Despite research proving nonfluoridated strategies to be effective, most dentists prefer fluoridated remineralization strategies. This could be due to dentists' lack of sufficient updated information about newer materials.
Toothpaste was the most preferred formulation prescribed to the patients while the combination of toothpaste and varnishes was least advised. This poses an issue, as evidence suggests that there is a 14% greater caries inhibiting effect with the use of fluoride varnish in combination with toothpaste compared with the other topical fluoride therapy (gels, mouth rinses, and toothpaste).[29,30,31,32] Hence, dentists should be educated about the use of varnish in conjunction with toothpaste. Colgate and Sensodyne were the most commonly prescribed remineralization toothpaste by clinicians. Dentists did not recommend toothpaste such as Patanjali, which may be due to new information about dentifrices that have demonstrated benefits and those that are heavily advertised but fail to deliver. Dentists, although prescribe Colgate, lack knowledge about the presence of arginine in it and its anti-caries effect.
Since it is a questionnaire analysis, it has limitations since most of the answers are self-reported and do not have precise data. Bias among participants is possible because they may not have expressed their true feelings and instead provided socially acceptable responses.
It is highly recommended that to address these severe dental public health problems:
An international global summit should be held to bring researchers from all over the world together to discuss the evidence and prepare a strategic plan to address improvements in dental caries prevalence
A new global epidemiologic study should be designed and introduced to scientifically collect valuable caries data that can help guide resources toward preventing and reversing the severe deterioration associated with dental caries
A renewed effort by the global dental profession to return to the preventive fundamentals that the population is not receiving. Fluorides, oral hygiene, nutritional therapy, dental sealants, and other proven approaches should be prioritized
Dedication of research resources to the creation of new anticaries materials and products to bring the best of science and technology to bear on the dental caries issue.[33]
CONCLUSION
Within the limitations of this study, it can be stated that dentists across the country have a holistic approach, are well aware, have sufficient knowledge, and prescribe preventive strategies such as fluoride application, pit and fissure sealants, regular oral health checkups, and counsel the patients about the importance of oral health. Although this indicates a positive attitude toward preventive care, there is an insufficient implementation of the same in clinical practice due to a lack of patient compliance.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or non-financial in this article.
Supplementary Data
Questionnaire
Demographics
1.Age
23–25 years
26–30 years
30–40 years
Above 40 years
2.Gender
Female
Male
Other
3.Designation
Clinicians
Academicians
Researcher
4.Years of experience
0–5 years
6–10 years
11–15 years
More than 15 years
5.Qualification
General Dentist
Specialists (MDS)
Doctorate (Ph.D.)
Questionnaire
1.What caries preventive measures do you practice?(multiple choices can be selected)
Pit and fissure sealants
Fluoride application
Counsel patients about oral hygiene maintenance
Regular recall of 6 months to 1 year
None
2.In your practice, which of the following is the most prescribed strategy for caries prevention?
Fluoridated remineralization strategies
Nonfluoridated remineralizing strategies
Both
Others
None
3.Do you think it is feasible to practice preventive dentistry in clinical practice?
Yes
No
4.What do you think are the limitations of practicing preventive dentistry?
Less profitable compared to other treatment options
Patient compliance is difficult
Time-consuming
Are not effective
5.Do you think pit and fissure sealants can be used in case of initial enamel margin breakdown?
Yes
No
6.What material do you use for sealing pits and fissures?
Do not use pit and fissure sealants
GIC-based sealants
Resin-based sealants
Others
7.What type of varnish do you use on exposed tooth surfaces in elderly patients?
Do not use
Fluoride
Chlorhexidine
Fluoride and chlorhexidine
8.Which remineralization formulation do you usually prescribe?
Mouth rinse
Varnish
Toothpaste
Gums and mints
None
9.Which of the following ingredients in toothpaste, according to you, has better scope of development in future in the prevention of dental caries?(multiple choices can be selected)
Dicalcium Phosphate Dihydrate (DCPD)
Bioactive glass
Arginine
Fluoride will remain prevalent
10.What is the meaning of the term “remineralizing agents?”
Materials that restore the minerals in demineralized structure
Deposition of calcium and phosphate in demineralized enamel
Both of the above
None of the above
11.Which remineralizing toothpaste do you usually prescribe?
Colgate
Sensodyne
Pepsodent
Patanjali
Others
REFERENCES
- 1.Pitts NB. Are we ready to move from operative to non-operative/preventive treatment of dental caries in clinical practice? Caries Res. 2004;38:294–304. doi: 10.1159/000077769. [DOI] [PubMed] [Google Scholar]
- 2.Ricketts PD, Ricketts D. Wiley/Blackwell: Oxford; 2015. Dental Caries: The Disease and its Clinical Management; p. 855. [Google Scholar]
- 3.Featherstone JD. The science and practice of caries prevention. J Am Dent Assoc. 2000;131:887–99. doi: 10.14219/jada.archive.2000.0307. [DOI] [PubMed] [Google Scholar]
- 4.Kidd EA, Giedrys-Leeper E, Simons D. Take two dentists: A tale of root caries. Dent Update. 2000;27:222–30. doi: 10.12968/denu.2000.27.5.222. [DOI] [PubMed] [Google Scholar]
- 5.Marsh P, Martin M. Dental plaque. Oral microbiology. 1992:98–132. [Google Scholar]
- 6.Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet. 2007;369:51–9. doi: 10.1016/S0140-6736(07)60031-2. [DOI] [PubMed] [Google Scholar]
- 7.Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jepsen S, Blanco J, Buchalla W, Carvalho JC, Dietrich T, Dörfer C, et al. Prevention and control of dental caries and periodontal diseases at individual and population level: Consensus report of group 3 of joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol. 2017;44(Suppl 18):S85–93. doi: 10.1111/jcpe.12687. [DOI] [PubMed] [Google Scholar]
- 9.Fontana M. Nonrestorative management of cavitated and noncavitated caries lesions. Dent Clin North Am. 2019;63:695–703. doi: 10.1016/j.cden.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Machiulskiene V, Campus G, Carvalho JC, Dige I, Ekstrand KR, Jablonski-Momeni A, et al. Terminology of dental caries and dental caries management: Consensus report of a workshop organized by ORCA and cariology research group of IADR. Caries Res. 2020;54:7–14. doi: 10.1159/000503309. [DOI] [PubMed] [Google Scholar]
- 11.Watt RG. Strategies and approaches in oral disease prevention and health promotion. Bull World Health Organ. 2005;83:711–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Fejerskov O, Kidd E. Dental Caries: The Disease and Its Clinical Management. John Wiley & Sons. 2009 [Google Scholar]
- 13.Burt B, Mascarenhas AK. 7th ed. Illinois: American Association of Public Health Dentistry; 2021. The practice of dentistry and dental public health. In: Burt and Eklund's Dentistry, Dental Practice, and the Community; pp. 2–9. [Google Scholar]
- 14.Petersen PE, Lennon MA. Effective use of fluorides for the prevention of dental caries in the 21st century: The WHO approach. Community Dent Oral Epidemiol. 2004;32:319–21. doi: 10.1111/j.1600-0528.2004.00175.x. [DOI] [PubMed] [Google Scholar]
- 15.Newbrun E. Topical fluorides in caries prevention and management: A North American perspective. J Dent Educ. 2001;65:1078–83. [PubMed] [Google Scholar]
- 16.Burt BA. Prevention policies in the light of the changed distribution of dental caries. Acta Odontol Scand. 1998;56:179–86. doi: 10.1080/000163598422956. [DOI] [PubMed] [Google Scholar]
- 17.Lin TH, Hsieh TY, Horowitz AM, Chen KK, Lin SS, Lai YJ, et al. Knowledge and practices of caries prevention among Taiwanese dentists attending a national conference. J Dent Sci. 2010;5:229–36. [Google Scholar]
- 18. [Last accessed on 2021 Apr 19]. Available from: http://www.cdc.gov/oralhealth/publications/library/burdenbook/pdfs/CDHP_policy_brief.pdf .
- 19.Riley JL, Gordan VV, Brad Rindal D, Fellows JL, Ajmo CT, Amundson C, et al. Preferences for caries prevention agents in adult patients: Findings from the dental practice-based research network. Community Dent Oral Epidemiol. 2010;38:360–70. doi: 10.1111/j.1600-0528.2010.00547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patil RU, Sahu A, Kambalimath HV, Panchakshari BK, Jain M. Knowledge, attitude and practice among dental practitioners pertaining to preventive measures in paediatric patients. J Clin Diagn Res. 2016;10:C71–5. doi: 10.7860/JCDR/2016/22300.9122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhardwaj T, Tandon S, Chand S, Bhargava A. Knowledge, attitude and practice towards preventive dental care- A KAP study. J Glob Oral Health. 2019;2:36–40. [Google Scholar]
- 22.Arheiam A, Bankia I, Ingafou M. Perceived competency towards preventive dentistry among dental graduates: The need for curriculum change. Libyan J Med. 2015;10:26666. doi: 10.3402/ljm.v10.26666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sushanth VH, Bhate P, Imranulla M, Kalra D, Kumar NG, Prashant GM. Assessment of knowledge, attitude, and practice regarding preventive options in oral care among dentists in Davangere city, Karnataka: A cross-sectional study. Dent Med Res. 2015;3:20. [Google Scholar]
- 24.Simonsen RJ. Clinical Applications of the Acid Etch Technique. Chicago: Quintessence Publishing (IL); 1978. p. 133. [Google Scholar]
- 25.Haznedaroğlu E, Güner Ş, Duman C, Menteş A. A 48-month randomized controlled trial of caries prevention effect of a one-time application of glass ionomer sealant versus resin sealant. Dent Mater J. 2016;35:532–8. doi: 10.4012/dmj.2016-084. [DOI] [PubMed] [Google Scholar]
- 26.Casamassimo PS, Fields HW, Jr, McTigue DJ, Nowak A. Pediatric Dentistry: Infancy through Adolescence. 5th ed. India: Elsevier; 2012. [Google Scholar]
- 27.Meyer-Lueckel H, Machiulskiene V, Giacaman RA. How to intervene in the root caries process? Systematic review and meta-analyses. Caries Res. 2019;53:599–608. doi: 10.1159/000501588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arifa MK, Ephraim R, Rajamani T. Recent advances in dental hard tissue remineralization: A review of literature. Int J Clin Pediatr Dent. 2019;12:139–44. doi: 10.5005/jp-journals-10005-1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marinho VC, Higgins JP, Logan S, Sheiham A. Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2003;2003 doi: 10.1002/14651858.CD002782. CD002782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marinho VC, Higgins JP, Logan S, Sheiham A. Fluoride mouthrinses for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2003;(3):CD002284. doi: 10.1002/14651858.CD002284. Update in: Cochrane Database Syst Rev. 2016;7:CD002284. PMID: 12917928. [DOI] [PubMed] [Google Scholar]
- 31.Marinho VC, Higgins JP, Logan S, Sheiham A. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2002;(3):CD002279. doi: 10.1002/14651858.CD002279. Update in: Cochrane Database Syst Rev. 2013;7:CD002279. PMID: 12137653. [DOI] [PubMed] [Google Scholar]
- 32.Marinho VC, Worthington HV, Walsh T, Chong LY. Fluoride gels for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2015;2015 doi: 10.1002/14651858.CD002280.pub2. CD002280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bagramian RA, Garcia-Godoy F, Volpe AR. The global increase in dental caries. A pending public health crisis. Am J Dent. 2009;22:3–8. [PubMed] [Google Scholar]