Abstract
A ventilation timing light (VTL) is a small commercially available single-use device that is programmed to light up at six-second intervals prompting rescuers to provide a single controlled breath during manual ventilation. The device also indicates the duration of the breath by remaining illuminated for the duration of the inspiratory time. The aim of this study was to evaluate the impact of the VTL on a selection of CPR quality metrics.
Methods
A total of 71 paramedic students who were already proficient in performing high-performance CPR (HPCPR) were required to perform HPCPR with and without a VTL. The quality of the HPCPR delivered, reflected by the selected quality metrics; chest compression fraction (CCF), chest compression rate (CCR), and ventilation rate (VR), was then evaluated.
Results
While HPCPR with and without a VTL were both able to achieve guideline-based performance targets of CCF, CCR, and VR, the group who had used the VTL to deliver HPCPR were able to consistently provide 10 ventilations for every minute of asynchronous compressions (10 breath/min vs 8.7 breath/min p < 0.001).
Conclusion
The use of a VTL allows for a VR target of 10 ventilations per minute to be consistently achieved without compromising guideline-based compression fraction targets (>80%), and chest compression rates when used during the delivery of HPCPR in a simulated OHCA event.
Keywords: Ventilation timing light, OHCA, HPCPR, CPR quality, EMS, Paramedic, Ventilation
Introduction and background
The crude incidence of out-of-hospital cardiac arrest (OHCA) in New Zealand (NZ) is 103.2 per 100,000 people per year.1 Averaging at just over 4000 per year, (only 15%) just under two in ten will survive.2 While these figures are comparable with countries with similar health systems.3, 4 strategies to improve cardiac arrest outcomes within the country are still constantly sought, particularly as OHCA in NZ appears to disproportionally affect individuals in the country who are already at risk of poor health status.5
Enhancing the quality of resuscitation that is delivered by the country’s emergency medical services (EMS) to OHCA patients appears to be the cornerstone of attempts to improve survival outcomes in the country.6 The country’s EMS responds to just under 50% of all OHCAs and delivers CPR through a highly choreographed, high-performance CPR (HPCPR) model, likened to a formula-one pit-crew response.6
High-Performance CPR (HPCPR)
HPCPR is very similar to traditional CPR but places more emphasis on maximizing the amount of hands-on chest compression time during a cardiac arrest. It does this by streamlining resuscitative strategies through a simplified, efficient, and choreographed approach that in turn results in rescuers instinctively knowing where to go and what to do during an OHCA.7 In comparison, traditional CPR focuses on defining roles and ensuring proficiency in delivering technical and non-technical skills to aid in the organisation of a chaotic scene. HPCPR also accomplishes this but emphasises the focus on early and continued compressions, minimum interruptions, and ensuring that defibrillation is provided expeditiously when indicated.8, 9 The success of the HPCPR approach is predictably dependent on continuous high-quality training and the ongoing commitment to monitoring performance, remediation, and retraining.7
While each country or EMS system may have its own localised version of HPCPR, there is consensus around the five key components of HPCPR and their respective quality performance targets.8 These include minimising interruptions in chest compressions (i.e., CCF > 80%), providing compressions of adequate rate (i.e., 100–120 pm) and depth (2–2.4 in), avoiding leaning on the chest between compressions, and avoiding excessive ventilations. The American Heart Association 2020 guideline recommend ventilating cardiac arrest patients at a rate of 8 to 10 breaths per minute prior to an advanced airway (endotracheal tube/laryngeal mask airway).10 Despite this, it is reported that 80% of patients still receive ventilation at higher rates and at higher volumes11 with hyperventilation having a risk of causing sudden increases in intrathoracic pressures which impair haemodynamics and lower the chances of survival.12 With this, many devices were introduced into the market and one such device is the ventilation timing light. The addition of the VTL, like with other previously trialled CPR adjuncts, is consistent with strategies that attempt to enhance the constant achievement of HPCPR quality performance targets.13
The ventilation timing light (VTL)
The adult VTL (‘O Two’, Ontario, Canada) used is a small commercially available single-use electrical tool programmed to light up at six-second intervals prompting rescuers to provide a single controlled ventilation using a bag-valve-device (BVD). The VTL also indicates the duration of the breath by remaining illuminated for the duration of the inspiratory time. In theory, the inclusion of the VTL during HPCPR would allow for 10 breaths, each given over a full second, to be delivered while chest compressions are contemporaneously provided.
The VTL and its utility was the focus of this study, particularly when used during HPCPR, as this is yet to be assessed, despite its continued use. Consequently, the primary aim of the study was to evaluate the impact of the VTL on CPR quality as reflected by; ventilation rate (VR), chest compression rate (CCR), and chest compression fraction (CCF). As a sub-aim, the study also examined whether significant associations existed between participant characteristics and their self-reported confidence levels in relation to being able to perform HPCPR and their actual performance, as evaluated in the study.
Methods
The study used a prospective, unblinded cross-over manikin-based design, enrolling paramedic students completing their training at the Auckland University of Technology in New Zealand. Participants who had completed year one of the paramedicine degree program were able to enrol in the study as this ensured proficiency in performing asynchronous HPCPR both with and without a VTL and were able to provide BVD ventilations on a manikin with an advanced airway established.
Participants were randomly paired into double-rescuer teams and then further divided into two randomised clusters where they either started their first scenario in the No-VTL-HPCPR room or in the VTL-HPCPR room. They were advised that as a double-rescuer team, to perform HPCPR in two simulated OHCA scenarios, each lasting eight minutes, with a ten-minute rest break between each scenario. Depending on their randomly assigned cluster, they started by either performing asynchronous double-rescuer HPCPR with a VTL (VTL- HPCPR) or without one (No-VTL-HPCPR) before taking the break and switching over to the alternate room. Approval for the study was granted by the Auckland University of Technology Ethics Committee (AUTEC 21/3), New Zealand.
Study protocol
Following consent, participants were advised that a diagnosis of cardiac arrest had already been confirmed and that all the necessary equipment for the HPCPR scenario were in place and no additional equipment was required. No further instructions or information regarding the interventions was provided to participants. Investigators in both the VTL-HPCPR and No-VTL-HPCPR rooms were required to read from a pre-established script to ensure consistency of instructions given to participants. Participants were asked not to communicate with anyone before the scenario, during the rest period, and up until the study was completed.
Data collection
Both the VTL-HPCPR and No-VTL-HPCPR performances were video-recorded to manually extract data at a later date. Lead researchers (KG, SA and BJ) provided each researcher with a formula and structure for data collection prior to review. Two team researchers independently watched the recording for data match. Any discrepancies were moderated for consistency by KG, SA or BJ. This extraction process required investigators to watch each recording, then calculate and confirm through consensus agreement the exact value for CCR, CCF, and VR across individual performances. CCR was calculated by manually counting every individual chest compression that was performed over each two-minute rotation and then averaging it out over the eight-minute event. Since participants were not required to confirm the cardiac arrest, the event started from the delivery of the first compression (start of the clock) and stopped eight minutes later. CCF was calculated by subtracting the sum of all periods where no compressions were performed from the eight-minute event, while VR was calculated by manually counting every ventilation given over each minute of the CPR cycle.
Statistical analysis
As shown by the Shapiro-Wilk results in Table 2, many of the results were non-normally distributed. Where non-normality was severe, non-parametric models were used to test for differences in results and bootstrapping was used to determine confidence intervals. Wilcoxon signed-rank tests were used to detect differences between VTL-HPCPR and No-VTL-HPCPR performances. One-way ANOVA and Kruskal-Wallis tests were used where appropriate for associations between participant characteristics as well as their self-reported confidence levels in performing HPCPR and their actual HPCPR performance.
Table 2.
Comparison between VTL-HPCPR and No-VTL-HPCPR dependent variables.
| Median | Mean | 95% CI UPPER | 95% CI LOWER | SD | Shapiro-Wilk p | Wilcoxon signed-rank p-value | ||
|---|---|---|---|---|---|---|---|---|
| Chest compressions per minute | No-VTL-HPCPR | 110.3 | 109.9 | 108.6 | 111.3 | 5.5 | 0.1 | 0.9 |
| VTL-HPCPR | 109.5 | 110.1 | 108.6 | 111.6 | 6.2 | 0.07 | ||
| Pairwise difference | 0.2 | −0.1 | −1.3 | 1.0 | 4.9 | 0.8 | ||
| Ventilations delivered per minute | No-VTL-HPCPR | 8.7 | 8.7 | 8.3 | 9.2 | 1.8 | 0.04 | 0.0000005 |
| VTL-HPCPR | 10.0 | 10.0 | 10.0 | 10.0 | 0.1 | 0.00 | ||
| Pairwise difference | −1.3 | −1.3 | −1.7 | −0.9 | 1.8 | 0.03 | ||
| Chest compression fraction achieved (%) | No-VTL-HPCPR | 98.8 | 98.1 | 97.7* | 98.6* | 1.8 | 0.00 | 0.6 |
| VTL-HPCPR | 98.9 | 98.2 | 97.8* | 98.6* | 1.7 | 0.00 | ||
| Pairwise difference | 0.0 | −0.1 | −0.3* | 0.2* | 1.0 | 0.03 |
Note VTL, Ventilation Timing Light; HPCPR, High-Performance Cardiopulmonary Resuscitation.
* Bootstrap CI calculated due to non-normal data.
For 68 participants, Monte Carlo simulation gives an 80% power for the Wilcoxon signed-rank tests at a mean difference of 0.5 standard deviations for the normally distributed results, assuming random pairing. For all characteristics except the frequency of prior training received, most participants fell into two categories, leaving the remaining groups sparsely populated. Characteristic values with n ≤ 5 were manually combined with their nearest neighbour resulting in n ≥ 11 for all groups. Monte Carlo simulation for this minimally balanced grouping gives an 80% power for ANOVA with a mean difference of 0.95 standard deviations, assuming a normal distribution. A p < 0.05 was considered statistically significant in all tests.
Results
In total 68 participants met the inclusion criteria and were enrolled in the study. As indicated in Table 1, females (43) and those aged between 18–25 years (57) made up the largest proportion of participants. While most participants did not have an authority to practice (ATP) (40 vs. 28) which indicated that their only experience with performing HPCPR was during training and supervised mentorships, a notable majority indicated being very confident in performing HPCPR and utilising all the required equipment.
Table 1.
Baseline characteristics of participants as raw and clustered totals.
| Characteristic | Clustered Value | n |
|---|---|---|
| Gender | Male | 25 |
| Female | 43 | |
| Age | 18–25 | 57 |
| 26–45 | 11 | |
| Experience | < 1 year | 31 |
| 1–5 years | 37 | |
| ATP | No | 40 |
| Yes | 28 | |
| Level of Academic Study | 1–2 years | 23 |
| > 2 years | 45 | |
| Frequency of Training Received | Never – Annually | 20 |
| Six-monthly | 21 | |
| Monthly | 15 | |
| Weekly | 12 | |
| Confidence in using a BVD | Very Confident | 41 |
| Somewhat confident - neutral | 27 | |
| Confidence in achieving the CCR targets in CPR | Very confident | 43 |
| Somewhat confident – unconfident | 25 | |
| Confidence in achieving the VR targets in CPR | Very confident | 45 |
| Somewhat confident – Neutral | 23 | |
| Confidence in using a VTL connected to a BVD | Very comfortable | 48 |
| Somewhat confident – unconfident | 20 | |
| Confidence in performing asynchronous HPCPR | Very confident | 45 |
| Somewhat confident – Very unconfident | 23 | |
| Confidence in performing synchronous HPCPR | Very Confident | 45 |
| Somewhat confident – Very unconfident | 23 |
Note: ATP, Authority to Practice; BVD, Bag Valve Device; CCR, Chest Compression Ratio; VTL, Ventilation Timing Light; HPCPR, High-Performance Cardiopulmonary Resuscitation; VR, Ventilation Rate.
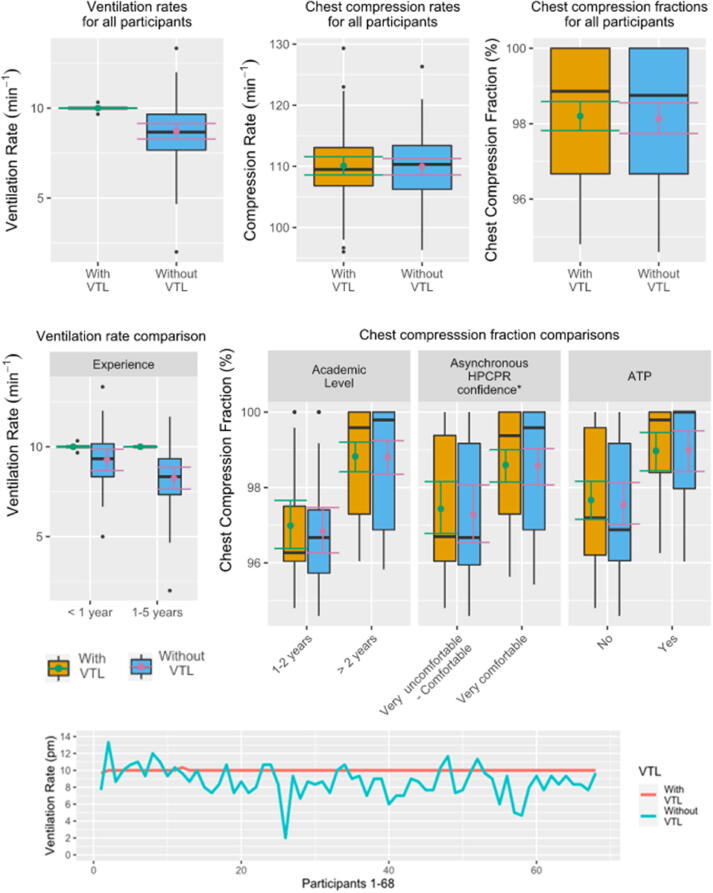
The VTL had a small and nonsignificant impact on the CPR quality metrics; CCR and CCF. As shown in Table 2, the differences in CCR and CCF between the No-VTL-HPCPR and VTL-HPCPR groups were so small that its impact can be considered negligible (CCR 109.9 vs 110.1 and CCF 98.1 vs 98.2). However, the mean VR achieved by the VTL-HPCPR group was significantly higher, and uniformly consistent compared to when the VTL was not used (10.0 vs 8.7p < 0.001) (Fig. 1).
Fig. 1.
Differences in CCF, CCR, and VR during VTL-HPCPR and No-VTL-HPCPR.
In Table 3, predictors of the CCF, CCR, and VR achieved during HPCPR are presented. As shown, the VR delivered in the No-VTL-HPCPR group significantly correlated with gender (p = 0.04) and experience (p = 0.02), while CCF in both the VTL-HPCPR and the No-VTL-HPCPR groups significantly correlated with higher confidence levels, possession of ATP, and being enrolled in year 2 (and above) when performing both synchronous and asynchronous HPCPR.
Table 3.
Associations between participant characteristics and CCF, CCR and VR.
|
No-VTL-CCR |
VTL-CCR |
No-VTL-VR |
No-VTL-CCF |
VTL-CCF |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model | One-way ANOVA |
One-way ANOVA |
One-way ANOVA |
Kruskal-Wallis |
Kruskal-Wallis |
|||||
| Characteristic | η2 | p | η2 | p | η2 | p | ε2 | P | ε2 | p |
| Gender | 0.00 | 0.6 | 0.00 | 0.6 | 0.06 | 0.05 | 0.00 | 0.7 | 0.00 | 0.6 |
| Age | 0.00 | 0.9 | 0.00 | 0.6 | 0.00 | 1 | 0.05 | 0.07 | 0.00 | 0.6 |
| Experience | 0.03 | 0.2 | 0.01 | 0.4 | 0.08 | 0.02 | 0.04 | 0.1 | 0.01 | 0.3 |
| ATP | 0.01 | 0.5 | 0.00 | 0.6 | 0.00 | 0.6 | 0.2 | 0.0008 | 0.1 | 0.002 |
| Academic Level | 0.02 | 0.2 | 0.02 | 0.3 | 0.02 | 0.2 | 0.3 | 0.00004 | 0.3 | 0.00002 |
| Training Frequency | 0.06 | 0.3 | 0.07 | 0.2 | 0.07 | 0.2 | 0.07 | 0.2 | 0.08 | 0.1 |
| BVD Confidence | 0.04 | 0.09 | 0.03 | 0.2 | 0.01 | 0.5 | 0.04 | 0.1 | 0.05 | 0.07 |
| CCR Confidence | 0.01 | 0.4 | 0.01 | 0.4 | 0.01 | 0.5 | 0.2 | 0.001 | 0.1 | 0.006 |
| VTL Confidence | 0.04 | 0.1 | 0.00 | 0.7 | 0.00 | 1 | 0.04 | 0.09 | 0.03 | 0.2 |
| Confidence with asynchronous HPCPR | 0.02 | 0.2 | 0.01 | 0.5 | 0.00 | 0.7 | 0.1 | 0.003 | 0.1 | 0.01 |
| Confidence with synchronous HPCPR | 0.01 | 0.4 | 0.01 | 0.5 | 0.01 | 0.4 | 0.1 | 0.004 | 0.09 | 0.01 |
| Confidence with ventilation | 0.07 | 0.03 | 0.01 | 0.5 | 0.00 | 1 | 0.1 | 0.008 | 0.07 | 0.03 |
Note: ATP, Authority to Practice; BVD, Bag Valve Device; CCR, Chest Compression Ratio; VTL, Ventilation Timing Light; HPCPR, High-Performance Cardiopulmonary Resuscitation; VR, Ventilation Rate; CCF, Chest Compression Fraction.
p values indicate the significance of the association. η2 and ε2 indicate the effect size.
Discussion
Despite not having been investigated before, the VTL has been widely used within the New Zealand pre-hospital environment for several years. Overall, our findings revealed that in this manikin-based HPCPR study, the addition of a VTL to a HPCPR model had an almost negligible impact on the CPR quality metrics CCF and CCR and their respective guideline-based targets (i.e., CCF > 80% and CCR 100 – 120 per min). Whilst not particularly surprising, having the data to support this suspicion is reassuring especially given the setting where the VTL is most likely to be utilised. In contrast, the increase in VR guideline adherence found in the VTL-HPCPR group was statistically significant. Although it does not appear to be a large improvement, given that neither group provided an excessive VR (i.e., > 12), improving consistency and adherence to standards helps to validate the tool, potentially increasing its use in the industry as VR is considered a CPR quality performance metric.14
While at face value the improvements the VTL made may be seen as minor, the design and setting of the study must be considered. To better isolate the effects of the VTL on CPR metrics, many clinical and non-clinical confounders, typically found in a real cardiac arrest were removed. For example, all resuscitation equipment was provided and pre-attached, and there was no defibrillator on the scene, so no charges, analyses, or shocks were required. Participants were instructed when to swap and were not required to investigate the cause of the arrest. Finally, there was no need to locate the patient, carry equipment, consider scene safety, and manage potentially upset or violent bystanders, therefore the psychological burdens EMS face during a typical cardiac arrest were not present. These additional factors can interfere with maintaining CPR quality metrics and in a real-world setting we hypothesise the addition of a VTL to a HPCPR model may play a bigger role in improving CCR, CCF, and VR.15, 16 However, the VTL and its impact on CPR quality metrics is yet to be studied in this setting despite its current use, so no recommendations can be made.
Outside of the real-world setting, the VTL may also provide value to the clinical education space. Delivering safe and guideline specific ventilations to a patient is a delicate yet vital skill for all novice medical professionals. It may also serve as a training tool for experienced professionals to refresh their understanding of ventilation guidelines. With this, the VTL may be used as an adjunct that helps support clinician’s psychomotor skills when developing a structured and accurate ventilation strategy. However, it must be clearly understood that the VTL only truly guides the clinician to a specified ventilation rate and not to a specific volume or ventilation pressure. Though the light illuminates for a set period to guide the length of ventilation, this cannot be relied upon to safeguard the patient from inappropriate tidal volumes being delivered during ventilation.
Limitations
Many of the confounders that are usually associated with real-life EMS-attended OHCAs were absent in this study. Therefore, it is highly possible that HPCPR performance with or without a VTL in a real-life OHCA may be worse than observed in this study. However, because the study was dependent on a high level of uniformity across both rooms’, confounders such as poor lighting, noise, fatigue-inducing activities, and bystander participation were excluded. This was done because pilot studies demonstrated that these factors not only impacted the consistency of the data collection process but also the homogeneity of collected data.
The pilot study further revealed that while the manikin was capable of automatically reporting CCR, VR, chest compression depth, and chest compression recoil, this was only accurate during synchronized CPR with pauses between compressions that allowed for unimpeded ventilations, as permitted in a 30:2 algorithm. As our study required asynchronous CPR to be performed, CCR, CCF, and VR needed to be manually recorded. The manual nature of measuring these variables unfortunately made measuring chest compression depth and recoil impossible. Finally, due to the functional limitations of the equipment used, the tidal volumes and ventilation pressures of each ventilation were unable to be assessed, though the measurement and analyses of these variables will be a future research consideration.
Because of the nature of cross-over studies, there is potential for unblinding when the effects of the intervention subsequently become obvious to the participants. Here, following participation in the first arm of the study, it was expected that participants might have had a carryover effect which may have better prepared them for the cross-over arm of the study. To mitigate this, a stand-down interval between the study crossover provided a ‘washout’ period to minimise any expected carryover effect.
Conclusion
The study’s results indicate that a VTL used during the delivery of HPCPR in a simulated OHCA event allows for a VR target of 10 ventilations per minute to be consistently achieved with negligible impact on CCF and CCR.
CRediT authorship contribution statement
Ben Jones: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Formal analysis, Project administration. Stephen Aiello: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Formal analysis, Visualization. Kevin Govender: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Visualization, Formal analysis, Supervision. Brayden Shaw: Methodology, Writing – review & editing, Data curation, Investigation, Formal analysis. Bruce Tseng: Writing – review & editing, Data curation, Investigation, Formal analysis. Zaid Dawad: Writing – review & editing, Data curation, Investigation, Formal analysis. Mel McAulay: Writing – review & editing, Data curation, Investigation, Formal analysis. Norm Wilkinson: Writing – review & editing, Data curation, Investigation, Formal analysis.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We would like to thank AUT, School of Clinical Sciences for funding the preparation of the paper and Jerome O'Connor for his assistance with the statistical analysis for the project.
References
- 1.Bray J., Howell S., Ball S. The epidemiology of out-of-hospital cardiac arrest in Australia and New Zealand: A binational report from the Australasian Resuscitation Outcomes Consortium (Aus-ROC) Resuscitation. 2022;172:74–83. doi: 10.1016/j.resuscitation.2022.01.011. [DOI] [PubMed] [Google Scholar]
- 2.Dicker B., Davey P., Smith T., Beck B. Incidence and outcomes of out-of-hospital cardiac arrest: A New Zealand perspective. Emerg Med Australas. 2018;30:662–671. doi: 10.1111/1742-6723.12966. [DOI] [PubMed] [Google Scholar]
- 3.Gräsner J.T., Lefering R., Koster R.W., et al. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: A prospective one-month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–195. doi: 10.1016/j.resuscitation.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Hasegawa K., Tsugawa Y., Camargo C.A., Hiraide A., Brown D.F.M. Regional variability in survival outcomes of out-of-hospital cardiac arrest: The All-Japan Utstein Registry. Resuscitation. 2013;84(8):1099–1107. doi: 10.1016/j.resuscitation.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 5.Goodyear-Smith F., Ashton T. New Zealand health system: universalism struggles with persisting inequities. Lancet. 2019;394:432–442. doi: 10.1016/S0140-6736(19)31238-3. [DOI] [PubMed] [Google Scholar]
- 6.Dicker B., Govender K., Howie G., Swain A., Todd V.F. Positive association between ambulance double-crewing and OHCA outcomes: a New Zealand observational study. Resuscitation Plus. 2021;8 doi: 10.1016/j.resplu.2021.100187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eisenberg M.S. University of Washington Press; 2013. Resuscitate! how your community can improve survival from sudden cardiac arrest. [Google Scholar]
- 8.Nolan J.P. High-quality cardiopulmonary resuscitation. Curr Opin Crit Care. 2014;20:227–233. doi: 10.1097/MCC.0000000000000083. [DOI] [PubMed] [Google Scholar]
- 9.Pearson D.A., Nelson R.D., Monk L., et al. Comparison of team-focused CPR vs standard CPR in resuscitation from out-of-hospital cardiac arrest: results from a statewide quality improvement initiative. Resuscitation. 2016;105:165–172. doi: 10.1016/j.resuscitation.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 10.Panchal A.R., Bartos J.A., Cabañas J.G., et al. Part 3: adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142:S366–S468. doi: 10.1161/CIR.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 11.Khoury A., Sall F.S., De Luca A., et al. Evaluation of bag-valve-mask ventilation in manikin studies: what are the current limitations? BioMed Res Int. 2016 doi: 10.1155/2016/4521767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aufderheide T.P., Lurie K.G. Death by hyperventilation: a common and life-threatening problem during cardiopulmonary resuscitation. Crit Care Med. 2004;32:S345–S351. doi: 10.1097/01.ccm.0000134335.46859.09. [DOI] [PubMed] [Google Scholar]
- 13.Obermaier M., Katzenschlager S., Kofler O., Weilbacher F., Popp E. Advanced and Invasive Cardiopulmonary Resuscitation (CPR) Techniques as an Adjunct to Advanced Cardiac Life Support. J Clin Med. 2022;11:7315. doi: 10.3390/jcm11247315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neth M.R., Idris A., McMullan J., Benoit J.L., Daya M.R. A review of ventilation in adult out-of-hospital cardiac arrest. J Am College Emerg Phys Open. 2020;1:190–201. doi: 10.1002/emp2.12065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cordioli R.L., Grieco D.L., Charbonney E., Richard J.C., Savary D. New physiological insights in ventilation during cardiopulmonary resuscitation. Curr Opin Crit Care. 2019;25:37–44. doi: 10.1097/MCC.0000000000000573. [DOI] [PubMed] [Google Scholar]
- 16.Chang M.P., Idris A.H. The past, present, and future of ventilation during cardiopulmonary resuscitation. Curr Opin Crit Care. 2017;23:188–192. doi: 10.1097/MCC.0000000000000415. [DOI] [PubMed] [Google Scholar]