Introduction
The calcaneus is the most commonly fractured tarsal bone in the setting of polytrauma, with a 17% prevalence in patients presenting with foot injuries. 19 Displaced intra-articular calcaneal fractures (DIACF) can be highly disabling injuries if left untreated. 21 Appropriate surgical management with open reduction and internal fixation (ORIF) has been associated with good outcomes regardless of fracture pattern, or patient characteristics.8,13 In particular, accurate subtalar anatomic joint reduction and restoring the Böhler angle are key features to improved functional outcomes and lower rates of secondary subtalar arthrodesis.
However, ORIF can be difficult in complex cases with comminuted intercalary fragments. 16 The extensile lateral approach (ELA) has been the gold standard for calcaneal ORIF because of the wide surgical exposure and ease of manipulation of fracture fragments. 4 However, it has been associated with significant wound complications, limiting its advantage over nonoperative treatment in different trials.4,9,10
On the other hand, the sinus tarsi approach (STA) is gradually becoming the standard surgical approach for calcaneal ORIF. 17 Recent data showed good functional and radiographic outcomes, with low morbidity and low rates of wound complications, making it one of the preferred surgical approaches among foot and ankle surgeons.7,11,20 However, the STA, with its narrow field of exposure, can represent a challenge to inexperienced surgeons dealing with complex intra-articular fractures of the calcaneus, leading to inferior quality of reduction. 6
The current article will describe a step-by-step technical note to successful ORIF of DIACF using a minimally invasive STA.
Surgical Technique
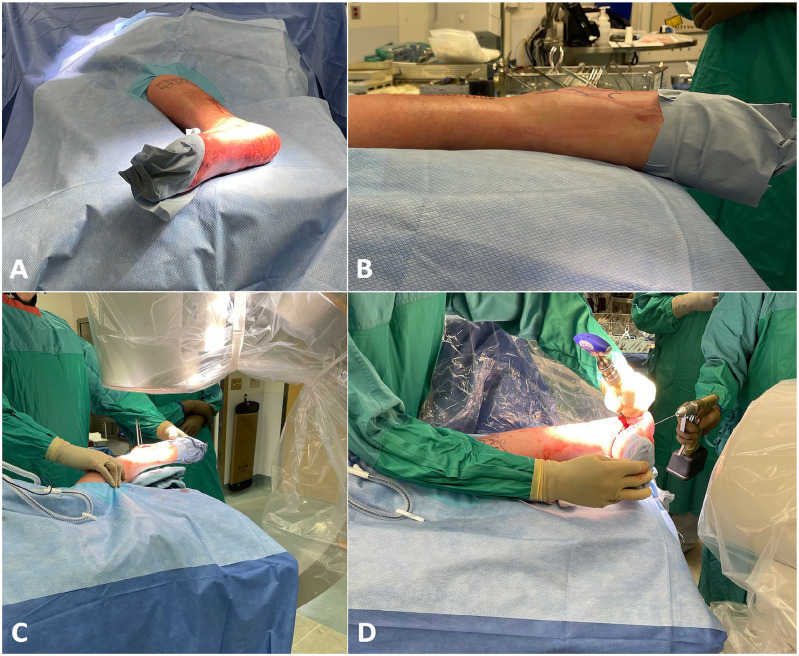
Patient Positioning and C-arm check (Figure 1)
Figure 1.
Patient positioning and C-arm intensifier setup. (A) The patient is placed in the lateral decubitus position with the operative side (left) up. (B) A bump is placed under the foot to elevate it and make it horizontal. The C-arm intensifier is positioned obliquely in order to obtain a (C) true lateral view as well as a (D) calcaneal axial view.
The patient is placed in the lateral decubitus position with the operative side facing upwards. A bump is placed under the foot to elevate it and make it strictly horizontal. The C-arm is positioned in an oblique plane in order to obtain simultaneously a true lateral view of the hindfoot as well as a calcaneal axial view. A mini-C-arm can be used if desired, but some of the surgical steps described below are typically performed under fluoroscopic control, and in particular in step 2, which can be challenging considering the smaller working space between the 2 arms.
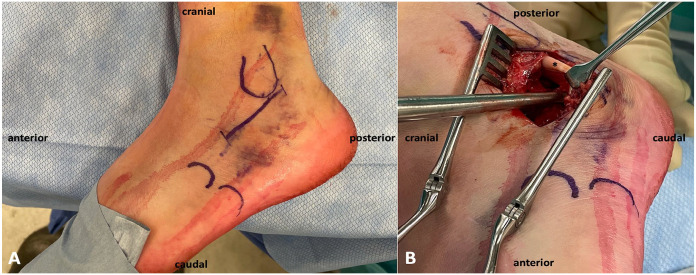
Surgical Approach
The surgeon stands on the dorsal side of the patient with the assistant on the other side. A 5-cm skin incision is started just below the tip of the lateral malleolus in line with the posterior malleolar cortex heading towards the base of the fourth metatarsal (Figure 2A).
Figure 2.
Superior views of a left foot. (A) Skin landmarks and incision. (B) Lateral wall blunt dissection. Careful dissection of the lateral wall as well as both proximal and distal edges of the calcaneal tuberosity in preparation for plate positioning. It is important to dissect proximal to the peroneal tendons (*), as this will make inferior retraction easier.
Dissection is carried bluntly above the peroneal tendons into the sinus tarsi with care to protect the peroneal tendons’ sheath. Care should also be taken to avoid injury to either the superficial peroneal or sural nerves, although this approach is often at a safe distance from both nerves’ trajectories. The sinus tarsi fat pad is then excised to expose the sinus tarsi space, the subtalar joint proximally and the anterior process distally. Care must be taken to avoid injury to the calcaneofibular ligament while exposing the subtalar joint at the proximal end of the incision. The next step is to bluntly dissect the lateral calcaneal wall using a large Cobb passed under the peroneal tendons. It is important to dissect proximal to the peroneal tendons, as this will make inferior retraction easier. Blunt dissection should be carried subperiosteally and should target the lateral wall as well as the calcaneal tuberosity to be able to reduce the bony fragments (Figure 2B).
Step-by-Step Approach to ORIF
There are 4 crucial steps to a successful reduction of a DIACF. Tables 1 and 2 highlight some tips to avoid expected pitfalls with this technique, in addition to the advantages and limitations of the STA.
Table 1.
Pearls and Pitfalls of the Surgical Technique.
| Pearls | Pitfalls |
|---|---|
| Maintaining the foot in a full lateral position will make fracture reduction and fluoroscopic assessment easier and more accurate | Avoid using the STA, or delay surgery, if excessive blistering around the incision field, as it could increase the risk of wound-related complications |
| A small needle can be used anteriorly to detect the calcaneocuboid joint line to avoid any capsular disruption | Attention should be paid to the peroneal tendons to avoid any iatrogenic injury during the approach |
| Subperiosteal blunt dissection of the lateral wall using a large Cobb is key to easier manipulation of the calcaneal tuberosity through the transcalcaneal Schanz pin and avoiding residual varus deformity | Avoid performing dissection between the subcutaneous layer and the peroneal tendons |
| During facet reduction, elevating the fragments against the talar facet to obtain full contact between both chondral surfaces is important to obtain good subtalar joint reduction | Accurate reduction of the posterior facet can be difficult because of limited exposure and the presence of multiple fragments. Thus, relying on the talar facet as a template is key to avoid malreduction and articular steps, which can be hard to detect by fluoroscopy |
| During facet elevation, start from the most medial and posterior part to the most lateral and anterior part | Severe comminution, especially of the intercalated subtalar fragments, can render articular anatomic reduction difficult. This could require additional bone grafting to hold the subtalar joint, or leaving pins in place temporarily if the fragments are small enough to prevent screw purchase |
| The plate should be inserted just below the articular surface to support the subchondral space and avoid any secondary joint depression, as show in Figure 6 | Avoid articular penetration of the subtalar joint during screw fixation. The axial view as shown in Figure 5 can confirm screw trajectory |
| Start plate fixation using a compression screw through the middle part of the plate to achieve good plate buttressing |
Abbreviation: STA, sinus tarsi approach.
Table 2.
Advantages and Disadvantages of the Surgical Technique.
| Advantages | Disadvantages |
|---|---|
| Applicable to most calcaneal fractures with intra-articular facet disruption, preferably in the acute setting within 7-10 days | Fragment manipulation and fracture reduction can be challenging if not performed within 7-10 days from date of injury |
| Limited skin incision, minimal soft tissue dissection, and nerve-sparing approach | Limited surgical exposure |
| Direct visualization of the subtalar joint, mainly of the middle facet and the anterior part of the posterior facet | Minimal visualization of the calcaneal tuberosity and the posterior facet, since the approach generally gives access to the anterior third of the posterior facet. Calcaneal tuberosity and posterior facet reduction is therefore guided by fluoroscopic views, which can be biased |
| Good safety profile with fewer wound complications compared to the ELA | Potential damage to the calcaneofibular ligament, but no reports of lateral instability with the STA, probably because of postoperative scarring |
| Moderate learning curve due to less visualization of the subtalar joint compared to the standard ELA; The hardest part is judging the reduction of the subtalar joint (step 3) |
Abbreviations: ELA, extensile lateral approach; STA, sinus tarsi approach.
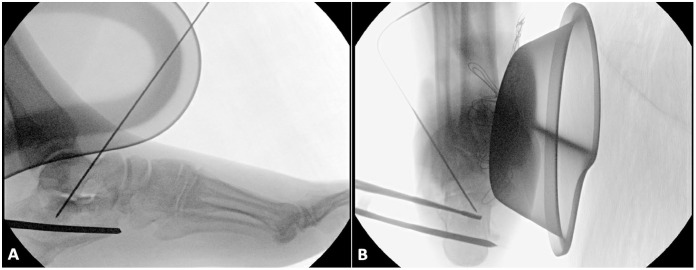
Step 1: Medial Wall Reduction (Figure 3)
Figure 3.
Fluoroscopic views (A, lateral view; B, axial view) of a left foot displaced intra-articular calcaneal fracture showing medial wall reduction. Once the medial wall is elevated against the talar chondral facet, a 1.6-mm Kirschner wire is used to pin it in place through a transtalar trajectory started from the superolateral talar cortex. A Howarth elevator was used in this case for reduction.
The first step of ORIF is to assess the medial wall stability, that is, the sustentacular fragment, which is not always stable, and can be displaced in half the cases. 3 If the medial fragment is stable, then we can proceed to the next step. If unstable, then the fragment should be reduced and fixed. The talar chondral facet can be used as template for reduction; The fragment should be reduced, usually by elevation, to become congruent and in full contact with the talar chondral facet. Once reduction is obtained, a percutaneous 1.6-mm Kirschner wire driven from the superior aspect of the talus is used to fix the medial wall temporarily. The wire should be started either medial to the anterior tibialis tendon or lateral to the extensor digitorum longus tendons to avoid injury to the anterior neurovascular bundle. A lateral fluoroscopic view at this point can confirm the position of the medial fragment through assessment of the medial subtalar joint.
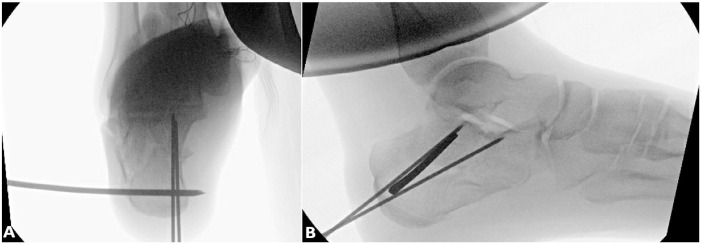
Step 2: Calcaneal Tuberosity Reduction (Figure 4)
Figure 4.
Fluoroscopic views (A, axial view; B, lateral view) of a left foot displaced intra-articular calcaneal fracture showing calcaneal tuberosity reduction. Two 1.6-mm Kirschner wires are used to fix the calcaneal tuberosity to the previously fixed medial wall. The axial view is used first to guide the wire trajectory, followed by the lateral view, which confirms the divergent pattern for a stable reduction. The fluoroscopic views used to illustrate this step and the following steps are taken from a separate operative case.
The fractured calcaneus often shows reduced height with a negative Böhler angle as well as a varus displacement on the axial views due to predominant varus forces of the Achilles tendon. The following step is therefore important to reduce both calcaneal height and varus displacement, in order to restore normal hindfoot alignment and prevent long-term sequalae.
Through a stab incision, a transcalcaneal 5-mm threaded pin is introduced from the lateral cortex into the inferior border of the calcaneal tuberosity with bicortical purchase. The pin can then be used as a joystick for easier reduction. Reduction often requires traction and medialization of the tuberosity with addition of a slight valgus moment to avoid varus deformity. The fluoroscopic axial view is used to confirm proper alignment. Once reduced, two 1.6-mm Kirschner wires are introduced percutaneously from the medial and inferior aspect of the tuberosity toward the medial wall fragment. For a right-handed surgeon operating on a right foot, the left hand is used to manipulate the pin and hold the reduction while the right hand is used to pin the fracture under fluoroscopic guidance. The 5-mm threaded pin can be removed at this point. A Steinmann pin can also be introduced into the tuberosity from posterior to anterior. However, although it could be easier to reduce the varus deformity from a posterior angle, it could make pinning it to the medial wall fragment harder to achieve.
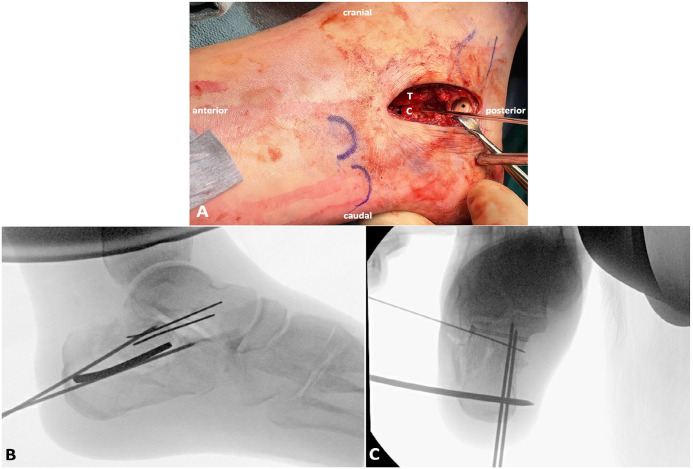
Step 3: Subtalar Joint Reduction (Figure 5)
Figure 5.
Subtalar joint reduction of a left foot displaced intra-articular calcaneal fracture. (A) Intraoperative superior view after retraction of the peroneal tendons (*). The calcaneal facet (C) is elevated against the talar facet (T) and pinned to the medial calcaneal part. (B, C) Fluoroscopic views (B, lateral view; C, axial view) confirming joint reduction. One or two 2.7-mm lag screws can be used for fixation. A cannulated design was used in this case. The lateral view (B) is important to confirm subtalar joint reduction and the axial view (C) to confirm the screw length.
The following step is performed under direct visualization after careful elevation of the lateral wall. The joint surface should be assessed to discern any intercalary fragments. Minor fragments unamenable to fixation and bearing chondral surface should be excised. Reduction is then achieved from medial to lateral to reconstruct the posterior facet anatomically. Both the medial facet and the talar facet are used to help with reduction assessment, but the key is to elevate the posterior calcaneal facet to obtain full contact with the talar facet and restore subtalar congruency (Figure 5A). A true lateral fluoroscopic view can confirm the reduction at this point (Figure 5B). Inability to obtain a clear view of the subtalar joint should raise suspicion for 1 or more malreduced subtalar fragments. However, judging the reduction can sometimes be hard or biased by fluoroscopy, which is important to rely on the talar undersurface to reconstruct the calcaneal posterior facet. An optimal alternative to assess medial reduction is the use of subtalar arthroscopy, which has shown to improve posterior facet reduction. 14 One or two 2.7-mm lag screws are then used for subtalar joint fixation in the subchondral space with bicortical purchase, aiming for the longest screws possible into the medial sustentacular cortex. With the foot strictly horizontal, often a straight vertical trajectory would target that area. A calcaneal axial view can be used to confirm the screw length (Figure 5C). It is important to sink the screw head sufficiently into the lateral cortex to avoid impingement with the plate. At this point, the subchondral space must be then assessed to decide if additional bone grafting is needed to support the subtalar joint. The lateral wall is finally reduced back to its position in preparation for plate positioning.
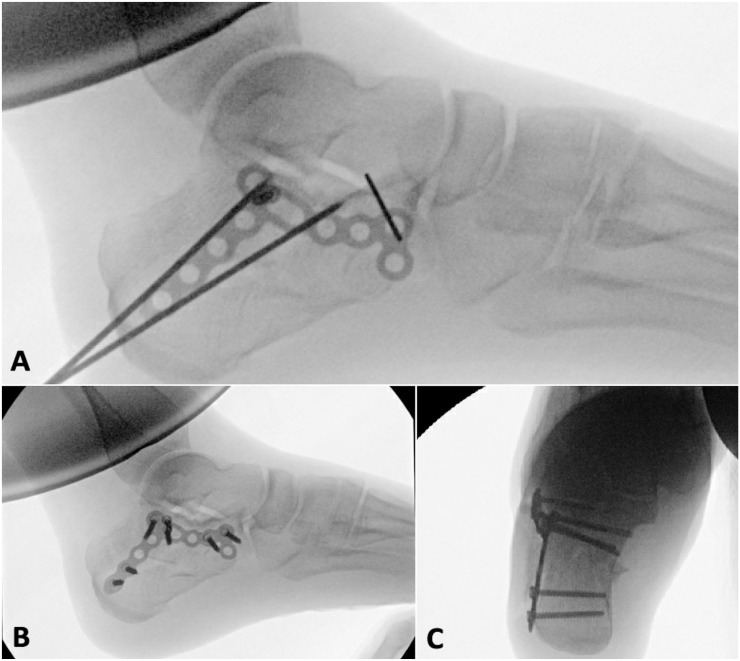
Step 4: Internal Fixation Using a Lateral Calcaneal Plate (Figures 6 and 7)
Figure 6.

Intraoperative superior view of the subtalar joint of a left foot displaced intra-articular calcaneal fracture after retraction of the peroneal tendons (*). The plate is buttressing the lateral wall of the calcaneus (C), with its middle part overlying the lag screw. The white dashed line indicates the stab wound incision used first to introduce the transcalcaneal reduction pin, and second to insert the screws targeting the calcaneal tuberosity.
Figure 7.
Fluoroscopic views (A, B, lateral views; C, axial view) of a left foot displaced intra-articular calcaneal fracture showing internal fixation with a calcaneal locking plate. (A) Correct plate positioning is confirmed with a lateral view, and a temporary wire fixing the anterior end of the plate allows fine control of the plate position prior to insertion of the first compression screw. Anatomic reduction is achieved with restored calcaneal height and subtalar joint (B), as well as a restored calcaneal axis (C).
The last step in ORIF is fixation of the remaining calcaneal fragments with a solid construct. The senior author’s (A.D.’s) preferred construct is the use of the percutaneous anatomic calcaneal fracture plate (Arthrex, Naples, FL). The plate’s posterior end is first introduced bluntly to cover the calcaneal tuberosity. The stab wound used to introduce the tuberosity pin can be used to aid plate positioning. The anterior end of the plate is then positioned to align anatomically with the anterior calcaneal process with care to avoid the calcaneocuboid joint. The middle segment should automatically align against the subchondral area of the subtalar joint (Figure 6). A lateral view is used to confirm plate positioning (Figure 7A). A combination of compression and locking screws are then used for fixation. At least 1 screw should be used in each of the 3 segments of the plate to have a stable construct. Additional screws can be used depending on bone quality and stability of the final construct. The calcaneal tuberosity screws can be introduced through the secondary stab incision. The subtalar and anterior process screws can be introduced through the main incision. Middle segment fixation is often started first using a 3.5-mm compression screw through the oblong hole of the plate to compress the plate and reduce the lateral wall. The remaining screws are locked to the plate after predrilling through the locking guides. Both lateral and axial views are then taken to confirm screw length and position, with care to avoid any articular penetration (Figure 7B and C).
Closure
The subcutaneous layer is closed with simple interrupted sutures. The skin is closed in a running fashion, using a No. 3.0 nylon suture. It is preferable to use a nonabsorbable suture to avoid any added risk of skin inflammation, and it can be kept more than 2 weeks in case of delayed wound healing.
Postoperative Protocol
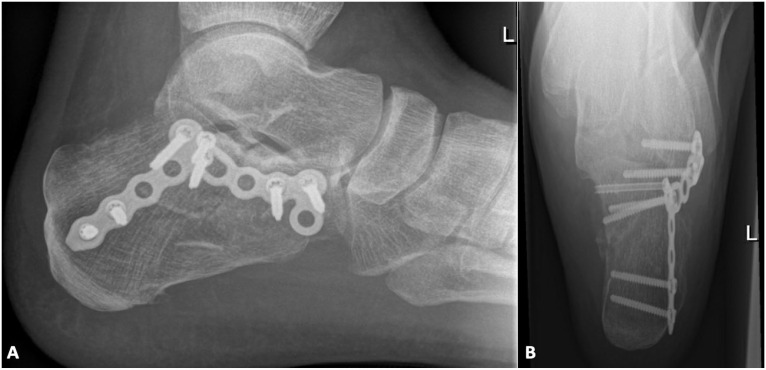
A posterior splint with the ankle in neutral dorsiflexion is used for 2 weeks. Passive and active range of motion is started the third week. The patient is kept nonweightbearing for 8 weeks in a walking boot, then full weight-bearing is initiated after radiographic assessment (Figure 8). Physical therapy at this point will focus on progressive strengthening, proprioception, and normal gait restoration. Return to sports with low-impact activities is allowed starting the fourth month, and with full activities by 6 months postoperatively.
Figure 8.
Postoperative radiographic views. A, lateral; B, axial.
Discussion
This article introduced a stepwise surgical approach to internal fixation of intra-articular calcaneal fractures through an STA, which can present a challenge to obtaining anatomic reduction.
Surgical management of DIACF has been shown to provide improved functional outcomes as well as long-term prevention of advanced posttraumatic osteoarthritis (OA) and lower rates of secondary fusions.8,13,21 Buckley and the Canadian Orthopedic Trauma Study (COTS) group conducted a multicenter randomized controlled trial (RCT) with 471 enrolled DIACF and showed better outcomes with surgical treatment compared with nonoperative treatment after excluding patients benefiting from worker’s compensation. 5 The COTS group also identified risk factors associated with poor outcomes and secondary subtalar fusion. 8 A negative Böhler angle was 10 times more likely to require secondary fusion. Sanders type IV fractures were 5.5 times more likely to require fusion. Similarly, Ågren et al 1 conducted a RCT with 76 patients enrolled having a DIACF. They showed better functional outcomes and reduced prevalence of posttraumatic OA in the operative group at 8-12 years of follow-up. More importantly, both Böhler angle and articular surface restoration were found to be correlated with superior outcomes. 2 The long-term benefit of surgical treatment against developing posttraumatic OA and the need of secondary subtalar fusion has also been shown when combining the evidence from different RCTs. 4 Moreover, initial ORIF was associated with better functional outcomes after subtalar fusion for symptomatic subtalar OA compared with initial nonoperative treatment. 15 Thus, appropriate reduction of DIACF is important not only to ensure improved short-term functional outcomes but also long-term outcomes, which can be life altering for most patients.
On the other hand, surgical treatment of calcaneal fractures can come at the cost of multiple complications, which can approach 20%. 21 These include infection, skin flap necrosis, neurovascular injury, malreduction, implant-related problems, and nonunion. Although these complications do occur with the STA, most of them are described with the ELA. This is in part due to the greater amount of literature written on the ELA as compared to the STA, which is only of late gaining more widespread use. Patient selection and timing of surgery are, therefore, crucial in the decision-making process when dealing with DIACF.
The optimal treatment for DIACF remains controversial. ORIF of calcaneal fractures through STA is gradually gaining attention because of its safety. Recent evidence comparing nonoperative to surgical treatment, including the standard ELA and the STA, favored the minimally invasive approaches considering the good radiographic outcomes and the lower incision-related complications. 18 In particular, patients who underwent STA exhibited a 96.4% satisfaction rate. The STA has proven to be reliable for reduction of DIACF as radiographic reduction has been shown to be similar between ELA and STA in Sanders type II and IV.6,12 ORIF through STA, therefore, could be a safer alternative to ELA in surgical treatment of DIACF.7,11 The currently described technique highlighted important steps that, when followed, can make reduction relatively easy when using an STA to address DIACF.
Conclusion
Anatomic reduction of complex calcaneal fractures can be achieved through a stepwise approach using the STA. Following the illustrated steps in order can render reduction easier, aiming for anatomic reduction and better functional outcomes.
Supplemental Material
Supplemental material, sj-pdf-1-fai-10.1177_10711007231165765 for A Stepwise Minimally Invasive Sinus Tarsi Approach to Open Reduction and Internal Fixation of Displaced Intra-articular Calcaneal Fractures: Technique Tip by Johnny Rayes, Paul Sharplin, Peter Maalouf, Scott Willms and Andrew Dodd in Foot & Ankle International
Footnotes
Ethical Approval: Ethical approval was not sought because the article is a surgical technique description. Patient consents were obtained for use of imaging.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Johnny Rayes, MD,  https://orcid.org/0000-0002-4158-7288
https://orcid.org/0000-0002-4158-7288
Scott Willms, MD,  https://orcid.org/0000-0002-4963-0383
https://orcid.org/0000-0002-4963-0383
References
- 1.Ågren PH, Wretenberg P, Sayed-Noor AS. Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures. A prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2013;95(15):1351-1357. [DOI] [PubMed] [Google Scholar]
- 2.Ågren PH, Mukka S, Tullberg T, Wretenberg P, Sayed-Noor AS. Factors affecting long-term treatment results of displaced intraarticular calcaneal fractures: a post hoc analysis of a prospective, randomized, controlled multicenter trial. J Orthop Trauma. 2014;28(10):564-568. [DOI] [PubMed] [Google Scholar]
- 3.Berberian W, Sood A, Karanfilian B, Najarian R, Lin S, Liporace F. Displacement of the sustentacular fragment in intra-articular calcaneal fractures. J Bone Joint Surg Am. 2013;95(11):995-1000. [DOI] [PubMed] [Google Scholar]
- 4.Bruce J, Sutherland A. Surgical versus conservative interventions for displaced intra-articular calcaneal fractures. Cochrane Database Syst Rev. 2013;(1):CD008628. [DOI] [PubMed] [Google Scholar]
- 5.Buckley R, Tough S, McCormack R, et al. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures. A prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2002;84(10):1733-1744. [DOI] [PubMed] [Google Scholar]
- 6.Busel G, Mir HR, Merimee S, et al. Quality of reduction of displaced intra-articular calcaneal fractures using a sinus tarsi versus extensile lateral approach. J Orthop Trauma. 2021;35(6):285-288. [DOI] [PubMed] [Google Scholar]
- 7.Ceccarini P, Manfreda F, Petruccelli R, Talesa G, Rinonapoli G, Caraffa A. Minimally invasive sinus tarsi approach in sanders II-III calcaneal fractures in high-demand patients. Med Glas. 2021;18(1):1-6. [DOI] [PubMed] [Google Scholar]
- 8.Csizy M, Buckley RE, Tough S, et al. Displaced intra-articular calcaneal fractures: variables predicting late subtalar fusion. J Orthop Trauma. 2003;17(2):106-112. [DOI] [PubMed] [Google Scholar]
- 9.Dickenson EJ, Parsons N, Griffin DR. Open reduction and internal fixation versus nonoperative treatment for closed, displaced, intra-articular fractures of the calcaneus: long-term follow-up from the HeFT randomized controlled trial. Bone Joint J. 2021;103-B(6):1040-1046. [DOI] [PubMed] [Google Scholar]
- 10.Griffin D, Parsons N, Shaw E, et al. ; UK Heel Fracture Trial Investigators. Operative versus non-operative treatment for closed, displaced, intra-articular fractures of the calcaneus: randomised controlled trial. BMJ. 2014;349(July):1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khazen G, Rassi CK. Sinus tarsi approach for calcaneal fractures: the new gold standard? Foot Ankle Clin. 2020;25(4):667-681. [DOI] [PubMed] [Google Scholar]
- 12.Lin J, Xie C, Chen K, et al. Comparison of sinus tarsi approach versus extensile lateral approach for displaced intra-articular calcaneal fractures Sanders type IV. Int Orthop. 2019;43(9):2141-2149. [DOI] [PubMed] [Google Scholar]
- 13.Liu GT, Vanpelt MD, Lalli T, Raspovic KM, Wukich DK. Surgical management of displaced intra-articular calcaneal fractures: what matters most? Clin Podiatr Med Surg. 2019;36(2):173-184. [DOI] [PubMed] [Google Scholar]
- 14.Park CH, Yoon DH. Role of subtalar arthroscopy in operative treatment of Sanders type 2 calcaneal fractures using a sinus tarsi approach. Foot Ankle Int. 2018;39(4):443-449. [DOI] [PubMed] [Google Scholar]
- 15.Radnay CS, Clare MP, Sanders RW. Subtalar fusion after displaced intra-articular calcaneal fractures: does initial operative treatment matter? J Bone Joint Surg Am. 2009;91(3):541-546. [DOI] [PubMed] [Google Scholar]
- 16.Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures: results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. 1993;290:87-95. [PubMed] [Google Scholar]
- 17.Schepers T. Fixation by open reduction and internal fixation or primary arthrodesis of calcaneus fractures: indications and technique. Foot Ankle Clin. 2020;25(4):683-695. [DOI] [PubMed] [Google Scholar]
- 18.Shi FL, Wu SY, Cai W, Zhao YM. Comparison of 5 treatment approaches for displaced intra-articular calcaneal fractures: a systematic review and bayesian network meta-analysis. J Foot Ankle Surg. 2020;59(6):1254-1264. [DOI] [PubMed] [Google Scholar]
- 19.van der Vliet QMJ, Lucas RC, Velmahos G, et al. Foot fractures in polytrauma patients: injury characteristics and timing of diagnosis. Injury. 2018;49(6):1233-1237. [DOI] [PubMed] [Google Scholar]
- 20.Wang CS, Tzeng YH, Yang TC, Lin CC, Chang MC, Chiang CC. Radiographic and clinical results of modified 2-incision sinus tarsi approach for treatment of calcaneus fracture. Injury. 2021;52(7):1971-1977. [DOI] [PubMed] [Google Scholar]
- 21.Wei N, Zhou Y, Chang W, Zhang Y, Chen W. Displaced intra-articular calcaneal fractures: classification and treatment. Orthopedics. 2017;40(6):e921-e929. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-fai-10.1177_10711007231165765 for A Stepwise Minimally Invasive Sinus Tarsi Approach to Open Reduction and Internal Fixation of Displaced Intra-articular Calcaneal Fractures: Technique Tip by Johnny Rayes, Paul Sharplin, Peter Maalouf, Scott Willms and Andrew Dodd in Foot & Ankle International