Abstract
Introduction
Compulsory treatment has decades of history in Iran; both before and after the Islamic Revolution, but there are many debates regarding its efficacy and effectiveness. Retention Rate is one of the best indices to estimate the efficacy of treatment. This study will compare Retention Rate among people referred from compulsory treatment centers and volunteer participants.
Methods
This was a retrospective (historical) cohort study that has been conducted among people who were taking methadone maintenance treatment (MMT). The study sample was selected from the MMT centers that admit both referral patients from compulsory centers and voluntary patients. All newly admitted patients from March 2017 to March 2018 were enrolled and followed up until March 2019.
Results
A total of 105 participants were recruited for the study. All were males with a mean age of 36.6 ± 7.9 years. Fifty-six percent of individuals were referred from compulsory residential centers. The total one-year retention rate of participants in this study was 15.84%. The one-year retention rate for the patients referred from compulsory residential centers and the non-referred patients was 12.28 and 20.45%, respectively (value of p = 0.128). Among the other studied factors, only marital status was significantly associated with MMT retention (p = 0.023).
Conclusion
Although the average treatment adherence time for non-referred patients was about 60 days higher than those referred from compulsory residential centers, this study found no significant differences in retention days and a one-year retention rate. Further studies with larger sample sizes and longer follow-ups are needed to explore the efficacy of compulsory treatment methods in Iran.
Keywords: compulsory treatment, volunteer treatment, methadone maintenance treatment, retention rate, Iran
1. Introduction
One of the greatest challenges for various parts of the community, including the judicial system, law enforcement, and undoubtedly the health system, is substance use around the world. In Iran, substance use accounts for a significant portion of the Disability Adjusted Life Years (DALY) and the Years Lived with Disability (YLD) index (1). According to estimations, Iran’s DALY index and YLD index are 698 per 100,000 people and 11.1 (2), respectively. The severity of the issue in Iran is evidenced by comparing with the average number of these indices in the world, which is 200 per 100,000 people and 4 per 100,000 (3).
Iran moved from conservative and criminalization programs towards a more liberal approach for medicalized drug addiction treatment and harm reduction with consequential drawbacks during the last 40 years after the Islamic Revolution. Contradictory liberal and conservative addiction treatment programs exist simultaneously in Iran’s current drug addiction treatment scene (4).
Since roughly 17 years ago (2003–2004), a significant network of outpatient substance use treatment clinics has been established in Iran. Currently, there are about 7,000 clinics with about 700,000 patients undergoing opioid substitution therapy (mostly methadone maintenance therapy) in the country (5).
Other than traditional opioid use among Iranian substance users, another substance use disorder that increased in the first decade of the new century was methamphetamine use. Methamphetamine seizures were reported in Iran for the first time in 2005 and scaled up as fast as that, putting Iran fifth in the world in 2010–2011 based on the number of methamphetamine seizures (6). It is essential to mention that methamphetamine use among the patients undergoing MMT is also common and many patients started using methamphetamine to cope with methadone side effects such as sexual dysfunction as well as lethargy and drowsiness (7, 8). One study reported that nearly 90% of female patients taking methadone from the MMT clinics were using methamphetamine to some degree simultaneously (9). In response to this situation, a guideline for the integration of methamphetamine harm reduction interventions into the ordinary harm reduction services for opioid users was developed by the ministry of health with support of the UNODC, Tehran (10).
Unfortunately, the issue still exists despite this extensive network of treatment centers and an almost adequate network of services and facilities for harm reduction, including Drop-in Centers (DIC), outreach teams, and hundreds of midterm residential campuses. Following an increased number of people with problematic substance use disorders, and public and political demand for more strict policies towards drug use, compulsory treatment programs which were on the path to decline, were scaled up again; especially after the emergence of the methamphetamine crisis.
People who use drugs (PWUD) were given the option of being sentenced to compulsory treatment if they refused to participate in a treatment program or harm reduction service or caused a public nuisance under a new amendment to the drug control law that took effect in 2010 (Iran Council of Expediency 2010, article 16). These compulsory rehabilitation centers offer OST or abstinence-based programs in a residential setting for a few months and are designed to be formally governed in a court-based setting. People who receive OST services later contact DICs to continue receiving maintenance treatments at a partial or full subsidized cost. Compulsory treatment has more than 50 years of history, as we can trace the first experiences back to 1961 in the United States (11). Iran also has a history of compulsory medical intervention both before and after the Islamic Revolution. There are still numerous arguments over its efficacy. Retention rate, one of the indicators that can be used to gage the effectiveness of the treatment, is impacted by a variety of circumstances (12–15).
Although some scientists made efforts to justify compulsory treatment with the rationale that long-lasting changes in the brain, hijack a person’s ability to refrain from drug use, and in this condition, others are allowed to put patients in a compulsory rehabilitation centers, some studies showed these models might have negative consequences for the patient rather than being effective (16). It is necessary to consider that there are many debates against compulsory treatment. i.e., a review evaluated the clinical effectiveness of compulsory treatment, and concluded that current evidence does not support the idea that compulsory treatment modalities are effective for drug dependence treatment. Some studies even suggest it to be harmful (17, 18).
In the Lancet Global Health, Martin Wegman and colleagues present their study of opioid use in opioid-dependent individuals released from compulsory drug detention centers (CDDCs) compared with those from voluntary methadone treatment centers (VTCs) in Malaysia. This study was the first prospective observational study to compare drug-use outcomes between the two facility types. The investigators showed that opioid-dependent individuals in CDDCs were significantly more likely to relapse to opioid use after release than opioid-dependent individuals receiving methadone in VTCs (in unadjusted analyses, CDDC participants had a significantly more rapid relapse to opioid use post-release compared with VTC participants [median time to relapse 31 days (IQR 26–32) vs. 352 days (256–inestimable), log-rank test p < 0·0001) (19)].
Studies in Iran found some factors influencing retention rates in treatment, such as methadone dose, polysubstance use, being treated in private or governmental clinics, (20), stimulant drug use, comorbidity disorders (21), distance to a clinic, perceived social support, and perceived pleasure with drug use (22). A qualitative study also revealed that treatment cost and family support are among the factors that can influence the retention rate in treatment (23).
Although the recent wave of compulsory treatment in Iran has lasted for nearly a decade, only a few independent studies have evaluated the effectiveness of these models compared to the voluntary-based modalities. To our knowledge this is one of the first studies in this field in Iran that has tried to find the retention rate of patients referred from compulsory treatment centers compared to those who are coming by their own will.
2. Materials and methods
2.1. Study design
This study was a retrospective cohort study. The study population was made up of patients who were taking methadone maintenance treatment (MMT) for the treatment of drug use. The study sample was selected from the ‘Haftoon’ MMT center. This center receives both volunteer individuals in addition to referred patients from compulsory rehabilitation centers in the city of Isfahan, Iran. Eligibility criteria include (1) age more than 18 years, and (2) being qualified for MMT based on the ministry of health protocol for MMT which recommend MMT for patients with one of these criteria:
Current heroin user
Opioid users with a history of injection of any drug
History of two-time failed abstinence treatment for opioid users
People living with HIV
and (3) referred from the judicial system and/or voluntarily admitted patients for MMT.
All newly admitted patients during the years 1,396 and 1,397 (March 21st, 2017 to March 20th, 2018) in the mentioned center were enrolled in the study and were followed up until March 20th, 2019. Patients whose follow-up data were missing and their treatment status was unclear were excluded from the study. The National Institute approved this study for the Medical Research Development (NIMAD) review board, and the following ethical approval code was granted: IR.NIMAD.REC.1398.123.
2.2. Data sources and measures
The study utilized the physical files, which are typically used for routine clinical and program monitoring. A researcher made questionnaire was used to collect demographic, drug history, mental health, and HIV risk behavior data, for each MMT client. Demographic data included age (in years), education level (primary-level schooling or less/more than primary-level schooling) and marital status (currently married/not married); Injection-related risk factors included shared needle use at last injection, shared other equipment at last injection, cleaned needles with bleach if sharing at the last injection, and poly-substance use (heroin and alcohol, cocaine, benzodiazepines, or amphetamine). Date of entry, possible date of drop-out, methadone daily dose, and days spent in compulsory rehabilitation centers were acquired from patient files.
Retention was defined as the number of days from entering the study to the end of the study or leaving the treatment. Two weeks of missed appointments were considered a drop-out for patients.
2.3. Statistical methods
Descriptive measures were used to describe the patients’ characteristics, including frequencies, mean, and standard deviation. The life tables and the Kaplan–Meyer method were used to calculate the retention rate for each group and compare between groups; the Cox proportional hazard model was used to find the factors associated with retention rate. The Hazard Ratio and 95% Interval for each variable are presented. Also, the level of significance was set at 0.05. All the analysis was carried out by SPSS software version 26.
3. Results
3.1. Study characteristics
A total of 105 patients were recruited; due to incomplete follow-up data, four were excluded from the study. All 101 participants were male, and 56.4% were referred from compulsory residential centers. Upon entry, they had a mean age of 36.5 years (SD = 7.9 years), and the age range was from 20 to 65 years. Nearly half were married (50.5%), and only 5% were HIV positive. Most of them used heroin (10.9%), and smoking was the most common route for substance use among them (11.9%). At the time of admission, the mean dose was 50.1 ± 18 mg, and the mean of the final dose that participants received was 61.5 ± 29. Analysis showed no difference in demographics except for the admission dose of methadone, which was higher in the referred group. Demographic characteristics are available in Table 1.
Table 1.
Demographic characteristics of participants.
| General | Referred from compulsory centers | Volunteer group | Value of p | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | Groups | Number | Percentage | Number | Percentage | Number | Percentage | |
| Referral | Yes | 57 | 56.4 | |||||
| No | 44 | 43.6 | ||||||
| Age | <30 | 21 | 20.8 | 15 | 26.3 | 6 | 13.6 | 0.053 |
| 31–40 | 53 | 52.5 | 32 | 56.1 | 21 | 47.7 | ||
| 41–50 | 21 | 20.8 | 9 | 15.8 | 12 | 27.3 | ||
| >50 | 6 | 5.9 | 1 | 1.8 | 5 | 11.4 | ||
| Marital status | Single | 50 | 49.5 | 29 | 50.9 | 21 | 47.7 | 0.754 |
| Married | 51 | 50.5 | 28 | 49.1 | 23 | 52.3 | ||
| HIV status | Negative | 96 | 95 | 56 | 98.2 | 40 | 90.9 | 0.092 |
| Positive | 5 | 5 | 1 | 1.8 | 4 | 9.1 | ||
| Main drug used | Heroin | 11 | 10.9 | 11 | 19.3 | - | - | - |
| Opium Juice | 1 | 1.0 | 1 | 1.8 | - | - | ||
| Opium | 1 | 1.0 | 1 | 1.8 | - | - | ||
| Crack | 1 | 1.0 | 1 | 1.8 | - | - | ||
| Missing | 87 | 86.1 | 43 | 75.4 | 44 | 100 | ||
| Main route of administration | Smoking | 12 | 11.9 | 11 | 19.3 | 1 | 2.3 | 0.875 |
| Injection | 2 | 2.0 | 2 | 3.5 | - | - | ||
| Oral | 1 | 1.0 | 1 | 1.8 | - | - | ||
| Missing | 86 | 85.1 | 43 | 75.4 | 43 | 97.7 | ||
| Admission dose | <50 | 41 | 40.6 | 15 | 26.3 | 26 | 59.1 | 0.002 |
| > = 50 | 60 | 59.4 | 42 | 73.7 | 18 | 40.9 | ||
| Final dose | <50 | 27 | 26.7 | 12 | 21.1 | 15 | 34.1 | 0.814 |
| > = 50 | 74 | 73.3 | 45 | 78.9 | 29 | 65.9 | ||
3.2. Retention rate
The total median of retention days was 92 days; 80 (79.2%) of participants did not adhere to treatment; the median of retention in non-adherent patients was 61.5 days, and the mean was 105.6 ± 108.9 days.
The median retention days for referred patients were 90 days, and for non-referred patients, it was 153 days. The life tables and the Kaplan–Meier method were used to calculate and compare retention durations totally and, in each group, separately. The retention rate between the two groups was not significantly different (p-value = 0.125; Figure 1). Six-month and one-year retention rates among participants receiving MMT voluntarily were higher compared to the referred patients (value of p = 0.093 & 0.128, respectively; Table 2).
Figure 1.
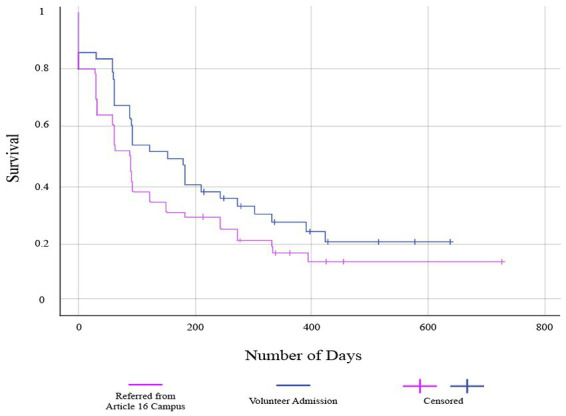
Retention rate among volunteers and patients referred from compulsory treatment centers.
Table 2.
6 Months and 1 year retention rate.
| Retention rate % | p-value | |||
|---|---|---|---|---|
| Total | Referred from compulsory centers | Volunteer group | ||
| 6 months | 39.60 | 31.57 | 50.0 | 0.093 |
| 1 year | 15.84 | 12.28 | 20.45 | 0.128 |
3.3. COX regression
Being referred from compulsory rehabilitation centers, age, marital status, admission dose, final dose, and HIV status were entered into the model; among them, only marital status was significantly associated with MMT retention, as married participants were more likely to adhere to treatment (p = 0.023); detailed associations with all variables for both referral groups are mentioned in Table 3.
Table 3.
Cox’s proportional hazards model analyses on factors associated with retention duration.
| Variable | Groups | Article 16 referred group | Volunteer group | total | |||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | ||
| Referred from compulsory centers | Yes | Ref | |||||
| no | - | - | - | - | 1.39 | 0.89–2.18 | |
| Age group | 20–29 | Ref | |||||
| 30–39 | 0.76 | 0.36–1.60 | 0.79 | 0.24–2.96 | 0.74 | 0.39–1.38 | |
| >40 | 0.73 | 0.31–1.73 | 0.73 | 0.22–2.82 | 0.66 | 0.34–1.32 | |
| Marital status | Single | Ref | |||||
| Married | 1.90* | 1.05 – 3.45 | 1.33 | 0.67–2.65 | 1.67* | 1.07 – 2.61 | |
| Admission dose | <50 | Ref | |||||
| > = 50 | 1.61 | 0.98–2.92 | 0.73 | 0.31–1.69 | 1.32 | 0.84–2.05 | |
| Final dose | <50 | Ref | |||||
| > = 50 | 0.79 | 0.44–1.44 | 2.0 | 0.99–4.03 | 1.17 | 0.75–1.83 | |
| HIV status | positive | Ref | |||||
| negative | 0.04 | 0.0–189 | 0.40 | 0.09–1.7 | 0.30 | 0.07–1.23 | |
p-Value < 0.05.
4. Discussion
In this study, we aimed to compare retention rates in voluntary and compulsory MMT treatment, which is an essential step in determining the effectiveness of drug detention (24). The results showed that the median retention days for the referred patients were lower than for voluntary patients (90 days vs. 153 days) but this was not statistically significant, which could be due to small sample size. Also marital status was the only factor affecting the retention, and married participants had higher retention duration.
The total one-year retention rate of participants in this study was 15.84%. A systematic review of 63 observational studies of opioid substitution treatment reported a 57% retention rate in 1 year (25). One of the reasons for this difference could be that the study mentioned above included MMT, buprenorphine, and mixed substantive opioid treatments, whereas our study only included MMT. In our study, the mean final dose of methadone was 61.5 mg/day, which was lower than in similar studies. Methadone dose has been shown to be an important factor in retaining patients on treatment. Likewise, in heroin users, doses higher than 80 mg/day predicted higher retention (26–28). The low-dose methadone also could be one of the other reasons for the lower retention rate in our study, which must be addressed in an appropriate manner by the responsible authorities considering the risk of diversion and overdose. It is good to mention that in another study that had been conducted in Iran, the average daily dose was 57.06 ± 18.04 mg/day, and the higher dose was known to have higher chance of one-year retention in the treatment (20).
The ethical dilemma of forced addiction treatment is complex from a public health perspective. Substance use disorders create a real threat to public health, and give governments and other formal institutions a justification to intervene in the lives of people who use drugs (PWUD). It must also be considered whether the benefits outweigh any negative consequences resulting from violating the individual’s right to make their own decisions about treatment. it is not clear whether the exposure to compulsory treatment is ultimately beneficial or harmful in the long term for the individual and for the public (29).
People in voluntary MMT have a stronger sense of ownership over their treatment and, consequently, are more likely to stay longer on treatment (30). In contrast, it is believed that those referred from compulsory residential centers may be less motivated to continue treatment after being released from the detention center. A study comparing the readiness to change and treatment in voluntary and compulsory treatment showed that although the compulsory patients scored significantly lower levels of motivation than the voluntary patients, both the compulsory and the voluntarily admitted patients were mostly at the highest level of readiness to seek help on admission and discharge, and that the change readiness stage at admission did not predict retention in treatment (31). In our study, the level of motivation was not assessed, but the results showed that the treatment of voluntary participants and those referred patients was equally effective in retaining patients. A cross-sectional study in China showed that occupation, family support, and social function equally increased in both voluntary and compulsory drug use rehabilitation centers after treatment (32).
In this study patients referred from compulsory residential centers had a higher admission dose but the final dose in the two groups was not significantly different. The decision for the initial dose is based on the clinical evaluation of the patient’s condition, the type and amounts of illicit drug use, and opioid tolerance (33); so this difference could be due to different types and amounts of previous drug use. The data about the type of drug used is missing in the voluntary group and we are not able to compare patients referred from compulsory treatment and voluntary patients in this category. The analysis of other demographic characteristics showed no other significant difference between these two groups. Among referred patients, heroin and other opioids were the most common type of drug used. A study in residential drug treatment centers in Iran showed that 72.5% of the patients were opioid users (34), also the rapid situation assessments in Iran almost always found that opioid substances are in the top of list among Iranian PWUD; which shows the importance of MMT treatment in Iran (35–37).
G.M. Heyman evaluated age of onset for substance use and explored that the most of PWUD in the US stop using illegal drugs around the age 30, due to legal concern, economic pressure, and desire for respect from their family members (38). Another qualitative study in Iran found that stigma from the family plays an important role for treatment adherence among the People living with HIV (39). In parallel with these findings, among the factors evaluated in this study only marital status significantly correlated with the duration of retention in MMT and married participants were more likely to stay on treatment. A systematic review found age, marital status, employment status, and gender to be positively associated with adherence to treatment with methadone (25). In our study, all of the included patients were male and employment status was not evaluated. The effect of age was not statistically significant in our study.
5. Conclusion
This study showed no significant difference in the retention rate between patients referred from the compulsory residential centers and those who voluntarily joined MMT treatment. Among the factors assessed in this study, only marital status significantly correlated with the retention rate —married patients stayed longer in treatment.
6. Limitations
This study was conducted at a single center over a period of 1 year. Designing a multi-center study with a longer data collection time will help to get a better understanding of the effectiveness of compulsory treatment in Iran. Data about the type of illicit drug used was missing in the voluntary treatment group, making it impossible for us to assess its effect on treatment retention and to compare the two groups. Illicit drug use during MMT treatment could be one of the confounding factors. Future studies can use urine toxicology results to compare and control the effects of illicit drug use in compulsory and voluntary participants.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was approved by the National Institute for Medical Research Development (NIMAD) review board and the following ethical approval code was granted: IR.NIMAD.REC.1398.123. The patients/participants provided their written informed consent to participate in this study.
Author contributions
For this study, AT-B and RR worked on the idea and design of the study. RR and NR gathered and organized the data. AAm performed the statistical analysis. AAz and FM wrote the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the “National Institute for Medical Research Development” under Grant number 977086.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We sincerely acknowledge the help and support provided by the “Haftoon” MMT center personnel and also the “National Institute of Medical Research Development.”
References
- 1.Naghavi M, Abolhassani F, Pourmalek F, Moradi Lakeh M, Jafari N, Vaseghi S, et al. The burden of disease and injury in Iran 2003. Popul Health Metrics. (2009) 7:1–21. doi: 10.1186/1478-7954-7-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Organization WH . Atlas: Substance use in the eastern Mediterranean region 2015. (2017)
- 3.World Health Organization . Atlas on substance use (2010): resources for the prevention and treatment of substance use disorders. Geneva: World Health Organization. (2010). [Google Scholar]
- 4.Ekhtiari H, Noroozi A, Farhoudian A, Radfar SR, Hajebi A, Sefatian S, et al. The evolution of addiction treatment and harm reduction programs in Iran: a chaotic response or a synergistic diversity? Addiction. (2020) 115:1395–403. doi: 10.1111/add.14905 [DOI] [PubMed] [Google Scholar]
- 5.Education M of H and M . Islamic Republic of Iran Progress report on monitoring of United Nations general assembly special session (UNGASS) on HIV and AIDS. Secretariat NAC, editor. (2014).
- 6.Radfar SR, Rawson RA. Current research on methamphetamine: epidemiology, medical and psychiatric effects, treatment, and harm reduction efforts. Addiction Health. (2014) 6:146–54. PMID: [PMC free article] [PubMed] [Google Scholar]
- 7.Radfar SR, Cousins SJ, Shariatirad S, Noroozi A, Rawson RA. Methamphetamine use among patients undergoing methadone maintenance treatment in Iran; a threat for harm reduction and treatment strategies: a qualitative study. Int J High Risk Behav Addiction. (2016) 5:1–8. doi: 10.5812/ijhrba.30327 [DOI] [Google Scholar]
- 8.Shariatirad S, Maarefvand M, Ekhtiari H. Methamphetamine use and methadone maintenance treatment: an emerging problem in the drug addiction treatment network in Iran. Int J Drug Policy. (2013) 24:e115–6. doi: 10.1016/j.drugpo.2013.05.003, PMID: [DOI] [PubMed] [Google Scholar]
- 9.Massah O, Moradi A. The prevalence of methamphetamine dependence among Iranian women in methadone maintenance therapy in Tehran, Iran. Iranian J Psychiatry. (2018) 13:10–4. PMID: [PMC free article] [PubMed] [Google Scholar]
- 10.Radfar SR, Mohsenifar S, Noroozi A. Integration of methamphetamine harm reduction into opioid harm reduction services in Iran: preliminary results of a pilot study. Iranian J Psychiatry Behav Sci. (2017) 11:1–7. doi: 10.5812/ijpbs.7730 [DOI] [Google Scholar]
- 11.Anglin MD, Hser Y-I. Treatment of drug abuse. Crime Justice. (1990) 13:393–460. doi: 10.1086/449179 [DOI] [Google Scholar]
- 12.Leukefeld CG, Tims FM. Drug abuse treatment in prisons and jails (Book). Rockville, MD, United States: Department of Health and Human Services Public Health Services. (1992) 299. [Google Scholar]
- 13.Joe GW, Simpson DD, Broome KM. Effects of readiness for drug abuse treatment on client retention and assessment of process. Addiction-Abingdon. (1998) 93:1177–90. doi: 10.1080/09652149835008 [DOI] [PubMed] [Google Scholar]
- 14.Hubbard RL, Craddock SG, Flynn PM, Anderson J, Etheridge RM. Overview of 1-year follow-up outcomes in the drug abuse treatment outcome study (DATOS). Psychol Addict Behav. (1997) 11:261–78. doi: 10.1037/0893-164X.11.4.261 [DOI] [Google Scholar]
- 15.Wild TC, Roberts AB, Cooper EL. Compulsory substance abuse treatment: an overview of recent findings and issues. Eur Addict Res. (2002) 8:84–93. doi: 10.1159/000052059, PMID: [DOI] [PubMed] [Google Scholar]
- 16.Carter A, Hall W. From coerced to compulsory treatment of addiction in the patient’s best interests: is it supported by the evidence? In: Critical perspectives on coercive interventions: Routledge; (2018). 14–29. [Google Scholar]
- 17.Werb D, Kamarulzaman A, Meacham MC, Rafful C, Fischer B, Strathdee SA, et al. The effectiveness of compulsory drug treatment: a systematic review. Int J Drug Policy. (2016) 28:1–9. doi: 10.1016/j.drugpo.2015.12.005, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lunze K, Lermet O, Andreeva V, Hariga F. Compulsory treatment of drug use in southeast Asian countries. Int J Drug Policy. (2018) 59:10–5. doi: 10.1016/j.drugpo.2018.06.009, PMID: [DOI] [PubMed] [Google Scholar]
- 19.Bergenstrom A, Vumbaca G. Compulsory drug detention centres: time to question their continued use? Lancet Glob Health. (2017) 5:e123–4. doi: 10.1016/S2214-109X(16)30352-7, PMID: [DOI] [PubMed] [Google Scholar]
- 20.Fathollahi MS, Torkashvand F, Najmeddin H, Rezaeian M. Predictors of one-year retention in methadone maintenance treatment (MMT) in Iran, Rafsanjan. Int J High Risk Behav Addiction. (2016) 5:1–7. doi: 10.5812/ijhrba.29121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pashaei T, Moeeni M, Roshanaei Moghdam B, Heydari H, Turner NE, Razaghi EM. Predictors of treatment retention in a major methadone maintenance treatment program in Iran: a survival analysis. J Res Health Sci. (2014) 14:291–5. PMID: [PubMed] [Google Scholar]
- 22.Shirinbayan P, Rafiey H, Roshan AV, Narenjiha H, Farhoudian A. Predictors of retention in methadone maintenance therapy: a prospective multi-center study. J SR, Essays. (2010) 5:3231–6. [Google Scholar]
- 23.Khazaee-Pool M, Moeeni M, Ponnet K, Fallahi A, Jahangiri L, Pashaei T. Perceived barriers to methadone maintenance treatment among Iranian opioid users. Int J Equity Health. (2018) 17:1–10. doi: 10.1186/s12939-018-0787-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dearing Barrick C, Dermen KH, Walitzer KSRL. Indicators of client engagement: influences on alcohol treatment satisfaction and outcomes. Psychol Addict Behav. (2005) 19:71–8. doi: 10.1037/0893-164X.19.1.71, PMID: [DOI] [PubMed] [Google Scholar]
- 25.O’Connor AM, Cousins G, Durand L, Barry J, Boland F. Retention of patients in opioid substitution treatment: a systematic review. PLoS One 20200514th ed. (2020) 15:e0232086. doi: 10.1371/journal.pone.0232086, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Farrell M, Ward J, Mattick R, Hall W, Stimson GV, Des Jarlais D, et al. Fortnightly review: methadone maintenance treatment in opiate dependence: a review. BMJ. (1994) 309:997–1001. doi: 10.1136/bmj.309.6960.997, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joseph H, Stancliff S, Langrod J. Methadone maintenance treatment (MMT): a review of historical and clinical issues. Mount Sinai J Med, New York. (2000) 67:347–64. PMID: [PubMed] [Google Scholar]
- 28.Cao X, Wu Z, Rou K, Li L, Lin C, Wang C, et al. Retention and its predictors among methadone maintenance treatment clients in China: a six-year cohort study. Drug Alcohol Depend. (2014) 145:87–93. doi: 10.1016/j.drugalcdep.2014.09.776, PMID: [DOI] [PubMed] [Google Scholar]
- 29.Urbanoski KA. Coerced addiction treatment: client perspectives and the implications of their neglect. Harm Reduct J. (2010) 7:13–07. doi: 10.1186/1477-7517-7-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WHO U . Principles of drug dependence treatment. Geneva: WHO; (2008). [Google Scholar]
- 31.Opsal A, Kristensen Ø, Clausen T. Readiness to change among involuntarily and voluntarily admitted patients with substance use disorders. Subst Abuse Treat, Prevent, Policy. (2019) 14:47. Available from. doi: 10.1186/s13011-019-0237-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang K, Yu CH, Chen XX, Hao YZ, Ding YD, Wu ZZ, et al. A quasi-experimental study on the effectiveness of compulsory and voluntary treatment settings for 1,299 drug abusers in Hunan, China. Front Psychiatry. (2021) 12:9. doi: 10.3389/fpsyt.2021.613665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.WHO . Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence. Geneva: World Health Organization. (2009). [PubMed] [Google Scholar]
- 34.Akbari H, Roshanpajouh M, Nourijelyani K, Mansournia M-A, Rahimi-Movaghar A, Yazdani K. Profile of drug users in the residential treatment centers of Tehran, Iran. Health Promotion Perspect. (2019) 9:248–54. doi: 10.15171/hpp.2019.34, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Razzaghi EM, Rahimi Movaghar A, Hosseini M, Madani S, Chatterjee A. Rapid situation assessment of drug abuse in Iran. Iranian Welfare Organization and UNDCP. (1999):1998–9. [Google Scholar]
- 36.Narenjiha H, Rafiey H, Baghestani AH, Noori R, Ghafori B, Soleimannia L. Rapid situation assessment of drug abuse and drug dependence in Iran. Circulated report [in Persian], Darius Institute. (2005).
- 37.Narenjiha H, Rafiei H, Baghestani AR, Nouri R, Ghafouri B, Soleimaninia L. Rapid Situation Assessment of Drug Abuse in Iran (year 2007). Tehran: Danjeh Publication; (2009). [Google Scholar]
- 38.Heyman GM. Addiction and choice: theory and new data. Front Psychol. (2013) 4:31. doi: 10.3389/fpsyt.2013.00031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Radfar SR, Sedaghat A, Banihashemi AT, Gouya M, Rawson RA. Behaviors influencing human immunodeficiency virus transmission in the context of positive prevention among people living with HIV/acquired immunodeficiency syndrome in Iran: a qualitative study. Int J Prev Med. (2014) 5:976–83. PMID: [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.


